Abstract
The spatial structure of diabetes-related mortality in US counties is evident from previous studies. However, it is not clear if spatial variation in diabetes-related mortality is associated with spatial variation in socioecological factors. We analyze the spatial spillover effect of changes in socioeconomic gradients (education, employment, household income), retail food environments, and access to health care, on diabetes-related mortality rates across the United States. Seven-year aggregates of multiple cause mortality data from the CDC WONDER compressed mortality database were merged with several sources of county-level data to examine mortality clusters, factors associated with the clusters, and spatial spillover effects in 3109 continuous US counties. The results suggest that high diabetes-related mortality cluster counties are located throughout the Southern Plains, Southeastern, and Appalachian regions. Lower socioeconomic status, a high density of fast food restaurants, a lack of access to grocery stores, a high proportion of Blacks, and low physical activity characterize high diabetes-related mortality rates clusters. The impacts from improvements in socioeconomic gradients and the retail food environment in neighboring counties spill over, and reduce the diabetes-related mortality rate in a particular county. This result implies that improvements in socioeconomic status and access to healthy food would significantly reduce diabetes-related mortality rates in contiguous US counties.
Keywords: Diabetes, Mortality, Socioeconomic gradients, Built environment, Social capital
1. Introduction
Adults with diagnosed diabetes have a greater than two-fold increased risk of mortality compared to the general population (Egede, Nietert, & Zheng, 2005). According to the International Diabetes Federation (2015), diabetes was responsible for more than 5 million premature deaths globally in 2014, which accounted for 8.4% of all-cause mortality among adults aged 20–70 years, and represented an 11% increase since 2011. The prevalence of diabetes in the United States increased from 4.5% to 9.3% from 1995 to 2012, and diabetes is the 7th leading cause of death (Murphy, Xu, & Kochanek, 2013).
Though the diabetes-related mortality rate (DRMR) in the United States showed signs of decline due to medical advances (Murphy et al., 2013; Saaddine et al., 2006), this benefit has not trickled down to all racial groups (Murphy et al., 2013) and geographical areas (Murray et al., 2006). The reasons behind regional disparities in DRMR are not well understood. Most studies on the determinants of DRMR disparity point to individual behaviors and socioeconomic characteristics (Dray-Spira, Gary-Webb, & Brancati, 2010; Saydah & Lochner, 2010; Saydah, Imperatore, & Beckles, 2013); however, DRMR is also driven by socio-ecological factors that are beyond individual control (Brown et al., 2004; Weng, Coppini, & Sönksen, 2000). Socio-ecological factors previously linked to DRMR include the availability of and access to healthy food as measured by the density of supermarkets or fast food restaurants (Alter & Eny, 2005), physical environments, including residential areas, workplaces, and highways, the accessibility of natural amenities, leisure, and pollution (Deshpande, Baker, Lovegreen, & Brownson, 2005; Gordon-Larsen, Nelson, Page, & Popkin, 2006; Wilcox, Castro, King, Housemann, & Brownson, 2000). DRMR is also associated with socioeconomic factors such as median income, income inequality, minimum wages, the availability of jobs (Dray-Spira et al., 2010; Saydah & Lochner, 2010), the proportion of minority populations in the county (McLaughlin & Stokes, 2002), and access to health services (Sommers, Baicker, & Epstein, 2012). For examples, Massing et al. (2004) found that county cardiovascular disease specific mortality rates are associated with income inequality, and Shi et al. (2005) showed that counties with high income inequality experienced 11–13% higher rates of heart disease and cancer mortality compared to their counterparts with high primary care resources and low inequality, respectively. Thus, in addition to individual health behaviors and socioeconomic status, socioecological factors surrounding individuals are important determinants of DRMR.
Further, previous studies showed that US DRMR displays a spatial structure (i.e., spatial variation, pattern, and dependence) (Voeks et al., 2008). This spatial structure in DRMR may manifest in the form of spatial dependence due to resources and health services ties between geographical areas, and spatial interactions between ecological determinants because of social, cultural, economic and political interactions between populations in neighboring geographic areas.
However, this spatial structure has not received much scholarly attention. Understanding the dynamic interactions between a county’s DRMR and socio-ecological factors within the same county and neighboring counties is potentially important in designing policy interventions and resource allocation for DRMR reduction efforts. That is, it will be valuable to understand how DRMR in one county affects the DRMR in neighboring counties, and how socioecological factors in one county affect the DRMR in neighboring counties.
The current study utilizes county-level age and sex standardized DRMR (ICD-9 code 250–250.9) and county-level ecological determinants (socioeconomic, demographic, health service and built environment), along with spatial statistics and spatial econometric models to disentangle: 1) the presence of spatial dependence in DRMR, 2) the ecological factors that contribute to the spatial variation in DRMR, and 3) spillover effects of changes in the ecological determinants of DRMR. This study hypothesizes that DRMR at the county-level is spatially interdependent and there are spillover effects from changes in ecological determinants.
County is the spatial unit of analysis for this study. It is the smallest spatial unit for which reliable data on cause specific mortality is publically available in the US. Data on causes of DRMR at smaller spatial units, for example census tracts, is suppressed due to concerns about the identification of individuals (confidentiality concerns) (O’Carroll, Yasnoff, Ward, & Ripp, 2002). Moreover, counties are sociopolitical and administrative geographic units that provide context within which many social, economic and public health policies are formulated and implemented (Singh, 2003). Most human service and public health administration is conducted at the county-level.
2. Conceptual framework
After the onset of diabetes, self-management is essential to prevent complications and mortality. However, self-management requires access to a variety of resources, including health care services, nutrition and physical activity related resources, as well as support for the initiation and maintenance of healthy behaviors (Evert et al., 2014). In the context of socio-ecological theory, a range of factors, which may include immediate environments, as well as social, organizational, governmental policy, and economic factors (Glasgow, 1995; McLeroy, Bibeau, & Steckler, 1988; Sallis & Owen, 2002) influence individual health behaviors. The degree of influence of these factors on the individuals’ health behavior, and access to resources, is mediated by the individuals’ geographical locations (e.g., residence and work place), ethnicity/race, and socioeconomic position (Cutler, Lleras-Muney, & Vogl, 2008). See supplemental material 1 for detailed literature review on independent variables association with DRMR and supplemental material 2 for conceptual framework diagram.
3. Methods
3.1. Variables and data sources
3.1.1. Dependent variable
The county-level mortality rate in the contiguous US is the dependent variable for this study. Multiple cause mortality data was extracted from the CDC WONDER compressed mortality database (CDC WONDER, 2013). DRMR was standardized based on the US Census 2000 age–sex population structure. The DRMR is defined as multiple causes of death wherein diabetes is either the direct cause of death or contributed to the death. The mortality rate was measured as the total number of deaths per 100,000 individuals in a county. The DRMR was totaled for years 2003–2010. Total mortality rates from eight years were used to reduce the number of counties with missing mortality data. Even using 7 years of aggregated data, the mortality rates are missing for 417 counties (187 are suppressed because they have less than 10 deaths, and 230 were flagged as unreliable because they have less than 20 deaths), which is about 13% of the total sample. For the 230 counties where mortality rate is flagged as unreliable, the number of deaths were used as reported but the crude rate was imputed with a multiple imputation technique using STATA 12 software based on the reported number of deaths and other county characteristics (proportion with college education, proportion-unemployed, proportion-minority and urbanization index of the county). For the suppressed 187 counties, the number of deaths were imputed using multiple imputation-interval regression technique, which limits the outcome to a censored range (0–10), and crude mortality rates were calculated. Finally, crude mortality rates were age-standardized using the direct age-standardization method and Census 2000 population estimates. The death rate was log-transformed to limit the influence of outliers.
3.1.2. Independent variables
Healthcare service
Healthcare service variables were extracted from the Health Resources and Services Administration (HRSA) Area Health Resource Files (AHRF, 2012–13), a database maintained by the US Department of Health and Human Services. Several variables were created to describe the healthcare infrastructure: the proportion of the population aged 18–65 years without health insurance, the total number of active medical doctors, the total number of non-federal primary care physicians, the total number of hospital beds and the total number of hospitals. The average of eight years (2003–2010) data was calculated for all four variables to smooth out variation over years. The values for the total number of active medical doctors and the total number of hospitals are expressed as per 10,000 in population based on inter-census population estimates.
