Abstract
Loneliness among older adults is a public health problem that has received particular attention since the emergence of the COVID-19 pandemic. Studies to date have however found a rather modest psychosocial impact of the pandemic on older adults, and scarce research has analyzed this impact using a comprehensive equity lens. The present study used an intersectional approach to examine social inequalities in loneliness before and during the early phase of the pandemic among older adults receiving eldercare in Sweden. The study population (analytical N = 205,529) came from two waves (2019 and 2020) of a total population survey to all older adult (>65 years of age) home care recipients and nursing home residents in Sweden. Loneliness was self-reported by a single-item measure, and survey data were linked to population register data on age, gender, residential setting, income, and country of birth. Additive binomial regression models were used to estimate prevalence differences and discriminatory accuracy according to an analysis of individual heterogeneity and discriminatory accuracy (AIHDA) approach. Results showed inequalities in loneliness arising particularly in the intersection of country of birth, income, and residential setting. The inequalities widened slightly but ubiquitously following the emergence of the pandemic in 2020, with particularly nursing home residents emerging as a risk group. The discriminatory accuracy of inequalities was consistently low to moderate throughout the analyses but increased marginally during the pandemic in 2020. The study illustrates how social inequalities engenders heterogeneity in the psychosocial risk of older adults before and during the pandemic. These findings should stimulate more nuanced and equity-oriented depictions, research and policies about loneliness among older adults in the peri-pandemic era.
Keywords: Loneliness, Intersectionality, Older adults, Sweden, Covid-19, Health inequalities, Discriminatory accuracy
Introduction
Loneliness among older adults has come into the spotlight during the COVID-19 pandemic (Chawla et al., 2021) as countries promptly introduced particularly restrictive policy measures for older adults (Dahlberg, 2021; Dyer, 2020). In Sweden, the setting of the present study, such targeted measures included strict but voluntary quarantine recommendations for all adults aged 70 years or older, and a visiting ban at all nursing homes for older adults, starting in March 2020 (Ludvigsson, 2020).
Despite this ostensibly vulnerable position of older adults, empirical research has found a surprisingly modest impact on elderly's loneliness during at least the early phase of the pandemic (Lebrasseur et al., 2021; Parlapani et al., 2021), including in Sweden (Gustafsson et al., 2022b; Kivi et al., 2021). These observations have subsequently led to measured discussions about older adults' vulnerability and resilience to the psychosocial impact of the pandemic (Fristedt et al., 2021; Gustafsson et al., 2022b; Losada-Baltar et al., 2021; Parlapani et al., 2021). However, any universal depiction of older adults' vulnerability or resilience fails to take into account the inherent heterogeneity within the group of older adults, for example, with regard to the deeply entrenched social inequalities shaping the outcomes of the pandemic (Bambra et al., 2020; Marmot and Allen, 2020; Pentaris et al., 2020). An equity lens has also been comparatively rarely applied in research on loneliness among older adults (Niedzwiedz et al., 2016), and little is thus know about how underlying social inequalities have influenced the welfare of older adults during the pandemic (Parlapani et al., 2021; Pentaris et al., 2020).
Recent debates within epidemiology (Agenor, 2020; Bauer and Scheim, 2019; Merlo, 2018; Richman and Zucker, 2019) have emphasized the inherent complexity of multiple simultaneous inequalities, a development promoted by the concept of intersectionality (Crenshaw, 1989; McCall, 2005). Intersectionality is an analytical framework that represents an epistemologically and methodologically heterogenous collection of scientific thoughts and practices (McCall, 2005). At its core, intersectionality emphasizes the intertwinement of complex social positions along multiple dimensions of power or inequity, and the consequences of this intertwinement, with attention paid to how societal changes generate, amplify, or temper inequalities (Bauer, 2014). The emergence of intersectionality within epidemiology has been followed by increasing use of analytical methods considering both estimation of group-average differences as well as discriminatory accuracy; the ability of social positions to discriminate between those with and without the outcome under study (Merlo, 2018; Wemrell et al., 2021a). This approach yields policy-relevant information as it gives guidance on the spectrum of universal and targeted intervention strategies, according to the principle of proportionate universalism (Merlo, 2018).
Applying an intersectional equity lens to loneliness among older adults during the pandemic requires consideration of multiple intertwined axes of power or inequality of potential relevance for loneliness. Older age, even within the population of adults already denoted as ‘older’, could potentially entail challenges to social interaction due to retirement, death of partner, relatives and friends, and health and financial barriers to participation in social activities, which also can exacerbate digital exclusion (Dahlberg et al., 2018, 2022; Seifert et al., 2021; Shin et al., 2020). While higher loneliness with increasing age has indeed been reported among the oldest old (Niedzwiedz et al., 2016), a recent meta-analysis showed similar levels of loneliness among older and younger older adults (Chawla et al., 2021). Gender inequalities in loneliness among older adults display a complex and context-dependent pattern, with similar or higher levels of loneliness, as well as greater impact of the COVID-19 pandemic (Hansen et al., 2021), among older women compared to older men (Cohen-Mansfield et al., 2016; Pinquart and Sorensen, 2001). Economic inequalities in loneliness, with greater loneliness among older adults with lower income or wealth (Bosma et al., 2015; Niedzwiedz et al., 2016), have been hypothesized to reflect poorer opportunities to develop relationships during working age, the direct financial barrier to social activities, and indirect barriers due to income-related inequalities in health and functional limitations (Niedzwiedz et al., 2016). Older immigrants in the European context also tend to experience loneliness more frequently than their native counterparts (Ten Kate et al., 2020). This can be rooted in language and cultural barriers (Park et al., 2019), as well as in the development of existential loneliness (Olofsson et al., 2021). With ageing, the residential setting also emerges as an important consideration from the principle of ‘ageing in (the right) place’ (Rogers et al., 2020), and which simultaneously can enable and limit the lives of older adults. For example, moving to a nursing home reflects a change in power relations and autonomy, with a tension between freedom and dependence (Caspari et al., 2018), and where residents can experience low autonomy, limitations to doing things they like, and little opportunities to engage in everyday activities (Sandgren et al., 2021). Such limitations have become more pronounced during pandemic (Lood et al., 2021).
The present study was motivated by the converging needs of research on social inequalities in loneliness among older adults, on the broader public health consequences of the pandemic for this population, and on the integration of intersectional perspectives to public health. The specific aims were to examine multiple inequalities in loneliness among older adults in eldercare before and during the pandemic, and the change in inequalities, with respect to:
-
1.
Singular inequalities by age, gender, income, country of birth and residence;
-
2.
Intersectional inequalities by intersectional strata; and
-
3.
Discriminatory accuracy of singular and intersectional inequalities.
Methods
The Swedish eldercare context
Swedish eldercare is a publicly funded, universal and needs-based service for all older adult residents. It is part of the range of Swedish welfare systems introduced according to egalitarian principles, and also includes, e.g., universal healthcare, childcare, and unemployment and sickness benefits. Eldercare is the responsibility of the 290 local municipalities of Sweden, and comprises two types of comprehensive and continuous care, home care and nursing homes, as well as more limited services such as meal distribution or safety alarms for older adults (Socialstyrelsen, 2021). Home care represents the first level of continuous care, aiming to support older adults to retain their residence even when illness or other limitations makes independent living difficult. Nursing homes, the second level of eldercare, are reserved for individuals for whom the care needs are greater than can be provided by home care and for whom a move to long-term facility therefore is required. Both home care and nursing homes are subsidized services, which are granted after individual needs assessment by the municipality, as regulated by The Social Services Act (1980:620).
