Abstract
The present study examined the association of contextual factors (social and food preparation location) with the energy density of meals and snacks consumed in a sample of young Australian adults (18–30 years old) identified using wearable camera technology. Over three consecutive days, a subsample of young adults wore a wearable camera that captured images in 30 s intervals. Eating episodes from 133 participants were annotated for preparation location and social context (covering social interaction and screen use). Over the same period, participants completed daily 24 h recalls. The nutritional composition of meals and snacks was calculated by matching the items identified in the camera to the 24 h recall using time and date stamps. Self-reported data (weight and height) was used to calculate body mass index and (residential postcode) to assign socio-economic status. The association of context and demographic factors with energy density was determined using a mixed linear regression model employing the bootstrap method with bias-corrected and accelerated. In total, 1817 eating episodes were included in the analysis (n 8 preparation unclear and n 15 food components could not be identified excluded). Food prepared within the home was 1⋅1 kJ/g less energy-dense than other preparation locations. Lunches (CI −1⋅7 to −0⋅3) and dinners (CI −1⋅6 to −0⋅5) were both 1⋅0 kJ/g lower in energy density than breakfasts. Snacks were 3⋅5 kJ/g (CI 2⋅8–4⋅1) more energy-dense than breakfasts. Food prepared outside the home and food consumption during snacking appear to be adversely contributing to energy-dense food intake.
Key words: Dietary assessment, Energy density, Social context, Wearable cameras, Young adults
Introduction
It is estimated that the 38 % of the burden of disease in Australians could be prevented by reducing or avoiding exposure to modifiable risk factors in 2018(1). Of these modifiable risk factors, overweight and obesity was the second highest cause that contributed 8⋅4 % to the burden of disease, this was followed by all dietary risk influences (5⋅4 %)(1). In Australia, young adults are more likely to experience weight gain than any other age group(2) with the proportion affected by overweight or obesity increasing from 39 % in 2014–15 to 46 % in 2017–18 in the National Health Survey(3).
Higher energy density diets have been previously found to be associated with higher odds of obesity(4). Young Australian adults who consumed energy-dense diets had poorer quality diets with fewer fruits and vegetables and more discretionary foods(5). Discretionary foods are defined in the Australian Guide to Healthy Eating (AGHE) as foods that are high in saturated fat, and/or added sugars, and/or salt, and/or low in fibre(6) and in some countries are referred to as energy-dense, nutrient-poor foods. Lower energy density foods tend to be higher in fibre and/or water content and can include fruits and vegetables(7,8). The energy density is the energy content (kJ) per unit of food consumed usually in grams (g). The World Cancer Research Fund (WCRF) recommended average energy density of dietary intake (excluding beverages) should be less than 5⋅23 kJ/g (1⋅25 kcal/g)(9).
Food prepared outside the home (FOH) for the present study is defined as any food item that was not prepared within the home and obtained from another location such as a fast food outlet, café, restaurant, or food from another outlet selling take away food such as a service station or convenience store. FOH tends to be more energy-dense and has higher amounts of nutrients of concern such as saturated fat, sodium and/or added sugars(6,10,11). This is of concern for young Australians who spend the highest proportion of their household income on eating out compared with older adults(12) and more frequently consume fast food than any other age group(13). In the cross-sectional Measuring Young Adult Meals Study (MYMeals) of 1001 Australians conducted from 2017 to 2018, one-third of food and beverages consumed were FOH(14).
Other factors that influence food consumption are social contextual factors including social interactions and screen usage. Social facilitation of eating, that is the observed increase in food intake when people eat in groups rather than when alone(15), has been widely studied. Several mechanisms have been proposed including extension of the time spent eating during social meals(16), larger portion size(17), reduced attention to satiety signals(18) and increased eating rate(19). Social modelling or matching may mediate food choices during social meals, where people modify their intake towards the norm(20). Additionally, the use of screens during mealtimes, such as watching television have previously been found to be associated with increased energy intake(21). Young adults that watched four or more hours of television per day, reported consuming more energy-dense snacks than those that watched less than 1 h of television(22).
Most studies cited above have used self-reported data or have been conducted within laboratory settings. Self-report data is sensitive to misreporting by participants and laboratory assessments may not be reflective of real-world behaviours(23). The use of wearable cameras that enables researchers to passively observe participants in their natural situations may provide new insights on the way food preparation and social contexts may influence dietary intake(24). Wearable cameras have been previously used to examine: contextual influences (including social interactions and the use of media screens) on meals in a sample of 40 adults(25), snacking context (including food source, social contact and screen usage) in children(26), food preparation behaviours in adolescents(27) and the influence of body weight on meal duration in 16 participants(28).
Previous MYMeals camera sub-studies have investigated the dietary habits during transport journeys(29), the identification of omitted foods and beverages from dietary assessment methods(30) and assessment of meals and snacks consumed as healthy versus unhealthy finding most FOH was discretionary food(31). To our knowledge, no studies of substantial scale have used wearable cameras to examine the association of social contexts and food preparation location on nutrients and energy density of dietary intake in young Australian adults.
The present study aimed to examine the impact of the social contexts (screen usage and social interactions), food preparation location and participant characteristics (gender, body mass index (BMI) and socio-economic status (SES)) on dietary energy density in a sample of young Australian adults (18–30 years) using wearable camera technology.
Methods
The MYMeals study was a large, three-day, cross-sectional study on the dietary intake of young Australian adults (18–30 years old) in New South Wales (NSW), Australia. Three days of recording were selected as the minimum to estimate the average food energy intake(32). The full MYMeals study procedure(33) and wearable camera sub-study(30,31) has been previously described in detail with an outline of the procedures provided below. Data were collected between March 2017 and December 2018 and the camera images were annotated between March 2019 and September 2020.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Institution's Human Research Ethics Committee (2016/546) on the 15th of July 2016. Written informed consent was obtained from all subjects/patients.
MYMeals sample population
Participants were recruited across NSW with quotas for geographic location and SES to ensure sampling was from a variety of demographic backgrounds. Self-reported postcode was used to assign participant's geographic location as urban or remote/rural (as defined by the Accessibility/Remoteness Index of Australia(34)) and SES (using the Socio-Economic Indexes for Areas (SEIFA)(35)). The SEIFA index assigns each area a decile for advantage versus disadvantage with lower deciles demonstrating more disadvantage. In the rare event, the participants’ residential postcode did not have an associated SEIFA value (n 2), SES was assigned based on the SEIFA decile of the adjacent postcode area.
Participant eligibility criteria
Prospective participants were eligible to take part in the study if they were within the age range (18–30 years old), lived in NSW, consumed a minimum of one meal, snack or drink purchased outside the home each week, owned or had access to a smart phone and could read and write English. Participants were excluded if they did not meet the eligibility criteria, were pregnant and/or breastfeeding and had ever had an eating disorder.
Recruitment methods
A variety of methods were used to recruit participants including social media, fundraising events by Cancer Council NSW, public bulletin boards, electronic newsletters, letters of invitation using names provided by the Australian Electoral Commission and snowball sampling.