Ethnic Segregation
Ethnic Segregation was represented by the Index of Spatial Proximity (ISP), which measures the extent to which subgroup populations (Whites, Blacks, and Hispanics) are clustered together in adjacent tracts, suggesting the presence of a cultural enclave (Massey, 2001). The data is extracted from the 2000 Research Triangle Institute (RTI) international database. The value of the variable ranged from 0 to 2. An ISP index of 1 indicates that there is no differential clustering between minority and majority populations, a value greater than 1 indicates that the majority and minority members live spatially closer to their own group, and values of less than 1 indicate that members of each group live closer to each other than to members of their own group (Massey & Denton, 1988).
Ethnic Composition:
Two variables representing ethnic composition are included in the analysis: the proportion of non-Hispanic Blacks (African Americans), and the proportion of Hispanics were included in the analysis as independent variables to represent the composition of the two minority groups in each county. The proportion of the non-Hispanic White population was excluded to avoid multicollinearity. These variables were extracted from American Community Survey (ACS) 5-year (2006–2010) estimates (US Census Bureau, 2010).
Socioeconomic factors:
Socioeconomic status is a multidimensional gradient, thus, it was measured as a composite score of several variables (Carpiano, Lloyd, & Hertzman, 2009). The data were extracted from AHRF (2012–13) files, and average values for years 2003–2010 were pooled for the unemployment rate, the percentage of the population under the official poverty rate, and household median income. For the percentage of population age 25-years-and-older with at least a bachelor’s degree, data was extracted from 5-year ACS data. Factor analysis was used to derive a socioeconomic factor score from the four variables.
Income inequality:
Income inequality was measured with the Gini index, which varies between zero and one. A value of one indicates perfect inequality where only one house-hold has any income. A value of zero indicates perfect equality, where all households have equal income. Data was extracted from the 5-year ACS to create the index.
Retail Food environment:
The retail food environment is measured by the density of grocery stores and supermarkets and the density of full service restaurants and of limited service restaurants (i.e., fast food restaurants). The number of grocery stores and supermarkets, number of full service restaurants, and number of limited service restaurants for year 2003–2010 were extracted from county business pattern data. The number of each type of business establishment in each county was divided by inter-census population estimates for respective years to obtain a density ratio, and the data were averaged over eight years. Finally, a modified version of the Retail Food Environment Index (RFEI) of UCLA Center for Health Policy Research (California Center for Public Advocacy, 2008) was constructed as follows:
Food accessibility:
This variable is represented by the percentage of households that have no vehicle and reside more than 1 mile (10 miles for rural residents) from the nearest grocery store or supermarket. The accessibility variable is extracted from Economic Research Service (ERS) food environment atlas data (2012). This variable is available only for 2010. Though patterns of infrastructure, such as grocery stores, may not change much over eight years, cautious interpretation is warranted when one year of data is regressed against eight year aggregate mortality data.
Social capital Index (SCI):
The social capital index was obtained from Rupasingha and Goetz (2008) which is based on the population weighted number of religious organizations, civic and social associations, business associations, political organizations, professional organizations, labor organizations, bowling centers, physical fitness facilities, public golf courses, sports clubs, managers, and promoters in counties for the years 2005 and 2009. This study utilizes the average of the two year index to overlap with the aggregated mortality rate for the years 2003–2010.
Percentage of Adults meeting Physical Activity guidelines:
The proportion of the sample population meeting physical activity guidelines is constructed by ERS based on the 2010 Behavioral Risk Factor Surveillance System (BRFSS) data. This variable is extracted from Economic Research Service food environment atlas database (ERS, 2012).
Rural-Urban continuum:
The extent of urbanization was measured as the percentage of the population living in metropolitan and micro-metropolitan areas. This variable was calculated based on US census data from 2000 to 2010. In addition, a rural-urban continuum code, developed in 2003 by US Department of Agriculture, was extracted from area resource file. The code ranges from one to nine, with one being the most metropolitan and nine the most rural.
3.2. Analytic methods
The overall spatial autocorrelation of diabetes-related mortality rate (DRMR) among contiguous US counties was analyzed with the global Moran’s-I statistic (Moran, 1950). This was computed using the raw standardized six-order queen spatial weight matrix. Global bivariate Moran’s-I is employed to identify socioeconomic, demographic, and environmental variables that are associated with a county’s diabetes-related mortality. The local Moran’s I was also used to identify clusters (Anselin, 1995). Note that the spatial clusters labeled in the local indicator of spatial association (LISA) cluster map are limited to the core of the clusters; it does not extend to the neighboring counties with similar value. Counties with such characteristics are color labeled on the cluster map but the neighboring counties with similar character are not color labeled as statistically significant clusters. Multinomial logistic model was employed to evaluate the characteristics of the clusters that were identified using Local Moran’s I.
We used Spatial Durbin model (SDM) (Elhorst, 2010) to estimate the direct and spill over effect of the change in the county characteristics on the DRMR. As detailed in Online Supplemental methods, the estimated SDM parameters need to be decomposed into direct and indirect effect (spatial spillover effect), which provide substantial interpretations (LeSage & Pace, 2009). The direct impact is the average impact of change in an explanatory variable in the same county; which also accounts for the feedback effect from all other counties in the sample. The indirect effect is the measure of spillover effect, which is the average change in a specific county’s DRMR due to change in explanatory variables in neighboring counties (LeSage & Pace, 2009, 2014, pp. 1535–1552; Pietrzak, 2013). Neighboring counties in this case are determined by first order queen contiguity spatial matrix. The total impact is interpreted as the average total impact of change in explanatory variables in all counties on the DRMR in a typical county (LeSage & Pace, 2014, pp. 1535–1552; LeSage & Pace, 2009; Pietrzak, 2013).
4. Results
4.1. Descriptive statistics
The results of the descriptive statistical analysis are summarized in Table 1. The diabetes-related mortality rate ranges from 5.84 to 229 per 100,000 in population, with a mean of 60.62 based on 3109 counties. The indicator for county segregation, SPI, ranges from zero to 1.68 with a mean of 1.06. The mean indicates that the average segregation level is close to neutral, although with substantial variance. The composition of minority ethnic groups of US counties also varies widely, with the Hispanic population ranging from zero to 99% of the total county population, with an average of about 8%, and the Black population ranging from zero to 87%, with the average being about 9%. Counties with a high proportion of Hispanic residents are in the Southern and Southwestern states bordering Mexico, while counties with a high proportion of Black residents tend to be located in southern and southeastern states.
Table 1.
Descriptive statistics summarizing diabetes-related mortality rate and explanatory variables (N = 3109 contiguous US counties, aggregated data span from 2003 to 2010).
| Variables | Quantiles (25%, 75%) | Mean (Std. Err.) [95% Conf. Interval] | SD | Min | Max | VIF |
|---|---|---|---|---|---|---|
| DRMR per 100,000 population | (9.80, 227.0) | 60.62 (0.57)[60.01, 62.25] | 31.86 | 5.84 | 229 | NA |
| Spatial Proximity Index (SPI) | (0.97, 1.62) | 1.06(0.00)[1.05,1.06] | 0.09 | 0.00 | 1.68 | 1.27 |
| Proportion of Hispanic Population | (0.00, 0.93) | 0.08(0.00)[0.07,0.08] | 0.13 | 0.00 | 0.99 | 2.03 |
| Proportion of Black Population | (0.00, 0.81) | 0.09(0.00)[0.08,0.09] | 0.14 | 0.00 | 0.87 | 1.59 |
| Socioeconomic index | (−2.80, 4.19) | 0.00(0.02)[−0.03,0.03] | 0.94 | −2.90 | 4.62 | 2.21 |
| GiniI coefficient (Income Disparity) | (0.31, 0.59) | 0.43(0.00)[0.43,0.43] | 0.04 | 0.21 | 0.65 | 1.67 |
| No. of Hospital beds per 1000 population | (0.00, 48.19) | 3.56 (0.09)[3.38,3.73] | 4.96 | 0.00 | 68.64 | 1.37 |
| No. of Active MD per 10,000 population | (0.00, 15.24) | 1.25(0.03)[1.20,1.31] | 1.49 | 0.00 | 26.94 | 1.70 |
| Proportion of uninsured Adults | (0.08, 0.46) | 0.64(0.00)[0.64,0.64] | 0.04 | 0.00 | 0.73 | 2.19 |
| Social Capital Index (SCI) | (−3.13, 7.54) | 0.00(0.02) [−0.05,0.05] | 1.34 | −3.86 | 15.97 | 1.87 |
| Proportion of Adults meets PA guideline | (0.52, 0.73) | 0.21(0.00)[0.21,0.21] | 0.06 | 0.07 | 0.51 | 1.25 |
| Retail food Environment Index (RFEI) | (0.00, 1.89) | 0.63(0.01)[0.62,0.64] | 0.30 | 0.00 | 2.29 | 1.59 |
| Percent Low Access to Grocery Stores | (0.00, 15.22) | 3.03(0.04)[2.95,3.11] | 2.18 | 0.00 | 29.51 | 1.85 |
| Rural-urban Continuum | (0.00, 1.00) | 0.40(0.01)[0.39,0.41] | 0.31 | 0.00 | 1.00 | 2.84 |
DRMR = Diabetes related mortality rate; MD = medical doctors; VIF = Variance Inflation Factor; PA = Physical Activity.
