Abstract
Objective
The improvement of patient experience (PE) is related to the experience of staff caring for them. Yet there is little evidence as to which interactions matter the most for both patients and staff, or how they are perceived by them. We aimed to summarise the interactions and the perceptions between patients and staff from studies by using both patient and staff experience data in healthcare institutions.
Design
Scoping review.
Methods
We conducted a scoping review, including studies dealing with PE and staff experience. Two authors independently reviewed each title/abstract and the selected full-text articles. A list of variables (objective, study design, data sources, tools used, results, interactions, perceptions and actions) was charted and summarised using a narrative approach including both qualitative and quantitative data. Studies were grouped according to their objective and the key interactions summarised according to this stratification. The perceptions of patients and staff were identified in the results of selected studies and were classified into four categories: commonalities and disagreements of perceptions, patients’ perceptions not perceived by professionals and professional’s perceptions not perceived by patients.
Results
A total of 42 studies were included. The stratification of studies by type of objective resulted in six groups that allowed to classify the key interactions (n=154) identified in the results of the selected studies. A total of 128 perceptions related to interaction between patient and staff were reported with the following distribution: commonalities (n=35), disagreements (n=18), patients’ perceptions not perceived by professionals (n=47) and professional’s perceptions not perceived by patients (n=28). We separated positive and negative perceptions, which resulted in seven scenarios, each with actions that can be carried out for one or both populations to overcome barriers.
Conclusion
The study of both patient and staff experience allowed the identification of actions that can be taken to change the perceptions of patients and staff.
Keywords: health & safety, quality in health care, education & training (see medical education & training), organisational development, public health, health policy
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This review adds a strategic value to studying both patient and staff experience by identifying the different types of perceptions according to the existing literature.
This review did not exclude any study according to quality.
The search and inclusion of studies was conducted by two reviewers, which adds to the validity of data collection.
Given the breadth of this topic, we may have missed relevant studies that did not include a required search term.
The lack of a shared definition and dimensions of staff experience prevents us from being fully exhaustive on the subject, and the heterogeneity of definition of staff experience could bring in to question the validity of pooling certain data.
Background
Patient experience (PE) has been recognised as a major lever to improve healthcare systems.1 However, there are a few studies that consider PE and the experience of the persons who work with patients every day,2 although it has been shown that the five most important components of PE are the interactions with staff3 and that both patient and staff experiences are related.4
Although there is an internationally recognised definition of PE,1 this is not the case for staff experience in healthcare studies; it is, however, defined by the UK National Health Service as ‘attitudinal or psychological factors that determine how an individual employee feels about their job, their colleagues and their organisation’,4 that is characterised by staff engagement, motivation, satisfaction, morale, work pressure, stress and intention to leave, and management behaviour and practices at work.4
The study of both experiences could allow the identification of key interactions (‘touchpoints of people, processes, policies, communications, actions and environment’1;) for patients and/or staff, and to investigate the perceptions of patients and staff of these interactions (‘what is recognised, understood and remembered’1). This could allow the identification of which interactions mattered the most for both patients and staff, and how they are perceived. This is of importance as same event or situation can be perceived differently by the patient and the staff.5
We; therefore, aimed to summarise the interactions and the perceptions from studies using both patient and staff experience data in healthcare structures. The secondary objectives were to describe the characteristics of the studies (methods implemented, tools used, quality and limitations, term used for staff experience) and the actions implemented to improve the interactions.
Methods
We conducted a scoping review. A scoping review is a synthesis technique of knowledge that is used when: it is difficult to identify a narrow review question; studies in the reviewed sources are likely to have employed a range of data collection and analysis techniques; and no prior synthesis has been undertaken on the topic.6
Data sources
We searched PubMed and Google Scholar in July 2021 for studies dealing with PE and staff experience that used patient and staff data, and that were published between 1 January 2007 and 21 July 2021. Six major search terms related to staff experience were used: staff experience, employee experience, clinician experience, physician experience, professional experience and workforce experience. A combination of multiple keywords and search terms was used (see online supplemental appendix 1).
bmjopen-2022-061155supp001.pdf (63.7KB, pdf)
Inclusion/exclusion criteria
Studies fulfilling the following criteria were included: (1) to focus on PE defined as ‘the sum of all interactions, shaped by an organisation’s culture, that influence patient perceptions, across the continuum of care’1; (2) to include patient and staff data in a common setting (no geographical or type of patient care restriction) and (3) to present original data. There was no restriction on the type of healthcare institution (public, private and academic). Studies published in a language other than English or French that did not focus on PE (but on other concepts such as patient satisfaction, engagement, etc), that focused only on trainees (residents, medical students), that only concerned staff behaviour and communication were excluded; as were opinion papers, presentations of protocol/study framework, thesis and case reports.
Study selection and data analysis
Two authors (MC and SC) independently reviewed each title/abstract and the selected full-text articles; a third author (JH) was called on to settle disagreements.
The following variables were charted: year of publication, country, term used for staff experience (physician experience, professional experience, etc), aim/objective/purpose, study design (qualitative, quantitative or mixed methods), data sources, tools used, results (key interactions and perceptions of patients and staff were dissociate), actions, conclusions and limitations. Substantial heterogeneity was anticipated in study design, measures, interventions and outcomes reported in the eligible studies, which would render it impossible to analyse pooled data; data were therefore summarised using a narrative approach including both qualitative and quantitative data.