While the provision of eldercare historically has been a public responsibility in Sweden, over the last decades, eldercare has undergone a gradual change towards marketization and privatization, where users choose their provider among municipal and for-profit private actors. This development matches the situation of eldercare in other Nordic countries (Szebehely and Meagher, 2018), and reflects the gradual but comprehensive neoliberal reorientation of the Swedish welfare discourse (Andersson and Kvist, 2015), where similar patient-choice and marketization policies have been ubiquitously implemented in other welfare sectors (Raphael, 2014), e.g., in primary health care (Burstrom, 2015).
In 2020, 29% the population 80 years or older received either home care (18.5%) or were nursing home residents (10.6%), of which about one third by private actors (Prochazka, 2021). This is a smaller proportion than before the Covid-19 pandemic in 2019 (31.5%), and the proportional coverage has also gradually declined over the last decades; from 34.5% in 2014, and from around 60% in the 1980s (Szebehely and Meagher, 2018).
Study population and procedures
The study employed a repeated cross-sectional design with two annual samples from the same target population. The data came from the Elderly Care Survey 2019 and 2020, which was conducted by the National Board of Health and Welfare to monitor the quality of eldercare delivery in Sweden. The survey targets the total population of Swedish residents, including temporary residents, permanent residents and citizens, 65 years or older, and who are recipients of either home care or residence at a nursing home (Socialstyrelsen, 2020). The population is identifiable by the Social Service Register, which registers all home care recipients and nursing home residents, and which through the unique Swedish Personal Identity Number provides linkage to other population registers.
The survey questionnaire comprises 20–25 items focusing on perceptions of the eldercare, but also survey-related information and perceived loneliness. Basic demographic information (gender, age) was routinely linked to the survey, and additional sociodemographic information (income, country of birth) was retrieved and linked to the survey data for the purpose of the present study.
The surveys were disseminated in the beginning of March in 2019 (the year before the pandemic) and 2020 (during the outbreak of the pandemic), respectively, and responses were received until end of May. For the nursing home sample, questionnaires were distributed to N = 72,431 nursing home residents in 2019 and N = 70,077 in 2020, with N = 36,248 respondents in 2019 (50% response rate) and N = 27,872 respondents in 2020 (40%). For the sample of community-dwelling older adults, questionnaires were sent to N = 160,283 home care recipients in 2019 and N = 159,527 in 2020, with N = 88,749 responses in 2019 (60%) and N = 82,843 in 2020 (57%). Due to missing data and applying complete case analysis, the effective sample available for analysis included N = 108,607 in 2019 and N = 96,922 in 2020, in total N = 205,529 older adults which was the sample used for all analyses.
The study was approved by the Swedish Ethics Review Authority (decision no. 2020–06879).
Perceived loneliness
Loneliness was measured by the single questionnaire item ‘Does it happen that you are troubled by loneliness?‘, which was constructed for the purpose of the survey. It has Likert-scale response options which were dichotomized (1 = ‘Yes, often’; 0 = ‘Yes, now and then’ or ‘No’). Dichotomization was done as a binary outcome was required for the analyses, and the cut-off chosen to correspond to previous operationalizations of ‘severe loneliness’ in contrast to ‘moderate loneliness’ (Gardiner et al., 2020). This was based on the reasoning that, in the context of the marked restrictions to social life during the pandemic, severe loneliness may be a more appropriate outcome, and occasional loneliness could arguably be considered a normal experience. The ambiguous ‘Don't know/No opinion’ was coded differently depending on the respondent, as individuals themselves selecting this option are unlikely to suffer from frequent loneliness, but when completed with help of another person it may also reflect unwillingness to disclose loneliness or communication difficulties. ‘Don't know/No opinion’ responses were therefore coded as ‘0’ if the questionnaire completed by respondent and as missing if completed with the aid of another person.
Inequality indicators
Five variables were used as inequality indicators. Residence indicated own residence with home care (coding = 0) or at a nursing home (=1). Age was coded as younger (65–84 years = 0) vs older (85 years or older = 1) older adults and gender was coded as men (=0) vs women (=1). Disposable income in 2019 was divided into tertiles and coded as high (=0) vs medium (=1) or low (=2) income. Country of birth was coded as Sweden (=0) vs outside Sweden (=1).
To operationalize singular social positions and inequalities, i.e., where each dimension is considered one by one and independently from each other, the five indicators were used separately. To operationalize intersectional inequalities, i.e., where the complex combinations of the social positions are additionally considered, the five indicators were cross-classified into 48 mutually exclusive intersectional strata.
Covariates
Two covariates were included as potential confounders, as they could potentially introduce response bias in the ratings of loneliness and could also be unequally distributed across the inequality dimensions: questionnaire form (web = 0, physical = 1) and respondent of the questionnaire (self = 0, with assistance = 1).
Statistical analyses
The analyses were conducted according to an Analysis of Individual Heterogeneity and Discriminatory Accuracy (AIHDA) framework, comprising both estimation of group-averages differences as well as of discriminatory accuracy of the social positions. All estimates were based on additive models estimated by generalized linear models with binomial family and identity link, rather than the logistic regression more commonly employed in AIHDA (Axelsson Fisk et al., 2021; Wemrell et al., 2021a). An additive model was chosen in order to provide estimates of absolute rather than relative inequalities, and to capture additive-rather than multiplicative-scale interactions, which have been a point of departure within intersectionality theory since its conception (Crenshaw, 1989) and emphasized specifically within intersectionality-informed epidemiology (Bauer, 2014).
Analyses were performed separately for the 2019 (before the pandemic) and 2020 (during the pandemic) surveys, as well as collapsed for comparison of estimates between the years. Collapsing all observations within each year was chosen as previous studies on the same population have found no specific loneliness impact attributable to the introduction of restrictive policies among either home care recipients (Gustafsson et al., 2022a) or nursing home residents (Gustafsson et al., 2022b).
Corresponding to the first aim, singular inequalities in loneliness were first estimated as prevalence differences (PD) of loneliness in crude models (Model 0), and in a model adjusted for covariates (Model 1). Each inequality dimension was treated as an independent variable using the theoretically most privileged category as reference (Sweden-born; high-educated; men; age 65–84 years; and living in own residence). To estimate the change in inequalities from before to during the pandemic, independent comparisons of each PDs in 2019 and 2020, respectively, were estimated in the form of absolute prevalence difference-in-differences (PDD), with confidence intervals yielded by the procedure proposed by Altman and Bland (2003).
For the second aim focusing on intersectional inequalities in loneliness, Model 0 and 1 and between-year comparisons were estimated in the same manner as described above but including the cross-classified variable comprising 48 intersectional strata in lieu of the individual inequality dimensions. The multiply privileged group of younger Sweden-born men with high income and living in their own residence was used as the reference group.