The socioeconomic index varied widely between counties (range −2.90 to 4.62, mean zero). The average income disparity also varied widely, counties with a lower socioeconomic index also exhibit higher income disparity. The Gini index ranges from 0.21 to 0.65, with higher income disparity and a lower socioeconomic index clustered in southern regions (southwest and southeast regions) where the proportions of Hispanic and Black populations are higher.
In terms of medical resources, the average number of hospitals beds per 1000 county residents is 0.58. The density of hospitals ranges from none to 8.86 per 1000 residents, with the highest density in the north mountain area, north central states, and some south-west states, and the lowest density in the mid-west, south-Atlantic and Mid-Atlantic States. Similarly, the average number of active medical doctors per 10,000 county residents is 1.25, with wide variation (range zero to 26.94). The highest concentrations are in the New England region and the lowest is in the Midwest and south-west parts of the US. The average proportion of uninsured residents in a county is approximately 64% (range zero to 73%). Counties with the highest uninsured proportion of residents are clustered in the south-west and south-Atlantic regions, while the lowest is clustered around the northeast, mid-west and New England states.
The Social Capital Index (SCI) ranged from −3.86 to 15.97 (with mean zero). The highest SCI is mostly concentrated in north central states, the northern part of mountain states, and the New England states. The proportion of adult residents who meet physical activity guidelines ranges from about 7% to about 51%; those counties with a high proportion meeting the guidelines are clustered around the mountain states, north Pacific states, and the New England states.
Physical food access and availability was represented by two variables. The Retail Food Environment Index (RFEI) measures physical healthy food availability, and ranges from none to 2.29 (with mean of 0.63), with high values representing unhealthy food environment. The highest values are found in the south and mid-west states. The physical access dimension is measured by the percent of residents who reside 1 mile (10 for rural residents) from supermarkets and have no autonomous access to a vehicle. It ranged from zero to 29.5%; the highest values are clustered in the southern contiguous US states (similar to RFEI).
4.2. Exploratory spatial data analysis results
4.2.1. Global Moran’s-I
The result from global Moran’s-I (I = 0.129, SD = 0.004, P-value = 0.001) showed small but positive and statistically significant spatial dependence among county’s DRMR. Thus, it is concluded that county diabetes-related mortality rates are spatially associated.
4.2.2. Univariate local indicator for spatial association (LISA)
The cluster analysis was performed in GeoDa and the map was plotted in ESRI’s ArcMap software programs. The results are presented as a cluster map in Fig. 1. Accordingly, the map is classified into five categories (four-quadrant significant correlation categories and one insignificant category). Thirteen percent of the counties were hot spot (High-High) clusters, with high mortality rate counties associated with high mortality rate counties. Ten percent of the counties were identified as cold spot (Low-Low) clusters, with low mortality rate counties associated with low mortality rate counties. Two percent and three percent of counties were identified as Low-High and High-Low clusters respectively. The remaining 72% (2235 counties) of the counties mortality rate did not show any statistically significant cluster. DRMR exhibited High–High clusters throughout the Southern Plains, Southeastern, and Appalachian regions of the US. The low–low clusters were observed in the western mountain regions of the US, in some parts of the Mid-west, Florida, and New-England.
Fig. 1.
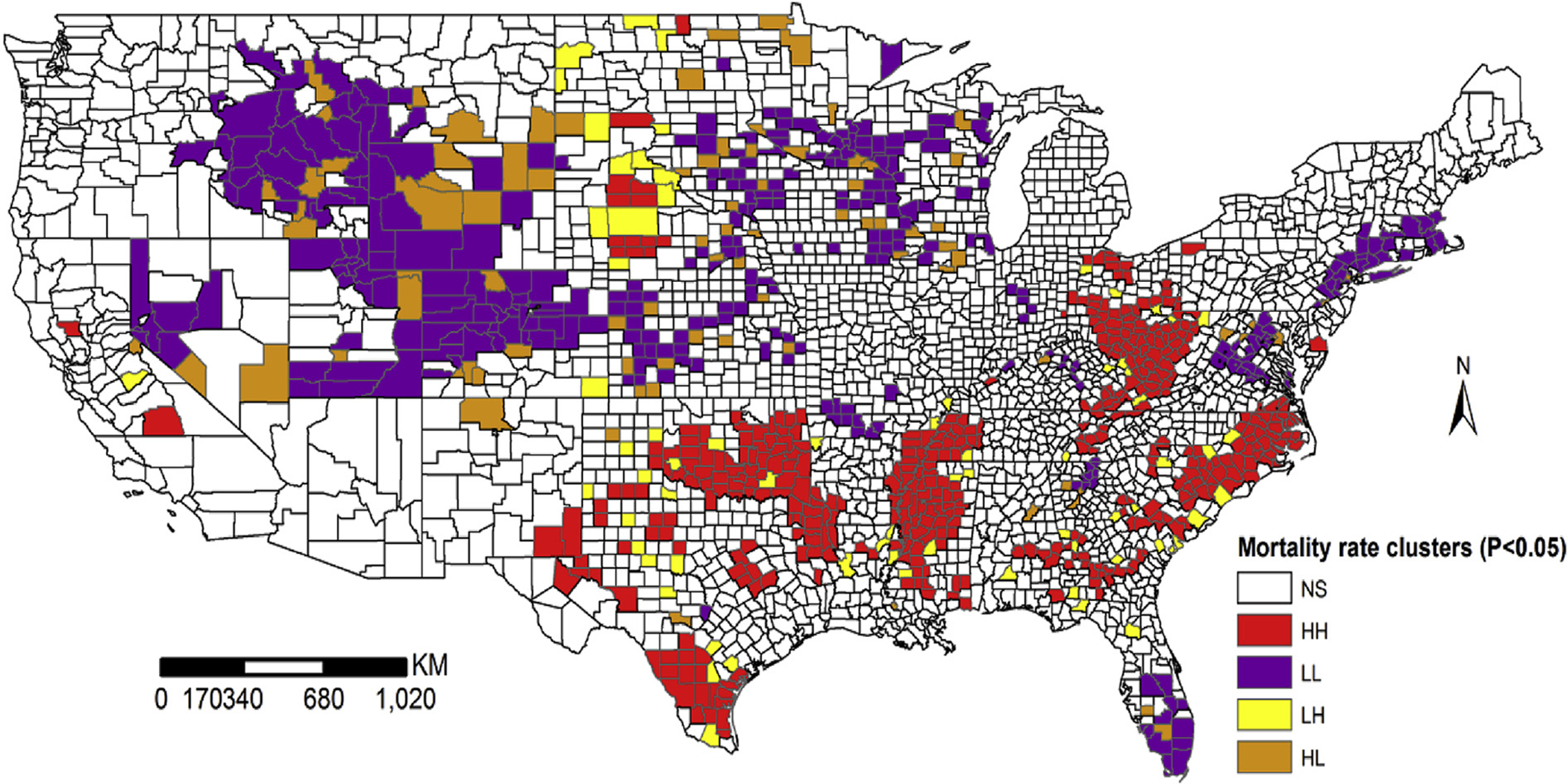
Spatial cluster of diabetes-related mortality rate (DRMR) in contiguous US counties. NS = non-significant, HH = high-high clusters, LL = low-low clusters, LH = low-high clusters and HL = high-low clusters.
