Abstract
Objectives
Previous studies showed that older adults with fair or poor self-rated health (SRH) were more likely to experience delayed care during the COVID-19 pandemic. We aim to understand delayed care patterns by SRH during the COVID-19 pandemic among US older adults.
Methods
Using a nationally representative sample of older adults (≥ 70 years old) from the National Health and Aging Trends Study (NHATS), we assessed the patterns of delayed care by good, fair, or poor SRH.
Results
Nearly one in five of the survey-weighted population of 9,465,117 older adults who experienced delayed care during the pandemic reported fair or poor SRH. The overall distributions of the numbers of types of delayed care (p = 0.16) and the numbers of reasons for delayed care (p = 0.12) did not differ significantly by SRH status. Older adults with good, fair, or poor SRH shared the four most common types of delayed care and three most common reasons for delayed care but differed in ranking. Older adults with poor SRH mostly delayed seeing a specialist (good vs. fair vs. poor SRH: 40.1%, 46.7%, 73%, p = 0.01).
Conclusions
The results suggest that utilizing SRH as a simple indicator may help researchers and clinicians understand similarities and differences in care needs for older adults during the pandemic. Targeted interventions that address differences in healthcare needs among older adults by SRH during the evolving pandemic may mitigate the negative impacts of delayed care.
Keywords: Delayed care, COVID-19, Self-rated health, Older adults, Care disruptions
1. Introduction
The COVID-19 pandemic has disrupted access to medical care worldwide, leading to increased health burdens related to the pandemic (Weinstein et al., 2020; Tavares, 2022). Older adults, particularly those with fair or poor general health, have more healthcare needs and may be more susceptible to care interruptions during the pandemic than those with good general health (Sands et al., 2020; Steinman et al., 2020).
Self-rated health (SRH) is a subjective indicator of an individual's perceived health status encompassing perceived disease burden, mental health, and social context (Lorem et al., 2020). SRH is not only known as a simple but effective indicator of morbidity and mortality, but also a valid predictor of healthcare demand (Lorem et al., 2020; Cislaghi and Cislaghi, 2019). Recent studies suggested that being in fair or poor SRH was associated with a higher probability of experiencing delayed care during the pandemic among older adults (Tavares, 2022; Callison and Ward, 2021; Lei and Maust, 2022). However, existing studies have not examined the specific types of and reasons for care delays by SRH among older adults during the COVID-19 pandemic. This gap may be a missed opportunity to utilize SRH as a simple indicator in helping us understand different care needs for older adults during the pandemic.
In this study, we aim to compare the types of and reasons for delayed care among older adults by SRH. This comparison can inform the design of targeted interventions to alleviate the negative impacts of delayed care, ultimately improving patient outcomes and reducing care costs (Mollborn et al., 2005).
2. Methods
We used publicly available data from the National Health and Aging Trends Study (NHATS), a longitudinal survey designed to study daily life changes and experiences in older age based on annual surveys of a nationally representative sample of Medicare beneficiaries aged 65 years and older in the US (National Health and Aging Trends Study, 2021a). From June to October 2020, NHATS mailed a one-time COVID-19 supplement questionnaire to eligible older adults aged 70 years or older (National Health and Aging Trends Study, 2021b; National Health and Aging Trends Study, 2021c). Collections of responses were continued through January 2021 (unweighted response rate = 82%) (National Health and Aging Trends Study, 2021b). NHATS has been reviewed and approved by the Johns Hopkins Bloomberg School of Public Health's Institutional Review Board. Our sample included participants who reported care delays during the pandemic and had non-missing individual characteristics (i.e., information on SRH and sociodemographic and clinical characteristics). Individual characteristics, including SRH, were derived from round 9 of the NHATS survey, which was administered before the pandemic. Good SRH was defined as reporting general health as “good,” “very good,” or “excellent”, fair SRH was defined as reporting general health as “fair,” and poor SRH was defined as reporting general health as “poor.” Participants were considered to have delayed care during the pandemic if they responded “Yes” to the question, “During the COVID-19 outbreak, has there ever been a time when you needed or had planned to see a doctor or other health care provider but put off getting care?” The types of delayed care and reasons for delayed care were based on responses to the subsequent questions: 1) “What type(s) of care did you put off? Mark all that apply” and 2) “What are the reason(s) that you put off that care? Mark all that apply.”
