Abstract
Introduction
Mortality disparities by SES, including education, have steadily increased in the U.S. over the past decades. This study examined whether these disparities overall and for 7 major causes of death were exacerbated in 2020, coincident with the emergence of the COVID-19 pandemic.
Methods
Using data on 7,123,254 U.S. deaths from 2017 to 2020, age-standardized death rates and mortality rate differences per 100,000 population and rate ratios comparing least with most educated were calculated by sex and race/ethnicity.
Results
All-cause death rates were approximately 2 times higher among adults with least than among those with most education. Disparities in all-cause mortality by educational attainment slightly increased from 2017 (rate ratio=1.97; 95% CI=1.95, 1.98; rate difference=739.9) to 2019 (rate ratio=2.04; 95% CI=2.03, 2.06; rate difference=761.3) and then greatly increased in 2020 overall (rate ratio=2.32; 95% CI=2.30, 2.33; rate difference=1,042.9) and when excluding COVID-19 deaths (rate ratio=2.27; 95% CI=2.25, 2.28; rate difference=912.3). Similar patterns occurred across race/ethnicity and sex, although Hispanic individuals had the greatest relative increase in disparities for all-cause mortality from 2019 (rate ratio=1.47; 95% CI=1.43, 1.51; rate difference=282.4) to 2020 overall (rate ratio=2.00; 95% CI=1.94, 2.06; rate difference=652.3) and when excluding COVID-19 deaths (rate ratio=1.84; 95% CI=1.79, 1.90; rate difference=458.7). Disparities in cause-specific mortality by education were generally stable from 2017 to 2019, followed by a considerable increase from 2019 to 2020 for heart disease, cancer, cerebrovascular disease, and unintentional injury. Among these causes of death, the relative increase in rate ratio from 2019 to 2020 was greatest for unintentional injury (24.8%; from 3.41 [95% CI=3.23, 3.60] to 4.26 [95% CI=3.99, 4.53]).
Conclusions
Mortality disparities by education widened in the U.S. in 2020, during the COVID-19 pandemic. Further research is warranted to understand the reasons for these widened disparities.
INTRODUCTION
Previous studies have reported steadily increasing SES mortality disparities in the U.S. over the past few decades.1, 2, 3 The emergence of the coronavirus disease 2019 (COVID-19) pandemic heightened the awareness of widening health disparities.4 , 5 The pandemic created an immense disturbance to the U.S. health system, including impacts on delivery of care and outcomes for other conditions. A study comparing provisional data from March through August 2020 with data from the same months in 2019 found disproportionately larger increases in cardiovascular disease deaths among Black, Hispanic, and Asian populations than among the White population.6 However, there are conflicting reports regarding whether overall mortality disparities by SES widened in 2020.7 , 8 This study examined whether trends in mortality disparities by educational attainment, a proxy for SES, overall and for 7 major causes of death in the U.S. were exacerbated during the COVID-19 pandemic in 2020.
METHODS
U.S. population9 and mortality10 data in 2017–2020 by age group (25–39, 40–54, 55–64, 65–74, and ≥75 years), sex, race/ethnicity (non-Hispanic White [White], non-Hispanic Black [Black], non-Hispanic Asian [Asian], or Hispanic), and educational attainment were obtained from the National Center for Health Statistics. Analyses were restricted to adults aged ≥25 years to allow adequate time for complete educational attainment, categorized as high school graduate or less (least educated), some college, and college graduate or more (most educated). The leading causes of death examined were heart disease, cancer, cerebrovascular disease, unintentional injury, chronic lower respiratory disease, diabetes, and Alzheimer disease. Death rates (age-standardized to the 2000 U.S. standard population, using the age groups 25–39, 40–54, 55–64, 65–74, and ≥75 years) by educational attainment and mortality rate differences (RDs) and rate ratios comparing least with most educated were calculated by sex and race/ethnicity. This study was exempt from IRB approval because data were deidentified and publicly available.
RESULTS
After excluding deaths with missing age (n=1,188; 0.02%) or educational attainment (n=224,043; 3.1%), this analysis included 7,123,254 deaths at age ≥25 years from 2017 to 2020. All-cause death rates were approximately 2 times higher among adults with the least education than among adults with the most education, with a slight annual increase in disparity during 2017–2019 that was accentuated in 2020 (Table 1 ). The rate ratio slightly increased from 1.97 (95% CI=1.95, 1.98; RD=739.9) in 2017 to 2.04 (95% CI=2.03, 2.06; RD=761.3) in 2019 and then increased to 2.32 (95% CI=2.30, 2.33; RD=1,042.9) in 2020 overall and to 2.27 (95% CI=2.25, 2.28; RD=912.3) when excluding COVID-19 deaths. Similar patterns occurred across race/ethnicity and sex (Table 1). Hispanic individuals had the greatest relative increase in disparities for all-cause mortality from 2019 (rate ratio=1.47; 95% CI=1.43, 1.51; RD=282.4) to 2020 overall (rate ratio=2.00; 95% CI=1.94, 2.06; RD=652.3) or when excluding COVID-19 deaths (rate ratio=1.84; 95% CI=1.79, 1.90; RD=458.7).
Table 1.