4.2.3. Global bivariate Moran’s-I
The global bivariate Moran’s-I statistics (and its significance), for association between DRMR and the neighboring counties’ explanatory variables, are provided in Table 2. The statistics show that there is spatial correlation between DRMR in one county and values of explanatory variables in neighboring counties. The level of residential segregation, income disparity, high proportions of Black and Hispanic residents, a fast food dominated food environment, low access to grocery stores, high proportions of uninsured, and high income disparity positively correlate with the DRMR in neighboring counties. County DRMR is negatively associated with neighboring counties’ socioeconomic index, proportion of uninsured residents, proportion of adults who meet physical activity guidelines, density of hospital beds, density of active medical doctors, increased social capital index, and metropolitan status.
Table 2.
Global bivariate Moran’s-I: global association between DRMR and neighboring county socioecological factors.
| Dependent variable | Lagged independent variables | Bivariate Moran’s I | Pseudo p-value |
|---|---|---|---|
| Log of DRMR per 100, 000 | Log of DRMR per 100, 000 population | 0.373 | <0.05 |
| Log of DRMR per 100, 000 | Spatial Proximity Index (SPI) | 0.036 | <0.05 |
| Log of DRMR per 100, 000 | Proportion of Hispanic Population | 0.021 | <0.05 |
| Log of DRMR per 100, 000 | Proportion of Black Population | 0.219 | <0.05 |
| Log of DRMR per 100, 000 | Socioeconomic index | −0.305 | <0.05 |
| Log of DRMR per 100, 000 | Gini coefficient (Income Disparity) | 0.161 | <0.05 |
| Log of DRMR per 100, 000 | No. of Hospital beds per 1000 population | −0.029 | <0.05 |
| Log of DRMR per 100, 000 | No. of Active MD per 10,000 population | −0.079 | <0.05 |
| Log of DRMR per 100, 000 | Proportion of uninsured Adults | 0.147 | <0.05 |
| Log of DRMR per 100, 000 | Social Capital Index (SCI) | −0.159 | <0.05 |
| Log of DRMR per 100, 000 | Proportion of Adults meets PA guideline | −0.214 | <0.05 |
| Log of DRMR per 100, 000 | Retail food Environment Index (RFEI) | 0.122 | <0.05 |
| Log of DRMR per 100, 000 | Percent Low Access to Grocery Stores | 0.224 | <0.05 |
| Log of DRMR per 100, 000 | Rural-Urban Continuum Index | −0.059 | <0.05 |
4.2.4. Bivariate local indicator of spatial association (LISA)
The results from the bivariate LISA are shown using the maps in Fig. 2a and b. The High-High and Low-Low locations (positive local spatial correlation) represent spatial clusters, while the high-low and low-high locations (negative local spatial correlation) represent spatial outliers. Significance was calculated at the 5% level based on 999 permutations.
Fig. 2.
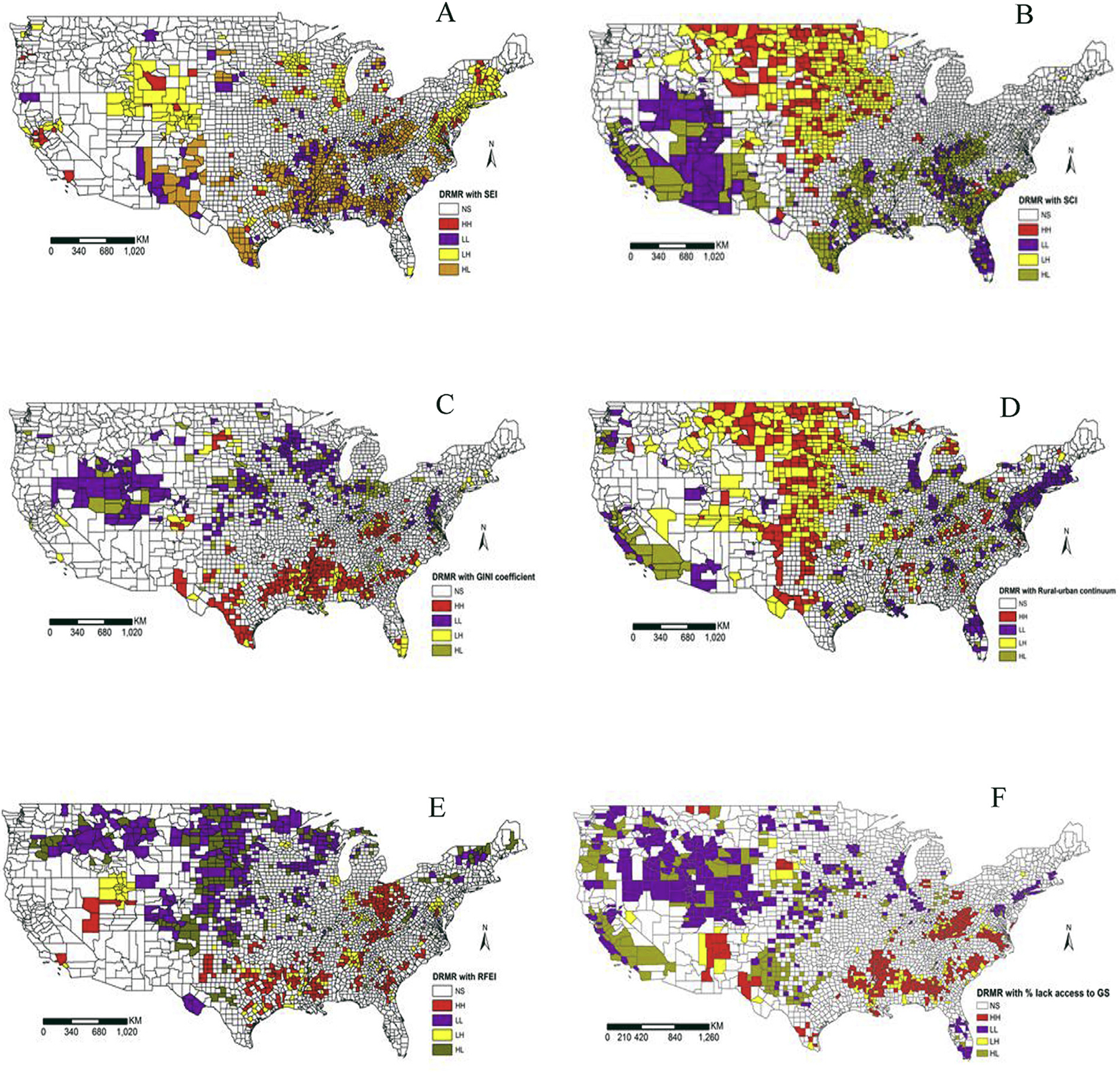
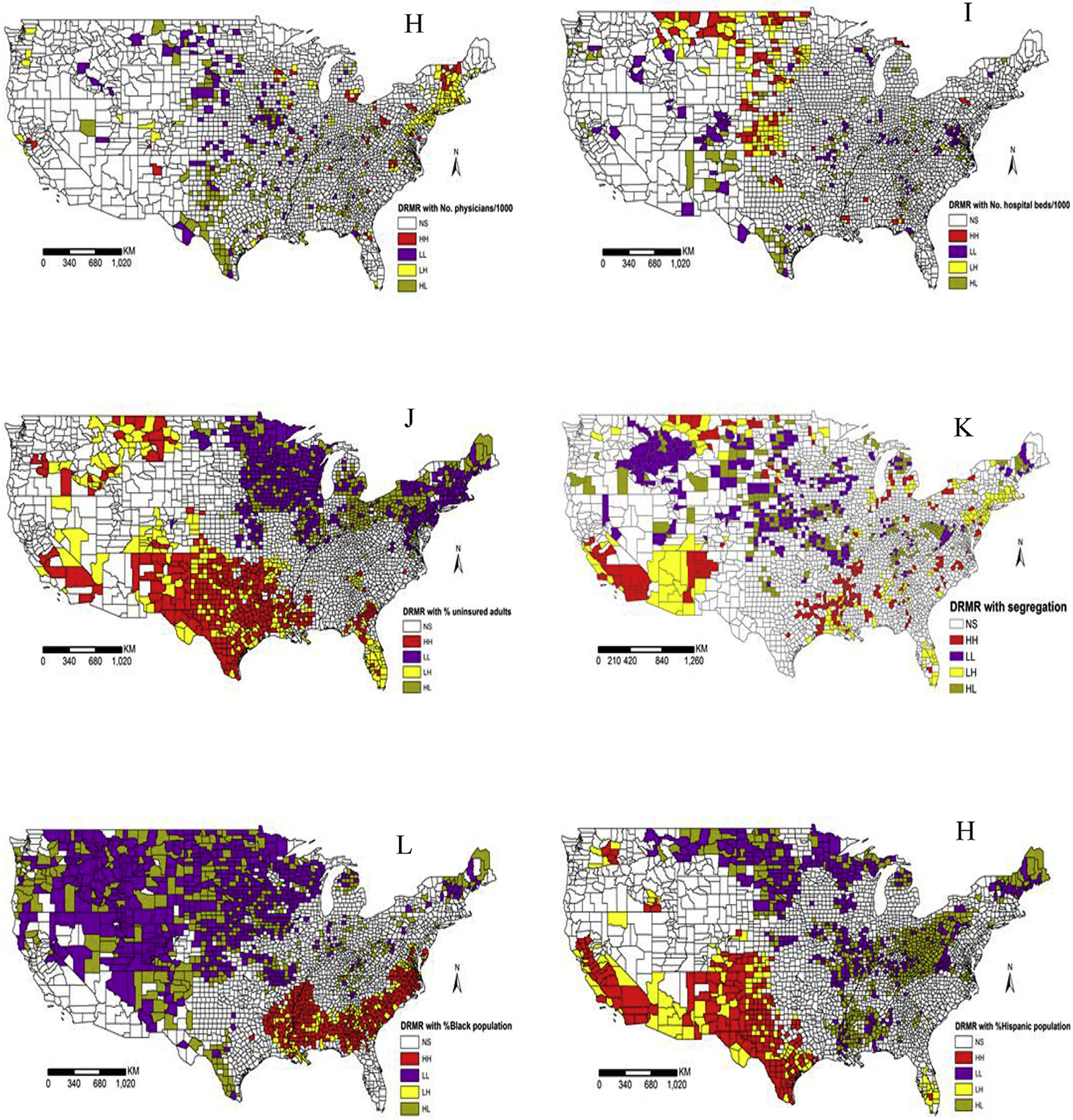
(2a). Bivariate LISA cluster map for DRMR and neighboring county (A) Socioeconomic index (SEI), (B) Social capital index (SCI), (C) Income disparity (Gini coefficient), (D) Proportion of urban resident, (E) Retail food environment index (RFEI), and (F) Proportion of households who lack access to grocery stores. NS = non-significant, HH = high-high clusters, LL = low-low clusters, LH = low-high clusters and HL = high-low clusters. (2b). Bivariate LISA cluster map for DRMR and neighboring county (H) medical doctor’s density, (I) hospital beds density, (J) proportion of uninsured residents, (K) spatial proximity index (SPI) for segregation, (L) proportion of Black population, and (M) proportion of Hispanic population. NS = non-significant, HH = high-high clusters, LL = low-low clusters, LH = low-high clusters and HL = high-low clusters.
Depictions in Fig. 2a and b reveal that the Southern Plains, Southeastern, and Appalachian regions, where DRMR is high, also have low socioeconomic status, low social capital, high income disparity, high proportions of Black population (except the Appalachian areas and southwest Texas counties), high proportion of population who lack independent access to grocery stores, and fast food dominated retail food environments. These counties are located in Ohio, West Virginia, Virginia (the southwest part), North Carolina, South Carolina, Kentucky, Tennessee, Mississippi, Oklahoma, and Texas (northeast, southern, and western parts). High DRMR cluster counties in south and west Texas and California have additional distinct characteristics, including a high proportion of Hispanic residents, a high proportion of uninsured adults, and a low density of