Abstract
Background
Chronic conditions are characterized by their long duration (≥1 year), need for ongoing medical attention, and limitations in activities of daily living. These can often co-occur with depression and anxiety as common and detrimental comorbidities among the growing population living with chronic conditions. Digital health interventions (DHIs) hold promise in overcoming barriers to accessing mental health support for these individuals; however, the design and implementation of DHIs for depression and anxiety in people with chronic conditions are yet to be explored.
Objective
This study aimed to explore what is known in the literature regarding DHIs for the prevention, detection, or treatment of depression and anxiety among people with chronic conditions.
Methods
A scoping review of the literature was conducted using the Arksey and O’Malley framework. Searches of the literature published in 5 databases between 1990 and 2019 were conducted in April 2019 and updated in March 2021. To be included, studies must have described a DHI tested with, or designed for, the prevention, detection, or treatment of depression or anxiety in people with common chronic conditions (arthritis, asthma, diabetes mellitus, heart disease, chronic obstructive pulmonary disease, cancer, stroke, and Alzheimer disease or dementia). Studies were independently screened by 2 reviewers against the inclusion and exclusion criteria. Both quantitative and qualitative data were extracted, charted, and synthesized to provide a descriptive summary of the trends and considerations for future research.
Results
Database searches yielded 11,422 articles across the initial and updated searches, 53 (0.46%) of which were included in this review. DHIs predominantly sought to provide treatment (44/53, 83%), followed by detection (5/53, 9%) and prevention (4/53, 8%). Most DHIs were focused on depression (36/53, 68%), guided (32/53, 60%), tailored to chronic physical conditions (19/53, 36%), and delivered through web-based platforms (20/53, 38%). Only 2 studies described the implementation of a DHI.
Conclusions
As a growing research area, DHIs offer the potential to address the gap in care for depression and anxiety among people with chronic conditions; however, their implementation in standard care is scarce. Although stepped care has been identified as a promising model to implement efficacious DHIs, few studies have investigated the use of DHIs for depression and anxiety among chronic conditions using such models. In developing stepped care, we outlined DHI tailoring, guidance, and intensity as key considerations that require further research.
Keywords: depression, anxiety, multiple chronic conditions, chronic disease, mental health, psychiatry, digital health, eHealth, telehealth, mobile health, mHealth, telemedicine
Introduction
Background
Chronic conditions often co-occur despite an emphasis on their singular occurrence in health interventions, research, and care [1,2]. Chronic conditions persist for long durations (≥1 year), require ongoing medical attention, and limit activities of daily living [3]. In Canada, national data have identified several common chronic conditions, including arthritis, asthma, diabetes mellitus, heart disease, chronic obstructive pulmonary disease, cancer, stroke, mood and anxiety disorders, and Alzheimer disease and related dementias [4]. When poorly managed, these conditions have been associated with negative outcomes, such as poor quality of life [5], increased health care use [6], and higher costs [7].
Concomitant mood and anxiety disorders, such as depression and anxiety, are of particular concern because of their high prevalence [8-10] and burden [11-13] but are often underdetected and undertreated [14,15]. Prevalence estimates of depression (9.3%-23% [16]) and anxiety (2.9%-8.8% [12]) range widely and often vary based on the type and severity of co-occurring chronic conditions. Nevertheless, several studies have suggested that these rates are higher among patients with co-occurring chronic conditions than among those without the conditions [17,18]. Independently, depression has been associated with decrements in physical health outcomes and quality of life [16] for people with chronic conditions, including poor chronic disease self-management [19], worse outcomes for co-occurring physical conditions [20], adverse health system outcomes such as higher use of urgent care [21], and higher costs [22]. Similar impacts have been found for anxiety with chronic conditions [19,23], although this has been less studied. People with chronic conditions face additional challenges in accessing health support in the face of multiple appointments, transportation barriers, and treatment burdens [24]. These barriers may be especially pronounced for those with depression or anxiety, who may have added challenges in accessing support owing to their mental health status and stigma [25].
Digital health interventions (DHIs), that is, health interventions delivered through digital technologies, may help overcome barriers to both delivering mental health care (ie, stigma and access) and care for chronic conditions (ie, communication barriers and lack of appropriate information) [26,27] because of their ability to be accessed remotely, discreetly, and in real time. Existing meta-analytic research [28-34] suggests that DHIs are effective interventions for improving both psychological and disease-specific outcomes for populations with chronic conditions, with small to moderate effect sizes [28,30,32]. The most recent and largest of these meta-analyses reported that self-guided web-based interventions were associated with significant reductions in depression and anxiety compared with usual care or waitlist control, with small effect sizes [34]. However, existing reviews have been limited to a narrow set of therapeutic strategies (eg, self-help [34,35], mindfulness interventions [31,36], cognitive behavioral therapy [CBT]; [28,30,32]), technologies (eg, web-based platforms) [28,30,32,34-36], and outcomes (eg, effectiveness) [28,30-37], leaving the design and implementation of such technologies less clear.
Objectives
To complement previous reviews, this study sought to examine a wider range of technologies (mobile apps, telemonitoring systems, etc), functions DHIs may serve with respect to depression and anxiety (prevention, detection, or treatment), and study designs (qualitative, quantitative, pilot studies, etc). Specifically, this scoping review aimed to explore what is known about DHIs to prevent, detect, and treat depression or anxiety among people living with chronic conditions. To our knowledge, this is the first scoping review of primary research on DHIs for depression or anxiety in people with chronic conditions.
Methods
Overview
This scoping review was based on the following framework for conducting scoping reviews as developed by Arksey and O’Malley [38] and refined by Levac et al [39]: (1) identifying the research questions in light of the research purpose; (2) identifying relevant studies while balancing feasibility with comprehensiveness; (3) identifying the study selection criteria using an iterative team approach; (4) charting the data to provide both a numerical summary and thematic analysis; and (5) reporting the results with implications for policy, practice, and research identified [1]. In addition to the framework by Arksey and O’Malley [38] and Levac et al [39], this review adhered to the scoping review guidelines outlined by the JBI [40]. Informed by these frameworks, the actions taken at each stage of the scoping review process are described in the following sections [2].
Stage 1: Identifying the Research Question
This scoping review was guided by the following research question: What is known about the use of DHIs to support the prevention, detection, or treatment of depression or anxiety among people with chronic conditions? To address this research question, this study sought to (1) describe the nature and extent of DHIs to support the prevention, detection, and treatment of depression or anxiety among people with chronic conditions; (2) describe existing research and its overall findings; and (3) identify gaps and opportunities for future research.
Stage 2: Identifying Relevant Studies
This scoping review was designed and reported in line with the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist (Multimedia Appendix 1) [41]. A protocol was developed to guide this review; however, it was not registered. Studies relevant to the research question were identified through searches of the following databases: Embase, CINAHL, PsycINFO, MEDLINE, and the Cochrane Library using terms related to the concepts of “digital health,” “chronic disease,” “depression,” and “anxiety.” As recommended by the Joanna Briggs Institute [40], a 3-step process was used to develop the search strategy. First, initial searches of MEDLINE and PsycINFO were conducted to identify the terms used in the titles and abstracts of the articles. This first step helped identify relevant keywords and subject headings. Second, terms identified in the initial searches were arranged into a search strategy for MEDLINE, which was later tailored and revised for other databases. An iterative team approach was used to develop the search strategy [39] by consulting with a discipline-specific research librarian and seeking feedback from the research team. After tailoring the initial search strategy for MEDLINE to the rest of the databases (Embase, CINAHL, PsycINFO, and the Cochrane Library), searches of all databases were conducted initially in April 2019 and later updated in March 2021 to capture new publications between April 2019 and March 2021. The search strategy for all databases was saved to ensure reproducibility of the search results (see Multimedia Appendix 2 for the search strategy for MEDLINE). In the third step, the reference lists of relevant studies were examined in other studies that could be pertinent to the research question. Journals related to digital health (Journal of Medical Internet Research and Internet Interventions) were also hand searched for potentially relevant articles.
Stage 3: Study Selection
The results of the research strategy were saved in the reference management software Mendeley (Elsevier) to identify duplicates and were then exported to Rayyan [42], an internet-based platform designed to expedite the process of screening articles in systematic reviews. As outlined by Arksey and O’Malley [38], studies were selected based on their relevance to the scoping review question rather than their methodological rigor. The studies were reviewed based on the inclusion and exclusion criteria listed in Textbox 1.
Study eligibility criteria.
Inclusion criteria
Article published in English in a peer-reviewed academic journal
Published after 1990, owing to our interest in newer technologies
Describe a digital health intervention (DHI) defined as a health intervention delivered via digital technologies including but not limited to web-based platforms, videoconferencing, mobile phone apps, SMS text messages, email, wearable devices, and monitoring sensors
Study population of individuals aged ≥18 years with one or more of the common chronic conditions identified by the Public Health Agency of Canada (PHAC) [43]: arthritis, asthma, diabetes mellitus, heart disease, chronic obstructive pulmonary disease, cancer, stroke, and Alzheimer disease and related dementias [4]. Although depression and anxiety are also deemed common chronic conditions per PHAC, these conditions were selected because of their high rate of comorbidity with the other common chronic conditions listed [8-10].
-
Intervention objective, in whole or in part, related to the prevention, detection, or treatment of depression or anxiety. This was operationalized by studies that either
Included a study population with depression or anxiety in addition to one or more of the common chronic conditions outlined by PHAC [43].
Explicitly stated that the intervention sought to prevent, detect, or treat depression or anxiety among those with one or more of the common chronic conditions outlined by PHAC [43].
Exclusion criteria
Editorials, case reports, abstracts, posters, or dissertations
Interventions that solely used the phone calling functionality of telephones [44] (including interactive voice response) were not included in our definition of DHIs stated previously
Interventions for other mood or mental disorders beyond depression and anxiety
Studies with a mixed youth and young adult population (eg, [45])
Lifestyle or survivorship programs
Overall, 2 reviewers (AS and NHS) screened studies yielded by the search strategy by title and abstract and excluded studies if they met any of the exclusion criteria. Rayyan QCRI [42] was used to coordinate screening between the reviewers. Efforts were made to retain studies until full-text review if the reviewers were unsure about the eligibility of the studies with respect to the scoping review criteria. Review articles (ie, systematic reviews, meta-analyses, meta-syntheses, scoping reviews, narrative reviews, rapid reviews, critical reviews, and integrative reviews) were collected, and the reference lists were scanned for potentially relevant articles. Once the reference lists were scanned and potentially relevant articles were identified, the review articles were excluded. The full text of the remaining studies was reviewed according to the inclusion and exclusion criteria. Studies that met the inclusion criteria and those that did not meet the exclusion criteria were included in the scoping review. Studies that met the exclusion criteria were excluded, and the reasons were recorded. Disagreements between the reviewers were resolved through discussion until a consensus was reached, and a third reviewer (ES) was engaged when needed to resolve any remaining conflicts.
Stage 4: Data Collection
Two reviewers (AS and NHS) independently extracted data from the studies included in the scoping review using a data extraction form. A preliminary data extraction form was drafted in Microsoft Excel with the following column headings: title, year of publication, study details (eg, location, objective, research design, methods, eligibility criteria, target population, conditions, outcomes measured, and findings), and intervention details (eg, name, goal, technology, therapeutic components, and guidance [where any in-person or digital correspondence with a human was considered guided]). The form was modified and revised as necessary during the charting process. Discrepancies between the reviewers regarding the extracted data were resolved through discussion.