Wearable camera sub-study enrolment procedure
Participants completed the online initial screening questions, provided informed consent and answered the basic demographic questionnaire. The demographic questions included: (i) gender (male, female or prefer not to say); (ii) age (18–24 or 25–30 years); (iii) postcode and (iv) expression of interest to undertake the wearable camera sub-study. Those that indicated willingness to take part in the camera sub-study were randomly selected until a 20 % subsample of the larger MYMeals study was achieved. Participants were contacted by the research team via telephone and briefed about the requirements of the sub-study prior to receiving the camera.
Wearable camera sub-study protocol
Participants were allocated three consecutive days for data collection such that across the study population the start days were distributed to encompass both weekdays and weekends. During the study period, participants: (i) wore a wearable camera and (ii) completed daily 24 h dietary recall interviews with research dietitians. Participants were provided with an Autographer camera and accessories (portable charger, cables, information card, instruction booklet and postage paid satchel), via post mail. The device was to be charged overnight.
The wearable camera had an inbuilt 136° wide angle lens. Participants were instructed to wear the device on the attached lanyard around their neck positioned on their sternum for all waking hours. Therefore, the cameras captured images from the participants’ perspective in a free-living setting and offered researchers a wide field of view capturing the surroundings of the participant which told a detailed story of their everyday life activities, such as food, screens and smartphones on tables or desks and people they dine with. The device was programmed to capture images every 30 s. The frequency of capture mean that a sequence of events is viewed, so for example one can see the person go to the refrigerator and start to cook (or their partner) or can see the packages delivered by food delivery services.
Participants were able to temporarily pause capturing images by (i) taking the camera off or (ii) closing the lens cover. This was done by participants when: (i) privacy was required (i.e. in bathrooms), (ii) on government premises or (iii) in certain settings when they (and/or others) felt uncomfortable being recorded. Participants had the chance to review and delete any private images prior to returning the cameras to the researchers. Upon completion of the three consecutive days, participants returned their cameras to the research team via postage paid mail.
In addition to the camera, participants also completed three 24 h recalls on each of the days directly after the camera collection capturing dietary information retrospectively for the same days that the camera was worn. The Automated Self-Administered 24 h recall Australia (ASA-24 Australia-2016) program was used so the interview process was standardised(36).
Participants received an AU $100 voucher in returning the camera and completion of the end of the study questionnaire that included questions on self-reported weight (kg) and height (cm). Weight and height were used to calculate Body Mass Index (BMI = weight (kg)/height (m2)). This self-reported weight and height have been validated in a previous paper(37).
Data storage
All participant data were de-identified. Upon receiving the returned cameras, captured image data was transferred onto a secure university research data store. Participant demographics, anthropometric information and dietary intake data were stored on REDCap electronic capture tool hosted at the University of Sydney(38,39). Access to the data was restricted to select members of the research team that were briefed on the strict privacy protocols.
Food and snack intake identification using wearable cameras
Through an iterative process, the image coding schedule and manual were generated. A sample coding schedule and a summarised manual have been previously published(31). The expanded version is available by request.
Prior to reviewing image data, the inter-rater reliability for coding was tested. A dataset of 3577 images was coded by an experienced coder (A.D.). Then, another coder who was an Accredited Practising Dietitian coded the data (V.C.). An agreement threshold of 90 % was considered an acceptable inter-rater agreement. Agreement was acceptable for eating episode label (100 %), food types (100 %), screen type (100 %), social interaction (100 %), preparation location (93 %), consumption location (100 %), overall rating (100 %) and meal length (100 %). Henceforth, one coder, V.C., annotated all the images. Not all variables tested were required in the analysis for this study.
To be included in the dataset, a decision was made to only include participants recording a minimum of 8 h of image data per day as compliance was an issue. This period was based on a previous wearable camera study conducted in 2011(40) and has been used in prior wearable accelerometer device studies(41).
All images captured by the wearable cameras were reviewed by the principal coder (V.C.) sequentially based on when they were captured. Consequently, one can use these images to follow the participant as they prepared and/or purchased food to determine the preparation location. The images prior to and while the participant consumed food was used to ascertain social networks of the eating episode.
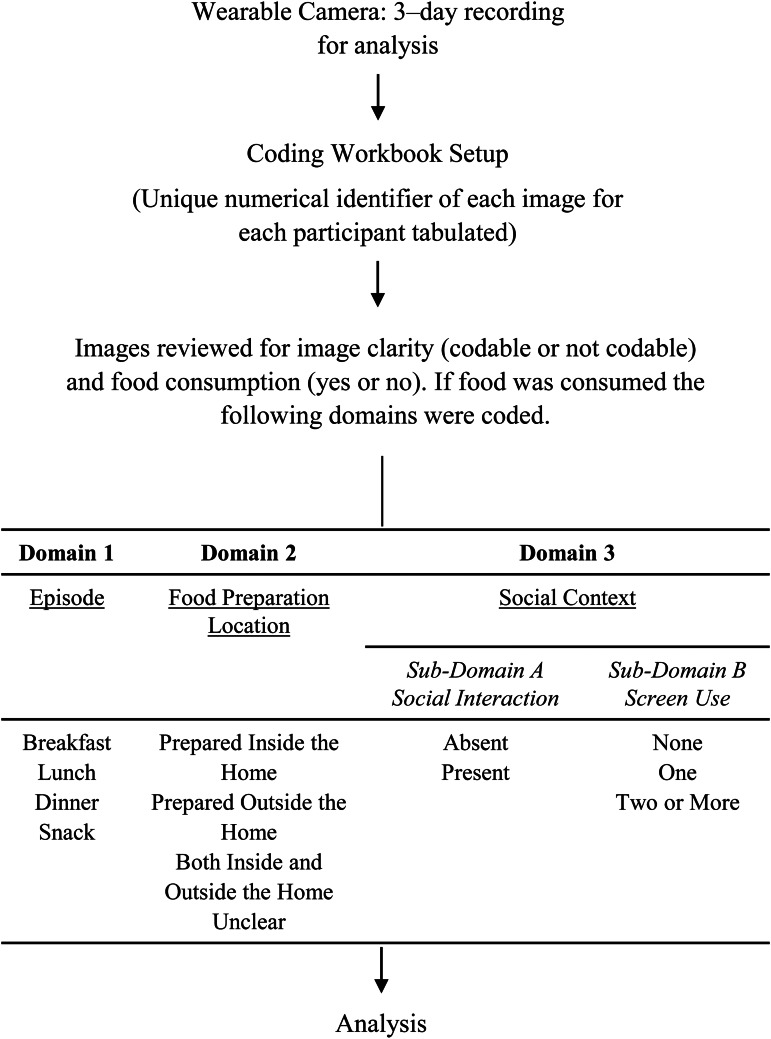
The unique numerical identifiers of the captured images for each participant were firstly tabulated in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) for annotation. Images were then reviewed for the consumption of food (yes or no) and image clarity (codable or not codable) and by an APD (V.C.). If food was consumed three coding domains (domain 1: eating episode, domain 2: food preparation location and domain 3: social contexts) were assessed, as illustrated in Fig. 1.
Fig. 1.
Flow diagram of wearable camera study procedure and image coding protocol.
