Abstract
Purpose
This study aimed to systematically review the literature on randomized controlled trials on weight reduction interventions using digital health for employees with obesity.
Methods
All relevant articles published until September 2021 were systematically identified from six electronic databases: MEDLINE, EMBASE, CINAHL, PsycINFO, RISS, and KISS. Data selection and extraction were independently performed by three researchers. Methodological quality was assessed using the JBI Critical Appraisal Checklist for Randomized Controlled Trials. The results were narratively synthesized.
Results
Eleven studies were included in the systematic review. All studies had a low risk of bias. The settings and sample sizes of the included studies were different. The contents of the interventions included nutrition, physical activity, behavioral change, incentives, and motivation. Four studies were based on social cognitive theory. A total of ten studies delivered web-based intervention, while the other used tele-monitoring device. A wide range of intervention strategies was used including providing online resources, tele-counseling, and patient-tailored advice. As a result of the intervention, a total of seven studies showed a significant weight reduction in both the intervention and comparison groups, with significant differences between groups.
Conclusion
Until now, use of digital health in weight reduction interventions for employees with obesity has been conducted on a web-based. Various contents such as nutrition, physical activity and theories were explored. Further study is required using more diverse delivery methods such as mobile application, use of wearable devices.
Keywords: obesity, weight reduction, digital health, telemedicine, occupational groups
Introduction
The number of individuals affected by overweight and obese has increased. In 2016, according to the World Health Organization, more than 1.9 billion adults were overweight and over 650 million of these were obese.1 Overweight and obesity are major risk factors for a number of chronic diseases, including diabetes and cardiovascular diseases such as heart disease and stroke.2 These diseases result in over 4 million deaths each year, according to the global burden of disease.3
Among the increasing overweight and obese population, there has been conducted a lot of researches which focused on overweight and obesity of employees, especially. Many previous studies have emphasized the importance of intervention for employees with overweight or obesity because they have longer sick leaves and are at increased risk of work disability.4–6 Numerous worksite interventions have been conducted to reduce the body weight and body mass index (BMI) of employees, including modification of diet and physical activity levels and behavioral therapy.7,8 In addition, some of them demonstrated the effectiveness of interventions based on theories such as Social Cognitive Theory and the Transtheoretical Stages of Change Model.9–12 These interventions not only brought physical and mental health improvements to employees, but also resulted in reduced sick leave and increased employee’s productivity and output for workplaces.13–15
With the advancement of technology, the use of digital health in weight reduction interventions have several advantages, such as convenience, cost-effectiveness, and the ability to tailor interventions according to their needs.16,17 Several systematic reviews have attempted to examine the potential of weight reduction interventions using digital health.16,18–22 These previous reviews demonstrated that weight-reduction interventions using digital health showed greater weight reduction than face-to-face interventions in adults with overweight or obesity. In addition, the effectiveness of the use of digital health intervention in the workplace has already been proven. The previous review has reported that digital-only health interventions for employees in the workplace have a positive impact on health-related outcomes.23 However, to our knowledge, no systematic review has been conducted on the development and implementation of weight-reduction interventions using digital health for employees with obesity.
This study aims to systematically review the literature on randomized controlled trials (RCT) of weight reduction interventions using digital health for employees with obesity to identify the characteristics of the literature including theoretical background, intervention contents, implementation approaches, and use of digital health, and to provide suggestions for future interventions through a comprehensive review.
Methods
This systematic review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.24
Search Strategy
All relevant articles were systematically identified from six electronic databases: MEDLINE, EMBASE, CINAHL, PsycINFO, RISS, and KISS. The search was conducted in October 2021 without conducting further manual searches. The timeframe for the analysis was restricted to September 2021. Based on the PICO model, the population was “employees with obesity”, intervention was “weight reduction interventions using digital health”, “weight reduction program using digital health”, or “weight reduction management using digital health”; comparisons and outcomes were not set in this systematic review search keywords. The search terms were conducted using indexing terms, Medical Subject Heading Terms (MeSH terms), and free-text search terms Appendix 1.
