Abstract
Introduction
The efficacy of azithromycin to prevent exacerbation for non-cystic fibrosis bronchiectasis remains controversial. We conduct this meta-analysis to explore the influence of azithromycin versus placebo for the treatment of non-cystic fibrosis bronchiectasis.
Methods
We have searched PubMed, EMbase, Web of science, EBSCO, and Cochrane library databases through July 2019 for randomized controlled trials (RCTs) assessing the efficacy of azithromycin versus placebo for non-cystic fibrosis bronchiectasis. This meta-analysis was performed using the random-effect model.
Results
Four RCTs were included in the meta-analysis. Overall, compared with control group for non-cystic-fibrosis bronchiectasis, azithromycin treatment was associated with improved free of exacerbation (odd ratios [OR] = 3.66; 95% confidence interval [CI] = 1.69–7.93; P = 0.001), reduced pulmonary exacerbations (OR = 0.27; 95% CI 0.13–0.59; P = 0.001) and number of pulmonary exacerbations (standard mean difference [SMD] = − 0.87; 95% CI − 1.21 to − 0.54; P < 0.00001), but demonstrate no obvious impact on forced expiratory volume in 1 s (FEV1), score on St George’s respiratory questionnaire, nausea or vomiting, adverse events.
Conclusions
Azithromycin is effective to prevent exacerbation of non-cystic fibrosis bronchiectasis.
Keywords: Azithromycin, Non-cystic fibrosis bronchiectasis, Exacerbation, Randomized controlled trials
Introduction
Bronchiectasis is featured by the inflammation and remodeling of bronchial wall, and is regarded as the end result of multiple diseases [1–3]. The inflammation mechanism is an exaggerated and uncontrolled neutrophilic responses which is triggered by an abnormal activation of pro-inflammatory cytokines such as interleukin-1b, interleukin-8, tumour necrosis factor-a and leukotrienes [4–6]. Blood and exhaled breath condensate levels of hydrogen peroxide, superoxide anion, 8-isoprostane and reactive nitrogen intermediates are elevated in patients with cystic fibrosis, bronchiectasis and chronic obstructive pulmonary disease [7–10].
Many antibiotics are developed for the control of bacterial infection during the exacerbations of bronchiectasis [11–13]. Growing evidences indicated that some drugs provided beneficial effects. For instance, macrolides can reduce the number of exacerbations and the decline in lung function, and improve health-related quality of life and survival rate in patients with bronchiectasis [14–17]. In a double-blind clinical trial, long-term macrolide maintenance therapy is effective to reduce the frequency of exacerbations in patients with chronic obstructive pulmonary disease or bronchiectasis [18–21].
Long-term prophylaxis with azithromycin has been reported to reduce the frequency of exacerbations and sputum volume, and improve lung function values in patients with non-cystic fibrosis bronchiectasis [22, 23]. Several studies have investigated the efficacy and safety of azithromycin for non-cystic fibrosis bronchiectasis, but the results are conflicting [7, 20, 24]. This meta-analysis of RCTs aims to assess the efficacy and safety of azithromycin treatment versus placebo for non-cystic fibrosis bronchiectasis.
Materials and methods
This meta-analysis was performed based on the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement and Cochrane Handbook for Systematic Reviews of Interventions [25, 26]. No ethical approval and patient consent were required because all analyses were based on previous published studies.
Literature search and selection criteria
We have systematically searched several databases including PubMed, EMbase, Web of science, EBSCO and Cochrane library from inception to July 2019 with the following keywords: “azithromycin” AND “bronchiectasis”. The reference lists of retrieved studies and relevant reviews were also hand-searched and the process above was performed repeatedly in order to include additional eligible studies.
The inclusion criteria were presented as follows: (1) study design was RCT, (2) patients were diagnosed with non-cystic fibrosis bronchiectasis, and (3) intervention treatments were azithromycin versus placebo.
