Abstract
Recruitment and retention of patients with acute pancreatitis (AP) in clinical studies can be challenging. While some obstacles are similar to other clinical conditions, some are unique to AP. Identifying potential barriers early and developing targeted solutions can help optimize recruitment and retention in AP studies. Such preemptive and detailed planning can help prospective, longitudinal studies focusing on exocrine and endocrine complications of AP in accurately measuring outcomes. This manuscript highlights the challenges in recruitment and retention strategies in AP studies and reviews available resources to create opportunities to address them. We describe the multifaceted approach used by the Recruitment and Retention Committee of the Type 1 Diabetes in Acute Pancreatitis Consortium (T1DAPC), which builds upon earlier experiences to develop a recruitment and retention plan for the DREAM (Diabetes RElated to Acute pancreatitis and its Mechanisms) study.
Keywords: acute pancreatitis, diabetes, enrollment, challenges and barriers, follow-up
Introduction
Acute pancreatitis (AP), an inflammatory condition of the exocrine pancreas with increasing incidence,1 can lead to metabolic complications, including diabetes mellitus (DM).2–4 The Type 1 Diabetes in Acute Pancreatitis Consortium (T1DAPC) was established by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) in 2020 to study the interplay between the exocrine and endocrine pancreas in the development of DM after AP. Its prospective longitudinal observational study, DREAM (Diabetes RElated to Acute pancreatitis and its Mechanisms), is designed to investigate the incidence, etiology, and pathophysiology of DM following AP, as described elsewhere in this issue. The T1DAPC Recruitment and Retention Committee (RRC) (Fig. 1), includes representatives from each of the T1DAPC clinical centers, the Data Coordinating Center (DCC), and the NIDDK. This manuscript describes the approach to recruitment and retention developed by the RRC for the DREAM study and highlights opportunities that may also be beneficial to future studies of AP.
FIGURE 1.
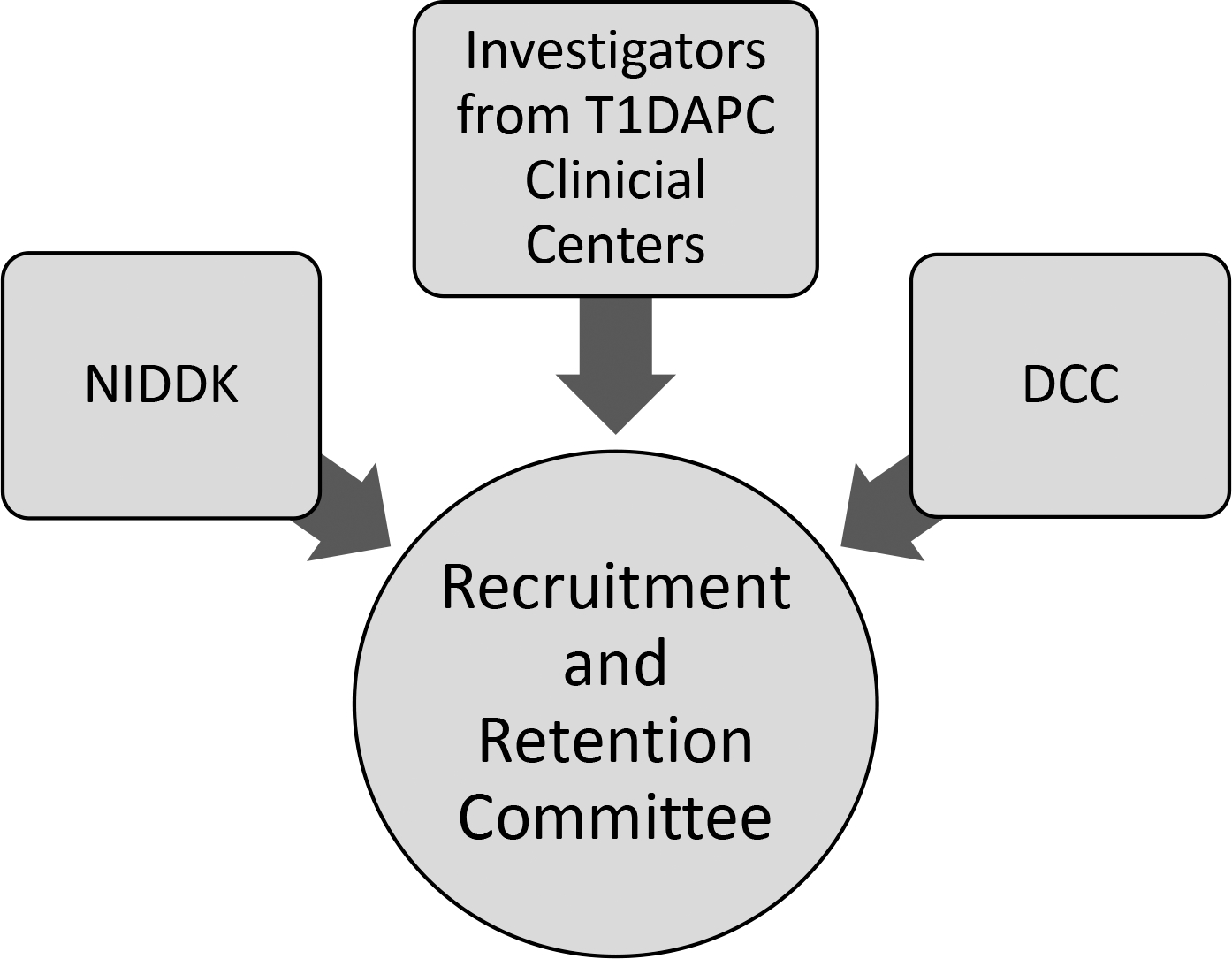
Schematic presentation of the T1DAPC Recruitment and Retention Committee that includes representatives from each of the T1DAPC clinical centers, DCC, and NIDDK.
Structure of the Type 1 Diabetes in Acute Pancreatitis Consortium (T1DAPC) Recruitment and Retention Committee
Challenges in Recruitment and Retention in the Setting of AP
