Abstract
Background
Given the long-term threat posed by COVID-19, predictors of mitigation behaviors are critical to identify. Prior studies have found that cognitive factors are associated with some COVID-19 mitigation behaviors, but few studies employ representative samples and no prior studies have examined cognitive predictors of vaccination status. The purpose of the present study was to examine associations between cognitive variables (executive function, delay discounting, and future orientation) and COVID-19 mitigation behaviors (mask wearing, social distancing, hand hygiene and vaccination) in a population representative sample.
Methods
A population representative sample of 2,002 adults completed validated measures of delay discounting, future orientation, and executive function. Participants also reported frequency of mitigation behaviors, vaccination status, and demographics.
Results
Future orientation was associated with more mask wearing (β = 0.160, 95 % CI [0.090, 0.220], p < 0.001), social distancing (β = 0.150, 95 % CI [0.070, 0.240], p < 0.001), hand hygiene behaviors (β = 0.090, 95 % CI [0.000, 0.190], p = 0.054), and a higher likelihood of being fully vaccinated (OR = 0.80, 95 % CI [0.670, 0.970], p = 0.020). Lower delay discounting predicted more consistent mask wearing (β = −0.060, 95 % CI[−0.120, −0.010], p = 0.032) and being fully vaccinated (OR = 1.28, 95 % CI [1.13, 1.44], p < 0.001), while more symptoms of executive dysfunction predicted less mask wearing (β = −0.240, 95 % CI [−0.320, −0.150] p < 0.001) and hand hygiene (β = −0.220, 95 % CI [−0.320, −0.130], p < 0.001), but not vaccination status (OR = 0.96, 95 % CI [0.80, 1.16], p = 0.690) or social distancing behaviors (β = −0.080, 95 % CI [−0.180, 0.020], p = 0.097). Overall, social distancing was the least well-predicted outcome from cognitive factors, while mask wearing was most well-predicted. Vaccination status was not a significant moderator of these effects of cognitive predictors on mitigation behaviors.
Conclusions
Cognitive variables predict significant variability in mitigation behaviors. regardless of vaccination status. In particular, thinking about the future and discounting it less may encourage more consistent implementation of mitigating behaviors.
Keywords: COVID-19, SARS-CoV-2, Mitigating behaviors, Executive functions, Vaccination
1. Introduction
The capacity to regulate attention, maintain goals in working memory, and resist transient impulses may be critical for implementation of novel, challenging or inconvenient behaviors in everyday life. Likewise, the ability to modulate stress and adapt to dynamically changing circumstances from moment to moment depends on cognitive processes emergent from the mind and brain. Thus, through direct and indirect routes, it is possible that cognitive capacities—which vary both between and within individuals over time—may predict consistency in behaviors that amplify or reduce infectious disease risk. In the COVID-19 context, considerable attention has been paid to sociodemographic, sociopolitical and attitudinal predictors of mitigation behavior performance, but relatively few studies have examined cognitive predictors specifically. Neurobiologically rooted decision-making processes and temporal biases have a long history within the field of behavioral economics and decision-making theory ([37], [38], [39], and so the omission of these factors as determinants of disease mitigation behaviors in COVID-19 would be shortsighted. The current study aims to fill this knowledge gap by testing the hypothesis that consistency in COVID-19 mitigation behaviors will be predicted by performance on a battery of cognitive tasks, decision making paradigms, and temporal bias measures while controlling for conventional sociodemographic variables. Moreover, given the relatively elementary level of operations supporting cognitive task performance, we envision that the predictive power of cognitive variables will be independent of vaccination status, which is known to be highly influenced by political orientation and ideology.
Understanding the determinants of COVID-19 mitigation behaviors is critically important for managing the current pandemic and future infectious disease outbreaks. Beyond vaccination, the most widely recommended individual mitigation behaviors for COVID-19 are mask wearing, physical distancing and hand hygiene [22]. These behaviors collectively require consistent implementation in a variety of social contexts and continually changing circumstances to prevent the spread of COVID-19 variants of concern. Maintaining behavioral consistency may require attention to cumulative benefits to the individual and society as a whole, attention to cues that impel the behaviors, holding social requirements in working memory, and the ability to flexibly alternate between implementation of behaviors (e.g., mask wearing) with dynamically changing environments (e.g., inside versus outside, in the presence of others versus alone). While previous work has highlighted the role of social factors in promoting mitigating behaviors, such as self- compared to group-related interests [15] and perceived risk of infection [35], a mindset oriented to future benefits, positive valuation of non-immediate contingencies, and strong executive functioning may be also be critical.
Consistent with this logic, several studies have shown that self-reported measures indexing executive functions (e.g., reports of cognitive failures and cognitive reflection; [32]; self-control and need for cognition scales; [41] and tasks examining working memory capacity [27], [33] are associated with adherence to COVID-19 mitigating behaviors in adults from the United States [27], [33], [34] and United Kingdom [32]. Relatedly, greater temporal discounting, a measure of impulsivity thought to be reflective of impaired executive functioning (i.e., inhibitory control; [2], assessed using behavioral tasks [10] and self-report measures [11] is associated with less mask-wearing and social distancing. Finally, future-oriented thinking has also been shown to increase satisfaction and compliance with COVID-19 restrictions [24]. These three cognitive factors associated with executive functions (impulsivity; self-control; and future-orientation) may be relevant for the ability to accurately accommodate and adjust to changes in public health regulations concerning mitigating behaviors (mask-wearing; social-distancing; and hand-hygiene). However, there is still a large gap in our understanding of the cognitive determinants of mitigating behaviors. Specifically, because no study has examined all three cognitive factors of executive functioning with all three mitigating behaviors within the same sample, their comparative importance is largely unknown.