Data extraction and outcome measures
Some baseline information was extracted from the original studies, and they included first author, number of patients, age, female, body mass index, forced expiratory volume in 1 s (FEV1) and detail methods in two groups. Data were extracted independently by two investigators, and discrepancies were resolved by consensus. The primary outcomes were free of exacerbation and pulmonary exacerbations. Secondary outcomes included number of pulmonary exacerbations, FEV1, score on St George’s respiratory questionnaire, nausea and vomiting, adverse events.
Quality assessment in individual studies
The methodological quality of each RCT was assessed by the Jadad Scale which consisted of three evaluation elements: randomization (0–2 points), blinding (0–2 points), dropouts and withdrawals (0–1 points) [27]. One point would be allocated to each element if they were conducted and mentioned appropriately in the original article. The score of Jadad Scale varied from 0 to 5 points. An article with Jadad score ≤ 2 was considered to have low quality. The study is thought to have high quality if Jadad score ≥ 3 [28].
Statistical analysis
We assessed standard mean difference (SMD) with 95% confidence interval (CI) for continuous outcomes (number of pulmonary exacerbations, FEV1, and score on St George’s respiratory questionnaire) and odd ratios (OR) with 95% CI for dichotomous outcomes (free of exacerbation, pulmonary exacerbations, nausea and voimiting, adverse events). Heterogeneity was evaluated using the I2 statistic, and I2 > 50% indicated significant heterogeneity [29]. The random-effects model was used for all meta-analysis. We searched for potential sources of heterogeneity when encountering significant heterogeneity. Sensitivity analysis was performed to detect the influence of a single study on the overall estimate via omitting one study in turn or performing the subgroup analysis. Owing to the limited number (< 10) of included studies, publication bias was not assessed. Results were considered as statistically significant for P < 0.05. All statistical analyses were performed using Review Manager Version 5.3 (The Cochrane Collaboration, Software Update, Oxford, UK).
Results
Literature search, study characteristics and quality assessment
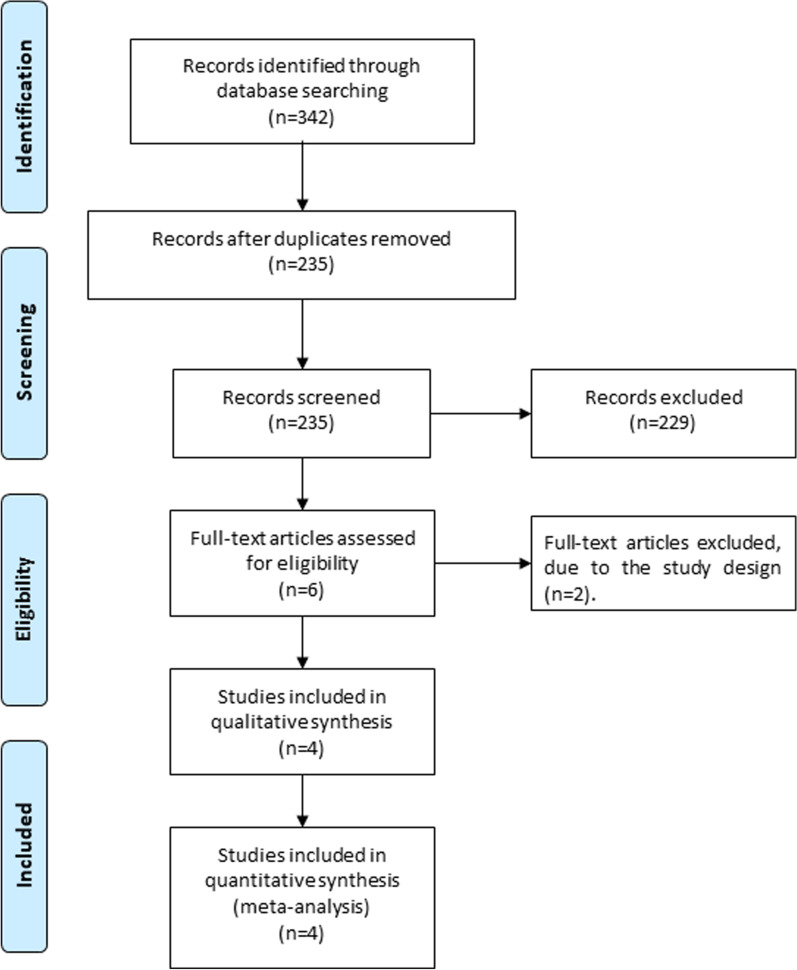
Figure 1 showed the detail flowchart of the search and selection results. 342 potentially relevant articles were initially identified and four RCTs were finally included in the meta-analysis [7, 20, 24, 30].
