Abstract
Introduction
Compared with other medical specialties, there are lower numbers of female trainees and lower rates of flexible working in gastroenterology. This study aims to examine the experience of male and female trainees to understand specialty demographics and the experience of training.
Methods
Gastroenterology training data were obtained from the British Society of Gastroenterology (BSG) trainee surveys from 2014, 2018 and 2020, and from the Royal College of Physicians Medical Workforce unit between 2011 and 2019. Data on endoscopy measures from 2011 to 2021 were obtained from the Joint Advisory Group (JAG) on gastrointestinal endoscopy, including the JAG Endoscopy training system and the National Endoscopy Database. Data were segregated and compared by gender.
Results
The percentage of female gastroenterology trainees remains at around 40%, largely unchanged over the previous decade. From the BSG trainee survey, 29.5% of women have flexible working patterns compared with 2.6% of men (p<0.001), which is lower than other medical specialties. Less than half of female trainees felt confident about their job prospects once they qualify. A greater proportion of male than female trainees achieved provisional colonoscopy certification during training (55% vs 45%, p=0.005) and female trainees took longer to certify than male trainees (63 months vs 56 months, p=0.004). The total length of training time from primary medical qualification to consultancy was the same for men and women.
Conclusion
Changes must be addressed from a national and institutional level to address equitable access to national training programmes and equality of outcome for male and female trainees.
Keywords: colonoscopy, endoscopic procedures, endoscopy
Summary box.
What is already known about this subject?
Workforce data indicate that the majority of UK gastroenterologists receiving a certificate of completion of training are male, and that there are fewer females working in gastroenterology than in comparable medical specialties.
What are the new findings?
Female trainees were more likely to have flexible working patterns than men, but the proportion of trainees working flexibly remains lower than in other specialties.
Female trainees are less confident than male trainees about their job prospects once they qualify.
A greater proportion of male trainees achieved provisional colonoscopy certification during training and female trainees took longer to certify than male trainees.
How might it impact on clinical practice in the foreseeable future?
The needs of flexible working trainees need to be considered when developing endoscopy training programmes to ensure equitable progression to independence.
Due to increased demand for female endoscopists, women should be supported to certify in colonoscopy.
Both male and female trainees need adequate support throughout their training to ensure they have the confidence and practical skills to obtain their desired consultancy post.
Introduction
It is well known that there are gender disparities in medicine, with women underrepresented at trainee and consultant level and in leadership roles.1 2 This is more prominent in interventional fields, such as surgery and gastroenterology.3 Female medical students have outnumbered men for the past 25 years,4 with 55% currently female, but only 36.6% of consultants are women.5 The British Society of Gastroenterology (BSG) 2020 Workforce Report identified that of 1607 gastroenterology and hepatology consultants in the UK, 22% are female.1 Although this has increased from 13% in 2007, gastroenterology is the second highest male-dominated medical specialty, behind cardiology with 18% female consultants, suggesting there are perceived barriers for female gastroenterology trainees which need to be actively addressed.
Founded in 1937, the BSG resembled a ‘gentleman’s club’ in its earliest iterations, and to date has had only two female presidents out of 65.6 In 2014, the BSG launched a new initiative entitled ‘Supporting Women in Gastroenterology (SWiG)’ with the aim of identifying problems in recruitment and raising awareness of the challenges facing women in gastroenterology.7 However, there are still limited data regarding whether the experience of UK gastroenterology training is different for men and women. The aim of this study was to identify whether there are gender differences in terms of trainees’ working pattern, endoscopy training, interest in academia and subspecialty preference.
Methods
Study population and design
Data were obtained from BSG trainee survey responses from 2014, 2018 and 2020. Information on the number of trainees working flexibly, academic roles, out of programme (OOP), subspecialty preference, confidence in role, perceived barriers to training and self-reported endoscopy measures were analysed for gender differences. Where possible, answers were collated from all three surveys.