Stage 5: Data Summary and Synthesis of Results
Data analysis was performed using the following steps. First, the results of the nature and extent of the studies and interventions were summarized. Second, details related to the findings of existing studies were collated, and trends were discussed with both reviewers (AS and NHS) to identify opportunities for further research.
Results
Overview
Initial searches of 5 databases in April 2019 yielded 6695 results, with one additional article identified through hand searches of a relevant journal (Journal of Medical Internet Research; Figure 1). After removing duplicates (n=381), two authors (AS and NHS) screened 6315 records by title and abstract. At this stage, 6228 articles were excluded, including 74 reviews whose reference lists were checked for potentially relevant articles. An additional 3 relevant studies were identified from these reference lists. This left 87 articles to be assessed by full text against the inclusion and exclusion criteria by an author (AS). Of these 87 articles, 61 (70%) were excluded for the following reasons: the study population or intervention goal was not depression or anxiety among individuals with common chronic conditions as identified by the Public Health Agency of Canada [43] (32/61, 52%), the intervention was not a DHI (15/61, 25%), and the intervention relied exclusively on phone calls (14/61, 23%). This resulted in a total of 26 articles. A search update was conducted using the same search strategy in March 2021 for studies published between April 2019 and March 2021. The search update yielded 5001 articles, 4727 (94.52%) and 4610 (92.18%) of which were reviewed in duplicate (AS and NHS) and excluded by title and abstract, respectively. The full text of the remaining 117 studies was reviewed, with 93 (79.5%) studies excluded, resulting in another 24 (20.5%) articles included. An additional 3 articles were identified by screening the reference lists. Overall, 53 articles [46-99] were included in this review (Multimedia Appendix 3 [46,47,50,52,54,55,57-60,62,64-66,70-72,74,77,78,80,81,84,86,88,90-92,95,96,98,99]). The following sections outline the characteristics of the included studies and report the details related to study objectives 1 and 2.
Figure 1.
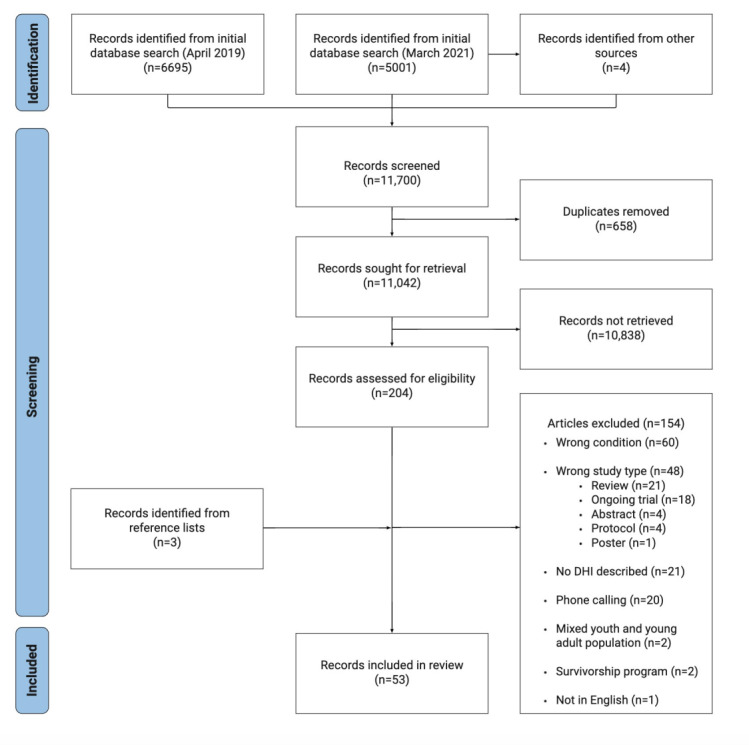
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram. DHI: digital health intervention.
Study Characteristics
Publication Frequency
Table 1 shows the frequency of the included studies by publication year. From 1990 to 2010, no study met our inclusion criteria, highlighting the recent and emerging nature of this area of research. The first study emerged in 2011, with most studies meeting the criteria published in 2019 (16/53, 30%).
Table 1.
Number of included articles by year of publication (N=53).
| Year | Studies, n (%) |
| 2011 | 3 (6) |
| 2012 | 1 (2) |
| 2013 | 1 (2) |
| 2014 | 1 (2) |
| 2015 | 3 (6) |
| 2016 | 5 (9) |
| 2017 | 4 (8) |
| 2018 | 5 (9) |
| 2019 | 16 (30) |
| 2020 | 13 (25) |
| 2021 | 1 (2) |
Setting
The included studies were predominantly conducted in the United States (15/53, 28%), Sweden (7/53, 13%), Australia (6/53, 11%), Canada (3/53, 6%), and India (4/53, 8%). Other study locations included Germany (3/53, 6%), the Netherlands (2/53, 4%), the United Kingdom (2/53, 4%), China (2/53, 4%), Peru (1/53, 2%), and Jordan (1/53, 2%; Table 2). A total of 4 studies did not specify the study location. On the basis of economy type (as determined by the World Bank classification [100]), studies were largely conducted in high-income countries (38/53, 72%) and to a lesser extent in upper–middle-income countries (4/53, 8%) and lower–middle-income countries (4/53, 8%). There were 3 instances in which studies involved multiple locations; however, these collaborations were between countries with similar economy types: multiple high-income countries (2/53, 4%) and between upper middle-income countries (1/53, 2%).
Table 2.
Summary of study characteristics (N=53).
|
|
Studies, n (%) | References | |
| Study location | |||
|
|
United States | 15 (28) | [48,54,58,62,66,69,76,79,82,84,87,89,94,95,97] |
|
|
Sweden | 7 (13) | [47,65,77,80,81,86,92] |
|
|
Australia | 6 (11) | [57,63,85,91,93,96] |
|
|
Canada | 3 (6) | [67,78,83] |
|
|
India | 4 (8) | [61,72,73,75] |
|
|
Germany | 3 (6) | [71,98,99] |
|
|
The Netherlands | 2 (4) | [52,88] |
|
|
United Kingdom | 2 (4) | [49,59] |
|
|
China | 2 (4) | [53,70] |
|
|
Peru | 1 (2) | [90] |
|
|
Jordan | 1 (2) | [51] |
|
|
Location not reported | 4 (8) | [50,55,60,64] |
| Economy type | |||
|
|
HICa | 38 (72) | [47-49,52,54,57-59,62,63,65-67,69,71,76-89,91-99] |
|
|
UMICb | 4 (8) | [51,53,68,70] |
|
|
Lower–middle-income country | 4 (8) | [61,72,73,75] |
|
|
Multiple HICs | 2 (4) | [56,74] |
|
|
Multiple UMICs | 1 (2) | [68] |
| Requirements for study eligibility | |||
|
|
Access or ownership of a digital device | 13 (25) | [49,59,63,65,73,82,85,87,91,93,95,97,98] |
|
|
Internet access | 9 (17) | [47,52,59,62,63,65,67,91,98] |
|
|
Digital literacy or skills | 6 (11) | [48,57,70,74,82,88] |
|
|
Owning an email address | 3 (6) | [52,74,98] |
| Sample sex distributions: predominantly female (≥60%) | 29 (55) | [49,51,52,54,55,57,60,62-64,68,74,76-81,83,87-91,93,94,97-99] | |
| Research design | |||
|
|
Randomized controlled trial | 29 (55) | [49,51-53,57-59,62,65,67,70-72,75,78,79,81,83-85,87-89,91,92,95,96,98,99] |
|
|
Quasi-experimental | 5 (9) | [47,60,63,68,76] |
|
|
Grounded theory | 2 (4) | [50,64] |
|
|
Observational | 1 (2) | [73] |
|
|
Case study | 1 (2) | [66] |
|
|
Phenomenological | 1 (2) | [56] |
| Methods | |||
|
|
Quantitative | 23 (43) | [52,58,60,62,65,68,73,74,76,78,83,84,88,89,91,93,99,101-106] |
|
|
Qualitative | 9 (17) | [50,55,56,64,66,77,80,90,97] |
|
|
Multi-methods | 8 (15) | [47,48,54,63,69,74,75,89] |
aHIC: high-income country.
bUMIC: upper–middle-income country.
Population
The sample size ranged from 6 to 3698. Approximately 40% (22/54) of the included studies specified digital requirements for study eligibility, such as access to or ownership of a digital device (13/53, 25%), internet access (9/53, 17%), digital literacy or skills (6/53, 11%), and owning an email address (3/53, 6%). Most articles reported that the study population was predominantly (≥60%) female (29/53, 55%).
Methods
Among the studies that reported a research design, the randomized controlled trial design was typically used (29/53, 55%), followed by quasi-experimental (5/53, 9%), grounded theory (2/53, 4%), observational design (1/53, 2%), case study (1/53, 2%), and phenomenological design (1/53, 2%). Different methods were used among the included studies, including quantitative (23/53, 43%), qualitative (9/53, 17%), and multi-methods research (8/53, 15%). A total of 3 articles [61,85,86] described the development of a DHI or the lessons learned in conducting a study but did not state a qualitative methodology.
Nature and Extent of DHIs
Intervention Purpose and Digital Technologies
The 53 studies included in this review described 36 unique DHIs. The purpose of the interventions was distributed as follows: prevention (4/53, 8%), detection (5/53, 9%), and treatment (44/53, 83%; Table 3). Over the past decade, the technologies most commonly used to deliver these interventions were web-based platforms (20/53, 38%) and mobile devices (17/53, 32%). Telehealth systems (3/53, 6%), electronic health records (2/53, 4%), and virtual reality devices (1/53, 2%) were also used. Several studies have described DHIs that leverage multiple technologies (10/53, 19%).
Table 3.