Fig. 1.
Flow diagram of study searching and selection process
The baseline characteristics of four included RCTs were shown in Table 1. These studies were published between 2012 and 2013, and the total sample size was 343. Three studies reported adults [7, 20, 24], while one study reported children [30]. The treatment duration ranged from 3 to 24 months, and detail methods of azithromycin differed in each RCT.
Table 1.
Characteristics of included studies
| NO | Author | Azithromycin group | Control group | Jada scores | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Age (years) | Female (n) | Body mass index (kg/m.2) | FEV1 (L) | Methods | Number | Age (years) | Female (n) | Body mass index (kg/m.2) | FEV1 (L) | Methods | |||
| 1 | Valery 2013 | 45 | 3.99 ± 2.14 | 19 | – | – | azithromycin (30 mg/kg) once a week for up to 24 months | 44 | 4.22 ± 2.30 | 23 | – | – | matched placebo | 4 |
| 2 | Diego 2013 | 16 | 57 ± 11 | 9 | 27 ± 1 | 1.48 ± 0.8 | Azithromycin 250 mg three times per week during 3 months | 14 | 61 ± 12 | 7 | 24 ± 2 | 1.63 ± 0.7 | Matched placebo | 4 |
| 3 | Altenburg 2013 | 43 | 59.9 ± 12.3 | 25 | 23.0 ± 3.4 | – | Azithromycin (250 mg daily) for 12 months | 40 | 64.6 ± 9.1 | 28 | 24.5 ± 4.0 | – | Matched placebo | 5 |
| 4 | Wong 2012 | 71 | 60.9 ± 13.6 | 48 | 28.8 ± 7.2 | 1.87 ± 0.74 | 500 mg azithromycin three times a week for 6 months | 70 | 59.0 ± 13.3 | 50 | 28.6 ± 6.9 | 1.88 ± 0.69 | Matched placebo | 5 |
FEV1, forced expiratory volume in 1 s
Two studies reported free of exacerbation and pulmonary exacerbations [20, 30], three studies reported number of pulmonary exacerbations [7, 20, 30], two studies reported FEV1 and score on St George’s respiratory questionnaire [7, 24], two studies reported nausea and vomiting [24, 30], as well as adverse events [20, 24, 30]. Jadad scores of four included studies varied from 3 to 5, and all four studies had high-quality.
Primary outcomes: free of exacerbation and pulmonary exacerbations
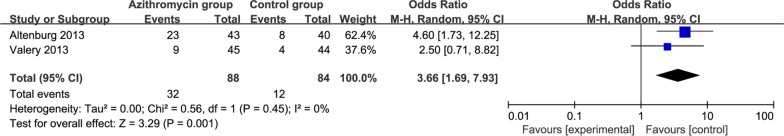
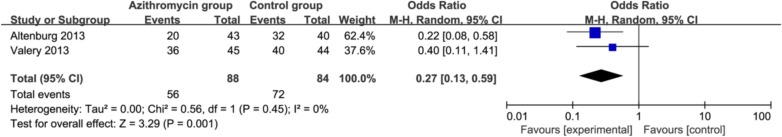
The random-effect model was used for primary outcomes. The results found that compared to control group for non-cystic-fibrosis bronchiectasis, azithromycin treatment was associated with significantly improved free of exacerbation (OR = 3.66; 95% CI 1.69–7.93; P = 0.001) with no heterogeneity among the studies (I2 = 0%, heterogeneity P = 0.45, Fig. 2) and reduced pulmonary exacerbations (OR = 0.27; 95% CI 0.13–0.59; P = 0.001) with no heterogeneity among the studies (I2 = 0%, heterogeneity P = 0.45, Fig. 3).