We used the Rao-Scott Chi-square test to compare the categorical characteristics of participants, the numbers of reported types of and reasons for delayed care, and individual type of and reason for delayed care by SRH. We used F-test in linear regression for comparison of the continuous age variable. To examine patterns of delayed care, we plotted weighted percentages of the types of delayed care and reasons for delayed care by SRH. All analyses were conducted using the survey procedures in SAS software (version 9.4TS1m6), and survey-weighted statistics were reported.
3. Results
We identified 1121 participants who reported delayed care during the COVID-19 pandemic, which represented 9,465,117 older adults nationally. Approximately 60.1% of the participants were female, and 86.3% were non-Hispanic Whites (Table S1). About 19.9% of the participants reported fair or poor SRH.
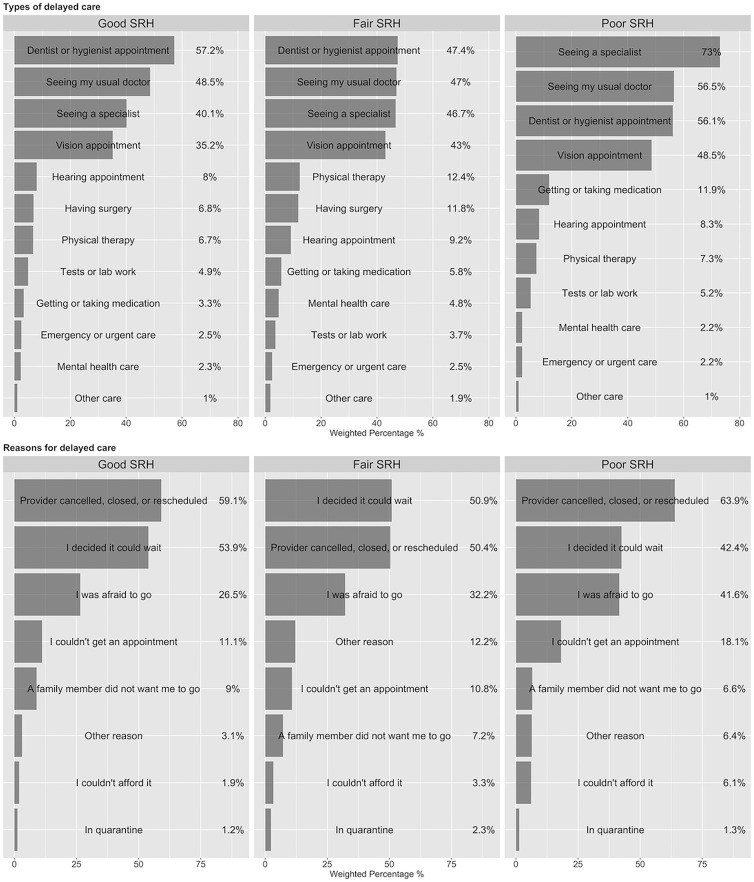
There were 12 types of delayed care and 8 reasons for delayed care (Fig. 1 , Table 1 ). About 31.8% of the participants reported one type of delayed care, 35.1% reported two types of delayed care, and the remaining 33.2% reported three or more types of delayed care. Regarding the numbers of reasons for delayed care, 52.5% of the participants reported one reason, 32.4% reported two reasons, and the remaining 15.1% reported three or more reasons. The overall distributions of the numbers of types of delayed care (p = 0.16) and the numbers of reasons for delayed care (p = 0.12) did not differ significantly by SRH status. Older adults with poor SHR had the highest proportion of those who experienced three or more types of delayed care (good<fair<poor SRH: 31.5% < 38.3% < 52.1%) and the highest proportion of those with three or more reasons for delayed care (good<fair<poor SRH: 13.9% < 19.6% < 23.4%).
Fig. 1.
Ranking of the types of and reasons for delayed care among older adults who reported delayed care by good, fair, or poor self-rated health (SRH).
Table 1.
Weighted percentages of types of and reasons for delayed care by self-rated health.