The first coding domain categorised eating episodes as: breakfast (commonly consumed between time of waking to 11:00); lunch (typically eaten from 12:00 to 15:00); dinner (usually between 18:00 and 21:00) or snack (consumed at any time prior or following any of the main meals). These time-blocks were based on a previous study examining dietary daily energy distribution among Australians(42) but refined to better reflect the dietary habits of this sample based on the visual inspection of time of food intake across the day (Supplementary Appendix S1). The assignment of the eating episodes was guided by the image timestamps, and the type and volume of food consumed (e.g. breakfast cereal).
The second coding domain assessed where the food was prepared: (i) inside the home; (ii) FOH; (iii) both inside and outside the home and (iv) unclear location. Components of meals and snacks were coded individually; therefore, eating episodes could consist of items that were prepared from a combination of inside and outside the home.
Foods prepared inside the home and outside the home were determined from the sequence of images leading to the food consumption. If a meal or snack was observed to be consumed but its preparation location could not be identified, it would be annotated as unclear.
The third coding domain assessed the social context during meal and snack consumption. This domain consisted of the two subdomains: (A) social interactions and (B) screen use.
Subdomain A of the third coding domain was for social interactions during the eating episode. This was coded as a binary: (i) absent or (ii) present. Social interaction was documented as present if the participant was observed from the series of images to interact and converse with another person (or people). This was indicated by evidence of conversation (e.g. changes in facial expression or maintained eye contact with the participant), smiling or other body language (e.g. hugging or hand gestures).
Subdomain B of the third coding domain identified the total number of electronic screens used during the eating episode. Types of screens that could be used by participants could include smart phones, televisions, computers or laptops. Screen use was coded as: (i) none, (ii) one screen present or (iii) two or more screens present. Screen use was documented as present if the participant was observed to interact with a screen (such as touching a smart phone). For example, a participant using a mobile phone and watching television would be coded as two or more screens.
Figure 2 provides an example of coding.
Fig. 2.
Sample image coding with time stamps of images provided in 24 h time. Sample images depicted in panel (a–d). Panel (a) coded as episode: lunch (time stamp: 13:08:52), preparation location: outside the home, social interaction: present and screen use: none. Panel (b) coded as episode: breakfast (time stamp: 09:31:02), preparation location: inside the home, social interaction: absent and screen use: two. Panel (c) coded as episode: dinner (time stamp: 20:15:06), preparation location: inside the home, social interaction: present and screen use: one. Panel (d) coded as not codable.
Nutrition calculation
Data from both the 24 h recall and wearable camera images had time and date stamps that were used to match the dietary intake between the 24 h recall with the wearable camera images. The wearable cameras were the primary source used to identify foods consumed. Previous studies have identified that participants may omit foods during 24 h recalls(30,43). The 24 h recall data was used to quantify the food consumed and the components that cannot be easily verified by the images from the wearable cameras (e.g. cooking oils). The foods reported in the 24 h recall were annotated as: (i) reported/identified by both methods, (ii) not reported in the 24 h recall or (iii) not identified by the wearable camera.
For items labelled as reported/identified in both methods – the nutritional information from the 24 h recall was used to calculate the nutritional composition of meals and snacks. The ASA-24 uses the AUSNUT 2011–13 Food Nutrient Database(44) that was prepared for the Australian Nutrition and Physical Activity Survey (NNPAS). For items not reported in the 24 h recall but identified in the wearable cameras, the most appropriate portion size was assigned using the AUSNUT 2011–13 Food Measures Database(45) or using commercial industry information for packaged items based on the detailed examination of the images. The AUSNUT 2011–13 Food Measures Database contains information on 16 152 commonly reported food measures in the NNPAS 2011–13(45). All portion sizes were assigned by an APD (V.C.) and verified by a second (A.D.). The consumption of food items that were not detected by the wearable camera images but reported in the 24 h recall were excluded from nutritional calculation.
The energy density (kJ/g) of meals and snacks was calculated by summing the total energy content of the food items (kJ) and dividing this by the total volume of food (g) consumed. Beverages were excluded from energy density calculations. The energy density of beverages is relatively low in comparison to food and can therefore disguise the relationship between energy-dense foods and outcomes(46–48). The WCRF diet energy density recommendation of <5⋅23 kJ/g is for food only and has excluded beverages(9).
Statistical analysis
Descriptive statistics (percentage (%) and mean with standard deviations (sd)) were used to summarise sample and camera wear characteristics. Chi-square test was used to determine any differences in demographics (gender, age group, BMI categories and SES) between completers and non-completers. The SES category was reduced to the bottom five deciles categorised as low SES and top five categories as high SES due to the small sample size in some cells.
Medians with interquartile range (IQR) were used to report dietary energy density (kJ) by contextual and demographic factors. Preparation location was reduced to two categories: (i) inside the home or (ii) other (which encompassed FOH and both inside and outside the home) as food prepared both inside and outside the home only occurred for 23 episodes.
A mixed linear regression model was used to investigate the association of energy density (kJ/g) as the outcome with preparation location, social context (social interactions and screen use), eating episode and participant demographics (BMI, SES and gender). Univariate analysis was used to identify factors that significantly contributed to energy density for inclusion in the final model. Significance for entry into the model was set at P = 0⋅05. Reported P-values and confidence intervals for the final model were obtained by the bootstrap method with bias-corrected and accelerated (BCa). The plot of residuals and predicted values was used to check for model assumptions. Data were analysed using SPSS version 25 (IBM Corporation).
Results
Participant characteristics and camera wear times
A total of 216 participants were recruited in the wearable camera sub-study. Participants were excluded from analysis if they: (i) withdrew for personal or employment reasons (n 5); (ii) failed the selection criteria (n 2); (iii) did not complete all 3 days of data collection (n 21); (iv) did not have camera data (n 4); (v) had camera data of less than 8 h per day on one or more of the three consecutive days (n 48) or (vi) had incorrect camera settings (n 3).
The sample comprised 45 % male (55 % female) participants and 55 % of participants were within the 18–24 years group (45 % aged 25–30 years group). Most participants were within the healthy weight range (60 %) with an average BMI of 25⋅1 kg/m2. The remainder of participants was within the underweight (2 %), overweight (25 %) or obese (13 %) weight range. In this sample, 65 % were classified as residing in higher socioeconomically advantaged location and 35 % resided in lower SES areas. Two participants reported postcodes that did not have a designated SEIFA(35) but they were assigned to the SEIFA for adjacent postcode (n 1 higher and n 1 lower).
There was no significant difference between the gender (P = 0⋅726), age group (P = 0⋅939), BMI categories (P = 0⋅924) or SES (P = 0⋅810) of those included in analysis and non-completers (those recruited for the validation study but were excluded).
Participants on average wore the camera for 8⋅6 (sd 1⋅6) h per day and 7 % (35 422 out of the 487 912) of images examined captured food intake. The wearable cameras identified 272 eating episodes (15 %) that were not reported in the 24 h recall. The wearable cameras did not detect 360 eating episodes that were reported by the participants in the 24 h recall. These were excluded from nutritional analysis of the meals as images about preparation location and social contexts were unavailable.