Fig. 2.
Forest plot for the meta-analysis of free of exacerbation
Fig. 3.
Forest plot for the meta-analysis of pulmonary exacerbations
Sensitivity analysis
There was no heterogeneity for primary outcomes, and thus we did not perform sensitivity analysis by omitting one study in each turn to detect the source of heterogeneity.
Secondary outcomes
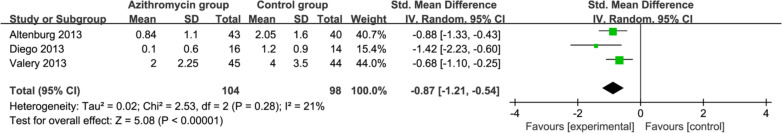
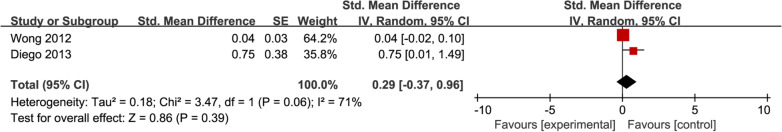
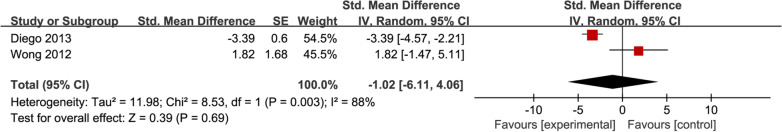
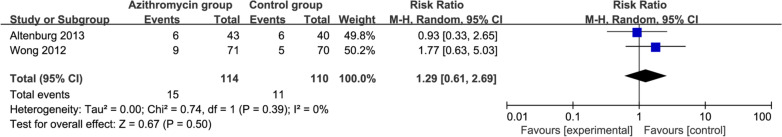
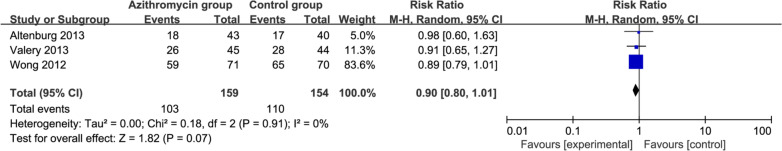
In comparison with control intervention for non-cystic-fibrosis bronchiectasis, azithromycin treatment can substantially reduce the number of pulmonary exacerbations (SMD = − 0.87; 95% CI − 1.21 to − 0.54; P < 0.00001; Fig. 4), but had no obvious influence on FEV1 (SMD = 0.29; 95% CI − 0.37 to 0.96; P = 0.39; Fig. 5), score on St George’s respiratory questionnaire (SMD = − 1.02; 95% CI − 6.11 to 4.06; P = 0.69; Fig. 6), nausea or vomiting (OR = 1.29; 95% CI 0.61–2.69; P = 0.50; Fig. 7), or adverse events (OR = 0.90; 95% CI 0.80–1.01; P = 0.07; Fig. 8).
Fig. 4.
Forest plot for the meta-analysis of number of pulmonary exacerbations
Fig. 5.
Forest plot for the meta-analysis of FEV1 (L)
Fig. 6.
Forest plot for the meta-analysis of score on St George’s respiratory questionnaire
Fig. 7.
Forest plot for the meta-analysis of nausea and vomiting
Fig. 8.