Endoscopy data were obtained from the Joint Advisory Group on Gastrointestinal Endoscopy (JAG); specifically, data entered into the JAG Endoscopy training system (JETS) and the National Endoscopy Database (NED). We analysed gender differences in time from commencing colonoscopy training to accreditation, number of procedures performed annually and the proportion of men and women performing advanced endoscopic procedures such as endoscopic retrograde cholangiopancreatography (ERCP) between 2011 and 2021. A freedom of information (FOI) request was made in 2019 of acute trusts in England, collecting data on number of physicians performing ERCP, broken down into gender.
The Royal College of Physicians (RCP) Medical Workforce Unit (MWU) annually surveys physicians who have gained their Certificate of Completion of Training (CCT) in the previous year. Data were obtained from the RCP MWU regarding the proportion of male and female trainees within each specialty between the 2011 and 2019, and the proportion of trainees working flexibly.
Statistical analysis
Data were analysed using Prism (Graphpad V.9) and Microsoft Excel 2019 (Microsoft, Redmond, Washington, USA). Categorical variables and ordinal data were summarised using counts and percentages and analysed using χ2 and Student’s t-test. Continuous data are presented as means and SD if normally distributed or medians and interquartile ranges otherwise. Multiple means were compared by one-way analysis of variance. A p<0.05 was considered to be statistically significant.
Results
Gender ratios and working patterns
There were 257, 293 and 345 trainees that responded to the BSG trainee surveys in 2014, 2018 and 2020, giving response rates of 32.6%, 48.1% and 50.2%, respectively. The percentage of female gastroenterology trainees in the UK were 37% (95/256), 37% (106/287) and 40% (137/339) in 2014, 2018 and 2020, respectively. These figures are consistent with RCP data, which stated that 29.6% of new gastroenterology CCT holders were female between 2011 and 2019, increasing to 34.1% from 2017. From RCP MWU data, only cardiology has a smaller proportion of female new CCT holders, (48/300, 14.5%) over the same period.
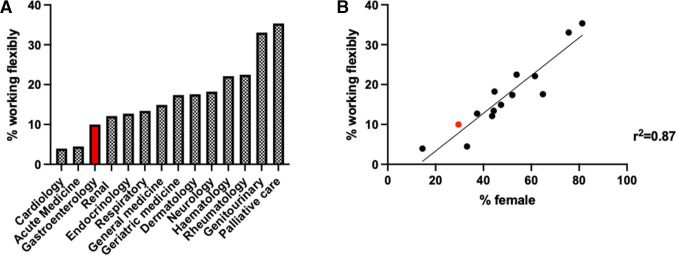
In 2020, 29.5% female BSG training survey respondents worked flexibly compared with 2.6% of men (p<0.001). Over the 2011–2019 RCP census period, 33.7% female gastroenterologists had flexible working patterns at some point in their training, with no responding male gastroenterologist having trained flexibly. Gastroenterology was among the three specialties with the lowest rates of flexible training (figure 1A). Although not possible to segregate data by gender, the proportion of female trainees in a given medical specialty was strongly correlated with flexible working (figure 1B). The mean time from primary medical qualification (PMQ) to CCT was 12.7 years for male trainees (SD 2.37 years) and 12.8 years for females (SD 2.44 years).
Figure 1.
(A) Percentage of flexible working trainees by specialty 2011–2019. Gastroenterology (highlighted in ref) has the third lowest proportion of flexible working trainees. (B) Specialties with a greater proportion of female trainees are more likely to see higher rates of flexible working (simple linear regression, r2=0.87).