Of the 1840 eating episodes identified using the wearable cameras, 23 episodes (1 %) were excluded from analysis as: (i) the preparation location could not be determined (n 8) or (ii) the component(s) of the meal or snack could not be accurately determined (n 15). A total of 1817 eating episodes were included in analysis: 296 breakfast (16 %), 365 lunch (20 %), 388 (21 %) dinner and 818 snacks (45 %) (Table 1). In 70 % of participants (n 93), the wearable cameras captured the intake of three main meals (breakfast, lunch and dinner) in at least one of the three recording days.
Table 1.
Median (IQR) energy (kJ) and nutrient (g or mg) intake stratified by meal type
| Breakfast | Lunch | Dinner | Snacks | |
|---|---|---|---|---|
| Na | 296 | 365 | 338 | 818 |
| Energy (kJ) | 1346 (854–2004) | 2126 (1347–3181) | 2703 (1835–3895) | 533 (283–1044) |
| Protein (g) | 12⋅5 (7⋅3–19⋅5) | 25⋅2 (14⋅2–40⋅3) | 33⋅6 (19⋅1–51⋅6) | 2⋅5 (1⋅0–6⋅6) |
| Total fat (g) | 10⋅9 (6⋅1–20⋅6) | 20⋅9 (11⋅3–32⋅7) | 26⋅7 (15⋅6–44⋅1) | 5⋅2 (0⋅3–12⋅3) |
| Saturated fat (g) | 3⋅9 (1⋅8–6⋅4) | 5⋅8 (2⋅8–10⋅8) | 8⋅6 (4⋅1–14⋅3) | 1⋅8 (0⋅0–5⋅2) |
| Carbohydrate (g) | 35⋅9 (22⋅0–53⋅1) | 42⋅6 (27⋅1–70⋅8) | 55⋅7 (31⋅4–84⋅6) | 16⋅8 (7⋅5–28⋅7) |
| Fibre (g) | 4⋅0 (2⋅3–6⋅5) | 5⋅8 (3⋅4–8⋅7) | 6⋅7 (3⋅9–10⋅2) | 1⋅0 (0⋅3–2⋅6) |
| Sodium (mg) | 297⋅2 (134⋅1–605⋅4) | 709⋅8 (287⋅1–1385⋅0) | 911⋅5 (328⋅7–1529⋅7) | 55⋅7 (6⋅1–198⋅4) |
Eating episodes are the composite of those captured from all participants and each participant does not contribute the same number of eating occasions.
Nutritional composition of meals and snacks consumed
The nutritional composition of meals and snacks consumed are presented in Table 1. The median energy and most nutrients for meals was highest for eating episodes designated as dinner, followed by lunch, breakfast, and then snacks.
Energy density of meals and snacks
Table 2 shows the energy density (kJ/g) of meals and snacks consumed grouped by preparation location, social context (social interactions and screen use) and participant characteristics (BMI, SES and gender) stratified by meal type. Snacks were more energy-dense (13⋅1 kJ/g) than the main meals (breakfast 7⋅8 kJ/g, lunch 7⋅5 kJ/g and dinner 7⋅2 kJ/g). Food prepared inside the home was lower in energy density across all meal types when compared with other preparation locations. Those participants classified with obesity consumed more energy-dense food when compared with any other weight classification. Energy density of meals and snacks were similar if social interactions were present or absent, the participants SES and gender.
Table 2.
Median (IQR) energy density (kJ/g) of eating episodes stratified by meal type and by contextual and personal factors
| N | Breakfast (kJ/g) | Lunch (kJ/g) | Dinner (kJ/g) | Snacks (kJ/g) | |
|---|---|---|---|---|---|
| Total energy density | 1817 | 7⋅8 (4⋅7–11⋅9) | 7⋅5 (5⋅4–10⋅0) | 7⋅2 (5⋅7–9⋅6) | 13⋅1 (4⋅4–18⋅1) |
| Preparation location | |||||
| Other | 546 | 9⋅3 (7⋅6–15⋅4) | 8⋅6 (6⋅4–12⋅7) | 8⋅9 (6⋅6–13⋅3) | 13⋅5 (8⋅0–21⋅2) |
| Inside the home | 1271 | 7⋅3 (4⋅7–16⋅3) | 6⋅8 (5⋅0–14⋅0) | 6⋅4 (5⋅2–13⋅4) | 12⋅5 (3⋅9–24⋅6) |
| Social interaction | |||||
| Absent | 1107 | 7⋅9 (4⋅7–16⋅1) | 7⋅4 (5⋅3–13⋅1) | 6⋅8 (5⋅4–12⋅8) | 13⋅0 (3⋅9–23⋅5) |
| Present | 710 | 7⋅2 (5⋅1–16⋅3) | 7⋅8 (5⋅6–14⋅0) | 7⋅4 (5⋅9–13⋅6) | 13⋅4 (7⋅0–22⋅1) |
| Screen use | |||||
| None | 707 | 8⋅0 (4⋅5–16⋅7) | 8⋅0 (6⋅2–12⋅8) | 7⋅5 (5⋅8–13⋅2) | 13⋅5 (6⋅0–22⋅1) |
| One | 774 | 7⋅8 (4⋅9–16⋅1) | 7⋅8 (5⋅0–14⋅0) | 7⋅1 (5⋅9–13⋅6) | 12⋅4 (4⋅8–22⋅7) |
| Two + | 336 | 7⋅6 (5⋅3–16⋅1) | 6⋅5 (4⋅7–13⋅8) | 6⋅6 (5⋅2–13⋅2) | 11⋅9 (3⋅8–25⋅2) |
| Body mass index | |||||
| Underweight or normal | 1190 | 7⋅8 (4⋅7–16⋅3) | 7⋅1 (5⋅2–13⋅8) | 6⋅7 (5⋅3–13⋅8) | 12⋅1 (3⋅9–22⋅9) |
| Overweight | 398 | 7⋅2 (5⋅2–14⋅7) | 7⋅0 (5⋅3–14⋅0) | 7⋅5 (5⋅9–12⋅5) | 13⋅5 (7⋅5–22⋅1) |
| Obese | 229 | 9⋅8 (4⋅9–15⋅6) | 9⋅3 (7⋅5–11⋅9) | 8⋅9 (6⋅6–13⋅3) | 14⋅8 (9⋅5–22⋅1) |
| Socio-economic statusa | |||||
| Lower | 623 | 6⋅3 (4⋅5–16⋅8) | 8⋅7 (6⋅1–12⋅5) | 7⋅1 (5⋅5–12⋅5) | 13⋅5 (5⋅3–22⋅1) |
| Higher | 1194 | 8⋅6 (5⋅2–15⋅9) | 7⋅0 (5⋅0–14⋅0) | 7⋅2 (5⋅8–13⋅8) | 12⋅5 (4⋅0–23⋅5) |
| Gender | |||||
| Male | 775 | 8⋅0 (5⋅2–15⋅6) | 8⋅0 (6⋅1–13⋅8) | 7⋅8 (6⋅0–13⋅2) | 12⋅2 (3⋅9–22⋅1) |
| Female | 1042 | 7⋅6 (4⋅5–16⋅3) | 7⋅1 (5⋅0–13⋅1) | 6⋅7 (5⋅5–13⋅8) | 13⋅4 (5⋅2–22⋅9) |
Socio-economic status (SES) was assigned using the Socio-Economic Indexes for Areas (SEIFA)(35). SEIFA index assigns each area a decile for disadvantage versus advantage with lower deciles demonstrating more disadvantage. The SES category was reduced to the bottom five SEIFA deciles categorised as low SES and top five SEIFA deciles as high SES due to the small sample size in some cells.