The current study addresses the limitation of past work by providing a more comprehensive examination of cognitive predictors of COVID-19 behavioral outcomes and broadens past work by including an examination of vaccination uptake. Previous work examining vaccination status is largely absent, as vaccines were not immediately available at the onset of the pandemic. Further, some studies involving prediction of vaccination status are limited by a relatively low proportion of vaccine hesitant (i.e., a delay or refusal of vaccine uptake despite availability of resources) participants; this is most likely to occur in countries wherein vaccine uptake is high. Vaccine hesitancy is a major concern for controlling the spread of COVID-19, thus identifying motivational and cognitive predictors of vaccination uptake is critical [31]. Recent work examining social predictors of vaccination intention and uptake suggests that greater self-reported perceived vulnerability of infection, response efficacy, self-efficacy and more positive injunctive and descriptive norms are associated with greater vaccine intentions and uptake in adults 50–64 years old from the United Kingdom[40]. Similarly, an online study of Israeli adults (18 and older; mean age 43.55; [29] suggests that attitudes, trust, and perceived barriers to vaccination are associated with vaccination intention and uptake. While these past studies identify social factors associated with vaccine uptake and vaccine hesitancy (see also [25] for psychosocial predictors in a UK and Ireland population sample), it is currently unknown how cognitive predictors influence vaccination uptake, nor how vaccination status may moderate the association between cognitive variables and mitigating behaviors. Thus, the current study extends past work examining vaccination status in two critical ways: (1) by identifying cognitive, rather than social, predictors of vaccination status; and (2) examining how vaccination status may moderate the associations between cognitive variables and COVID-19 mitigating behaviors.
The current study was intended to examine cognitive predictors of COVID-19 mitigation behaviors (mask-wearing; social-distancing; hand-hygiene; vaccination uptake) in a demographically representative sample of Canadian adults between the ages of 18–55 through an online study. To ensure an equal number of vaccinated and vaccine-hesitant individuals, quota sampling of vaccine hesitant relative to vaccinated participants was implemented. At the time of data collection (November 2021), mandatory indoor mask wearing was mandated in most provinces, and guidelines for hand hygiene and distancing were well known and reminders ubiquitous; vaccines were widely available for all adults and strongly recommended country-wide. Within this context, it was hypothesized that higher self-control, future-orientation, and lower impulsivity would be associated with more consistent performance of COVID-19 mitigation behaviors, and a higher likelihood of receiving all recommended vaccinations. This study advances existing literature by examining three conceptually important cognitive and motivational variables using a large population-based dataset with sampling and statistical methods that allows for generalization to the population.
2. Methods
2.1. Participants
Participants were respondents in a baseline wave of the Canadian COVID-19 Experiences Survey (CCES; [20], a national cohort survey of 2002 Canadian adults aged 18–55 (Mean = 37, SD = 10.4; 60.8 % female). The cohort was recruited from Leger Opinion, the largest nationally representative panel in Canada, from three age groups (18–24, 25–39, and 40–54) across six geographic regions (British Columbia, Alberta, Saskatchewan and Manitoba, Ontario, Quebec, and the Maritimes: New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador). The quota system ensured an equal proportion of vaccinated and vaccine hesitant individuals. In the recruited sample, 50.2 % reported receiving two vaccine shots (i.e., fully vaccinated by the standards at the time of data collection), and 43.3 % reported receiving no vaccinations. Further 5.5 % reported receiving one vaccine shot but were not intending to receive a second shot. For each of the vaccinated and vaccine hesitant groups, sampling weights were computed using a raking procedure and calibrated based on population benchmarks from the 2016 Canadian census data and the disposition code in the sample to target marginal joint population distributions of the geographic regions, and the gender and age group combinations, thus allowing generalization to the Canadian population.
2.2. Procedure
The online survey was administered between September 28th and October 21st, 2021. Participants were contacted by email with an invitation to participate in the survey, with a link provided to all eligible participants. The survey was hosted by Leger Opinion using Qualtrics via the University of Waterloo Survey Research Centre. A quota target of equal numbers of vaccinated and vaccine hesitate and was applied to ensure an equal sample of vaccinated and vaccine hesitant individuals. Within each quota target, participants were recruited across ten Canadian provinces. The survey firm (Leger) and the University of Waterloo research team monitored the survey to ensure the final sample reached the intended quota targets. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008 and received ethical clearance from the University of Waterloo. Informed consent was obtained from all participants in this study.
2.3. Measures
2.3.1. Executive functions (self-control)
Executive functioning was assessed across four ‘self-restraint’ subscale items from the Barkley Deficits in Executive Functioning Scale short-form (BDEFS-SF; [3]. The following four items were used: “I am unable to inhibit my reactions or responses to events or to other people”, “I make impulsive comments to others”, “I am likely to do things without considering the consequences for doing them”, and “I act without thinking”. Participants were asked to report how often they have experienced each of the four problems over the past 6 months on a numeric scale, where 1 = “never or rarely”, 2 = “sometimes”, 3 = “often”, and 4 = “very often”. The four items were z-transformed and averaged together to create a composite executive function measure, with higher scores reflecting lower executive functioning. Because values were positively skewed, a Log10 transformation was applied. Cronbach’s alpha for the 4-item scale was 0.815, indicating good reliability.
2.3.2. Delay discounting (impulsivity)
A validated 5-item delay discounting (DD) task was used to assess valuation of non-immediate contingencies. The 5-item DD task presents respondents with a series of choices between a fixed immediate monetary amount ($500) and a larger reward at varying delay times (i.e., “Would you rather have $500 now, or $1000 in 4 h; 1 day; 3 weeks; 2 years?”; [23]. From these an indifference point can be calculated, reflecting the time at which the preference for a larger later reward reverts to a preference for the smaller immediate reward, denoted by the variable k. Higher k values are indicative of more impulsive decisions, that is, a higher discount rate, preferring a lower immediate reward over waiting for a higher reward. k values were positively skewed, and so a Log10 transformation was applied to improve normality. Because k values are between 0 and 1, log k values are negative, therefore lower log k values are associated with greater impulsivity.