Subspecialty interest and confidence
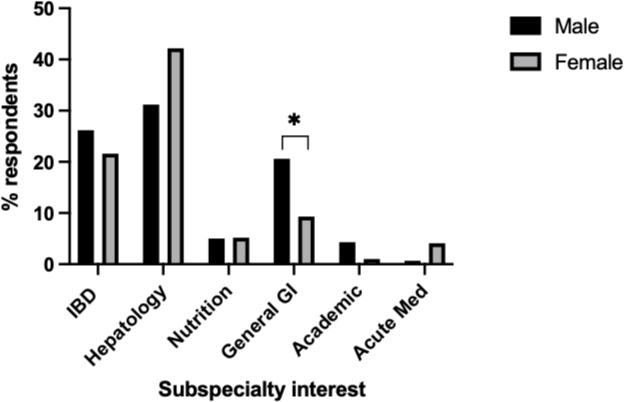
Men were more likely to state an intent to pursue a career in general gastroenterology than women (20.6% M vs 9.3% F, p=0.02). More female than male trainees reported an interest in hepatology, but this did not reach significance (42.2% F vs 31.2% M, p=0.08) (figure 2). There was no gender difference in subspecialty preference for inflammatory bowel disease (26.2% M vs 21.6% F, p=0.42), nutrition (5.2% M vs 5.4% F, p=0.95) or academia (4.3% M vs 1.0% F, p=0.15). A greater proportion of men than women stated confidence in their job prospects on qualification (51% vs 44%, p=0.02).
Figure 2.
Gender differences in reported subspecialty interest by UK gastroenterology trainees in 2014 and 2018. Men were more likely than women to report an intention to pursure a career in general gastroenterology (20.6% vs 9.3%, p=0.02). *denotes P < 0.05. GI, gastrointestinal; IBD, inflammatory bowel disease.
Endoscopy skills training
A total of 959 gastroenterology trainees were listed on JAG records between 2011 and 2021, of which 68.9% (661) were male and 31.1% (298) were female. A total of 499 trainees recorded provisional colonoscopy certification during this time. A greater proportion of male trainees (364/661, 51%) achieved provisional certification than females (135/298, 45.3%); p=0.005. Female trainees took longer to certify than males (62.9 months (IQR 9.1–143.2 months) vs 55.7 months (6.7–189.7 months), p=0.004). Training time was not adjusted for flexible working, as these data are not held by JAG. In 2019, the mean number of oesophago-gastro-duodenoscopies (OGDs) documented by male and female trainees were 31 and 36 (p=0.43), and 30 vs 30 (p=1.00), respectively, for colonoscopies. Of 267 practitioners (trainees and consultants) undertaking ERCP in 2019 listed via NED, 91.7% (245) were male and 8.3% (22) were female. From the FOI request, 109 acute trusts responded reporting 341 consultants performing ERCPs, of which 19 (5.3%) were women.
Academia and OOP
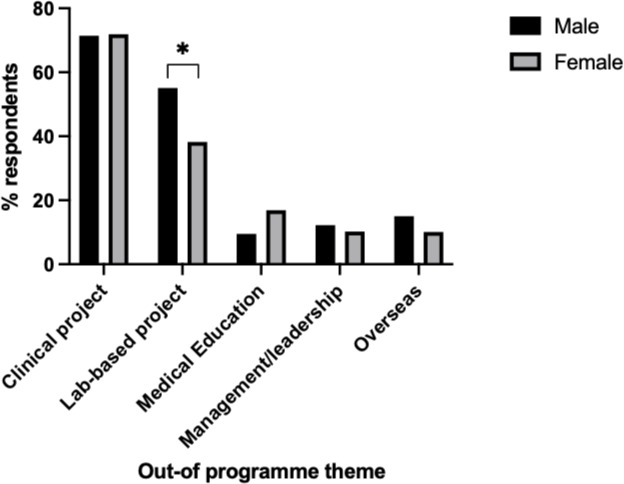
There was no gender difference in the proportion of trainees undertaking academic training, with 9/106 (8.49%) females in academic training vs 13/179 (7.26%) of males. There were no differences in perceived barriers to arranging OOP (32.5% M vs 39% F) or academic clinical training (76.7% M vs 76.7% F). Of trainees taking time OOP, males were more likely than females to undertake a lab-based project (55.1% vs 38.2%, p=0.01) (figure 3). There were no other significant differences in OOP theme by gender.