Eligibility Criteria for Study Selection
The inclusion criteria were as follows: (a) adult employees affected by obesity or overweight in jobs; (b) interventions for weight reduction using digital health devices such as computers, tablets, personal digital assistants (PDAs), and smartphones; (d) measurement of participants’ bodyweight or BMI; (e) original articles published in English or Korean; and (f) the study design was RCT.
Selection of Studies
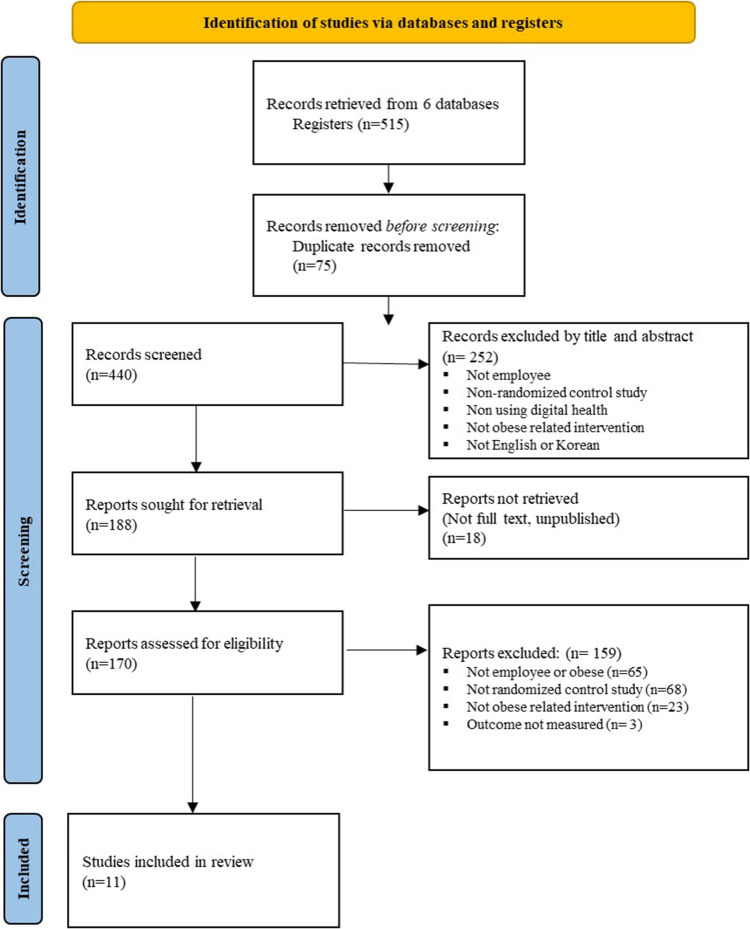
A flowchart of the study selection process is presented in Figure 1. Duplicate studies were removed using bibliographical software and manual searches. Subsequently, the studies were screened by reading the title and abstract following the inclusion criteria. The entire texts of the screened studies were assessed at the end stage, and appropriate studies were selected. The selection process was independently performed by three researchers. Two researchers conducted screening for the half of included studies. The other researcher conducted screening for all included studies. The screening results were compared. Any disagreement between them was resolved through group discussion.
Figure 1.
PRISMA Flow Diagram for Systematic Review.