Studies were grouped according to their objective (irrespectively of the context), and the key interactions summarised according to this stratification. The perceptions of patient and staff were identified in the results of selected studies; these were classified into four categories: (1) commonalities (when patients and staff have the same perception of a same event, situation, interaction, etc), (2) disagreements (when patients and staff do not have the same perceptions), (3) patients’ perceptions not perceived by professionals and (4) professional’s perceptions not perceived by patients. Only clear and non-anecdotal perceptions were retained, that is, those that presented an unambiguous formulation and that involved more than one individual. Commonalities and disagreements were summarised in a table and formulated in a way that does not require contextual elements to understand them.
Quality assessment
Two authors (MC and SH) independently abstracted and assessed the quality of each study; a third author (JH) was called on to settle disagreements. The studies were assessed according to their methodology (qualitative, quantitative, mixed) by using the appropriate analysis grid (Critical Appraisal Skills Programme (CASP) Qualitative Research Checklist; Effective Public Health Practice Project (EPHPP) Quality Assessment Tool; Mixed Methods Appraisal Tool (MMAT)).
Patient and public involvement
Patients and the public were not involved in this study.
Results
Selected studies
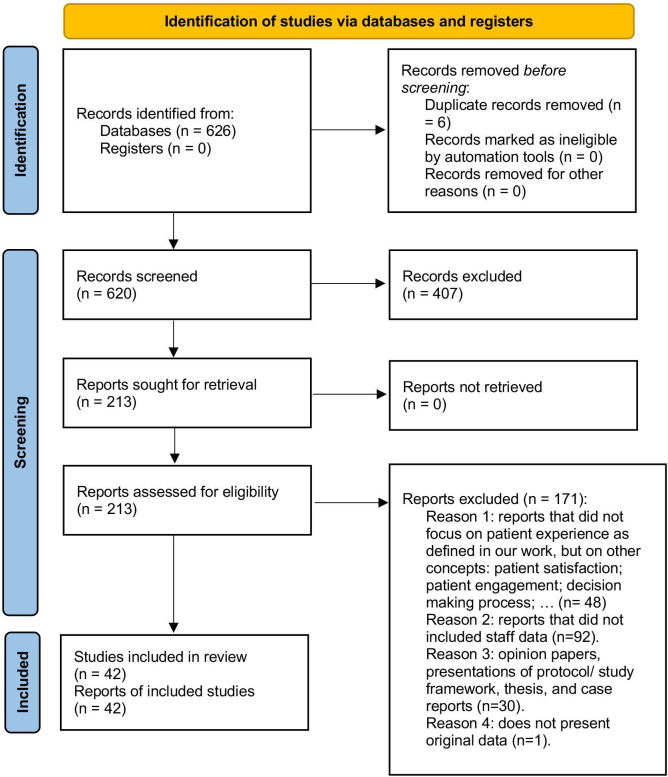
The initial search identified 626 records; there were 6 duplicates that were excluded, as were 407 records following the screening phase, and 171 after abstract and full-text assessment. Two disagreements were resolved through discussion with the third author. A total of 42 studies were included (figure 1).
Figure 1.
PRISMA 2020 flow diagram from Page et al.10 PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Country and timeline
Most studies were conducted in the UK (n=18) or in the USA (n=17). More than half of the studies (n=25) were published in the last 5 years (between 2017 and 2021).
Methodology and tools used
The study design was qualitative (n=16), quantitative (n=15) or mixed methodology (n=11). Data were collected using surveys (n=28), interviews (n=20), observation (n=8), focus groups (n=5), workshop or cocreation sessions (n=3), document analysis (n=2) and time and/or motion baseline (tools to measure the time spent, the number of steps; n=2).
Quality assessment
According to the CASP Qualitative Research Checklist, the quality of qualitative studies (n=16) was strong for 10, moderate for 3 and weak for 3. The limitations of the studies with quality issues were: insufficiently rigorous data analysis (n=5); no clear statement of findings (n=5); no description of biases of the relationship between researcher and participants (n=4); lack of detailed recruitment strategy (n=4); lack of description on the data collection (n=1); no consideration of ethical issues (n=1).
According to the EPHPP quality assessment tool, the quality of quantitative studies (n=15) was strong for 9, moderate for 3 and weak for 3. The quality issues were: selection biases (n=6); method not appropriate (n=4); lack of detailed recruitment strategy (n=1); lack of description on the data collection (n=1); no clear statement of findings (n=1).
According to the MMAT appraisal tool, the quality of mixed-method studies (n=11) was good for 4, strong limitations for 4 and poor for 3. Four studies with strong limitations raised two issues: lack of detailed of divergencies and inconsistencies between qualitative and quantitative results (n=4); lack of description of the quantitative method and results (n=3). Three studies in the poor category had an insufficiently detailed method as the articles were the presentation of the application of a programme.
Staff experience
In 42 studies, the terms used more than once were: staff experience (n=11), clinician experience (n=5) and physician experience (n=3).