Corresponding to the third aim, the discriminatory accuracy of the singular and intersectional inequalities in loneliness was estimated by the Area Under the Receiver Operating Characteristics curve (AU-ROC, or AUC) in three models separately for 2019 and 2020, respectively. Values of the AUC range from 0.5, indicating no discriminatory ability at all, to 1, indicating perfect discriminatory ability. While there is no universal cut-off to what constitutes a large or small AUC (Hosmer et al., 2013), in the present study we used previously suggested denominations to pre-defined ranges of the AUC (Axelsson Fisk et al., 2021; Wemrell et al., 2021b), whereby discriminatory ability is labelled as ‘absent or very small’ (0.5 < AUC<0.6), ‘moderate’ (0.6 = AUC<0.7), ‘large’ (0.7 = AUC<0.8) and ‘very large’ (AUC≥0.8). First, a model with only covariates was run, representing the baseline model (Model 1); second, a model with covariates plus the five separate inequity dimensions, illustrating the discriminatory accuracy of the inequity dimensions when considered as separate and independent (Model 2); and last, a model with covariates plus the cross-classified intersectional strata, representing the discriminatory accuracy when considering the interaction of the inequity dimensions (Model 3). The ΔAUC between the nested models was reported to illustrate the incremental discriminatory value of considering socioeconomic inequalities (Model 2 vs Model 1), and of considering the intersectional positions (Model 3 vs Model 1; and Model 3 vs Model 2). Testing the pairwise differences between AUC estimates across nested models within the same year, and between AUC estimates in 2019 and 2020 across independent models, was done using the DeLong method (DeLong et al., 1988), which allows for comparison of either dependent or independent ROC curves. Model fit was evaluated by the Akaike Information Criterion (AIC), where >2 units difference between nested models was considered a significant difference in model fit.
All analyses and graphical displays were conducted using R software, version 4.0.2. Descriptive analyses and regression models were performed by using “finalfit” package v1.0.4, and for ROC curves and AUC calculations and comparisons were done using the package “pROC”, v1.18.0, including the function “roc.test” for comparison of independent/dependent ROC curves. Finally, package “ggplot2”, version 3.3.5 was used to create the figures.
Results
Sample characteristics
As seen in a descriptive summary of the study population (Table 1 ), the 2019 and 2020 samples were comparable when it comes to the relative distributions of age (57.5 vs 56.4% ≥ 85 years), gender (66.9 vs 65.8% women), income (33.5 vs 33.0% lowest income tertile), and country of birth (11.7 vs 11.8% outside Sweden), but the proportion from nursing homes declined from 2019 (29.5%) to 2020 (24.3%). From 2019 to 2020, an increasing proportion of older adults also completed the questionnaire on their own (41.3% in 2019 and 49.8% in 2020) and by the web (5.4% in 2019 and 8.2% in 2020).
Table 1.
Distribution of characteristics and prevalence of loneliness in Swedish older adults in eldercare in 2019 and 2020. Numbers are N (%).
| Variable | Category | 2019, Total |
2019, Loneliness |
2020, Total |
2020, Loneliness |
|---|---|---|---|---|---|
| Total sample | 108,607 (100) | 15,645 (14.4) | 96,922 (100) | 13,628 (14.1) | |
| Covariates | |||||
| Respondent | Self | 44,863 (41.3) | 4327 (9.6) | 48,241 (49.8) | 4602 (9.5) |
| Other | 63,744 (58.7) | 11,318 (17.8) | 48,681 (50.2) | 9026 (18.5) | |
| Questionnaire | Postal | 102,763 (94.6) | 14,538 (14.1) | 88,958 (91.8) | 12,137 (13.6) |
| Web | 5844 (5.4) | 1107 (18.9) | 7964 (8.2) | 1491 (18.7) | |
| Inequality dimension | |||||
| Age | 65–84 | 46,109 (42.5) | 6207 (13.5) | 42,304 (43.6) | 5574 (13.2) |
| 85+ | 62,498 (57.5) | 9438 (15.1) | 54,618 (56.4) | 8054 (14.7) | |
| Sex | Men | 35,961 (33.1) | 4280 (11.9) | 33,193 (34.2) | 3906 (11.8) |
| Women | 72,646 (66.9) | 11,365 (15.6) | 63,729 (65.8) | 9722 (15.3) | |
| Residence | Own home | 76,612 (70.5) | 10,022 (13.1) | 73,386 (75.7) | 9090 (12.4) |
| Nursing home | 31,995 (29.5) | 5623 (17.6) | 23,536 (24.3) | 4538 (19.3) | |
| Income | High | 35,248 (32.5) | 4643 (13.2) | 33,426 (34.5) | 4200 (12.6) |
| Medium | 36,967 (34.0) | 5726 (15.5) | 31,554 (32.6) | 4823 (15.3) | |
| Low | 36,392 (33.5) | 5276 (14.5) | 31,942 (33.0) | 4605 (14.4) | |
| Country of birth | Sweden | 95,898 (88.3) | 13,145 (13.7) | 85,509 (88.2) | 11,446 (13.4) |
| Other | 12,709 (11.7) | 2500 (19.7) | 11,413 (11.8) | 2182 (19.1) |
The overall prevalence of loneliness was similar in 2019 (14.4%) and 2020 (14.1%) and was patterned by each of the five inequality dimensions in both 2019 and 2020, with higher prevalence among older participants, women, immigrants, nursing home residents, and participants with medium or low income, in both 2019 and 2020.
Singular inequalities in loneliness before and during the pandemic
Corresponding to the first aim, the estimated absolute singular inequalities in loneliness are reported in Table 2 . In crude models in 2019, the largest inequality was seen for country of birth with 5.96 percentage points (pp) higher loneliness prevalence among immigrants, followed by residence (4.49pp higher among nursing home residents), gender (3.74pp higher among women), income (2.32pp higher among medium-income and 1.33pp higher among low-income groups), and age (1.64pp higher among older participants). In adjusted model, the inequality estimates were majorly attenuated for age (0.01pp) and income (medium income: 0.81pp; low income: 1.25pp), with notable inequalities remaining for country of birth (5.36pp), gender (3.49pp) and residence (1.81pp).
Table 2.
Absolute inequalities in loneliness among Swedish older adults in eldercare by single inequality dimensions in crude and adjusted models 2019 (N = 108,607) and 2020 (N = 96,922). Estimates are prevalence difference (PD), or prevalence difference differences (PDD) expressed in percentage points, with 95% confidence intervals (CI).
| Variable | Category | 2019 Crude | 2019 Adjusteda | 2020 Crude | 2020 Adjusteda | 2020 vs 2019 Adjusteda |
|---|---|---|---|---|---|---|
| Inequality dimensions | ||||||
| Age | 65–84 | Ref | Ref | Ref | Ref | Ref |
| 85+ | 1.64 (1.22–2.06) | 0.01 (−0.4 to 0.42) | 1.57 (1.13–2.01) | −0.1 (−0.52 to 0.32) | −0.11 (−0.69 to 0.48) | |
| Gender | Men | Ref | Ref | Ref | Ref | Ref |
| Women | 3.74 (3.32–4.17) | 3.42 (3–3.85) | 3.49 (3.04–3.93) | 2.98 (2.54–3.42) | −0.44 (−1.05 to 0.17) | |
| Residence | Own residence | Ref | Ref | Ref | Ref | Ref |
| Nursing home | 4.49 (4.01–4.97) | 1.81 (1.3–2.32) | 6.89 (6.34–7.45) | 3.66 (3.07–4.24) | 1.85 (1.07–2.62) | |
| Income | High | Ref | Ref | Ref | Ref | Ref |
| Medium | 2.32 (1.81–2.83) | 0.81 (0.32–1.31) | 2.72 (2.19–3.25) | 1.47 (0.95–1.98) | 0.65 (−0.06 to 1.37) | |
| Low | 1.33 (0.82–1.83) | −1.25 (−1.75 to −0.75) | 1.85 (1.33–2.38) | −0.41 (−0.93 to 0.11) | 0.84 (0.12–1.56) | |
| Country of birth | Sweden | Ref | Ref | Ref | Ref | Ref |
| Other | 5.96 (5.24–6.69) | 5.36 (4.65–6.08) | 5.73 (4.98–6.49) | 4.72 (3.98–5.46) | −0.64 (−1.67 to 0.39) | |
| Covariates | ||||||
| Questionnaire | Postal | Ref | Ref | Ref | Ref | Ref |
| Web | 4.8 (3.77–5.82) | 3.18 (2.18–4.17) | 5.08 (4.19–5.96) | 2.11 (1.25–2.96) | 0.24 (−0.39 to 0.88) | |
| Respondent | Self | Ref | Ref | Ref | Ref | Ref |
| Other | 8.11 (7.71–8.51) | 7.11 (6.68–7.55) | 9 (8.57–9.43) | 7.35 (6.89–7.82) | −1.07 (−2.38 to 0.24) |
Model adjusted for questionnaire form (web/physical) and respondent of questionnaire (self/with assistance).