All-Cause and COVID-19 Death Rates and Rate Ratios by Sex, Race/Ethnicity, and Education, 2017–2020
| Sex and race/ethnicity | ≤High school graduate/GED | Some college | ≥College graduate | ≤High school graduate/GED versus ≥college graduate |
|
|---|---|---|---|---|---|
| n (rate) | n (rate) | n (rate) | Rate difference | Rate ratio (95% CI) | |
| Sexes combined | |||||
| Alla | |||||
| 2017 | 1,692,867 (1,506.1) | 510,992 (856.4) | 462,094 (766.2) | 739.9 | 1.97 (1.95, 1.98) |
| 2018 | 1,707,786 (1,508.6) | 523,044 (844.4) | 478,299 (746.8) | 761.8 | 2.02 (2.01, 2.03) |
| 2019 | 1,701,482 (1,491.2) | 533,349 (836.6) | 490,282 (729.9) | 761.3 | 2.04 (2.03, 2.06) |
| 2020 | |||||
| Overall | 2,021,119 (1,835.5) | 624,100 (939.3) | 582,064 (792.6) | 1,042.9 | 2.32 (2.30, 2.33) |
| Excluding COVID-19 | 1,790,813 (1,631.9) | 567,365 (854.3) | 528,711 (719.6) | 912.3 | 2.27 (2.25, 2.28) |
| COVID-19 | 230,306 (203.6) | 56,735 (85.1) | 53,353 (73) | 130.6 | 2.79 (2.71, 2.86) |
| NH-White | |||||
| 2017 | 1,288,191 (1,696) | 413,104 (884.4) | 391,024 (787.3) | 908.7 | 2.15 (2.14, 2.17) |
| 2018 | 1,293,588 (1,705.1) | 419,601 (869.1) | 403,405 (768.5) | 936.6 | 2.22 (2.20, 2.24) |
| 2019 | 1,280,491 (1,685.6) | 426,300 (863.2) | 412,286 (751.5) | 934.1 | 2.24 (2.22, 2.26) |
| 2020 | |||||
| Overall | 1,448,534 (2,019) | 483,709 (963.7) | 478,467 (811) | 1,208.0 | 2.49 (2.47, 2.51) |
| Excluding COVID-19 | 1,318,322 (1,855.5) | 447,014 (892) | 439,960 (745.3) | 1,110.2 | 2.49 (2.47, 2.51) |
| COVID-19 | 130,212 (163.5) | 36,695 (71.68) | 38,507 (65.7) | 97.8 | 2.49 (2.42, 2.56) |
| NH-Black | |||||
| 2017 | 213,081 (1,668.4) | 59,733 (989.3) | 33,725 (893.6) | 774.8 | 1.87 (1.82, 1.91) |
| 2018 | 217,298 (1,675.5) | 62,484 (977.3) | 35,384 (881.7) | 793.8 | 1.90 (1.86, 1.94) |
| 2019 | 219,646 (1,665.5) | 64,147 (951.9) | 36,434 (860.6) | 804.9 | 1.94 (1.89, 1.98) |
| 2020 | |||||
| Overall | 284,538 (2,280.6) | 82,937 (1,204.8) | 48,371 (1,051.3) | 1,229.3 | 2.17 (2.12, 2.22) |
| Excluding COVID-19 | 246,349 (1,979.3) | 72,634 (1,052.6) | 42,288 (920.8) | 1,058.5 | 2.15 (2.10, 2.20) |
| COVID-19 | 38,189 (301.4) | 10,303 (152.2) | 6,083 (130.5) | 170.9 | 2.31 (2.16, 2.47) |
| NH-Asian | |||||
| 2017 | 37,768 (769.9) | 10,332 (548.9) | 20,525 (538.1) | 231.8 | 1.43 (1.40, 1.47) |
| 2018 | 38,415 (776.9) | 11,054 (575.9) | 21,939 (531.4) | 245.5 | 1.46 (1.43, 1.50) |
| 2019 | 39,348 (777.7) | 11,415 (587.1) | 22,825 (498) | 279.7 | 1.56 (1.52, 1.60) |
| 2020 | |||||
| Overall | 50,404 (1,034.9) | 14,303 (704.9) | 29,809 (631.5) | 403.4 | 1.64 (1.60, 1.68) |
| Excluding COVID-19 | 43,376 (893.5) | 12,454 (616.6) | 25,617 (543.8) | 349.7 | 1.64 (1.60, 1.69) |
| COVID-19 | 7,028 (141.4) | 1,849 (88.22) | 4,192 (87.7) | 53.7 | 1.61 (1.51, 1.72) |
| Hispanic | |||||
| 2017 | 139,159 (883.3) | 23,164 (585) | 14,689 (606.3) | 277 | 1.46 (1.42, 1.50) |
| 2018 | 144,204 (889.6) | 25,045 (587.1) | 15,560 (578) | 311.6 | 1.54 (1.50, 1.58) |
| 2019 | 148,213 (885.8) | 26,648 (586.3) | 16,730 (603.4) | 282.4 | 1.47 (1.43, 1.51) |
| 2020 | |||||
| Overall | 219,211 (1,307) | 36,517 (703.1) | 22,798 (654.7) | 652.3 | 2.00 (1.94, 2.06) |
| Excluding COVID-19 | 167,433 (1,002.4) | 29,812 (579.4) | 18,670 (543.7) | 458.7 | 1.84 (1.79, 1.90) |
| COVID-19 | 51,778 (304.5) | 6,705 (123.7) | 4,128 (111) | 193.5 | 2.74 (2.50, 3.02) |
| Male | |||||
| Alla | |||||
| 2017 | 818,299 (1,756.8) | 256,346 (978.8) | 270,495 (858.3) | 898.5 | 2.05 (2.03, 2.07) |
| 2018 | 831,296 (1,763.3) | 263,187 (966.1) | 279,242 (839.8) | 923.5 | 2.10 (2.08, 2.12) |
| 2019 | 834,516 (1,743.5) | 269,011 (961.6) | 285,671 (824.5) | 919 | 2.11 (2.10, 2.13) |
| 2020 | |||||
| Overall | 1,009,949 (2,144.1) | 317,514 (1,094.9) | 339,132 (902.8) | 1,241.3 | 2.37 (2.35, 2.40) |
| Excluding COVID-19 | 888,547 (1,888.1) | 286,984 (989.1) | 305,258 (812.9) | 1,075.3 | 2.32 (2.30, 2.35) |
| COVID-19 | 121,402 (255.9) | 30,530 (105.8) | 33,874 (89.9) | 166 | 2.85 (2.75, 2.95) |
| NH-White | |||||
| 2017 | 607,569 (1,954.20) | 207,923 (1,012.80) | 233,084 (880.6) | 1,070.70 | 2.22 (2.21, 2.22) |
| 2018 | 614,428 (1,964.60) | 205,829 (980.8) | 239,757 (863.8) | 1,097.80 | 2.27 (2.27,2.28) |
| 2019 | 613,104 (1,941.00) | 215,741 (992.5) | 244,810 (849.8) | 1,088.30 | 2.28 (2.28, 2.29) |
| 2020 | |||||
| Overall | 700,575 (2,311.40) | 246,023 (1,121.90) | 283,963 (920.9) | 1,390.50 | 2.51 (2.48, 2.54) |
| Excluding COVID-19 | 637,148 (2,114.40) | 226,459 (1,033.00) | 259,218 (841.2) | 1,273.20 | 2.51 (2.48, 2.54) |
| COVID-19 | 63,427 (197.1) | 19,564 (88.9) | 24,745 (79.8) | 117.3 | 2.47 (2.38, 2.56) |
| NH-Black | |||||
| 2017 | 112,372 (1,987.80) | 27,557 (1,103.70) | 15,055 (993.6) | 987.3 | 1.99 (1.98, 2.00) |
| 2018 | 115,378 (2,030.60) | 28,773 (1,062.30) | 15,851 (978.5) | 1,045.30 | 2.07 (2.06, 2.08) |