Modelling food preparation and social context factors on energy density of eating episodes
Univariate mixed linear regression model identified food preparation location, screen use, BMI and eating episode as significantly associated with energy density and were included in the final model (Table 3). Food prepared within the home was 1⋅1 kJ/g lower in energy density than items of FOH (P = 0⋅001). The energy density of all food consumed at eating episodes with two or more screens present was 0⋅8 kJ/g lower than those with no screens (P = 0⋅028). Participants classified with obesity consumed more energy-dense food (1⋅2 kJ/g) than those classified as underweight or of a normal weight range (P = 0⋅001). Lunches (P = 0⋅007) and dinners (P = 0⋅003) were both 1⋅0 kJ/g less energy-dense than breakfast. However, snacks were 3⋅5 kJ/g more energy-dense than breakfast (P = 0⋅001). Social interactions, SES and gender were not significantly associated with energy density of food consumed.
Table 3.
Final mixed linear regression model on the influence of preparation location, social context (screen use), body mass index (BMI) and eating episode on energy density (kJ/g). Reported estimate, P-values and confidence intervals for the model were obtained by the bootstrap method with BCa (bias-corrected and accelerated)
| Variable | Estimate | P-value | 95 % Confidence interval |
|---|---|---|---|
| Preparation location | |||
| Other (Ref) | 0⋅0 | ||
| Inside the home | −1⋅1 | 0⋅001 | −1⋅5 to −0⋅7 |
| Social context – Screen use | |||
| None (Ref) | 0⋅0 | ||
| One | −0⋅2 | 0⋅542 | −0⋅7 to 0⋅4 |
| Two or more | −0⋅8 | 0⋅028 | −1⋅6 to −0⋅1 |
| Eating episode | |||
| Breakfast (Ref) | 0⋅0 | ||
| Lunch | −1⋅0 | 0⋅007 | −1⋅7 to −0⋅3 |
| Dinner | −1⋅0 | 0⋅003 | −1⋅6 to −0⋅5 |
| Snacks | 3⋅5 | 0⋅001 | 2⋅8 to 4⋅1 |
| Body mass index | |||
| Underweight or normal (Ref) | 0⋅0 | ||
| Overweight | 0⋅1 | 0⋅577 | −0⋅5 to 0⋅7 |
| Obese | 1⋅2 | 0⋅001 | 0⋅6 to 1⋅8 |
Discussion
The present study indicates that where food is prepared is a key determinant of energy density. Home-cooked food had a lower energy density than that prepared in commercial kitchens outside home. The energy density also differed by meal or snack episode with snacks at high likelihood of being energy-dense. Eating with others did not appear to be associated with consuming more energy-dense meals but using multiple screens at the time of eating was associated with lower meal energy density. Dinner meals had the highest median energy and nutrients out of all meal types and have previously identified to be the largest meal of the day(49).
Our findings about the importance of home meal preparation are in agreement with a previous study conducted in young people from the UK (16–25 years), that identified that food sourced from home environments had lower energy densities and convenience outlets and retail bakers had higher energy densities(11). High energy density diets have been shown to be associated with higher amounts of discretionary foods in young Australians including foods like sweet biscuits and cakes(4,5). Previous analysis of the complete data of the MYMeals study of 1001 young Australians found that approximately one-third of food and beverage intake was FOH but contributed to more than 40 % of total energy intake(14). Our qualitative analysis of this subsample also identified that most FOH was likely to be discretionary in nature(31). In a study of 1710 young adults in the US (18–23 years), it was reported more frequently preparing food within the home was associated with lower intake of fast food and was more likely to meet dietary objectives(50). However, young adults often reported time constraints, low confidence and motivation to cook as key barriers to preparing food more frequently at home(50). Combined with the societal trend to consume FOH(51), encouraging young adults to prepare their food at home may only be part of the solution and improved education that facilitates healthier choices when dining out is necessary.
Individual meal episodes were significantly associated with energy density and are a potential avenue for public health intervention. The median daily energy density in the present study was 7⋅3 kJ/g and exceeded the WCRF recommendations of 5⋅23 kJ/g(9). Our findings are similar to the secondary analysis of the NNPAS 2011–12 that found the mean energy density of young Australians to be 7⋅4 kJ/g(5). We identified that snacking episodes were of the greatest concern with an energy density 2⋅5 times more than that recommended(9). In a sample of 104 265 French inclusive of all adult age groups (>18 years), snacks were found to be more energy-dense than main meals(52). Snacks are frequently consumed by young adults, with 88 % of Australians aged 19–30-year-old reporting snacking(53). Snacks contributed to 45 % of all eating episodes identified in the present study. A study of Scottish young people (18–25 years) reported that 60 % of their participants consumed at least four ‘unhealthy’ snacks per day(54). A wearable camera study conducted in New Zealand children (11–13 years) found most snacks involved discretionary items(26). Snacking frequency has been previously associated with overweight/obesity in Australian adults (>19 years)(55). This is of particular concern for young Australians as they are more likely to gain weight than any other age range(2).
Previous studies have linked screen use such as television watching with heightened risk of overweight and obesity in US adults (18–75 years)(56), poorer quality diets in adolescents(57) and increased energy intake in young people (5–24 years)(21). A study conducted in Canadian university students (18–25 years) found that those who viewed more than 4 h of television per day consumed more energy-dense snacks than those watching less than 1 h(22). However, in the present study, we found food consumed with two or more screens in use was lower in energy density than when no screens were used. It is possible that the impact of screens may be different according to device types. A Brazilian survey of 1897 adults (>18 years) examined the association of diet and changes in screen time by device type during the COVID-19 pandemic. They identified that increased time spent using the computer was negatively associated with intake of sweetened foods, whereas increased television and mobile phone usage were associated with higher consumption of sweetened foods(58). The authors hypothesised that these findings may be related to differences in device types used during different tasks, computers may be more frequently used for work or study(58). Our previous study found no association of screen use with diet quality, but it should be noted we only studied the presence or absence of screens and not the number, device type in use nor the task performed(31). A longitudinal study of 4013 Australian children that examined behaviours during screen use, found that passive forms of screen use (including watching television) were negatively associated with health outcomes such as waist circumference, whereas educational screen time (such as using computers for homework) was not associated with health outcomes(59). The interaction between screen use and task might be a mediator for the effects of screens on the quality of food consumed and should be included in future research in young adults.