2.3.3. Time perspective (temporal-orientation)
Participants responded to 4 questions assessing their degree of present and future orientation. Participants responded from 1 = ”strongly agree” to 5 = ”strongly disagree”, with 3 = “neither agree nor disagree” to two present-orientation questions (i.e., “Living for the moment is more important than planning for the future”, and “I spend a lot more time thinking about today than thinking about the future”) and to two future-orientation questions (i.e., “I spend a lot of time thinking about how my present actions will have an impact on my life later on”, and “I consider the long-term consequences of an action before I do it”(reversed scored; [21]. Participants responding with “Refused”, or “Don’t know” were removed from analyses (n = 179). The two present perspective, and two reverse-scored future perspective questions were first standardized and averaged together, with higher scores representing greater future relative to present orientation. Cronbach alphas for each of the subscales indicated acceptable reliability (present orientation: α = 0.742; future orientation: α = 0.665).
2.3.4. COVID-19 mitigating behaviors
Participants responded to questions assessing social distancing (“When outside your home, how consistently do you currently maintain a distance from others of at least 2 m?”), mask wearing (“How often do you currently wear a mask when you are in INDOOR public places?”), and hand hygiene (“How often do you thoroughly wash your hands during the day?”). Participants responded using the following response options: 1 = “Not at all”, 2 = “Rarely”, 3 = “Sometimes”, 4 = “Most of the time” and 5 = “All of the time”. Higher scores on these items reflected an increased consistency in behavioral performance. Participants responding “Refused”, or “Don’t know” to the items were removed from analyses (n = 74). The social distancing item module also contained a “I haven’t had contact with others” response, and the mask wearing item module contained a “I am never in indoor public places” response. Participants giving these responses (n = 49) were also removed, as it was assumed that such participants did not have an opportunity to enact the response being queried (e.g., immunocompromised individuals avoiding all indoor public spaces).
2.3.5. Vaccination status
Vaccination status was queried using the following item: “Have you received any COVID-19 vaccine shots?” Responses available were as follows, “I have NOT received any vaccine shot”, “Received ONE vaccine shot”, “Received TWO vaccine shots” [coded as fully vaccinated] or refused/don’t know. Those indicating that they had received only one shot were asked the following additional question: “What best describes your intention to get your next shot?” Response options were as follows: “I have NO plan to get a second shot”, “I am unsure whether I will get the second shot” [coded as unvaccinated without intention], “I plan to get the second shot, but have NOT yet scheduled an appointment”, and “I am planning to get the second shot and have scheduled an appointment”.
2.3.6. Demographics
Gender, age, income, ethnicity, and geographic region within Canada assessed by respondent report. Geographical region was coded directly from the online survey profile of each respondent.
2.4. Statistical analysis
All analyses were conducted in SAS version 9.4. Separate hierarchical multiple regression models were conducted, predicting behavioral outcomes from the following predictors: (1) BDEFS score (executive function), (2) Delay Discounting (k-value), (3) TPQ score (future orientation). The first analysis examined behavioral outcomes from each cognitive predictor without vaccination status, followed by analyses with vaccination status entered as a covariate. Control variables were entered on the first step, followed by main effects and interactions on subsequent steps. As such, all analyses were examined while controlling for demographic factors and vaccination status moderation effects were tested.
An additional analysis was conducted using multinominal regression models predicting vaccine hesitancy (no vaccines and one vaccine) from (1) BDEFS score, (2) Delay Discounting (k-value), and (3) TPQ score using the same parameters as described above. However, vaccination status, and the interaction with vaccination status, was not included in these models.
3. Results
In general, BDEF scores (M = 1.62, SD = 0.647) were low for unvaccinated (M = 1.56, SD = 0.621), single dose (M = 1.90, SD = 0.810), and fully vaccinated participants (M = 1.64, SD = 0.637). Participants were also generally more future oriented (M = 3.36, SD = 0.661; unvaccinated: M = 3.35, SD = 0.690; single dose: M = 3.17, 0.635; fully vaccinated: M = 3.41, SD = 0.633). Finally, participants generally scored low in impulsivity (M = 0.502, SD = 3.13; unvaccinated: M = 0.475, SD = 2.96; single dose: M = 1.11, SD = 4.74: fully vaccinated: M = 0.447, SD = 3.01).
3.1. Mitigation behaviors
Following adjustment for demographics (age, gender, income, ethnicity) and geographic region, a stronger future orientation was associated with more frequent social distancing (β = 0.14, 95 % CI [0.06, 0.22], t = 3.56, p < 0.001), mask wearing (β = 0.16, 95 % CI [0.10, 0.22, t = 4.98, p < 0.001), and hand hygiene (β = 0.10, 95 % CI [0.02, 0.19], t = 2.44, p = 0.015). Fewer symptoms of executive dysfunction were associated with more consistent mask wearing (β = −0.22, 95 % CI [−0.30, −0.15], t = −5.75, p < 0.001) and hand hygiene (β = −0.22, 95 % CI [−0.31, −0.14], t = −5.15, p < 0.001), but not social distancing (β = −0.07, 95 % CI [−0.16, 0.01], t = −1.65, p = 0.098). Finally, less delay discounting was associated with more mask wearing (β = −0.06, 95 % CI [−0.11, −0.02], t = −2.60, p = 0.009), but was unrelated to hand hygiene frequency (β = −0.00, 95 % CI [−0.06, 0.06], t = −0.01, p = 0.994) or social distancing (β = −0.02, 95 % CI [−0.07, 0.03], t = −0.71, p = 0.479).
When considering each behavior in turn, entering predictors simultaneously, mask wearing was uniquely predicable from both future orientation and executive dysfunction, while social distancing was not uniquely predictable from any focal variable (Table 1 ).
Table 1.