| Participants who reported delayed care N = 1121 Weighted % = 100% Weighted N = 9,465,117 |
Self-rated health |
p-value | |||
|---|---|---|---|---|---|
| Excellent/very good/good N = 875 Weighted % = 80.1% Weighted N = 7,579,271 |
Fair N = 218 Weighted % = 18.0% Weighted N = 1,703,016 |
Poor N = 28 Weighted % = 1.9% Weighted N = 182,831 |
|||
| Total number of reported types of delayed care | 0.16 | ||||
| 1 | 31.8 | 33.1 | 28.1 | 12.8 | |
| 2 | 35.1 | 35.4 | 33.6 | 35.1 | |
| ≥3 | 33.2 | 31.5 | 38.3 | 52.1 | |
| Total number of reported reasons for delayed care | 0.12 | ||||
| 1 | 52.5 | 51.9 | 56.0 | 47.1 | |
| 2 | 32.4 | 34.2 | 24.4 | 29.5 | |
| ≥3 | 15.1 | 13.9 | 19.6 | 23.4 | |
| Types of delayed care | |||||
| Seeing my usual doctor | 48.4 | 48.5 | 47.0 | 56.5 | 0.79 |
| Seeing a specialist | 42.0 | 40.1 | 46.7 | 73.0 | 0.01 |
| Vision appointment | 36.9 | 35.2 | 43.0 | 48.5 | 0.06 |
| Dentist or hygienist appointment | 55.4 | 57.2 | 47.4 | 56.1 | 0.07 |
| Other | 30.7 | 28.4 | 40.7 | 31.8 | <0.01 |
| Reasons for delayed care | |||||
| The provider cancelled, closed, or suggested rescheduling | 57.7 | 59.1 | 50.4 | 63.9 | 0.08 |
| I decided it could wait | 53.2 | 53.9 | 50.9 | 42.4 | 0.52 |
| I was afraid to go | 27.8 | 26.5 | 32.2 | 41.6 | 0.15 |
| Other | 25.0 | 23.6 | 31.2 | 28.2 | 0.10 |
Notes: All analyses were conducted using the survey procedures, incorporating survey strata, primary sampling units, and weight, in SAS software (version 9.4TS1m6), and survey-weighted statistics were reported.
Other types of delayed care including hearing appointment, having surgery, mental health care (therapist, psychologist, counselor), emergency or urgent care, getting or taking medication, tests or lab work and others”.
Other reasons for delayed care including “I couldn't afford it”, “I couldn't get an appointment”, “A family member did not want me to go”, “in quarantine”, and others.
Among participants who reported delayed care, 11 participants didn't select any types of delayed care and 23 participants didn't select any reasons for delayed care.
Older adults with good, fair, or poor SRH shared the four most common types of delayed care and three most common reasons for delayed care but differed in ranking. The four most common types of delayed care were seeing a dentist or hygienist appointment (good vs. fair vs. poor SRH: 57.2%, 47.4%, 56.1%, p = 0.07), seeing a usual doctor (48.5%, 47%, 56.5%, p = 0.79), seeing a specialist (40.1%, 46.7%, 73%, p = 0.01), and vision appointment (35.2%, 43%, 48.5%, p = 0.06). The three most common reasons for delayed care were “provider cancelled, closed, or rescheduled” (good vs. fair vs. poor SRH: 59.1%, 50.4%, 63.9%, p = 0.08), “I decided it could wait” (53.9%, 50.9%, 42.2%, p = 0.52), or “I was afraid to go” (26.5%, 32.2%, 41.6%, p = 0.15). Compared to older adults with good or poor SRH, more of those with fair SRH selected at least one type of delayed care other than the four most common types of delayed care (good vs. fair vs. poor SRH: 28.4%, 40.7%, 31.8%, p < 0.01).
Within each subgroup by SRH, we found that older adults with fair SRH reported similar degrees of care delays across the four common care types (i.e., the proportions of reported care delays were similar across specialist, dental, usual doctor, and vision appointments. The differences between these care types were less than <5%). In comparison, those with good SRH experienced substantially more delayed dental appointments than the other care types (the percentage of reported delays for dental appointments was 57.2%, while for the other types, the range was from 35.2%–48.5%). Those with poor SRH experienced substantially more delays seeing a specialist (the percentage of reported delays for specialist appointment was 73% and for the other care types, it ranged from 48.5%–56.5%).
4. Discussion
Based on a nationally representative sample of older adults (≥ 70 years old), we found that nearly one in five older adults who experienced care delays during the pandemic also had fair or poor SRH. While previous studies showed that older adults with fair or poor SRH were more likely to experience delayed care during the pandemic (Tavares, 2022; Callison and Ward, 2021; Lei and Maust, 2022), our results, for the first time, showed that there were more similarities than differences in delayed care patterns by SRH. We also provided a unique perspective on the extent to which care delays were initiated by the patient or the provider.
