Abstract
With the large-scale use of antibiotics, antibiotic resistant bacteria (ARB) continue to rise, and antibiotic resistance genes (ARGs) are regarded as emerging environmental pollutants. The new tetracycline-class antibiotic, tigecycline is the last resort for treating multidrug-resistant (MDR) bacteria. Plasmid-mediated horizontal transfer enables the sharing of genetic information among different bacteria. The tigecycline resistance gene tet(X) threatens the efficacy of tigecycline, and the adjacent ISCR2 or IS26 are often detected upstream and downstream of the tet(X) gene, which may play a crucial driving role in the transmission of the tet(X) gene. Since the first discovery of the plasmid-mediated high-level tigecycline resistance gene tet(X4) in China in 2019, the tet(X) genes, especially tet(X4), have been reported within various reservoirs worldwide, such as ducks, geese, migratory birds, chickens, pigs, cattle, aquatic animals, agricultural field, meat, and humans. Further, our current researches also mentioned viruses as novel environmental reservoirs of antibiotic resistance, which will probably become a focus of studying the transmission of ARGs. Overall, this article mainly aims to discuss the current status of plasmid-mediated transmission of different tet(X) genes, in particular tet(X4), as environmental pollutants, which will risk to public health for the “One Health” concept.
Keywords: antibiotic resistant bacteria, tigecycline resistance gene, plasmid-mediated, tet(X4), transmission, one health
Introduction
The discovery of antibiotics is a milestone event in human medicine. With the large-scale use of antibiotics, while reducing the morbidity and mortality of bacterial infections, strains carrying different antibiotic resistance genes (ARGs) appeared and spread rapidly (Davies and Davies, 2010; Ahmad and Khan, 2019). The global sales of antimicrobials are estimated to reach 104,079 tons in 2030, an increase of 11.5% since 2017 (Tiseo et al., 2020). Antimicrobial resistance (AMR) is one of the public health issues of widely concern around the world, and ARGs are regarded as new environmental pollutants (Plantinga et al., 2015; Zhang et al., 2020c).Tetracycline have many desirable properties of antibiotics, such as their excellent anti-bacterial activity and oral benefits. They have been widely used in the treatment of human and animal infections or as animal growth-promoting feed additives (Roberts, 2003). However, only a small part of tetracycline can be absorbed after entering the body, and more than 75% of tetracycline will be excreted in the form of a prototype or metabolite (Liao et al., 2021).
Tigecycline belonged to tetracycline-class drugs, is a new class of glycylcycline antibiotics, approved by the FDA in 2005 (Wenzel et al., 2005; Stein and Babinchak, 2013; Hirabayashi et al., 2021). It has broad-spectrum anti-bacterial activity, especially against multidrug-resistant (MDR) gram-negative bacteria (Zha et al., 2020). Tigecycline is also considered as a drug of last resort to combat bacterial infections, and which is mainly used for the treatment of infections within skin tissue, anti-tumor, bacterial pneumonia, and complex intra-abdominal (Olson et al., 2006; Kaewpoowat and Ostrosky-Zeichner, 2015; Zhao et al., 2021). Furthermore, it is a third-generation tetracycline-class antibiotic, which was improved by adding a 9-tert-butyl-glycylamido side-chain modification structure to the central framework of minocycline, and thereby forming a steric hindrance, overcoming normal mechanisms of resistance to tetracyclines, such as parts of the efflux pump mechanism[tet(A-E), tet(K)] and ribosome protection mechanism[tet(M)] (Chopra, 2002; Livermore, 2005; Linkevicius et al., 2016). Tigecycline can act on bacterial ribosomes and inhibit bacterial protein synthesis by interfering with aminoacyl-tRNA binding to ribosomes (Chopra and Roberts, 2001). We have gathered, appraised, and reviewed the accessible relevant literature from online sources, including Science Direct, PubMed, and Google Scholar. The keywords were included but not limited to tet(X) genes, Escherichia coli (E. coli), ISCR2, IS26, antibiotic resistant bacteria (ARB), AMR, ARGs, MDR, plasmids, environmental pollutants, public health, resistance contact, clinical and veterinary settings. Moreover, the cited references were also explored for further referencing. This article summarized the mechanisms of tigecycline resistance and the prevalence of the plasmid-mediated high-level tigecycline resistance gene tet(X4) among the environment, animals, and humans. In addition, the origin of the tet(X) and the importance of mobile genetic elements (MGEs) during the dissemination of the tet(X) are discussed. The purpose of this article is to collect and organize the information available so far in one platform, and to provide a bridge for readers to understand that the prevalence of plasmid-mediated high-level tigecycline resistance genes, which can contaminate the natural environment, and further risking to public health. Moreover, we also made a positive outlook for the transmission of ARGs by viruses.
Mechanism of tigecycline resistance
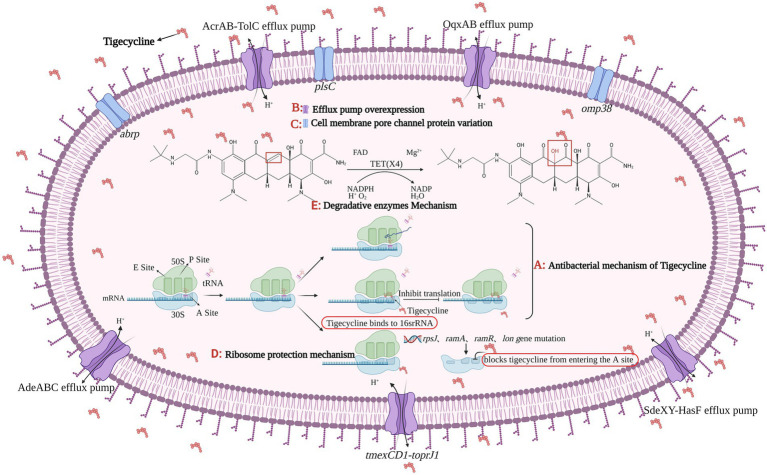
At present, the main mechanisms of bacterial resistance to tigecycline are efflux pump mechanism, cell membrane pore channel protein variation, ribosome protection mechanism, and drug-degrading enzyme mechanism (Figure 1).
Figure 1.
The figure was created with “BioRender.com” showing antibacterial mechanism and drug resistance mechanism of Tigecycline. (A) Tigecycline can act on bacterial ribosomes. After entering bacteria, tigecycline reversibly binds to the 16S rRNA in the 30S subunit of the ribosome, preventing tRNA from entering the A site, which eventually inhibits the process of transcription and translation in protein synthesis. There are four main tigecycline resistance mechanisms: (B) efflux pump overexpression; (C) cell membrane porin mutation; (D) ribosomal protection and (E) degrading enzyme mechanism. Among them, the expression product of plasmid-mediated tet(X4) gene belongs to the core member of degradative enzyme mechanism, and the Tet(X4) can catalyze the selective hydroxylation of tigecycline in the presence of FAD, Mg2+, O2 and NADPH, thus making tigecycline ineffective.
Efflux pump mechanism
An active efflux pump is a protein transport system of bacteria, it can excrete antibiotics entering the bacteria from itself, reducing antibiotic concentration in bacteria, so as to promote the growth of ARB (Venter et al., 2015; Bankan et al., 2021). There are five main efflux pump families involved in the active efflux of antibiotics, one is the ATP binding cassette (ABC) superfamily, which is the “primary active” transporter that directly uses ATP binding and hydrolysis to drive the free efflux of drugs (Rempel et al., 2019). The other four families are secondary active transport proteins, which are energy-acquiring transporters with proton pumps, including the major facilitator super (MFS) family, multidrug and toxic compound extrusion (MATE) family, small multidrug resistance (SMR) family, and resistance modulation division (RND) superfamily (Kumar et al., 2016; Lamut et al., 2019). In Gram-negative bacteria, overexpression of MFS family and RND family efflux pumps plays a significant role in tigecycline resistance, such as Tet(A), AcrAB-TolC, OqxAB, and AdeABC (Ruzin et al., 2007; Zhong et al., 2014; Chen et al., 2017), Tet(A) and AcrAB-TolC efflux pumps have been studied relatively comprehensively (Munita and Arias, 2016), their coding genes can be located on chromosomes or plasmids and can be transmitted via plasmids or transposons (Sheykhsaran et al., 2019). As a tetracycline efflux pump gene, tet(A) has no effect on tigecycline sensitivity (Fluit et al., 2005), but studies showed the double frameshift mutation of tet(A) can make strains resistant to tigecycline at a low level (Hentschke et al., 2010; Akiyama et al., 2013). A new RND type efflux pump gene cluster, named tmexCD1-toprJ1, was first identified in Klebsiella pneumoniae (K. pneumonia) in 2020. TmexCD1-toprJ1 is widely present in K. pneumoniae, leading to a 4–32 fold increase in the minimal inhibitory concentration (MIC) of K. pneumoniae to tigecycline and eravacycline (Lv L. et al., 2020).
Cell membrane porin variation
The 1-acyl-3-glycerol phosphatidyl transferase encoded by the plsC gene is located on the cell membrane of E. coli, and its primary function is to catalyze the synthesis of phospholipids, and then participate in the biosynthesis of bacterial cell membranes (Lu et al., 2005). By inducing Acinetobacter baumannii (A. baumannii) to be resistant to tigecycline, the researchers performed whole-genome sequencing analysis of the strains before and after induction, and found three factors that could reduce the sensitivity of tigecycline, which were the frameshift mutation of plsC and omp38 as well as SNP synonymous mutation (Li et al., 2015). A new abrp gene was found in A. baumannii, which encodes the C13 family of peptidases and makes the bacteria less sensitive to tigecycline (Li et al., 2016).
Ribosome protection mechanisms
The rpsJ gene can encode the production of the ribosomal structural protein S10. When there is a 12 bp deletion in rpsJ, the amino acid Rath at positions 53–56 of the S10 protein will be removed, resulting in a change in the binding site of tigecycline and bacteria, making bacteria resistant to tigecycline (Beabout et al., 2015; Bender et al., 2020). In addition to the S10 protein, mutations in the S3 and S13 proteins can also make bacteria resistant to tigecycline (Lupien et al., 2015). In K. pneumoniae, mutations in the ramR operon, ramA, lon, and rpsJ genes result in decreasing bacterial sensitivity to tigecycline (Fang et al., 2016). Mutation of rpsJ in Enterococci also leads to resistance to tigecycline (Cattoir et al., 2015). Mutations in the rff, ropB and adeS genes in A. baumannii can affect the normal function of the ribosome and thus confer tigecycline resistance to the strain (Hua et al., 2021).
Mechanism of drug enzymatic degradation
Tet(X) is a FAD-dependent monooxygenase that regioselectively hydroxylates tetracycline substrates, leading to the non-enzymatic breakdown of an unstable compound (Ghosh et al., 2015). Tet(X) can only produce effect in the presence of FAD, NADPH, Mg2+, and O2 at the same time (Moore et al., 2005). Researchers proved that tigecycline was a substrate of Tet(X) by X-ray crystallography (Volkers et al., 2011), and in fact, Tet(X) can effectively degrade almost all tetracycline antibiotics, making bacteria resistant to tetracycline (Ghosh et al., 2015; Xu et al., 2022). Tet(X) gene was originally isolated from the anaerobic bacteria Bacteroides fragilis (Speer et al., 1991), however, according to recent reports, tet(X) appeared in Riemerella anatipestifer (R. anatipestifer) as early as the 1860s (Zhang et al., 2021a). In 2004, the tet(X) gene and its variant tet(X2) were discovered in anaerobic Bacteroides, then pointing out Tet(X) can degrade tigecycline, although it showed low levels of resistance to tigecycline, this phenomenon would still exist when tet(X) was transferred into E. coli (Guiney et al., 1984; Yang et al., 2004). Various tet(X) gene variants mediate different levels of tigecycline resistance. Compared with the Tet(X-X7), the enzymatic activity of the Tet(X4) has increased significantly. Researchers found five key residues (H231, M372, E43, R114, D308) could affect Tet(X4) enzyme activity in the tetracycline and FAD binding regions of the Tet(X4) (Xu et al., 2019). Subsequently, a new study has identified five mutants (L282S, A339T, D340N, V350I and K351E) in the structural domain of Tet(X2) when compared to Tet(X4), and demonstrated that the MIC of tigecycline increased 2–8 folds, when these five amino acid residues were mutated in the Tet(X2)-producing strain (Cui et al., 2021).
The plasmid-mediated tigecycline resistance genes tet(X3) and tet(X4) were first isolated from animal samples in 2019, which mediate high levels of antibiotic resistance to tigecycline, the MIC value can reach 32–64 mg/l (He et al., 2019). Tet(X4) is most commonly found in mobile plasmids and occasionally in chromosomes (Sun J. et al., 2019, 2020; Li et al., 2020b). Since the report of tet(X3/4), the degradative enzyme mechanism has gained more and more attention (He et al., 2019; Xu et al., 2022). At present, bismuth drugs and plumbagin can be used as Tet(X) inhibitors to improve the sensitivity of strains to tigecycline, which provides a new therapeutic strategy for the treatment of tigecycline-resistant bacterial infections (Deng et al., 2022; Xu et al., 2022).