Up to 20% of all clinical studies either terminate early from failure to reach accrual goals or close enrollment prematurely leading to loss of study power to address the primary hypothesis.5 Some of the general barriers for enrollment include financial constraints (eg, time away from work, travel to clinical site), difficulties in decision making (eg, struggle to understand risk benefit ratio), distrust and fear towards research, and lack of social support.6,7 Another factor, influenced by practice and referral patterns, is the common tendency of community based hospital and practitioner to delay referral to academic medical centers, where most of clinical research takes place in the US. Challenges unique to AP studies include defining the study population, lack of infrastructure for identification of those with AP, and lack of consistent clinical follow up, particularly after mild AP.6 Factors related to disease itself may complicate recruitment and retention. For example, heavy alcohol use is an important risk factor for AP, but some individuals with alcohol abuse disorders may have psychosocial comorbidities that make retention challenging. Individuals with mild AP that completely resolves, regardless of the etiology, may not see a benefit from long-term follow up and thus may be more prone to withdraw or not comply with study procedures during follow up. Consequently, planning trials around recruitment and retention is critical for efficient, generalizable, and cost-effective research.5
The majority of previous clinical studies in AP were designed to assess inpatient and short interval outpatient outcomes such as organ failure, infected pancreatic necrosis, or mortality.8,9 To date, few prospective cohort studies in pancreatitis have been designed with comprehensive long-term assessments, protocol-mandated evaluations, and rigorous biological sample collections10–15 but most were endoscopically driven with short term follow up, and only one reported retention rate of 77% at 12-month follow up. Participation of many T1DAPC investigators in the design and execution of prior studies offers important “lessons learned” from struggles with recruitment and/or retention. The DREAM study will present unique and new challenges in recruiting a broader AP population including those with mild disease and retaining participants for years of follow up.
MATERIALS AND METHODS
Consultation With Recruitment Innovation Center
The DREAM study provided a unique opportunity to capitalize on this emerging experience studying AP to design systematic recruitment and retention strategies ready for implementation at the time of enrollment of the first subject. To achieve this goal, the T1DAPC applied for, and was awarded, a consult with the Recruitment Innovation Center (RIC) through the Trial Innovation Network (TIN) for expert, third party review to identify barriers to and develop novel strategies for the recruitment and retention of participants.16 The RIC is a resource offered through the TIN supported by Clinical and Translational Science Award hubs. The RIC serves as a national resource and collaborative “storefront” for investigators seeking guidance for research subject engagement, recruitment, and retention.16,17 A detailed overview of their consultation process is outlined by Wilkins et al16 (Fig. 2).