| 2019 | 116,855 (1,995.70) | 29,937 (1,062.20) | 16,440 (973) | 1,015.80 | 2.04 (2.03, 2.05) |
| 2020 | |||||
| Overall | 153,479 (2,686.50) | 39,100 (1,400.30) | 21,907 (1,232.30) | 1,454.30 | 2.18 (2.11, 2.25) |
| Excluding COVID-19 | 132,914 (2,316.90) | 34,147 (1,215.20) | 18,755 (1,057.20) | 1,259.80 | 2.19 (2.11, 2.27) |
| COVID-19 | 20,565 (369.6) | 4,953 (184.1) | 3,152 (175.1) | 194.5 | 2.11 (1.94, 2.30) |
| NH-Asian | |||||
| 2017 | 16,345 (940.4) | 5,787 (674.2) | 12,864 (649.2) | 282.8 | 1.44 (1.43, 1.44) |
| 2018 | 16,662 (946.2) | 6,156 (722.5) | 13,779 (640.9) | 296.9 | 1.46 (1.46, 1.47) |
| 2019 | 17,176 (946.2) | 6,282 (722.4) | 14,117 (592.8) | 345 | 1.58 (1.57, 1.59) |
| 2020 | |||||
| Overall | 22,658 (1,281.80) | 8,277 (898.4) | 18,671 (780.4) | 501.4 | 1.64 (1.59, 1.70) |
| Excluding COVID-19 | 19,064 (1,084.10) | 7,031 (768.1) | 15,742 (660.8) | 423.3 | 1.64 (1.58, 1.70) |
| COVID-19 | 3,594 (197.6) | 1,246 (130.3) | 2,929 (119.6) | 78.1 | 1.65 (1.52, 1.79) |
| Hispanic | |||||
| 2017 | 74,047 (1,053.40) | 12,651 (692.4) | 8,328 (693.2) | 355.7 | 1.51 (1.50, 1.52) |
| 2018 | 76,906 (1,052.80) | 13,856 (724.5) | 8,803 (664.2) | 384.1 | 1.58 (1.57, 1.59) |
| 2019 | 79,743 (1,062.10) | 14,569 (707.8) | 9,246 (672.8) | 384.7 | 1.57 (1.56, 1.58) |
| 2020 | |||||
| Overall | 122,946 (1,602.10) | 20,611 (838.3) | 13,236 (733.9) | 868.2 | 2.18 (2.09, 2.28) |
| Excluding COVID-19 | 90,861 (1,185.00) | 16,448 (674.1) | 10,422 (588.7) | 596.3 | 2.01 (1.93, 2.10) |
| COVID-19 | 32,085 (417.1) | 4,163 (164.2) | 2,814 (145.2) | 271.9 | 2.87 (2.55, 3.24) |
| Female | |||||
| Alla | |||||
| 2017 | 874,568 (1,294.60) | 254,646 (759.6) | 191,599 (667.6) | 627 | 1.94 (1.92, 1.96) |
| 2018 | 876,490 (1,291.50) | 259,857 (747.6) | 199,057 (648.5) | 643 | 1.99 (1.97, 2.01) |
| 2019 | 866,928 (1,273.00) | 264,336 (737.5) | 204,610 (631.1) | 641.9 | 2.02 (2.00, 2.04) |
| 2020 | |||||
| Overall | 1,011,170 (1,557.60) | 306,586 (816.6) | 242,932 (680.2) | 877.4 | 2.29 (2.27, 2.31) |
| Excluding COVID-19 | 902,266 (1,395.30) | 280,381 (747.3) | 223,453 (624.7) | 770.69 | 2.23 (2.21, 2.26) |
| COVID-19 | 108,904 (162.2) | 26,205 (69.3) | 19,479 (55.6) | 106.7 | 2.92 (2.79, 3.05) |
| NH-White | |||||
| 2017 | 680,608 (1,474.20) | 205,179 (780.7) | 157,937 (684.2) | 790 | 2.15 (2.15, 2.16) |
| 2018 | 679,138 (1,478.50) | 207,770 (766) | 163,647 (664.5) | 814 | 2.22 (2.22, 2.23) |
| 2019 | 667,366 (1,459.00) | 210,558 (758.1) | 167,475 (645.7) | 813.3 | 2.26 (2.25, 2.27) |
| 2020 | |||||
| Overall | 747,949 (1,749.50) | 237,686 (836.2) | 194,504 (694.4) | 1,055.2 | 2.52 (2.49, 2.55) |
| Excluding COVID-19 | 681,164 (1,610.60) | 220,555 (777.4) | 180,742 (644) | 966.5 | 2.5 (2.47, 2.54) |
| COVID-19 | 66,785 (139) | 17,131 (58.7) | 13,762 (50.3) | 88.6 | 2.76 (2.62, 2.91) |
| NH-Black | |||||
| 2017 | 100,704 (1,394.20) | 32,176 (910.4) | 18,669 (828.1) | 566.1 | 1.68 (1.68, 1.69) |
| 2018 | 101,975 (1,380.60) | 33,710 (914) | 19,533 (817.7) | 562.8 | 1.69 (1.68, 1.70) |
| 2019 | 102,779 (1,379.30) | 34,210 (873.1) | 19,994 (787.6) | 591.7 | 1.75 (1.74, 1.76) |
| 2020 | |||||
| Overall | 131,059 (1,904.20) | 43,837 (1,072.7) | 26,464 (940.7) | 963.5 | 2.02 (1.97, 2.08) |
| Excluding COVID-19 | 113,435 (1,655.50) | 38,487 (941) | 23,533 (837.3) | 818.2 | 1.98 (1.92, 2.04) |
| COVID-19 | 17,624 (248.6) | 5,350 (131.7) | 2,931 (103.4) | 145.2 | 2.40 (2.18, 2.65) |
| NH-Asian | |||||
| 2017 | 21,423 (659.3) | 4,545 (447.2) | 7,661 (415) | 244.4 | 1.59 (1.57, 1.60) |
| 2018 | 21,753 (664.6) | 4,898 (463) | 8,160 (411) | 253.7 | 1.62 (1.60, 1.63) |
| 2019 | 22,172 (662.1) | 5,132 (481.2) | 8,708 (396.5) | 265.6 | 1.67 (1.65, 1.69) |
| 2020 | |||||
| Overall | 27,746 (865.5) | 6,026 (549.6) | 11,138 (479.4) | 386.1 | 1.81 (1.73, 1.88) |
| Excluding COVID-19 | 24,312 (759.1) | 5,423 (495) | 9,875 (423.6) | 335.5 | 1.79 (1.72, 1.87) |
| COVID-19 | 3,434 (106.5) | 603 (54.7) | 1,263 (55.8) | 50.6 | 1.91 (1.68, 2.17) |
| Hispanic | |||||
| 2017 | 65,110 (739.6) | 10,513 (499.3) | 6,361 (522) | 217.6 | 1.42 (1.41, 1.43) |
| 2018 | 67,293 (748) | 11,189 (483.2) | 6,757 (495.7) | 252.4 | 1.51 (1.50, 1.52) |
| 2019 | 68,466 (734.3) | 12,079 (492) | 7,484 (536) | 198.3 | 1.37 (1.36, 1.38) |
| 2020 | |||||
| Overall | 96,265 (1,046.40) | 15,906 (590.9) | 9,562 (580.5) | 465.9 | 1.80 (1.73, 1.88) |
| Excluding COVID-19 | 76,572 (834.5) | 13,364 (500.6) | 8,248 (502.5) | 332 | 1.66 (1.59, 1.73) |
| COVID-19 | 19,693 (211.9) | 2,542 (90.4) | 1,314 (78) | 133.9 | 2.72 (2.30, 3.21) |
The entire U.S. population, including racial/ethnic groups not listed in this table.
bRates are per 100,000 person-years and age standardized to the 2000 U.S. standard population.
NH, non-Hispanic.