Origin and spread of tet(X4)
Although, the tet(X) gene was first isolated from the anaerobic Bacteroidetes, the current study points the origin of the tet(X) to R. anatipestifer, the tet(X) and its variants share the same ancestry with the monooxygenase gene carried in the chromosomes of Flavobacteriaceae bacteria. In Zhu’s study, 170 of 212 strains of R. anatipestifer carried the tet(X) gene (Zhu et al., 2018). Among 6,692 strains isolated from 13 different hospitals, almost all of the tet(X)-positive strains belonged to the Flavobacteriaceae. They then performed a phylogenetic analysis of the different evolutionary patterns of tet(X), in which one of the pathways involving the Flavobacteriaceae produced a major evolutionary branch, suggesting that it can be considered as the potential ancestral source of tet(X) (Zhang et al., 2020a). Umar et al. collect 57 non-repetitive sequences of R. anatipestifer in GenBank, of which tet(X) gene was detected in 47 genomes, and they have high similarity when compared with tet(X4) gene (Umar et al., 2021). The same finding was also reported in other study (Cui et al., 2021). When analyzing the evolutionary trajectory of the tet(X) gene, they found that most of the tet(X)-positive strains belonged to the Flavobacteriaceae, it has a higher detection rate than other species and is widely distributed in different clades of tet(X). Their latest study also inferred that the tet(X) gene originated in Flavobacteriaceae and can be transmitted to environmental and clinical strains such as E. coli and Acinetobacter with the help of the mobilization of ISCR2 element (Chen et al., 2020).
The MGE such as ISCR2 and IS26 are essential for the spread of tet(X) gene. A 4608 bp element consisting of an ISCR2, a tet(X4) and a partner gene catD forms a canonical RC transposable unit (RC-TU) mediated by ISCR2, of which the 2,760 bp element of catD-tet(X4) is highly conserved. When transposition occurs, the ISCR2-catD-tet(X4)-ISCR2 composite transposon structure is often generated, and the upstream or downstream of ISCR2 element may be inserted and truncated by other IS elements, such as IS26 (Chen et al., 2021; Liu et al., 2022). In addition, only single-copy ISCR2 elements was sufficient to transpose adjacent DNA sequences through the process of rolling circle transposition (Poirel et al., 2009; Partridge et al., 2018). IS26 was also often found in plasmids resistant to antibiotics, and it can participate in the progress of plasmid fusion and gene recombination (He et al., 2015; Du et al., 2020; Li et al., 2020b), and IS26 can also be inserted into both ends of RC-TU, allowing ISCR2 residues-tet(X4) to spread through a novel transmission mechanism (Liu et al., 2022). It has been found that the ISCR2 element is frequent adjacent to tet(X4) or other tet(X) variants, which suggests ISCR2 is more likely to participate in spread of tet(X) variants (Wang L. et al., 2019; Liu et al., 2020; Fu et al., 2021). In a conserved genetic environment and uncertain transferability among different bacteria, the co-action of ISCR2 and IS26 may be the main driving forces for the widespread of tet(X4; Dai et al., 2022; Zhang et al., 2022).
Prevalence of tet(X4)
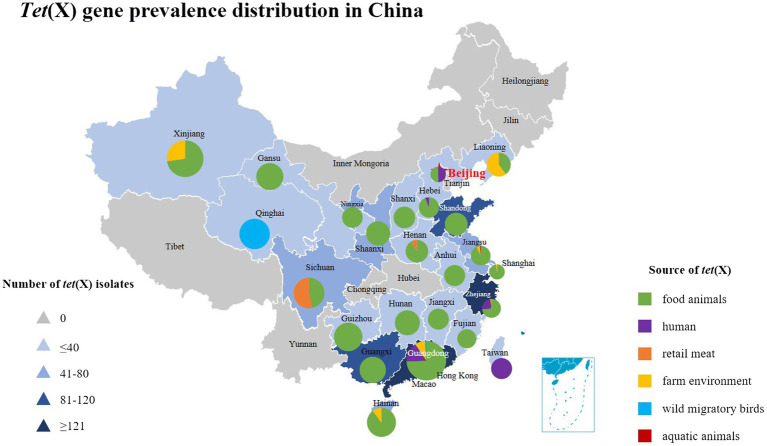
Tetracycline resistance genes speculated to be of environmental origin but are now widely distributed in commensal and pathogenic bacteria (Thaker et al., 2010). The extensive use of first or second-generation tetracycline-class drugs played a major role in the emergance of tetracycline resistance genes, especially oxytetracycline, chlortetracycline, and doxycycline (Aminov, 2021). Since the discovery of the plasmid-mediated high-level tigecycline resistance genes tet(X3/X4) in 2019, reports of tet(X) have gradually increased around the world (Table 1). Tet(X4)-positive strains have spread globally and have been detected in animals, humans and the environment, which largely limited the use of tigecycline (Xu et al., 2022). The tet(X) gene and its variants were present in 23 countries on six continents (Pan et al., 2020; Wang J. et al., 2021), which are also widely present in various bacterial species, including R. anatipestifer, E. coli, Acinetobacter, K. pneumoniae, Salmonella, Proteus, La Providencia bacteria, Bacteroides bacteria, Pseudomonas bacteria, and Aeromonas caviae (Chen et al., 2019a, 2020). Moreover, most of the tet(X4) genes are located on different types of plasmids such as IncQ1, IncX1, IncFIB, IncHI1, F-:A18:B-, ColE2-like, IncN, p0111 and hybrid plasmids (Fang et al., 2020), among which the IncX1 type is the most common (Cai et al., 2021; Cui et al., 2022). The Nomenclature Center1 recommends that only tet(X) will be used in the future, because the tet(X) gene variant DNA similarity is in the range of 83–100% among tet(X2)-tet(X14), corresponding amino acid similarity is between 82 and 100%, which is greater than the standard of 79% amino acid similarity. In this article, for the convenience of description, the previous classification method is still used. This article also summarizes the prevalence of tet(X) gene and its variants in China in recent years as shown in Figure 2.
Table 1.
Global prevalence of different tet(X) genes in recent years.
| Province/Country | Years of samples | Source (Reference or NCBI database) | Sample sources | Tet(X) types | Localization of gene | Plasmid types | Sequence types | Tet(X)-positive isolates | ESBLs/mcr genes | Bacterial strains |
|---|---|---|---|---|---|---|---|---|---|---|
| Sichuan | 2018–2020 | (Bai et al., 2019; Sun C. et al., 2019, 2020; Li et al., 2021a; Tang et al., 2021; Feng et al., 2022) | Food animals | tet(X4) | Plasmid | IncQ1-IncY IncX1 |
ST48, ST4541, ST9772, ST972, ST410, ST10, ST195, ST3696, ST25, ST196 | 27 |
cfr
mcr-1 bla TEM-1B |
E. coli
Citrobacter freundii |
| (Li, 2020a; Lv H. et al., 2020; Sun et al., 2021b) | Retail meat | tet(X4) | Plasmid | IncFIA-IncHI1A-IncHI1B IncX1 | ST4656, ST1788, ST871, ST48, ST1638, ST542, ST877, ST641, ST10, ST3858, ST195, ST515 | 31 |
blaNDM-5
blaSHV-12 blaCTX-M-55 blaCTX-M-14 |
E. coli | ||
| Guangdong | 2016–2019 | (He et al., 2019; Sun C. et al., 2019,Sun J. et al., 2019; Chen et al., 2020; Cheng et al., 2020; Cui et al., 2020; Sun et al., 2020; Zheng et al., 2020; Chen et al., 2021; Li et al., 2021a; Yu et al., 2021; Wu et al., 2022) | Food animals |
tet(X/X2) tet(X3) tet(X4) tet(X5) tet(X6) tet(X14) |
Plasmid Chromosome |
IncFIA-IncHI1A-IncHI1B | ST4535, ST10, ST23, ST215, ST206, ST789, ST1196, ST2144, ST195, ST101, ST109, ST789, ST2064, ST980, ST355, ST542, ST8302 | 236 |
blaTEM-1B
blaNDM-1 blaOXA-58 |
E. coli
Acinetobacter Citrobacter freundii Enterococcus faecalis Enterobacter cloacae |
| (Chen et al., 2019a; Cui et al., 2020; Sun et al., 2020; Wang Y. et al., 2020; Zheng et al., 2020; Chen et al., 2021; Yu et al., 2021; Gao et al., 2022) | Farm environment |
tet(X) tet(X3) tet(X4) tet(X6) |
Plasmid Chromosome |
IncFIA-IncHI1A–IncHI1B | ST645, ST10, ST37 | 28 |
bla
SHV-81 bla SHV-110 |
Acinetobacter
E. coli K. pneumoniae Aeromonas cavive |
||
| (Chen et al., 2019b) | Wild migratory birds | tet(X4) | Plasmid Chromosome |
F-:A18:B- IncHI1 |
ST1196, ST6833, ST641 | 3 | – | E. coli | ||
| (Chen et al., 2020; Wang Y. et al., 2020; Cui et al., 2022) | Human |
tet(X3) tet(X4) |
Plasmid | IncX1, IncFIA, IncHIA, IncHIB | ST10, ST48, ST877, ST2144, ST101, ST515, ST542, ST871, ST4456, ST38, ST137, ST201, ST7176, ST10548, ST6984, ST46, ST1249, ST195, ST155, ST58, ST4014, ST7686, ST1114, ST7450, ST1684 | 51 |
mcr-5.2 blaNDM blaOXA blaTEM blaSHV blaCTX-M |
E. coli
Acinetobacter |
||
| Jiangsu | 2015–2020 | (He et al., 2019; Sun J. et al., 2019; Chen et al., 2020; Peng et al., 2020; Li et al., 2020b; He T. et al., 2020; Li et al., 2020c; Yu et al., 2021; Cheng et al., 2021a; Li et al., 2021b) | Food animals |
tet(X3) tet(X4) tet(X6) tet(X15) |
Plasmid Chromosome |
IncHI1, IncFIB(K), IncX1, IncA/C2 | ST3997, ST284, ST93, ST1286, ST155, ST327, ST1459, ST48, ST3944, ST10170, ST8302 | 137 |
blaCTX-M cfr blaNDM-1 blaTEM − 1B |
E. coli
Acinetobacter Proteus Citrobacter freundii Providencia |
| (Li et al., 2020b; Yu et al., 2021) | Farm environment | tet(X4) | Plasmid | – | – | 21 | – | E. coli | ||
| (Li et al., 2019) | Aquatic animal | tet(X2/3.2) | Plasmid | – | – | 1 | – | Brevibacterium brevis | ||
| Shanghai | 2015–2019 | (Chen et al., 2020; Sun et al., 2020; Wang J. et al., 2020; Li et al., 2021a; Wang J. et al., 2021) | Food animals |
tet(X) tet(X3) tet(X) |
Plasmid | IncFIA18-IncFIB(K)-IncX1 IncX1, IncQ |
ST761, ST165, ST195, ST295, ST2144 | 41 | bla OXA-58 |
E. coli
Acinetobacter K. pneumoniae |
| (Wang J. et al., 2021) | Farm environment | tet(X) | Chromosome | – | – | 1 | – | Proteus | ||
| Henan | 2013–2019 | (Sun C. et al., 2019, 2020; Li et al., 2020d; Li et al., 2021a) | Food animals |
tet(X4) tet(X6) |
Plasmid Chromosome |
IncX1 IncFIA-IncFIB(K)-IncX1 |
ST10, ST48, ST641, ST2345 | 11 | mcr-1 | E. coli |
| (He D. et al., 2020) | Retail meat | tet(X6) | – | – | – | 1 | – | Proteus | ||
| Hebei | 2019 | (Li et al., 2021a) | Food animals | tet(X4) | Plasmid | IncX1, IncQ, IncFIA-IncHI1A-IncHI1B | ST48, ST10, ST4156, ST195, ST6833, ST515, ST2064, ST58 | 16 | – |
E. coli
K. pneumoniae |
| 2017 | (Wang L. et al., 2019) | Human | tet(X5) | Plasmid | – | – | 1 | – | Acinetobacter | |
| Shandong | 2017–2019 | (Bai et al., 2019; He et al., 2019; Cui et al., 2020; Du et al., 2020; Liu et al., 2020; Li et al., 2021a; Yu et al., 2021) | Food animals |
tet(X/X2) tet(X3) tet(X4) tet(X6) |
Plasmid Chromosome |
IncFII, IncFIA-IncHI1B-IncHI1A | ST761, ST746, ST101, ST10, ST847 | 83 |
bla
TEM − 1B
bla CTX-M-55 |