Aims, results and key interactions
A total of 154 key interactions were identified in the results of the 42 studies included. The studies were classified into six groups according to their objective (irrespectively of the context). (1) Studies that explored associations between patient and staff experience (n=11) described key interactions (n=59) for patient or staff that have an impact on the other population experience (eg, work-related stress was negatively associated with PE). (2) Studies that measured the impact of a change of tool or process (n=11) presented key interactions improvements (eg, reduction in time spent on patient related administration) or failures (eg, technical problems; n=11). (3) Studies that measured the impact of a change of environment (n=3) found both improvements (eg, better patient privacy) and deteriorations (eg, patient felt isolated) of their key interactions (n=23). (4) Studies that aimed to uniquely describe the experience of patients and professionals (n=11) identified the key interactions (n=35) for patients and/or professionals (eg, waiting for medical treatments or procedures). (5) Studies that explored the perceptions of patients and professionals regarding a type of therapy or care management (n=3) identified key interactions (n=18) that were barriers to successful care management or therapy (eg, medication issues encountered by the patients). (6) Studies that evaluated the impact of a specific nurse role on the experience of patients and staff (n=3) reported improvements (eg, reduction of waiting time) in their key interactions (n=8; box 1).
Box 1. List of interactions identified in the results of selected studies, classified by groups of objective of the selected studies.
1. Explore associations between patient and staff experience (n=11 studies; n=59 key interactions identified).4 11–20
Associations between staff and patient experience (n=3 studies; n=18 key interactions identified):
Factors positively associated with patients’ responses: support from immediate managers (n=2); witnessing potential errors (n=2); effectiveness of team working (n=1); opportunities for career progression or promotion (n=1); satisfaction about the quality of work and patient care (n=1); satisfaction about the use of patient feedback (n=1) and availability of hand-washing materials (n=1).
Factors negatively associated with patients’ responses: work-related stress (n=1); working extra hours (n=1); work pressure felt by staff (n=1); poor staffing (n=1); issues with ward leadership (n=1); poor coworker relationships (n=1); staff experiencing physical violence from colleagues (n=1); staff experiencing discrimination (n=1) and staff witnessing potentially harmful errors, near misses or incidents (n=1).
Associations between staff burn-out and patient experience (n=4 studies; n=13 key interactions identified):
Neither burn-out nor engagement on their own was associated with quality or patient experience measures (n=3).
Physician burn-out had a negative impact on patient-reported experience of patient–provider communication (n=1).
Clinicians reporting more frequent symptoms of burn-out reported less ability to decompress and less feeling of activation. Individual elements of decompression (n=1) and activation (n=1) were associated with patient experience.
Clinicians feeling that their work makes a difference (n=1) and believing it is meaningful (n=1) were positively associated with patient experience with their care provider.
Elements of decompression such as being able to free one’s mind from work (n=1) and being able to disconnect from work communications such as emails (n=1) were negatively associated with patient experience with their care providers.
Clinicians with high burn-out but with high engagement had the highest average ratings for all three patient experience domains: clinician communication (n=1); overall rating of the clinician (n=1); overall rating of the clinic (n=1).
Associations between physician behaviour, work processes, and productivity and patient experience (n=1 study; n=17 key interactions identified):
Characteristics of physicians with strong productivity and strong patient satisfaction were: focused on teaching and explanations (n=1); conveys warmth from the start (n=1); well-planned flow of visit with focus on patient’s agenda (n=1); controlled script with clear parts (n=1); extremely personable (n=1); always looking for buy-in from the patient that the patient fully understands (n=1); recap the patient history (n=1); confident but not arrogant (n=1); finishes dictation and coding each day (n=1); clinical staff enters orders and prepares after-visit summary (n=1).
Characteristics of physicians with weak productivity and weak patient satisfaction: lack of being there emotionally (n=1); lack of smiling (n=1); abrupt actions (n=1); behaviour changes when not interested in the patient’s case (n=1); patients kept waiting; no handshake (n=1); sense of interrogating to get a diagnosis (n=1); no attempt to match the patient’s energy (n=1).
Associations between patient–physician communication about pain and patient and physician visit experience (n=1 study; n=5 key interactions identified):
Two communication variables—patient–physician disagreement (n=1) and patient requests for opioid dose increases (n=1)—were each associated with both worse ratings of patient experience and greater physician-reported visit difficulty.
Patient desire for increased pain medicine was positively associated with both worse ratings of patient experience and greater physician-reported visit difficulty (n=1).
Greater pain severity (n=1) and more patient questions (n=1) were each associated with greater physician-reported visit difficulty, but not with patient experience.
Associations between staff civility climate and civility towards patients (n=1study; n=5 key interactions identified):
Positive association between civility climate and civility toward patients (n=1).
Direct effect of civility climate on overall hospital rating (n=1); intent to recommend (n=1); and willingness to return (n=1) and an indirect effect mediated by civility toward patients (n=1).
Associations between patient experience and patient–physician racial/ethnic and gender concordance (n=1; n=1 key interactions identified):
Compared with racially/ethnically concordant patient–physician dyads, discordance was associated with a lower likelihood of physicians receiving the maximum score (n=1).
2. Measure the impact of a change of tool or process (n=11 studies; n=11 key interactions identified).21–31
The change of tool (eg, mobile devices) or process (eg, hospital discharge process) had a positive impact on: feedback from patients and staff (n=2); reduction in time spent on patient related administration (n=2); collaborative work between professionals (n=1); patient grievances (n=1).