Summary of intervention characteristics (N=53).
|
|
Studies, n (%) | References | |||
| Purpose | |||||
|
|
Prevention | 4 (8) | [57,89,93,96] | ||
|
|
Detection | 5 (8) | [56,67,73,76,82] | ||
|
|
Treatment | 44 (83) | [47-55,58-66,68-72,74,75,77-81,83-88,90-92,94,95,97-99] | ||
| Technology | |||||
|
|
Web based | 20 (38) | [47,49,52,54,58,62,65,74,77,80,81,84-86,88,91-93,96,98] | ||
|
|
Mobile device | 17 (32) | [48,53,56,61,67-70,73,75,79,82,87,89,90,94,97] | ||
|
|
Telehealth system | 3 (6) | [66,71,95] | ||
|
|
Electronic health records | 2 (4) | [72,76] | ||
|
|
Virtual reality | 1 (2) | [51] | ||
|
|
Multiple technologies | 10 (19) | [50,55,57,59,60,63,64,78,83,99] | ||
| Target conditions (mental) | |||||
|
|
Depression | 36 (68) | [50,52,55-58,60-66,68,69,71-76,78,82-85,87,88,90-93,95,97-99] | ||
|
|
Anxiety | 3 (6) | [51,59,79] | ||
|
|
Depression and anxiety | 14 (26) | [47-49,53,54,67,70,77,80,81,86,89,94,96] | ||
| Target conditions (physical) | |||||
|
|
Diabetes | 19 (36) | [49,52,61,63,68,72-76,82,85,88,90,91,93,95,98,99] | ||
|
|
Cancer | 13 (25) | [51,53,54,70,77,79-81,86,87,94,96,97] | ||
|
|
Hypertension | 5 (9) | [47,61,68,75,90] | ||
|
|
Heart failure | 3 (6) | [65,71,92] | ||
|
|
Chronic obstructive pulmonary disease | 2 (4) | [56,67] | ||
|
|
Stroke | 1 (2) | [59] | ||
|
|
Any chronic condition | 8 (15) | [50,55,60,62,64,66,69,84] | ||
|
|
Multiple chronic conditions | 6 (11) | [48,57,58,78,83,89] | ||
| Role of digital health intervention | |||||
|
|
Sole intervention | 42 (79) | [47-52,55,57,59,60,62-65,68,69,71,73,74,77-99] | ||
|
|
Component of intervention | 11 (21) | [53,54,56,58,61,66,67,70,72,75,76] | ||
| Intervention components | |||||
|
|
Education | 30 (57) | [46,49,50,52,55,59,60,63,64,66,67,69,70,73,74,77,78,80,81,83-86,88-91,93,94,96] | ||
|
|
Cognitive behavioral therapy | 21 (40) | [47,49,51,52,59,63,65,69,70,74,75,77-81,83,85,92-94] | ||
|
|
Behavioral activation | 4 (8) | [46,73,90,91] | ||
|
|
Problem-solving therapy | 2 (4) | [73,91] | ||
|
|
Acceptance and commitment therapy | 1 (2) | [54] | ||
|
|
Monitoring mental health status or symptoms | 14 (26) | [48,49,56,57,63,69,72,78,82,83,85,88,93,98] | ||
|
|
Peer support | 9 (17) | [50,55,60,64,66,77,80,81,86] | ||
|
|
Communication with health care providers | 9 (17) | [48,67,71,72,77,80,81,86,95] | ||
|
|
Mindfulness | 3 (6) | [75,87,97] | ||
|
|
Chat rooms or forums | 7 (13) | [66,77,80,81,84,86,96] | ||
| Tailoring: tailored to chronic physical conditions | 19 (36) | [47,48,52,54,59,65,70,73,74,77,79-81,84,86,88,91,92,96] | |||
| Guidance: guided | 32 (60) | [46,47,50-52,55,58-60,64-66,69-74,77,78,80,81,83,84,86,90-92,94-96,98] | |||
| Guidance provider | |||||
|
|
Nurse | 9 (17) | [47,65,68,70,71,86,90,92,96] | ||
|
|
Psychologist | 6 (11) | [52,57,74,88,91,98] | ||
|
|
Certified peer specialist | 4 (8) | [50,55,60,64] | ||
|
|
Trained lay individual | 2 (4) | [78,83] | ||
|
|
Allied health professional | 2 (4) | [1,2] | ||
|
|
Study staff members | 2 (4) | [58,62] | ||
|
|
Physician | 1 (2) | [59] | ||
|
|
Multiple professionals | 6 (11) | [54,77,80,81,84,99] | ||
|
|
Unclear | 1 (2) | [66] | ||
| Guidance purpose | |||||
|
|
Responding to questions | 11 (21) | [47,57,62,65,77,80,81,86,92,95,96] | ||
|
|
Information and feedback | 9 (17) | [52,74,80,81,88,95,96,98,99] | ||
|
|
Promoting engagement and adherence | 8 (15) | [50,55,57,60,62,64,91,99] | ||
|
|
Sending reminders | 7 (13) | [47,52,65,74,88,92,98] | ||
|
|
Offering support | 6 (11) | [50,55,60,64,70,91] | ||
|
|
Monitoring symptoms | 4 (8) | [72,78,83,95] | ||
|
|
Training to use the intervention | 4 (8) | [58,68,90,95] | ||
|
|
Encouragement or positive reinforcement | 4 (8) | [57,68,90,95] | ||
|
|
Moderating forum | 3 (6) | [80,81,86] | ||
|
|
Counseling | 2 (4) | [59,72] | ||
|
|
Check-ins | 1 (2) | [54] | ||
|
|
Unclear | 2 (4) | [66,84] | ||
| Delivery of guidance | |||||
|
|
Combination | 13 (25) | [50,54,55,57,60,64,72,77,90,91,95,98,99] | ||
|
|
Phone calls | 7 (13) | [59,68,71,78,83,84,96] | ||
|
|
Emails | 6 (11) | [47,52,65,74,88,92] | ||
|
|
Web-based messages | 3 (6) | [80,81,86] | ||
|
|
In-person visits | 2 (4) | [58,62] | ||
|
|
WeChat messages | 1 (2) | [70] | ||
|
|
Unclear | 1 (2) | [66] | ||
Target Conditions
Most of the studies included in this review sought to address depression (36/53, 68%) among those with chronic conditions, with some studies (14/53, 26%) focusing on both depression and anxiety. Only 6% (3/32) of studies focused exclusively on anxiety. Regarding co-occurring chronic conditions, most interventions were designed for people with diabetes (19/53, 36%) and cancer (13/53, 25%). Other chronic physical conditions represented in the included studies were hypertension (5/53, 9%), heart failure (3/53, 6%), chronic obstructive pulmonary disease (2/53, 4%), and stroke (1/53, 2%). In addition, 8 studies were for any chronic condition, and 6 studies were for multiple chronic conditions (2 or more chronic physical conditions).
Intervention Design and Components
Of the 53 included studies, 42 (79%) described the DHI as the sole intervention, whereas in 11 (21%) studies, the DHI was a component of the intervention. DHIs commonly included education (30/53, 57%), psychological therapy (28/53, 53%; eg, CBT 21/53, 40%; behavioral activation 4/53, 8%; problem-solving therapy 2/53, 4%; and acceptance and commitment therapy 1/53, 2%), and monitoring of mental health status or symptoms (14/53, 26%). However, peer support (9/53, 17%), communication with health care providers (9/53, 17%), mindfulness (3/53, 6%), and chat rooms or forums (7/53, 13%) were also used. Mental health intervention content was frequently tailored to chronic physical conditions (19/53, 36%; Multimedia Appendix 4 [47-99]).
Most interventions included in this review were guided (32/53, 27%), with the frequency at which guidance was provided ranging from as needed to daily (Multimedia Appendix 5 [47-99]). Among the guided interventions, the provider of guidance varied widely across the studies, including nurse specialists, nurse practitioners, or nurse assistants (9/32, 28%); psychologists (6/32, 19%); certified peer supporters (4/32, 13%); trained lay individuals (2/32, 6%); allied health professionals (2/32, 6%; eg, dieticians or social workers 1/32, 3% and pharmacists 1/32, 3%); study staff members (2/32, 6%); and physicians (1/32, 3%). In 19% (6/32) of studies, guidance was provided by multiple professionals (eg, nurses and psychologists, social workers and psychologists, psychology graduate students, and psychologists). In 3% (1/32) of studies, the provider of guidance was unclear. Guidance served a wide range of functions, including responding to questions (11/32, 34%), providing information and feedback (9/32, 28%), promoting engagement and adherence (8/32, 25%), sending reminders (7/32, 22%), offering support (6/32, 19%), monitoring symptoms (4/32, 13%), training to use the intervention (4/32, 13%), providing encouragement or positive reinforcement (4/32, 13%), moderating a forum (3/32, 9%), counseling (2/32, 6%), and check-ins (1/32, 3%). In some studies (2/32, 6%), the purpose of guidance was unclear. Of the studies describing a guided intervention, most (13/32, 41%) used a combination of modalities (eg, in-person, phone calls, and SMS text messages) to provide guidance. In some studies, guidance was offered exclusively through phone calls (7/32, 22%), emails (6/32, 19%), web-based messages (3/32, 9%), in-person visits (2/32, 6%), and WeChat messages (1/32, 3%). In 3% (1/32) of studies, the method of delivery for guidance was unclear.
Findings of Existing Studies
The objectives of the included studies ranged from design and development (5/53, 9%), feasibility and acceptability (19/53, 36%), determining effectiveness (17/53, 32%) or efficacy (7/53, 13%) of the DHI, and conducting a secondary analysis to explore predictors, mediators, or moderators of DHI outcomes (6/53, 11%; Table 4). Only 4% (2/32) of studies described the implementation of an intervention, one of which [48] described a planned study but was included because of its discussion of the strategies used to implement the DHI. Other study objectives were to describe the adherence and use of a DHI (1/53, 2%), evaluate a prediction model (1/53, 2%), determine the validity of delivering screening tools via text (1/53, 2%), and analyze SMS text messages from a DHI (1/53, 2%). Several studies reported objectives spanning multiple research stages (8/53, 15%). Among the studies investigating the effectiveness (17/53, 32%) or efficacy (7/53, 13%) of a DHI, 54% (13/32) of studies reported significant changes in mental health outcomes. A study reported significant changes in patients’ health behavior (medication adherence [95]) and another in health care provider behavior (depression screening [76]). Multimedia Appendix 3 provides a detailed summary of the findings of each study included in the review.
Table 4.
Summary of study findings (N=53).
|
|
Studies, n (%) | References | |
| Study objective | |||
|
|
Design and development | 5 (9) | [47,61,69,74,86] |
|
|
Feasibility and acceptability | 19 (36) | [47,50,54,56,59,60,62-64,66,68,70,76,77,80,85,87,90,97] |
|
|
Effectiveness | 17 (32) | [51-53,58,60,63,65,68,70,72,75,76,78,81,89,93,96] |
|
|
Efficacy | 7 (13) | [49,57,79,84,91,95,99] |
|
|
Secondary analysis | 6 (11) | [71,83,88,92,94,98] |
|
|
Implementation | 2 (4) | [48,70] |
|
|
Other | 3 (6) | [1-3] |
| Impact: significant differences in mental health outcomes | 13 (25) | [51,52,57,58,62,63,68,70,72,78,81,91,99] | |
Discussion
Principal Findings
This review aimed to explore what is known about DHIs to prevent, detect, and treat depression or anxiety among people with chronic conditions. This review extends the existing meta-analytic evidence of DHIs by reviewing technologies beyond web-based platforms and exploring design and implementation considerations. The findings of this review highlight the significant potential of DHIs to have a profound public health impact on people living with chronic conditions. Per study objective 3, the following section outlines opportunities for further research for this rapidly growing area of investigation: tailoring, guidance, intensity, and stepped care.
Opportunities for Further Research
Tailoring
There was mixed evidence among the studies reviewed regarding the value of tailoring the intervention content to chronic physical conditions. The benefits of both condition-specific and generic DHIs were discussed among the studies reviewed. For instance, van Bastelaar et al [74] found that 80% of the patients reported that a diabetes-specific approach for coping with depression intervention was needed. In a previous review, van Beugan et al [30] highlighted the importance of disease-specific tailoring in attributing the larger improvements in disease-related outcomes observed among these interventions for this feature. However, studies in our review also indicated that generic DHIs were beneficial in addressing depression among people with chronic conditions [58,62,91]. It is possible that certain conditions may require a condition-specific approach owing to the existence of condition-specific mental health constructs (eg, diabetes distress) [93]. However, the growing prevalence of multiple chronic conditions globally and emerging literature on transdiagnostic interventions for depression and anxiety [107-109] calls into question the value of disease-specific approaches.