Acinetobacter Myroides sp. E. coli K. pneumoniae Proteus |
| Zhejiang | 2015–2019 | (Chen et al., 2020; Zhang et al., 2020b; Li et al., 2021a; Cheng et al., 2021b; Zheng et al., 2022) | Food animals |
tet(X2) tet(X3) tet(X4) tet(X6) tet(X5.2) tet(X14) |
Plasmid Chromosome |
IncFIA-IncHI1B-IncHI1A IncFIA-IncHI1B-IncX1 | ST10, ST773, ST1196, ST6883, ST641, ST515, ST767 | 100 |
bla
OXA-58
bla NDM-1 |
Acinetobacter
Enterococcus faecalis Proteus E. coli |
| (Cheng et al., 2021b) | Farm environment | tet(X2) | – | – | – | 3 | – | Myroides sp. | ||
| (He et al., 2019; Ruan et al., 2020; Zeng et al., 2021) | Human | tet(X4) | Plasmid | IncX1 | ST773 | 33 | mcr-1 bla CTX-M-14 | E. coli | ||
| Jiangxi | 2015–2018 | (Sun J. et al., 2019; Chen et al., 2020) | Food animals |
tet(X4) tet(X3) |
Plasmid Chromosome |
IncQ1 | ST761, ST515, ST871, ST8302 | 37 | mcr-1, blaCTX-M-14 |
E. coli
Acinetobacter |
| Hainan | 2017–2018 | (Chen et al., 2020; Cui et al., 2020) | Food animals |
tet(X) tet(X3) |
Plasmid | – | – | 43 | bla NDM-1 | Acinetobacter |
| Farm environment | tet(X) | Plasmid | – | – | 5 | bla OXA-58 | Acinetobacter | |||
| Guangxi | 2017–2020 | (Sun J. et al., 2019; Cui et al., 2020; Feng et al., 2022) | Food animals |
tet(X) tet(X4) |
Plasmid | – | ST1196, ST10, ST1415, ST34, ST109, ST48, ST195, ST799, ST2223, ST1244, ST3888, ST6404, ST641, ST677, ST452, ST1250 | 97 | – |
Acinetobacter
E. coli |
| Fujian | 2018 | (Sun J.et al., 2019; Chen et al., 2020; Cui et al., 2020) | Food animals |
tet(X) tet(X4) |
Plasmid | – | ST8302, ST761, ST515, ST8338 | 26 | – | Acinetobacter |
| Qinghai | 2015–2018 | (Chen et al., 2020) | Wild migratory birds | tet(X4) | – | – | – | 5 | – | Acinetobacter |
| Xinjiang | 2017–2018 | (Cui et al., 2020) | Food animals | tet(X) | – | – | – | 8 | bla NDM-1 | Acinetobacter |
| Farm environment | tet(X) | – | – | – | 3 | – | Acinetobacter | |||
| Liaoning | 2018 | (Cui et al., 2020) | Food animals | tet(X) | – | – | – | 2 | – | Acinetobacter |
| Farm environment | tet(X) | – | – | – | 3 | – | Acinetobacter | |||
| Taiwan | 2019–2020 | (Hsieh et al., 2021; Wang et al., 2021a) | Human Environment |
tet(X) tet(X10) |
Chromosome | – | ST793, ST723 | 7 1 |
bla OXA-72 |
Acinetobacter
Amniculibacterium aquaticum |
| Shanxi | 2018–2020 | (Li et al., 2021a; Feng et al., 2022) | Food animals | tet(X4) | Plasmid | IncFIA-IncHI1B-IncHI1A IncX1 | ST641, ST58, ST515, ST2064, ST6833, ST10, ST48, ST4156 | 11 | – | E. coli |
| Gansu | 2019 | (Li et al., 2021a) | Food animals | tet(X4) | Plasmid | IncFII | ST540 | 1 | – | E. coli |
| Anhui | 2019 | (Li et al., 2021a) | Food animals | tet(X4) | Plasmid | IncFIA-IncHI1B-IncHI1A IncFIA-IncFIB-IncX1 IncX1, IncFII | ST877, ST2035, ST218 | 8 | – | E. coli |
| Beijing | 2018 | (Zhai et al., 2022) | Human | tet(X4) | Plasmid | IncFIIK | ST534 | 1 | – | K. pneumoniae |
| (Sun et al., 2020) | Food animals | tet(X4) | Plasmid | IncFIA-IncHI1B-IncHI1A | ST744 | 1 | – | E. coli | ||
| Shaanxi Ningxia |
2018–2020 | (Sun et al., 2020; Feng et al., 2022) | Food animals | tet(X4) | Plasmid | IncX1, IncN, IncR, IncY, IncFIA, IncFIB | ST877, ST2035, ST10392, ST10, ST7366, ST890, ST3580, ST442, ST278, ST4429, ST1602, ST746, ST48, ST189, ST8504, ST1437, ST7604 | 7,346 | – | E. coli |
| Guizhou | 2018 | (Sun et al., 2020) | Food animals | tet(X4) | Plasmid | – | ST48, ST202, ST542, ST206, ST890 | 1 | – | E. coli |
| Hunan | 2015–2018 | (Chen et al., 2020) | Food animals | tet(X3) | Plasmid | – | – | 14 | – | Acinetobacter |
| Vietnam | 2021 | (Dao et al., 2022) | River | tet(X4) | Chromosome | – | – | 1 | bla OXA-48 | Shewanella Xiamen |
| Sierra Leone | 2010–2011 | (Leski et al., 2013) | Human | tet(X) | – | – | – | 11 | – |
Enterobacter cloacae E. coli
K. pneumoniae Pseudomonas Delftia acidovorans Comamonas testosteroni |
| Singapore | 2018 | (Ding et al., 2020) | Human | tet(X4) | Plasmid | IncI1 | ST73 | 2 | mcr-1 | E. coli |
| Japan | 2012 | (Usui et al., 2021) | Food animals | tet(X6) | Plasmid | IncW | – | 1 | – | E. coli |
| Chile | 2010–2021 | (Concha et al., 2021; Wang et al., 2021a) | Aquatic animals |
tet(X) tet(X10) |
– | – | – | 3 | – |
Epilithonimonas Chryseobacterium sp. |
| Pakistan | 2018–2019 | (Mohsin et al., 2021; Li et al., 2022) | Food animals Farm environment Human |
tet(X4) tet(X7) |
Plasmid | IncFII, IncQ | ST6726, ST694, ST4388、ST224 | 41 1 |
mcr-1 |
E. coli
Pseudomonas aeruginosa |
| United Kingdom | 1966–2020 | (Martelli et al., 2022) | Food animals Human Rainbow trout |
tet(X4) tet(X12) tet(X4) tet(X7) tet(X6) |
Plasmid – – – |
IncX1-IncY – – – |
ST1140 – – – |
1 1 5 2 2 |
– |
E. coli Riemerella anatipestifer Salmonella Shigella soneii Enterobacter hormaechei Salmonella Typhimurium Chryseobacterium sp. |
| Norway | – | (Marathe et al., 2021) | Wastewater treatment plants | tet(X4) | Plasmid | IncFIA/FIB | ST167 | 1 | bla CTX-M-14 | E. coli |
| Belgium | 2007–2017 |
LDIS01000001.1 SELG01000025.1 |
Food animals Musca domestica |
tet(X10) | – – |
– – |
– – |
1 1 |
– – |
Arcobacter thereius
Apibacter muscae |
| South Africa | 2013 | MKSZ01000121.1 | Thiocyanate stock biobioreactor | tet(X10) | – | – | – | 1 | – | Bacteroidales bacterium |
| United States of America | 2010–2018 | (Wang et al., 2021a) | Human Environment |
tet(X10) tet(X7) tet(X10) |
– – – |
– – – |
– – – |
47 1 2 |
– – – |
Bacteroides sp. E. coli Chryseobacterium sp. Bacteroides sp. |
| Australia | 2018 | VSOP01000024.1 | Mus musculus | tet(X10) | – | – | – | 1 | – | Alistipes sp. |
| Ireland | 2017 |
VLSQ01000048.1 VLSR01000042.1 SMTB01000142.1 |
Environment Food animals |
tet(X3) tet(X6) |
– – |
– – |
– – |
2 1 |
– – |
Acinetobacter sp. |
| Bolivia | 2016 | PQTA01000018.1 | Human | tet(X7) | – | – | – | 1 | – | E. coli |
| Turkey | 2021 | (Kürekci et al., 2022) | Wastewater | tet(X4) | Plasmid | IncFIA-IncHI1-IncFIB(K) | ST609 | 2 | bla SHV-12 | E. coli |
Figure 2.
The distribution of tet(X) genes in different parts of China showing these genes have been found in 24 provinces from 2015 to 2022. The triangle in the figure indicates the number of tet(X)-positive strains isolated in each region of China, and the square indicates different sources of tet(X) genes, which corresponds to the pie chart in the figure. Furthermore, the different sources of tet(X) genes in the listed provinces can also be found, using color indication.
Prevalence of tet(X4) in animals
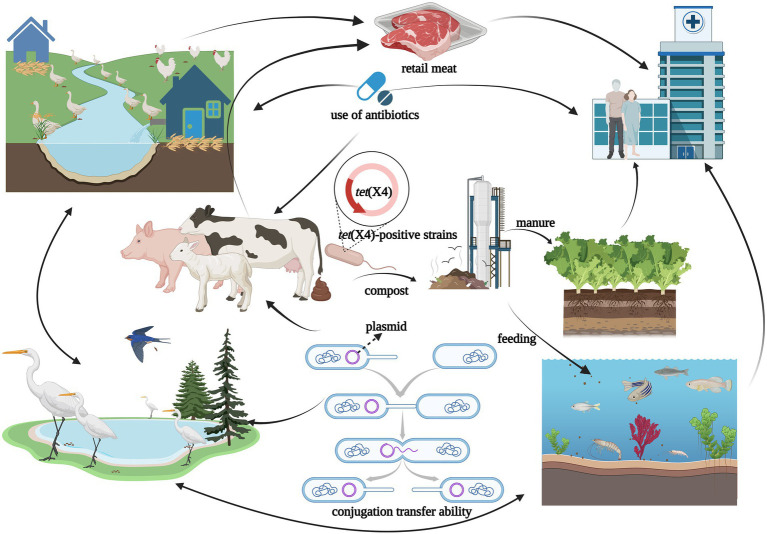
Antibiotics are commonly used in livestock production to maintain animal health and productivity. However, the absorption of antibiotics in the body is low, and most of them are excreted in the form of metabolites with feces and urine (Qiu et al., 2016). The antibiotic residues and ARGs carried in animal feces can be transmitted to the environment or humans, showing a potential source of ARGs (Ji et al., 2012; Van Boeckel et al., 2015). Tigecycline is currently approved for Human clinical use only, but the tet(X4) gene has been detected in food animals, retail meat, aquatic animals, and wild animals (Figure 3). Moreover, tet(X4) is currently detected in isolates from various animal origin samples, including pigs, ducks, geese, chickens, cattle, freshwater fish and shrimp, and migratory birds, with pig sources in particular predominating (Table 1). In a study based on a metagenomics approach, it was shown that among the abundant of ARGs in pig manure and its receiving environment (sewage, crops, soil, etc.), the tetracycline resistance genes were prevalent in pig farms (Tong et al., 2022). The same is true for pig slaughterhouses, suggesting that tet(X4)-carrying plasmids play an essential role in the spread of this drug related ARGs (Li et al., 2020b). Worth noting that the first isolation of plasmid mediated-tet(X4) was also obtained from the pig-derived sample (He et al., 2019). So far, 24 provinces in China have reported the emergence of tet(X), with Guangdong, Zhejiang, and Shandong having the largest number of positive strains (Figure 2). Li et al. (2021c) isolated 32 tet(X4)-positive strains from feces and anal swabs of pigs in Shanxi. At the same time, tet(X4)-positive E. coli were also detected in the sewage and soil of the pig farm environment. These isolates have different ST types, but their tet(X4)-carrying plasmids have the same replicon type, indicating that these plasmids are transferred horizontally among different reservoirs, and horizontal transfer maybe the main way for tet(X4) to spread in the surrounding environment (Sun J. et al., 2019). During 2016–2018, researchers isolated the tet(X)-positive Acinetobacter from pig, chicken, duck and goose feces in multi-regional farms of seven provinces, China (Guangdong, Hainan, Guangxi, Fujian, Shandong, Xinjiang, and Liaoning; Cui et al., 2020). Zhang et al. have detected 51 (17%) tet(X)-positive strains from 296 rectal swabs of healthy dairy cows, including the strains of tet(X3)-positive Acinetobacter and tet(X4)-positive E. coli (Zhang et al., 2020b). The prevalent range of tet(X) continues to expand, tet(X) and its variant genes have been detected in different reservoirs, and tet(X)-carrying plasmids have high mobility, which can be transmitted horizontally among different species.
Figure 3.
The figure was created with “BioRender.com” showing transmission routes illustration of tet(X4)-positive strains in natural environment. Possible dissemination routes of tet(X4)-positive strains showed by arrows among different reservoirs such as ducks, geese, migratory birds, chickens, pigs, cattle, aquatic animal, agricultural field, meat, and humans. The horizontal transmission of tet(X4) among reservoirs risked to public health for the “One Health” concept.