The most common types of and reasons for delayed care were in general similar among older adults with different SRH status with one notable exception. Those respondents with poor SRH experienced a significantly higher delay in seeing specialists than those with fair or good SRH. These findings may reflect the unique specialized care needs among older adults with poor SRH. As poor SRH is significantly associated with comorbidities and polypharmacy (≥ 3 drugs per day), delaying appointments with specialists may exacerbate the disease morbidity among older adults with poor SRH (Machón et al., 2016). We also found that half of the older adults with poor SRH reported at least three types of delayed care and one in five reported at least three reasons for delayed care, suggesting that these older adults experienced multiple types of unmet care needs simultaneously and faced multiple barriers when trying to access care during the pandemic. To reduce the negative impact of delayed medical care, clinicians and policymakers need a nuanced approach to address older adults' heterogeneous healthcare needs. Care management guidelines should be adapted to reflect situations during or post-pandemic for patients with poor SRH and conditions that require regular patient-provider interactions. For example, the providers should prioritize follow-up with patients at high risk of relapse, facilitate the expansion of telemedicine services to ensure continuity of care and access to prescribed medicines, and increase the availability of in-person appointments (Richards et al., 2020; Beran et al., 2021).
The three most common reasons for delayed care (i.e., “provider cancelled, closed, or rescheduled”, “I decided it could wait”, and “I was afraid to go”) may reflect provider and patient response to recommendations on postponing non-urgent care to free up healthcare resources in response to surges of COVID-19 in 2020 (Nab et al., 2021). The fact that a higher proportion of older adults with poor SRH selected “I was afraid to go” than those with good or fair SRH may suggest heightened psychological distress they were experiencing due to fear of exposure to the virus (Caston et al., 2021), and the realization that their health may put them at a higher risk of severe COVID-19. Overall, the results also suggest that delays in medical care are primarily attributable to both challenges experienced by providers (e.g., “provider cancelled, closed, or rescheduled”) and patients (e.g., “I decided it could wait”, “I was afraid to go”), which appear in our study to be more significant than cost-related barriers to accessing timely care (e.g., “I couldn't afford it”) (Lazzerini et al., 2020; Anderson et al., 2021).
This study has several limitations. First, the generalizability of findings may be limited as the NHATS COVID-19 questionnaire only accounts for the time between June 2020 to January 2021. Further research on the more recent stages of the pandemic about the causes and consequences of delayed care is needed. Second, the lack of specific types of specialist care delayed and measures of healthcare utilization in the survey prevented us from making detailed recommendations. Finally, this study relied on patient self-rated information and may be subject to recall bias. However, as the COVID questionnaire was initiated in June 2020, soon after the first wave of the COVID-19 pandemic in the US (i.e., between April and June), the short average recall window is likely to minimize the extent of issues relative to surveys with more extended look-back periods.
Despite the recent decline in new infections and related deaths, COVID-19 and its variants may continue to be a threat to public health in the US in the long term. Continued research into the causes and consequences of disruptions in care access during and post-pandemic are warranted. Future research may benefit from information on measures of healthcare utilization (e.g., changes in hospitalization rates and usage of outpatient services), which will provide an opportunity to further understand the effect of care delays.
Types of and reasons for delayed care by SRH may reflect the disparities in healthcare needs during the pandemic and following health problems post the pandemic. To mitigate potentially negative impact of delayed care and prepare for the possible health problems, clinicians and policymakers should adapt the care management guidelines to reflect situations during or post-pandemic for older adults with poor SRH and conditions that require regular patient-provider interactions. As SRH is one of the most commonly used and simple summary measures of overall health and well-being, clinics may consider taking advantage of this measure to understand patients' care needs and focus on appropriate follow-up care (Lorem et al., 2020; Cislaghi and Cislaghi, 2019). Example interventions could include setting an automatic reminder of checkups for all older adults, increasing psychosocial support, and implementing a structured medication refill program for those with poor SRH (Caston et al., 2021).
Funding
This study is in part funded by a grant from the National Institute on Aging (5P30AG028741–07) awarded to the Claude D Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai and the National Institute on Aging of the National Institutes of Health (T32AG066598).
Credit author statement
Conceptualization, Data curation, and Formal analysis: W.L. and B.L.; Writing - original draft: W.L.; Writing - review & editing: B.L., J.F., Y.L., and W.L.
Conflict of interests
The authors have no conflicts of interests to declare that are relevant to the content of this article.
Acknoledgements
National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (grant number NIA U01AG32947) and was conducted by the Johns Hopkins University, and produced and distributed by www.nhats.org with funding from the National Institute on Aging (grant number NIA U01AG32947).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2022.107308.
Appendix A. Supplementary data
Characteristics of older adults who experienced delayed care during the COVID-19 pandemic by self-rated health.
Data availability
The authors do not have permission to share data.