The change negatively impacts the emergency admissions (n=1) but positively impacts elective admissions (n=1) and outpatient attendance (n=1).
Technical problems experienced by patients (=1) and clinicians (n=1).
3. Measure the impact of a change of environment (n=3 studies; n=23 key interactions identified).32–34
The impact of a change of environment (eg, single rooms) was positively reported by patients for: comfort (n=1); privacy (n=1); confidentiality (n=1); flexibility for visitors (n=1); trust of the physicians (n=1); better experience with their care (n=1); better interactions with physicians (n=1); better access to care (n=1); better care coordination (n=1); better involvement in their care (n=1).
Patients used more email, phone and specialist visits, but fewer emergency services (n=1).
The impact of a change of environment were positively reported by staff for: patient comfort (n=1); patient confidentiality (n=1); patient care (n=1); relationships with patients (n=1); comprehension of environmental and social factors affecting patients (n=1); reduction of staff burn-out (n=1).
The negative impact for patients was the feeling of isolation (n=1).
The negative impact for staff were: worse for visibility (n=1); surveillance (n=1); teamwork (n=1); monitoring and keeping patients safe (n=1); increased walking distances (n=1).
4. Investigate the experience of patients and professionals (n=11 studies; n=35 key interactions identified).35–45
Factors, themes and issues that are key concerns for patient and/or professionals, and that could improve patient and/or staff experience: communication and information flow (n=10); environmental context and resources (n=8); personal relationships between patient and staff (n=6); waiting for medical treatments or procedures (n=3); staff morale (n=2); treatment of condition (n=2); organisational and administrative issues (n=1); patient’s transport solution (n=1); patient’s transition from home to hospital (n=1); lack of a consistent approach in identifying and preparing patients for treatment (n=1).
5. Explore the perceptions of patients and professionals regarding a type of therapy or care management (n=3 studies; n=18 key interactions identified).7 46–48
Key barriers to successful care management or therapy: patients’ personal constraints (n=3); patients’ social constraints (n=3); communication failures encountered by the patients (n=2); medication issues encountered by the patients (n=3); healthcare system barriers encountered by the patients to collaborate with their clinicians (n=2); lack of knowledge of patient (n=2); patients’ feeling isolated with their symptom (n=1) and patient’s feeling stress (n=1); environmental context and resources (n=1).
6. Evaluate the impact of a specific nurse role (eg, advanced nurse practitioner) on the experience of patients and staff (n=3 studies; n=8 key interactions identified).48–50
Improved communications between the patient and the service (n=2); positive impact on care (n=1); better coordination of services (n=1); patients described an increased level of confidence in the service (n=1); reduction in unnecessary hospital admissions (n=1); reduction of waiting time (patient’s perceptions; n=1); improved practice (n=1).
Commonalities and disagreements in perceptions
A total of 128 perceptions related to interaction between patient and staff were reported in the 42 included studies. The perceptions were commonalities (n=35), disagreements (n=18), patients’ perceptions not perceived by professionals (n=47) and professional’s perceptions not perceived by patients (n=28). The commonalities (n=35) were either win–win interactions (n=21) where patients and staff both had positive perceptions, or deadlock interactions (n=14) with negative perceptions on both sides. Disagreements in perceptions (n=18) were either staff having a positive perception while patients had a negative perception (n=15) or the converse (n=3); in the former, staff thought they were doing the right thing (eg, providing sufficient information, providing clear information) while patients reported negative perceptions on these, and in the latter, patients reported good patient experience while staff reported poor experience or assumed that the patient had a poor experience. The patients’ perceptions not perceived by staff (n=47) where either positive (n=8) or negative (n=39). These perceptions either concerned staff, processes, policies or environment. The perceptions concerning staff were blind spots of the staff on their attitudes (eg, importance of smiling), patients’ fears that prevent them from interacting as they would like with staff (eg, patients were afraid to be judged by staff), and aspects that patients hid from staff (eg, concealment of significant symptoms). The professional’s perceptions not perceived by patients (n=28) had a focus on issues encountered to deliver a good patient experience (box 2).
Box 2. Summary of patient and staff perceptions in the selected studies.
Commonalities (n=35).
Positive perceptions on both sides (n=21).
Reassurance (n=5): Patients needed reassurance and felt that staff were helping them to feel better. Staff perceived the need for reassurance and tried to be attentive and sensitive to the patients.
Popularisation of explanations (n=4): Patients had a better understanding thanks to a popularisation of explanations. Staff tried to facilitate the understanding of the patients (choice of words, use of sketches, etc.).
Quality of work and patient care (n=2): Patients were satisfied with the quality of care they received. Staff were satisfied with the quality of work and patient care they were able to deliver.
Personal relationships (n=2): Both patients and staff reported that the knowledge of the interlocutor provided a better interaction and the development of personal relationship.
Discretionary care (n=1): Patients were cognisant of their vulnerability to becoming seen by staff as difficult or demanding patients and sought to manage their relationships with staff accordingly. Staff reported having patients for whom they preferred to care for and by extension offer good care selectively to them.
Communication facility (n=1): Patients and physicians reported being comfortable discussing primary non-compliance.
Feeling care (n=1): Patients reported that their clinicians made them feel cared for. Clinicians tended to treat patients in the same way as family members.