The co-existence of tet(X4) with other important ARGs is noteworthy. Specifically, the tet(X) gene co-existed with the flor gene in most cases, the latter encoding chloramphenicol efflux pumps, which can be also co-transferred (Du et al., 2004; Fu et al., 2021). Further, ESBL genes and colistin resistance genes often co-existed with tet(X4) in Enterobacteriaceae (Table 1). In a retrospective study, five pig-derived tet(X4)-positive strains were detected in Sichuan, Henan, and Guangdong of China, and two of these tet(X4)-positive E. coli also carried the mcr-1 gene (Sun C. et al., 2019). Tang et al. (2021) found eight tet(X4)-positive strains in two commercial pig farms in Sichuan, and three of them co-existed with the cfr gene in E. coli, and both ARGs were located on a novel hybrid plasmid, which could be transferred to the recipient bacteria. Li et al. (2020c) screened one strain of tet(X4)-positive E. coli and two strains of tet(X6)-positive aspergillus in different chicken farms, while the tet(X6) gene co-existed with the carbapenem resistance gene blaNDM-1. The same situation also existed in other country, where the tet(X4) gene was detected to co-exist with the colistin resistance gene in Pakistan (Mohsin et al., 2021; Li et al., 2022). Specifically, Li et al. (2022) detected 36 tet(X4)-positive strains, of which 24 tet(X4)-positive strains co-carried the mcr-1 gene. Mohsin et al. (2021) detected four tet(X4)-positive E. coli from farm animals and slaughterhouse effluents, and three E. coli contained the mcr-1.1 gene. It should be noted that the resistance to tigecycline or colistin can be transferred by the transmission of plasmids, which posed an enormous threat to the clinical treatment of MDR bacterial infections (Ruan et al., 2020; Xu et al., 2021; Zhang et al., 2021b).
Food animals such as pigs and poultry are the primary source of high-quality protein for humans (Henchion et al., 2014), they have been slaughtered in slaughterhouses before entering the market, and tet(X) has also been detected in retail meat, which indicated that the slaughterhouse might be a potential reservoir for tet(X) (Homeier-Bachmann et al., 2021; Mohsin et al., 2021). There are also some reports on tet(X) from retail meat sources in Sichuan and Henan. In 2019, Sun et al. collected 311 retail meat samples from Sichuan province and detected 25 tet(X4)-positive E. coli strains, most of which were isolated from the raw pork (52%), chicken (40%), duck (4%), and beef (4%; Sun et al., 2021a). In addition, five tet(X4)-positive E. coli strains were isolated from retail chicken during routine monitoring of ARGs in the Sichuan market in 2020. Interestingly, one of the tet(X4)-carrying plasmids from retail chicken was 99% identity to the pig-derived tet(X4)-carrying plasmid, and others had the tet(X4) gene localized on hybrid plasmids (Lv H. et al., 2020). This phenomenon suggests that tet(X4)-carrying plasmids can spread among different animals, which lead to the dissemination of tet(X4) in the ecological environment.
In addition to food animals, tigecycline resistance genes have also been detected in wild animals. In 2018, Chen et al. (2019b) isolated three strains of tet(X4)-positive E. coli from the feces of migratory birds in Guangdong, two of which were located on the plasmid, and the remaining one was located on the chromosome. The tet(X4)-carrying plasmid isolated from the migratory birds had a high degree of similarity with one plasmid isolated from human samples. In addition, five tet(X4)-positive Acinetobacter were also isolated from the bar-headed goose samples in Qinghai (Chen et al., 2020). In the latest report, researchers also detected the tet(X) variant genes in wild fish and shrimp (Li et al., 2019; Concha et al., 2021). Wild animals were not directly exposed to clinical antibiotics, but more and more ARGs were detected in them, indicating wild animals including migratory birds, were likely to be involved in the large-scale exchange of ARGs, especially long-distance transmission of cross species (Allen et al., 2010; Wang et al., 2017; Zeballos-Gross et al., 2021; Luo et al., 2022).
Prevalence of tet(X4) in humans
Tigecycline was approved for clinical use in 2005, and which was introduced in China in 2012. Tet(X) was detected in human clinical samples in 2013, with 11 tet(X) positive strains isolated from 52 samples, including stool, semen, blood, and urine in a Sierra Leonean hospital (Leski et al., 2013). Ding et al. (2020) conducted a retrospective screening study on 109 fecal samples, and detected tet(X4)-positive strains in the intestinal microflora of healthy human, with an isolation rate of 10.1%. Subsequently, tet(X4)-positive E. coli were also reported in clinical isolates from Guangdong, Hebei, Zhejiang, Beijing, Sichuan, and other places in China (Table 1). It can be seen that the tet(X) gene is not uncommon in hospital clinical isolates, and tet(X4) may be widely distributed in the human gut microflora, with great risk of transmission. In 2019, Cui et al. (2022) collected 1,001 stool samples from hospital inpatients in Guangdong Province of China, isolated 48 (4.8%) tet(X4)-positive E. coli. Notably, the hybrid plasmid was found to be prevalent in tet(X4)-positive strains of animal origin, with the characteristics of stable existence and horizontal transfer (Sun C. et al., 2019), which predicted this tet(X4)-carrying plasmid can be transmitted among humans, animals and the environment, thus facilitating the wide spread of tet(X4) in the ecosystem. The co-existence of tet(X4) with mcr and ESBL genes in the clinical setting is a great concern. Ruan et al. (2020) found one E. coli strain co-harboring tet(X4) with mcr-1 on the same conjugative plasmid from the urine sample of a clinical patient in Zhejiang Province, China. Further, two E. coli strains carrying both mcr-1 and tet(X4) were isolated in Singapore (Ding et al., 2020). Meanwhile, blaCTX, blaOXA, blaNDM, and blaSHV genes were also detected to be co-existence with tet(X) in one strain (Table 1). Tigecycline and colistin are the last resort for treating MDR bacteria, and the co-existence of tet(X) with mcr and ESBL genes limited the choice of clinical antibiotics, which subsequently poses a significant threat to public health.
ARB are persistent pollutants in the environment in which humans are in close contact (Kim and Aga, 2007). ARB can be transmitted to other hosts through human activities when conditions are favorable (Allen et al., 2010). Except for the hospital clinical environment, the live poultry market (LPM) is also a vast reservoir of ARGs (Wang Y. et al., 2019; Wang et al., 2021b). The tet(X3) and tet(X4) genes have been detected in the intestinal flora of LPM workers and the surrounding environment (Wang Y. et al., 2020), which indicated that the plasmid-mediated tigecycline resistance gene might exist in LPM for a long period. The ARGs are likely to be transmitted from live poultry to LPM staff, ecological environments or other animals.
Prevalence of tet(X4) in the environment
Antibiotics and ARGs were detected in various environments (Qiao et al., 2018). The humans, animals, and ecological environments are components of the “One health” concept, and they have important connections and can influence each other. Therefore, they can acquire ARGs through different pathways and achieve the flow of ARGs among different reservoirs (Anyanwu et al., 2021), including tet(X4) (Figure 3). In recent years, the environment has played an increasing role on the spread of antibiotic resistance (Finley et al., 2013; Bengtsson-Palme et al., 2014; Bondarczuk et al., 2016; Lerminiaux and Cameron, 2019). The ARGs and ARB existed in large numbers within the environment and can be transmit to reservoirs (Lin et al., 2021), such as rivers contaminated by animal manure, the soil around livestock farms, manure-irrigated agricultural fields, and sewage treatment plants. The abuse use of antibiotics and the spread of antibiotic resistance caused by animal husbandry is one of the main concerns of sustainable agriculture(Manyi-Loh et al., 2018), where the use of first or second-generation tetracycline-class drugs was high, with subtherapeutic dosing in the forage (Yezli and Li, 2012). In animal husbandry, a wider range of antibiotic options lead to the spread of ARGs in agriculture to the human microbiota (Aminov, 2011). Animal manure as the valuable renewable fertilizer was often applied to the cropland (Zhou X. et al., 2019; Lima et al., 2020), which was found to contain different ARB and ARGs. Moreover, water as a good transport route for nutrients and contaminants was also a major reservoir for ARGs (Vaz-Moreira et al., 2014; Manaia et al., 2016; Miłobedzka et al., 2022). Specifically, macrogenomic analysis of wetland effluents and sediments in the Yangtze Delta region revealed a high abundance of the tet(X) gene (Du et al., 2022). Tet(X) and their variants were detected in farm soil, manure, and lettuce samples near chicken farms in Jiangsu, Jiangxi, and Sichuan provinces of China, and even in soil samples far from these farms (He et al., 2021). Cui et al. (2020) collected samples from some poultry farms in seven provinces across China, where tet(X)-positive strains from sewage and soil were isolated at 7.5% and 6.7%, respectively, and tet(X) was detected to be localized on the same plasmid with blaNDM-1. These reports on identification and analysis of tet(X4) in the farm environment suggest that animal manure, sewage, and soil can influence with each other in this ecology. Moreover, tet(X4) can be transmitted among them, and the farm environment may be a massive reservoir of ARGs.
Discussion and prospects
The phenomenon of MDR of bacteria is a significant concern worldwide. Colistin and tigecycline are considered as the last resort drugs against carbapenem-resistant bacteria (Cunha et al., 2017; Zhou Y. et al., 2019). Either the global distribution of colistin-resistant E. coli or the rapid spread of the carbapenem-resistant Enterobacteriaceae have created enormous challenges for public health security. It is a more and more headache to solve the infection caused by MDR pathogens in human clinical treatment and animal husbandry (Gao et al., 2016; Potter et al., 2016; Rehman et al., 2020; Zhang et al., 2021b, 2021c). As a result, tigecycline has been recognized as the important antibiotic of last resort for the clinical treatment of certain bacterial infections. Through this article, we found that the tet(X) is prevalent on six continents around the world, with China having the highest prevalence, and most of tet(X4)-carrying plasmids can spread tigecycline resistance among different bacteria by means of horizontal transfer.
The mechanisms that cause antibiotic resistance to tigecycline are mainly overexpression of active efflux pump and ribosomal protection mechanisms. However, more and more tet(X4) has been detected in plasmids, and many different types of tet(X4)-carrying plasmids have strong ability of horizontal transfer, which means plasmids mediated transmission of tigecycline resistance genes may gradually increase, risking to public health (Pereira et al., 2021). The widespread use of antimicrobial drugs in domestic animals is an important reason for the rapid increase of AMR. The researchers reported the AMR monitoring results of E. coli in China’s pig farms from 2018 to 2019, showing that multidrug resistance was detected in 91% of isolates (1871 in total), and resistance to last resort drugs including tigecycline, colistin and carbapenem was found (Peng et al., 2022). Recent studies have also found the antibiotic resistance of livestock has increased from 1970 to 2019, indicating that if the use of antibiotics is not restricted, it may not be able to effectively protect the livestock. By testing the sensitivity of several recent strains of E. coli to various antibiotics, researchers found their resistance was far higher than that of the strains in the 1970s. In addition, the researchers also pointed out although the specific antibiotics used to treat bacterial infections may be different, the types are often the same, so the rapid rise in drug resistance will eventually affect human beings (Yang et al., 2022). Surprisingly, the potential spread of virus-mediated ARGs is likely to exacerbate AMR, including tetracycline resistance and harm to public health (Calero-Cáceres et al., 2019; Debroas and Siguret, 2019; Shi et al., 2022), which needs our wider attention. Moreover, viruses might be linked to Enterobacteriaceae or Vibrionaceae and were considered as gene shuttles in ARGs transfer, like plasmids. This indicates that viruses and bacteria may have a synergistic effect on the transmission of ARGs. Therefore,we should look at AMR from a holistic perspective that includes humans, animals as well as the environment, and develop a plan for rational use of antibiotics to reduce the long-term and single use of tigecycline in the clinical environment, avoiding reduced clinical efficacy and increased mortality (Yahav et al., 2011). Controlling the “spillover effect” of ARGs is also important from “One Health” concept (Collignon, 2015; Tyrrell et al., 2019; Olesen et al., 2020; Aslam et al., 2021). In-depth studies of tigecycline resistance or transmission mechanisms, and continuous monitoring of tet(X) prevalence are urgent needed to determine the precise transmission route of ARB and ARGs, so as to provide reference for designing more effective public health intervention strategies. However, due to the limitation of the length of the article, we did not summarize the current methods and strategies of various countries or regions to limit the transmission of tet(X4)-positive strains, and what beneficial substances (like probiotics, prebiotics and antimicrobial peptide) can replace use of specific antibiotics in the post-antibiotic era to avoid the spread of tigecycline resistance.