We found no association between social interaction and the dietary energy density. This is consistent with our previous qualitative study of social interaction on diet quality(31) and another Australian study of young adults (18–30 years) reporting social environments were not associated with diet quality(60). The influence of social interactions is complex and may be dependent on the dietary habits of the other individuals present. Social modelling has been a widely studied mechanism that has been proposed to influence dietary intake during social mealtimes. In social modelling, individuals adapt both their food intake and choices to be similar to those around them(20). A study conducted in female Dutch university students (16–31 years) identified participants were likely to have a higher intake of vegetables when exposed to a high vegetable intake peer(61). In a study with a convenience sample recruitment of adults, it was reported that when purchasing FOH, participants purchased lunches that reflected the choice of the customer ordering ahead of them(62). For the present study, we only examined the presence or absence of social interactions. More detailed relationship data between the participant and other(s) present in the images were also coded, however was not included in analysis due to the inability of wearable cameras to be able to categorise all relationship types without confirmation from the participant (e.g. who is a flatmate and who is a friend). To better utilise wearable camera technology to explore the influence of social context on eating behaviours, participants could be asked to confirm relationships observed in the images. Future studies could simultaneously employ ecological momentary assessment (EMA) or retrospectively have participants assist with annotation of social interactions. EMA has been previously employed to measure social context during family mealtimes in real time(63) and to examine the situational characteristics during meal times in young adults (18–23 years)(64).
The present study found that participants classified as obese consumed meals and snacks that were higher in energy density than those categorised as being underweight or normal BMI. Dietary energy density has been previously found to be associated with increased odds of overweight and obesity in a US sample of adult females (30–59 years)(65) and Australian young adults (18–30 years)(4). A study examining the snacking behaviours of 10 092 English adults (29–64 years) found that those classified as overweight and obese were more likely to snack on energy-dense foods such as sweets, chocolates and ice-creams than participants within the normal BMI range(66). The promotion of healthier snacking habits through education and social marketing campaigns targeting young adult populations may be influential in reducing energy density.
In the present study, participant gender and SES were not associated with energy density. Young Australian males residing in lower SES areas have been previously found to be more likely to follow a dietary pattern that was higher in energy density(4). Secondary analysis of the Australian NNPAS 2011–12 of females (18–39 years) did not find an association between energy density and SES(67). Lower energy density diets may contain more fruits and vegetables(5) and are higher in fibre and/or water content(7,8). However, the association of gender and SES with energy density may not have been observed in this study as young Australians are overall low consumers of fruits and vegetables, with only 15 % meeting national dietary guidelines for fruits and vegetables(68).
A key strength of this present study is the use of wearables cameras that enabled researchers to passively observe the social contexts and food preparation location of meals and snacks. The use of wearable cameras can reduce limitations such as misreporting when using self-reported data collection methods that rely on memory and may be affected by social desirability. One previous study showed under-reporting of dietary energy intake that might have resulted from memory lapse could be reduced by 8 % for men and 6 % for women with the use of cameras(43). A second study indicated discretionary snacks were among the top foods not reported in a 24 h recall and perhaps that could be related to social desirability(30). Additionally, as the image data was time and date stamped, we were able to bring together the novel wearable camera assessment of context with traditional quantitative dietary data from the 24 h recall, shedding new light on the ways young adults consume food.
A limitation of the present study is that the camera did not identify all food consumed by participants and may not have captured all the social contexts during an eating episode. These may have been missed as participants could temporarily turn off the wearable cameras due to privacy reasons or if other people (during social interactions) did not feel comfortable having their images captured. Additionally, we included participants with a minimum 8 h of recording each day but acknowledge this may be insufficient to capture all meals and snacks. The eating episodes that were not detected in the wearable cameras but reported by the participants in the 24 h were excluded from analysis as there was no food preparation, social interaction nor screen use data. The impact of these missed meals is expected to be minimal as our study aimed to examine the associations between energy density per meal type rather than total daily energy and/or nutrient intake. However, it does indicate that a wearable camera does not immediately solve the complexities of collecting dietary assessment data for full nutrient analysis and needs to be accompanied by a traditional method such as 24 h recall. Despite advising participants to undertake their normal activities, like most dietary assessment methods participants may have modified their activities during the study period. Beverages were not included in analysis as the energy density of beverages is lower than food and can obscure the impact of energy density on outcomes(46,47). A previous study identified that the contribution of energy and nutrients of concern such as sodium, saturated fat and sugars to total daily intake from independent food outlets was greater than chain outlets in the young adult population(14). While specific preparation locations were coded (i.e. fast food outlets), they were not examined because the sample sizes were too small for some cells for additional analysis.
The use of wearable camera data to assess some of the associations in this study is opportunistic and not based on power calculations and as such influences of SES and gender may not be detected. Image coding was both labour and time-intensive process that took over 18 months to perform for this study and wearable cameras are not suggested for large studies. However, images have been demonstrated as a useful prompt for participants’ memory using more traditional dietary assessment methods such as the 24 h recall(43). In the present study, the wearable cameras identified an additional 272 eating episodes that were not reported in the 24 h recall. Developments in artificial intelligence that allows machine recognition of food in images and for automated or semi-automated image coding will be important for more widespread use of wearable cameras in dietary assessment. However, the angle of image capture remains problematic for food identification in some cases and the privacy request of others may restrict data capture.
Future studies could also employ more discrete cameras that may improve camera wear time and capture potential missed eating episodes and social contexts during eating episodes. The time-blocks used to guide the labelling of eating episodes was based on research conducted on all Australians (>2 years) using the older National Nutrition Survey 1995(42). To be more appropriate for this young adult sample (18–30 years), these time-blocks were refined by reviewing mealtime distributions. Therefore, the assignment of eating episodes (breakfast, lunch, dinner or snack) was crude but sufficient to show the energy density of foods consumed when prepared within the home or FOH. Research to confirm these time-blocks and the involvement of participants in characterising eating episodes, food preparation location, screen use and social interactions may assist coding of information. Longer battery life for video recording or capturing images with shorter time intervals may also be able to capture small quick bites that are consumed faster than the 30 s image capture interval used in this study.
In conclusion, food preparation location and meal episodes were significantly associated with the energy density of food consumed by young Australian adults. Young Australians should be encouraged to make more home-cooked meals but also be enabled to make healthier choices when they inevitably consume FOH. Snacks were the most energy-dense meal type and could be targeted for change in future programs. As screens were frequently used during eating episodes, social media could be an avenue to deliver public health interventions. The use of wearable cameras enabled researchers to simultaneously review food intake, food preparation location, social interactions and screen use. However, wearable cameras are not recommended to be used as the sole method of assessing total daily energy and nutrient intake.
Acknowledgements
The authors acknowledge the assistance of Korina Richmond for study administration, Ryan Gage and Louise Signal who provided advice on coding methods and the technical assistance of (Jim Matthews) the Sydney Informatics Hub, a Core Research Facility of the University of Sydney and all investigators of the MYMeals Study.
This research was funded by a competitive peer-reviewed Linkage Grant from the Australian Research Council (75 %) and Cancer Council NSW (who provided 25 %) LP150100831. V. C. and A. D. are funded by the Australian Government research training program (PhD scholarship).
Conceptualisation: M. A.-F. and L. W.-C.; methodology: V. C., A. D., L. W.-C. and M. A.-F.; analysis: V. C. and M. A.-F.; writing—original draft preparation: V. C. and M. A.-F.; writing—review and editing: A. D. and L. W.-C.; funding acquisition: M. A.-F. All authors have read and agreed to the published version of the manuscript.