Unique predictors of each mitigation behavior.
| Variables | Social Distancing |
Mask Wearing |
Hand Hygiene |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta [95 % CI] |
t | p | Beta [95 % CI] |
t | p | Beta [95 % CI] |
t | p | ||||
| Executive function | −0.04 [−0.13, 0.05] |
−0.86 | 0.391 |
−0.19 [−0.27, −0.11] |
−4.77 | <0.001 |
−0.19 [−0.27, −0.11] |
−4.84 | <0.001 | |||
| Delay Discounting (k) | 0.00 [0.05, 0.06] |
0.06 | 0.953 | −0.03 [−0.08, 0.02] |
−1.33 | 0.184 | −0.02 [−0.07, 0.03] |
−0.80 | 0.424 | |||
| Temporal Orientation |
0.13 [0.05, 0.21] |
3.13 | 0.002 |
0.10 [0.04, 0.17] |
3.12 | 0.002 |
0.09 [0.03, 0.16] |
2.86 | 0.004 | |||
Note: Coefficients are standardized Beta weights predicting each target behavior, with the three cognitive variables entered as a single block, controlling for gender, age, income, ethnicity, and geographic region within Canada. Significant outcomes are highlighted in bold. BDEFS scores represent symptoms of executive dysfunction; as such higher scores indicate lower executive function. A negative coefficient indicates that relatively more intact executive function predicts more consistent mitigation behavior.
3.2. Main effects and interactions involving vaccination status
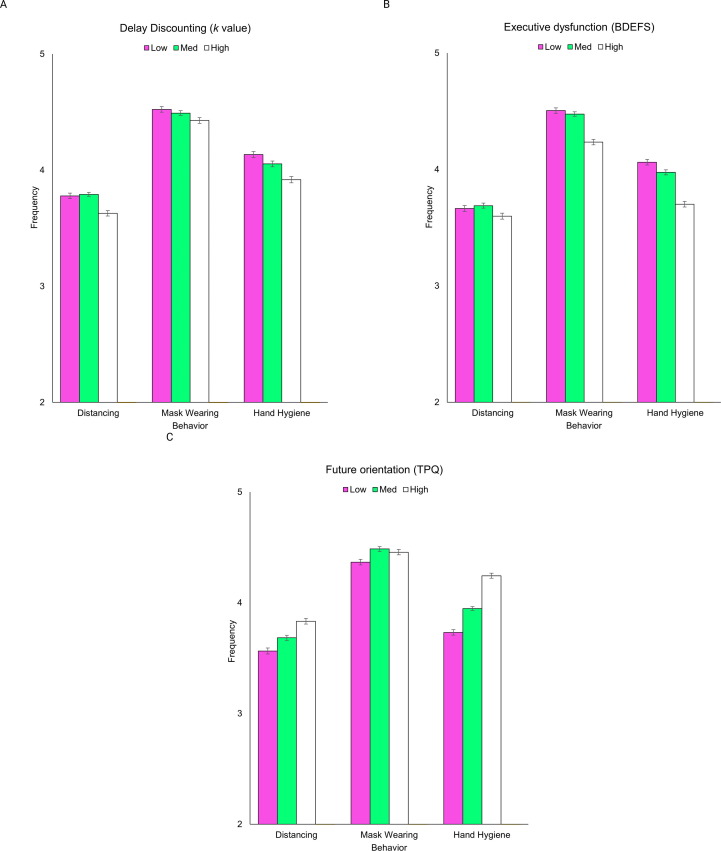
Higher BDEFS scores were associated with lower frequency of mask wearing (β = −0.240, 95 % CI [−0.320, −0.150] p < 0.001; Table 2 ) and hand hygiene behaviors (β = −0.220, 95 % CI [−0.320, −0.130], p < 0.001; Table 2; Fig. 1 ). BDEFS scores were not significantly associated with frequency of social distancing behaviors (β = −0.080, 95 % CI [−0.180, 0.020], p = 0.097). Greater delay discounting was not associated with social distancing behaviors (β = −0.010, 95 % CI [−0.070, 0.050], p = 0.812), or hand hygiene behaviors (β = 0.000, 95 % CI [−0.060, 0.070], p = 0.915), but lower delay discounting was associated with more consistent mask wearing (β = −0.060, 95 % CI [−0.120, −0.010], p = 0.032). Greater future orientation was associated with more consistent mask wearing (β = 0.160, 95 % CI [0.090, 0.220], p < 0.001), compliance with social distancing (β = 0.150, 95 % CI [0.070, 0.240], p < 0.001), and marginally associated with hand hygiene behaviors (β = 0.090, 95 % CI [0.000, 0.190], p = 0.054).
Table 2.
Regression analyses predicting mitigation behaviors from cognitive variables.