Author contributions
SZ and JW wrote this manuscript. JW, YuW, and SZ contributed to the design of this manuscript. MW, XO, QY, YiW, RJ, ML, DZ, SC, and QG provided ideas for the conception of this manuscript. BT, DS, XZ, SM, and JH helped to create figures and tables. SZ and AC modified this manuscript, and acquired funding. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the NSFC (31902267), the earmarked fund for China Agriculture Research System (CARS-42-17), the funds of Key Laboratory of Livestock and Poultry Provenance Disease Research in Mianyang, Sichuan Veterinary Medicine and Drug Innovation Group of China Agricultural Research System (SCCXTD-2022-18), and the Applied Basic Research Programs of Science and Technology Department of Sichuan Province (2019YJ0410).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
- Ahmad M., Khan A. (2019). Global economic impact of antibiotic resistance: a review. J. Glob. Antimicrob. Resist. 19, 313–316. doi: 10.1016/j.jgar.2019.05.024 [DOI] [PubMed] [Google Scholar]
- Akiyama T., Presedo J., Khan A. (2013). The tetA gene decreases tigecycline sensitivity of Salmonella enterica isolates. Int. J. Antimicrob. Agents 42, 133–140. doi: 10.1016/j.ijantimicag.2013.04.017, PMID: [DOI] [PubMed] [Google Scholar]
- Allen H., Donato J., Wang H., Cloud-Hansen K., Davies J., Handelsman J. (2010). Call of the wild: antibiotic resistance genes in natural environments. Nat. Rev. Microbiol. 8, 251–259. doi: 10.1038/nrmicro2312, PMID: [DOI] [PubMed] [Google Scholar]
- Aminov R. (2011). Horizontal gene exchange in environmental microbiota. Front. Microbiol. 2:158. doi: 10.3389/fmicb.2011.00158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aminov R. (2021). Acquisition and spread of antimicrobial resistance: a tet(X) case study. Int. J. Mol. Sci. 22:3905. doi: 10.3390/ijms22083905, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anyanwu M., Okpala C., Chah K., Shoyinka V. (2021). Prevalence and traits of mobile colistin resistance gene harbouring isolates from different ecosystems in Africa. Biomed. Res. Int. 2021, 1–20. doi: 10.1155/2021/6630379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aslam B., Khurshid M., Arshad M., Muzammil S., Rasool M., Yasmeen N., et al. (2021). Antibiotic resistance: one health one world outlook. Front. Cell. Infect. Microbiol. 11:771510. doi: 10.3389/fcimb.2021.771510, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai L., Du P., Du Y., Sun H., Zhang P., Wan Y., et al. (2019). Detection of plasmid-mediated tigecycline-resistant gene tet(X4) in Escherichia coli from pork, Sichuan and Shandong provinces, China, February 2019. Euro Surveill. 24. doi: 10.2807/1560-7917.ES.2019.24.25.1900340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bankan N., Koka F., Vijayaraghavan R., Basireddy S., Jayaraman S. (2021). Overexpression of the ade B efflux pump gene in Tigecycline-resistant Acinetobacter baumannii clinical isolates and its inhibition by (+)Usnic acid as an adjuvant. Antibiotics 10:1900340. doi: 10.3390/antibiotics10091037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beabout K., Hammerstrom T., Perez A., Magalhães B., Prater A., Clements T., et al. (2015). The ribosomal S10 protein is a general target for decreased tigecycline susceptibility. Antimicrob. Agents Chemother. 59, 5561–5566. doi: 10.1128/AAC.00547-15, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender J., Klare I., Fleige C., Werner G. (2020). A nosocomial cluster of Tigecycline-and vancomycin-resistant enterococcus faecium isolates and the impact of rps J and tet (M) mutations on tigecycline resistance. Microb. Drug Resist. 26, 576–582. doi: 10.1089/mdr.2019.0346, PMID: [DOI] [PubMed] [Google Scholar]
- Bengtsson-Palme J., Boulund F., Fick J., Kristiansson E., Larsson D. (2014). Shotgun metagenomics reveals a wide array of antibiotic resistance genes and mobile elements in a polluted lake in India. Front. Microbiol. 5:648. doi: 10.3389/fmicb.2014.00648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bondarczuk K., Markowicz A., Piotrowska-Seget Z. (2016). The urgent need for risk assessment on the antibiotic resistance spread via sewage sludge land application. Environ. Int. 87, 49–55. doi: 10.1016/j.envint.2015.11.011, PMID: [DOI] [PubMed] [Google Scholar]
- Cai W., Tang F., Jiang L., Li R., Wang Z., Liu Y. (2021). Histone-like nucleoid structuring protein modulates the fitness of tet(X4)-bearing Inc X1 plasmids in gram-negative bacteria. Front. Microbiol. 12:763288. doi: 10.3389/fmicb.2021.763288, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calero-Cáceres W., Ye M., Balcázar J. L. (2019). Bacteriophages as environmental reservoirs of antibiotic resistance. Trends Microbiol. 27, 570–577. doi: 10.1016/j.tim.2019.02.008, PMID: [DOI] [PubMed] [Google Scholar]
- Cattoir V., Isnard C., Cosquer T., Odhiambo A., Bucquet F., Guérin F., et al. (2015). Genomic analysis of reduced susceptibility to tigecycline in Enterococcus faecium. Antimicrob. Agents Chemother. 59, 239–244. doi: 10.1128/AAC.04174-14, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Chen L., Zhang Y., Cui C., Wu X., He Q., et al. (2019a). Detection of chromosome-mediated tet(X4)-carrying Aeromonas caviae in a sewage sample from a chicken farm. J. Antimicrob. Chemother. 74, 3628–3630. doi: 10.1093/jac/dkz387, PMID: [DOI] [PubMed] [Google Scholar]
- Chen C., Cui C., Wu X., Fang L., He Q., He B., et al. (2021). Spread of tet (X5) and tet(X6) genes in multidrug-resistant Acinetobacter baumannii strains of animal origin. Vet. Microbiol. 253:108954. doi: 10.1016/j.vetmic.2020.108954, PMID: [DOI] [PubMed] [Google Scholar]
- Chen C., Cui C., Yu J., He Q., Wu X., He Y., et al. (2020). Genetic diversity and characteristics of high-level tigecycline resistance Tet(X) in Acinetobacter species. Genome Med. 12:111. doi: 10.1186/s13073-020-00807-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Cui C., Zhang Y., He Q., Wu X., Li G., et al. (2019b). Emergence of mobile tigecycline resistance mechanism in Escherichia coli strains from migratory birds in China. Emerg. Microbes Infect. 8, 1219–1222. doi: 10.1080/22221751.2019.1653795, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Hu D., Zhang Q., Liao X., Liu Y., Sun J. (2017). Efflux pump overexpression contributes to tigecycline heteroresistance in Salmonella enterica serovar Typhimurium. Front. Cell. Infect. Microbiol. 7:37. doi: 10.3389/fcimb.2017.00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Chen Y., Liu Y., Guo Y., Zhou Y., Xiao T., et al. (2020). Identification of novel tetracycline resistance gene tet(X14) and its co-occurrence with tet(X2) in a tigecycline-resistant and colistin-resistant Empedobacter stercoris. Emerg. Microbes Infect. 9, 1843–1852. doi: 10.1080/22221751.2020.1803769, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Chen Y., Liu Y., Song J., Chen Y., Shan T., et al. (2021a). Detection of a new tet(X6)-encoding plasmid in Acinetobacter towneri. J. Glob. Antimicrob. Resist. 25, 132–136. doi: 10.1016/j.jgar.2021.03.004, PMID: [DOI] [PubMed] [Google Scholar]
- Cheng Y., Liu Y., Chen Y., Huang F., Chen R., Xiao Y., et al. (2021b). Sporadic dissemination of tet(X3) and tet(X6) mediated by highly diverse plasmidomes among livestock-associated Acinetobacter. Microbiol. Spectr. 9:e0114121. doi: 10.1128/Spectrum.01141-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra I. (2002). New developments in tetracycline antibiotics: glycylcyclines and tetracycline efflux pump inhibitors. Drug Resist. Updat. 5, 119–125. doi: 10.1016/S1368-7646(02)00051-1, PMID: [DOI] [PubMed] [Google Scholar]
- Chopra I., Roberts M. (2001). Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol. Mol. Biol. Rev. 65, 232–260; second page, table of contents. doi: 10.1128/MMBR.65.2.232-260.2001, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collignon P. (2015). Antibiotic resistance: are we all doomed? Intern. Med. J. 45, 1109–1115. doi: 10.1111/imj.12902, PMID: [DOI] [PubMed] [Google Scholar]
- Concha C., Miranda C., Santander J., Roberts M. (2021). Genetic characterization of the tetracycline-resistance gene tet(X) carried by two Epilithonimonas strains isolated from farmed diseased rainbow trout, Oncorhynchus mykiss in Chile. Antibiotics 10:1051. doi: 10.3390/antibiotics10091051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui C., Chen C., Liu B., He Q., Wu X., Sun R., et al. (2020). Co-occurrence of plasmid-mediated tigecycline and carbapenem resistance in Acinetobacter spp. from waterfowls and their neighboring environment. Antimicrob. Agents Chemother. 64:e02502-19. doi: 10.1128/AAC.02502-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui C., He Q., Jia Q., Li C., Chen C., Wu X., et al. (2021). Evolutionary trajectory of the Tet(X) family: critical residue changes towards high-level Tigecycline resistance. mSystems 6:e00050-21. doi: 10.1128/mSystems.00050-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui C., Li X., Chen C., Wu X., He Q., Jia Q., et al. (2022). Comprehensive analysis of plasmid-mediated tet(X4)-positive Escherichia coli isolates from clinical settings revealed a high correlation with animals and environments-derived strains. Sci. Total Environ. 806:150687. doi: 10.1016/j.scitotenv.2021.150687, PMID: [DOI] [PubMed] [Google Scholar]
- Cunha B., Baron J., Cunha C. (2017). Once daily high dose tigecycline – pharmacokinetic/pharmacodynamic based dosing for optimal clinical effectiveness: dosing matters, revisited. Expert Rev. Anti-Infect. Ther. 15, 257–267. doi: 10.1080/14787210.2017.1268529, PMID: [DOI] [PubMed] [Google Scholar]
- Dai S., Liu D., Han Z., Wang Y., Lu X., Yang M., et al. (2022). Mobile tigecycline resistance gene tet(X4) persists with different animal manure composting treatments and fertilizer receiving soils. Chemosphere 307:135866. doi: 10.1016/j.chemosphere.2022.135866 [DOI] [PubMed] [Google Scholar]
- Dao T., Kasuga I., Hirabayashi A., Nguyen D., Tran H., Vu H., et al. (2022). Emergence of mobile tigecycline resistance gene tet(X4)-harbouring Shewanella xiamenensis in a water environment. J. Glob. Antimicrob. Resist. 28, 140–142. doi: 10.1016/j.jgar.2021.12.022, PMID: [DOI] [PubMed] [Google Scholar]
- Davies J., Davies D. (2010). Origins and evolution of antibiotic resistance. Microbiol. Mol. Biol. Rev. 74, 417–433. doi: 10.1128/MMBR.00016-10, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debroas D., Siguret C. (2019). Viruses as key reservoirs of antibiotic resistance genes in the environment. ISME J. 13, 2856–2867. doi: 10.1038/s41396-019-0478-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng T., Jia Y., Tong Z., Shi J., Wang Z., Liu Y. (2022). Bismuth drugs reverse Tet(X)-conferred tigecycline resistance in gram-negative bacteria. Microbiol. Spectr. 10:e0157821. doi: 10.1128/spectrum.01578-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y., Saw W., Tan L., Moong D., Nagarajan N., Teo Y., et al. (2020). Emergence of tigecycline-and eravacycline-resistant Tet(X4)-producing Enterobacteriaceae in the gut microbiota of healthy Singaporeans. J. Antimicrob. Chemother. 75, 3480–3484. doi: 10.1093/jac/dkaa372, PMID: [DOI] [PubMed] [Google Scholar]
- Du J., Xu T., Guo X., Yin D. (2022). Characteristics and removal of antibiotics and antibiotic resistance genes in a constructed wetland from a drinking water source in the Yangtze River Delta. Sci. Total Environ. 813:152540. doi: 10.1016/j.scitotenv.2021.152540, PMID: [DOI] [PubMed] [Google Scholar]
- Du P., Liu D., Song H., Zhang P., Li R., Fu Y., et al. (2020). Novel IS26-mediated hybrid plasmid harbouring tet(X4) in Escherichia coli. J. Glob. Antimicrob. Resist. 21, 162–168. doi: 10.1016/j.jgar.2020.03.018, PMID: [DOI] [PubMed] [Google Scholar]
- Du X., Xia C., Shen J., Wu B., Shen Z. (2004). Characterization of florfenicol resistance among calf pathogenic Escherichia coli. FEMS Microbiol. Lett. 236, 183–189. doi: 10.1111/j.1574-6968.2004.tb09645.x, PMID: [DOI] [PubMed] [Google Scholar]