Listening (n=1): Patients felt to be listened to and understood. Staff took time to listen non-judgementally.
Professionalism (n=1): Patients described the professionalism of their clinicians. Clinicians were aware of their professional image and tended to appear calm regardless of the circumstances.
Respect and grievances (n=1): Patients reported better communication with staff and better courtesy and respect from staff. Staff reported hearing fewer grievances from patients.
Skills training (n=1): Professionals provided progressive patients skills training. Patients felt more aware and described an increase of their knowledge.
Summary notes (n=1): Both patient and staff felt that summary notes helped patients to better understand their care, through both improved recall and enhanced communication.
Negative perceptions on both sides (n=14).
Time constraints (n=3): Patients and staff felt that the staff’s time constraints affected the availability of staff, the interactions with the patients and the quality of service.
Administrative issue (n=2): Patients and staff identified similar administrative issues impacting interactions and care delivery.
Organisational issues (n=2): Patients and staff identified similar organisational issues impacting the interactions with patients and the quality of service.
Absence of interaction (n=1): Reciprocal dynamic where both patients and staff withdrew from interactions, having felt the other did not want to engage with them.
Burn-out (n=1): Converging views of patient and staff on the impact of staff burn-out on communication.
Confidentiality (n=1): Both patients and staff reported privacy issues during the interactions.
Discretionary care (n=1): Patients reported dehumanising aspects of their care; staff saw these patients as difficult or demanding.
Environment (n=1): Patients and staff highlighted that noisy, distracting and demanding environment impact on the therapeutic quality of one-to-ones.
Lack of staff (n=1): Patients and staff felt that the lack of staff affects the availability of nursing staff and impact on rehabilitation.
Respect of patient intimacy (n=1): Both practitioners and patients reported negative perceptions on the respect of patients’ intimacy.
Disagreements (n=18).
Staff had a positive perception while patient had negative perception (n=15).
Diverging views on the amount of information (n=4): Patients were unaware of information, had to ask for more information while staff thought they deliver enough information.
Diverging views on the quality of information (n=3): Patients were confused about some aspect of disease process, role of medications, or treatment plan while staff thought patients were fully aware of them.
Divergences in expectations (n=3): Patients wanted to talk about different points (quality of life, different health issues, family, …), while physicians focused on the characteristics of the disease and asked very specific question.
(Ambulance Service) diagnosis (n=1): Patient did not want to hear diagnosis, while clinicians assumed that patients expected them to offer a diagnosis and felt that they had a duty to be honest to patients.
Disparity between staff self-reported care performance and patient rated care performance (n=1): Staff consistently rated the patient care they provided much higher than the ratings of the patients themselves.
Loneliness and anxiety (n=1): Patients felt loneliness and anxiety, specifically between diagnosis and commencement of treatment, when interactions with health professionals were minimal. Health professionals perceived patients to be under this level of stress.
Pharmacological approach (n=1): Management of condition was influenced by the clinical condition and was pharmacologically driven. Patient lacked understanding of the pharmacological approach and perceived a loss of control.
Wrong assumption (n=1): Elderly patients wanted to talk about sexual function. Health professionals indicated that older patients were not interested in sexual rehabilitation.
Staff had a negative perception while patient had positive perception (n=3).
After implementing a programme (n=1): Patient reported a more positive experience with staff while staff did not report reduced barriers with patients or a better care experience.
Telemedicine 1/2 (n=1): Patients wanted and were comfortable doing telemedicine while professionals thought patient were not ready for it.
Telemedicine 2/2 (n=1): Non-shared satisfaction about telemedicine. High level of satisfaction was reported by patients, while clinicians reported dissatisfaction due to technical problems and complexity of the platform.
Patients’ perceptions not perceived by staff (n=47).
Positive perception (n=8).
Staff knowing the patient (n=1): Patients said they felt reassured when staff clearly knew about them.
Personable (n=1): Patients were satisfied when physicians were extremely personable, connected with every patient.
Recap history (n=1): Patients were satisfied when their physicians recapped their history.
Staff confidence (n=1): Patients were satisfied when their physicians were confident but not arrogant.
Warmth (n=1): Patients were satisfied when their physicians conveyed warmth from the start.
Negative perception (n=39).
Waiting (n=6): Patients had to wait for medical treatments or procedures or results. Staff seemed to be unaware of this issue.
Quality of information (n=3): Patients were confused about some aspect of disease process, role of medications, or treatment plan. Staff did not mention information issues.
Involved in decisions (n=2): Patients felt that their physician was or was not involving them in the care decisions.
Rigidity of process (n=2): Patients reported frustration with rules and procedures but never mentioned discussing these system issues with physicians.
Fear to be stigmatise (n=2): Patients were afraid to be judged by staff.
Isolation (n=2): Patients felt alone and isolated. Staff did not discuss this issue.
Access to medications (n=1): Patients hid from clinicians their problems obtaining medications.
Choose the physician (n=1): Patients found difficulties to see a physician or nurse of their choice.
Compared care with other patients (n=1): Patients observed the care other patients receive, they tended to note and reflect on, the witnessed care of patients who they felt to be more vulnerable than themselves.
Concealment of symptoms (n=1): Patients’ concealment of significant symptoms.
Concerns (n=1): Patients felt their concerns were dismissed.