Notes: PRISMA figure adapted from Moher D, Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology. 2009;62(10). Creative Commons.24
Methodological Quality Appraisal
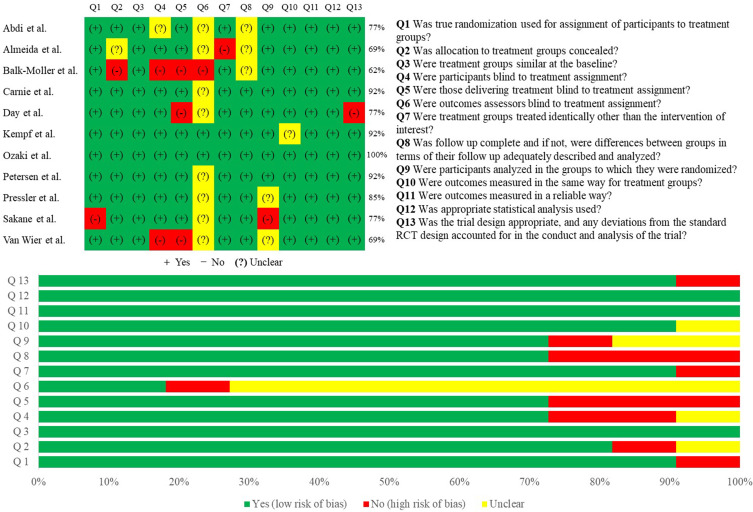
Methodological quality was assessed using the JBI critical appraisal checklist for RCT.25 The tool consisted of 13 items. Each item was answered as “Yes”, “No”, “Unclear”, or “Not/Applicable”. The overall scores were calculated as the proportion of “yes”. The result of the quality appraisal was scored as i) ≤49% = high risk of bias and ii) above 50% = low risk of bias.26,27 Four researchers independently performed the assessment, and a group discussion was conducted to reach agreement on the quality appraisal.
Data Extraction and Synthesis
The data extracted for characteristics of the studies included the first author, publication year, country, population, characteristics of sample (sample size, age), characteristics of intervention (contents, theoretical background, intervention length, and follow-up), and major results (outcome variables, results). In addition, we summarized the use of digital health in these studies. These tables were thoroughly assessed by four reviewers through group discussion. A quality analysis was adopted rather than a meta-analysis because the studies included had differences in the types of digital health used for intervention, intervention length, and research outcomes.28
Results
Search Results
A total of 521 articles were initially retrieved from the databases and 449 articles were obtained after duplicate removal. After screening titles and abstracts, 188 full-text articles were retrieved. An additional 159 articles were excluded because they did not meet the inclusion criteria. Eleven articles met the inclusion criteria and were used in this systematic review.
Quality Appraisal of Included Studies
The results of the risk of bias assessment for the 11 included studies are presented in Figure 2. All studies were scored as ‘low risk of Bias’. As for the quality assessment by each item, item 6 “were outcomes assessors blind to treatment assignment?” were unclear or unable to blind in 9 studies. Item 3: “Were the treatment groups similar at baseline?”, Item 11 “Were outcomes measured reliably?” and Item 12 “Was appropriate statistical analysis used?” were assured in all included studies.
Figure 2.
Risk of Bias Results of the Included Studies.
Characteristics of the Included Studies
Table 1 presented characteristics of the included studies. A growing number of publications occurred within 10 years, with 81.8% (n = 9) published between 2012 and 2022. The United States had the largest number of publications (36.4%), followed by Germany (18.2%), and Japan (18.2%).
Table 1.
Characteristics of the Included Studies
| Author (Year) | Country | Population | Interventions | Results |
|---|---|---|---|---|
|
|
|
||
| Abdi et al (2015)29 | Iran |
|
|
|
| Almeida et al (2015)38 | USA |
|
|
|
| Balk-Moller et al (2017)39 | Denmark |
|
|
|
| Carnie et al (2013)30 | USA |
|
|
|
| Day et al (2019)31 | USA |
|
|
|
| Kempf et al (2019)32 | Germany |
|
|
|
| Ozaki et al (2018)33 | Japan |
|
|
|
| Petersen et al (2008)34 | USA |
|
|
|
| Pressler et al (2010)35 | Germany |
|
|
|
| Sakane et al (2013)36 | Japan |
|
|
|
| Van Wier et al (2012)37 | Netherlands |
|
|
|
Abbreviations: IG, intervention group; CG, comparison group; wk, week; m, month; BW, body weight; WC, waist circumference; BP, blood pressure; BMI, body mass index; HC, hip circumference; HDL, high-density lipoprotein; FBG, fasting blood glucose.