The studies in this review also proposed additional tailoring factors for future consideration. In a qualitative investigation, Igelström et al [80] recommended further tailoring of DHI information, design, and features to the individual with regard to their treatment as well as other factors that appeared to affect the user’s experience such as computer experience, internet activity, and interactions with social media. In another study on the same platform [77], patients desired further tailoring to their specific diagnosis, age, sex, treatment, and symptoms, despite the DHI being tailored to the condition (cancer). For the PeerTECH intervention, certified peer specialists personalized SMS text messages on topics such as stories of recovery, medication adherence, coping skills training, and sleep hygiene [50]. Others have raised the possibility of tailoring to participants’ preconceptions of the interventions, such as meditation [97] and symptom tracking [80]. Thus, although tailoring can be an important component of DHIs for this population, whether tailoring should be to the person instead of the condition requires further investigation.
Guidance
Interventions reported among the included studies were predominately guided; however, both guided and self-guided DHIs were represented among studies reporting effective outcomes, suggesting that outcomes may not be compromised without guidance. The qualifications of individuals providing guidance varied considerably (eg, laypersons to psychiatrists), as did their training and role in the intervention. Similar findings regarding the heterogeneity in the guidance of internet-based CBT for chronic conditions have been reported previously by a meta-analysis by van Began et al [30]. Such variability may arise because of confusion regarding whether guidance constitutes the intervention itself or the supporting context (promoting engagement with technology or study procedures). Indeed, although several interventions relied on guidance to promote engagement with the intervention [50,55,57,60,64,91,99], studies have noted that this limited the scalability of the intervention. Guidance provided by lay individuals and peer supporters was feasible and well accepted [46,60], whereas interventions supported by nurses at times faced challenges in integrating additional workload into their roles [90]. Although several alternatives exist to improve the feasibility of guidance (eg, reduced frequency of guidance, partial guidance, no guidance, blending guided sessions with self-help modules [110], and automated guidance via chatbots [80]), the findings of this review and previous studies underscore the potential for allied health professionals and nonclinicians in guiding DHIs. Nevertheless, clarity is needed regarding the time spent by these individuals and the nature of the support provided (ie, technical support or health-related support) to understand how to support DHIs safely and effectively for this population.
Intensity
Given the complexity of the population with chronic conditions and comorbid depression or anxiety, identifying for whom DHIs are most appropriate was a significant line of investigation [88,94,98]. Among the studies included in this review, those with more severe depressive symptoms often benefited most from DHI treatment. Puzia et al [94] found that patients with myeloproliferative neoplasms with the poorest baseline global mental health experienced the largest reductions in depression and anxiety symptoms when using a calm mindfulness meditation app. Similarly, despite finding no significant differences in anxiety between a tailored CBT app and control, Greer et al [79] reported that patients with more severe anxiety at baseline benefited the most from the CBT app. Although it is commonly accepted that those with more severe mental health symptoms warrant more intensive treatment [111,112], the findings of this review and previous studies suggest that these individuals also benefit from DHIs [113-115]. Taken together, these findings indicate that individuals with severe symptoms of depression or anxiety can benefit from interventions of varying intensity, especially when intensity is defined by clinician time and contacts. It should be noted that the qualitative findings of the included studies reported that participants found DHIs to be demanding in terms of the time and skills required to read the intervention content and completing exercises in addition to the work involved in learning a new platform and troubleshooting technical and navigation issues [47]. Therefore, an expanded conceptualization of intervention intensity may be fruitful in not only considering intervention intensity in terms of health system resources (eg, clinician time and involvement) but also the patient work involved.
Stepped Care
Presumably, resolving the mixed findings regarding the previously mentioned factors may not require standardizing the same level of guidance and tailoring for all interventions. It is possible that a variety of DHIs may be delivered and supported through a spectrum of guidance ranging from lay individuals to psychiatrists, with guidance tailored and intensified based on individual needs and preferences. This approach is consistent with a stepped care model that was envisioned to benefit from DHIs in several of the included studies [57,65,77,80,98] and previous reviews on this topic [28,35]. Although over a decade has passed since Cuijpers et al [28] first envisioned the role of DHIs for this population existing within stepped care models, this review identified that the application of these interventions in stepped care models has only recently begun. Nevertheless, the emerging work by Igelström et al [80] demonstrates the promise of this approach in their iCAN-DO stepped care model for patients with cancer, with depression or anxiety symptoms, which included nurse-led (step 1, psychoeducation) and psychologist-led (step 2, internet-based CBT) DHIs. As most patients (60%) in the study did not use the second step of support, a stepped care approach may allow for efficient use of scarce mental health human resources [80]. Early findings on the iCAN-DO stepped care intervention indicated promising results regarding the efficacy of this intervention with reductions in depressive symptoms in some patients with cancer [116]. However, more definitive research is needed to determine whether individuals with single and multiple chronic conditions [57] can benefit from stepped care models, particularly those delivered digitally.
Limitations
This review had several limitations. First, this review was limited to DHIs for depression or anxiety among people with one or more common chronic conditions identified by the Public Health Agency of Canada [43]. Although not included in this review, other chronic conditions not within the scope of this study (chronic pain, irritable bowel syndrome, tinnitus, epilepsy, etc) have been investigated in previous syntheses [28-32,35,37]. Second, despite engaging a discipline-specific research librarian when developing the search strategy and using multiple search methods (eg, hand searching and reviewing reference lists), the search strategy may have missed relevant studies. Third, because of our interest in DHIs that leverage newer technologies, studies that relied solely on phone calls were excluded. Thus, interventions that may be beneficial, such as telephone-based counseling [117-119] and automated telephone screening [120,121] were not within the scope of this study. As studies with older adults with chronic conditions have identified telephone-based support as a desirable component of mental health support [122], further research is needed on the use of phone calls. Fourth, the restriction to studies that were published in peer-reviewed journals in the English language may have missed publicly available DHIs (eg, mobile apps in app stores) that have not yet been researched or limited the inclusion of studies from non–English-speaking countries. Fifth, to be included, studies in this review must have recruited participants with co-occurring depression or anxiety with chronic conditions or explicitly stated that the goal of the DHI was to prevent, detect, or treat depression or anxiety among people with one or more chronic conditions. Broader aspects of mental health (ie, psychological distress [123], social support [124]), general self-management programs [125], and other mental health conditions (ie, eating disorders and substance use disorders) were beyond the scope of this study and warrant investigation [126].
Conclusions
Amidst meta-analytic research documenting the potential benefits of DHIs to address depression or anxiety among people living with chronic conditions, this scoping review addresses the paucity of research focusing on the design and implementation considerations of such interventions. This review found that the use of DHIs for depression or anxiety among individuals with chronic conditions is a rapidly growing area of research, with most interventions seeking to provide depression treatment using DHIs that are web based, guided, and tailored to chronic physical conditions. With few studies conducted to date, stepped care models are a promising model to implement efficacious DHIs into standard care, although more definitive research is needed to determine whether individuals with single and multiple chronic conditions can benefit from these models. In constructing such models, questions regarding DHI guidance, tailoring, and intensity are key considerations and require future research. Developments in these areas will aid in realizing the potential of DHIs to transform care for patients with chronic conditions consistent with their holistic health needs.
Abbreviations
- CBT
cognitive behavioral therapy
- DHI
digital health intervention
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist.
Sample search strategy (MEDLINE).
Summary of digital health interventions.
Summary of digital health intervention components.
Summary of digital health intervention guidance.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Garin N, Koyanagi A, Chatterji S, Tyrovolas S, Olaya B, Leonardi M, Lara E, Koskinen S, Tobiasz-Adamczyk B, Ayuso-Mateos JL, Haro JM. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci. 2016 Feb;71(2):205–14. doi: 10.1093/gerona/glv128. https://europepmc.org/abstract/MED/26419978 .glv128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Afshar S, Roderick PJ, Kowal P, Dimitrov BD, Hill AG. Multimorbidity and the inequalities of global ageing: a cross-sectional study of 28 countries using the World Health Surveys. BMC Public Health. 2015 Aug 13;15(1):776. doi: 10.1186/s12889-015-2008-7. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-2008-7 .10.1186/s12889-015-2008-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schenker M, Costa DH. Advances and challenges of health care of the elderly population with chronic diseases in Primary Health Care. Cien Saude Colet. 2019 Apr;24(4):1369–80. doi: 10.1590/1413-81232018244.01222019. https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-81232019000401369&lng=en&nrm=iso&tlng=en .S1413-81232019000401369 [DOI] [PubMed] [Google Scholar]