Overall, the inequalities displayed a similar direction and magnitude in 2020 as in 2019 (Table 2). However, 2020 saw a significant 1.85pp increase in residence-related inequalities in the risk of loneliness in the adjusted model, amounting to 3.66pp higher loneliness prevalence among nursing home residents compared to community-dwelling older adults. Moreover, the lower risk in the low-compared to high-income group seen in the 2019 adjusted analyses was attenuated by 0.84pp, ending up in similar risk estimates to the high-income group. The changes for the other inequalities from 2019 to 2020 were all small (0.1–0.7pp) and non-significant.
Intersectional inequalities in loneliness before and during the pandemic
Corresponding to the second aim, the distribution of participants across the 48 intersectional strata, and the prevalence of loneliness in each stratum, are shown in Table 3 . The prevalence of loneliness varied markedly across the intersectional strata, ranging between 8.5% and 26.1% in 2019 and 7.7%–26.6% in 2020.
Table 3.
Distribution of intersectional strata and prevalence of loneliness in Swedish older adults in eldercare in 2019 (N = 108,607) and 2020 (N = 96,922). Numbers are N (%).
| Intersectional stratum | 2019, Total | 2019, Lonely | 2020, Total | 2020, Lonely |
|---|---|---|---|---|
| Total | 108,607 (100.0) | 15,645 (14.4) | 96,922 (100.0) | 13,628 (14.1) |
| Sweden; OR; M; High; 65-84 | 6437 (5.9) | 569 (8.8) | 6569 (6.8) | 506 (7.7) |
| Sweden; OR; M; High; 85+ | 5714 (5.3) | 610 (10.7) | 5734 (5.9) | 568 (9.9) |
| Sweden; OR; M; Medium; 65-84 | 3694 (3.4) | 390 (10.6) | 3395 (3.5) | 400 (11.8) |
| Sweden; OR; M; Medium; 85+ | 3063 (2.8) | 312 (10.2) | 3021 (3.1) | 292 (9.7) |
| Sweden; OR; M; Low; 65-84 | 2410 (2.2) | 205 (8.5) | 2319 (2.4) | 235 (10.1) |
| Sweden; OR; M; Low; 85+ | 2015 (1.9) | 179 (8.9) | 1890 (2.0) | 166 (8.8) |
| Sweden; OR; W; High; 65-84 | 4831 (4.4) | 605 (12.5) | 4714 (4.9) | 535 (11.3) |
| Sweden; OR; W; High; 85+ | 7077 (6.5) | 1037 (14.7) | 6717 (6.9) | 888 (13.2) |
| Sweden; OR; W; Medium; 65-84 | 6691 (6.2) | 931 (13.9) | 6108 (6.3) | 832 (13.6) |
| Sweden; OR; W; Medium; 85+ | 9034 (8.3) | 1423 (15.8) | 8405 (8.7) | 1255 (14.9) |
| Sweden; OR; W; Low; 65-84 | 6763 (6.2) | 778 (11.5) | 6494 (6.7) | 688 (10.6) |
| Sweden; OR; W; Low; 85+ | 9504 (8.8) | 1241 (13.1) | 9174 (9.5) | 1158 (12.6) |
| Sweden; NH; M; High; 65-84 | 1870 (1.7) | 290 (15.5) | 1513 (1.6) | 297 (19.6) |
| Sweden; NH; M; High; 85+ | 2344 (2.2) | 383 (16.3) | 1860 (1.9) | 310 (16.7) |
| Sweden; NH; M; Medium; 65-84 | 1357 (1.2) | 231 (17.0) | 1002 (1.0) | 173 (17.3) |
| Sweden; NH; M; Medium; 85+ | 1673 (1.5) | 265 (15.8) | 1207 (1.2) | 206 (17.1) |
| Sweden; NH; M; Low; 65-84 | 740 (0.7) | 98 (13.2) | 563 (0.6) | 85 (15.1) |
| Sweden; NH; M; Low; 85+ | 875 (0.8) | 125 (14.3) | 622 (0.6) | 100 (16.1) |
| Sweden; NH; W; High; 65-84 | 1060 (1.0) | 192 (18.1) | 965 (1.0) | 181 (18.8) |
| Sweden; NH; W; High; 85+ | 3157 (2.9) | 543 (17.2) | 2654 (2.7) | 517 (19.5) |
| Sweden; NH; W; Medium; 65-84 | 1974 (1.8) | 353 (17.9) | 1409 (1.5) | 264 (18.7) |
| Sweden; NH; W; Medium; 85+ | 5599 (5.2) | 1023 (18.3) | 3733 (3.9) | 733 (19.6) |
| Sweden; NH; W; Low; 65-84 | 1843 (1.7) | 317 (17.2) | 1428 (1.5) | 286 (20.0) |
| Sweden; NH; W; Low; 85+ | 6173 (5.7) | 1045 (16.9) | 4013 (4.1) | 771 (19.2) |
| Other; OR; M; High; 65-84 | 569 (0.5) | 66 (11.6) | 545 (0.6) | 57 (10.5) |
| Other; OR; M; High; 85+ | 426 (0.4) | 49 (11.5) | 476 (0.5) | 55 (11.6) |
| Other; OR; M; Medium; 65-84 | 428 (0.4) | 67 (15.7) | 365 (0.4) | 45 (12.3) |
| Other; OR; M; Medium; 85+ | 259 (0.2) | 33 (12.7) | 244 (0.3) | 38 (15.6) |
| Other; OR; M; Low; 65-84 | 819 (0.8) | 168 (20.5) | 783 (0.8) | 144 (18.4) |
| Other; OR; M; Low; 85+ | 344 (0.3) | 54 (15.7) | 349 (0.4) | 60 (17.2) |
| Other; OR; W; High; 65-84 | 425 (0.4) | 60 (14.1) | 456 (0.5) | 67 (14.7) |
| Other; OR; W; High; 85+ | 603 (0.6) | 102 (16.9) | 579 (0.6) | 89 (15.4) |
| Other; OR; W; Medium; 65-84 | 983 (0.9) | 189 (19.2) | 875 (0.9) | 172 (19.7) |
| Other; OR; W; Medium; 85+ | 1031 (0.9) | 240 (23.3) | 942 (1.0) | 200 (21.2) |
| Other; OR; W; Low; 65-84 | 1960 (1.8) | 417 (21.3) | 1802 (1.9) | 370 (20.5) |
| Other; OR; W; Low; 85+ | 1532 (1.4) | 297 (19.4) | 1430 (1.5) | 270 (18.9) |
| Other; NH; M; High; 65-84 | 167 (0.2) | 30 (18.0) | 151 (0.2) | 32 (21.2) |
| Other; NH; M; High; 85+ | 169 (0.2) | 31 (18.3) | 137 (0.1) | 30 (21.9) |
| Other; NH; M; Medium; 65-84 | 147 (0.1) | 28 (19.0) | 118 (0.1) | 29 (24.6) |
| Other; NH; M; Medium; 85+ | 159 (0.1) | 28 (17.6) | 104 (0.1) | 25 (24.0) |
| Other; NH; M; Low; 65-84 | 164 (0.2) | 39 (23.8) | 135 (0.1) | 32 (23.7) |
| Other; NH; M; Low; 85+ | 118 (0.1) | 30 (25.4) | 91 (0.1) | 21 (23.1) |
| Other; NH; W; High; 65-84 | 118 (0.1) | 19 (16.1) | 110 (0.1) | 25 (22.7) |
| Other; NH; W; High; 85+ | 281 (0.3) | 57 (20.3) | 246 (0.3) | 43 (17.5) |
| Other; NH; W; Medium; 65-84 | 272 (0.3) | 71 (26.1) | 197 (0.2) | 45 (22.8) |
| Other; NH; W; Medium; 85+ | 603 (0.6) | 142 (23.5) | 429 (0.4) | 114 (26.6) |
| Other; NH; W; Low; 65-84 | 387 (0.4) | 94 (24.3) | 288 (0.3) | 74 (25.7) |
| Other; NH; W; Low; 85+ | 745 (0.7) | 189 (25.4) | 561 (0.6) | 145 (25.8) |
*Country of birth (Sweden, Other); Residence (OR=Own residence, NH=Nursing home); Gender (M = Man, W=Woman); Education (Low, Medium, High); Age (65–84 years, 85+ years).