The settings of the studies were different, and included government, pharmaceutical companies, healthcare centers, and automobile manufacturing. The participants in the studies were employees with overweight or obese, 81.8% were those with obese and 18.2% were those with either overweight or obese. In the eight studies that reported the mean age of participants, the mean age of included participants was 43.5 years.29–33,37–39 The sample sizes of the included studies ranged from 34 to 7743 in the intervention group and from 22 to 1001 in the control group.32–34,38
The intervention contents across the included studies consisted of nutrition, physical activity, behavioral change, incentives, and motivation. Except for Pressler and Knebel’s study,35 ten studies included nutrition contents related to nutrient information, health eating, health, recipes, and fluid intake. All studies included physical activity contents related to explanations of exercises, fitness videos, and consultations with fitness advisors. A total of seven studies29,31–34,37,39 included behavioral change contents related to assessing dietary changes, physical activity changes, and personalized goal setting changes. Two studies32,34 included motivation contents related to consultation or discussion with experts regarding barriers to change, encouragement, and emotional support. Two studies30,38 provided incentives based on the percent of weight loss.
Four studies29,36–38 were based on social cognitive theory. Interventions were conducted for an average of 23.8 weeks and follow-up was measured at a minimum of 3 months and maximum of 36 months from the baseline.
As a result of the intervention, all studies reported a statistically significant reduction in body weight after intervention. Among them, seven studies29–31,33,34,36,39 showed significant differences between the intervention and comparison groups. A total of six studies29,30,33,34,36,39 showed weight reduction after intervention in both the intervention and comparison groups, and the intervention group lost more weight than the comparison group. In Day et al31 the intervention group showed a significant weight loss after intervention, but the comparison group significantly gained the weight. In the remaining four studies,32,35,37,38 there was significant weight loss in both the intervention and comparison groups after intervention, but with no significant difference between the groups.
Use of Digital Health of the Included Studies
The use of digital health in the included studies is shown in Table 2. Except for the study by Kempf et al32 conducted using a tele-monitoring device, all interventions in the included studies were web-based. Most included studies provided online resources as intervention strategies. Ten studies29,31–39 delivered online education on diet, nutrition, exercise, motivation, and behavioral changes. Nine studies30,31,33–39 implemented programs focusing on patient-tailored advice such as “daily emails tailored to each participant”, “personalized goal setting”, “tailored remote group sessions”, “personalized structured exercise schedules”, and “self-selected healthy activities”. Eight studies29,31,32,34,36–39 delivered tele-counseling interventions. A personal counselor called, or e-mailed, and explained the goal of the program, and counseled them about weight reduction. Seven studies30–35,39 monitored patients’ health-related data, such as food intake, pulse rate, and heart rate. Online social support interventions were used in four studies.29,33,34,39
Table 2.
Use of Digital Health
| Author (Year) | Delivering Method | Intervention Strategies | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Website | Mobile App | Tele-Monitoring Device | Tele-Counseling | Patient-Tailored Advice | Telemonitoring of Patient’s Generated Health Related Data | Providing Online Resources | Online Social Support | ||
| Abdi et al (2015)29 | √ | √ | √ | √ | |||||
| Almeida et al (2015)38 | √ | √ | √ | √ | |||||
| Balk-Moller et al (2017)39 | √ | √ | √ | √ | √ | √ | √ | ||
| Carnie et al (2013)30 | √ | √ | √ | ||||||
| Day et al (2019)31 | √ | √ | √ | √ | √ | ||||
| Kempf et al (2019)32 | √ | √ | √ | √ | |||||
| Ozaki et al (2018)33 | √ | √ | √ | √ | √ | ||||
| Petersen et al (2008)34 | √ | √ | √ | √ | √ | √ | |||
| Pressler et al (2010)35 | √ | √ | √ | √ | |||||
| Sakane et al (2013)36 | √ | √ | √ | √ | |||||
| Van Wier et al (2012)37 | √ | √ | √ | √ | |||||
Discussion
A systematic review of weight reduction interventions using digital health for employees with obesity was conducted on 11 weight reduction interventions. We described the characteristics of selected studies, including study population (characteristics, mean age, and sample size), interventions (contents, theoretical background, and intervention length), and results (outcome variables, follow-up, and major results). The use of digital health, including delivery methods and intervention strategies, was also reviewed. All studies used body weight as the outcome measure. All studies reported a statistically significant reduction in body weight after intervention. Four studies32,35,37,38 reported no significant differences between the intervention and comparison groups. All studies had a low risk of bias.