- Fang L., Chen Q., Shi K., Li X., Shi Q., He F., et al. (2016). Step-wise increase in tigecycline resistance in Klebsiella pneumoniae associated with mutations in ram R, lon and rpsJ. PLoS One 11:e0165019. doi: 10.1371/journal.pone.0165019, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang L., Chen C., Cui C., Li X., Zhang Y., Liao X., et al. (2020). Emerging high-level tigecycline resistance: novel tetracycline destructases spread via the Mobile Tet(X). BioEssays 42:e2000014. doi: 10.1002/bies.202000014 [DOI] [PubMed] [Google Scholar]
- Feng J., Su M., Li K., Ma J., Li R., Bai L., et al. (2022). Extensive spread of tet(X4) in multidrug-resistant Escherichia coli of animal origin in western China. Vet. Microbiol. 269:109420. doi: 10.1016/j.vetmic.2022.109420, PMID: [DOI] [PubMed] [Google Scholar]
- Finley R., Collignon P., Larsson D., Mcewen S., Li X., Gaze W., et al. (2013). The scourge of antibiotic resistance: the important role of the environment. Clin. Infect. Dis. 57, 704–710. doi: 10.1093/cid/cit355, PMID: [DOI] [PubMed] [Google Scholar]
- Fluit A., Florijn A., Verhoef J., Milatovic D. (2005). Presence of tetracycline resistance determinants and susceptibility to tigecycline and minocycline. Antimicrob. Agents Chemother. 49, 1636–1638. doi: 10.1128/AAC.49.4.1636-1638.2005, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Y., Chen Y., Liu D., Yang D., Liu Z., Wang Y., et al. (2021). Abundance of tigecycline resistance genes and association with antibiotic residues in Chinese livestock farms. J. Hazard. Mater. 409:124921. doi: 10.1016/j.jhazmat.2020.124921, PMID: [DOI] [PubMed] [Google Scholar]
- Gao R., Hu Y., Li Z., Sun J., Wang Q., Lin J., et al. (2016). Dissemination and mechanism for the MCR-1 Colistin resistance. PLoS Pathog. 12:e1005957. doi: 10.1371/journal.ppat.1005957, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao X., He X., Lv L., Cai Z., Liu Y., Liu J. (2022). Detection of Tet(X4)-producing Klebsiella pneumoniae from the environment and wide spread of Inc FIA-Inc HI1A-Inc HI1B plasmid carrying tet(X4) in China. J. Glob. Antimicrob. Resist. 30, 130–132. doi: 10.1016/j.jgar.2022.05.028, PMID: [DOI] [PubMed] [Google Scholar]
- Ghosh S., Lapara T., Sadowsky M. (2015). Transformation of tetracycline by Tet X and its subsequent degradation in a heterologous host. FEMS Microbiol. Ecol. 91:fiv059. doi: 10.1093/femsec/fiv059, PMID: [DOI] [PubMed] [Google Scholar]
- Guiney D., Jr., Hasegawa P., Davis C. (1984). Expression in Escherichia coli of cryptic tetracycline resistance genes from bacteroides R plasmids. Plasmid 11, 248–252. doi: 10.1016/0147-619X(84)90031-3, PMID: [DOI] [PubMed] [Google Scholar]
- He D., Wang L., Zhao S., Liu L., Liu J., Hu G., et al. (2020). A novel tigecycline resistance gene, tet(X6), on an SXT/R391 integrative and conjugative element in a Proteus genomospecies 6 isolate of retail meat origin. J. Antimicrob. Chemother. 75, 1159–1164. doi: 10.1093/jac/dkaa012, PMID: [DOI] [PubMed] [Google Scholar]
- He S., Hickman A., Varani A., Siguier P., Chandler M., Dekker J., et al. (2015). Insertion sequence IS26 reorganizes plasmids in clinically isolated multidrug-resistant bacteria by replicative transposition. MBio 6:e00762. doi: 10.1128/mBio.00762-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He T., Li R., Wei R., Liu D., Bai L., Zhang L., et al. (2020). Characterization of Acinetobacter indicus co-harbouring tet(X3) and blaNDM-1 of dairy cow origin. J. Antimicrob. Chemother. 75, 2693–2696. doi: 10.1093/jac/dkaa182, PMID: [DOI] [PubMed] [Google Scholar]
- He T., Wang R., Liu D., Walsh T., Zhang R., Lv Y., et al. (2019). Emergence of plasmid-mediated high-level tigecycline resistance genes in animals and humans. Nat. Microbiol. 4, 1450–1456. doi: 10.1038/s41564-019-0445-2, PMID: [DOI] [PubMed] [Google Scholar]
- He T., Wei R., Zhang L., Gong L., Zhu L., Gu J., et al. (2021). Dissemination of the tet(X)-variant genes from layer farms to manure-receiving soil and corresponding lettuce. Environ. Sci. Technol. 55, 1604–1614. doi: 10.1021/acs.est.0c05042, PMID: [DOI] [PubMed] [Google Scholar]
- Henchion M., Mccarthy M., Resconi V., Troy D. (2014). Meat consumption: trends and quality matters. Meat Sci. 98, 561–568. doi: 10.1016/j.meatsci.2014.06.007, PMID: [DOI] [PubMed] [Google Scholar]
- Hentschke M., Christner M., Sobottka I., Aepfelbacher M., Rohde H. (2010). Combined ram R mutation and presence of a Tn1721-associated tet(A) variant in a clinical isolate of Salmonella enterica serovar Hadar resistant to tigecycline. Antimicrob. Agents Chemother. 54, 1319–1322. doi: 10.1128/AAC.00993-09, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirabayashi A., Dao T., Takemura T., Hasebe F., Trang L., Thanh N., et al. (2021). A transferable Inc C-Inc X3 hybrid plasmid cocarrying blaNDM-4, tet(X), and tmex CD3-topr J3 confers resistance to carbapenem and tigecycline. mSphere 6:e0059221. doi: 10.1128/mSphere.00592-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homeier-Bachmann T., Heiden S., Lübcke P., Bachmann L., Bohnert J., Zimmermann D., et al. (2021). Antibiotic-resistant Enterobacteriaceae in wastewater of abattoirs. Antibiotics 10:568. doi: 10.3390/antibiotics10050568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh Y., Wu J., Chen Y., Quyen T., Liao W., Li S., et al. (2021). An outbreak of tet(X6)-carrying tigecycline-resistant Acinetobacter baumannii isolates with a new capsular type at a hospital in Taiwan. Antibiotics 10:1239. doi: 10.3390/antibiotics10101239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua X., He J., Wang J., Zhang L., Zhang L., Xu Q., et al. (2021). Novel tigecycline resistance mechanisms in Acinetobacter baumannii mediated by mutations in ade S, rpo B and rrf. Emerg. Microbes Infect. 10, 1404–1417. doi: 10.1080/22221751.2021.1948804, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji X., Shen Q., Liu F., Ma J., Xu G., Wang Y., et al. (2012). Antibiotic resistance gene abundances associated with antibiotics and heavy metals in animal manures and agricultural soils adjacent to feedlots in Shanghai; China. J. Hazard. Mater. 235–236, 178–185. doi: 10.1016/j.jhazmat.2012.07.040 [DOI] [PubMed] [Google Scholar]
- Kaewpoowat Q., Ostrosky-Zeichner L. (2015). Tigecycline: a critical safety review. Expert Opin. Drug Saf. 14, 335–342. doi: 10.1517/14740338.2015.997206, PMID: [DOI] [PubMed] [Google Scholar]
- Kim S., Aga D. (2007). Potential ecological and human health impacts of antibiotics and antibiotic-resistant bacteria from wastewater treatment plants. J. Toxicol. Environ. Health B Crit. Rev. 10, 559–573. doi: 10.1080/15287390600975137, PMID: [DOI] [PubMed] [Google Scholar]
- Kumar S., He G., Kakarla P., Shrestha U., Ranjana K., Ranaweera I., et al. (2016). Bacterial multidrug efflux pumps of the major facilitator superfamily as targets for modulation. Infect. Disord. Drug Targets 16, 28–43. doi: 10.2174/1871526516666160407113848, PMID: [DOI] [PubMed] [Google Scholar]
- Kürekci C., Lu X., Celil B., Disli H., Mohsin M., Wang Z., et al. (2022). Emergence and characterization of tigecycline resistance gene tet(X4) in ST609 Escherichia coli isolates from wastewater in Turkey. Microbiology Spectrum 10, e00732–e00722. doi: 10.1128/spectrum.00732-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamut A., Peterlin Mašič L., Kikelj D., Tomašič T. (2019). Efflux pump inhibitors of clinically relevant multidrug resistant bacteria. Med. Res. Rev. 39, 2460–2504. doi: 10.1002/med.21591, PMID: [DOI] [PubMed] [Google Scholar]
- Lerminiaux N., Cameron A. (2019). Horizontal transfer of antibiotic resistance genes in clinical environments. Can. J. Microbiol. 65, 34–44. doi: 10.1139/cjm-2018-0275 [DOI] [PubMed] [Google Scholar]
- Leski T., Bangura U., Jimmy D., Ansumana R., Lizewski S., Stenger D., et al. (2013). Multidrug-resistant tet(X)-containing hospital isolates in Sierra Leone. Int. J. Antimicrob. Agents 42, 83–86. doi: 10.1016/j.ijantimicag.2013.04.014, PMID: [DOI] [PubMed] [Google Scholar]
- Li B. (2020a). Investigation of tigecycline resistant Escherichia coli from raw meat reveals potential transmission among food-producing animals. Food Control 121:107633. doi: 10.1016/j.foodcont.2020.107633 [DOI] [Google Scholar]
- Li R., Li Y., Peng K., Yin Y., Liu Y., He T., et al. (2021a). Comprehensive genomic investigation of tigecycline resistance gene tet(X4)-bearing strains expanding among different settings. Microbiol. Spectr. 9:e0163321. doi: 10.1128/spectrum.01633-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Liu Z., Peng K., Liu Y., Xiao X., Wang Z. (2019). Co-occurrence of two tet(X) variants in an Empedobacter brevis of shrimp origin. Antimicrob. Agents Chemother. 63:e01636-19. doi: 10.1128/AAC.01636-19, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Lu X., Munir A., Abdullah S., Liu Y., Xiao X., et al. (2022). Widespread prevalence and molecular epidemiology of tet(X4) and mcr-1 harboring Escherichia coli isolated from chickens in Pakistan. Sci. Total Environ. 806:150689. doi: 10.1016/j.scitotenv.2021.150689, PMID: [DOI] [PubMed] [Google Scholar]
- Li R., Lu X., Peng K., Liu Z., Li Y., Liu Y., et al. (2020b). Deciphering the structural diversity and classification of the mobile tigecycline resistance gene tet(X)-bearing plasmidome among bacteria. mSystems 5:e00134-20. doi: 10.1128/mSystems.00134-20, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Peng K., Li Y., Liu Y., Wang Z. (2020c). Exploring tet(X)-bearing tigecycline-resistant bacteria of swine farming environments. Sci. Total Environ. 733:139306. doi: 10.1016/j.scitotenv.2020.139306, PMID: [DOI] [PubMed] [Google Scholar]
- Li X., Liu L., Ji J., Chen Q., Hua X., Jiang Y., et al. (2015). Tigecycline resistance in Acinetobacter baumannii mediated by frameshift mutation in pls C, encoding 1-acyl-sn-glycerol-3-phosphate acyltransferase. Eur. J. Clin. Microbiol. Infect. Dis. 34, 625–631. doi: 10.1007/s10096-014-2272-y, PMID: [DOI] [PubMed] [Google Scholar]
- Li X., Quan J., Yang Y., Ji J., Liu L., Fu Y., et al. (2016). Abrp, a new gene, confers reduced susceptibility to tetracycline, glycylcine, chloramphenicol and fosfomycin classes in Acinetobacter baumannii. Eur. J. Clin. Microbiol. Infect. Dis. 35, 1371–1375. doi: 10.1007/s10096-016-2674-0, PMID: [DOI] [PubMed] [Google Scholar]
- Li Y., Peng K., Yin Y., Sun X., Zhang W., Li R., et al. (2021b). Occurrence and molecular characterization of abundant tet(X) variants among diverse bacterial species of chicken origin in Jiangsu, China. Front. Microbiol. 12:751006. doi: 10.3389/fmicb.2021.751006, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang Q., Peng K., Liu Y., Li R., Wang Z. (2020d). Emergence of carbapenem- and tigecycline-resistant Proteus cibarius of animal origin. Front. Microbiol. 11:1940. doi: 10.3389/fmicb.2020.01940, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang Q., Peng K., Liu Y., Xiao X., Mohsin M., et al. (2021c). Distribution and genomic characterization of tigecycline-resistant tet(X4)-positive Escherichia coli of swine farm origin. Microb. Genom. 7:000667. doi: 10.1099/mgen.0.000667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Q., Rong H., Zhao M., Luo H., Chu Z., Wang R. (2021). Interaction between tetracycline and microorganisms during wastewater treatment: a review. Sci. Total Environ. 757:143981. doi: 10.1016/j.scitotenv.2020.143981, PMID: [DOI] [PubMed] [Google Scholar]
- Lima T., Domingues S., Da Silva G. (2020). Manure as a potential hotspot for antibiotic resistance dissemination by horizontal gene transfer events. Vet. Sci. 7:110. doi: 10.3390/vetsci7030110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Z., Yuan T., Zhou L., Cheng S., Qu X., Lu P., et al. (2021). Impact factors of the accumulation, migration and spread of antibiotic resistance in the environment. Environ. Geochem. Health 43, 1741–1758. doi: 10.1007/s10653-020-00759-0, PMID: [DOI] [PubMed] [Google Scholar]