Emotional implication (n=1): Patients felt that staff were not there emotionally.
Energy (n=1): Patients were not satisfied when physicians did not attempt to match their energy.
Fear of complaining (n=1): Patients feared to become unpopular with staff or care worsening as a result.
Handshake (n=1): Patients were not satisfied when physicians did not handshake.
Health beliefs (n=1): Health beliefs were omitted by the patients from discussions with physicians.
Heavy-handed (n=1): Patients believed that staff were unnecessarily heavy-handed.
Importance of smile (n=1): Patients were not satisfied when physicians lack of smiling.
Interest of physician (n=1): Patients were not satisfied when the behaviours of physicians changed when they were not interested in their case.
Interrogating (n=1): Patient did not appreciate the sense of interrogating to get a diagnosis.
Knowledge of the patient (n=1): Patients felt insecure if the nurse did not appear to know about their care or treatments.
Lack of interaction (n=1): Patient felt that staff’s lack of communication during interaction.
Memory (n=1): Patients were unable to remember what they had been told because of their disease.
Must repeat (n=1): Patients needed to repeat information to staff.
Other treatment (n=1): Patients were looking for a cure and/or better treatment options.
Social and work challenges (n=1): Patient fear to speak of social and work challenges.
Softness in gestures (n=1): Patients were not satisfied when their physicians made abrupt actions.
Staff workload (n=1): Patients did not always ask for help when needed because they thought that staff were too busy.
Staff’s perceptions not perceived by patients (n=28).
Trainings (n=5): Lack or inadequacy of trainings that impact the interactions with the patients.
Coworker relationships (n=5): Importance of coworker relationship and collaboration to deliver a good patient experience.
Autonomy and decision making (n=3): Staff felt their level of discretion and autonomy in making decisions at work was insufficient to deliver a good patient experience.
Time constraints (n=3): Staff felt that the time schedule/time pressure affect their availability and quality of service/care.
Staffing level (n=2): Inadequate or unpredictable staffing levels that impacted patient experience.
Tools (n=2): Issues encountered with tools that impacted interactions and patient experience.
Confidentiality and privacy (n=1): Staff expressed concerns regarding confidentiality, discomfort at talking about a patient in front of them, lack of privacy leading to divulging sensitive information.
Inadequate resources to work with (n=1): Inadequate resources to work that impacted staff care (tools, syringes, gloves, …) and patient experience.
Information transfer (n=1): Issues with the information transfer were encountered by staff and impacted the patient experience.
Job title (n=1): Staff noted that patients are more likely to share sensitive information with the physician only.
Keep reminding (n=1): Staff needed to keep reminding patients of the time of their appointments and how to prepare for them.
Logistical problem (n=1): Staff reported logistic issues that affect both experiences.
Organisational (n=1): Organisational and administrative issues impacting on care delivery and both experiences.
Workload (n=1): Staff reported too much workload that affect both experiences.
Actions taken
The actions (n=19) developed in reply to the results of selected studies concerned either patients (n=8), staff (n=8) or both patients and staff (n=4).
The actions developed for the patients were: admission or discharge pack (n=2); checklist to help patients to prepare their visit (n=1); information kit (n=1); postcard to help patients navigate around the hospital (n=1); tool to help patients explain what they are going through to their family or caregivers (n=1); improvements in the environment in which patients are treated (n=1); instruments to measure PE (n=1).
The actions developed for the staff were: tools to help staff (educational tool to help physicians broaden their understanding of the kinds of behaviours and characteristics expected by patients, and an online tool to facilitate communication among nurses; n=2); communication training (individual, n=1; group, n=1); shadow coaching programme for physicians (n=1); development of autonomous nursing actions (n=1); changes in the nurses’ schedule (n=1).
The actions developed that involved both patients and staff (n=4) showed initiatives that encouraged staff to adopt new postures (eg, trained nurses acting as coaches for the patients, n=1) and to create new moments for exchange (eg, development of staff feedback to patients, n=1). Another action was the inclusion of peer support in the development of a new programme (eg, development of a prehabilitation programme (inclusion of peer support, group exercises and a multidisciplinary team education approach, n=1)). Furthermore, the actions described initiatives that encourage a greater involvement of patient and their family members in their care and to develop a partnership between patients and staff (eg, development of meetings where staff, patients and family members can share their experiences, n=1).
Discussion
The study of perceptions allows to understand how the interactions between patients and staff are perceived by both populations, and this study identified seven scenarios, each with actions that can be carried out. These include win–win interactions with positive perceptions of patients and staff; these touchpoints can be seen as pillars of the experience and be fostered and deployed. Conversely, there are also deadlock interactions with negative perceptions on both sides, which should be treated as a priority since both populations suffer from them. There are also interactions where patients and staff disagree, for instance when the staff believe they are doing the right thing, but the patient is not satisfied; one answer to such interactions is to raise awareness among staff on what patients are going through and what they expect. Conversely, patients may be satisfied but staff unsatisfied; to retain patient satisfaction, it seems important to help staff with their issues so that they continue to invest in these interactions. In addition, there are two scenarios where the staff are unaware of patient perception, the first is the stroke of luck with satisfied patients but staff who seem unaware of the impact of their actions; in such cases, there is a need to raise staff awareness so that they continue. The second is blind spot when patients are unsatisfied and staff who are unaware of their difficulties; there are two situations in such cases, either staff understanding of the PE or the patient is hiding information from staff. The first could require raising awareness or to develop training for professionals, and the second is more problematic as it is related to patient’s fears and culture, but it remains one of the most essential perceptions to prioritise since it can prevent the correct treatment or diagnosis of the patient (eg, patients hide from physicians their problems obtaining medication, concealment of significant symptoms).7 The last scenario is when professional’s perceptions are not perceived by patients; such situations are more related to their work than to their postures with patients, and staff describe very practical needs: training, tools, level of autonomy, etc.