Most previous studies on employees with obesity have focused on interventions to encourage physical activity.40–42 Our findings differ from those of previous interventions in that the interventions not only focused on physical activity, but also included nutrition, behavior change, and provision of incentives. This could be due to differences in the study populations included in this review. Most previous studies included sedentary employees; however, our study included employees of various occupations working in various workplaces.
Four studies29,36–38 used social cognitive theory, which is one of the most common theories informing intervention design, while the remaining studies did not have a theoretical background. Our findings differ from those of a review of models that concluded that the theory of planned behavior and socio-ecological model was the most promising for obesity prevention, as none of our studies used those models.43 This could be due to differences in aim: the previous review dealt with primary prevention, while our study dealt with secondary intervention, which is consistent with a previous study.44 In addition, among the four studies based on social cognitive theory, two37,38 were not significantly different between the intervention and comparison groups. In a previous systematic review of workplace health promotion programs,44 other theories, such as the stages of change model and the transtheoretical model, were used and showed a significant reduction in BMI. However, it is not yet possible to conclude whether it is effective to develop and implement an intervention program using theories for employees with obesity, and it requires to be proven in future study.
Except for the study by Kempf et al32 all studies included in this review used web-based weight reduction interventions rather than mobile app-based interventions. Many previous studies using mobile applications have been actively conducted within the last 10 years and have reported notable success in obesity control, weight reduction, physical activity increase, and quality of life improvement.45–47 Considering that nine studies, except for two,34,35 were published within 10 years, it can be seen that few mobile app-based interventions have been conducted on employees with obesity. This may be because the cost of the development of a mobile app-base intervention may be considered expensive for academic purposes. A mobile app makes employees engage in an intervention program any time at any place, so that it is useful in that employees can comfortably access it at worksites. Future research is required to perform well-designed RCT using mobile applications.
Diverse intervention strategies were used in most of the studies included in this review. However, the digital technologies used in the included studies were limited to counseling through telephone or e-mail and monitoring of the data entered by employees with obesity. With the advancement of technology, the intervention strategies of weight reduction interventions have been diversified. Use of video call have proven to be more effective as a means of health guidance than face to face.48 In addition, it has been proven that the introduction of wearable device and mobile application is more effective for weight reduction in patients with overweight or obese than others.49,50 Attempts should be made in future research to apply more up-to-date intervention strategies, such as performing an online video call or automatically collecting multimodal data such as body weight and BMI from a digital scale or physical activity from a wearable device. These attempts could be effective and useful in the current healthcare environment and should be evaluated in future research.
This systematic review has some limitations. First, the review included only 11 studies published in peer-reviewed literature. It excluded gray literature and unpublished literature, which present potential publication bias. To integrate with the wider literature, it is required to utilize an agreed language such as BCT taxonomy in a future study.51 Second, heterogeneous population and settings of included studies might reduce generalizability of the study and downgrade the overall strength of the evidence. In addition, only studies published in English were included in this review, with almost conducted in relatively advanced countries such as USA, Germany, and Japan. Therefore, the review is limited in the generalizability to other countries where other cultural factors associated with weight reduction intervention and use of digital health.
Conclusion
The results of this review have several important implications for future research in employees with obesity. The studies conducted so far have only been web-based even if digital health is used. In a future study, delivery methods and intervention strategies require to reflect the latest technology, such as the development of a mobile app-based intervention program, the use of video calls, wearable devices, and digital scales. In addition, weight reduction interventions for employees with obesity have been developed and applied using limited theory to date. It is necessary to verify whether the theory is effective in intervention targeting these groups.
Acknowledgments
This work was supported by the Seoul National University Hospital.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization. Obesity and overweight; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed October 6, 2022.