hospital beds and physicians. Some DRMR cluster counties (for example, some of northern Ohio counties) have high DRMR as well as high socioeconomic and low-income disparity. The high DRMR in the Southern Plains region (Alabama, and Mississippi) coincided with higher proportions of the Black population, while the high DRMR in southern and western Texas counties coincided with high proportions of the Hispanic population. High levels of residential segregations in some parts of North Carolina, South Carolina, Oklahoma, Mississippi, Arkansas, Alabama, Texas, Ohio, and Tulare county (California) overlap with high DRMR. On the contrary, low DRMR counties are described as having high social capital and high socioeconomic indicators (except Montana), a low proportion of minority population, and better retail food environments in neighboring counties. These counties are located in the western parts of the Midwest and Mountain regions.
4.2.5. Multivariate association of DRMR clusters and explanatory variables
Bivariate LISA analysis indicated that spatial dependence between DRMR and explanatory variables exhibits heterogeneity. Results from multinomial logistic regressions, shown in Table 3, help to identify the socioeconomic, demographic, retail food access, and health service factors that are driving the observed high–high DRMR county clusters. The type of clusters that were identified using Moran’s I a priori are High-High, Low-Low, High-Low, Low-High and insignificant (non-clustered). The base comparison class for the multinomial logistic regression was the insignificant (non-clustered) group. The results reveal that high-high DRMR cluster counties are characterized by: a low socioeconomic index (OR = 0.48; 95% CI = 0.38,0.60), fast food dominated retail food environments (OR = 4.52; 95% CI = 2.92,7.01), a high proportion of White population (OR = 0.98; 95% CI = 0.96,0.99), a high proportion of Hispanic population (OR = 0.98; 95% CI = 0.96,0.99), a low proportion of the adult population who meet PA guideline (OR = 0.93; 95% CI = 0.91,0.96), a high proportion of uninsured adults under age 65 (OR = 1.05; segregation 95% CI = 1.03,1.08), higher between subpopulations and (OR = 0.12; 95% CI = 0.03,0.57). On the other hand, low-low DRMR cluster counties are characterized by: a high proportion of households who lack independent access to grocery stores (OR = 0.76; 95% CI = 0.68,0.86), a high percent of adults that meet PA guidelines, and a high proportion of the White population (OR = 1.06; 95% CI = 1.02,1.10).
Table 3.
Results of multinomial logistic regression to depict the association between DRMR clusters and socioecological factors.
| Variables | Type of clusters | |||
|---|---|---|---|---|
| High-High | Low-Low | Low-High | High-Low | |
| Social Capital Index (SKI) | 1.06 [0.94,1.19] | 0.97 [0.85,1.10] | 1.19* [1.00,1.42] | 1.19* [1.01,1.41] |
| Socioeconomic index (SEI) | 0.48*** [0.38,0.60] | 2.63*** [2.19,3.17] | 1.01 [0.66,1.55] | 1.11 [0.79,1.55] |
| Income disparity(Gini coefficient) | 0.03 [0.00,2.25] | 7.23 [0.10,545.87] | 4798.23* [3.20,7.19 × 106] | 0.00 [0.00,3.25] |
| Percent with low access to grocery store | 1.06 [1.00,1.13] | 0.79*** [0.70,0.89] | 0.96 [0.83,1.10] | 0.91 [0.79,1.06] |
| Retail Food Environment Index (RFEI) | 4.52*** [2.92,7.01] | 0.48* [0.27,0.87] | 2.54* [1.03,6.26] | 0.28* [0.10,0.82] |
| Spatial Proximity Index (SPI) | 0.12** [0.03,0.57] | 3.46 [0.42,28.48] | 1.92 [0.10,36.52] | 0.13 [0.02,1.02] |
| Percent of uninsured adults | 1.05*** [1.02,1.08] | 1.04** [1.01,1.08] | 1.07* [1.02,1.13] | 1.00 [0.95,1.05] |
| No. of hospital beds per 1000 population | 0.98 [0.95,1.01] | 1.02 [1.00,1.05] | 1.01 [0.96,1.06] | 1.04* [1.00,1.07] |
| No. of active physicians per 1000 population | 0.85 [0.50,1.46] | 0.94 [0.63,1.39] | 0.64 [0.25,1.67] | 0.86 [0.45,1.64] |
| Percent Whites | 0.97*** [0.96,0.99] | 1.06** [1.02,1.11] | 0.98 [0.95,1.01] | 0.95*** [0.93,0.98] |
| Percent of Blacks | 1.00 [0.98,1.01] | 1.00 [0.95,1.04] | 0.99 [0.96,1.02] | 0.97* [0.94,1.00] |
| Percent of Hispanics | 0.98** [0.96,0.99] | 1.04 [1.00,1.09] | 0.98 [0.95,1.02] | 0.97 [0.95,1.00] |
| Percent adults meet PA guideline | 0.93*** [0.91,0.96] | 1.08*** [1.04,1.12] | 0.95 [0.89,1.01] | 1.08* [1.01,1.15] |
| Percent urban population | 1.28 [0.66,2.46] | 1.55 [0.78,3.08] | 0.38 [0.11,1.37] | 1.51 [0.50,4.60] |
| Constant | 409.08** [9.83,17,032.28] | 0.00*** [0.00,0.00] | 0.02 [0.00,29.08] | 3.64 [0.00,2971.29] |
p < 0.05,
p < 0.01,
p < 0.001.