- 4.CCDI Steering Committee The 2017 Canadian chronic disease indicators. Health Promot Chronic Dis Prev Can. 2017 Aug;37(8):248–51. doi: 10.24095/hpcdp.37.8.03. doi: 10.24095/hpcdp.37.8.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fortin M, Bravo G, Hudon C, Lapointe L, Almirall J, Dubois M, Vanasse A. Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual Life Res. 2006 Feb;15(1):83–91. doi: 10.1007/s11136-005-8661-z. [DOI] [PubMed] [Google Scholar]
- 6.van Oostrom SH, Picavet HS, de Bruin SR, Stirbu I, Korevaar JC, Schellevis FG, Baan CA. Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam Pract. 2014 Apr 07;15(1):61. doi: 10.1186/1471-2296-15-61. https://bmcfampract.biomedcentral.com/articles/10.1186/1471-2296-15-61 .1471-2296-15-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bähler C, Huber CA, Brüngger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015 Jan 22;15:23. doi: 10.1186/s12913-015-0698-2. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-015-0698-2 .s12913-015-0698-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roy-Byrne PP, Davidson KW, Kessler RC, Asmundson GJ, Goodwin RD, Kubzansky L, Lydiard RB, Massie MJ, Katon W, Laden SK, Stein MB. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry. 2008;30(3):208–25. doi: 10.1016/j.genhosppsych.2007.12.006.S0163-8343(07)00259-9 [DOI] [PubMed] [Google Scholar]
- 9.Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009 Apr 06;190(S7):S54–60. doi: 10.5694/j.1326-5377.2009.tb02471.x.cla10974_fm [DOI] [PubMed] [Google Scholar]
- 10.Gold SM, Köhler-Forsberg O, Moss-Morris R, Mehnert A, Miranda JJ, Bullinger M, Steptoe A, Whooley MA, Otte C. Comorbid depression in medical diseases. Nat Rev Dis Primers. 2020 Aug 20;6(1):69. doi: 10.1038/s41572-020-0200-2.10.1038/s41572-020-0200-2 [DOI] [PubMed] [Google Scholar]
- 11.Schmitz N, Wang J, Malla A, Lesage A. Joint effect of depression and chronic conditions on disability: results from a population-based study. Psychosom Med. 2007 May;69(4):332–8. doi: 10.1097/PSY.0b013e31804259e0.PSY.0b013e31804259e0 [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Ormel J, Demler O, Stang PE. Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the National Comorbidity Survey. J Occup Environ Med. 2003 Dec;45(12):1257–66. doi: 10.1097/01.jom.0000100000.70011.bb. [DOI] [PubMed] [Google Scholar]
- 13.Scott KM, Bruffaerts R, Tsang A, Ormel J, Alonso J, Angermeyer MC, Benjet C, Bromet E, de Girolamo G, de Graaf R, Gasquet I, Gureje O, Haro JM, He Y, Kessler RC, Levinson D, Mneimneh ZN, Oakley Browne MA, Posada-Villa J, Stein DJ, Takeshima T, Von Korff M. Depression-anxiety relationships with chronic physical conditions: results from the World Mental Health Surveys. J Affect Disord. 2007 Nov;103(1-3):113–20. doi: 10.1016/j.jad.2007.01.015.S0165-0327(07)00017-1 [DOI] [PubMed] [Google Scholar]
- 14.Calleo J, Stanley MA, Greisinger A, Wehmanen O, Johnson M, Novy D, Wilson N, Kunik M. Generalized anxiety disorder in older medical patients: diagnostic recognition, mental health management and service utilization. J Clin Psychol Med Settings. 2009 Jun;16(2):178–85. doi: 10.1007/s10880-008-9144-5. https://europepmc.org/abstract/MED/19152056 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hill N, Joubert L, Epstein I. Encouraging self-management in chronically ill patients with co-morbid symptoms of depression and anxiety: an emergency department study and response. Soc Work Health Care. 2013;52(2-3):207–21. doi: 10.1080/00981389.2012.737900. [DOI] [PubMed] [Google Scholar]
- 16.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007 Sep 08;370(9590):851–8. doi: 10.1016/S0140-6736(07)61415-9.S0140-6736(07)61415-9 [DOI] [PubMed] [Google Scholar]
- 17.Patten SB. Long-term medical conditions and major depression in a Canadian population study at waves 1 and 2. J Affective Disord. 2001 Mar;63(1-3):35–41. doi: 10.1016/s0165-0327(00)00186-5. [DOI] [PubMed] [Google Scholar]
- 18.Gadalla T. Association of comorbid mood disorders and chronic illness with disability and quality of life in Ontario, Canada. Chronic Dis Can. 2008;28(4):148–54. doi: 10.24095/hpcdp.28.4.04. [DOI] [PubMed] [Google Scholar]
- 19.Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29(2):147–55. doi: 10.1016/j.genhosppsych.2006.11.005.S0163-8343(06)00220-9 [DOI] [PubMed] [Google Scholar]
- 20.Stein MB, Cox BJ, Afifi TO, Belik S, Sareen J. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective. Psychol Med. 2006 May;36(5):587–96. doi: 10.1017/S0033291706007239.S0033291706007239 [DOI] [PubMed] [Google Scholar]
- 21.Dickens C, Katon W, Blakemore A, Khara A, McGowan L, Tomenson B, Jackson J, Walker L, Guthrie E. Does depression predict the use of urgent and unscheduled care by people with long term conditions? A systematic review with meta-analysis. J Psychosom Res. 2012 Nov;73(5):334–42. doi: 10.1016/j.jpsychores.2012.08.018.S0022-3999(12)00223-1 [DOI] [PubMed] [Google Scholar]
- 22.Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, Galea A. Long-term Conditions and Mental Health The Cost of Co-morbidities. London, United Kingdom: The King's Fund; 2012. [Google Scholar]
- 23.Härter MC, Conway KP, Merikangas KR. Associations between anxiety disorders and physical illness. Eur Arch Psychiatry Clin Neurosci. 2003 Dec;253(6):313–20. doi: 10.1007/s00406-003-0449-y. [DOI] [PubMed] [Google Scholar]
- 24.Ho JW, Kuluski K, Im J. "It's a fight to get anything you need" - accessing care in the community from the perspectives of people with multimorbidity. Health Expect. 2017 Dec 24;20(6):1311–9. doi: 10.1111/hex.12571. doi: 10.1111/hex.12571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DiNapoli EA, Cinna C, Whiteman KL, Fox L, Appelt CJ, Kasckow J. Mental health treatment preferences and challenges of living with multimorbidity from the veteran perspective. Int J Geriatr Psychiatry. 2016 Oct 21;31(10):1097–104. doi: 10.1002/gps.4550. https://europepmc.org/abstract/MED/27442187 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mallow JA, Theeke LA, Theeke E, Mallow BK. The effectiveness of mI SMART: a nurse practitioner led technology intervention for multiple chronic conditions in primary care. Int J Nurs Sci. 2018 Apr 10;5(2):131–7. doi: 10.1016/j.ijnss.2018.03.009. https://linkinghub.elsevier.com/retrieve/pii/S2352-0132(17)30361-7 .S2352-0132(17)30361-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Melchiorre MG, Papa R, Rijken M, van Ginneken E, Hujala A, Barbabella F. eHealth in integrated care programs for people with multimorbidity in Europe: insights from the ICARE4EU project. Health Policy. 2018 Jan;122(1):53–63. doi: 10.1016/j.healthpol.2017.08.006. https://linkinghub.elsevier.com/retrieve/pii/S0168-8510(17)30206-3 .S0168-8510(17)30206-3 [DOI] [PubMed] [Google Scholar]
- 28.Cuijpers P, van Straten A, Andersson G. Internet-administered cognitive behavior therapy for health problems: a systematic review. J Behav Med. 2008 Apr;31(2):169–77. doi: 10.1007/s10865-007-9144-1. https://europepmc.org/abstract/MED/18165893 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matcham F, Rayner L, Hutton J, Monk A, Steel C, Hotopf M. Self-help interventions for symptoms of depression, anxiety and psychological distress in patients with physical illnesses: a systematic review and meta-analysis. Clin Psychol Rev. 2014 Mar;34(2):141–57. doi: 10.1016/j.cpr.2014.01.005. https://linkinghub.elsevier.com/retrieve/pii/S0272-7358(14)00033-6 .S0272-7358(14)00033-6 [DOI] [PubMed] [Google Scholar]
- 30.van Beugen S, Ferwerda M, Hoeve D, Rovers MM, Spillekom-van Koulil S, van Middendorp H, Evers AW. Internet-based cognitive behavioral therapy for patients with chronic somatic conditions: a meta-analytic review. J Med Internet Res. 2014 Mar 27;16(3):e88. doi: 10.2196/jmir.2777. https://www.jmir.org/2014/3/e88/ v16i3e88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mikolasek M, Berg J, Witt CM, Barth J. Effectiveness of mindfulness- and relaxation-based eHealth interventions for patients with medical conditions: a systematic review and synthesis. Int J Behav Med. 2018 Feb;25(1):1–16. doi: 10.1007/s12529-017-9679-7.10.1007/s12529-017-9679-7 [DOI] [PubMed] [Google Scholar]
- 32.Mehta S, Peynenburg VA, Hadjistavropoulos HD. Internet-delivered cognitive behaviour therapy for chronic health conditions: a systematic review and meta-analysis. J Behav Med. 2019 Apr;42(2):169–87. doi: 10.1007/s10865-018-9984-x.10.1007/s10865-018-9984-x [DOI] [PubMed] [Google Scholar]
- 33.Sasseville M, LeBlanc A, Tchuente J, Boucher M, Dugas M, Gisèle M, Barony R, Beaulieu M, Beaudet N, Cholette P, Aspiros C, Larouche A, Chabot G, Gagnon M-P. The impact of technology systems and professional support in digital mental health interventions: a secondary meta-analysis. medRxiv. 2021 Apr; doi: 10.1101/2021.04.12.21255333. https://www.medrxiv.org/content/10.1101/2021.04.12.21255333v1.abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.White V, Linardon J, Stone JE, Holmes-Truscott E, Olive L, Mikocka-Walus A, Hendrieckx C, Evans S, Speight J. Online psychological interventions to reduce symptoms of depression, anxiety, and general distress in those with chronic health conditions: a systematic review and meta-analysis of randomized controlled trials. Psychol Med. 2020 Jul 17;52(3):548–73. doi: 10.1017/s0033291720002251. [DOI] [PubMed] [Google Scholar]
- 35.Beatty L, Lambert S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin Psychol Rev. 2013 Jun;33(4):609–22. doi: 10.1016/j.cpr.2013.03.004.S0272-7358(13)00044-5 [DOI] [PubMed] [Google Scholar]
- 36.Toivonen KI, Zernicke K, Carlson LE. Web-based mindfulness interventions for people with physical health conditions: systematic review. J Med Internet Res. 2017 Aug 31;19(8):e303. doi: 10.2196/jmir.7487. https://www.jmir.org/2017/8/e303/ v19i8e303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sasseville M, LeBlanc A, Boucher M, Dugas M, Mbemba G, Tchuente J, Chouinard M, Beaulieu M, Beaudet N, Skidmore B, Cholette P, Aspiros C, Larouche A, Chabot G, Gagnon M. Digital health interventions for the management of mental health in people with chronic diseases: a rapid review. BMJ Open. 2021 Apr 05;11(4):e044437. doi: 10.1136/bmjopen-2020-044437. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33820786 .bmjopen-2020-044437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol. 2005 Feb;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 39.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010 Sep 20;5(1):69. doi: 10.1186/1748-5908-5-69. https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-5-69 .1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The Joanna Briggs Institute . Joanna Briggs Institute Reviewers’ Manual: 2014 edition / Supplement. Adelaide, Australia: The Joanna Briggs Institute; 2014. [Google Scholar]
- 41.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Oct 02;169(7):467–73. doi: 10.7326/M18-0850. https://www.acpjournals.org/doi/abs/10.7326/M18-0850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .2700389 [DOI] [PubMed] [Google Scholar]