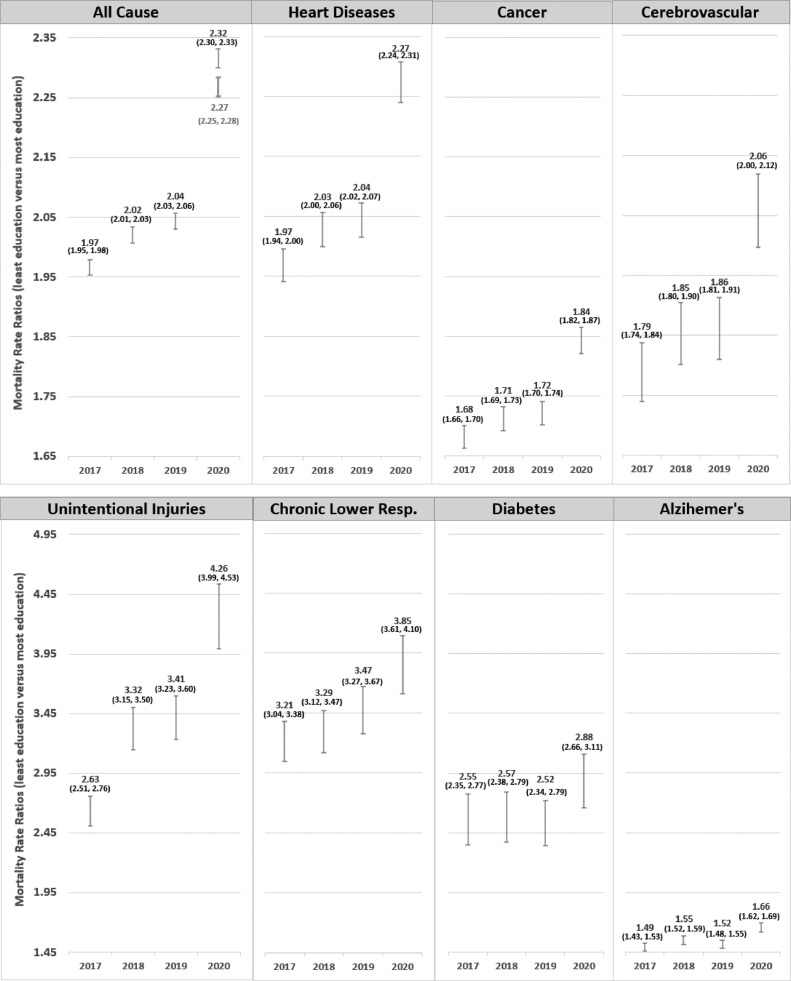
Disparities in cause-specific mortality by education were generally stable from 2017 to 2019, followed by considerable increases from 2019 to 2020 for heart disease, cancer, cerebrovascular disease, and unintentional injury (Figure 1 ). For example, the rate ratio for heart disease mortality slightly increased from 1.97 (95% CI=1.94, 2.00; RD=168.6) in 2017 to 2.04 (95% CI=2.02, 2.07; RD=172.8) in 2019, increasing to 2.27 (95% CI=2.24, 2.31; RD=205.5) in 2020. The increase in rate ratio for unintentional injury was greater, increasing from 2.63 (95% CI=2.51, 2.76; RD=42.21) in 2017 to 3.41 (95% CI=3.23, 3.60; RD=70.01) in 2019 and to 4.26 (95% CI=3.99, 4.53; RD=94.95) in 2020. The relative increase in rate ratio from 2019 to 2020 was greatest for unintentional injury (24.8%), followed by heart disease (11.4%), cerebrovascular disease (10.8%), and cancer (7.0%).
Figure 1.
All-cause and cause-specific mortality rate ratios by educational attainment for all races combined from 2017 to 2020, ages ≥25 years, U.S.
Note: The rate ratio shown in gray is for all-cause mortality in 2020, excluding COVID-19 deaths. ICD-10 codes examined: COVID-19 (U071), heart disease (I00-I09, I11, I13, I20-I51), cancer (C00-C97), cerebrovascular disease (I60-I69), unintentional injury (V01-X59, Y85-Y86), chronic lower Resp. disease (J40-J47).
Resp., respiratory.
Generally, similar patterns existed across racial/ethnic groups. However, there were few deaths for some causes among Black and Asian individuals, particularly among the higher-education group, which resulted in relatively wide CIs (Table 2 ). Changes in rate ratio from 2019 to 2020 were most notable among Hispanic individuals. For example, from 2019 to 2020, the rate ratio for heart disease mortality among Hispanic individuals increased by 27.8%, from 1.42 (95% CI=1.35, 1.50; RD=56.37) to 1.79 (95% CI=1.82, 1.94; RD=98.71), whereas it increased in Black individuals by 12.0%, from 1.94 (95% CI=1.85, 2.03; RD=190.62) to 2.17 (95% CI=2.07, 2.28; RD=254.36), and in White individuals by 10.8%, from 2.22 (95% CI=2.19, 2.26; RD=207.97) to 2.46 (95% CI=2.42, 2.51; RD=242.82). Similar patterns were observed among men and women (Appendix Table 1, available online).
Table 2.
Cause-Specific Death Rates and Rate Ratios by Race Ethnicity and Education, Sex Combined, U.S., 2017–2020
| Cause of death by race/ethnicity | ≤High school graduate/GED, | Some college, | ≥College graduate, | ≤High school graduate/GED versus ≥college graduate |
|
|---|---|---|---|---|---|
| n (rate) | n (rate) | n (rate) | Rate difference | Rate ratio (95% CI) | |
| Heart disease | |||||
| Alla | |||||
| 2017 | 395,916 (342.63) | 113,360 (193.04) | 102,430 (174.01) | 168.62 | 1.97 (1.94, 2.00) |
| 2018 | 399,776 (343.33) | 116,590 (190.78) | 106,222 (169.32) | 174.00 | 2.03 (2.00, 2.06) |
| 2019 | 397,955 (338.5) | 118,385 (187.62) | 109,279 (165.63) | 172.82 | 2.04 (2.02, 2.07) |
| 2020 | 416,747 (366.97) | 125,557 (189.59) | 117,054 (161.45) | 205.52 | 2.27 (2.24, 2.31) |
| NH-White | |||||
| 2017 | 304,015 (379.88) | 91,730 (196.86) | 86,919 (178.11) | 201.77 | 2.13 (2.10, 2.17) |
| 2018 | 305,815 (382.17) | 93,760 (194.28) | 89,656 (173.18) | 208.98 | 2.21 (2.17, 2.24) |
| 2019 | 303,389 (377.84) | 94,754 (191.13) | 92,215 (169.87) | 207.97 | 2.22 (2.19, 2.26) |
| 2020 | 308,819 (408.63) | 98,749 (194.47) | 97,319 (165.80) | 242.82 | 2.46 (2.42, 2.51) |
| NH-Black | |||||
| 2017 | 50,954 (396.42) | 13,985 (235.20) | 7,734 (207.97) | 188.45 | 1.91 (1.82, 2.00) |
| 2018 | 52,305 (400.77) | 14,741 (233.09) | 8,146 (206.90) | 193.88 | 1.94 (1.85, 2.03) |
| 2019 | 52,373 (394.09) | 15,066 (225.27) | 8,493 (203.47) | 190.62 | 1.94 (1.85, 2.03) |
| 2020 | 59,337 (471.83) | 17,430 (252.99) | 9,923 (217.48) | 254.36 | 2.17 (2.07, 2.28) |
| NH-Asian | |||||
| 2017 | 8,378 (167.40) | 2,176 (117.38) | 4,315 (119.16) | 48.24 | 1.40 (1.33, 1.48) |
| 2018 | 8,485 (168.04) | 2,350 (125.16) | 4,707 (118.57) | 49.47 | 1.42 (1.35, 1.49) |
| 2019 | 8,705 (168.34) | 2,453 (128.31) | 4,755 (107.63) | 60.71 | 1.56 (1.48, 1.66) |
| 2020 | 9,903 (199.91) | 2,713 (135.83) | 5,493 (120.40) | 79.50 | 1.66 (1.57, 1.76) |
| Hispanic | |||||
| 2017 | 29,637 (194.83) | 4,564 (127.53) | 2,980 (134.75) | 60.08 | 1.45 (1.36, 1.53) |
| 2018 | 30,306 (193.37) | 4,781 (122.42) | 3,256 (132.41) | 60.97 | 1.46 (1.38, 1.55) |
| 2019 | 30,865 (190.11) | 5,133 (123.49) | 3,387 (133.74) | 56.37 | 1.42 (1.35, 1.50) |