Forest plot for the meta-analysis of adverse events
Discussion
Several studies have reported the benefit of azithromycin for non‐cystic fibrosis bronchiectasis [18–21, 24, 31]. In one open-label prospective study of 30 patients, azithromycin at the dose of 250 mg three times per week for 3 months resulted in a significant reduction in sputum volume, symptoms, health-related quality of life and frequency of exacerbations for non‐cystic fibrosis bronchiectasis [7]. Long-term azithromycin treatment was found to provide beneficial effects on exacerbations, forced expiratory volume in 1 s and sputum volume for these patients [22].
Our meta-analysis suggested that azithromycin treatment can substantially improve free of exacerbation, reduce pulmonary exacerbations and number of pulmonary exacerbations for non-cystic-fibrosis bronchiectasis, but showed no significantly favorable impact on FEV1 or St George’s respiratory questionnaire. In the EMBRACE trial, 6 months of azithromycin treatment was found to reduce the rate of event-based exacerbations and increase the time to the first exacerbation compared with placebo [24]. In addition, azithromycin can produce a significant improvement in health-related quality of life and disease symptoms in the BAT trial [20].
In a previous study, azithromycin was reported to provide beneficial effects regardless of infection [16]. In contrast, the post-hoc analysis comparing the effect of treatment in patients with or without P. aeruginosa, the benefits are more pronounced in patients with P. aeruginosa [7]. Macrolides act through the inhibition of cell chemotaxis, cytokine synthesis, adhesion molecule expression and reactive oxygen species generation [7]. No increase in adverse events is observed after azithromycin based on the results of this meta-analysis. In addition, bronchiectasis are divided into nonperfused and perfused types [32]. The surgical indication of bronchiectasis is localized bronchiectasis documented by high-resolution computed tomography and obvious symptom such as chronic productive cough, repeated or significant hemoptysis, recurrent pulmonary infection and failure of medical treatment [33].
Several limitations exist in this meta-analysis. Firstly, our analysis is based on only four RCTs, and more RCTs with large sample size should be conducted to explore this issue. Next, although there is no significant heterogeneity, different duration and methods of azithromycin therapy and characteristics of patients may have some influence on the pooling results. Finally, some unpublished and missing data may lead to some bias for the pooled effect.
Conclusion
Azithromycin treatment benefits to prevent the exacerbations among patients with non-cystic fibrosis bronchiectasis.
Acknowledgements
None.
Abbreviations
- RCTs
Randomized controlled trials
- MDs
Mean differences
- CIs
Confidence intervals
- RRs
Risk ratios
Author contributions
KL and LL conducted the design, YO conducted the study planning, data analysis and data interpretation, KL wrote and revised the article. All authors read and approved the final manuscript.
Funding
Exploration on the curriculum reform of pharmaceutical marketing and entrepreneurship foundation based on the cultivation and practice of socialist core values , Subject number :201065S.
Availability of data and materials
Not applicable.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kui Li, Email: nx7446@163.com.
Li Liu, Email: xiangweineng@163.com.
Yan Ou, Email: 595497621@qq.com.
References
- 1.Barker AF. Bronchiectasis. N Engl J Med. 2002;346(18):1383–1393. doi: 10.1056/NEJMra012519. [DOI] [PubMed] [Google Scholar]
- 2.Fuschillo S, De Felice A, Balzano G. Mucosal inflammation in idiopathic bronchiectasis: cellular and molecular mechanisms. Eur Respir J. 2008;31(2):396–406. doi: 10.1183/09031936.00069007. [DOI] [PubMed] [Google Scholar]
- 3.Ramsey K, Radicioni G, Hill D, Ehre C, Button B, Alexis NE, Knowles M, Donaldson S, Kesimer M, Mcguckin M. Airways mucus pathogenesis in patients with non-cystic fibrosis bronchiectasis. Eur Respiratory Soc. 2018.