The inequalities in loneliness by intersectional strata, with adjusted analyses illustrated in Fig. 1 and unadjusted and adjusted reported in Supplementary Table S1, introduced nuances to the singular inequalities reported in Table 2. The largest inequalities in the risk of loneliness included, as expected, the most disadvantaged group (older, low-income, immigrant women in nursing homes; PD = 12.67pp in 2019 and 13.76pp in 2020 in adjusted models). Inequalities of similar magnitude (PD > 10pp in adjusted analyses) were however also seen, in both 2019 and 2020, for several other strata comprising immigrant nursing home residents with medium or low income, but also including medium- and low-income women living in their own residence.
Fig. 1.
Absolute inequalities in loneliness across intersectional strata among Swedish older adults in eldercare in 2019 (N = 108,607) and 2020 (N = 96,922), with younger Swedish-born men with high income in own residence as the reference stratum. Estimates are prevalence differences (PD) with 95% confidence intervals, adjusted for questionnaire form and respondent of questionnaire.
Moreover, despite the concentration of the highest prevalence of loneliness found in intersections of country of birth, income and residential setting, disadvantaged positions along these axes did not consistently entail a markedly high risk of loneliness. For example, certain strata of immigrants - men with high income in their own residence - did not report markedly higher risk of loneliness than did the multiply privileged group (<3pp in adjusted analyses). Moreover, the overall lower risk in low-income group that was suggested by the singular inequalities in Table 2 was seemingly isolated to the Swedish-born strata, while low-income strata of immigrants instead consistently displayed numerically higher prevalence of loneliness compared to their high-income counterpart (Fig. 1 and Supplementary Table S1).
When it comes to change of intersectional inequalities in loneliness from 2019 to 2020 in adjusted analyses, overall, the descriptive changes in strata-level inequalities tended toward increased or unchanged inequalities from 2019 to 2020 (see Fig. 2 and Supplementary Table S1). Specifically, 26 strata displayed a numerical increase >1pp, 15 strata displayed an insubstantial change <1pp (negative or positive), and only six strata showed a numerical decrease >1pp in the magnitude of the inequality. The largest descriptive increases were seen among strata comprising immigrants in nursing homes with medium or high income, but the low stratum-level sample sizes rendered these estimates uncertain. The between-year comparisons were thus only significant for seven larger strata, all including Swedish-born individuals; mostly diverse strata of nursing home residents (1.95–4.65pp increase), but also medium- and low-income men in their own residence (2.17–2.40pp increase) (Supplementary Table 1).
Fig. 2.

Change in absolute inequalities in loneliness from 2019 (N = 108,607) to 2020 (N = 96,922) for intersectional strata of Swedish older adults in eldercare. Estimates are prevalence differences (PD) reported as prevalence points (pp), with younger Swedish-born men with high income in own residence as the reference stratum, and adjusted for questionnaire form and respondent of questionnaire.
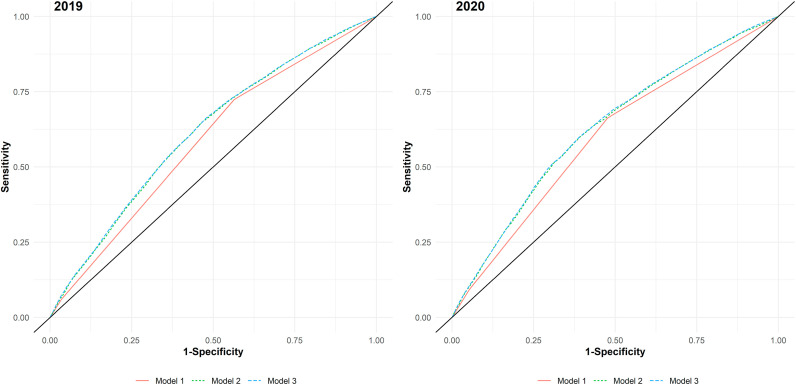
Discriminatory accuracy before and after the pandemic
In the next step, and corresponding to the third aim, the reported singular and intersectional inequalities in loneliness were examined from the point of discriminatory accuracy, with results summarized in Table 4 and with ROC curves displayed in Fig. 3 .
Table 4.
Discriminatory accuracy and model fit of models in 2019 (N = 108,607) and 2020 (N = 96,922). Estimates are reported as Area Under the Receiver Operating Characteristic Curve (AUC) and Akaike Information Criterion (AIC).
| Model and comparison | 2019 AUC | 2019 AIC | 2020 AUC | 2020 AIC |
|---|---|---|---|---|
| Model estimates | ||||
| Model 1: Covariates onlya | 0.5842 | 88044.55 | 0.5977 | 77033.01 |
| Model 2: Covariates + single dimensionsb | 0.6138 | 87471.48 | 0.6269 | 76474.95 |
| Model 3: Covariates + intersectional stratac | 0.6160 | 87448.96 | 0.6293 | 76447.29 |
| Model comparisons, within-year, ΔAUC (p) | ||||
| Model 2 vs Model 1 (ref), ΔAUC (p) | 0.0296d | 0.0292d | ||
| Model 3 vs Model 1 (ref), ΔAUC (p) | 0.0318d | 0.0316d | ||
| Model 3 vs Model 2 (ref), ΔAUC (p) | 0.0022d | 0.0024d | ||
| Model comparison, between-year | ||||
| Model 2 2020 vs 2019 (ref), ΔAUC (p) | Ref | 0.0131d | ||
| Model 3 2020 vs 2019 (ref), ΔAUC (p) | Ref | 0.0134d |
Model 1: Covariates only: questionnaire form (web/physical) and respondent of questionnaire (self/with assistance).