Figure 3.
Gender differences in type of out of programme undertaken by UK gastroenterology trainees in 2014 and 2018. Men were more likely than women to undertake a laboratory-based project (55.1% vs 38.2%). *denotes p < 0.05.
Discussion
We report key gender differences in working patterns between men and women in gastroenterology. There was a significant difference between the proportion of men and women working flexibly. This is consistent with recent reports from the BSG and RCP, demonstrating that only 14% gastroenterology consultants and 20% of female trainees work flexibly.1 2 Compared with other medical specialties in which 42% of female consultants and 25% of female trainees work flexibly, there is a marked discrepancy in gastroenterologists’ working patterns.2 However, the findings are similar to surveys of UK surgical trainees, in which 18% of women reported working flexibly,8 and to other procedural medical specialties such as cardiology. This suggests that specialties involving procedural competencies pose particular challenges to flexible working, such as the lack of adjustment made for annual JAG procedural targets for part-time endoscopists.9
We were unable to ascertain the reasons for trainees’ working patterns, although previous medical workforce surveys give childcare responsibilities as the primary reason.10 While the introduction of shared parental leave (SPL) has enabled fathers to take longer periods of paternity leave,11 women are still more likely than men to take on a greater proportion of childcare responsibility, either through personal choice (including the choice to breastfeed), cultural expectations or financial considerations.12 Studies have shown very low uptake for SPL, with only 2%–8% of eligible men applying.11 Despite differences in working patterns between males and females, the length of training from PMQ to CCT was the same. Given the higher proportion of female trainees working flexibly, this suggests that male trainees may be spending longer than women in career-enhancing OOP activities.
While a majority of trainees across all specialties report a desire to work flexibly, there is hesitation due to perceived negative attitudes.13 In a study of UK-based surgical trainees, over half received undermining workplace behaviour regarding their decision to work flexibly and a majority felt information provided regarding logistics was inadequate.8 American surveys of gastroenterologists highlight fears that those who work flexibly will be taken less seriously than their full-time colleagues, with the additional fear of losing key training opportunities, particularly endoscopy.14 15 With gastroenterologists reporting the highest burnout rates of any physician specialty in the UK,2 facilitating and increasing the acceptability of flexible working could benefit both male and female trainees, and enable more men to take an active role in early years childcare.
Despite no difference in the number of procedures performed per year, women take longer to accredit in colonoscopy than men, with a greater proportion of men certifying in colonoscopies by the end of training compared with women. Further research is needed to understand if this is directly related to parental leave; gaps in procedural training leading to setbacks in skill acquisition; or merely a representation of an overall longer training period as a result of flexible training. Previous surveys have indicated that many trainees use annual leave and ‘off’ days to undertake ad hoc endoscopy training,16 but this may be more difficult for trainees with caring responsibilities. The expectation for trainees to ‘catch up’ on leave days may also contribute to high burn-out rates.
A very low proportion of women are undertaking advanced endoscopy; the FOI report suggests that only 5% of the UK ERCP workforce are female. In the USA, 24.7% of female fellows plan to pursue advanced endoscopy compared with 37.5% of male fellows.17 Women were more likely to be deterred by perceived gender bias, family planning, lack of flexible hours, fertility/pregnancy risks from radiation and lack of ergonomic equipment.17 18 An absence of same-sex mentors and the lack of visibility of female endoscopists at national conferences/courses were also cited as barriers.3 17–19 Women also face unique physical challenges in endoscopy. Endoscopy dials come in standard sizes which may be better suited to the male hand19 and there are concerns about radiation exposure for women of childbearing age.17 19 20 Nonetheless, there is a high demand for female colonoscopists with many female patients expressing a preference for a same-sex endoscopist. This is particularly prevalent in South Asian and Islamic cultures.3 21 It is important, therefore, to ensure that the different needs of female trainees are taken into account to ensure equity of access to endoscopy training to provide the endoscopy workforce most suited to patients’ needs.