- 42.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 05;5(1):210. doi: 10.1186/s13643-016-0384-4. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0384-4 .10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Varin M, Baker M, Palladino E, Lary T. Canadian Chronic Disease Indicators, 2019 - Updating the data and taking into account mental health. Health Promot Chronic Dis Prev Can. 2019 Oct;39(10):281–8. doi: 10.24095/hpcdp.39.10.02. doi: 10.24095/hpcdp.39.10.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ito H, Sato T, Satoh-Asahara N, Noda M. Impact of medication adherence on renal function in comorbid patients with type 2 diabetes and depression: protocol for a cohort study. BMC Fam Pract. 2015 Sep 15;16:124. doi: 10.1186/s12875-015-0339-1. https://bmcfampract.biomedcentral.com/articles/10.1186/s12875-015-0339-1 .10.1186/s12875-015-0339-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lunkenheimer F, Domhardt M, Geirhos A, Kilian R, Mueller-Stierlin AS, Holl RW, Meissner T, Minden K, Moshagen M, Ranz R, Sachser C, Staab D, Warschburger P, Baumeister H, COACH consortium Effectiveness and cost-effectiveness of guided internet- and mobile-based CBT for adolescents and young adults with chronic somatic conditions and comorbid depression and anxiety symptoms (youthCOACH): study protocol for a multicentre randomized controlled trial. Trials. 2020 Mar 12;21(1):253. doi: 10.1186/s13063-019-4041-9. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-4041-9 .10.1186/s13063-019-4041-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCusker J, Yaffe M, Faria R, Lambert S, Li M, Poirier-Bisson J, Magalhaes M, de Raad M. Phase II trial of a depression self-care intervention for adult cancer survivors. Eur J Cancer Care (Engl) 2018 Jan 06;27(1):e12763. doi: 10.1111/ecc.12763. [DOI] [PubMed] [Google Scholar]
- 47.Lundgren J, Andersson G, Dahlström Ö, Jaarsma T, Köhler AK, Johansson P. Internet-based cognitive behavior therapy for patients with heart failure and depressive symptoms: a proof of concept study. Patient Educ Couns. 2015 Aug;98(8):935–42. doi: 10.1016/j.pec.2015.04.013.S0738-3991(15)00193-7 [DOI] [PubMed] [Google Scholar]
- 48.Kearney SM, Williams K, Nikolajski C, Park MJ, Kraemer KL, Landsittel D, Kang C, Malito A, Schuster J. Stakeholder impact on the implementation of integrated care: opportunities to consider for patient-centered outcomes research. Contemp Clin Trials. 2021 Feb;101:106256. doi: 10.1016/j.cct.2020.106256.S1551-7144(20)30334-7 [DOI] [PubMed] [Google Scholar]
- 49.Baldwin PA, Sanatkar S, Clarke J, Fletcher S, Gunn J, Wilhelm K, Campbell L, Zwar N, Harris M, Lapsley H, Hadzi-Pavlovic D, Christensen H, Proudfoot J. A web-based mental health intervention to improve social and occupational functioning in adults with type 2 diabetes (the springboard trial): 12-month outcomes of a randomized controlled trial. J Med Internet Res. 2020 Dec 01;22(12):e16729. doi: 10.2196/16729. https://www.jmir.org/2020/12/e16729/ v22i12e16729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fortuna KL, Storm M, Aschbrenner KA, Bartels SJ. Integration of peer philosophy into a standardized self-management mobile health intervention. Psychiatr Q. 2018 Dec;89(4):795–800. doi: 10.1007/s11126-018-9578-3. https://europepmc.org/abstract/MED/29671155 .10.1007/s11126-018-9578-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bani Mohammad E, Ahmad M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Pall Supp Care. 2018 Sep 10;17(1):29–34. doi: 10.1017/s1478951518000639. [DOI] [PubMed] [Google Scholar]
- 52.van Bastelaar KM, Pouwer F, Cuijpers P, Riper H, Snoek FJ. Web-based depression treatment for type 1 and type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2011 Feb;34(2):320–5. doi: 10.2337/dc10-1248. https://europepmc.org/abstract/MED/21216855 .dc10-1248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ye Z, Chen J, Zhang Y, Hu X, Xuan Z, Yang S, Mao X, Rao Y. Video education reduces pain and anxiety levels in cancer patients who first use fentanyl transdermal patch: a randomized controlled trial. Drug Des Devel Ther. 2020;14:3477–83. doi: 10.2147/DDDT.S264112. doi: 10.2147/DDDT.S264112.264112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arch JJ, Fishbein JN, Ferris MC, Mitchell JL, Levin ME, Slivjak ET, Andorsky DJ, Kutner JS. Acceptability, feasibility, and efficacy potential of a multimodal acceptance and commitment therapy intervention to address psychosocial and advance care planning needs among anxious and depressed adults with metastatic cancer. J Palliat Med. 2020 Oct 01;23(10):1380–5. doi: 10.1089/jpm.2019.0398. [DOI] [PubMed] [Google Scholar]
- 55.Fortuna KL, Naslund JA, Aschbrenner KA, Lohman MC, Storm M, Batsis JA, Bartels SJ. Text message exchanges between older adults with serious mental illness and older certified peer specialists in a smartphone-supported self-management intervention. Psychiatr Rehabil J. 2019 Mar;42(1):57–63. doi: 10.1037/prj0000305. https://europepmc.org/abstract/MED/30010355 .2018-33259-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kayyali R, Savickas V, Spruit MA, Kaimakamis E, Siva R, Costello RW, Chang J, Pierscionek B, Davies N, Vaes AW, Paradiso R, Philip N, Perantoni E, D'Arcy S, Raptopoulos A, Nabhani-Gebara S. Qualitative investigation into a wearable system for chronic obstructive pulmonary disease: the stakeholders' perspective. BMJ Open. 2016 Aug 31;6(8):e011657. doi: 10.1136/bmjopen-2016-011657. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=27580831 .bmjopen-2016-011657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Read J, Sharpe L, Burton AL, Arean PA, Raue PJ, McDonald S, Titov N, Gandy M, Dear BF. A randomized controlled trial of internet-delivered cognitive behaviour therapy to prevent the development of depressive disorders in older adults with multimorbidity. J Affect Disord. 2020 Mar 01;264:464–73. doi: 10.1016/j.jad.2019.11.077.S0165-0327(19)30828-6 [DOI] [PubMed] [Google Scholar]
- 58.Druss BG, Ji X, Glick G, von Esenwein SA. Randomized trial of an electronic personal health record for patients with serious mental illnesses. Am J Psychiatry. 2014 Mar;171(3):360–8. doi: 10.1176/appi.ajp.2013.13070913.1815010 [DOI] [PubMed] [Google Scholar]
- 59.Chun HY, Carson AJ, Tsanas A, Dennis MS, Mead GE, Calabria C, Whiteley WN. Telemedicine cognitive behavioral therapy for anxiety after stroke: proof-of-concept randomized controlled trial. Stroke. 2020 Aug;51(8):2297–306. doi: 10.1161/STROKEAHA.120.029042. https://www.ahajournals.org/doi/abs/10.1161/STROKEAHA.120.029042?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fortuna KL, DiMilia PR, Lohman MC, Bruce ML, Zubritsky CD, Halaby MR, Walker RM, Brooks JM, Bartels SJ. Feasibility, acceptability, and preliminary effectiveness of a peer-delivered and technology supported self-management intervention for older adults with serious mental illness. Psychiatr Q. 2018 Jun;89(2):293–305. doi: 10.1007/s11126-017-9534-7. https://europepmc.org/abstract/MED/28948424 .10.1007/s11126-017-9534-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jindal D, Gupta P, Jha D, Ajay VS, Goenka S, Jacob P, Mehrotra K, Perel P, Nyong J, Roy A, Tandon N, Prabhakaran D, Patel V. Development of mWellcare: an mHealth intervention for integrated management of hypertension and diabetes in low-resource settings. Glob Health Action. 2018;11(1):1517930. doi: 10.1080/16549716.2018.1517930. https://europepmc.org/abstract/MED/30253691 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wilson M, Hewes C, Barbosa-Leiker C, Mason A, Wuestney KA, Shuen JA, Wilson MP. Engaging adults with chronic disease in online depressive symptom self-management. West J Nurs Res. 2018 Jun;40(6):834–53. doi: 10.1177/0193945916689068. [DOI] [PubMed] [Google Scholar]
- 63.Clarke J, Proudfoot J, Ma H. Mobile phone and web-based cognitive behavior therapy for depressive symptoms and mental health comorbidities in people living with diabetes: results of a feasibility study. JMIR Ment Health. 2016 May 31;3(2):e23. doi: 10.2196/mental.5131. https://mental.jmir.org/2016/2/e23/ v3i2e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fortuna KL, Storm M, Naslund JA, Chow P, Aschbrenner KA, Lohman MC, Bartels SJ. Certified peer specialists and older adults with serious mental illness' perspectives of the impact of a peer-delivered and technology-supported self-management intervention. J Nerv Ment Dis. 2018 Nov;206(11):875–81. doi: 10.1097/NMD.0000000000000896. https://europepmc.org/abstract/MED/30371642 .00005053-201811000-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lundgren JG, Dahlström Ö, Andersson G, Jaarsma T, Kärner Köhler A, Johansson P. The effect of guided web-based cognitive behavioral therapy on patients with depressive symptoms and heart failure: a pilot randomized controlled trial. J Med Internet Res. 2016 Aug 03;18(8):e194. doi: 10.2196/jmir.5556. https://www.jmir.org/2016/8/e194/ v18i8e194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sorocco KH, Bratkovich KL, Wingo R, Qureshi SM, Mason PJ. Integrating care coordination home telehealth and home based primary care in rural Oklahoma: a pilot study. Psychol Serv. 2013 Aug;10(3):350–2. doi: 10.1037/a0032785.2013-28609-003 [DOI] [PubMed] [Google Scholar]
- 67.Whelan ME, Velardo C, Rutter H, Tarassenko L, Farmer AJ. Mood monitoring over one year for people with chronic obstructive pulmonary disease using a mobile health system: retrospective analysis of a randomized controlled trial. JMIR Mhealth Uhealth. 2019 Nov 22;7(11):e14946. doi: 10.2196/14946. https://mhealth.jmir.org/2019/11/e14946/ v7i11e14946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Menezes P, Quayle J, Garcia Claro H, da Silva S, Brandt LR, Diez-Canseco F, Miranda JJ, Price LN, Mohr DC, Araya R. Use of a mobile phone app to treat depression comorbid with hypertension or diabetes: a pilot study in Brazil and Peru. JMIR Ment Health. 2019 Apr 26;6(4):e11698. doi: 10.2196/11698. https://mental.jmir.org/2019/4/e11698/ v6i4e11698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fortuna KL, Lohman MC, Gill LE, Bruce ML, Bartels SJ. Adapting a psychosocial intervention for smartphone delivery to middle-aged and older adults with serious mental illness. Am J Geriatr Psychiatry. 2017 Aug;25(8):819–28. doi: 10.1016/j.jagp.2016.12.007. https://europepmc.org/abstract/MED/28169129 .S1064-7481(16)30336-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sui Y, Wang T, Wang X. The impact of WeChat app-based education and rehabilitation program on anxiety, depression, quality of life, loss of follow-up and survival in non-small cell lung cancer patients who underwent surgical resection. Eur J Oncol Nurs. 2020 Apr;45:101707. doi: 10.1016/j.ejon.2019.101707.S1462-3889(19)30175-9 [DOI] [PubMed] [Google Scholar]
- 71.Koehler J, Stengel A, Hofmann T, Wegscheider K, Koehler K, Sehner S, Rose M, Deckwart O, Anker SD, Koehler F, Laufs U. Telemonitoring in patients with chronic heart failure and moderate depressed symptoms: results of the Telemedical Interventional Monitoring in Heart Failure (TIM-HF) study. Eur J Heart Fail. 2021 Jan;23(1):186–94. doi: 10.1002/ejhf.2025. doi: 10.1002/ejhf.2025. [DOI] [PubMed] [Google Scholar]