FIGURE 2.
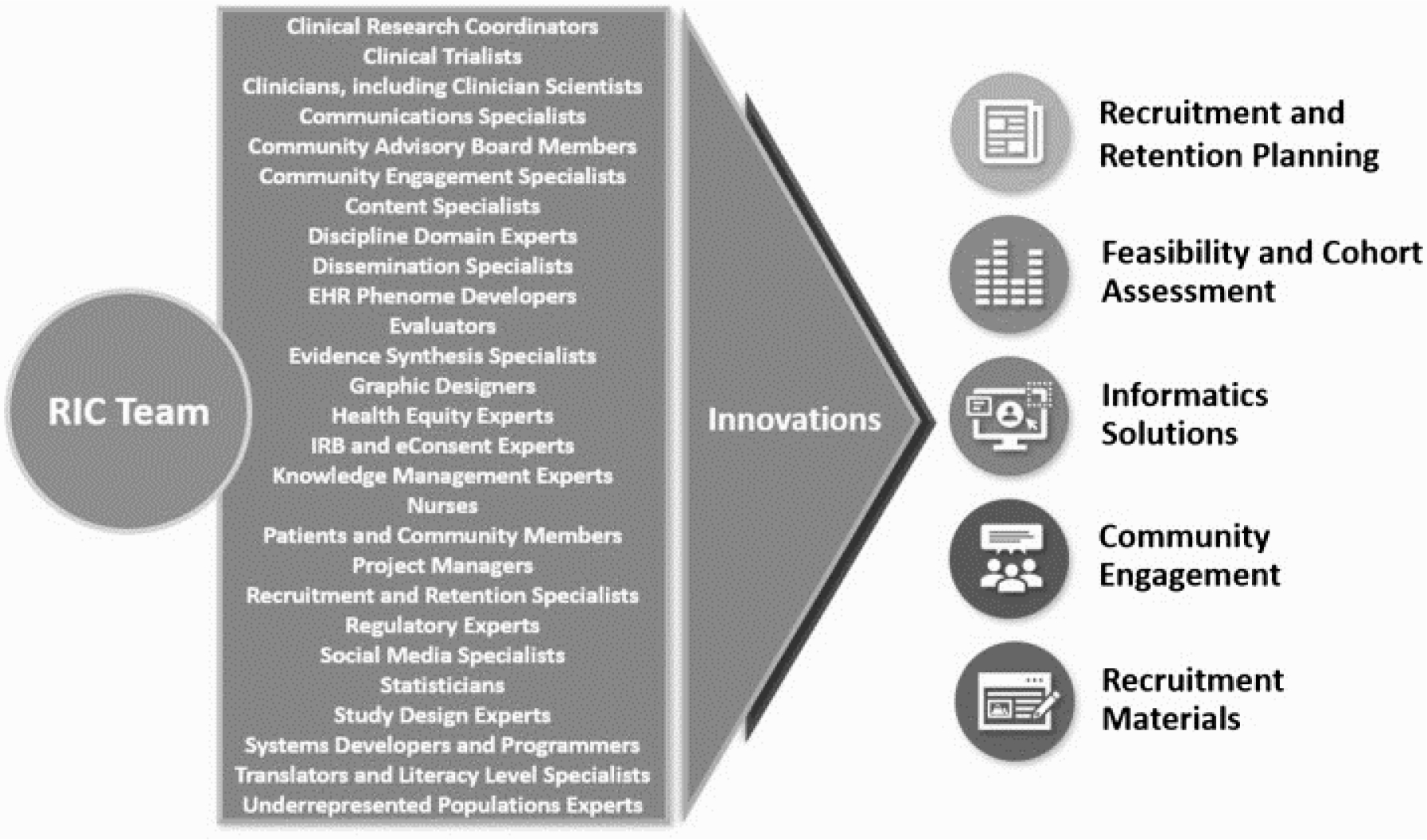
The Recruitment Innovation Center (RIC) consultation involves engaging multidisciplinary RIC team in recruitment and retention planning and results in development of innovative solutions (obtained with permission from Wilkins et al16).