| 2020 | 35,762 (219.67) | 5,681 (121.06) | 3,874 (120.96) | 98.71 | 1.82 (1.70, 1.94) |
| Cancer | |||||
| Alla | |||||
| 2017 | 345,359 (305.57) | 122,397 (191.99) | 117,883 (181.7) | 123.86 | 1.68 (1.66, 1.70) |
| 2018 | 344,679 (302.34) | 123,451 (187.17) | 120,520 (176.58) | 125.76 | 1.71 (1.69, 1.73) |
| 2019 | 341,306 (295.78) | 125,514 (185.49) | 122,228 (171.81) | 123.97 | 1.72 (1.70, 1.74) |
| 2020 | 338,971 (302.14) | 125,582 (178.43) | 126,755 (163.95) | 138.19 | 1.84 (1.82, 1.87) |
| NH-White | |||||
| 2017 | 260,365 (342.06) | 98,184 (197.23) | 98,065 (185.04) | 158.01 | 1.85 (1.83, 1.88) |
| 2018 | 259,128 (341.42) | 98,665 (192.35) | 99,859 (180.08) | 161.33 | 1.90 (1.87, 1.92) |
| 2019 | 255,071 (333.55) | 99,811 (190.83) | 99,864 (173.02) | 160.53 | 1.93 (1.90, 1.96) |
| 2020 | 252,705 (347.55) | 99,658 (187.6) | 104,324 (169.6) | 177.95 | 2.05 (2.02, 2.08) |
| NH-Black | |||||
| 2017 | 44,767 (338.67) | 14,513 (225.4) | 8,905 (213.98) | 124.69 | 1.58 (1.52, 1.65) |
| 2018 | 44,613 (331.92) | 14,536 (213.94) | 9,167 (208.99) | 122.93 | 1.59 (1.53, 1.65) |
| 2019 | 44,895 (328.11) | 14,914 (208.72) | 9,426 (204.36) | 123.74 | 1.61 (1.55, 1.67) |
| 2020 | 44,328 (241.79) | 15,002 (206.39) | 9,936 (200.58) | 141.21 | 1.70 (1.64, 1.77) |
| NH-Asian | |||||
| 2017 | 8,678 (175.75) | 2,905 (142.45) | 6,212 (145.83) | 29.92 | 1.21 (1.16, 1.26) |
| 2018 | 8,639 (173.96) | 3,075 (146.87) | 6,540 (143.04) | 30.92 | 1.22 (1.17, 1.27) |
| 2019 | 8,931 (175.34) | 3,117 (147.45) | 6,697 (134.38) | 40.96 | 1.3 (1.25, 1.36) |
| 2020 | 9,113 (184.5) | 3,138 (144.83) | 7,130 (138.69) | 45.81 | 1.33 (1.27, 1.39) |
| Hispanic | |||||
| 2017 | 28,937 (180.23) | 5,866 (136.44) | 4,185 (149.98) | 30.26 | 1.2 (1.15, 1.25) |
| 2018 | 29,797 (179.46) | 6,238 (134.85) | 4,435 (144.33) | 35.13 | 1.24 (1.19, 1.30) |
| 2019 | 30,005 (175.23) | 6,713 (138.28) | 4,709 (148.84) | 26.39 | 1.18 (1.13, 1.23) |
| 2020 | 30,415 (178.76) | 6,852 (124.57) | 4,863 (125.38) | 53.38 | 1.43 (1.36, 1.49) |
| Cerebrovascular disease | |||||
| Alla | |||||
| 2017 | 79,766 (68.19) | 22,663 (40.07) | 21,809 (38.14) | 30.06 | 1.79 (1.74, 1.84) |
| 2018 | 79,746 (67.59) | 23,088 (39.04) | 22,312 (36.5) | 31.1 | 1.85 (1.80, 1.90) |
| 2019 | 79,101 (66.48) | 23,594 (38.42) | 23,022 (35.72) | 30.76 | 1.86 (1.81, 1.91) |
| 2020 | 82,993 (72.15) | 25,025 (38.78) | 24,895 (35.07) | 37.08 | 2.06 (2.00, 2.12) |
| NH-White | |||||
| 2017 | 58,022 (69.94) | 17,770 (39.21) | 17,948 (37.73) | 32.22 | 1.85 (1.80, 1.91) |
| 2018 | 57,638 (69.48) | 17,985 (38.03) | 18,344 (36.16) | 33.32 | 1.92 (1.86, 1.99) |
| 2019 | 56,621 (68.16) | 18,273 (37.42) | 18,618 (34.94) | 33.22 | 1.95 (1.89, 2.02) |
| 2020 | 58,031 (73.69) | 19,173 (38.29) | 20,079 (34.7) | 38.99 | 2.12 (2.05, 2.20) |
| NH-Black | |||||
| 2017 | 11,406 (89.14) | 2,994 (54.28) | 1,769 (51.76) | 37.38 | 1.72 (1.57, 1.89) |
| 2018 | 11,551 (88.71) | 3,085 (53.01) | 1,790 (48.97) | 39.74 | 1.81 (1.65, 1.99) |
| 2019 | 11,573 (87.25) | 3,233 (52.67) | 1,986 (52.04) | 35.21 | 1.68 (1.54, 1.82) |
| 2020 | 12,774 (101.79) | 3,623 (56.91) | 2,171 (51.13) | 50.66 | 1.99 (1.81, 2.19) |
| NH-Asian | |||||
| 2017 | 2,626 (52.9) | 670 (36.83) | 1,242 (34.46) | 18.43 | 1.53 (1.38, 1.71) |
| 2018 | 2,613 (51.9) | 689 (37.31) | 1,297 (33.28) | 18.62 | 1.56 (1.40, 1.74) |
| 2019 | 2,606 (50.14) | 747 (40.01) | 1,412 (32.34) | 17.81 | 1.55 (1.40, 1.72) |
| 2020 | 2,923 (59.28) | 745 (37.66) | 1,589 (35.14) | 24.14 | 1.69 (1.52, 1.88) |
| Hispanic | |||||
| 2017 | 7,180 (47.36) | 1,083 (32.13) | 787 (36.67) | 10.69 | 1.29 (1.17, 1.43) |
| 2018 | 7,488 (48.25) | 1,178 (32.4) | 810 (34.88) | 13.37 | 1.38 (1.24, 1.54) |
| 2019 | 7,814 (48.72) | 1,189 (29.54) | 941 (39.64) | 9.08 | 1.23 (1.13, 1.34) |
| 2020 | 8,733 (54.18) | 1,321 (30.76) | 977 (33.2) | 20.98 | 1.63 (1.46, 1.83) |
| Unintentional injury | |||||
| Alla | |||||
| 2017 | 61,849 (68.11) | 21,723 (36.08) | 16,237 (25.9) | 42.21 | 2.63 (1.51, 2.76) |
| 2018 | 84,692 (95.08) | 27,031 (43.92) | 19,006 (28.64) | 66.44 | 3.32 (3.15, 3.50) |
| 2019 | 88,264 (99.07) | 28,194 (45.52) | 20,017 (29.05) | 70.01 | 3.41 (3.23, 3.60) |
| 2020 | 103,295 (124.12) | 32,511 (52.01) | 21,746 (29.17) | 94.95 | 4.26 (3.99, 4.53) |
| NH-White | |||||
| 2017 | 61,853 (123.95) | 21,724 (51.68) | 16,237 (32.73) | 91.22 | 3.79 (3.54, 4.05) |
| 2018 | 61,833 (124.96) | 21,356 (50.11) | 16,278 (31.4) | 93.56 | 3.98 (3.71, 4.27) |
| 2019 | 63,471 (128.47) | 21,981 (51.77) | 17,056 (31.86) | 96.61 | 4.03 (3.76, 4.33) |