| Variables | Social Distancing |
Mask Wearing |
Hand Hygiene |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Beta [95 % CI] |
p | Beta [95 % CI] |
p | Beta [95 % CI] |
p | ||||
| Executive function (Mean) |
BDEFS | −0.08 [−0.18, 0.02] |
0.097 |
−0.24 [−0.32, −0.15] |
<0.001 |
−0.22 [−0.32, −0.13] |
<0.001 | ||
| Vaccination (NO vaccinations) |
−0.72 [−1.03, −0.40] |
<0.001 | −0.75 [−1.02, −0.47] |
<0.001 | −0.41 [−0.71, −0.11] |
0.008 | |||
| Vaccination (ONE vaccine shot) |
−0.018 [−0.84, 0.48] |
0.599 | −0.34 [−0.81, 0.13] |
0.155 | 0.32 [−0.29, 0.93] |
0.308 | |||
| Vaccination (TWO vaccine hosts) |
REF | REF | REF | REF | REF | REF | |||
| BDEFS*Vaccination (NO vaccinations) |
0.13 [−0.07, 0.32] |
0.197 | 0.14 [−0.04, 0.31] |
0.118 | 0.10 [−0.08, 0.29] |
0.284 | |||
| BDEFS*Vaccination (ONE vaccinations) |
−0.06 [−0.35, 0.24] |
0.714 | −0.03 [−0.30, 0.24] |
0.819 | −0.27 [−0.61, 0.07] |
0.121 | |||
| BDEFS*Vaccination (TWO vaccinations) |
REF | REF | REF | REF | REF | REF | |||
| Delay Discounting (DD) | DD | −0.01 [−0.07, 0.05] |
0.812 |
−0.06 [−0.12, −0.01] |
0.032 | 0.00 [−0.06, 0.07] |
0.915 | ||
| Vaccination (NO vaccinations) |
−0.36 [−0.63, −0.09] |
0.01 | −0.43 [−0.70, −0.17] |
0.001 | −0.12 [−0.39, 0.14] |
0.353 | |||
| Vaccination (ONE vaccine shot) |
−0.33 [−0.66, 0.00] |
0.052 | −0.35 [−0.70, 0.00] |
0.049 | −0.52 [−0.99, −0.05] |
0.031 | |||
| Vaccination (TWO vaccine hosts) |
REF | REF | REF | REF | REF | REF | |||
| DD*Vaccination (NO vaccinations) |
0.07 [−0.04, 0.18] |
0.223 | 0.03 [−0.08, 0.14] |
0.546 | 0.06 [−0.05, 0.17] |
0.281 | |||
| DD*Vaccination (ONE vaccinations) |
−0.02 [−0.15, 0.11] |
0.802 | 0.05 [−0.09, 0.18] |
0.498 | −0.12 [−0.29, 0.05] |
0.158 | |||
| DD*Vaccination (TWO vaccinations) |
REF | REF | REF | REF | REF | REF | |||
| Temporal Orientation | Time |
0.15 [0.07, 0.24] |
<0.001 |
0.16 [0.09, 0.22] |
<0.001 | 0.09 [0.00, 0.19] |
0.054 | ||
| Vaccination (NO shot) |
−0.12 [−0.71, 0.47] |
0.697 | −0.13 [−0.65, 0.39] |
0.628 | −0.42 [−0.99, 0.15] |
0.149 | |||
| Vaccination (ONE shot) |
−0.16 [−1.22, 0.90] |
0.768 | −0.60 [−1.57, 0.37] |
0.228 | 0.02 [−1.56, 1.60] |
0.982 | |||
| Vaccination (TWO shots) |
REF | REF | REF | REF | REF | REF | |||
| Time*Vaccination (NO shot) |
−0.12 [−0.29, 0.06] |
0.185 | −0.12 [−0.26, 0.03] |
0.126 | 0.06 [−0.11, 0.22] |
0.510 | |||
| Time*Vaccination (ONE shot) |
−0.04 [−0.39, 0.31] |
0.817 | 0.05 [−0.25, 0.35] |
0.750 | −0.09 [−0.61, 0.43] |
0.731 | |||
| Time*Vaccination (TWO shots) |
REF | REF | REF | REF | REF | REF | |||
Note: Main effects and two-way interactions for focal predictors and vaccination status controlling for gender, age, income, ethnicity, and geographic region within Canada. Those reporting ‘don’t know’; ‘refused’; and ‘NA’ vaccination status were classified as unvaccinated. All coefficients are standardized Beta weights. Significant main effects of cognitive measures are highlighted in bold. BDEFS scores represent symptoms of executive dysfunction; as such higher scores indicate lower executive function. A negative coefficient indicates that relatively more intact executive function predicts more consistent mitigation behavior.
Fig. 1.
Main effects of (a) delay discounting, (b) executive function, and (c) future orientation on frequency of COVID-19 mitigation behaviors. Higher scores on the y-axis reflect increased frequency of behavior performance. Participants were split into the lower (pink), mid (green), and higher categories (white) based on z-scores (-1.0, 0, +1.0). Error bars represent standard errors. Created with BioRender.com. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
With reference to being fully vaccinated, in all models involving BDEFS and delay discounting, not being fully vaccinated predicted less compliance with mitigation measures. For example, in models involving BDEFS, having received no vaccination predicted lower mask wearing (β = −0.750, 95 % CI [−1.02, −0.470], p < 0.001), hand hygiene (β = −0.410, 95 % CI [−0.710, −0.110], p = 0.008) and social distancing (β = -0.720, 95% CI [-1.03, -0.40], p < 0.001). No vaccine effects were evident in models involving future orientation. Additionally, no interactions involving vaccination status were evident for any models (Table 2).
3.2.1. Vaccination hesitancy and mitigating behaviors
With reference to fully vaccinated, Higher BDEFS scores did not significantly predict increased odds of being unvaccinated (OR = 0.96, 95 % CI [0.80, 1.16], p = 0.690; Table 3 ), but did predict higher likelihood of being partially vaccinated without intention to be fully vaccinated (OR = 1.95, 95 % CI [1.40, 2.70], p < 0.001). Those showing higher impulsivity on the delay discounting task were more likely to be unvaccinated (OR = 1.28, 95 % CI [1.13, 1.44], p < 0.001) and partially vaccinated without intentions to be fully vaccinated (OR = 1.46, 95 % CI [1.17, 1.83], p < 0.001). Similarly, greater future orientation predicted lower odds of being unvaccinated (OR = 0.80, 95 % CI [0.67, 0.97], p = 0.020) and lower odds of being partially vaccinated without intention to be fully vaccinated (OR = 0.54, 95 % CI [0.36, 0.80], p = 0.002).
Table 3.