- 4.Chang-Macchiu P, Traversi L, Polverino E. Bronchiectasis phenotypes. Curr Opin Pulm Med. 2019;25(3):281–288. doi: 10.1097/MCP.0000000000000569. [DOI] [PubMed] [Google Scholar]
- 5.Athanazio R, da Costa JC, de la Rosa Carrillo D, Martínez-García MÁ. Current and future pharmacotherapy options for non-cystic fibrosis bronchiectasis. Expert Rev Respir Med. 2018;12(7):569–584. doi: 10.1080/17476348.2018.1481392. [DOI] [PubMed] [Google Scholar]
- 6.Polverino E, Dimakou K, Hurst J, Martinez-Garcia M-A, Miravitlles M, Paggiaro P, Shteinberg M, Aliberti S, Chalmers JD. The overlap between bronchiectasis and chronic airway diseases: state of the art and future directions. Eur Respir J. 2018;52(3):1800328. doi: 10.1183/13993003.00328-2018. [DOI] [PubMed] [Google Scholar]
- 7.Diego AD, Milara J, Martinez-Moragón E, Palop M, León M, Cortijo J. Effects of long-term azithromycin therapy on airway oxidative stress markers in non-cystic fibrosis bronchiectasis. Respirology. 2013;18(7):1056–1062. doi: 10.1111/resp.12130. [DOI] [PubMed] [Google Scholar]
- 8.Loukides S, Horvath I, Wodehouse T, Cole PJ, Barnes PJ. Elevated levels of expired breath hydrogen peroxide in bronchiectasis. Am J Respir Crit Care Med. 1998;158(3):991–994. doi: 10.1164/ajrccm.158.3.9710031. [DOI] [PubMed] [Google Scholar]
- 9.Shoemark A, Wilson R. Bronchial and peripheral airway nitric oxide in primary ciliary dyskinesia and bronchiectasis. Respir Med. 2009;103(5):700–706. doi: 10.1016/j.rmed.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Makris D, Paraskakis E, Korakas P, Karagiannakis E, Sourvinos G, Siafakas NM, Tzanakis N. Exhaled breath condensate 8-isoprostane, clinical parameters, radiological indices and airway inflammation in COPD. Respiration. 2008;75(2):138–144. doi: 10.1159/000106377. [DOI] [PubMed] [Google Scholar]
- 11.Kelly C, Chalmers JD, Crossingham I, Relph N, Felix LM, Evans DJ, Milan SJ, Spencer S. Macrolide antibiotics for bronchiectasis. Cochrane Database Syst Rev. 2018;(3). [DOI] [PMC free article] [PubMed]
- 12.Felix LM, Grundy S, Milan SJ, Armstrong R, Harrison H, Lynes D, Spencer S. Dual antibiotics for bronchiectasis. Cochrane Database Syst Rev. 2018;(6). [DOI] [PMC free article] [PubMed]
- 13.Kaehne A, Milan SJ, Felix LM, Sheridan E, Marsden PA, Spencer S. Head-to-head trials of antibiotics for bronchiectasis. Cochrane Database Syst Rev. 2018;9:CD012590. doi: 10.1002/14651858.CD012590.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tagaya E, Tamaoki J, Kondo M, Nagai A. Effect of a short course of clarithromycin therapy on sputum production in patients with chronic airway hypersecretion. Chest. 2002;122(1):213–218. doi: 10.1378/chest.122.1.213. [DOI] [PubMed] [Google Scholar]
- 15.Wolter J, Seeney S, Bell S, Bowler S, Masel P, McCormack J. Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomised trial. Thorax. 2002;57(3):212–216. doi: 10.1136/thorax.57.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clement A, Tamalet A, Leroux E, Ravilly S, Fauroux B, Jais J-P. Long term effects of azithromycin in patients with cystic fibrosis: a double blind, placebo controlled trial. Thorax. 2006;61(10):895–902. doi: 10.1136/thx.2005.057950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kadota J, Mukae H, Ishii H, Nagata T, Kaida H, Tomono K, Kohno S. Long-term efficacy and safety of clarithromycin treatment in patients with diffuse panbronchiolitis. Respir Med. 2003;97(7):844–850. doi: 10.1016/S0954-6111(03)00042-8. [DOI] [PubMed] [Google Scholar]
