Abstract
Multinodular and vacuolating neuronal tumor (MVNT) of the cerebrum is a rare and benign lesion which has been recently included in World Health Organization Classification of the central nervous system tumors. Another entity of lesions would present the same radiological characteristics; however, it would be in the posterior fossa, hence its name: infratentorial multinodular and vacuolating neuronal tumor. They are frequently characterized by the presence of cystic (or cyst-like) nodular lesions and may show cortical involvement. They mainly can be differentiated from other cystic entities, by their clustered and unchanging nature over time. We present the case of a 54-year-old patient who has consulted for epileptic seizures. Magnetic Resonance Imaging showed a multicystic-looking mass involving the vermis and the left cerebellar hemisphere that had no changes at follow-up in the last year suggestive of infratentorial multinodular and vacuolating neuronal tumor.
Keywords: Multinodular and vacuolating neuronal tumor of the cerebrum, Infratentorial multinodular and vacuolating neuronal tumor, Imaging characteristics, Magnetic resonance imaging
Abbreviations: MRI, magnetic resonance imaging; MVNT, multinodular and vacuolating neuronal tumors; MV-PLUS, multinodular and vacuolating posterior fossa lesions of unknown significance; Cho, choline; NAA, N-acetyl-aspartate
Introduction
Multinodular and vacuolating neuronal tumors are rare and benign, mixed glial and neuronal lesions, first described by Huse et al. in 2013 following work on a series of 10 patients [1]. Subsequently, they were included in 2016 in the World Health Organization classification of central nervous system tumors [2]. The majority of multinodular and vacuolating neuronal tumors of the supratentorial stage that have been reported in the recent literature were diagnosed based on imaging criteria only [3]. As such, lesions with the same radiological characteristics but located in the posterior fossa have been described without histological confirmation and have been named according to their location, multinodular and vacuolating posterior fossa lesions of unknown significance [4].
Through this work, we report an additional case of this unique entity, elaborating essentially on its radiological aspect.
Presentation of the case
This is a 54-year-old patient, followed for rheumatic and prostatic pathologies, who presented partial epileptic seizures for one year. He first underwent an EEG which showed focal epilepsy. Then he was referred to our department, to benefit from a cerebral magnetic resonance imaging (MRI) which was performed using a 1.5 Tesla device according to the following protocol: sagittal and axial on T1-weighted sequences, axial on T2-weighted sequences, T2 flair and diffusion, anatomical sequence, 3DFSPGR, axial on T1-weighted sequences with gadolinium injection and spectroscopy.
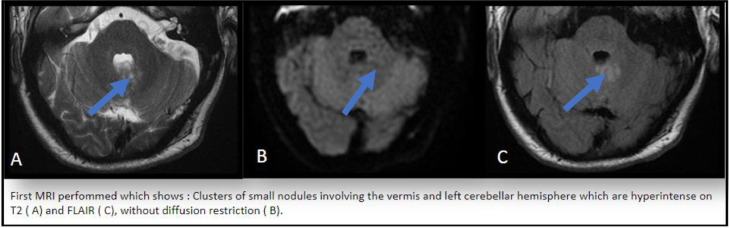
It showed left cerebellar hemisphere and vermis signal abnormalities centered on the middle cerebellar peduncle, producing a clustered nodular appearance hyperintense on T2-weighted sequences, containing small formations, frankly hyperintense on T2-weighted sequences (Fig. 1A), not cancelling on the Flair sequence (Fig. 1B), hypointense on T1-weighted, without diffusion restriction, not enhancing after injection of gadolinium (Fig. 2D), without alteration of the metabolites on spectroscopic analysis (Fig. 2E) and measuring overall 15 mm in long axis.
Fig. 1.
First MRI performed which shows: clusters of small nodules involving the vermis and left cerebellar hemisphere which are hyperintense on T2 (A) and FLAIR (C), without diffusion restriction (B).
Fig. 2.
Control MRI (1 year later): stability of the nodular lesions. No contrast enhancement (D). No significant alterations of main brain metabolites (E and F).