Model 2: Model 1 covariates + Country of birth; Residence; Gender; Education; Age.
Model 3: Model 1 covariates + 48 intersectional strata.
p < 0.001.
Fig. 3.
Received operating characteristics (ROC) curves among Swedish older adults in eldercare in models with only covariates (Model 1), covariates plus single inequality dimensions (Model 2) and covariates plus intersectional strata (Model 3), in 2019 (N = 108,607) and 2020 (N = 96,922).
The base model (Model 1) including only covariates indicated a low discriminatory accuracy, with AUC = 0.5842 in 2019 and AUC = 0.5977 in 2020. Discriminatory accuracy and model fit improved slightly but significantly after adding either the single dimensions of inequality (Model 2, AUC = 0.6269) or the intersectional strata (Model 3, AUC = 0.6293). Compared to the single dimension Model 2, discriminatory accuracy and model fit was marginally higher in the intersectional Model 3, in both 2019 (ΔAUC = 0.0022, p < 0.001) and 2020 (ΔAUC = 0.0024, p < 0.001). Comparing the discriminatory accuracy between the years, both the single dimension Model 2 (ΔAUC = 0.0131, p < 0.001) and intersectional Model 3 (ΔAUC = 0.0134, p < 0.001) were marginally but significantly larger in 2020 than in 2019. The same inferences were yielded in analyses excluding the covariates (data not shown).
Discussion
The present study demonstrated complex patterns of social inequality in loneliness before and during the early phase of COVID-19 pandemic among older adults in Swedish eldercare. First, when considering singular inequalities, we found that particularly country of birth and gender inequalities emerged as consistently important dimensions, but with increasing importance of residential inequalities during the pandemic. Second, when considering inequalities as intertwined, the highest risk of loneliness was found particularly in intersections of immigrants, nursing home residents, and those of lower income. However, surprisingly low levels of loneliness were also found in some strata, including Swedish-born strata with low income, and among immigrants in own residence and high income. Overall, these intersectional inequalities increased marginally but ubiquitously from before to during the pandemic. Third, the analyses of discriminatory accuracy suggested an added discriminatory value of intersectional above singular inequalities, and with a larger importance of both single-dimension and intersectional inequalities during, compared to before, the pandemic. Taken together, these findings illustrate the importance of complexity and contingency of multiple social positions for loneliness among older adults around the emergence of the COVID-19 pandemic.
The findings suggest that the risk of loneliness among older adults in eldercare is not merely a universal public health problem, but which instead is an experience distributed unequally along multiple and interdependent axes of inequality, even in the comparatively egalitarian context of Sweden. While our findings generally confirm prior findings of inequalities along age (Chawla et al., 2021), gender (Cohen-Mansfield et al., 2016; Pinquart and Sorensen, 2001), financial situation (Bosma et al., 2015; Niedzwiedz et al., 2016), migration background (Ten Kate et al., 2020) and residential setting (Ayalon, 2019; Freedman et al., 2021), this study highlights how the interdependence of these axes may be important to understand loneliness in the population of older adults. While the results overall conformed to a multiple jeopardy hypothesis, with greater risks among those of multiple disadvantages, certain dimensions, e.g., country of birth, were also overall more formative for the experience of loneliness than were others, e.g., age.
The overall patterns in the prevalence of loneliness appeared entrenched already before the emergence of the pandemic, and increased slightly but ubiquitously during its early phase, and specifically by residential setting. This differential impact, rooted in underlying social inequalities, expands previous findings of increased inequalities in loneliness by gender (Hansen et al., 2021) and in social contacts by residential setting (Freedman et al., 2021) during the pandemic. Taken together, it provides a complex picture of social vulnerability and resiliency among older adults, which stands in stark contrast to common depictions and empirical approaches treating older adults as one homogenous vulnerable group. A greater attention to such heterogeneity may be important to understand the overall small to moderate impact of the pandemic on older adults’ loneliness reported in previous research (Lebrasseur et al., 2021; Parlapani et al., 2021), as population-averages might conceal differential impact and also the deeply inequitable preconditions within the population group of older adults.
The analysis of discriminatory accuracy gives a complementary picture of the magnitude of the inequalities. The effect sizes of the discriminatory accuracy found in this study were consistently low to moderate, which suggests that universal interventions, i.e., targeting the entire population of older adults in eldercare, complemented with a smaller measure of targeted interventions to high-risk groups, e.g., immigrant nursing home residents, are likely to be the most effective strategy to prevent and address loneliness among older adults.
Methodological considerations
The strengths of the study include the large sample from a total population survey; the inclusion of the understudied target populations of the oldest old and nursing home residents; and the application and extension of novel and comprehensive analytical methods that are informed by theory and yield estimates of policy relevance.
The sampling frame included the total population of older adults in eldercare, including the understudied group of oldest old and nursing home residents. This is a considerable strength when it comes to generalizability of the results. Nevertheless, aspects of culture and organization of society and of health and social services can be expected to influence the configuration of inequalities in loneliness in any given context. Moreover, particularly during the early phase of the pandemic, the preconditions and pandemic responses varied considerably between countries. Caution and careful consideration should therefore be applied when generalizing the findings to corresponding populations in other contexts differing wildly from the Swedish one.
Relatedly, when it comes to selection bias, the 2019 and 2020 samples overall had a similar composition, except for the proportion of individuals in nursing homes, where 40% (2020) versus 50% (2019) of residents responded to the survey. Drop-out analysis (Socialstyrelsen, 2020) has showed similar participation rate for women and men but lower participation rate for younger respondents than for older. No information of the non-responders was accessible to the researchers for detailed analysis of the attrition, but it is likely that the sample is underrepresented when it comes to the frailest older adults, which is a common challenge in studies of the oldest old (Dahlberg, 2021). This underrepresentation is furthermore likely more pronounced in 2020, as the visiting ban in place limited aid from close ones to complete the questionnaire (Socialstyrelsen, 2020). Together with the high mortality in nursing homes during the first wave of the pandemic, survival bias could also influence the findings. This could lead to a differential underestimation of loneliness in 2020 among nursing home residents, and a corresponding underestimation of the residence-related inequalities in loneliness.
The study used a single-item measure of loneliness constructed for the purpose of this survey and which has not been evaluated psychometrically. Although it could be judged to possess acceptable face validity, its psychometric properties cannot be ascertained, which may possibly bias the finding in an unknown direction. When it comes to the inequality dimensions, all of them where crudely operationalized into two or three categories; and additionally, there are multitude of other potential inequality dimensions that were unavailable in the data (e.g., wealth, ethnic minority, sexual orientation, and functional variations). Nevertheless, despite the comparatively large sample in this study, the granularity and comprehensiveness of intersectional position that feasibly can be considered are limited in practice, as exemplified by the limited statistical power in the between-year stratum-level analyses of this study.
To avoid overadjustment of the estimation of the inequalities, only two design-related covariates were included as potential confounders (questionnaire form and respondent), in addition to the potential mutual confounding of the inequality dimensions which was taken into account analytically by mutual adjustment or cross-classification. In observational studies, there is always a risk for residual confounding which can bias the estimates, which is aggravated by the complexity of the underlying causal pathways of intersectional inequalities in health and health determinants. Residual confounding is therefore a remaining risk in the present study.