- 72.Ali MK, Chwastiak L, Poongothai S, Emmert-Fees KM, Patel SA, Anjana RM, Sagar R, Shankar R, Sridhar GR, Kosuri M, Sosale AR, Sosale B, Rao D, Tandon N, Narayan KM, Mohan V, INDEPENDENT Study Group Effect of a collaborative care model on depressive symptoms and glycated hemoglobin, blood pressure, and serum cholesterol among patients with depression and diabetes in India: the INDEPENDENT randomized clinical trial. JAMA. 2020 Aug 18;324(7):651–62. doi: 10.1001/jama.2020.11747. https://europepmc.org/abstract/MED/32809002 .2769466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sarda A, Munuswamy S, Sarda S, Subramanian V. Using passive smartphone sensing for improved risk stratification of patients with depression and diabetes: cross-sectional observational study. JMIR Mhealth Uhealth. 2019 Jan 29;7(1):e11041. doi: 10.2196/11041. https://mhealth.jmir.org/2019/1/e11041/ v7i1e11041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van Bastelaar K, Cuijpers P, Pouwer F, Riper H, Snoek FJ. Development and reach of a web-based cognitive behavioural therapy programme to reduce symptoms of depression and diabetes-specific distress. Patient Educ Couns. 2011 Jul;84(1):49–55. doi: 10.1016/j.pec.2010.06.013.S0738-3991(10)00372-1 [DOI] [PubMed] [Google Scholar]
- 75.Prabhakaran D, Jha D, Prieto-Merino D, Roy A, Singh K, Ajay VS, Jindal D, Gupta P, Kondal D, Goenka S, Jacob PD, Singh R, Kumar BG, Perel P, Tandon N, Patel V, Members of the Research Steering Committee‚Investigators‚Members of the Data SafetyMonitoring Board Effectiveness of an mHealth-based electronic decision support system for integrated management of chronic conditions in primary care: the mWellcare cluster-randomized controlled trial. Circulation. 2019 Jan 15;139(3):380–91. doi: 10.1161/CIRCULATIONAHA.118.038192. https://www.ahajournals.org/doi/abs/10.1161/CIRCULATIONAHA.118.038192?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 76.Bajracharya P, Summers L, Amatya AK, DeBlieck C. Implementation of a depression screening protocol and tools to improve screening for depression in patients with diabetes in the primary care setting. J Nurse Pract. 2016 Nov;12(10):690–6. doi: 10.1016/j.nurpra.2016.08.009. [DOI] [Google Scholar]
- 77.Hauffman A, Alfonsson S, Igelström H, Johansson B. Experiences of internet-based stepped care in individuals with cancer and concurrent symptoms of anxiety and depression: qualitative exploration conducted alongside the U-CARE adultCan randomized controlled trial. J Med Internet Res. 2020 Mar 30;22(3):e16547. doi: 10.2196/16547. https://www.jmir.org/2020/3/e16547/ v22i3e16547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McCusker J, Cole MG, Yaffe M, Strumpf E, Sewitch M, Sussman T, Ciampi A, Lavoie K, Platt RW, Belzile E. A randomized trial of a depression self-care toolkit with or without lay telephone coaching for primary care patients with chronic physical conditions. Gen Hosp Psychiatry. 2016;40:75–83. doi: 10.1016/j.genhosppsych.2016.02.004.S0163-8343(16)30015-9 [DOI] [PubMed] [Google Scholar]
- 79.Greer JA, Jacobs J, Pensak N, MacDonald JJ, Fuh C, Perez GK, Ward A, Tallen C, Muzikansky A, Traeger L, Penedo FJ, El-Jawahri A, Safren SA, Pirl WF, Temel JS. Randomized trial of a tailored cognitive-behavioral therapy mobile application for anxiety in patients with incurable cancer. Oncologist. 2019 Aug;24(8):1111–20. doi: 10.1634/theoncologist.2018-0536. https://academic.oup.com/oncolo/article-lookup/doi/10.1634/theoncologist.2018-0536 .theoncologist.2018-0536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Igelström H, Hauffman A, Alfonsson S, Sjöström J, Cajander Å, Johansson B. User experiences of an internet-based stepped-care intervention for individuals with cancer and concurrent symptoms of anxiety or depression (the U-CARE adultCan trial): qualitative study. J Med Internet Res. 2020 May 19;22(5):e16604. doi: 10.2196/16604. https://www.jmir.org/2020/5/e16604/ v22i5e16604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hauffman A, Alfonsson S, Bill-Axelson A, Bergkvist L, Forslund M, Mattsson S, von Essen L, Nygren P, Igelström H, Johansson B. Cocreated internet-based stepped care for individuals with cancer and concurrent symptoms of anxiety and depression: results from the U-CARE AdultCan randomized controlled trial. Psychooncology. 2020 Dec 22;29(12):2012–8. doi: 10.1002/pon.5489. https://europepmc.org/abstract/MED/32691455 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jin H, Wu S. Text messaging as a screening tool for depression and related conditions in underserved, predominantly minority safety net primary care patients: validity study. J Med Internet Res. 2020 Mar 26;22(3):e17282. doi: 10.2196/17282. https://www.jmir.org/2020/3/e17282/ v22i3e17282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.McCusker J, Lambert S, Cole M, Ciampi A, Strumpf E, Freeman EE, Belzile E. Activation and self-efficacy in a randomized trial of a depression self-care intervention. Health Educ Behav. 2016 Dec;43(6):716–25. doi: 10.1177/1090198116637601. https://journals.sagepub.com/doi/abs/10.1177/1090198116637601 .1090198116637601 [DOI] [PubMed] [Google Scholar]
- 84.Steel J, Geller DA, Tsung A, Marsh JW, Dew MA, Spring M, Grady J, Likumahuwa S, Dunlavy A, Youssef M, Antoni M, Butterfield LH, Schulz R, Day R, Helgeson V, Kim KH, Gamblin TC. Randomized controlled trial of a collaborative care intervention to manage cancer-related symptoms: lessons learned. Clin Trials. 2011 Jun;8(3):298–310. doi: 10.1177/1740774511402368. https://europepmc.org/abstract/MED/21730078 .8/3/298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fletcher S, Clarke J, Sanatkar S, Baldwin P, Gunn J, Zwar N, Campbell L, Wilhelm K, Harris M, Lapsley H, Hadzi-Pavlovic D, Proudfoot J. Recruiting to a randomized controlled trial of a web-based program for people with type 2 diabetes and depression: lessons learned at the intersection of e-mental health and primary care. J Med Internet Res. 2019 May 24;21(5):e12793. doi: 10.2196/12793. https://www.jmir.org/2019/5/e12793/ v21i5e12793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hauffman A, Alfonsson S, Mattsson S, Forslund M, Bill-Axelson A, Nygren P, Johansson B. The development of a nurse-led internet-based learning and self-care program for cancer patients with symptoms of anxiety and depression—a part of U-CARE. Cancer Nurs. 2017;40(5):E9–16. doi: 10.1097/ncc.0000000000000402. [DOI] [PubMed] [Google Scholar]
- 87.Huberty J, Eckert R, Larkey L, Kurka J, Rodríguez De Jesús SA, Yoo W, Mesa R. Smartphone-based meditation for myeloproliferative neoplasm patients: feasibility study to inform future trials. JMIR Form Res. 2019 Apr 29;3(2):e12662. doi: 10.2196/12662. https://formative.jmir.org/2019/2/e12662/ v3i2e12662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.van Bastelaar KM, Pouwer F, Cuijpers P, Riper H, Twisk JW, Snoek FJ. Is a severe clinical profile an effect modifier in a web-based depression treatment for adults with type 1 or type 2 diabetes? Secondary analyses from a randomized controlled trial. J Med Internet Res. 2012 Jan 05;14(1):e2. doi: 10.2196/jmir.1657. https://www.jmir.org/2012/1/e2/ v14i1e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wittink MN, Walsh P, Yilmaz S, Mendoza M, Street RL, Chapman BP, Duberstein P. Patient priorities and the doorknob phenomenon in primary care: can technology improve disclosure of patient stressors? Patient Educ Couns. 2018 Feb;101(2):214–20. doi: 10.1016/j.pec.2017.08.004. https://europepmc.org/abstract/MED/28844522 .S0738-3991(17)30478-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Brandt LR, Hidalgo L, Diez-Canseco F, Araya R, Mohr DC, Menezes PR, Miranda JJ. Addressing depression comorbid with diabetes or hypertension in resource-poor settings: a qualitative study about user perception of a nurse-supported smartphone app in Peru. JMIR Ment Health. 2019 Jun 18;6(6):e11701. doi: 10.2196/11701. https://mental.jmir.org/2019/6/e11701/ v6i6e11701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Newby J, Robins L, Wilhelm K, Smith J, Fletcher T, Gillis I, Ma T, Finch A, Campbell L, Andrews G. Web-based cognitive behavior therapy for depression in people with diabetes mellitus: a randomized controlled trial. J Med Internet Res. 2017 May 15;19(5):e157. doi: 10.2196/jmir.7274. https://www.jmir.org/2017/5/e157/ v19i5e157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Johansson P, Jaarsma T, Andersson G, Lundgren J. The impact of internet-based cognitive behavioral therapy and depressive symptoms on self-care behavior in patients with heart failure: a secondary analysis of a randomised controlled trial. Int J Nurs Stud. 2021 Apr;116:103454. doi: 10.1016/j.ijnurstu.2019.103454.S0020-7489(19)30261-5 [DOI] [PubMed] [Google Scholar]
- 93.Clarke J, Sanatkar S, Baldwin PA, Fletcher S, Gunn J, Wilhelm K, Campbell L, Zwar N, Harris M, Lapsley H, Hadzi-Pavlovic D, Christensen H, Proudfoot J. A web-based cognitive behavior therapy intervention to improve social and occupational functioning in adults with type 2 diabetes (The SpringboarD Trial): randomized controlled trial. J Med Internet Res. 2019 May 21;21(5):e12246. doi: 10.2196/12246. https://www.jmir.org/2019/5/e12246/ v21i5e12246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Puzia ME, Huberty J, Eckert R, Larkey L, Mesa R. Associations between global mental health and response to an app-based meditation intervention in myeloproliferative neoplasm patients. Integr Cancer Ther. 2020;19:1534735420927780. doi: 10.1177/1534735420927780. https://journals.sagepub.com/doi/10.1177/1534735420927780?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cohen LB, Taveira TH, Wu W, Pirraglia PA. Pharmacist-led telehealth disease management program for patients with diabetes and depression. J Telemed Telecare. 2020 Jun;26(5):294–302. doi: 10.1177/1357633X18822575. [DOI] [PubMed] [Google Scholar]
- 96.Stevenson W, Bryant J, Watson R, Sanson-Fisher R, Oldmeadow C, Henskens F, Brown C, Ramanathan S, Tiley C, Enjeti A, Guest J, Tzelepis F, Paul C, D'Este C. A multi-center randomized controlled trial to reduce unmet needs, depression, and anxiety among hematological cancer patients and their support persons. J Psychosoc Oncol. 2020 Dec 13;38(3):272–92. doi: 10.1080/07347332.2019.1692991. [DOI] [PubMed] [Google Scholar]
- 97.Huberty J, Eckert R, Larkey L, Joeman L, Mesa R. Experiences of using a consumer-based mobile meditation app to improve fatigue in myeloproliferative patients: qualitative study. JMIR Cancer. 2019 Jul 22;5(2):e14292. doi: 10.2196/14292. https://cancer.jmir.org/2019/2/e14292/ v5i2e14292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schlicker S, Weisel KK, Buntrock C, Berking M, Nobis S, Lehr D, Baumeister H, Snoek FJ, Riper H, Ebert DD. Do nonsuicidal severely depressed individuals with diabetes profit from internet-based guided self-help? Secondary analyses of a pragmatic randomized trial. J Diabetes Res. 2019;2019:2634094. doi: 10.1155/2019/2634094. doi: 10.1155/2019/2634094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nobis S, Lehr D, Ebert DD, Baumeister H, Snoek F, Riper H, Berking M. Efficacy of a web-based intervention with mobile phone support in treating depressive symptoms in adults with type 1 and type 2 diabetes: a randomized controlled trial. Diabetes Care. 2015 May;38(5):776–83. doi: 10.2337/dc14-1728.dc14-1728 [DOI] [PubMed] [Google Scholar]
- 100.How are the income group thresholds determined? World Bank Data. [2019-10-28]. https://datahelpdesk.worldbank.org/knowledgebase/articles/378833-how-are-the-income-group-thresholds-determined .