Although there were no differences in the proportion of male and female trainees undertaking academic training, or expressing a career interest in academic gastroenterology, women still struggle for academic representation. Of the 15 BSG guidelines published between January 2019 and December 2021, only one (6.7%) had a woman listed as first author; three (20%) were listed as senior authors. Only two of thirteen (15.4%) BSG section committees have female chairs, excluding SWiG. 13% female representation has been reported at BSG Council and Executive level from 2013 to 2015, with poor attendance at conferences, as well as under-representation in delivery of named lectures and prizes awarded.22 There is evidence suggesting that women have been disadvantaged by inequalities in obtaining fellowship/research funding, with reported success rates of 41.8% male vs 15.1% female applicants in 2007, though improvements were seen in 2016 (41.9% M vs 35.9% F).23 Encouragingly, of the 24 current BSG trainee committee members, 9 (37.5%) are female.
Finally, less than half the women surveyed in 2018 felt confident in their job prospects at time of qualification, although confidence was also low among male trainees. This suggests that current UK gastroenterology training is not adequately equipping either men or women to feel confident in obtaining their desired consultant post. Harvey et al examined factors influencing successful UK consultant applications, finding that female gender (66.2% F vs 57.6% M, p<0.001) and flexible working vs full time training (65.5% vs 61.5%, p=0.022) were more likely to be associated with successful consultant appointment (Personal communication, Philip Harvey). This suggests that neither female gender nor working flexibly are disadvantageous in the long term; or it may suggest that a select cohort of women have learnt to compensate for systemic inequities, by obtaining additional achievements enabling them to be recognised alongside their male counterparts. Regardless, trainees’ low confidence should be addressed by providing greater support to both male and female trainees to help overcome perceived barriers and challenges. Early career mentorship has been shown to be a helpful tool, with a scheme launched through SWiG in 2018 offering mentor-matching for men and women.7
We show little change in gender breakdown of trainees over a ten-year era, although this may reflect the fact that training takes a minimum of 5 years, and for individual trainees who take parental leave or time OOP, training may be considerably longer. The same trainee may, therefore, be recorded at different time points in workforce and survey data. Our study is limited by responder bias from voluntarily completed surveys. Although response rates have increased over the years, this does not represent a complete picture of training experience. It has also been reported that women are more likely to respond to online surveys than men,21 meaning that women’s experience of training may be over-represented. While JETS represents the largest available worldwide endoscopy training database, this information is based on self-reported data. Training/accreditation by year of training is not captured by JETS or NED, nor do we have access to granularity in the data that would allow tracking of an individual’s training journey. ERCP NED data were not a mandatory upload over the study time period, so may not provide a complete insight.
We highlight the lack of information regarding gender differences in gastroenterology, particularly with regard to the journey of flexible working trainees. As in other medical specialties, feminisation of the workforce is likely to lead to increased demand for flexible working patterns. While this will be a challenge to workforce planning in the medium term, it also represents an opportunity to address what have historically been unsustainable practices, contributing to high levels of burn-out. Increased acceptability of flexible working will benefit men as well as women, and has been explicitly supported by the BSG in its 2021 Position Statement on Flexible Working.24 In order to ensure national training programmes serve trainees who wish to work flexibly, we believe there are key data to be collected on the current trainee journey, which is summarised in box 1.
Box 1. Summary of missing data, and proposed solutions to move towards gender equity in training.
Missing data: What more do we need to understand about the current gastroenterology training experience?
What are the reasons for trainees requesting flexible working?
What proportion of trainees would wish to work flexibly if there were no perceived barriers to them doing so?
What percentage of full-time equivalent working do flexible trainees do?
What proportion of men and women take parental leave during higher specialty training (HST)? How many periods of parental leave are typically taken during training?
What is the average length of parental leave for men and women?
At what stage during HST do trainees request flexible working? Do training commitments influence trainees’ family planning?