Schematic overview of Recruitment Innovation Center consultation process
The RIC supported the RRC in optimizing feasibility of the DREAM study across the T1DAPC Clinical Centers. Additionally, through the RIC’s partnership with the Regenstrief Institute, the RRC was able to consult with Clinical Systems Optimization experts. For example, how to best design algorithms to utilize existing informatics infrastructure (eg, electronic health records [EHR] queries and alert tools) for screening and identifying potential participants. The RIC also helped us developing an inventory and provided advice on balancing existing clinical studies locally, regionally, and nationally that may compete with DREAM for participants. The RIC helped in the design and review of resources to increase awareness of DREAM such as social media announcements, and patient and clinician facing recruitment materials, which offered novel and important enhancements such as the addition of smartphone quick response (QR) codes directing participants to DREAM website(s). We worked collaboratively to ensure there are appropriate compensation practices for participants, methods to eliminate redundant study procedures/visits, and guidelines for investigators to share results of study procedures. Suggestions focusing on solutions for anticipated difficulties with participant engagement and how to best build and maintain trust were also considered for incorporation into training guidelines for staff. These guidelines are expected to serve as a foundation for lasting relationships with participants and create the best circumstances for retention.
RESULTS
Recruitment and Retention Plan for the DREAM Study
The RRC has met regularly with an early focus on developing a variety of recruitment and retention strategies that will provide flexible adaptation and implementation for site specific needs across a geographically diverse consortium. The RRC developed an expected enrollment target for each T1DAPC Clinical Center taking into consideration the pool of available patients, participant burden, and the potential of competing studies. In addition, an accrual report and screening failure log were developed. The accrual report which will be generated by the DCC on a regular basis is designed to summarize enrollment by each site, completed visits, withdrawals and reasons for withdrawal. The clinical research coordinators (CRCs) will use a screening log to document participants potentially eligible on prescreening who were approached for enrollment, but declined participation.
Enrollment of Underrepresented Racial and Ethnic Minorities
African Americans (AAs) are at 2–3 times higher risk for AP compared to whites18,19 and Hispanic patients have delayed access to care during AP attacks,20 illustrating that minority populations are disproportionally affected. In addition, the prevalence of type 2 diabetes in the US differs by race and ethnicity. Thus, recruitment strategies that target enrollment reflective of the racial and ethnic distribution of the US population are needed to improve the generalizability of the DREAM study results, particularly related to diabetes.
Many of the T1DAPC clinical centers serve diverse populations that include AA or Hispanic communities. Racial and ethnic characteristics of the study population as well as participants who electively withdrawal from the study will be monitored in the accrual reports.
Recruitment and Retention Methods
Participant Identification
Potential participants with an episode of AP in the preceding 90 days will be identified during hospitalization or from ambulatory clinics. Clinical centers will use daily serum amylase and lipase alerts (eg, serum levels greater than 3× upper limits of normal) to identify patients who are hospitalized with AP. Additionally, searches will be tailored using diagnosis codes or discharge diagnoses for AP. Qualifiers for exclusion criteria (eg, chronic pancreatitis, pancreatic cancer, pancreatic surgery) may be used to refine EHR-based queries. Ambulatory patients will be identified by review of clinic schedules, provider referrals, or responses to study advertisements. The study team will review EHR of all patients to confirm eligibility prior to approaching.
Approach and Enrollment
Potential participants will be approached by their clinical care team to ask if a study team member can reach out to discuss the study. Participants will be approached in-person or via electronic communications (email or through patient portals), telephone, letter or virtually through audiovisual communication to introduce the study and confirm eligibility criteria. If permitted by local policy, participants may be directly contacted by a study team member. Reasons for non-participation for those who were screened, but declined participation or were later found to be ineligible will be recorded in the screening log.
When approaching potential participants, CRCs will provide them with a study flyer and review the consent form. Depending on local institutional review board (IRB) guidelines, study flyers may be included with discharge papers of patients potentially eligible for the study. The CRCs will contact eligible participants in the weeks after discharge to review the study and discuss participation. If patients are interested in joining the study, an enrollment visit will be scheduled. Site-specific recruitment and retention plans have been developed to proactively identify and address recruitment barriers and mitigate roadblocks. A portfolio of recruitment materials will be available to adapt for local sites. A general overview of recruitment and retention methods, developed in consultation with the RIC, can be found in Table 1.