95% confidence intervals in brackets. The multinomial logistic odd ratio is in comparison to non-significant cluster (base model).; PA=physical activity
4.3. Spatial econometrics estimation results
4.3.1. Spatial Durbin Model
The direct and indirect effects derived from SDM are presented in Table 4. The findings suggest that a unit increase in the proportion of Black and Hispanic residents in neighboring counties would increase the DRMR in a specific county by 41.5% and 60.2%, respectively. If the proportion of the Black and Hispanic population increased by one unit simultaneously in all other counties, DRMR would increase by 43.6% and 47.6% in a typical contiguous US county, respectively. Similarly, residential segregation is associated with DRMR in the same county but there is no spillover effect. A one unit increase in the spatial proximity index would entail increase of DRMR by 20.1% in the same county. Socioeconomic indicators, such as education, employment and household income, and retail food environment and access, usually follow the pattern of ethnic composition and residential segregation in a county. Therefore, the demographic composition results should be interpreted within the context of socioeconomic status of the subpopulation and their genetic predisposition to diabetes.
Table 4.
Direct and indirect impacts of change in health care access, socioeconomic, and built environment variables on county DRMR.
| Explanatory variables | SDM Lag (Std. error) | SDM impacts | % of indirect impacts | ||
|---|---|---|---|---|---|
| Direct | Indirect | Total | |||
| Social capital index (SCI) | 0.023*(0.010) | 0.009 | 0.045** | 0.054** | 84.08 |
| Socioeconomic index (SEI) | 0.137***(0.018) | −0.288*** | 0.003 | −0.286*** | |
| Income disparity (Gini coefficient) | −1.011**(0.358) | −1.222*** | −2.687*** | −3.908*** | 68.75 |
| Retail food environment index (RFEI) | 0.113**(0.043) | 0.091*** | 0.264*** | 0.355*** | 74.37 |
| Percent HH with low access to grocery stores | 0.004(0.007) | 0.008* | 0.013 | 0.022 | |
| No. of hospital beds per 1000 population | −0.002(0.003) | −0.001 | −0.004 | −0.004 | |
| No. of active physicians per 1000 population | 0.002(0.001) | 0.001 | 0.005* | 0.006* | 82.62 |
| Proportion of uninsured Adults | 0.575(0.288) | −0.579* | 0.515 | −0.064 | |
| Proportion of Blacks | 0.197(0.114) | 0.015 | 0.347* | 0.362** | 95.85 |
| Proportion of Hispanics | 0.316*(0.135) | −0.082 | 0.471** | 0.389** | 85.17 |
| Spatial proximity index (SPI) | −0.214(0.127) | 0.186** | −0.215 | −0.030 | |
| Proportion of adults meets PA guideline | −0.923***(0.262) | 0.279 | −1.344*** | −1.066*** | 82.81 |
| Percent of urban population | −0.051(0.057) | 0.183*** | 0.060 | 0.243* | |
Significance levels:
< 0.001,
<0.01, &
<0.05.;
HH = households; PA = physical activity
The impact of an improvement in socioeconomic status, at the county and at national level, would reduce DRMR. A unit increase in socioeconomic index of a particular county would decrease the DRMR by 25.0% in the same county. In addition, a unit increase in socioeconomic index simultaneously in all counties would decreases DRMR by 24.9% in a typical contiguous US county. Socioeconomic status did not have immediate spillover effects on neighboring counties. The direct impact of the social capital index (SCI) on DRMR is not statistically significant but it has a spillover effect on neighboring counties. If SCI increased by one unit in neighboring counties, DRMR would increase by 4.6% in a specific county. The positive association between increased neighboring counties’ SCI and increased DRMR in a specific county can be interpreted as the negative psychological effect of neighboring counties’ relatively high social capital on the health of residents of a neighboring county with low social capital. Similarly, income inequality did not yield the expected result. Once economic characteristics and social capital are captured in the model, income disparity is only measuring differences in average income between counties. Thus, the negative sign on the direct, indirect, and total effects of income disparity indicate that the impact of increased income in neighboring counties and within the same county would have reduced the DRMR in a specific county as well as in a typical US county.
After controlling for socioeconomic status, hospital and physician density did not yield statistically significant results. Similarly, the direct impact of the proportion of the uninsured population (age 18–64) has the opposite effect than expected, but no spillover effect from a change in the proportion of the uninsured in neighboring counties. This is evident if we break down the regression results by region. In the Western and Mountain regions of the US, where the proportion of adults who meet physical activity guidelines was high and mortality rate was low, the proportion of the uninsured was also high. In addition, it should be noted that our outcome is a mortality rate.
The Rural-Urban continuum index has a statistically significant impact. If the proportion of the urban population increases by a unit, DRMR in the same county would increase by 20.1%. If the proportion of the urban population increases simultaneously in all counties, DRMR would decrease by 27.5% in a typical contiguous US county. This “rural-urban paradox” only appears after the socioeconomic index was included in the model. The “rural-urban paradox” refers to standardized mortality rates in rural areas that are unexpectedly low in view of well-known economic and infra structural disadvantages there.
The impact of a change in the Retail Food Environment Index (RFEI) was not limited to a direct effect. There was also a spillover effect to neighboring counties. An increase in RFEI in a particular county would increase the DRMR by 9.5% in the same county. A unit increase in RFEI in neighboring counties would increase DRMR by 30.2% in a specific county. A unit increase in RFEI simultaneously in all other counties would increase DRMR by 42.6% in a typical contiguous US county. Similarly, an increase in the proportion of residents who lack independent access to grocery stores would increase DRMR by 0.8% in the same county but have no spillover effect. In the Western, Southwestern, and Mountain regions of the US, a lack of access to grocery stores was negatively associated with DRMR. In Northern, Southeast, and western sections of the Midwest, Appalachia, and New England, a lack of access to grocery stores was positively associated with DRMR.
5. Discussion
This study was designed to test three hypotheses: 1) diabetes-related mortality rates (DRMR) in US counties are spatially auto correlated, 2) DRMR is spatially associated with socioeconomic, demographic, and health service factors and 3) there is spatial spillover effect from the association between socioeconomic, demographic, and health service factors. The study found that DRMR in US counties is spatially correlated and identified clusters of counties where DRMR is high or low. Hotspot counties are located throughout the Southern Plains, Southeastern, and Appalachian regions of the US. States where high DRMR is clustered include Ohio, West Virginia, the western part of Virginia, Pennsylvania, North Carolina, South Carolina, Kentucky, Tennessee, Mississippi, Oklahoma, and Texas. Cold spots were observed in the Mountain regions (Montana, Wyoming, Idaho, South Dakota, Utah, Colorado), and Southwest states (Nevada and northwestern California). These regions were previously described as less economically favorable regions with high proportion of unemployment and access to social capital (Dray-Spira et al., 2010; Murray et al., 2006; Saydah & Lochner, 2010).
Understanding the regional clustering of DRMR and associated ecological factors is vital to developing effective strategies and health delivery policies in order to reduce the burden of DRMR. In light of this, using exploratory and spatial econometrics analysis we showed that counties where DRMR is high have distinct socioeconomic, demographic and food environment characteristics. They have lower median household income, lower levels of education, and high unemployment rates. Fast food restaurants and a lack of access to grocery stores and full service restaurants dominate the food environment in these counties. A significant percentage of residents in these counties lack access to healthy food due to the distance to grocery stores and a lack of independent access to vehicles. Large proportions of residents in high DRMR counties also did not meet the PA guideline compared to counties where DRMR did not cluster. This is an indication that a majority of the population in high DRMR clusters lack awareness of the health benefits from engaging in PA and may also lack the opportunities to engage in physical activities. This result is similar to the findings of Shrestha et al. (2012) on the association between socioecological factors and clusters of diabetes.
The spatial spillover effect was tested using the Spatial Durbin Model (SDM). According to this model, in addition to the direct impact within the same counties, simultaneous one-unit improvements in the socioeconomic index (SEI) in all other contiguous counties would reduce DRMR by about 29% in a typical US county. However, the spillover effect from changes in SEI in immediate neighboring counties to a particular county was not statistically significant. These results are partially consistent with other spatial studies of the association between socioeconomic status and overall mortality (Chen, Deng, Yang, & Matthews, 2012; Yang, Noah, & Shoff, 2013). However, unlike Yang et al. (2013) this study did not find a spillover effect of socioeconomic change on the immediate neighboring county.