The diagnosis of multinodular and vacuolating neuronal posterior fossa lesion of unknown significance was then made post imaging. Surveillance was recommended for this patient with levetiracetam (500 mg / 12 hours) for seizure management. A follow-up MRI was conducted a year later. This follow-up MRI showed no change, confirming our diagnosis.
Discussion
The different series dealing with the topic of multinodular and vacuolating neuronal tumor have established their main radiological characteristics on MRI essentially, being the exploration standard of care. These tumors are often observed as clustered, round or ovoid, millimetric, sub- or juxta cortical nodules, occupying the supratentorial level [3]. Lecler et al. were interested in lesions located at the infratentorial level and closely resembling radiologically MVNTs and, consequently, attributed to them the name of MV-PLUS with respect to their location. MV-PLUS typically appear hypointense on T1-weighted sequences, hyperintense on T2 sequences and T2 Flair, similar to our study as well as those conducted by Nunes et al. [5]. Agarwal et al. found lesions that partially or totally cancel on the T2 Flair sequence. Most studies suggest that these lesions do not show enhancement after contrast injection or diffusion restriction, which is consistent with our case [6].
Literature provides few and contradictory information on the spectroscopic profile of these tumors. While the majority of studies, such as the Mauro et al., show no significant alteration of metabolites, and more specifically, no peak of Cho. Other studies reveal a Cho peak with a decrease in NAA. In our case, we note no alteration of metabolites [3]. Very few data concerning perfusion are found in literature. We note, however, a decrease in perfusion in some cases [6]. Finally, the unchanging nature of these lesions over time is also an important diagnostic criterion to take into account. This is confirmed in almost all studies as well as in our case, which demonstrates the benign nature of these tumors, not requiring histological evidence. Therapeutic management consists of monitoring, especially when the patient is asymptomatic. Surgical resection may however be required in case of epileptic seizures not managed by anticonvulsants treatment.
Conclusion
Infratentorial multinodular and vacuolating neuronal tumor have a typical radiological appearance. They consist of nodular lesions grouped in clusters, hyperintense on T2 FLAIR, without diffusion restriction, without enhancement after injection of Gadolinium, without alteration of metabolites in spectroscopy and which are invariable in time. These lesions, although rare, should be known by radiologists and clinicians. They have the particularity of requiring neither biopsy nor surgical management except in the case of uncontrolled seizures. Monitoring is sufficient and can even confirm the diagnosis. Only MRI allows the diagnosis of these tumors and their monitoring over time, making it the gold standard for these cases.
Patient consent
The patient has been informed and has given his consent to the publication of this case report.
Footnotes
Competing Interests: The authors declare no conflict of interest.
References
- 1.Huse JT, Edgar M, Halliday J, Mikolaenko I, Lavi E, Rosenblum MK. Multinodular and vacuolating neuronal tumors of the cerebrum: 10 cases of a distinctive seizure-associated lesion. Brain Pathol. 2013;23:515–524. doi: 10.1111/bpa.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 3.Mauro M, Daniele B. World Neurosurg. Vol. 136. Elsevier; 2020. Infratentorial multinodular and vacuolating neuronal tumor or multinodular and vacuolating posterior fossa lesions of unknown significance? Clinico-radiologic findings from 2 cases; pp. 58–61. [DOI] [PubMed] [Google Scholar]
- 4.Kış N, Erok B, Kılıç H, Önder H. A benign entity—cerebral multinodular and vacuolating neuronal tumor. Eur J Clin Exp Med. 2022;20(1):126–128. [Google Scholar]
- 5.Nunes RH, Hsu CC, Osborn AG. Presumptive diagnosis of multinodular vacuolating tumor: “more than meets the eye!”. Neuroradiology. 2017;59:1067–1068. doi: 10.1007/s00234-017-1916-x. [DOI] [PubMed] [Google Scholar]
- 6.Lecler A, Bailleux J, Carsin B, et al. Multinodular and vacuolating posterior fossa lesions of unknown significance. Am J Neuroradiol. 2019;40:1689–1694. doi: 10.3174/ajnr.A6223. [DOI] [PMC free article] [PubMed] [Google Scholar]