Do trainees continue to work flexibly for the remainder of their training? What proportion return to a full-time role?
What proportion of male and female trainees relinquish their training number?
How can we achieve equity in training?
-
Role modelling:
Regional flexible working representatives to assist with requests for flexible working and workforce planning
Awareness of gender representation on conference and society committees; avoidance of the ‘manel’.
National and international support groups for under-represented trainees, for example, supporting women in gastroenterology.
Mentoring—personalised support and coaching for trainees
-
Culture change:
Creating an environment in which there is zero tolerance for gender-based discrimination.
Training for all department staff to effectively and respectfully challenge gender-based microaggressions.
Tackle negative perceptions of flexible/‘part-time’ trainees as less committed.
Awareness that flexible working can benefit trainees of all genders in terms of physical and mental health, family responsibilities and other caring roles.
Remove expectation that additional training must be taken during leave periods to achieve key competencies.
-
Technical:
Investment in medical equipment suited to the typically smaller female frame.
Provision of equipment within department to meet needs of individual trainees, for example, stools to allow scoping whilstwhile in the later stages of pregnancy, foot stools for shorter trainees assisting in endoscopy.
In conclusion, while there is limited evidence of improvement in female representation over time, this has not kept pace with representation across other medical specialties. Recognising and acknowledging gender inequity in gastroenterology training is the first step in understanding that the additional challenges faced by female trainees impede their ability to deliver high-quality care to patients, and take away the collective strength that diversity and inclusion brings to the profession. Changes now need to come from a national and institutional level to ensure equality of outcome for both male and female trainees.
Footnotes
Twitter: @sonika_sethi, @dr_dee_kumar, @Phil_Harvey1, @Charl0tteRutter
Contributors: SS wrote the first draft of the manuscript. AK and JC developed the concept, analysed the results and made critical revisions of the manuscript. PH, SR, RH and SAR collated the data and helped analyse the results. MJB, CSR and HS were involved with critical revisions of the manuscript. All authors approved the final manuscript and AK and JC take equal ownership as guarantors of the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: AK and JC are trainee associate editors for MJB has received grants and travel expenses from Vifor International and Tillotts Pharma, outside of the submitted work. HS has received travel and conference expenses from Tillotts Pharma, Norgine, MSD, Abbvie and Janssen outside of the submitted work. CSR has received travel and conference expenses and course sponsorship from Norgine, Nutricia, Shire, Takeda, Astellas and Dr Falk outside of the submitted work
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1. Rutter C. British Society of gastroenterology Workforve report 2021, 2021. Available: https://www.bsg.org.uk/wp-content/uploads/2021/05/British-Society-of-Gastroenterology-Workforce-Report-2020.pdf
- 2. Focus on physicians: 2018-2019 census (UK consultants and higher specialty trainees), 2021. Available: https://www.rcplondon.ac.uk/projects/outputs/focus-physicians-2018-19-census-uk-consultants-and-higher-specialty-trainees
- 3. Kamani L, Hooft JEV. Rising trend of women in gastroenterology: a paradigm shift. J Coll Physicians Surg Pak 2021;31:121–2. 10.29271/jcpsp.2021.02.121 [DOI] [PubMed] [Google Scholar]
- 4. Moberly T. Men outnumber women three to one in some specialties. BMJ 2018;363:k4098. 10.1136/bmj.k4098 [DOI] [PubMed] [Google Scholar]
- 5. The state of medical education and practice in the UK 2019, 2019. Available: https://www.gmc-uk.org/-/media/documents/somep-2019-full-report_pdf-81131156.pdf?la=en&hash=B80CB05CE8596E6D2386E89CBC3FDB60BFAAE3CF
- 6. Delamothe T. British Society of gastroenterology: golden jubilee. BMJ 1987;295:622. 10.1136/bmj.295.6599.622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith KH, Hallett RJ, Wilkinson-Smith V, et al. Results of the British Society of gastroenterology supporting women in gastroenterology mentoring scheme pilot. Frontline Gastroenterol 2019;10:50–5. 10.1136/flgastro-2018-100971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harries RL, Gokani VJ, Smitham P, et al. Less than full-time training in surgery: a cross-sectional study evaluating the accessibility and experiences of flexible training in the surgical trainee workforce. BMJ Open 2016;6:e010136. 10.1136/bmjopen-2015-010136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Joint Advisory Group on GI Endoscopy (JAG) . JAG accreditation programme guide to meeting the quality and safety standards, 2019. [Google Scholar]
- 10. Lachish S, Svirko E, Goldacre MJ, et al. Factors associated with less-than-full-time working in medical practice: results of surveys of five cohorts of UK doctors, 10 years after graduation. Hum Resour Health 2016;14:62. 10.1186/s12960-016-0162-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chris Barrell, S.H., shared parental leave, I.a.S. department for business, editor. 2013: London..