- Linkevicius M., Sandegren L., Andersson D. (2016). Potential of tetracycline resistance proteins to evolve tigecycline resistance. Antimicrob. Agents Chemother. 60, 789–796. doi: 10.1128/AAC.02465-15, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Wang T., Shao D., Song H., Zhai W., Sun C., et al. (2022). Structural diversity of the ISCR2-mediated rolling-cycle transferable unit carrying tet(X4). Sci. Total Environ. 826:154010. doi: 10.1016/j.scitotenv.2022.154010, PMID: [DOI] [PubMed] [Google Scholar]
- Liu D., Zhai W., Song H., Fu Y., Schwarz S., He T., et al. (2020). Identification of the novel tigecycline resistance gene tet(X6) and its variants in Myroides, Acinetobacter and Proteus of food animal origin. J. Antimicrob. Chemother. 75, 1428–1431. doi: 10.1093/jac/dkaa037, PMID: [DOI] [PubMed] [Google Scholar]
- Livermore D. (2005). Tigecycline: what is it, and where should it be used? J. Antimicrob. Chemother. 56, 611–614. doi: 10.1093/jac/dki291 [DOI] [PubMed] [Google Scholar]
- Lu B., Jiang Y., Man M., Brown B., Elias P., Feingold K. (2005). Expression and regulation of 1-acyl-sn-glycerol-3-phosphate acyltransferases in the epidermis. J. Lipid Res. 46, 2448–2457. doi: 10.1194/jlr.M500258-JLR200, PMID: [DOI] [PubMed] [Google Scholar]
- Luo Y., Tan L., Zhang H., Bi W., Zhao L., Wang X., et al. (2022). Characteristics of wild bird resistomes and dissemination of antibiotic resistance genes in interconnected bird-habitat systems revealed by similarity of blaTEM polymorphic sequences. Environ. Sci. Technol. doi: 10.1021/acs.est.2c01633, PMID: [DOI] [PubMed] [Google Scholar]
- Lupien A., Gingras H., Leprohon P., Ouellette M. (2015). Induced tigecycline resistance in Streptococcus pneumoniae mutants reveals mutations in ribosomal proteins and rRNA. J. Antimicrob. Chemother. 70, 2973–2980. doi: 10.1093/jac/dkv211, PMID: [DOI] [PubMed] [Google Scholar]
- Lv H., Huang W., Lei G., Liu L., Zhang L., Yang X. (2020). Identification of novel plasmids containing the tigecycline resistance gene tet(X4) in Escherichia coli isolated from retail chicken meat. Foodborne Pathog. Dis. 17, 792–794. doi: 10.1089/fpd.2020.2822, PMID: [DOI] [PubMed] [Google Scholar]
- Lv L., Wan M., Wang C., Gao X., Yang Q., Partridge S., et al. (2020). Emergence of a plasmid-encoded resistance-nodulation-division efflux pump conferring resistance to multiple drugs, including tigecycline, in Klebsiella pneumoniae. MBio 11:e02930-19. doi: 10.1128/mBio.02930-19, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manaia C., Macedo G., Fatta-Kassinos D., Nunes O. (2016). Antibiotic resistance in urban aquatic environments: can it be controlled? Appl. Microbiol. Biotechnol. 100, 1543–1557. doi: 10.1007/s00253-015-7202-0, PMID: [DOI] [PubMed] [Google Scholar]
- Manyi-Loh C., Mamphweli S., Meyer E., Okoh A. (2018). Antibiotic use in agriculture and its consequential resistance in environmental sources: potential public health implications. Molecules 23:150689. doi: 10.3390/molecules23040795, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marathe N., Svanevik C., Ghavidel F., Grevskott D. (2021). First report of mobile tigecycline resistance gene tet(X4)-harbouring multidrug-resistant Escherichia coli from wastewater in Norway. J. Glob. Antimicrob. Resist. 27, 37–40. doi: 10.1016/j.jgar.2021.07.019, PMID: [DOI] [PubMed] [Google Scholar]
- Martelli F., Abuoun M., Cawthraw S., Storey N., Turner O., Ellington M., et al. (2022). Detection of the transferable tigecycline resistance gene tet(X4) in Escherichia coli from pigs in the United Kingdom. J. Antimicrob. Chemother. 77, 846–848. doi: 10.1093/jac/dkab439, PMID: [DOI] [PubMed] [Google Scholar]
- Miłobedzka A., Ferreira C., Vaz-Moreira I., Calderón-Franco D., Gorecki A., Purkrtova S., et al. (2022). Monitoring antibiotic resistance genes in wastewater environments: the challenges of filling a gap in the one-health cycle. J. Hazard. Mater. 424:127407. doi: 10.1016/j.jhazmat.2021.127407, PMID: [DOI] [PubMed] [Google Scholar]
- Mohsin M., Hassan B., Martins W., Li R., Abdullah S., Sands K., et al. (2021). Emergence of plasmid-mediated tigecycline resistance tet(X4) gene in Escherichia coli isolated from poultry, food and the environment in South Asia. Sci. Total Environ. 787:147613. doi: 10.1016/j.scitotenv.2021.147613, PMID: [DOI] [PubMed] [Google Scholar]
- Moore I., Hughes D., Wright G. (2005). Tigecycline is modified by the flavin-dependent monooxygenase Tet X. Biochemistry 44, 11829–11835. doi: 10.1021/bi0506066, PMID: [DOI] [PubMed] [Google Scholar]
- Munita J., Arias C. (2016). Mechanisms of antibiotic resistance. Microbiol. Spectr. 4:VMBF-0016-2015. doi: 10.1128/microbiolspec.VMBF-0016-2015, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen S., Lipsitch M., Grad Y. (2020). The role of “spillover” in antibiotic resistance. Proc. Natl. Acad. Sci. U. S. A. 117, 29063–29068. doi: 10.1073/pnas.2013694117, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson M., Ruzin A., Feyfant E., Rush T., 3rd, O'connell J., Bradford P. (2006). Functional, biophysical, and structural bases for antibacterial activity of tigecycline. Antimicrob. Agents Chemother. 50, 2156–2166. doi: 10.1128/AAC.01499-05, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan Y., Awan F., Zhenbao M., Zhang X., Zeng J., Zeng Z., et al. (2020). Preliminary view of the global distribution and spread of the tet(X) family of tigecycline resistance genes. J. Antimicrob. Chemother. 75, 2797–2803. doi: 10.1093/jac/dkaa284, PMID: [DOI] [PubMed] [Google Scholar]
- Partridge S., Kwong S., Firth N., Jensen S. (2018). Mobile genetic elements associated with antimicrobial resistance. Clin. Microbiol. Rev. 31:e00088-17. doi: 10.1128/CMR.00088-17, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng K., Li R., He T., Liu Y., Wang Z. (2020). Characterization of a porcine Proteus cibarius strain co-harbouring tet(X6) and cfr. J. Antimicrob. Chemother. 75, 1652–1654. doi: 10.1093/jac/dkaa047, PMID: [DOI] [PubMed] [Google Scholar]
- Peng Z., Hu Z., Li Z., Zhang X., Jia C., Li T., et al. (2022). Antimicrobial resistance and population genomics of multidrug-resistant Escherichia coli in pig farms in mainland China. Nat. Commun. 13:1116. doi: 10.1038/s41467-022-28750-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira A., Paranhos A., De Aquino S., Silva S. (2021). Distribution of genetic elements associated with antibiotic resistance in treated and untreated animal husbandry waste and wastewater. Environ. Sci. Pollut. Res. Int. 28, 26380–26403. doi: 10.1007/s11356-021-13784-y, PMID: [DOI] [PubMed] [Google Scholar]
- Plantinga N., Wittekamp B., Van Duijn P., Bonten M. (2015). Fighting antibiotic resistance in the intensive care unit using antibiotics. Future Microbiol. 10, 391–406. doi: 10.2217/fmb.14.146, PMID: [DOI] [PubMed] [Google Scholar]
- Poirel L., Mugnier P., Toleman M., Walsh T., Rapoport M., Petroni A., et al. (2009). ISCR2, another vehicle for blaVEB gene acquisition. Antimicrob. Agents Chemother. 53, 4940–4943. doi: 10.1128/AAC.00414-09, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter R., D'souza A., Dantas G. (2016). The rapid spread of carbapenem-resistant Enterobacteriaceae. Drug Resist. Updat. 29, 30–46. doi: 10.1016/j.drup.2016.09.002, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiao M., Ying G., Singer A., Zhu Y. (2018). Review of antibiotic resistance in China and its environment. Environ. Int. 110, 160–172. doi: 10.1016/j.envint.2017.10.016 [DOI] [PubMed] [Google Scholar]
- Qiu J., Zhao T., Liu Q., He J., He D., Wu G., et al. (2016). Residual veterinary antibiotics in pig excreta after oral administration of sulfonamides. Environ. Geochem. Health 38, 549–556. doi: 10.1007/s10653-015-9740-x, PMID: [DOI] [PubMed] [Google Scholar]
- Rehman M., Yang H., Zhang S., Huang Y., Zhou R., Gong S., et al. (2020). Emergence of Escherichia coli isolates producing NDM-1 carbapenemase from waterfowls in Hainan island, China. Acta Trop. 207:105485. doi: 10.1016/j.actatropica.2020.105485, PMID: [DOI] [PubMed] [Google Scholar]
- Rempel S., Stanek W., Slotboom D. (2019). ECF-type ATP-binding cassette transporters. Annu. Rev. Biochem. 88, 551–576. doi: 10.1146/annurev-biochem-013118-111705, PMID: [DOI] [PubMed] [Google Scholar]
- Roberts M. (2003). Tetracycline therapy: update. Clin. Infect. Dis. 36, 462–467. doi: 10.1086/367622 [DOI] [PubMed] [Google Scholar]
- Ruan Z., Jia H., Chen H., Wu J., He F., Feng Y. (2020). Co-existence of plasmid-mediated tigecycline and colistin resistance genes tet(X4) and mcr-1 in a community-acquired Escherichia coli isolate in China. J. Antimicrob. Chemother. 75, 3400–3402. doi: 10.1093/jac/dkaa317, PMID: [DOI] [PubMed] [Google Scholar]
- Ruzin A., Keeney D., Bradford P. (2007). Ade ABC multidrug efflux pump is associated with decreased susceptibility to tigecycline in Acinetobacter calcoaceticus-Acinetobacter baumannii complex. J. Antimicrob. Chemother. 59, 1001–1004. doi: 10.1093/jac/dkm058, PMID: [DOI] [PubMed] [Google Scholar]
- Sheykhsaran E., Baghi H., Soroush M., Ghotaslou R. (2019). An overview of tetracyclines and related resistance mechanisms. Rev. Med. Microbiol. 30, 69–75. doi: 10.1097/MRM.0000000000000154 [DOI] [Google Scholar]
- Shi L. D., Dong X., Liu Z., Yang Y., Lin J. G., Li M., et al. (2022). A mixed blessing of viruses in wastewater treatment plants. Water Res. 215:118237. doi: 10.1016/j.watres.2022.118237, PMID: [DOI] [PubMed] [Google Scholar]
- Speer B., Bedzyk L., Salyers A. (1991). Evidence that a novel tetracycline resistance gene found on two Bacteroides transposons encodes an NADP-requiring oxidoreductase. J. Bacteriol. 173, 176–183. doi: 10.1128/jb.173.1.176-183.1991, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein G., Babinchak T. (2013). Tigecycline: an update. Diagn. Microbiol. Infect. Dis. 75, 331–336. doi: 10.1016/j.diagmicrobio.2012.12.004, PMID: [DOI] [PubMed] [Google Scholar]
- Sun C., Cui M., Zhang S., Liu D., Fu B., Li Z., et al. (2020). Genomic epidemiology of animal-derived tigecycline-resistant Escherichia coli across China reveals recent endemic plasmid-encoded tet(X4) gene. Commun. Biol. 3:412. doi: 10.1038/s42003-020-01148-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C., Cui M., Zhang S., Wang H., Song L., Zhang C., et al. (2019). Plasmid-mediated tigecycline-resistant gene tet(X4) in Escherichia coli from food-producing animals, China, 2008–2018. Emerg. Microbes Infect. 8, 1524–1527. doi: 10.1080/22221751.2019.1678367, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun H., Wan Y., Du P., Liu D., Li R., Zhang P., et al. (2021a). Investigation of tigecycline resistant Escherichia coli from raw meat reveals potential transmission among food-producing animals. Food Control 121:107633. doi: 10.1016/j.foodcont.2020.107633 [DOI] [Google Scholar]
- Sun H., Zhai W., Fu Y., Li R., Du P., Bai L. (2021b). Co-occurrence of plasmid-mediated resistance genes tet(X4) and blaNDM-5 in a multidrug-resistant Escherichia coli isolate recovered from chicken in China. J. Glob. Antimicrob. Resist. 24, 415–417. doi: 10.1016/j.jgar.2021.02.010, PMID: [DOI] [PubMed] [Google Scholar]
- Sun J., Chen C., Cui C., Zhang Y., Liu X., Cui Z., et al. (2019). Plasmid-encoded tet(X) genes that confer high-level tigecycline resistance in Escherichia coli. Nat. Microbiol. 4, 1457–1464. doi: 10.1038/s41564-019-0496-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y., Lai Y., Kong L., Wang X., Li C., Wang Y., et al. (2021). Characterization of three porcine Escherichia coli isolates co-harbouring tet(X4) and cfr. J. Antimicrob. Chemother. 76, 263–264. doi: 10.1093/jac/dkaa384, PMID: [DOI] [PubMed] [Google Scholar]