- 18.Albert RK, Connett J, Bailey WC, Casaburi R, Cooper JAD, Jr, Criner GJ, Curtis JL, Dransfield MT, Han MK, Lazarus SC. Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689–698. doi: 10.1056/NEJMoa1104623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Serisier DJ, Martin ML, McGuckin MA, Lourie R, Chen AC, Brain B, Biga S, Schlebusch S, Dash P, Bowler SD. Effect of long-term, low-dose erythromycin on pulmonary exacerbations among patients with non-cystic fibrosis bronchiectasis: the BLESS randomized controlled trial. JAMA. 2013;309(12):1260–1267. doi: 10.1001/jama.2013.2290. [DOI] [PubMed] [Google Scholar]
- 20.Altenburg J, de Graaff CS, Stienstra Y, Sloos JH, van Haren EH, Koppers RJ, van der Werf TS, Boersma WG. Effect of azithromycin maintenance treatment on infectious exacerbations among patients with non-cystic fibrosis bronchiectasis: the BAT randomized controlled trial. JAMA. 2013;309(12):1251–1259. doi: 10.1001/jama.2013.1937. [DOI] [PubMed] [Google Scholar]
- 21.McShane PJ, Naureckas ET, Tino G, Strek ME. Non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2013;188(6):647–656. doi: 10.1164/rccm.201303-0411CI. [DOI] [PubMed] [Google Scholar]
- 22.Anwar G, Bourke S, Afolabi G, Middleton P, Ward C, Rutherford R. Effects of long-term low-dose azithromycin in patients with non-CF bronchiectasis. Respir Med. 2008;102(10):1494–1496. doi: 10.1016/j.rmed.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 23.Davies G, Wilson R. Prophylactic antibiotic treatment of bronchiectasis with azithromycin. Thorax. 2004;59(6):540–541. [PMC free article] [PubMed] [Google Scholar]
- 24.Wong C, Jayaram L, Karalus N, Eaton T, Tong C, Hockey H, Milne D, Fergusson W, Tuffery C, Sexton P. Azithromycin for prevention of exacerbations in non-cystic fibrosis bronchiectasis (EMBRACE): a randomised, double-blind, placebo-controlled trial. Lancet. 2012;380(9842):660–667. doi: 10.1016/S0140-6736(12)60953-2. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.HigginsJPT G. Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011], The cochrane collaboration; 2011.
- 27.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 28.Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med. 2001;135(11):982–989. doi: 10.7326/0003-4819-135-11-200112040-00010. [DOI] [PubMed] [Google Scholar]
- 29.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 30.Valery PC, Morris PS, Byrnes CA, Grimwood K, Torzillo PJ, Bauert PA, Masters IB, Diaz A, McCallum GB, Mobberley C. Long-term azithromycin for Indigenous children with non-cystic-fibrosis bronchiectasis or chronic suppurative lung disease (Bronchiectasis Intervention Study): a multicentre, double-blind, randomised controlled trial. Lancet Respir Med. 2013;1(8):610–620. doi: 10.1016/S2213-2600(13)70185-1. [DOI] [PubMed] [Google Scholar]
- 31.Gang L, Chen Y, Ding F, Zhou X. The impact of different doses of azithromycin maintenance treatment on expiratory flow limitation and quality of life among stable patients with non-cystic fibrosis bronchiectasis. Chin J Postgrad Med. 2018;41(6):493–497. [Google Scholar]
- 32.Balci AE, Balci TA, Ozyurtan MO. Current surgical therapy for bronchiectasis: surgical results and predictive factors in 86 patients. Ann Thorac Surg. 2014;97(1):211–217. doi: 10.1016/j.athoracsur.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 33.Hao X, Dazhong L, Lei Y, Jiaying Z, Linyou Z. Surgical treatment of bronchiectasis: 5 years of experience at a single institution. J Laparoendosc Adv Surg Tech Part A. 2019;29(6):826–830. doi: 10.1089/lap.2018.0694. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.