| 2020 | 72,219 (164.47) | 24.678 (59.77) | 18,427 (32.55) | 131.92 | 5.05 (4.64, 5.50) |
| NH-Black | |||||
| 2017 | 10,299 (87.14) | 2,883 (36.45) | 1,023 (22.08) | 65.06 | 3.95 (3.00, 5.19) |
| 2018 | 10,889 (90.74) | 3,042 (38) | 1,053 (20.89) | 69.85 | 4.34 (3.24, 5.83) |
| 2019 | 11,965 (99.71) | 3,256 (39.69) | 1,180 (23.47) | 76.24 | 4.25 (3.24, 5.57) |
| 2020 | 15,749 (139.91) | 4,329 (53.82) | 1,405 (25.95) | 113.96 | 5.39 (3.96, 7.34) |
| NH-Asian | |||||
| 2017 | 1,341 (32.66) | 411 (19.59) | 776 (17.87) | 14.79 | 1.83 (1.54, 2.17) |
| 2018 | 1,449 (35.62) | 473 (22.48) | 832 (17.99) | 17.63 | 1.98 (1.65, 2.37) |
| 2019 | 1,435 (35.7) | 500 (23.34) | 888 (17.27) | 18.43 | 2.07 (1.72, 2.48) |
| 2020 | 1,587 (42.38) | 597 (27.62) | 893 (17.14) | 25.24 | 2.47 (1.99, 3.06) |
| Hispanic | |||||
| 2017 | 8,948 (47.5) | 1,634 (25.22) | 666 (19.26) | 28.24 | 2.47 (1.97, 3.09) |
| 2018 | 9,271 (48.43) | 1,760 (25.92) | 748 (19.45) | 28.98 | 2.49 (2.01, 3.08) |
| 2019 | 10,174 (52.46) | 2,047 (29.45) | 795 (19.64) | 32.82 | 2.67 (2.13, 3.35) |
| 2020 | 12,279 (64.49) | 2,373 (30.61) | 897 (18.51) | 45.98 | 3.48 (2.66, 4.57) |
| Chronic lower respiratory disease | |||||
| Alla | |||||
| 2017 | 111,208 (94.74) | 27,323 (46.2) | 17,100 (29.53) | 65.21 | 3.21 (3.04, 3.38) |
| 2018 | 110,557 (93.13) | 28,085 (45.29) | 17,434 (28.29) | 64.84 | 3.29 (3.12, 3.47) |
| 2019 | 108,637 (90.47) | 27,951 (43.57) | 17,041 (26.1) | 64.37 | 3.47 (3.27, 3.67) |
| 2020 | 104,802 (89.87) | 27,599 (40.87) | 16,776 (23.37) | 66.5 | 3.85 (3.61, 4.10) |
| NH-White | |||||
| 2017 | 96,659 (119.02) | 24,390 (50.94) | 15,357 (31.55) | 87.47 | 3.77 (3.53, 4.03) |
| 2018 | 95,599 (117.36) | 24,936 (49.95) | 15,686 (30.4) | 86.96 | 3.86 (3.61, 4.12) |
| 2019 | 94,103 (115.05) | 24,800 (48.25) | 15,306 (28.15) | 86.9 | 4.09 (3.81, 4.39) |
| 2020 | 89,504 (115.03) | 24,242 (45.96) | 14,874 (25.21) | 89.82 | 4.56 (4.21, 4.94) |
| NH-Black | |||||
| 2017 | 7,964 (61) | 1,846 (32.56) | 885 (25.98) | 35.02 | 2.35 (1.98, 2.79) |
| 2018 | 8,243 (61.87) | 2,055 (33.24) | 877 (23.65) | 38.22 | 2.62 (2.16, 3.17) |
| 2019 | 8,115 (59.52) | 2,003 (30.87) | 852 (21.08) | 38.44 | 2.82 (2.29, 3.49) |
| 2020 | 8,683 (67.36) | 2,198 (32.66) | 911 (21.14) | 46.23 | 3.19 (2.54, 4.00) |
| NH-Asian | |||||
| 2017 | 1,276 (24.98) | 304 (17.98) | 413 (12.36) | 12.62 | 2.02 (1.61, 2.54) |
| 2018 | 1,345 (25.88) | 263 (15.43) | 441 (12.17) | 13.71 | 2.13 (1.68, 2.69) |
| 2019 | 1,252 (23.34) | 291 (16.62) | 437 (10.63) | 12.7 | 2.19 (1.72, 2.80) |
| 2020 | 1,271 (24.97) | 309 (16.57) | 516 (12.29) | 12.68 | 2.03 (1.64, 2.51) |
| Hispanic | |||||
| 2017 | 4,437 (30.28) | 574 (18.58) | 364 (18.43) | 11.85 | 1.64 (1.37, 1.97) |
| 2018 | 4,591 (30.39) | 635 (18.42) | 364 (16.42) | 13.97 | 1.85 (1.51, 2.27) |
| 2019 | 4,437 (28.33) | 643 (17.67) | 380 (16.54) | 11.79 | 1.71 (1.42, 2.07) |
| 2020 | 4,641 (29.42) | 668 (15.67) | 407 (14.45) | 14.96 | 2.04 (1.64, 2.52) |
| Diabetes | |||||
| Alla | |||||
| 2017 | 20,981 (18.66) | 20,981 (35.4) | 4,634 (7.31) | 11.34 | 2.55 (2.35, 2.77) |
| 2018 | 22,033 (19.45) | 6,994 (10.74) | 5,049 (7.55) | 11.9 | 2.57 (2.38, 2.79) |
| 2019 | 23,088 (20.22) | 7,614 (11.41) | 5,620 (8.02) | 12.21 | 2.52 (2.34, 2.72) |
| 2020 | 27,855 (25.18) | 9,113 (13.13) | 6,678 (8.75) | 16.43 | 2.88 (2.66, 3.11) |
| NH-White | |||||
| 2017 | 13,375 (17.68) | 4,631 (9.5) | 3,485 (6.65) | 11.03 | 2.66 (2.40, 2.94) |
| 2018 | 14,047 (18.6) | 4,812 (9.54) | 3,745 (6.81) | 11.79 | 2.73 (2.47, 3.02) |
| 2019 | 14,517 (19.2) | 5,290 (10.23) | 4,168 (7.28) | 11.92 | 2.64 (2.40, 2.90) |
| 2020 | 16,807 (23.55) | 6,089 (11.65) | 4,784 (7.8) | 15.75 | 3.02 (2.73, 3.34) |
| NH-Black | |||||
| 2017 | 3,056 (23.76) | 1,025 (17) | 451 (11.64) | 12.12 | 2.04 (1.64, 2.53) |
| 2018 | 3,294 (25.22) | 1,129 (16.87) | 545 (13.55) | 11.67 | 1.86 (1.55, 2.23) |
| 2019 | 3,356 (25.25) | 1,193 (17.44) | 594 (13.73) | 11.52 | 1.84 (1.55, 2.18) |
| 2020 | 4,366 (34.43) | 1,569 (22.62) | 793 (16.89) | 17.54 | 2.04 (1.73, 2.40) |
| NH-Asian | |||||
| 2017 | 807 (16.1) | 274 (13.85) | 424 (11.42) | 4.68 | 1.41 (1.19, 1.67) |
| 2018 | 926 (18.21) | 273 (13.7) | 457 (11.54) | 6.66 | 1.58 (1.31, 1.89) |
| 2019 | 949 (18.19) | 326 (16.49) | 486 (10.88) | 7.21 | 1.67 (1.39, 2.02) |
| 2020 | 1,216 (24.34) | 379 (17.74) | 676 (14.7) | 9.64 | 1.66 (1.41, 1.94) |
| Hispanic | |||||
| 2017 | 3,358 (21.51) | 547 (13.57) | 237 (10.18) | 11.32 | 2.11 (1.56, 2.85) |