Regression analyses of cognitive factors predicting vaccination.
| Variables | NO vaccine shots |
ONE vaccine shot |
|||||
|---|---|---|---|---|---|---|---|
| Odds Ratio [95 % CI] |
p | Odds Ratio [95 % CI] |
p | ||||
| Executive Function (mean) | BDEFS | 0.96 [0.80, 1.16] |
0.690 | 1.95 [1.40, 2.70] |
<0.001 | ||
| Delay Discounting (DD) | DD | 1.28 [1.13, 1.44] |
<0.001 | 1.46 [1.17, 1.83] |
<0.001 | ||
| Temporal Orientation | Time | 0.80 [0.67, 0.97] |
0.020 | 0.54 [0.36, 0.80] |
0.002 | ||
Note: Those receiving two vaccinations are the reference classification for this analysis. This analysis controlled for gender, age, income, ethnicity, and geographic region within Canada. Those reporting ‘don’t know’; ‘refused’; and ‘NA’ vaccination status were classified as unvaccinated. BDEFS scores represent symptoms of executive dysfunction; as such higher scores indicate lower executive function. A negative coefficient indicates that relatively more intact executive function predicts more consistent mitigation behavior.
4. Discussion
In this population-based sample, we examined cognitive determinants of COVID-19 mitigation behaviors among a Canadian representative sample of adults between the ages of 18 and 55 years. Findings demonstrated that those who adopted a future-oriented mindset were more likely to report consistent mask wearing, distancing, and were more likely to be fully vaccinated. Participants scoring lower in impulsivity on the delay discounting task predicted more consistent mask wearing and full vaccination status, while higher self-reported self-control (lower BDEFS) predicted mask wearing and hand hygiene, but not vaccination status or distancing. Overall, social distancing was the least well-predicted outcome from cognitive factors, while mask wearing was most well-predicted. These findings were robust following adjustment for demographics, income level, and geographic region. Among the three cognitive variables future orientation was the most consistently predictive of COVID-19 mitigation behaviors. Finally, moderating effects of vaccination status were negligible, suggesting that each of the cognitive variables is similarly predictive among vaccinated and vaccine hesitant sub-populations.
The association between participants’ delay discounting scores and self-reported future orientation with more consistent engagement with COVID-19 mitigating behaviors suggests that value processing wherein non-immediate outcomes are protected from discounting is generally important in COVID-19 mitigation. Although there are links to neurobiological substrates, delay discounting and future orientation are potentially malleable cognitive processes wherein a conscious appreciation of (and belief in) connections between present actions and later outcomes could become a target for public health communications. Indeed, gain-framed messaging (i.e., highlighting the benefits of engaging in a particular behavior; e.g. “Exercising regularly can help you lose weight”) has been identified as a particularly powerful messaging framework to encourage preventative health behaviors (i.e., [18]). Moreover, perceived risk of infection is associated with greater compliance with COVID-19 mitigative behaviors [12], [15], [26], [36], however risk perception may decrease as the initial threats of COVID-19 subside. Thus, health messaging that highlights the long-term positive outcomes of engaging in COVID-19 mitigating behaviors may be particularly important to deploy population wide.
The self-reported measure of self-control, on the other hand, was associated with a more circumscribed set of COVID-19 mitigating behaviors. Specifically, lower self-control predicted less consistent mask wearing and hand hygiene—both are repetitive, discrete behaviors and acts of commission, therefore likely require self-control particularly in the constant changing environment surrounding COVID-19. However, this measure of self-control should be considered carefully: the BDEFS is an assessment tool designed for clinical practice, and it may therefore miss some important dimensional aspects of cognitive function more relevant to vaccination and distancing in a population survey format (i.e., working memory; [27], [33]. Notably, vaccination and social distancing are highly multi-determined, such that political orientation and other beliefs may overshadow the predictive power of any relatively coarse cognitive indicator. Moreover, the self-reported nature of this measure, as with any self-report, should be considered, as participants may not be reliable in their responses.
The cognitive factors highlighted in the present study may influence other important determinants of COVID-19 mitigation behaviors, including the perceived severity of disease, perceived susceptibility to infection [15], and the perceived costs of engaging in preventive behaviors (e.g., balance of costs of physical distancing to perceived benefit). Additionally, because perceived trust in authorities has emerged as a significant predictor of compliance with previous influenzas [7] and with COVID-19 [5], [14], future work should examine how other social-cognitive variables may mediate the associations between cognitive variables and mitigating behaviors. For example, previous work demonstrated that increasing the perceived social norm of mask wearing in the context of reducing the spread of COVID-19 resulted in increased mask wearing behavior [8]. Moreover, social factors may be particularly important for social distancing, a behavior that was least predictable from the neurocognitive variables tested. It is possible that social distancing can be better predicted from social-cognitive variables (e.g., beliefs about and attitudes towards other individuals and groups [6], [13], [17], [19], [28], [30], [35], given its links to the social fabric of everyday life, as opposed to the physical environment and de-contextualized behavior. Given that social distancing is fundamentally a relational behavior with interpersonal consequences, this possibility in comparison to cognitive variables may warrant further investigation. With these additional variables, this work may inform government messaging (e.g., providing clear and direct messaging; [4], [9]; e.g., avoiding false dichotomies; [16] to improve intervention uptake within the population.
Our findings are consistent with several other studies that have found associations between executive functions and mitigation behaviors [27], [32], [33], [34]. However, our study goes beyond these prior studies through the inclusion of multiple cognitive and behavioral variables, and vaccination status. The latter cannot be tested with sufficient power in samples that do not contain a high proportion of both vaccinated and vaccine hesitant individuals. Our study—which used a sampling quota such that a large and approximately equal numbers of fully vaccinated and vaccine hesitant individuals were surveyed—is the largest study conducted to date, allowing for a strong test of the hesitancy moderation hypothesis. We determined that, although there are reliable effects of vaccination status on the implementation of mitigation behaviors, these effects are largely independent from cognitive variables on the implementation of mitigation behaviors.