L. W.-C. is employed by Cancer Council NSW which co-funded the grant. M. A.-F. has received funding from NHMRC, ARC and NSW Health. V. C. and A. D. do not have any conflicts of interest to report.
Ethics approval was obtained by the Institution's Human Research Ethics Committee (2016/546) on the 15th of July 2016.
Informed consent was obtained from all subjects involved in the study.
Informed consent for publication was obtained from all subjects involved prior to the commencement of the study.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/jns.2022.76.
click here to view supplementary material
References
- 1.Australian Institute of Health and Welfare (2021) Australian Burden of Disease Study: Impact and Causes of Illness and Death in Australia 2018. Canberra: Australian Institute of Health and Welfare. [Google Scholar]
- 2.Allman-Farinelli MA, Chey T, Bauman AE, et al. (2008) Age, period and birth cohort effects on prevalence of overweight and obesity in Australian adults from 1990 to 2000. Eur J Clin Nutr 62, 898–907. [DOI] [PubMed] [Google Scholar]
- 3.Australian Bureau of Statistics (2018) 4364.0.55.001 - National Health Survey: First Results. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release (accessed 12 August 2021).
- 4.Livingstone KM, Sexton-Dhamu MJ, Pendergast FJ, et al. (2022) Energy-dense dietary patterns high in free sugars and saturated fat and associations with obesity in young adults. Eur J Nutr 61, 1595–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grech A, Rangan A & Allman-Farinelli M (2017) Social determinants and poor diet quality of energy-dense diets of Australian young adults. Healthcare 5, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Health and Medical Research Council (2013) Australian Dietary Guidelines. https://www.eatforhealth.gov.au/guidelines (accessed 12 August 2021).
- 7.Drewnowski A & Specter S (2004) Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 79, 6–16. [DOI] [PubMed] [Google Scholar]
- 8.Vernarelli JA, Mitchell DC, Rolls BJ, et al. (2018) Dietary energy density and obesity: how consumption patterns differ by body weight status. Eur J Nutr 57, 351–361. [DOI] [PubMed] [Google Scholar]
- 9.World Cancer Research Fund/Institute for Cancer Research (2007) Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective (Summary). Washington, DC: World Cancer Research Fund/Institute for Cancer Research. [Google Scholar]
- 10.Wellard-Cole L, Davies A & Allman-Farinelli M (2021) Contribution of foods prepared away from home to intakes of energy and nutrients of public health concern in adults: a systematic review. Crit Rev Food Sci Nutr, 62, 1–12. [DOI] [PubMed] [Google Scholar]
- 11.Tyrrell RL, Greenhalgh F, Hodgson S, et al. (2016) Food environments of young people: linking individual behaviour to environmental context. J. Public Health 39, 95–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Australian Bureau of Statistics. 6530.0 - Household Expenditure Survey, Australia: Summary of Results 2015–16. https://www.abs.gov.au/statistics/economy/finance/household-expenditure-survey-australia-summary-results/latest-release.
- 13.Mohr P, Wilson C, Dunn K, et al. (2007) Personal and lifestyle characteristics predictive of the consumption of fast foods in Australia. Public Health Nutr 10, 1456–1463. [DOI] [PubMed] [Google Scholar]
- 14.Wellard-Cole L, Davies A, Chen J, et al. (2021) The contribution of foods prepared outside the home to the diets of 18- to 30-year-old Australians: the MYMeals study. Nutrients 13, 1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Castro JM & De Castro ES (1989) Spontaneous meal patterns of humans: influence of the presence of other people. Am J Clin Nutr 50, 237–247. [DOI] [PubMed] [Google Scholar]
- 16.De Castro JM (1990) Social facilitation of duration and size but not rate of the spontaneous meal intake of humans. Physiol Behav 47, 1129–1135. [DOI] [PubMed] [Google Scholar]
- 17.Ruddock HK, Long EV, Brunstrom JM, et al. (2021) People serve themselves larger portions before a social meal. Sci Rep 11, 11072–11072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herman CP, Roth DA & Polivy J (2003) Effects of the presence of others on food intake: a normative interpretation. Psychol Bull 129, 873–886. [DOI] [PubMed] [Google Scholar]
- 19.De Castro JM (1994) Family and friends produce greater social facilitation of food intake than other companions. Physiol Behav 56, 445–445. [DOI] [PubMed] [Google Scholar]
- 20.Cruwys T, Bevelander KE & Hermans RCJ (2015) Social modeling of eating: a review of when and why social influence affects food intake and choice. Appetite 86, 3–18. [DOI] [PubMed] [Google Scholar]
- 21.Marsh S, Ni Mhurchu C & Maddison R (2013) The non-advertising effects of screen-based sedentary activities on acute eating behaviours in children, adolescents, and young adults. A systematic review. Appetite 71, 259–273. [DOI] [PubMed] [Google Scholar]
- 22.Thomson M, Spence JC, Raine K, et al. (2008) The association of television viewing with snacking behavior and body weight of young adults. Am J Health Promot: AJHP 22, 329–335. [DOI] [PubMed] [Google Scholar]
- 23.Althubaiti A (2016) Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc 9, 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doherty AR, Hodges SE, King AC, et al. (2013) Wearable cameras in health: the state of the art and future possibilities. Am J Prev Med 44, 320–323. [DOI] [PubMed] [Google Scholar]
- 25.Gemming L, Doherty A, Utter J, et al. (2015) The use of a wearable camera to capture and categorise the environmental and social context of self-identified eating episodes. Appetite 92, 118–125. [DOI] [PubMed] [Google Scholar]
- 26.Gage R, Girling-Butcher M, Joe E, et al. (2020) The frequency and context of snacking among children: an objective analysis using wearable cameras. Nutrients 13, 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raber M, Patterson M, Jia W, et al. (2018) Utility of eButton images for identifying food preparation behaviors and meal-related tasks in adolescents. Nutr J 17, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alshurafa N, Zhang S, Romano C, et al. (2021) Association of number of bites and eating speed with energy intake: wearable technology results under free-living conditions. Appetite 167, 105653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davies A, Chan V, Bauman A, et al. (2020) Using wearable cameras to monitor eating and drinking behaviours during transport journeys. Eur J Nutr. 60, 1875–1885. [DOI] [PubMed] [Google Scholar]
- 30.Chan V, Davies A, Wellard-Cole L, et al. (2021) Using wearable cameras to assess foods and beverages omitted in 24 hour dietary recalls and a text entry food record App. Nutrients 13, 1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chan V, Wellard-Cole L, Davies A, et al. (2022) The association of social and food preparation location context with the quality of meals and snacks consumed by young adults: findings from the MYMeals wearable camera study. Eur J Nutr. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Basiotis PP, Welsh SO, Cronin FJ, et al. (1987) Number of days of food intake records required to estimate individual and group nutrient intakes with defined confidence. J Nutr 117, 1638–1641. [DOI] [PubMed] [Google Scholar]
- 33.Wellard-Cole L, Jung J, Kay J, et al. (2018) Examining the frequency and contribution of foods eaten away from home in the diets of 18- to 30-year-old Australians using smartphone dietary assessment (MYMeals): protocol for a cross-sectional study. JMIR Res Protoc 7, e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Australian Bureau of Statistics (2011) 1270.0.55.005 - Australian Statistical Geography Standard (ASGS): Volume 5 - Remoteness Structure.