| 2018 | 3,461 (21.52) | 643 (14.31) | 252 (9.44) | 12.09 | 2.28 (1.66, 3.13) |
| 2019 | 3,907 (23.35) | 691 (15.14) | 326 (11.45) | 11.89 | 2.04 (1.58, 2.62) |
| 2020 | 5,032 (30.12) | 910 (17.6) | 381 (10.71) | 19.42 | 2.81 (2.05, 3.86) |
| Alzheimer disease | |||||
| Alla | |||||
| 2017 | 77,017 (62.26) | 20,239 (39.51) | 22,192 (41.66) | 20.61 | 1.49 (1.46, 1.53) |
| 2018 | 77,137 (61.7) | 20,483 (37.87) | 22,871 (39.8) | 21.9 | 1.55 (1.52, 1.59) |
| 2019 | 75,246 (59.53) | 20,845 (36.92) | 23,951 (39.22) | 20.31 | 1.52 (1.48, 1.55) |
| 2020 | 81,687 (66.71) | 23,522 (39.08) | 27,225 (40.27) | 26.44 | 1.66 (1.62, 1.69) |
| NH-White | |||||
| 2017 | 62,751 (69.16) | 17,812 (41.48) | 19,857 (43.85) | 25.31 | 1.58 (1.54, 1.62) |
| 2018 | 62,444 (68.47) | 17,801 (39.5) | 20,441 (42.02) | 26.45 | 1.63 (1.59, 1.67) |
| 2019 | 60,349 (65.97) | 18,037 (38.59) | 21,181 (41.13) | 24.83 | 1.60 (1.56, 1.64) |
| 2020 | 64,036 (73.55) | 20,226 (41.51) | 23,889 (42.46) | 31.09 | 1.73 (1.69, 1.78) |
| NH-Black | |||||
| 2017 | 6,370 (51.3) | 1,303 (34.86) | 1,101 (41.21) | 10.09 | 1.24 (1.15, 1.35) |
| 2018 | 6,180 (48.84) | 1,422 (34.09) | 1,048 (35.97) | 12.87 | 1.36 (1.24, 1.49) |
| 2019 | 6,358 (48.74) | 1,493 (32.86) | 1,236 (39.52) | 9.22 | 1.23 (1.14, 1.33) |
| 2020 | 7,448 (60.48) | 1,738 (36.01) | 1,498 (43.11) | 17.38 | 1.40 (1.30, 1.52) |
| NH-Asian | |||||
| 2017 | 1,599 (31.07) | 330 (22.15) | 585 (19.33) | 11.74 | 1.61 (1.38, 1.87) |
| 2018 | 1,726 (32.82) | 400 (26.5) | 661 (19.87) | 12.95 | 1.65 (1.42, 1.92) |
| 2019 | 1,788 (33.03) | 410 (26.9) | 753 (19.68) | 13.35 | 1.68 (1.45, 1.94) |
| 2020 | 2,105 (40.93) | 462 (27.54) | 916 (23.44) | 17.49 | 1.75 (1.52, 2.00) |
| Hispanic | |||||
| 2017 | 5,944 (43.09) | 708 (29.92) | 590 (34.07) | 9.02 | 1.26 (1.13, 1.41) |
| 2018 | 6,457 (45.47) | 775 (29.22) | 596 (30.69) | 14.78 | 1.48 (1.31, 1.68) |
| 2019 | 6,486 (44.04) | 833 (29.12) | 716 (36.58) | 7.47 | 1.20 (1.10, 1.32) |
| 2020 | 7,761 (52.31) | 1,000 (29.93) | 850 (33.78) | 18.53 | 1.55 (1.39, 1.73) |
The entire U.S. population, including racial/ethnic groups not listed in this table.
bRates are per 100,000 person-years and age standardized to the 2000 U.S. standard population. ICD-10 codes examined include COVID-19 (U071), heart disease (I00-I09, I11, I13, I20-I51), cancer (C00-C97), cerebrovascular disease (I60-I69), unintentional injury (V01-X59, Y85-Y86), chronic lower respiratory disease (J40-J47), diabetes (E10-E14), and Alzheimer disease (G30).
NH, non-Hispanic.
DISCUSSION
In this study using nationwide data from 2017 to 2020, widening educational attainment disparities in overall and cause-specific mortality were exacerbated in 2020, coincident with the emergence of the COVID-19 pandemic. Disparities in cause-specific mortality by educational attainment were particularly heightened in heart disease-, cancer-, cerebrovascular-, and unintentional injury-related deaths. Similar patterns were observed across race/ethnicity and sex, although Hispanic individuals had the greatest relative increase in disparities.
Differential access to care and COVID-19 death misclassification may explain the widened disparities. The pandemic brought fluctuations in health insurance coverage (by abrupt changes in employment) and health system disruptions in the U.S., adversely affecting healthcare access and quality, especially among people of color and of lower SES.11 , 12 For example, delays in radiation therapy13 and cancer surgery14 occurred more often among Black individuals and people of lower SES than among other patients with cancer during the height of the pandemic. Delays in cancer screening during the pandemic are also predicted to widen disparities in cancer mortality in the coming years.11 Although telemedicine partially mitigated the pandemic disruption on the health system for some health conditions, it created further disparities in access to care involving technology.15
The indirect relationship of COVID-19 with comorbidities may also lead to potential under or overreporting of COVID-19 deaths.16 The literature supports the accuracy of COVID-19 deaths using official death certificates.17 However, although coronial autopsy reports in the U.K. have suggested that most unnatural deaths were not caused by COVID-19,18 the extent to which COVID-19 deaths in the U.S. were misclassified as other causes is unknown. This indicates the need for further research on factors that contributed to increased disparities in mortality in 2020.