TABLE 1.
Available Recruitment and Retention Strategies for the Conduct of the DREAM (Diabetes RElated to Acute pancreatitis and its Mechanisms) Study
| Study Awareness | Site Engagement | Participant Engagement | Retention and Participant Satisfaction |
|---|---|---|---|
|
| |||
| Study website | Study clinician education | eConsent | Participant perception/satisfaction survey |
| Quick response (QR) code | Resident physician engagement | Return of Results with Clinician Consultation | Participant testimonials |
| Encounter during hospitalization | Gamification of Participant Enrollment | Thank you cards | Contacting participants with reminders about study visits |
| Study flyer to be included with discharge papers | Diabetes information materials | ||
| Post-hospitalization | Diabetes support referrals | ||
| Advertising via Social Media | |||
| Advertising via Print Materials | |||
| Participant testimonials | |||
Participant Compensation
Participants will be compensated for their time and effort commensurate with the complexity and duration of each study visit. Additionally, when appropriate parking and travel charges will be provided by reimbursements or vouchers, according to local IRB guidelines.
Delivery of Study Results to Participants
A summary of clinical test results (laboratory, imaging) performed as part of the research protocol will be provided to participants and included in their medical records. Participants will have an opportunity to discuss these findings with a study team member. In case a subject has abnormal findings on clinical tests or is diagnosed with pre-diabetes or diabetes, a site investigator or designated study team member will review the results with the participant.
Barriers and Solutions
Study Team Barriers
The investigators will ensure that study staff have the necessary skills and cultural competencies to recruit and retain underrepresented racial and ethnic minorities. Site-specific recruitment plans will address study team turnover with each site’s study team prior to enrollment of the first participant.
Participant-related Barriers
Characteristics that may potentially influence recruitment and retention include language barrier, patient reliability, a reliable method of communication, timing of introduction to proposed study, distance from the clinical site, costs related to study visits such as travel or parking, and social support status for patients who depend on family or friends to come to study visits.
In order to address language barrier, study consent and flyers will be translated into the native language of the potential participants. Similarly, having a native speaker or a translator during recruitment process can help in addressing language barrier. Since prior history of patient unreliability correlates to passive refusal rates, we may consider screening only those outpatients who consistently attend their ambulatory clinic appointments. Establishing the patient preferred method of contact prior to hospital discharge or at initial outpatient visit appears to be an effective strategy. Patients may not want to participate in a research study while having ongoing health-related concerns or pain, which take precedence over other activities. Ideally, approaching these patients on the day of discharge and obtaining their best contact information may decrease active refusals, facilitating subsequent outpatient contact. Recruitment and Retention methods described above have been described in detail (Supplemental Table 1) and developed to mitigate any barriers from these characteristics. Additional potential barriers and proposed mitigation strategies developed are included in Table 2.
TABLE 2.
Potential Participant Barriers and Solutions
| Potential Barrier | Mitigation Plan |
|---|---|
|
| |
| Lack of early engagement with participants, as many potential participants won’t have recurring symptoms after discharge from hospital | 1) Encourage clinical research coordinator to reach out to participants. 2) Have a dedicated staff member whose main role is outreach. 3) Automated outreach via MyChart (or similar methods) per local IRB guidelines. |
| Long-term participation in the study is too burdensome | 1) Study procedures that can be done remotely have been identified and will be discussed with participants. 2) Identify barriers to retention early and modify study based on the participant perceptions. 3) Allow flexibility in timing of study visits. 4) Provide ride services if needed or pay for parking and travel-related costs. |
| Competing studies limiting available participants | 1) All sites have agreed to prioritize the DREAM study. 2) Enrollment into DREAM study will not preclude participation in other studies. 3) New studies enrolling an overlapping population will be reviewed on a case-by-cases basis to ensure participant safety and integrity. |
Communication Plan
Communication with research participants, between collaborating investigators, and with external stakeholders is essential to the success of the DREAM study. The purpose, benefits, and risks of the study are communicated to participants not only through consent documents, but also through easy-to-read flyers and summary sheets. The DCC will share study information with the site CRC through the T1DAPC website and regular CRC calls, and via e-mail on an as-needed basis. The RRC will review and discuss accrual and retention with site Principal Investigators (PIs) during monthly Steering Committee calls.