Successful management of diabetes may require frequent contact with primary care facilities and hospitals (Willens, Cripps, Wilson, Wolff, & Rothman, 2011). Increased density of health care facilities and physicians promote more access to care, thereby, reducing mortality rate. However, density of facilities and services by themselves do not increase utilization rate. Once socioeconomic, social capital and the proportion of minority in the county is controlled, hospital bed density did not yield the expected results. The spillover effect from increased hospital bed density and the proportion of uninsured on other counties was statistically insignificant. The spillover effect from physician’s density (whether it is all physicians or primary care physicians) contradicted expectations; it was positively associated with DRMR in other counties. This result implies that physicians are located in places where there is the greatest demand, so a diabetes cluster attracts more primary care physicians.
The result for the proportion of uninsured is contrary to the prior finding that insurance coverage increases access to medical care, thereby reducing mortality rates (Sommers et al., 2012; Sommers, Long, & Baicker, 2014). Once underlying factors, such as socioeconomic status and the proportion of Black and Hispanic populations, were captured in the model, the proportion of the uninsured population measures the proportion of adults that were not participating in the insurance market. Nonparticipants in the insurance market tend to be healthy young adults (age 19–34) and tend to be employed in agriculture and construction sectors and small business (Kaiser Family Foundation, 2013). Prior to passage of the Affordable Care Act, young adults were found to be less concerned with health insurance, so less likely to participate in the insurance market (Holahan & Kenney, 2008). Somewhat differently, agricultural workers and employees of small businesses are typically not covered by employer based insurance. Thus, counties where either agriculture is a major economic sector or where a high proportion of young adults live may also have a high proportion of uninsured non-senior adults.
In addition, the Hill-Burton Act established the requirement that hospitals provide necessary services to stabilize a patient regardless of the patient’s ability to pay (Melhado, 2006). Therefore, it makes intuitive sense that insurance coverage would influence healthcare utilization, as implied in the literature, but would not be a significant predictor of mortality rates.
The spatial spillover effect from a unit change in the retail food environment in a neighboring county would increase DRMR by 26% in a particular county, and simultaneously one-unit increase in RFEI in all other counties would increase DRMR by 35% in a typical contiguous US county. Therefore, improvements in the retail food environment in a particular county may have beneficial spillover effects on the immediate neighboring counties’ DRMR, which is consistent with the fact that many people commute to the neighboring counties for work. This is especially the case for counties near large metropolitan counties where business is concentrated in counties with large cities (Zhong, 2016). The implication that can be drawn from these results is that economic, social capital and retail food environments are the most important factors associated with DRMR. Improvements in socioeconomic status and access to healthy food would significantly reduce DRMR in contiguous US counties.
In sum, this study affirms socioeconomic, social capital, behavioral, and ecological factors are the major contributors for diabetes related mortality. Currently, Centers for Disease Control and Prevention (CDC) recommends use of the National Diabetes Prevention Program (NDPP) as the primary diabetes prevention and management program (Diabetes Prevention Program Research Group, 2002). First, currently the program is offered in few metropolitan areas by national organizations such as the Young Men’s Christian Association and Weight Watchers. ACTIVE (Appalachians Coming Together to Increase Vital Exercise) is one encouraging program that was developed for the rural Appalachian region (De Groot et al., 2012). The program is not available in areas with high diabetes prevalence and mortality including the Appalachian region of the United States. Second, the program recommends promoting dietary modification and physical activity to reduce the incidence of diabetes and manage diabetes. However, diabetes prevalence and diabetes related mortality is high among residents of counties with low socioeconomic index and social capital, fast food dominated food environment, and low access to grocery stores, which makes it very difficult to implement this CDC recommended program. Furthermore, our finding of significant spatial correlation as well as spillover effect of socioeconomic and ecological factors on county DRMR suggests that the effects of public health interventions may focus on improving the socioeconomic and ecological factors confounding the implementation of the intervention programs and the target counties with high DRMR.
This study has several limitations. First, the use of counties as the unit of analysis for the study implies that interpretations of the associations between DRMR and socio-ecological factors should be made with caution. A well-known problem with aggregated data is the ecologic fallacy, or the assumption that associations among variables assessed from aggregate data apply to analogous individual-level variables, which may lead to incorrect inferences at the individual level. It hides the heterogeneity between individuals and the joint distribution of explanatory variables at the individual level (Morgenstern, 1995). The variables in this study are mostly at the ecological level, so interpretations of the results strictly followed the ecological nature of the variables. Second, not all the socioecological phenomena explored in this study necessarily operate at the county-level, so the conclusions may be affected by the so-called modifiable areal unit problem. That is, results from a county-level study may not hold for smaller (e.g. neighborhood or census tract) or larger (e.g. a state) geographical units. The migration of people from county to county is also not accounted for in this study. On the other hand, the county is the smallest geographical unit for which mortality data is publicly available. Moreover, the planning and execution of health services often occurs at county-level. Thus, the use of counties as the unit of analysis for mortality data is justified. Even with the limitations, ecologic analysis is often preferred when a phenomenon under study is public health implementation, where geographic boundaries are meaningful so long as variable selection is appropriate (Portnov, Dubnov, & Barchana, 2006). In addition, smaller mortality counts are either suppressed or flagged as unreliable in the CDC WONDER data. The unreliability of this data for the smaller mortality counts and imputation of the missing data could introduce heteroscedasticity into the parameter estimates.
Despite the inherent limitations of ecological study, the findings from this study have strengths. First, the study not only confirmed that contiguous US county DRMR is spatially correlated but also clustered in some regions. Second, the study showed how to combine exploratory spatial analysis and spatial econometric methods to identify high DRMR cluster counties and associated socio-ecological factors. It combined exploratory spatial statistics, multinomial regression and spatial regression models to overcome some of the issues posed by heterogeneity in prior ecological studies. For example, the combination of Moran’s-I statistics and multinomial regressions helped in identifying socio-ecological factors that are associated with cold spots and hot spots. Identification of DRMR clusters can be helpful in health resource allocation and management, and health managers could target resources to areas identified as high DRMR clusters. Third, this study used spatial autoregressive and Spatial Durbin Models to identify the most impactful socio-ecological factors for use in future interventions.
6. Conclusions
Our study showed that improvements in socioeconomic and ecological gradients in one county could have an impact on reducing DRMR beyond the immediate county. The policy implication from these findings is that efforts to reduce DRMR should invest in the most impactful ecological factors, such as improving socioeconomic gradients (income, education, and employment), access to healthy food and social capital (e.g., the environment where residents engage in physical activities and social activities). Intervention programs should target counties within high DRMR clusters while strategically considering the heterogeneous interrelationships between counties due to socioeconomic and policy interactions and shared resources.
Supplementary Material
Acknowledgements
We would like to thank Sara McLafferty and Mary Arends-Kuenning for comments on early drafts of the manuscript.
Footnotes
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.apgeog.2017.05.005.