The use of discriminatory accuracy used in the study gives informative evidence for public health policy compared to traditional means-centric analyses focusing solely on group averages (Merlo, 2018). The judgement of what constitutes a high and low discriminatory accuracy in a public health context, beyond essentially arbitrary cut-offs and labels, and how such judgements should be translated into decisions about the balance of strategies at different levels of intervention, is however yet to be clarified. In making such judgements, it is important to consider that even small effects can have relevance when applied to the entire population, as well as the generally low discriminatory accuracy reported for cardiovascular risk factors that are well-established in clinical practice and guidelines (Merlo et al., 2017). Using the AUC as a measure of the magnitude or policy importance of social inequalities in health therefore necessitates a measured interpretation that considers both the population perspective and the range of discriminatory accuracy that reasonably can be expected in a public health context. Otherwise, social, and particularly intersectional, inequalities may be selectively interpreted as unimportant for public health policy, in comparison with research on other health determinants, which base the evidence on conventional means-centric methods.
Conclusions
The present study demonstrates complex social inequalities in loneliness among older adults in eldercare in Sweden, particularly in the intersection of country of birth, income, and residential setting. With the emergence of the COVID-19 pandemic, there was a slight but general widening of inequalities, and where nursing home residents emerged as a group hit particularly hard. Still, the results indicate that universal interventions should remain a core strategy when addressing loneliness among older adults before as well as during the pandemic. Taken together, the findings challenge simplified depictions of older adults, and instead illustrate an inherent heterogeneity when it comes to social vulnerability to and resilience against experience of loneliness among older adults before and during the pandemic, which is rooted in entrenched yet dynamic social inequalities. We hope that this study stimulates further research utilizing a nuanced and comprehensive equity lens to the experiences and risks of older adults in the peri-pandemic era.
Credit statement
Per E. Gustafsson: Conceptualization, Methodology, Data Curation, Investigation, Resources, Writing - Original Draft, Supervision, Project administration, Funding acquisition, Osvaldo Fonseca-Rodríguez: Methodology, Software, Validation, Formal analysis, Data Curation, Visualization, Writing - Review & Editing, Ingeborg Nilsson: Conceptualization, Writing - Review & Editing, Miguel San Sebastián: Conceptualization, Methodology, Data Curation, Writing - Review & Editing.
Acknowledgement
This work was supported by Forte– Swedish Research Council for Health, Working Life and Welfare to Per E Gustafsson (grant number 2020–01565) and by The Faculty of Medicine, Umeå University to Per E Gustafsson (grant number FS2.1.6-339-20).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.115447.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
The data that has been used is confidential.
References
- Agenor M. Future directions for incorporating intersectionality into quantitative population health research. Am. J. Publ. Health. 2020 doi: 10.2105/AJPH.2020.305610. e1-e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman D.G., Bland J.M. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson K., Kvist E. The neoliberal turn and the marketization of care: the transformation of eldercare in Sweden. Eur. J. Wom. Stud. 2015;22:274–287. doi: 10.1177/1350506814544912. [DOI] [Google Scholar]
- Axelsson Fisk S., Lindstrom M., Perez-Vicente R., Merlo J. Understanding the complexity of socioeconomic disparities in smoking prevalence in Sweden: a cross-sectional study applying intersectionality theory. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-042323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayalon L. Subjective social status as a predictor of loneliness: the moderating effect of the type of long-term care setting. Res. Aging. 2019;41:915–935. doi: 10.1177/0164027519871674. Artn 01640275198716741177/0164027519871674. [DOI] [PubMed] [Google Scholar]
- Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health. 2020 doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer G.R. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc. Sci. Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Bauer G.R., Scheim A.I. Methods for analytic intercategorical intersectionality in quantitative research: discrimination as a mediator of health inequalities. Soc. Sci. Med. 2019;226:236–245. doi: 10.1016/j.socscimed.2018.12.015. [DOI] [PubMed] [Google Scholar]
- Bosma H., Jansen M., Schefman S., Hajema K.J., Feron F. Lonely at the bottom: a cross-sectional study on being ill, poor, and lonely. Publ. Health. 2015;129:185–187. doi: 10.1016/j.puhe.2014.11.016. [DOI] [PubMed] [Google Scholar]
- Burstrom B. Sweden--Recent changes in welfare state arrangements. Int. J. Health Serv. 2015;45:87–104. doi: 10.2190/HS.45.1.g. [DOI] [PubMed] [Google Scholar]
- Caspari S., Raholm M.B., Saeteren B., Rehnsfeldt A., Lillesto B., Lohne V., et al. Tension between freedom and dependence - a challenge for residents who live in nursing homes. J. Clin. Nurs. 2018;27:4119–4127. doi: 10.1111/jocn.14561. [DOI] [PubMed] [Google Scholar]
- Chawla K., Kunonga T.P., Stow D., Barker R., Craig D., Hanratty B. Prevalence of loneliness amongst older people in high-income countries: a systematic review and meta-analysis. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield J., Hazan H., Lerman Y., Shalom V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int. Psychogeriatr. 2016;28:557–576. doi: 10.1017/S1041610215001532. [DOI] [PubMed] [Google Scholar]
- Crenshaw K. University of Chicago Legal Forum; 1989. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics; pp. 139–167. [Google Scholar]
- Dahlberg L. Loneliness during the COVID-19 pandemic. Aging Ment. Health. 2021;25:1161–1164. doi: 10.1080/13607863.2021.1875195. [DOI] [PubMed] [Google Scholar]
- Dahlberg L., Agahi N., Lennartsson C. Lonelier than ever? Loneliness of older people over two decades. Arch. Gerontol. Geriatr. 2018;75:96–103. doi: 10.1016/j.archger.2017.11.004. [DOI] [PubMed] [Google Scholar]
- Dahlberg L., McKee K.J., Frank A., Naseer M. A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment. Health. 2022;26:225–249. doi: 10.1080/13607863.2021.1876638. [DOI] [PubMed] [Google Scholar]
- DeLong E.R., DeLong D.M., Clarke-Pearson D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- Dyer C. Covid-19: care home residents in England should have "safe spaces" for visits from family and friends, says guidance. BMJ. 2020;371 doi: 10.1136/bmj.m4302. [DOI] [PubMed] [Google Scholar]
- Freedman V.A., Hu M., Kasper J.D. Changes in older adults' social contact during the COVID-19 pandemic. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021 doi: 10.1093/geronb/gbab166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fristedt S., Carlsson G., Kylen M., Jonsson O., Granbom M. Changes in daily life and wellbeing in adults, 70 years and older, in the beginning of the COVID-19 pandemic. Scand. J. Occup. Ther. 2021:1–11. doi: 10.1080/11038128.2021.1933171. [DOI] [PubMed] [Google Scholar]
- Gardiner C., Laud P., Heaton T., Gott M. What is the prevalence of loneliness amongst older people living in residential and nursing care homes? A systematic review and meta-analysis. Age Ageing. 2020;49:748–757. doi: 10.1093/ageing/afaa049. [DOI] [PubMed] [Google Scholar]