Continuous Evaluation and Optimization
A Monitoring Committee has been established to oversee the execution of the DREAM study. This committee consists of the protocol chairs, members of the DCC, at least one co-chair from each working group (Diabetes, Pancreatitis, Immunology, Imaging and Artificial Intelligence), committees (RRC, Biospecimen), and the NIDDK. The monitoring committee will provide a centralized location for monitoring the progress of the DREAM study, respond to queries from sites relating to the study protocol and day to day operations, and propose potential solutions. Updates will be provided to the Steering Committee on a monthly basis, and include discussions regarding the need for modifications to the Manual of Procedures or study protocol. Monitoring plans will include review of monitoring reports generated by the DCC consisting of information on different aspects of study execution such as recruitment and retention, completion of study procedures, study withdrawal, screen failure rate, completion of case report forms, biospecimen collection, etc. The DCC has developed a plan for quality control, with feedback from the working groups and committees on specific measures (eg, performance of metabolic testing).
Examples of early quality control are listed and will be refined as the study progresses:
a. Diabetes and Metabolic Testing
Verification of clinical center specific, proper execution of metabolic testing early during the course of the study. In addition, the proportion of individuals with pre-existing diabetes, diabetes incidence, monitoring for failed/missing test results and need for cancellation, adherence to sampling timing during metabolic testing, and number of tests rescheduled due to high or low fasting plasma glucose levels will be monitored.
b. Immunology
Results received from the autoantibody laboratory and data collected from the clinical centers will be routinely reviewed. RNA will be extracted and quality evaluated from a limited number of participants from each clinical center early in the course of the study.
c. Pancreatitis
Best practices for algorithmic identification of potential participants admitted with AP has been disseminated to all clinical sites. The recruitment of AP patients will be monitored, including enrollment during the index hospitalization, distribution of etiology, severity, demographic (race, ethnicity) distribution, and reasons for screen failure or withdrawal.
d. Imaging and Artificial Intelligence
Each participating site will receive certification by performing a test magnetic resonance imaging (MRI). Transfer of completed scans to the imaging repository, file naming, and deidentification will be monitored. The Core Image Analysis Lab will provide administrative coordination for the retrieval, processing, testing and temporary storage of the research MR images from the clinical centers and transfer of research MRI images to the AI Core lab. Core Lab will coordinate the uploading of all data and images to the T1DAPC permanent repository.
DISCUSSION
The DREAM study is the largest prospective study in AP in the US for which the T1DAPC has developed a comprehensive plan for recruitment, retention, and monitoring. From a scientific standpoint, the study will provide novel information on the risk and pathophysiology of diabetes, immune alterations, and additional epidemiologic relationships in AP. The experience gained during the planning and conduct of the study may be beneficial for designing future studies in this patient population. Feasibility and strategies for successful recruitment and retention will be critical to understand for future studies, especially those involving intervention.
For AP, enrolling participants early in the disease course (within hours of pain onset) has been recognized to be of importance for intervention studies and those aiming to understand the markers of disease severity. An enrollment window of up to 90 days after diagnosis of AP in DREAM provides an opportunity for the study teams to approach potential participants for participation during hospitalization as well as following hospital or emergency room discharge. Longitudinal follow-up will provide information on subject burden, compliance with study procedures and study withdrawal. Taken together, successful development and launch of the DREAM study lays the foundation for future multicenter studies in AP.