- Thaker M., Spanogiannopoulos P., Wright G. (2010). The tetracycline resistome. Cell. Mol. Life Sci. 67, 419–431. doi: 10.1007/s00018-009-0172-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiseo K., Huber L., Gilbert M., Robinson T., Van Boeckel T. (2020). Global trends in antimicrobial use in food animals from 2017 to 2030. Antibiotics 9:918. doi: 10.3390/antibiotics9120918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong C., Xiao D., Xie L., Yang J., Zhao R., Hao J., et al. (2022). Swine manure facilitates the spread of antibiotic resistome including tigecycline-resistant tet(X) variants to farm workers and receiving environment. Sci. Total Environ. 808:152157. doi: 10.1016/j.scitotenv.2021.152157, PMID: [DOI] [PubMed] [Google Scholar]
- Tyrrell C., Burgess C. M., Brennan F., Walsh F. (2019). Antibiotic resistance in grass and soil. Biochem. Soc. Trans. 47, 477–486. doi: 10.1042/BST20180552 [DOI] [PubMed] [Google Scholar]
- Umar Z., Chen Q., Tang B., Xu Y., Wang J., Zhang H., et al. (2021). The poultry pathogen Riemerella anatipestifer appears as a reservoir for Tet(X) tigecycline resistance. Environ. Microbiol. 23, 7465–7482. doi: 10.1111/1462-2920.15632, PMID: [DOI] [PubMed] [Google Scholar]
- Usui M., Fukuda A., Suzuki Y., Nakajima C., Tamura Y. (2021). Broad-host-range Inc W plasmid harbouring tet(X) in Escherichia coli isolated from pigs in Japan. J. Glob. Antimicrob. Resist. 28, 97–101. doi: 10.1016/j.jgar.2021.12.012 [DOI] [PubMed] [Google Scholar]
- Van Boeckel T., Brower C., Gilbert M., Grenfell B., Levin S., Robinson T., et al. (2015). Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. U. S. A. 112, 5649–5654. doi: 10.1073/pnas.1503141112, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaz-Moreira I., Nunes O., Manaia C. (2014). Bacterial diversity and antibiotic resistance in water habitats: searching the links with the human microbiome. FEMS Microbiol. Rev. 38, 761–778. doi: 10.1111/1574-6976.12062, PMID: [DOI] [PubMed] [Google Scholar]
- Venter H., Mowla R., Ohene-Agyei T., Ma S. (2015). RND-type drug efflux pumps from gram-negative bacteria: molecular mechanism and inhibition. Front. Microbiol. 6:377. doi: 10.3389/fmicb.2015.00377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkers G., Palm G., Weiss M., Wright G., Hinrichs W. (2011). Structural basis for a new tetracycline resistance mechanism relying on the Tet X monooxygenase. FEBS Lett. 585, 1061–1066. doi: 10.1016/j.febslet.2011.03.012, PMID: [DOI] [PubMed] [Google Scholar]
- Wang J., Ma Z., Zeng Z., Yang X., Huang Y., Liu J. (2017). The role of wildlife (wild birds) in the global transmission of antimicrobial resistance genes. Zool. Res. 38, 55–80. doi: 10.24272/j.issn.2095-8137.2017.003, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Wang Y., Wu H., Wang Z., Shen P., Tian Y., et al. (2020). Coexistence of blaOXA-58 and tet(X) on a novel plasmid in Acinetobacter sp. from pig in Shanghai, China. Front. Microbiol. 11:578020. doi: 10.3389/fmicb.2020.578020, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Wu H., Mei C., Wang Y., Wang Z., Lu M., et al. (2021). Multiple mechanisms of tigecycline resistance in Enterobacteriaceae from a pig farm, China. Microbiol. Spectr. 9:e0041621. doi: 10.1128/Spectrum.00416-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Liu D., Lv Y., Cui L., Li Y., Li T., et al. (2019). Novel plasmid-mediated tet (X5) gene conferring resistance to tigecycline, eravacycline, and omadacycline in a clinical Acinetobacter baumannii isolate. Antimicrob. Agents Chemother. 64:e01326-19. doi: 10.1128/AAC.01326-19, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Hu Y., Cao J., Bi Y., Lv N., Liu F., et al. (2019). Antibiotic resistance gene reservoir in live poultry markets. J. Infect. 78, 445–453. doi: 10.1016/j.jinf.2019.03.012, PMID: [DOI] [PubMed] [Google Scholar]
- Wang Y., Liu F., Xu X., Huang H., Lyu N., Ma S., et al. (2021a). Detection of plasmid-mediated tigecycline resistance gene tet(X4) in a Salmonella enterica serovar Llandoff Isolate. Infect. Microb. Dis. 3, 198–204. doi: 10.1097/IM9.0000000000000077 [DOI] [Google Scholar]
- Wang Y., Liu F., Zhu B., Gao G. (2020). Discovery of tigecycline resistance genes tet(X3) and tet(X4) in live poultry market worker gut microbiomes and the surrounded environment. Sci. Bull. 65, 340–342. doi: 10.1016/j.scib.2019.12.027 [DOI] [PubMed] [Google Scholar]
- Wang Y., Lyu N., Liu F., Liu W., Bi Y., Zhang Z., et al. (2021b). More diversified antibiotic resistance genes in chickens and workers of the live poultry markets. Environ. Int. 153:106534. doi: 10.1016/j.envint.2021.106534, PMID: [DOI] [PubMed] [Google Scholar]
- Wenzel R., Bate G., Kirkpatrick P. (2005). Tigecycline. Nat. Rev. Drug Discov. 4, 809–810. doi: 10.1038/nrd1857 [DOI] [PubMed] [Google Scholar]
- Wu Y., He R., Qin M., Yang Y., Chen J., Feng Y., et al. (2022). Identification of plasmid-mediated tigecycline-resistant gene tet(X4) in Enterobacter cloacae from pigs in China. Microbiol. Spectr. 10:e0206421. doi: 10.1128/spectrum.02064-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., Zhou Y., Niu S., Liu Z., Zou Y., Yang Y., et al. (2022). A novel inhibitor of monooxygenase reversed the activity of tetracyclines against tet(X3)/tet(X4)-positive bacteria. EBioMedicine 78:103943. doi: 10.1016/j.ebiom.2022.103943, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Liu L., Zhang H., Feng Y. (2021). Co-production of Tet(X) and MCR-1, two resistance enzymes by a single plasmid. Environ. Microbiol. 23, 7445–7464. doi: 10.1111/1462-2920.15425, PMID: [DOI] [PubMed] [Google Scholar]
- Xu Y., Liu L., Sun J., Feng Y. (2019). Limited distribution and mechanism of the Tet X4 tetracycline resistance enzyme. Sci. Bull. 64, 14–17. doi: 10.1016/j.scib.2019.08.024 [DOI] [PubMed] [Google Scholar]
- Yahav D., Lador A., Paul M., Leibovici L. (2011). Efficacy and safety of tigecycline: a systematic review and meta-analysis. J. Antimicrob. Chemother. 66, 1963–1971. doi: 10.1093/jac/dkr242, PMID: [DOI] [PubMed] [Google Scholar]
- Yang L., Shen Y., Jiang J., Wang X., Shao D., Lam M., et al. (2022). Distinct increase in antimicrobial resistance genes among Escherichia coli during 50 years of antimicrobial use in livestock production in China. Nat. Food 3, 197–205. doi: 10.1038/s43016-022-00470-6 [DOI] [PubMed] [Google Scholar]
- Yang W., Moore I., Koteva K., Bareich D., Hughes D., Wright G. (2004). Tet X is a flavin-dependent monooxygenase conferring resistance to tetracycline antibiotics. J. Biol. Chem. 279, 52346–52352. doi: 10.1074/jbc.M409573200, PMID: [DOI] [PubMed] [Google Scholar]
- Yezli S., Li H. (2012). Antibiotic resistance amongst healthcare-associated pathogens in China. Int. J. Antimicrob. Agents 40, 389–397. doi: 10.1016/j.ijantimicag.2012.07.009, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y., Cui C., Kuang X., Chen C., Wang M., Liao X., et al. (2021). Prevalence of tet(X4) in Escherichia coli from duck farms in Southeast China. Front. Microbiol. 12:716393. doi: 10.3389/fmicb.2021.716393, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeballos-Gross D., Rojas-Sereno Z., Salgado-Caxito M., Poeta P., Torres C., Benavides J. (2021). The role of gulls as reservoirs of antibiotic resistance in aquatic environments: a scoping review. Front. Microbiol. 12:703886. doi: 10.3389/fmicb.2021.703886, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y., Lu J., Liu C., Ling Z., Sun Q., Wang H., et al. (2021). A method for screening tigecycline-resistant gene tet(X) from human gut. J. Glob. Antimicrob. Resist. 24, 29–31. doi: 10.1016/j.jgar.2020.11.010, PMID: [DOI] [PubMed] [Google Scholar]
- Zha L., Pan L., Guo J., French N., Villanueva E., Tefsen B. (2020). Effectiveness and safety of high dose tigecycline for the treatment of severe infections: a systematic review and meta-analysis. Adv. Ther. 37, 1049–1064. doi: 10.1007/s12325-020-01235-y, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai W., Tian Y., Lu M., Zhang M., Song H., Fu Y., et al. (2022). Presence of mobile tigecycline resistance gene tet(X4) in clinical Klebsiella pneumoniae. Microbiol. Spectr. 10:e0108121. doi: 10.1128/spectrum.01081-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Dong N., Shen Z., Zeng Y., Lu J., Liu C., et al. (2020a). Epidemiological and phylogenetic analysis reveals Flavobacteriaceae as potential ancestral source of tigecycline resistance gene tet(X). Nat. Commun. 11:4648. doi: 10.1038/s41467-020-18475-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Dong N., Zeng Y., Shen Z., Lu J., Liu C., et al. (2020b). Chromosomal and plasmid-borne tigecycline resistance genes tet(X3) and tet(X4) in dairy cows on a Chinese farm. Antimicrob. Agents Chemother. 64:e00674-20. doi: 10.1128/AAC.00674-20, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Sun J., Sun R. Y., Wang M., Cui C., Fang L., et al. (2021a). Source tracking and global distribution of the Tigecycline non-susceptible tet(X). Microbiol. Spectr. 9:e0116421. doi: 10.1128/Spectrum.01164-21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Abbas M., Rehman M. U., Huang Y., Zhou R., Gong S., et al. (2020c). Dissemination of antibiotic resistance genes (ARGs) via integrons in Escherichia coli: a risk to human health. Environ. Pollut. 266:115260. doi: 10.1016/j.envpol.2020.115260, PMID: [DOI] [PubMed] [Google Scholar]
- Zhang S., Abbas M., Rehman M. U., Wang M., Jia R., Chen S., et al. (2021b). Updates on the global dissemination of colistin-resistant Escherichia coli: an emerging threat to public health. Sci. Total Environ. 799:149280. doi: 10.1016/j.scitotenv.2021.149280, PMID: [DOI] [PubMed] [Google Scholar]
- Zhang S., Chen S., Rehman M. U., Yang H., Yang Z., Wang M., et al. (2021c). Distribution and association of antimicrobial resistance and virulence traits in Escherichia coli isolates from healthy waterfowls in Hainan, China. Ecotoxicol. Environ. Saf. 220:112317. doi: 10.1016/j.ecoenv.2021.112317, PMID: [DOI] [PubMed] [Google Scholar]
- Zhang Z., Zhan Z., Shi C. (2022). International spread of Tet(X4)-producing Escherichia coli isolates. Foods 11:2010. doi: 10.3390/foods11142010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao E., Wang X., Ji J., Wang Z., Wang Y., Cui H. (2021). Anti-tumor activity of tigecycline: a review. Sheng Wu Gong Cheng Xue Bao 37, 3031–3041. doi: 10.13345/j.cjb.200630, PMID: [DOI] [PubMed] [Google Scholar]
- Zheng X., Ma J., Lu Y., Sun D., Yang H., Xia F., et al. (2022). Detection of tet(X6) variant-producing Proteus terrae subsp. cibarius from animal cecum in Zhejiang, China. J. Glob. Antimicrob. Resist. 29, 124–130. doi: 10.1016/j.jgar.2022.02.011, PMID: [DOI] [PubMed] [Google Scholar]
- Zheng X., Zhu J., Zhang J., Cai P., Sun Y., Chang M., et al. (2020). A novel plasmid-borne tet(X6) variant co-existing with blaNDM-1 and blaOXA-58 in a chicken Acinetobacter baumannii isolate. J. Antimicrob. Chemother. 75, 3397–3399. doi: 10.1093/jac/dkaa342, PMID: [DOI] [PubMed] [Google Scholar]
- Zhong X., Xu H., Chen D., Zhou H., Hu X., Cheng G. (2014). First emergence of acr AB and oqx AB mediated tigecycline resistance in clinical isolates of Klebsiella pneumoniae pre-dating the use of tigecycline in a Chinese hospital. PLoS One 9:e115185. doi: 10.1371/journal.pone.0115185, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X., Qiao M., Su J. Q., Wang Y., Cao Z., Cheng W., et al. (2019). Turning pig manure into biochar can effectively mitigate antibiotic resistance genes as organic fertilizer. Sci. Total Environ. 649, 902–908. doi: 10.3389/fmicb.2019.02957, PMID: [DOI] [PubMed] [Google Scholar]
- Zhou Y., Liu P., Zhang C., Liao X., Sun J., Liu Y. (2019). Colistin combined with tigecycline: a promising alternative strategy to combat Escherichia coli harboring blaNDM-5 and mcr-1. Front. Microbiol. 10:2957. doi: 10.3389/fmicb.2019.02957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu D., Luo H., Liu M., Zhao X., Jia R., Chen S., et al. (2018). Various profiles of tet genes addition to tet(X) in Riemerella anatipestifer isolates from ducks in China. Front. Microbiol. 9:585. doi: 10.3389/fmicb.2018.00585, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]