Strengths of the current investigation include the use of a population representative sample, ensuring the findings may be generalized to the larger population from which they were drawn. Additionally, the use of quota sampling to ensure approximately 50 % vaccine hesitant ensures adequate statistical power to determine the moderating impact of vaccination status on any findings. No other investigations to date have this feature and would for the most part be unable to determine uniformity of prediction across vaccination status groups. Limitations include the use of self-reported vaccination status and executive function, and abbreviated versions of time perspective measures due to the population survey format. Although reliance on self-report is a limitation in some respects, self-reports of the predictor variables are reliable in this sample, and self reports correlate well with health-related behaviors, sometimes better than imperfect objective measures [1]. The cross-sectional analysis is also a limitation in terms of predictive power, and future work would benefit from a longitudinal approach. Finally, the sample age range is from 18 to 55 years, thereby excluding older adults and adolescents. However, statistics were weighted based on the 2016 Canadian Census to control for this limitation, and this working age population is arguably a key population in which to study mitigation behaviors as such individuals tend to be highly mobile and more variable in the implementation of precautions relative to older age groups.
5. Conclusion
Our findings suggest that cognitive variables reflecting future-oriented thinking, evaluative processing and self-control are associated with likelihood of being fully vaccinated against COVID-19 and predict more consistent implementation of mitigation behaviors. Among the three constructs, delay discounting and future orientation were the most consistent predictors of COVID-19 mitigation behaviors and vaccination status. Health communication campaigns that reinforce and emphasize positive valuation of future outcomes, and connections between present actions and later outcomes, may facilitate better response from the general public. However, it is also possible that among the less observant public, behavior may be more influenced by communications emphasizing more immediate benefit.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This research was supported by an operating grant to P. Hall, G. Fong and S. Hitchman by the Canadian Institutes for Health Research (CIHR), Institute for Population and Public Health (GA3-177733).
Data availability
Data will be made available on request.
References
- 1.Armitage C.J., Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(4):471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 2.Bari A., Robbins T.W. Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol. 2013;108:44–79. doi: 10.1016/j.pneurobio.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Barkley RA. Barkley Deficits in executive functioning scale (BDEFS). Guilford Press; 2011.
- 4.Benham J.L., Lang R., Kovacs Burns K., MacKean G., Léveillé T., McCormack B., Sheikh H., Fullerton M.M., Tang T., Boucher J.-C., Constantinescu C., Mourali M., Oxoby R.J., Manns B.J., Hu J., Marshall D.A. Attitudes, current behaviours and barriers to public health measures that reduce COVID-19 transmission: a qualitative study to inform public health messaging. PLoS ONE. 2021;16(2) doi: 10.1371/journal.pone.0246941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bicchieri C., Fatas E., Aldama A., Casas A., Deshpande I., Lauro M., Parilli C., Spohn M., Pereira P., Wen R. In science we (should) trust: expectations and compliance across nine countries during the COVID-19 pandemic. PLoS ONE. 2021;16(6) doi: 10.1371/journal.pone.0252892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bigot A., Banse E., Cordonnier A., Luminet O. Sociodemographic, cognitive, and emotional determinants of two health behaviors during SARS-CoV-2 outbreak: an online study among French-Speaking Belgian responders during the Spring Lockdown. Psychologica Belgica. 2021;61(1):63–78. doi: 10.5334/pb.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bish A., Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. 2010;15(4):797–824. doi: 10.1348/135910710X485826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bokemper S.E., Cucciniello M., Rotesi T., Pin P., Malik A.A., Willebrand K., Paintsil E.E., Omer S.B., Huber G.A., Melegaro A. Experimental evidence that changing beliefs about mask efficacy and social norms increase mask wearing for COVID-19 risk reduction: results from the United States and Italy. PLOS ONE. 2021;16(10) doi: 10.1371/journal.pone.0258282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonell C., Michie S., Reicher S., West R., Bear L., Yardley L., et al. Harnessing behavioural science in public health campaigns to maintain ‘social distancing’ in response to the COVID-19 pandemic. Key Principles. 2020;3 doi: 10.1136/jech-2020-214290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byrne K.A., Six S.G., Anaraky R.G., Harris M.W., Winterlind E.L. Risk-taking unmasked: using risky choice and temporal discounting to explain COVID-19 preventative behaviors. PLOS ONE. 2021;16(5) doi: 10.1371/journal.pone.0251073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Camargo J., Passarelli D.A., de Oliveira M.A., de Rose J.C. Probability discounting and adherence to preventive behaviors during the COVID-19 pandemic. PsyArXiv. 2021 doi: 10.31234/osf.io/p4a76. [DOI] [Google Scholar]
- 12.Cori L., Bianchi F., Cadum E., Anthonj C. Risk perception and COVID-19. Int J Environ Res Public Health. 2020;17(9):3114. doi: 10.3390/ijerph17093114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coroiu A., Moran C., Campbell T., Geller A.C. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLOS ONE. 2020;15(10) doi: 10.1371/journal.pone.0239795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Devine D., Gaskell J., Jennings W., Stoker G. Trust and the coronavirus pandemic: what are the consequences of and for trust? An early review of the literature. Polit Stud Rev. 2021;19(2):274–285. doi: 10.1177/1478929920948684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elharake J.A., Shafiq M., McFadden S.M., Malik A.A., Omer S.B. The association of coronavirus disease 2019 risk perception, county death rates, and voluntary health behaviors among United States adult population. J Infect Dis. 2022;225(4):593–597. doi: 10.1093/infdis/jiab131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Escandón K., Rasmussen A.L., Bogoch I.I., Murray E.J., Escandón K., Popescu S.V., et al. COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC Infect Dis. 2021;21(1):710. doi: 10.1186/s12879-021-06357-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frounfelker R.L., Santavicca T., Li Z.Y., Miconi D., Venkatesh V., Rousseau C. COVID-19 experiences and social distancing: insights from the theory of planned behavior. Am J Health Promot. 2021;35(8):1095–1104. doi: 10.1177/08901171211020997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gallagher K.M., Updegraff J.A. Health message framing effects on attitudes, intentions, and behavior: a meta-analytic review. Ann Behav Med. 2012;43(1):101–116. doi: 10.1007/s12160-011-9308-7. [DOI] [PubMed] [Google Scholar]