- 2.Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–1686. doi: 10.1016/S0140-6736(09)61457-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Global Health Estimates: life expectancy and leading causes of death and disability; 2019. Available from: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death. Accessed October 6, 2022.
- 4.Van Duijvenbode D, Hoozemans M, Van Poppel M, et al. The relationship between overweight and obesity, and sick leave: a systematic review. Int J Obes. 2009;33(8):807–816. doi: 10.1038/ijo.2009.121 [DOI] [PubMed] [Google Scholar]
- 5.Lehnert T, Stuhldreher N, Streltchenia P, et al. Sick leave days and costs associated with overweight and obesity in Germany. J Occup Environ Med. 2014;56(1):20–27. doi: 10.1097/JOM.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 6.Amiri S, Behnezhad S. Body mass index and risk of sick leave: a systematic review and meta-analysis. Clin obes. 2019;9(6):e12334. doi: 10.1111/cob.12334 [DOI] [PubMed] [Google Scholar]
- 7.Anderson LM, Quinn TA, Glanz K, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am j Prev Med. 2009;37(4):340–357. doi: 10.1016/j.amepre.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 8.Mhurchu CN, Aston LM, Jebb SA. Effects of worksite health promotion interventions on employee diets: a systematic review. BMC Public Health. 2010;10(1):1–7. doi: 10.1186/1471-2458-10-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cash SW, Duncan GE, Beresford SA, et al. Increases in physical activity may affect quality of life differently in men and women: the PACE project. Qual life res. 2013;22(9):2381–2388. doi: 10.1007/s11136-013-0389-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lemon SC, Zapka J, Li W, et al. Step ahead: a worksite obesity prevention trial among hospital employees. Am j Prev Med. 2010;38(1):27–38. doi: 10.1016/j.amepre.2009.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elliot DL, Goldberg L, Kuehl KS, et al. The PHLAME (Promoting Healthy Lifestyles: alternative Models’ Effects) firefighter study: outcomes of two models of behavior change. J Occup Environ Med. 2007;49:204–213. doi: 10.1097/JOM.0b013e3180329a8d [DOI] [PubMed] [Google Scholar]
- 12.Mastellos N, Gunn LH, Felix LM, et al. Transtheoretical model stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst Rev. 2014;(2). doi: 10.1002/14651858.CD008066.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morgan PJ, Collins CE, Plotnikoff RC, et al. The impact of a workplace-based weight loss program on work-related outcomes in overweight male shift workers. J Occup Environ Med. 2012;54(2):122–127. doi: 10.1097/JOM.0b013e31824329ab [DOI] [PubMed] [Google Scholar]
- 14.Zinn C, Schofield GM, Hopkins WG. Efficacy of a ”small-changes” workplace weight loss initiative on weight and productivity outcomes. J Occup Environ Med. 2012;54(10):1224–1229. doi: 10.1097/JOM.0b013e3182440ac2 [DOI] [PubMed] [Google Scholar]
- 15.Nepper MJ, McAtee JR, Chai W. Effect of a Workplace Weight-Loss Program for Overweight and Obese Healthcare Workers. Am J Health Promot. 2021;35(3):352–361. doi: 10.1177/0890117120960393 [DOI] [PubMed] [Google Scholar]
- 16.Patel ML, Wakayama LN, Bennett GG. Self‐monitoring via digital health in weight loss interventions: a systematic review among adults with overweight or obesity. Obesity. 2021;29(3):478–499. doi: 10.1002/oby.23088 [DOI] [PubMed] [Google Scholar]
- 17.Senecal C, Collazo-Clavell M, Larrabee BR, et al. A digital health weight-loss intervention in severe obesity. Digit Health. 2020;6:2055207620910279. doi: 10.1177/2055207620910279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beleigoli AM, Andrade AQ, Cançado AG, et al. Web-Based Digital Health Interventions for Weight Loss and Lifestyle Habit Changes in Overweight and Obese Adults: systematic Review and Meta-Analysis. J Med Internet Res. 2019;21(1):e298. doi: 10.2196/jmir.9609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khokhar B, Jones J, Ronksley PE, et al. Effectiveness of mobile electronic devices in weight loss among overweight and obese populations: a systematic review and meta-analysis. BMC Obes. 2014;1:22. doi: 10.1186/s40608-014-0022-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berry R, Kassavou A, Sutton S. Does self-monitoring diet and physical activity behaviors using digital technology support adults with obesity or overweight to lose weight? A systematic literature review with meta-analysis. Obes Rev. 2021;22(10):e13306. doi: 10.1111/obr.13306 [DOI] [PubMed] [Google Scholar]