References
- Anderson K.E., McGinty E.E., Presskreischer R., Barry C.L. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Netw. Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.34882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beran D., Aebischer Perone S., Castellsague Perolini M., et al. Beyond the virus: ensuring continuity of care for people with diabetes during COVID-19. Primary Care Diabetes. 2021;15(1):16–17. doi: 10.1016/j.pcd.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callison K., Ward J. Associations between individual demographic characteristics and involuntary health care delays as a result of COVID-19. Health Aff. 2021;40(5):837–843. doi: 10.1377/hlthaff.2021.00101. [DOI] [PubMed] [Google Scholar]
- Caston N.E., Lawhon V.M., Smith K.L., et al. Examining the association among fear of COVID-19, psychological distress, and delays in cancer care. Cancer Med. 2021;10(24):8854–8865. doi: 10.1002/cam4.4391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cislaghi B., Cislaghi C. Self-rated health as a valid indicator for health-equity analyses: evidence from the Italian health interview survey. BMC Public Health. 2019;19(1):533. doi: 10.1186/s12889-019-6839-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health. 2020;4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L., Maust D.T. Delayed care related to COVID-19 in a nationally representative sample of older Americans. J. Gen. Intern. Med. 2022;37(5):1337–1340. doi: 10.1007/s11606-022-07417-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorem G., Cook S., Leon D.A., Emaus N., Schirmer H. Self-reported health as a predictor of mortality: a cohort study of its relation to other health measurements and observation time. Sci. Rep. 2020;10(1):4886. doi: 10.1038/s41598-020-61603-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machón M., Vergara I., Dorronsoro M., Vrotsou K., Larrañaga I. Self-perceived health in functionally independent older people: associated factors. BMC Geriatr. 2016;16(1):66. doi: 10.1186/s12877-016-0239-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollborn S., Stepanikova I., Cook K.S. Delayed care and unmet needs among health care system users: when does fiduciary trust in a physician matter? Health Serv. Res. 2005;40(6 Pt 1):1898–1917. doi: 10.1111/j.1475-6773.2005.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nab M., van Vehmendahl R., Somers I., Schoon Y., Hesselink G. Delayed emergency healthcare seeking behaviour by Dutch emergency department visitors during the first COVID-19 wave: a mixed methods retrospective observational study. BMC Emerg. Med. 2021;21(1):56. doi: 10.1186/s12873-021-00449-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health and Aging Trends Study National Health and Aging Trends Study (NHATS) User Guide. 2021. https://nhats.org/sites/default/files/2022-03/NHATS_User_Guide_R10_Final_Release.pdf Published 2021. Accessed January.
- National Health and Aging Trends Study COVID-19 Supplement to the National Health and Aging Trends Study. 2021. https://www.nhats.org/sites/default/files/2021-06/NHATS%20COVID-19%20User%20Guide%20Final.pdf USER GUIDE chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/ Published 2020. Accessed January.
- National Health and Aging Trends Study National Health and Aging Trends Study COVID-19 Questionnaire. 2021. https://www.nhats.org/sites/default/files/2021-01/NHATS%20R10%20COVID-19%20Questionnaires.pdf Published 2020. Accessed January.
- Richards M., Anderson M., Carter P., Ebert B.L., Mossialos E. The impact of the COVID-19 pandemic on cancer care. Nat. Can. 2020;1(6):565–567. doi: 10.1038/s43018-020-0074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sands L.P., Albert S.M., Suitor J.J. Understanding and addressing older adults’ needs during COVID-19. Innov. Aging. 2020;4(3) doi: 10.1093/geroni/igaa019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman M.A., Perry L., Perissinotto C.M. Meeting the care needs of older adults isolated at home during the COVID-19 pandemic. JAMA Intern. Med. 2020;180(6):819–820. doi: 10.1001/jamainternmed.2020.1661. [DOI] [PubMed] [Google Scholar]
- Tavares A.I. Older Europeans’ experience of unmet health care during the COVID-19 pandemic (first wave) BMC Health Serv. Res. 2022;22(1):182. doi: 10.1186/s12913-022-07563-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein E., Ragazzoni L., Burkle F., Allen M., Hogan D., Della Corte F. Delayed primary and specialty care: the coronavirus disease–2019 pandemic second wave. Disaster Med. Public Health Preparedness. 2020;14(3):e19–e21. doi: 10.1017/dmp.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of older adults who experienced delayed care during the COVID-19 pandemic by self-rated health.
Data Availability Statement
The authors do not have permission to share data.