- 19.Gouin J.-P., MacNeil S., Switzer A., Carrese-Chacra E., Durif F., Knäuper B. Socio-demographic, social, cognitive, and emotional correlates of adherence to physical distancing during the COVID-19 pandemic: a cross-sectional study. Can J Public Health. 2021;112(1):17–28. doi: 10.17269/s41997-020-00457-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall P.A., Fong G.T., Hitchman S.C., Quah A.C.K., Agar T., Meng G., et al. Brain and behavior in health communication: The Canadian COVID-19 Experiences Project. Brain, Behavior, & Immunity - Health. 2022;22:100467. doi: 10.1016/j.bbih.2022.100467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall P.A., Fong G.T., Sansone G. In: Time Perspective Theory; Review, Research and Application: Essays in Honor of Philip G. Zimbardo. Stolarski M., Fieulaine N., van Beek W., editors. Springer International Publishing; 2015. Time Perspective as a Predictor of Healthy Behaviors and Disease-Mediating States; pp. 339–352. [DOI] [Google Scholar]
- 22.Honein M.A., Christie A., Rose D.A., Brooks J.T., Meaney-Delman D., Cohn A., et al. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. MMWR Morb Mortal Wkly Rep. 2020;69(49):1860–1867. doi: 10.15585/mmwr.mm6949e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koffarnus M.N., Bickel W.K. A 5-trial adjusting delay discounting task: accurate discount rates in less than one minute. Exp Clin Psychopharmacol. 2014;22(3):222–228. doi: 10.1037/a0035973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lalot F., Abrams D., Ahvenharju S., Minkkinen M. Being future-conscious during a global crisis: the protective effect of heightened futures consciousness in the COVID-19 pandemic. Personality Individ Differ. 2021;178 doi: 10.1016/j.paid.2021.110862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1):29. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nese M., Riboli G., Brighetti G., Sassi V., Camela E., Caselli G., et al. Delay discounting of compliance with containment measures during the COVID-19 outbreak: a survey of the Italian population. J Public Health. 2022;30(2):503–511. doi: 10.1007/s10389-020-01317-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Shea D.M., Davis J.D., Tremont G. Verbal memory is associated with adherence to COVID-19 protective behaviors in community dwelling older adults. Aging Clin Exp Res. 2021;33(7):2043–2051. doi: 10.1007/s40520-021-01905-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pfattheicher S., Nockur L., Böhm R., Sassenrath C., Petersen M.B. The emotional path to action: empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol Sci. 2020;31(11):1363–1373. doi: 10.1177/0956797620964422. [DOI] [PubMed] [Google Scholar]
- 29.Shiloh S., Peleg S., Nudelman G. Vaccination against COVID-19: a longitudinal trans-theoretical study to determine factors that predict intentions and behavior. Ann Behav Med. 2022;56(4):357–367. doi: 10.1093/abm/kaab101. [DOI] [PubMed] [Google Scholar]
- 30.Shushtari Z.J., Salimi Y., Ahmadi S., Rajabi-Gilan N., Shirazikhah M., Biglarian A., et al. Social determinants of adherence to COVID-19 preventive guidelines: a comprehensive review. Osong Public Health Res Perspect. 2021;12(6):346–360. doi: 10.24171/j.phrp.2021.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taylor S., Landry C.A., Paluszek M.M., Groenewoud R., Rachor G.S., Asmundson G.J.G. A proactive approach for managing COVID-19: the importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.575950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thoma V., Weiss-Cohen L., Filkuková P., Ayton P. Cognitive predictors of precautionary behavior during the COVID-19 pandemic. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.589800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xie W., Campbell S., Zhang W. Working memory capacity predicts individual differences in social-distancing compliance during the COVID-19 pandemic in the United States. Proc Nat Acad Sci. 2020;117(30):17667–17674. doi: 10.1073/pnas.2008868117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu P., Cheng J. Individual differences in social distancing and mask-wearing in the pandemic of COVID-19: the role of need for cognition, self-control and risk attitude. Personality Individ Differ. 2021;175 doi: 10.1016/j.paid.2021.110706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yan Y., Malik A.A., Bayham J., Fenichel E.P., Couzens C., Omer S.B. Measuring voluntary and policy-induced social distancing behavior during the COVID-19 pandemic. Proc Natl Acad Sci. 2021;118(16) doi: 10.1073/pnas.2008814118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yıldırım M., Geçer E., Akgül Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol Health Med. 2021;26(1):35–43. doi: 10.1080/13548506.2020.1776891. [DOI] [PubMed] [Google Scholar]
- 37.Frederick S., Loewenstein G., O’Donoghue T. Time Discounting and Time Preference: A Critical Review. Journal of Economic Literature. 2002;XL:351–401. [Google Scholar]
- 38.McClure S.M., Laibson D.I., Loewenstein G., Cohen J.D. Separate Neural Systems Value Immediate and Delayed Monetary Rewards. Science. 2004;306(5695):503–507. doi: 10.1126/science.1100907. [DOI] [PubMed] [Google Scholar]
- 39.Sanfey A.G., Loewenstein G., McClure S.M., Cohen J.D. Neuroeconomics: cross-currents in research on decision-making. Trends in Cognitive Science. 2006;10(3):108–116. doi: 10.1016/j.tics.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 40.Griffin B., Conner M., Normal P. Applying an extended protection motivation theory to predict Covid-19 vaccination intentions and uptake in 50–64 year olds in the UK. Social Science and Medicine. 2022;298(114819) doi: 10.1016/j.socscimed.2022.114819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu P., Cheng J. Individual differences in social distancing and mask-wearing in the pandemic of COVID-19: The role of need for cognition, self-control and risk attitude. Personality and Individual Differences. 2021;175(110706) doi: 10.1016/j.paid.2021.110706. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.