Supplementary Material
Acknowledgments
Grant Support: Research reported in this publication was supported by funding from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) for the Type 1 Diabetes in Acute Pancreatitis Consortium (T1DAPC) under award numbers U01 DK127367 (MDB), U01 DK127377 (DY), U01 DK127378 (CY), U01 DK127382 (JJE, ZIS, EF), U01 DK127384 (AMD, NTR-K), U01 DK127388 (DLC, PAH, GIP), U01 DK127392 (AC), U01 DK127395 (MB), U01 DK127400 (EA), and U01 DK127403 (CYJ) and U01 DK127404 (CG). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- AP
Acute Pancreatitis
- RRC
Recruitment and Retention Committee
- T1DAPC
Type 1 Diabetes in Acute Pancreatitis Consortium
- DREAM
Diabetes RElated to Acute pancreatitis and its Mechanisms
- DM
Diabetes Mellitus
- NIDDK
National Institute of Diabetes and Digestive and Kidney Diseases
- DCC
Data Coordinating Center
- RIC
Recruitment Innovation Center
- EHR
Electronic Health Records
- QR
Quick Response
- CRC
Clinical Research Coordinator
- AA
African American
- IRB
Institutional Review Board
- MRI
Magnetic Resonance Imaging
Footnotes
Conflicts of interest/disclosures:
The following authors disclose potential conflicts of interest: Afghani (advisory board for Nestle), Bellin (research support from Viacyte and Dexcom; advisory board for Insulet), Casu (advisory board for GSK, expert opinion for Guidepoint), Lee (advisory board for Abbvie), Papachristou (research support from Abbvie; consulting activities with Olympus and Nestle; equity with Ariel Precision Medicine). The remaining authors do not have any potential conflicts to disclose.
Contributor Information
Cemal Yazici, Division of Gastroenterology and Hepatology, University of Illinois at Chicago, Chicago, IL.
Anne-Marie Dyer, Department of Public Health Sciences, Penn State College of Medicine, Hershey, PA.
Darwin L. Conwell, Division of Gastroenterology, Hepatology, and Nutrition, The Ohio State University Wexner Medical Center, Columbus, OH.
Elham Afghani, Division of Gastroenterology and Hepatology, Johns Hopkins Hospital, Baltimore, MD.
Dana K. Andersen, Division of Digestive Diseases and Nutrition, National Institutes of Diabetes and Digestive and Kidney Diseases, National Institute of Health, Bethesda, MD.
Marina Basina, Division of Endocrinology, Gerontology, and Metabolism, Stanford University School of Medicine, Palo Alto, CA.
Melena D. Bellin, Departments of Pediatrics and Surgery, University of Minnesota Medical School, Minneapolis, MN.
Leslie R. Boone, Recruitment Innovation Center, Vanderbilt Institute for Clinical and Translational Research, Nashville, TN.
Anna Casu, Translational Research Institute, AdventHealth, Orlando, FL.
Jeffrey J. Easler, Division of Gastroenterology and Hepatology, Indiana University School of Medicine, Indianapolis, IN.
Carla J. Greenbaum, Center for Interventional Immunology, Benaroya Research Institute at Virginia Mason, Seattle, WA.
Phil A. Hart, Division of Gastroenterology, Hepatology, and Nutrition, The Ohio State University Wexner Medical Center, Columbus, OH.
Christie Y. Jeon, Department of Medicine, Cedars-Sinai Medical Center, Los Angeles, CA; Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, CA.
Peter J. Lee, Division of Gastroenterology, Hepatology, and Nutrition, The Ohio State University Wexner Medical Center, Columbus, OH.
Shelby Meier, Recruitment Innovation Center, Vanderbilt Institute for Clinical and Translational Research, Nashville, TN.
Georgios I. Papachristou, Division of Gastroenterology, Hepatology, and Nutrition, The Ohio State University Wexner Medical Center, Columbus, OH.
Nazia T. Raja-Khan, Division of Endocrinology, Diabetes and Metabolism, Penn State University College of Medicine, Hershey, PA.
Zeb I. Saeed, Division of Endocrinology, Indiana University School of Medicine, Indianapolis, IN.
Jose Serrano, Division of Digestive Diseases and Nutrition, National Institutes of Diabetes and Digestive and Kidney Diseases, National Institute of Health, Bethesda, MD.
Dhiraj Yadav, Division of Gastroenterology, Hepatology, and Nutrition, University of Pittsburgh School of Medicine, Pittsburgh, PA.
Evan L. Fogel, Division of Gastroenterology and Hepatology, Indiana University School of Medicine, Indianapolis, IN.