- 21.Hutchesson MJ, Rollo ME, Krukowski R, et al. e Health interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obes Rev. 2015;16(5):376–392. doi: 10.1111/obr.12268 [DOI] [PubMed] [Google Scholar]
- 22.Arem H, Irwin M. A review of web‐based weight loss interventions in adults. Obes Rev. 2011;12(5):e236–e43. doi: 10.1111/j.1467-789X.2010.00787.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howarth A, Quesada J, Silva J, et al. The impact of digital health interventions on health-related outcomes in the workplace: a systematic review. Digit Health. 2018;4:2055207618770861. doi: 10.1177/2055207618770861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 25.Joanna Briggs Institute. Checklist for Randomized Controlled Trials, Critical Appraisal Tools for Use in JBI Systematic Reviews. Joanna Briggs Institute; 2020. [Google Scholar]
- 26.Kerr D, Ostaszkiewicz J, Dunning T, et al. The effectiveness of training interventions on nurses’ communication skills: a systematic review. Nurse Educ Today. 2020;89:104405. doi: 10.1016/j.nedt.2020.104405 [DOI] [PubMed] [Google Scholar]
- 27.Wonggom P, Kourbelis C, Newman P, et al. Effectiveness of avatar-based technology in patient education for improving chronic disease knowledge and self-care behavior: a systematic review. JBI Database System Rev Implement Rep. 2019;17(6):1101–1129. doi: 10.11124/JBISRIR-2017-003905 [DOI] [PubMed] [Google Scholar]
- 28.Kim S, Park J, Seo H, et al. NECA’s guidance for undertaking systematic reviews and meta-analyses for intervention. Seoul. 2011;1;25. [Google Scholar]
- 29.Abdi J, Eftekhar H, Mahmoodi M, et al. Effect of the intervention based on new communication technologies and the social-cognitive theory on the weight control of the employees with overweight and obesity. J Res Health Sci. 2015;15(4):256–261. [PubMed] [Google Scholar]
- 30.Carnie A, Lin J, Aicher B, et al. Randomized trial of nutrition education added to internet-based information and exercise at the work place for weight loss in a racially diverse population of overweight women. Nutr Diabetes. 2013;3(12):e98–e. doi: 10.1038/nutd.2013.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Day RS, Jahnke SA, Haddock CK, et al. Occupationally tailored, web-based, nutrition and physical activity program for firefighters: cluster randomized trial and weight outcome. J Occup Environ Med. 2019;61(10):841–848. doi: 10.1097/JOM.0000000000001685 [DOI] [PubMed] [Google Scholar]
- 32.Kempf K, Röhling M, Martin S, et al. Telemedical coaching for weight loss in overweight employees: a three-armed randomised controlled trial. BMJ open. 2019;9(4):e022242. doi: 10.1136/bmjopen-2018-022242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ozaki I, Watai I, Nishijima M, et al. Randomized controlled trial of web-based weight-loss intervention with human support for male workers under 40. J Occup Health. 2019;61(1):110–120. doi: 10.1002/1348-9585.12037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petersen R, Sill S, Lu C, et al. Effectiveness of employee internet-based weight management program. J Occup Environ Med. 2008;50(2):163–171. doi: 10.1097/JOM.0b013e31815c6cf6 [DOI] [PubMed] [Google Scholar]
- 35.Pressler A, Knebel U, Esch S, et al. An internet-delivered exercise intervention for workplace health promotion in overweight sedentary employees: a randomized trial. Prev Med. 2010;51(3–4):234–239. doi: 10.1016/j.ypmed.2010.07.008 [DOI] [PubMed] [Google Scholar]