Furthermore, studies that consider both patient and staff experience lead to specific actions deployed to improve one or both experiences. The actions developed only for patients show improvements that target different stages of the patient journey: pre-admission, admission, movement within the establishment, etc. For professionals, the actions described are linked either to themes that depend on human resources (training and coaching, educational tool, level of autonomy), or to subjects related to the organisation of work (changes in schedule, tool to help communication during a team change). The actions developed that involved both populations include improvements that are longer and more complex, but which are also part of deeper changes in perceptions and practices; an example of such action is the development of the patient participation in healthcare and within the health system.8 9 The results here indicate that this integration of the perspective of patients and their family members is not limited to the patient but is a request made by both patients and staff to improve both experiences.
Three main expectations emerged from patients and can be translated into proposals or recommendations for staff to improve their interactions with patients. (1) Ensuring personalised interactions (eg, knowing the staff member or being able to choose who they will meet). The patients expect staff to have a good knowledge of their case (eg, staff who clearly knows the patient’s medial file, as well as their treatment, and the patient does not have to repeat information). (2) Being pleasant and adopting welcoming postures (eg, handshake, smile, showing emotional implication). (3) Adopting a more patient-centred approach with the patients during the investigation. The latter is of importance as patients have a negative perception when the investigation is only driven by clinical condition, and in such cases they do not spontaneously mention opinion, belief or fear that could have an impact on their treatment (eg, financial issues, family matters, health beliefs). Patients also are disappointed by the lack of information that are meaningful to them and could have a strong impact on their daily life (eg, quality of life, autonomy, sexual rehabilitation). For instance, Newcomb et al described the concealment of significant asthma symptoms by patients from clinicians during hospital visits; the authors suggest that this was due to a lack of questioning/investigation by staff and that this lack of communication promoted visit efficiency but hindered therapeutic dialogue.7
A strong point of this review is that it adds a strategic value to studying both patient and staff experience, by identifying the different types of perceptions according to the existing literature, without excluding any study according to quality. In addition, the search and inclusion process were conducted by two reviewers, which adds to the validity of data collection. The review does, however, have certain limitations. For instance, given the breadth of this topic, we may have missed relevant studies that did not include a required search term. In addition, the lack of a shared definition and dimensions of staff experience prevents us from being fully exhaustive on the subject and the heterogeneity of definition of staff experience could bring in to question the validity of pooling certain data.
Conclusions
The study of both patient and staff experience allows healthcare facilities to identify the actions that can be taken to change the perceptions of patients and staff; among them, the actions directed to both populations include the development of patient partnership, a promising field for reinforcing ownership of action by professionals and patients, therefore optimising the efficiency of quality and safety improvement actions.
Supplementary Material
Acknowledgments
The authors acknowledge and thank Philip Robinson for his assistance with the search and review.
Footnotes
Twitter: @JulieHaeseb
Contributors: MC, PM and JH conceived and designed the study, drafted the manuscript. SC and SH acquired, analysed and interpreted the data. MC is responsible for the overall content as guarantor and accepts full responsibility for the work and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
The data that support the findings of this study are available from the corresponding author, MC, upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Wolf JA, Niederhauser V, Marshburn D. Defining patient experience. Patient Exp J 2014;1:7–19. [Google Scholar]
- 2.Christensen T. Rebalancing the patient experience: 20 years of a pendulum swing. Patient Exp J 2017;4:6–8. 10.35680/2372-0247.1257 [DOI] [Google Scholar]
- 3.Wolf JA. Consumer perspectives on patient experience 2018. The Beryl Institute, 2018. [Google Scholar]
- 4.Dawson J. Links between NHS staff experience and patient satisfaction: analysis of surveys from 2014 and 2015. NHS 2018. [Google Scholar]
- 5.Maben J, Peccei R, Adams M. Patients’ experiences of care and the influence of staff motivation, affect and wellbeing. NIHR 2012. [Google Scholar]
- 6.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 7.Newcomb PA, McGrath KW, Covington JK, et al. Barriers to patient-clinician collaboration in asthma management: the patient experience. J Asthma 2010;47:192–7. 10.3109/02770900903486397 [DOI] [PubMed] [Google Scholar]
- 8.Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff 2013;32:223–31. 10.1377/hlthaff.2012.1133 [DOI] [PubMed] [Google Scholar]