- 101.Proudfoot J, Clarke J, Gunn J, Fletcher S, Sanatkar S, Wilhelm K, Campbell L, Zwar N, Harris M, Lapsley H, Hadzi-Pavlovic D, Christensen H. A web-based public health intervention to reduce functional impairment and depressive symptoms in adults with type 2 diabetes (the Springboard Trial): randomized controlled trial protocol. JMIR Res Protoc. 2017 Aug 03;6(8):e145. doi: 10.2196/resprot.7348. https://www.researchprotocols.org/2017/8/e145/ v6i8e145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cockayne NL, Glozier N, Naismith SL, Christensen H, Neal B, Hickie IB. Internet-based treatment for older adults with depression and co-morbid cardiovascular disease: protocol for a randomised, double-blind, placebo controlled trial. BMC Psychiatry. 2011 Jan 14;11:10. doi: 10.1186/1471-244X-11-10. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-11-10 .1471-244X-11-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Jin H, Wu S. Screening depression and related conditions via text messaging versus interview assessment: protocol for a randomized study. JMIR Res Protoc. 2019 Mar 29;8(3):e12392. doi: 10.2196/12392. https://www.researchprotocols.org/2019/3/e12392/ v8i3e12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Monreal-Bartolomé A, Barceló-Soler A, Castro A, Pérez-Ara MA, Gili M, Mayoral F, Hurtado MM, Moreno EV, Botella C, García-Palacios A, Baños RM, López-Del-Hoyo Y, García-Campayo J. Efficacy of a blended low-intensity internet-delivered psychological programme in patients with multimorbidity in primary care: study protocol for a randomized controlled trial. BMC Psychiatry. 2019 Feb 11;19(1):66. doi: 10.1186/s12888-019-2037-3. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-019-2037-3 .10.1186/s12888-019-2037-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Robins L, Newby J, Wilhelm K, Smith J, Fletcher T, Ma T, Finch A, Campbell L, Andrews G. Internet-delivered cognitive behaviour therapy for depression in people with diabetes: study protocol for a randomised controlled trial. BMJ Open Diabetes Res Care. 2015;3(1):e000144. doi: 10.1136/bmjdrc-2015-000144. https://drc.bmj.com/lookup/pmidlookup?view=long&pmid=26688735 .bmjdrc-2015-000144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.van Bastelaar KM, Pouwer F, Cuijpers P, Twisk JW, Snoek FJ. Web-based cognitive behavioural therapy (W-CBT) for diabetes patients with co-morbid depression: design of a randomised controlled trial. BMC Psychiatry. 2008 Feb 19;8:9. doi: 10.1186/1471-244X-8-9. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-8-9 .1471-244X-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dindo L, Van Liew JR, Arch JJ. Acceptance and commitment therapy: a transdiagnostic behavioral intervention for mental health and medical conditions. Neurotherapeutics. 2017 Jul;14(3):546–53. doi: 10.1007/s13311-017-0521-3. https://europepmc.org/abstract/MED/28271287 .10.1007/s13311-017-0521-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Newby JM, Twomey C, Yuan Li SS, Andrews G. Transdiagnostic computerised cognitive behavioural therapy for depression and anxiety: a systematic review and meta-analysis. J Affect Disord. 2016 Jul 15;199:30–41. doi: 10.1016/j.jad.2016.03.018.S0165-0327(16)30050-7 [DOI] [PubMed] [Google Scholar]
- 109.Păsărelu CR, Andersson G, Bergman Nordgren L, Dobrean A. Internet-delivered transdiagnostic and tailored cognitive behavioral therapy for anxiety and depression: a systematic review and meta-analysis of randomized controlled trials. Cogn Behav Ther. 2017 Jan;46(1):1–28. doi: 10.1080/16506073.2016.1231219. [DOI] [PubMed] [Google Scholar]
- 110.Shapira S, Yeshua-Katz D, Cohn-Schwartz E, Aharonson-Daniel L, Sarid O, Clarfield AM. A pilot randomized controlled trial of a group intervention via Zoom to relieve loneliness and depressive symptoms among older persons during the COVID-19 outbreak. Internet Interv. 2021 Apr;24:100368. doi: 10.1016/j.invent.2021.100368. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(21)00008-7 .S2214-7829(21)00008-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Webb CA, Rosso IM, Rauch SL. Internet-based cognitive-behavioral therapy for depression: current progress and future directions. Harv Rev Psychiatry. 2017;25(3):114–22. doi: 10.1097/HRP.0000000000000139. https://europepmc.org/abstract/MED/28475503 .00023727-201705000-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Weisel KK, Lehr D, Heber E, Zarski A, Berking M, Riper H, Ebert DD. Severely burdened individuals do not need to be excluded from internet-based and mobile-based stress management: effect modifiers of treatment outcomes from three randomized controlled trials. J Med Internet Res. 2018 Jun 19;20(6):e211. doi: 10.2196/jmir.9387. https://www.jmir.org/2018/6/e211/ v20i6e211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Button KS, Wiles NJ, Lewis G, Peters TJ, Kessler D. Factors associated with differential response to online cognitive behavioural therapy. Soc Psychiatry Psychiatr Epidemiol. 2012 May 4;47(5):827–33. doi: 10.1007/s00127-011-0389-1. [DOI] [PubMed] [Google Scholar]
- 114.Spek V, Nyklícek I, Cuijpers P, Pop V. Predictors of outcome of group and internet-based cognitive behavior therapy. J Affect Disord. 2008 Jan;105(1-3):137–45. doi: 10.1016/j.jad.2007.05.001.S0165-0327(07)00172-3 [DOI] [PubMed] [Google Scholar]
- 115.Warmerdam L, Van Straten A, Twisk J, Cuijpers P. Predicting outcome of internet-based treatment for depressive symptoms. Psychother Res. 2013;23(5):559–67. doi: 10.1080/10503307.2013.807377. [DOI] [PubMed] [Google Scholar]
- 116.Johansson B, Hauffman A, Bill-Axelsson A, Alfonsson S, von Essen L, Nygren H, Igelström H. Internet-based stepped care for individuals with cancer and concurrent anxiety or depression symptoms: results from a randomized controlled trial. Ann Oncol. 2019 Oct;30:v667–8. doi: 10.1093/annonc/mdz262.002. [DOI] [Google Scholar]
- 117.Cassin SE, Sockalingam S, Du C, Wnuk S, Hawa R, Parikh SV. A pilot randomized controlled trial of telephone-based cognitive behavioural therapy for preoperative bariatric surgery patients. Behav Res Ther. 2016 May;80:17–22. doi: 10.1016/j.brat.2016.03.001. https://europepmc.org/abstract/MED/26990279 .S0005-7967(16)30037-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sockalingam S, Cassin SE, Wnuk S, Du C, Jackson T, Hawa R, Parikh SV. A pilot study on telephone cognitive behavioral therapy for patients six-months post-bariatric surgery. Obes Surg. 2017 Mar;27(3):670–5. doi: 10.1007/s11695-016-2322-x. https://europepmc.org/abstract/MED/27491293 .10.1007/s11695-016-2322-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Costa-Dookhan KA, Leung SE, Cassin SE, Sockalingam S. Psychosocial predictors of response to telephone-based cognitive behavioural therapy in bariatric surgery patients. Can J Diabetes. 2020 Apr;44(3):236–40. doi: 10.1016/j.jcjd.2019.06.008.S1499-2671(19)30006-1 [DOI] [PubMed] [Google Scholar]
- 120.Ramirez M, Wu S, Jin H, Ell K, Gross-Schulman S, Myerchin Sklaroff L, Guterman J. Automated remote monitoring of depression: acceptance among low-income patients in diabetes disease management. JMIR Ment Health. 2016 Jan 25;3(1):e6. doi: 10.2196/mental.4823. https://mental.jmir.org/2016/1/e6/ v3i1e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wu S, Ell K, Gross-Schulman SG, Sklaroff LM, Katon WJ, Nezu AM, Lee P, Vidyanti I, Chou C, Guterman JJ. Technology-facilitated depression care management among predominantly Latino diabetes patients within a public safety net care system: comparative effectiveness trial design. Contemp Clin Trials. 2014 Mar;37(2):342–54. doi: 10.1016/j.cct.2013.11.002.S1551-7144(13)00173-0 [DOI] [PubMed] [Google Scholar]
- 122.Grundberg A, Ebbeskog B, Gustafsson SA, Religa D. Mental health-promoting dialogues from the perspective of community-dwelling seniors with multimorbidity. J Multidiscip Healthc. 2014;7:189–99. doi: 10.2147/JMDH.S59307. doi: 10.2147/JMDH.S59307.jmdh-7-189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bisseling E, Cillessen L, Spinhoven P, Schellekens M, Compen F, van der Lee M, Speckens A. Development of the therapeutic alliance and its association with internet-based mindfulness-based cognitive therapy for distressed cancer patients: secondary analysis of a multicenter randomized controlled trial. J Med Internet Res. 2019 Oct 18;21(10):e14065. doi: 10.2196/14065. https://www.jmir.org/2019/10/e14065/ v21i10e14065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lally RM, Kupzyk K, Gallo S, Berry D. Use of an unguided, web-based distress self-management program after breast cancer diagnosis: sub-analysis of CaringGuidance pilot study. J Med Internet Res. 2020 Jul 06;22(7):e19734. doi: 10.2196/19734. https://www.jmir.org/2020/7/e19734/ v22i7e19734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhang X, Tan SS, Fierloos I, Zanutto O, Alhambra-Borrás T, Vasiljev V, Bennett S, Rentoumis T, Buranello A, Macchione S, Rouwet E, van Grieken A, Raat H. Evaluation design of the social engagement framework for addressing the chronic-disease-challenge (SEFAC): a mindfulness-based intervention to promote the self-management of chronic conditions and a healthy lifestyle. BMC Public Health. 2019 May 30;19(1):664. doi: 10.1186/s12889-019-6979-7. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-6979-7 .10.1186/s12889-019-6979-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Murray E, Kerr C, Stevenson F, Gore C, Nazareth I. Internet interventions can meet the emotional needs of patients and carers managing long-term conditions. J Telemed Telecare. 2016 Dec 02;13(1_suppl):42–4. doi: 10.1258/135763307781644960. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist.
Sample search strategy (MEDLINE).
Summary of digital health interventions.
Summary of digital health intervention components.
Summary of digital health intervention guidance.