References
- Alter DA, & Eny K (2005). The relationship between the supply of fast food chains and cardiovascular outcomes. Canadian Journal of Public Health, 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anselin L (1995. Apr 1). Local indicators of spatial association—LISA. Geographical Analysis, 27(2), 93–115. [Google Scholar]
- Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, Karter AJ, Safford M, Waitzfelder B, Prata PA, & Beckles GL (2004. Jul 1). Socioeconomic position and health among persons with diabetes mellitus: A conceptual framework and review of the literature. Epidemiologic Reviews, 26(1), 63–77. [DOI] [PubMed] [Google Scholar]
- California Center for Public Health Advocacy. (2008). Policy Link, the UCLA Center for Health Policy Research: Designed for Disease: The Link Between Local Food Environments and Obesity and Diabetes. Davis, CA: http://healthpolicy.ucla.edu/publications/search/pages/detail.aspx?PubID=190. [Google Scholar]
- Carpiano RM, Lloyd JEV, & Hertzman C (2009). Concentrated affluence, concentrated disadvantage, and children’s readiness for school: A population-based, multi-level investigation. Social Science and Medicine, 69(3), 420–432. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Compressed Mortality File (CMF) on CDC WONDER Online Database. The current release for years 1999–2010 is compiled from: CMF 1999–2010, Series 20, No. 2P, 2013. [Google Scholar]
- Chen VY, Deng WS, Yang TC, & Matthews SA (2012. Apr 1). Geographically weighted quantile regression (GWQR): An application to US mortality data. Geographical Analysis, 44(2), 134–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler DM, Lleras-Muney A, & Vogl T (2008). Socioeconomic status and health: dimensions and mechanisms (No. w14333). National Bureau of Economic Research. [Google Scholar]
- De Groot M, Doyle T, Kushnick M, Shubrook J, Merrill J, Rabideau E, et al. (2012). Can lifestyle interventions do more than reduce diabetes risk? Treating depression in adults with type 2 diabetes with exercise and cognitive behavioral therapy. Current Diabetes Reports, 12(2), 157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshpande AD, Baker EA, Lovegreen SL, & Brownson RC (2005). Environmental correlates of physical activity among individuals with diabetes in the rural Midwest. Diabetes Care, 28(5), 1012–1018. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program (DPP) Research Group. (2002). The diabetes prevention program (DPP). Diabetes Care, 25(12), 2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dray-Spira R, Gary-Webb LT, & Brancati FL (June 2010). Educational disparities in mortality among adults with diabetes in the U.S. Diabetes Care, 33, 1200–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede LE, Nietert PJ, & Zheng D (2005). Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care, 28, 1339–1345. [DOI] [PubMed] [Google Scholar]
- Elhorst JP (2010). Applied spatial Econometrics: Raising the bar. Spatial Economic Analysis, 5(1), 9–28. [Google Scholar]
- Economic Research Service(ERS) food atlas data. (2012). US department of agriculture (USDA). https://www.ers.usda.gov/data-products/food-environment-atlas/.
- Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, Neumiller JJ, Nwankwo R, Verdi CL, Urbanski P, & Yancy WS (2014. Jan 1). Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care, 37(Suppl. 1), S120–S143. [DOI] [PubMed] [Google Scholar]
- Glasgow RE (1995). A practical model of diabetes management and education. Diabetes Care, 18(1), 117–126. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, & Popkin BM (2006). Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics, 117, 417–424. [DOI] [PubMed] [Google Scholar]
- Holahan J, & Kenney G (2008). Health insurance coverage of young Adults: Issues and broader considerations. Washington DC: Urban Institute. Retrieved from: http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2008/rwjf28260. [Google Scholar]
- International Diabetes Federation. (2015). Atlas. http://www.diabetesatlas.org/atlas/atlas.html. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured/Urban Institute analysis of the 2013. ASEC Supplement to the CPS. [Google Scholar]
- LeSage JP, & Pace RK (2009). Introduction to spatial econometrics. CRC press. [Google Scholar]
- LeSage JP, & Pace RK (2014). Interpreting spatial econometric models. Handbook of Regional Science. [Google Scholar]
- Massey DS, & Denton NA (1988). The dimensions of residential segregation. Social forces, 67(2), 281–315. [Google Scholar]
- Massey DS (2001). Residential segregation and neighborhood conditions in US metropolitan areas. America Becoming: Racial Trends and Their Consequences, 1(1), 391–434. [Google Scholar]
- Massing MW, Rosamond WD, Wing SB, Suchindran CM, Kaplan BH, & Tyroler HA (2004). Income, income inequality, and cardiovascular disease mortality: Relations among county populations of the United States, 1985 to 1994. Southern Medical Journal, 97(5), 475–484. [DOI] [PubMed] [Google Scholar]
- McLaughlin DK, & Stokes CS (2002). Income inequality and mortality in US counties: does minority racial concentration matter? American Journal of Public Health, 92, 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy K, Bibeau D, & Steckler A (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15, 351–377. [DOI] [PubMed] [Google Scholar]
- Melhado E (2006). Health planning in the United States and the decline of public-interest policymaking. Milbank Quarterly, 84(2), 359–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran PAP (1950). Notes on continuous stochastic phenomena. Biometrika, 37(1), 17–23. [PubMed] [Google Scholar]
- Morgenstern H (1995). Ecologic studies in epidemiology: Concepts, principles, and methods. Annual Review of Public Health, 16(1), 61–81. [DOI] [PubMed] [Google Scholar]
- Murphy SL, Xu JQ, & Kochanek KD (2013). National Vital Statistics Reports. Deaths: Final data for 2010 (Vol. 61, No. 4). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, & Ezzati M (2006. Sep 12). Eight Americas: Investigating mortality disparities across races, counties, and race-counties in the United States. Plos Medicine, 3(9), e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Carroll PW, Yasnoff WA, Ward ME, & Ripp LH (2002). Public health informatics and information systems. New York: Springer-Verlag. [Google Scholar]
- Pietrzak MB (2013). Interpretation of structural parameters for models with spatial autoregression. Equilibrium, 8(2), 129–155. [Google Scholar]
- Portnov BA, Dubnov J, & Barchana M (2006). On ecological fallacy, assessment errors stemming from misguided variable selection, and the effect of aggregation on the outcome of epidemiological study. Journal of Exposure Science and Environmental Epidemiology, 17(1), 106–121. [DOI] [PubMed] [Google Scholar]
- Rupasingha A, & Stephan JG (2008). US County-Level Social Capital Data, 1990–2005. The Northeast Regional Center for Rural Development, Penn State University, University Park, PA. [Google Scholar]
- Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, & Narayan KV (2006. Apr 4). Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Annals of Internal Medicine, 144(7), 465–474. [DOI] [PubMed] [Google Scholar]
- Sallis JF, & Owen N (2002). Ecological models of health behavior. In Glanz K, Lewis FM, & Rimer BK (Eds.), Health behavior and health Education: Theory, Research, and Practice (pp. 462–484). San Francisco, Calif: Jossey-Bass. [Google Scholar]
- Saydah S, Imperatore G, & Beckles GL (2013). Socioeconomic Status and Mortality: Contribution of health care access and psychological distress among U.S. adults with diagnosed diabetes. Diabetes Care, 36(1), 49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saydah S, & Lochner K (2010). Socioeconomic status and risk of diabetes-related mortality in the U.S. Annals of Internal Medicine, 125(3), 377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Macinko J, Starfield B, Politzer R, Wulu J, & Xu J (2005). Primary care, social inequalities, and all-cause, heart disease, and cancer mortality in US counties, 1990. American Journal of Public Health, 95(4), 674–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha SS, Kirtland KA, Thompson TJ, Barkerb L, Gregg EW, & Geiss L (2012). Spatial clusters of county-level diagnosed diabetes and associated risk factors in the United States. The Open Diabetes Journal, 5, 29–37. [Google Scholar]
- Singh GK (2003). Area deprivation and widening inequalities in US mortality, 1969–1998. The American Journal of Public Health, 93, 1137–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers BD, Baicker K, & Epstein AM (2012). Mortality and access to care among adults after state Medicaid expansions. New England Journal of Medicine, 367(11), 1025–1034. [DOI] [PubMed] [Google Scholar]
- Sommers BD, Long SK, & Baicker K (2014). Changes in mortality after Massachusetts health care reform: A quasi-experimental study. Annals of Internal Medicine, 160(9), 585–593. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. https://www.census.gov/2010census/data/.
- Voeks JH, McClure LA, Go RC, Prineas RJ, Cushman M, Kissela BM, et al. (2008). Regional differences in diabetes as a possible contributor to the geographic disparity in stroke mortality the REasons for geographic and racial differences in stroke study. Stroke, 39(6), 1675–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weng C, Coppini DV, & Sönksen PH (2000). Geographic and social factors are related to increased morbidity and mortality rates in diabetic patients. Diabetic Medicine, 17(8), 612–617. [DOI] [PubMed] [Google Scholar]
- Wilcox S, Castro C, King AC, Housemann R, & Brownson RC (2000). Determinants of leisure time physical activity in rural compared with urban older and ethnically diverse women in the United States. The Journal of Epidemiology and Community Health, 54, 667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willens D, Cripps R, Wilson A, Wolff K, & Rothman R (2011). Interdisciplinary team care for diabetic patients by primary care physicians, advanced practice nurses, and clinical pharmacists. Clinical Diabetes, 29(2), 60–68. [Google Scholar]
- Yang TC, Noah AJ, & Shoff C (2013). Exploring geographic variation in US mortality rates using a spatial Durbin approach. Population, Space and Place. 10.1002/psp.1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong L (2016. Sep 20). Metropolitan spillover effects and economic growth of non-metropolitan Areas: Evidence from Indiana counties. International Journal of Regional Development, 3(2), 107. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