- 12. Jolly S, Griffith KA, DeCastro R, et al. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med 2014;160:344–53. 10.7326/M13-0974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Amy Illsley AO-B, Sutherland R, McLeod A. Less than full time training: the trainee perspective, 2019. Available: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Fwww.rcpe.ac.uk%2Fsites%2Fdefault%2Ffiles%2Fltft_report_final.pdf&clen=883805&chunk=true
- 14. Zimmermann EM. How to foster academic promotion and career advancement of women in gastroenterology. Gastroenterology 2019;157:598–601. 10.1053/j.gastro.2019.07.041 [DOI] [PubMed] [Google Scholar]
- 15. Singh A, Burke CA, Larive B, et al. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol 2008;103:1589–95. 10.1111/j.1572-0241.2008.01976.x [DOI] [PubMed] [Google Scholar]
- 16. Clough J, FitzPatrick M, Harvey P, et al. Shape of training review: an impact assessment for UK gastroenterology trainees. Frontline Gastroenterol 2019;10:356–63. 10.1136/flgastro-2018-101168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. David YN, Dixon RE, Kakked G, et al. Gender-Specific factors influencing Gastroenterologists to Pursue careers in advanced endoscopy: perceptions vs reality. Am J Gastroenterol 2021;116:539–50. 10.14309/ajg.0000000000001112 [DOI] [PubMed] [Google Scholar]
- 18. Yu JX, Berzin TM, Enestvedt B, et al. Gender disparities in advanced endoscopy fellowship. Endosc Int Open 2021;9:E338–42. 10.1055/a-1311-0899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shukla R. Current challenges facing women in gastroenterology: how do we move forward? ACG Case Rep J 2016;3:144–5. 10.14309/crj.2016.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Suzuki H. Balancing act: the need for work style reform for young and/or female Gastroenterologists. Dig Dis Sci 2020;65:1–2. 10.1007/s10620-019-05871-5 [DOI] [PubMed] [Google Scholar]
- 21. Shah DK, Karasek V, Gerkin RD, et al. Sex preferences for colonoscopists and GI physicians among patients and health care professionals. Gastrointest Endosc 2011;74:122–7. 10.1016/j.gie.2011.02.014 [DOI] [PubMed] [Google Scholar]
- 22. Brooks AJ, Taylor EJ, Arthurs EA, et al. Gender differences in leadership, workforce and scholarly presentation within a national Society: a gastroenterology perspective. Frontline Gastroenterol 2019;10:2–6. 10.1136/flgastro-2018-100981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McFarlane M, Bhala N, China L, et al. Attitudes to out-of-programme experiences, research and academic training of gastroenterology trainees between 2007 and 2016. Frontline Gastroenterol 2019;10:57–66. 10.1136/flgastro-2018-100993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. British Society of gastroenterology position statement on flexible working, 2021. Available: https://www.bsg.org.uk/workforce-reports/british-society-of-gastroenterology-position-statement-on-flexible-working/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.