The rate ratio increases in unintentional injury‒deaths are mostly credited to the disproportionate increase in drug overdoses19 and a shift in accidents during stay-at-home periods20 in 2020 among populations of lower SES. The Hispanic community also experienced greater barriers in access to care during the height of the pandemic among those with lower SES,21 , 22 which may partially explain the increases in mortality disparities observed in this study. Such barriers include disproportionately lower-wage occupations that lack health benefits with employer-sponsored health plans,23 limiting access to and affordability of health care.
The strengths of this study include using nationally representative data and stratifying by educational attainment, race/ethnicity, and sex to better understand the patterns in mortality disparities. Conflicting patterns in recent mortality disparities reported in previous studies are likely the result of using preliminary and regional data.
Limitations
Limitations in this study include a lack of data on access to care or other relevant data to investigate the potential reasons for widened mortality disparities by education attainment in 2020 and the time lag between disruptions in care and related mortality. Moreover, although education attainment is a common proxy for SES in the U.S., it does not fully represent the social determinants of health and may under-represent certain groups.24
CONCLUSIONS
Mortality disparities by educational attainment substantially widened in the U.S. in 2020. Further research is warranted to fully understand the contributing factors to the widening disparities and to plan mitigation strategies in anticipation of future healthcare crises.
Acknowledgments
ACKNOWLEDGMENTS
The funders of the study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
This study was supported by the Surveillance & Health Equity Science Department of the American Cancer Society (grant number not applicable).
All authors are employed by the American Cancer Society, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside the submitted work. ECM's postdoctoral fellowship is supported by the American Cancer Society by a grant from Pfizer. JZ received funding from AstraZeneca for an unrelated project. No other financial disclosures were reported.
CRediT AUTHOR STATEMENT
Emily C. Marlow: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft. Ahmedin Jemal: Conceptualization, Writing – review and editing. Blake Thomson: Writing – review and editing. Daniel Wiese: Writing – review and editing. Jingxuan Zhao: Writing – review and editing. Rebecca L. Siegel: Writing – review and editing. Farhad Islami: Conceptualization, Methodology, Supervision, Visualization, Writing – review and editing.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2022.08.015.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Bosworth B. Increasing disparities in mortality by socioeconomic status. Annu Rev Public Health. 2018;39(1):237–251. doi: 10.1146/annurev-publhealth-040617-014615. [DOI] [PubMed] [Google Scholar]
- 2.Anderson NW, Zimmerman FJ. Trends in health equity in mortality in the United States, 1969–2019. SSM Popul Health. 2021;16 doi: 10.1016/j.ssmph.2021.100966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montez JK, Zajacova A, Hayward MD, Woolf SH, Chapman D, Beckfield J. Educational disparities in adult mortality across U.S. States: how do they differ, and have they changed since the mid-1980s? Demography. 2019;56(2):621–644. doi: 10.1007/s13524-018-0750-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Center for Disease Control. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Updated September 15, 2022. Accessed June 26, 2022.
- 5.Clouston SAP, Natale G, Link BG. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: a examination of the emergence of social inequalities. Soc Sci Med. 2021;268 doi: 10.1016/j.socscimed.2020.113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wadhera RK, Figueroa JF, Rodriguez F, et al. Racial and ethnic disparities in heart and cerebrovascular disease deaths during the COVID-19 pandemic in the United States. Circulation. 2021;143(24):2346–2354. doi: 10.1161/CIRCULATIONAHA.121.054378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwandt H, Currie J, von Wachter T, Kowarski J, Chapman D, Woolf SH. Changes in the relationship between income and life expectancy before and during the COVID-19 pandemic, California, 2015–2021. JAMA. 2022;328(4):360–366. doi: 10.1001/jama.2022.10952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Case A, Deaton A. National Bureau of Economic Research; Cambridge, MA: October 2021. Mortality rates by college degree before and during COVID-19. [Google Scholar]
- 9.2020 ACS 1-year public use microdata sample with experimental weights 2017-2020. United States Census Bureau. https://www.census.gov/programs-surveys/acs/data/experimental-data/2020-1-year-pums.html. Updated May 27, 2022. Accessed June 26, 2022.
- 10.National Center for Health Statistics, Centers for Disease Control and Prevention; 2022. Vital statistics online data portal: mortality multiple cause files 2017-2020.https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm#Mortality_Multiple Updated August 29, 2022. Accessed October 5, 2022. [Google Scholar]
- 11.Williams PA, Zaidi SK, Sengupta R. AACR report on the impact of COVID-19 on cancer research and Patient Care. Clin Cancer Res. 2022;28(4):609–610. doi: 10.1158/1078-0432.CCR-22-0192. [DOI] [PubMed] [Google Scholar]
- 12.Pujolar G, Oliver-Anglès A, Vargas I, Vázquez ML. Changes in access to health services during the COVID-19 pandemic: a scoping review. Int J Environ Res Public Health. 2022;19(3):1749. doi: 10.3390/ijerph19031749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsapatsaris A, Babagbemi K, Reichman MB. Barriers to breast cancer screening are worsened amidst COVID-19 pandemic: a review. Clin Imaging. 2022;82:224–227. doi: 10.1016/j.clinimag.2021.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernstein AN, Talwar R, Handorf E, et al. Assessment of prostate cancer treatment among black and white patients during the COVID-19 pandemic. JAMA Oncol. 2021;7(10):1467–1473. doi: 10.1001/jamaoncol.2021.2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eberly LA, Kallan MJ, Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77(2):159–169. doi: 10.1016/j.jacc.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gundlapalli AV, Lavery AM, f Boehmer, et al. Death certificate-based ICD-10 diagnosis codes for COVID-19 mortality surveillance - United States, January-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(14):523–527. doi: 10.15585/mmwr.mm7014e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pell R, Fryer E, Manek S, Winter L, Roberts ISD. Coronial autopsies identify the indirect effects of COVID-19. Lancet Public Health. 2020;5(9):e474. doi: 10.1016/S2468-2667(20)30180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghose R, Forati AM, Mantsch JR. Impact of the COVID-19 pandemic on opioid overdose deaths: a spatiotemporal analysis. J Urban Health. 2022;99(2):316–327. doi: 10.1007/s11524-022-00610-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin L, Shi F, Li W. Assessing inequality, irregularity, and severity regarding road traffic safety during COVID-19. Sci Rep. 2021;11(1):13147. doi: 10.1038/s41598-021-91392-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia MA, Homan PA, García C, Brown TH. The color of COVID-19: structural racism and the disproportionate impact of the pandemic on older Black and latinx adults. J Gerontol B Psychol Sci Soc Sci. 2021;76(3):e75–e80. doi: 10.1093/geronb/gbaa114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Velasco F, Yang DM, Zhang M, et al. Association of healthcare access with Intensive Care Unit utilization and mortality in patients of Hispanic ethnicity hospitalized with COVID-19. J Hosp Med. 2021;16(11):659–666. doi: 10.12788/jhm.3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown TH. Racial stratification, immigration, and health inequality: a life course-intersectional approach. Soc Forces. 2018;96(4):1507–1540. doi: 10.1093/sf/soy013. [DOI] [Google Scholar]
- 24.Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc. 2007;99(9):1013–1023. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2575866/ Accessed October 5, 2022. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.