- 36.Sakane N, Dohi S, Sakata K, et al. Effects of visceral fat accumulation awareness on a web-based weight-loss program: Japanese study of visceral adiposity and lifestyle information—Utilization and evaluation (J-VALUE). Int Sch Res Notices. 2013;2013. doi: 10.1155/2013/473764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Wier MF, Dekkers JC, Hendriksen IJ, et al. Effectiveness of phone and e-mail lifestyle counseling for long term weight control among overweight employees. J Occup Environ Med. 2011;53:680–686. doi: 10.1097/JOM.0b013e31821f2bbb [DOI] [PubMed] [Google Scholar]
- 38.Almeida FA, You W, Harden SM, et al. Effectiveness of a worksite‐based weight loss randomized controlled trial: the worksite study. Obesity. 2015;23(4):737–745. doi: 10.1002/oby.20899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balk-Møller NC, Poulsen SK, Larsen TM. Effect of a nine-month web-and app-based workplace intervention to promote healthy lifestyle and weight loss for employees in the social welfare and health care sector: a randomized controlled trial. J Med Internet Res. 2017;19(4):e6196. doi: 10.2196/jmir.6196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhu X, Yoshikawa A, Qiu L, et al. Healthy workplaces, active employees: a systematic literature review on impacts of workplace environments on employees’ physical activity and sedentary behavior. Build Environ. 2020;168:106455. doi: 10.1016/j.buildenv.2019.106455 [DOI] [Google Scholar]
- 41.Barranco-Ruiz Y, Villa-González E. Health-related physical fitness benefits in sedentary women employees after an exercise intervention with Zumba Fitness®. Int J Environ Res Public Health. 2020;17(8):2632. doi: 10.3390/ijerph17082632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel MS, Volpp KG, Rosin R, et al. A randomized, controlled trial of lottery-based financial incentives to increase physical activity among overweight and obese adults. Am J Health Promot. 2018;32(7):1568–1575. doi: 10.1177/0890117118758932 [DOI] [PubMed] [Google Scholar]
- 43.Baranowski T, Cullen KW, Nicklas T, et al. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obes Res. 2003;;11(S10):23S–43S. doi: 10.1038/oby.2003.222 [DOI] [PubMed] [Google Scholar]
- 44.Tam G, Yeung MP. A systematic review of the long-term effectiveness of work-based lifestyle interventions to tackle overweight and obesity. Prev Med. 2018;107:54–60. doi: 10.1016/j.ypmed.2017.11.011 [DOI] [PubMed] [Google Scholar]
- 45.Mateo GF, Granado-Font E, Ferré-Grau C, et al. Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res. 2015;17(11):e4836. doi: 10.2196/jmir.4836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Islam MM, Poly TN, Walther BA, et al. Use of mobile phone app interventions to promote weight loss: meta-analysis. JMIR Mhealth Uhealth. 2020;8(7):e17039. doi: 10.2196/17039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Turner-McGrievy G, Tate D. Tweets, Apps, and Pods: results of the 6-month Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. J Med Internet Res. 2011;13(4):e1841. doi: 10.2196/jmir.1841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fujii H, Yokoyama T, Yoshimi I, et al. A Randomized Controlled Trial to Evaluate the Effects of Health Guidance with Video Call as Compared to Face-to-Face Health Guidance. Int Med J. 2017;24(2):186–191. [Google Scholar]
- 49.Granado-Font E, Flores-Mateo G, Sorlí-Aguilar M, et al. Effectiveness of a Smartphone application and wearable device for weight loss in overweight or obese primary care patients: protocol for a randomised controlled trial. BMC Public Health. 2015;15:531. doi: 10.1186/s12889-015-1845-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McDonough DJ, Su X, Gao Z. Health wearable devices for weight and BMI reduction in individuals with overweight/obesity and chronic comorbidities: systematic review and network meta-analysis. Br J Sports Med. 2021;55(16):917–925. doi: 10.1136/bjsports-2020-103594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]