- 35.Australian Bureau of Statistics (2018) Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA). http://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 (accessed 15 January 2021)
- 36.Park Y, Dodd KW, Kipnis V, et al. (2018) Comparison of self-reported dietary intakes from the automated self-administered 24-h recall, 4-d food records, and food-frequency questionnaires against recovery biomarkers. Am J Clin Nutr 107, 80–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davies A, Wellard-Cole L, Rangan A, et al. (2020) Validity of self-reported weight and height for BMI classification: a cross-sectional study among young adults. Nutrition 71, 110622. [DOI] [PubMed] [Google Scholar]
- 38.Harris PA, Taylor R, Minor BL, et al. (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95, 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harris PA, Taylor R, Thielke R, et al. (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42, 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doherty AR, Caprani N, Conaire CÓ, et al. (2011) Passively recognising human activities through lifelogging. Comput Hum Behav 27, 1948–1958. [Google Scholar]
- 41.Ruiz JR, Ortega FB, Martínez-Gómez D, et al. (2011) Objectively measured physical activity and sedentary time in European adolescents: the HELENA study. Am J Epidemiol 174, 173–184. [DOI] [PubMed] [Google Scholar]
- 42.Fayet F, Mortensen A & Baghurst K (2012) Energy distribution patterns in Australia and its relationship to age, gender and body mass index among children and adults. Nutrition & Dietetics 69, 102–110. [Google Scholar]
- 43.Gemming L, Rush E, Maddison R, et al. (2015) Wearable cameras can reduce dietary under-reporting: doubly labelled water validation of a camera-assisted 24 h recall. Br J Nutr 113, 284–291. [DOI] [PubMed] [Google Scholar]
- 44.Food Standards Australia New Zealand. AUSNUT 2011-13 Food Nutrient Database. https://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/ausnutdatafiles/Pages/foodnutrient.aspx
- 45.Food Standards Australia New Zealand. AUSNUT 2011-13 Food Measures Database. https://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/ausnutdatafiles/Pages/foodmeasures.aspx.
- 46.Hebestreit A, Börnhorst C, Pala V, et al. (2014) Dietary energy density in young children across Europe. Int J Obes 38, S124–S134. [DOI] [PubMed] [Google Scholar]
- 47.Johnson L, Wilks DC, Lindroos AK, et al. (2009) Reflections from a systematic review of dietary energy density and weight gain: is the inclusion of drinks valid? Obes Rev 10, 681–692. [DOI] [PubMed] [Google Scholar]
- 48.Vernarelli JA, Mitchell DC, Rolls BJ, et al. (2013) Methods for calculating dietary energy density in a nationally representative sample. Procedia Food Sci 2, 68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sui Z, Raubenheimer D & Rangan A (2017) Exploratory analysis of meal composition in Australia: meat and accompanying foods. Public Health Nutr 20, 2157–2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Larson NI, Perry CL, Story M, et al. (2006) Food preparation by young adults is associated with better diet quality. J Am Diet Assoc 106, 2001–2007. [DOI] [PubMed] [Google Scholar]
- 51.Venn D, Banwell C & Dixon J (2017) Australia's evolving food practices: a risky mix of continuity and change. Public Health Nutr 20, 2549–2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hassen WS, Castetbon K, Tichit C, et al. (2018) Energy, nutrient and food content of snacks in French adults. Nutr J 17, 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fayet-Moore F, McConnell A, Petocz P, et al. (2021) Contribution of dietary snacking behaviours to discretionary energy intake and anthropometric measures in Australian adults: a comparison using an objective vs subjective definition for snacking. Nutr Diet 78, 154–164. [DOI] [PubMed] [Google Scholar]
- 54.Poobalan AS, Aucott LS, Clarke A, et al. (2014) Diet behaviour among young people in transition to adulthood (18–25 year olds): a mixed method study. Health Psychol Behav Med 2, 909–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leech RM, Worsley A, Timperio A, et al. (2018) The role of energy intake and energy misreporting in the associations between eating patterns and adiposity. Eur J Clin Nutr 72, 142–147. [DOI] [PubMed] [Google Scholar]
- 56.Kegler MC, Hermstad A & Haardörfer R (2021) Home food environment and associations with weight and diet among U.S. Adults: a cross-sectional study. BMC Public Health 21, 1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fulkerson JA, Loth K, Bruening M, et al. (2014) Time 2 tlk 2nite: use of electronic media by adolescents during family meals and associations with demographic characteristics, family characteristics, and foods served. J Acad Nutr Diet 114, 1053–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tebar WR, Christofaro DGD, Diniz TA, et al. (2021) Increased screen time is associated with alcohol desire and sweetened foods consumption during the COVID-19 pandemic. Front Nutr 8, 630586–630586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sanders T, Parker PD, del Pozo-Cruz B, et al. (2019) Type of screen time moderates effects on outcomes in 4013 children: evidence from the longitudinal study of Australian children. Int J Behav Nutr Phys Act 16, 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sexton-Dhamu MJ, Livingstone KM, Pendergast FJ, et al. (2021) Individual, social–environmental and physical–environmental correlates of diet quality in young adults aged 18–30 years. Appetite 162, 105175. [DOI] [PubMed] [Google Scholar]
- 61.Hermans RCJ, Larsen JK, Herman CP, et al. (2009) Effects of social modeling on young women's nutrient-dense food intake. Appetite 53, 135–138. [DOI] [PubMed] [Google Scholar]
- 62.Christie CD & Chen FS (2018) Vegetarian or meat? Food choice modeling of main dishes occurs outside of awareness. Appetite 121, 50–54. [DOI] [PubMed] [Google Scholar]
- 63.Bell BM, Alam R, Abu Sayeed M, et al. (2022) Validity and feasibility of the monitoring and modeling family eating dynamics system to automatically detect in-field family eating behavior: observational study. JMIR MHealth UHealth 10, e30211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Laska MN, Graham D, Moe SG, et al. (2011) Situational characteristics of young adults’ eating occasions: a real-time data collection using personal digital assistants. Public Health Nutr 14, 472–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hartline-Grafton HL, Rose D, Johnson CC, et al. (2009) Energy density of foods, but not beverages, is positively associated with body mass index in adult women. Eur J Clin Nutr 63, 1411–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.O'Connor L, Brage S, Griffin SJ, et al. (2015) The cross-sectional association between snacking behaviour and measures of adiposity: the fenland study, UK. Br J Nutr 114, 1286–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Latter R, Brown LJ, Rae KM, et al. (2020) The role of socio-economic status and energy-density in Australian women of child-bearing age. J Hum Nutr Diet 33, 718–728. [DOI] [PubMed] [Google Scholar]
- 68.Nour M, Sui Z, Grech A, et al. (2017) The fruit and vegetable intake of young Australian adults: a population perspective. Public Health Nutr 20, 2499–2512. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/jns.2022.76.
click here to view supplementary material