REFERENCES
- 1.Krishna SG, Kamboj AK, Hart PA, et al. The changing epidemiology of acute pancreatitis hospitalizations: a decade of trends and the impact of chronic pancreatitis. Pancreas. 2017;46:482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Das SL, Singh PP, Phillips AR, et al. Newly diagnosed diabetes mellitus after acute pancreatitis: a systematic review and meta-analysis. Gut. 2014;63:818–831. [DOI] [PubMed] [Google Scholar]
- 3.Shen HN, Yang CC, Chang YH, et al. Risk of diabetes mellitus after first-attack acute pancreatitis: A national population-based study. Am J Gastroenterol. 2015;110:1698–1706. [DOI] [PubMed] [Google Scholar]
- 4.Zhi M, Zhu X, Lugea A, et al. Incidence of new onset diabetes mellitus secondary to acute pancreatitis: A systematic review and meta-analysis. Front Physiol. 2019;10:637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlisle B, Kimmelman J, Ramsay T, et al. Unsuccessful trial accrual and human subjects protections: an empirical analysis of recently closed trials. Clin Trials. 2015;12:77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nipp RD, Hong K, Paskett ED. Overcoming barriers to clinical trial enrollment. Am Soc Clin Oncol Educ Book. 2019;39:105–114. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez-Torres E, Gonzalez-Perez MM, Diaz-Perez C. Barriers and facilitators to the participation of subjects in clinical trials: An overview of reviews. Contemp Clin Trials Commun. 2021;23:100829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Afghani E, Pandol SJ, Shimosegawa T, et al. Acute pancreatitis-progress and challenges: A report on an international symposium. Pancreas. 2015;44:1195–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uc A, Andersen DK, Borowitz D, et al. Accelerating the drug delivery pipeline for acute and chronic pancreatitis-knowledge gaps and research opportunities: Overview summary of a National Institute of Diabetes and Digestive and Kidney Diseases workshop. Pancreas. 2018;47:1180–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elmunzer BJ, Serrano J, Chak A, et al. Rectal indomethacin alone versus indomethacin and prophylactic pancreatic stent placement for preventing pancreatitis after ERCP: study protocol for a randomized controlled trial. Trials. 2016;17:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coté GA, Durkalski-Mauldin VL, Serrano J, et al. SpHincterotomy for Acute Recurrent Pancreatitis randomized trial: Rationale, methodology, and potential implications. Pancreas. 2019;48:1061–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yadav D, Park WG, Fogel EL, et al. PROspective evaluation of Chronic pancreatitis for EpidEmiologic and translational stuDies: Rationale and study design for PROCEED from the Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer. Pancreas. 2018;47:1229–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paragomi P, Phillips AE, Machicado JD, et al. Post-acute pancreatitis pancreatic exocrine insufficiency: Rationale and methodology of a prospective, observational, multicenter cohort study. Pancreas. 2021;50:147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marta K, Szabo AN, Pecsi D, et al. High versus low energy administration in the early phase of acute pancreatitis (GOULASH trial): protocol of a multicentre randomised double-blind clinical trial. BMJ Open. 2017;7:e015874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bharmal SH, Cho J, Alarcon Ramos GC, et al. Trajectories of glycaemia following acute pancreatitis: a prospective longitudinal cohort study with 24 months follow-up. J Gastroenterol. 2020;55:775–788. [DOI] [PubMed] [Google Scholar]
- 16.Wilkins CH, Edwards TL, Stroud M, et al. The Recruitment Innovation Center: Developing novel, person-centered strategies for clinical trial recruitment and retention. J Clin Transl Sci. 2021;5:e194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah MR, Culp MA, Gersing KR, et al. Early vision for the CTSA Program Trial Innovation Network: A perspective from the National Center for Advancing Translational Sciences. Clin Transl Sci. 2017;10:311–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cervantes A, Waymouth EK, Petrov MS. African-Americans and indigenous peoples have increased burden of diseases of the exocrine pancreas: a systematic review and meta-Analysis. Dig Dis Sci. 2019;64:249–261. [DOI] [PubMed] [Google Scholar]
- 19.Frey CF, Zhou H, Harvey DJ, et al. The incidence and case-fatality rates of acute biliary, alcoholic, and idiopathic pancreatitis in California, 1994–2001. Pancreas. 2006;33:336–344. [DOI] [PubMed] [Google Scholar]
- 20.Wu BU, Banks PA, Conwell DL. Disparities in emergency department wait times for acute gastrointestinal illnesses: results from the National Hospital Ambulatory Medical Care Survey, 1997–2006. Am J Gastroenterol. 2009;104:1668–1673. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