- Gustafsson P.E., Nilsson I., San Sebastian M. Venerable vulnerability or remarkable resilience? A prospective study of the impact of the first wave of the COVID-19 pandemic and quarantine measures on loneliness in Swedish older adults with home care. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-060209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson P.E., Schröders J., Nilsson I., San Sebastian M. Surviving through solitude: a prospective national study of the impact of the early COVID-19 pandemic and a visiting ban on loneliness among nursing home residents in Sweden. J. Gerontol. B Psychol. Sci. Soc. Sci. 2022 doi: 10.1093/geronb/gbac126. Accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen T., Kafkova M.P., Katz R., Lowenstein A., Naim S., Pavlidis G., et al. Exclusion from social relations in later life: micro- and macro-level patterns and correlations in a European perspective. Int. J. Environ. Res. Publ. Health. 2021;18 doi: 10.3390/ijerph182312418. ARTN 124183390/ijerph182312418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer D.W., Lemeshow S., Sturdivant R.X. Chicester; 2013. Applied Logistic Regression. [Google Scholar]
- Kivi M., Hansson I., Bjalkebring P. Up and about: older adults' well-being during the COVID-19 pandemic in a Swedish longitudinal study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76:e4–e9. doi: 10.1093/geronb/gbaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebrasseur A., Fortin-Bedard N., Lettre J., Raymond E., Bussieres E.L., Lapierre N., et al. Impact of the COVID-19 pandemic on older adults: rapid review. JMIR Aging. 2021;4 doi: 10.2196/26474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lood Q., Haak M., Dahlin-Ivanoff S. Everyday life in a Swedish nursing home during the COVID-19 pandemic: a qualitative interview study with persons 85 to 100 years. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-048503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada-Baltar A., Martinez-Huertas J.A., Jimenez-Gonzalo L., Pedroso-Chaparro M.D.S., Gallego-Alberto L., Fernandes-Pires J., et al. Longitudinal correlates of loneliness and psychological distress during the lockdown situation due to COVID-19. Effects of age and self-perceptions of aging. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021 doi: 10.1093/geronb/gbab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludvigsson J.F. The first eight months of Sweden's COVID-19 strategy and the key actions and actors that were involved. Acta Paediatr. 2020;109:2459–2471. doi: 10.1111/apa.15582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M., Allen J. COVID-19: exposing and amplifying inequalities. J. Epidemiol. Community Health. 2020;74:681–682. doi: 10.1136/jech-2020-214720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall L. The complexity of intersectionality. Signs. 2005;30:1771–1800. [Google Scholar]
- Merlo J. Multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA) within an intersectional framework. Soc. Sci. Med. 2018;203:74–80. doi: 10.1016/j.socscimed.2017.12.026. [DOI] [PubMed] [Google Scholar]
- Merlo J., Mulinari S., Wemrell M., Subramanian S.V., Hedblad B. The tyranny of the averages and the indiscriminate use of risk factors in public health: the case of coronary heart disease. SSM - Population Health. 2017;3:684–698. doi: 10.1016/j.ssmph.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzwiedz C.L., Richardson E.A., Tunstall H., Shortt N.K., Mitchell R.J., Pearce J.R. The relationship between wealth and loneliness among older people across Europe: is social participation protective? Prev. Med. 2016;91:24–31. doi: 10.1016/j.ypmed.2016.07.016. [DOI] [PubMed] [Google Scholar]
- Olofsson J., Ramgard M., Sjogren-Forss K., Bramhagen A.C. Older migrants' experience of existential loneliness. Nurs. Ethics. 2021;28:1183–1193. doi: 10.1177/0969733021994167. Artn 0969733021994167177/0969733021994167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H.J., Morgan T., Wiles J., Gott M. Lonely ageing in a foreign land: social isolation and loneliness among older Asian migrants in New Zealand. Health Soc. Care Community. 2019;27:740–747. doi: 10.1111/hsc.12690. [DOI] [PubMed] [Google Scholar]
- Parlapani E., Holeva V., Nikopoulou V.A., Kaprinis S., Nouskas I., Diakogiannis I. A review on the COVID-19-related psychological impact on older adults: vulnerable or not? Aging Clin. Exp. Res. 2021;33:1729–1743. doi: 10.1007/s40520-021-01873-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pentaris P., Willis P., Ray M., Deusdad B., Lonbay S., Niemi M., et al. Older people in the context of COVID-19: a European perspective. J. Gerontol. Soc. Work. 2020;63:736–742. doi: 10.1080/01634372.2020.1821143. [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sorensen S. Influences on loneliness in older adults: a meta-analysis. Basic Appl. Soc. Psychol. 2001;23:245–266. doi: 10.1207/S15324834basp2304_2. [DOI] [Google Scholar]
- Prochazka M. Socialstyrelsen; Stockholm: 2021. Vård Och Omsorg För Äldre – Lägesrapport 2021 [Elderly Care - Status Report 2021] [Google Scholar]
- Raphael D. Challenges to promoting health in the modern welfare state: the case of the Nordic nations. Scand. J. Publ. Health. 2014;42:7–17. doi: 10.1177/1403494813506522. [DOI] [PubMed] [Google Scholar]
- Richman L.S., Zucker A.N. Quantifying intersectionality: an important advancement for health inequality research. Soc. Sci. Med. 2019;226:246–248. doi: 10.1016/j.socscimed.2019.01.036. [DOI] [PubMed] [Google Scholar]
- Rogers W.A., Ramadhani W.A., Harris M.T. Defining aging in place: the intersectionality of space, person, and time. Innovation in Aging. 2020;4(36) doi: 10.1093/geroni/igaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandgren A., Arnoldsson L., Lagerholm A., Bokberg C. Quality of life among frail older persons (65+ years) in nursing homes: a cross-sectional study. Nursing Open. 2021;8:1232–1242. doi: 10.1002/nop2.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert A., Cotten S.R., Xie B. A double burden of exclusion? Digital and social exclusion of older adults in times of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76:e99–e103. doi: 10.1093/geronb/gbaa098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin O., Park S., Amano T., Kwon E., Kim B. Nature of retirement and loneliness: the moderating roles of social support. J. Appl. Gerontol. 2020;39:1292–1302. doi: 10.1177/0733464819886262. [DOI] [PubMed] [Google Scholar]
- Socialstyrelsen Metodbeskrivning 2020. Vad tycker de äldre om äldreomsorgen? [Description of methods 2020. What do the elderly think about the elderly care?] Socialstyrelsen. 2020 [Google Scholar]
- Socialstyrelsen . Sveriges officiella statistik; Stockholm: 2021. Statistik Om Socialtjänstinsatser till Äldre 2020 [Statistics about Social Service Provision to Elderly 2020] (Socialstyrelsen) [Google Scholar]
- Szebehely M., Meagher G. Nordic eldercare - weak universalism becoming weaker? J. Eur. Soc. Pol. 2018;28:294–308. doi: 10.1177/0958928717735062. [DOI] [Google Scholar]
- Ten Kate R.L.F., Bilecen B., Steverink N. A closer look at loneliness: why do first-generation migrants feel more lonely than their native Dutch counterparts? Gerontol. 2020;60:291–301. doi: 10.1093/geront/gnz192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wemrell M., Karlsson N., Perez Vicente R., Merlo J. An intersectional analysis providing more precise information on inequities in self-rated health. Int. J. Equity Health. 2021;20:54. doi: 10.1186/s12939-020-01368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wemrell M., Lenander C., Hansson K., Perez R.V., Hedin K., Merlo J. Socio-economic disparities in the dispensation of antibiotics in Sweden 2016-2017: an intersectional analysis of individual heterogeneity and discriminatory accuracy. Scand. J. Publ. Health. 2021;1403494820981496 doi: 10.1177/1403494820981496. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.