- 9.Karazivan P, Dumez V, Flora L, et al. The patient-as-partner approach in health care: a conceptual framework for a necessary transition. Acad Med 2015;90:437–41. 10.1097/ACM.0000000000000603 [DOI] [PubMed] [Google Scholar]
- 10.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boffeli TJ, Thongvanh KL, Evans SJH, et al. Patient experience and physician productivity: debunking the mythical divide at HealthPartners clinics. Perm J 2012;16:19–25. 10.7812/TPP/12-049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chung S, Dillon EC, Meehan AE, et al. The relationship between primary care physician burnout and patient-reported care experiences: a cross-sectional study. J Gen Intern Med 2020;35:2357–64. 10.1007/s11606-020-05770-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henry SG, Bell RA, Fenton JJ, et al. Communication about chronic pain and opioids in primary care: impact on patient and physician visit experience. Pain 2018;159:371–9. 10.1097/j.pain.0000000000001098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howell TG, Mylod DE, Lee TH, et al. Physician burnout, resilience, and patient experience in a community practice: correlations and the central role of activation. J Patient Exp 2020;7:1491–500. 10.1177/2374373519888343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maben J, Adams M, Peccei R, et al. ‘Poppets and parcels’: the links between staff experience of work and acutely ill older peoples' experience of hospital care. Int J Older People Nurs 2012;7:83–94. 10.1111/j.1748-3743.2012.00326.x [DOI] [PubMed] [Google Scholar]
- 16.Oppel E-M, Mohr DC. ‘Paying it forward’: The link between providers’ civility climate, civility toward patients and patient experience outcomes. Health Care Manage Rev 2020;45:141–50. 10.1097/HMR.0000000000000209 [DOI] [PubMed] [Google Scholar]
- 17.Raleigh VS, Hussey D, Seccombe I, et al. Do associations between staff and inpatient feedback have the potential for improving patient experience? An analysis of surveys in NHS acute trusts in England. Qual Saf Health Care 2009;18:347–54. 10.1136/qshc.2008.028910 [DOI] [PubMed] [Google Scholar]
- 18.Scheepers RA, Lases LSS, Arah OA, et al. Job resources, physician work engagement, and patient care experience in an academic medical setting. Acad Med 2017;92:1472–9. 10.1097/ACM.0000000000001719 [DOI] [PubMed] [Google Scholar]
- 19.Takeshita J, Wang S, Loren AW, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw Open 2020;3:e2024583. 10.1001/jamanetworkopen.2020.24583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Willard-Grace R, Knox M, Huang B, et al. Primary care clinician burnout and engagement association with clinical quality and patient experience. J Am Board Fam Med 2021;34:542–52. 10.3122/jabfm.2021.03.200515 [DOI] [PubMed] [Google Scholar]
- 21.Algauer A, Rivera S, Faurote R. Patient-centered care transition for patients admitted through the ED: improving patient and employee experience. J Patient Exp 2015;2:25–8. 10.1177/237437431500200106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Banks J, Corrigan D, Grogan R, et al. LoVE in a time of CoVID: clinician and patient experience using telemedicine for chronic epilepsy management. Epilepsy Behav 2021;115:107675. 10.1016/j.yebeh.2020.107675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barkai G, Gadot M, Amir H, et al. Patient and clinician experience with a rapidly implemented large-scale video consultation program during COVID-19. Int J Qual Health Care 2021;33:mzaa165. 10.1093/intqhc/mzaa165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bohot KL, Hammond RC, Stanbrook TA. An organisational study into the impact of mobile devices on clinician and patient experience in Auckland, New Zealand. Patient Exp J 2017;4:79–89. 10.35680/2372-0247.1159 [DOI] [Google Scholar]
- 25.Congiusta S, Ascher EM, Ahn S, et al. The use of online physician training can improve patient experience and physician burnout. Am J Med Qual 2020;35:258–64. 10.1177/1062860619869833 [DOI] [PubMed] [Google Scholar]
- 26.Crucefix AL, Fleming APL, Lebus CS, et al. Sharing a written medical summary with patients on the post-admission ward round: a qualitative study of clinician and patient experience. J Eval Clin Pract 2021;27:1235–42. 10.1111/jep.13574 [DOI] [PubMed] [Google Scholar]
- 27.Derrick LM, Mangold K. Education resource nurse: engaging clinical nurses to enhance the patient experience. Nurs Adm Q 2020;44:159–67. 10.1097/NAQ.0000000000000415 [DOI] [PubMed] [Google Scholar]
- 28.Di Capua P, Clarke R, Tseng C-H, et al. The effect of implementing a care coordination program on team dynamics and the patient experience. Am J Manag Care 2017;23:494–500. [PubMed] [Google Scholar]
- 29.Hakim A. E-prescribing and primary noncompliance: physician and patient experience. Prof Case Manag 2010;15:62–7. 10.1097/NCM.0b013e3181bcc823 [DOI] [PubMed] [Google Scholar]
- 30.McNicholas A, McCall A, Werner A, et al. Improving patient experience through nursing satisfaction. J Trauma Nurs 2017;24:371–5. 10.1097/JTN.0000000000000328 [DOI] [PubMed] [Google Scholar]
- 31.Roland M, Lewis R, Steventon A, et al. Case management for at-risk elderly patients in the English integrated care pilots: observational study of staff and patient experience and secondary care utilisation. Int J Integr Care 2012;12:e130. 10.5334/ijic.850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maben J, Griffiths P, Penfold C, et al. One size fits all? Mixed methods evaluation of the impact of 100% single-room accommodation on staff and patient experience, safety and costs. BMJ Qual Saf 2016;25:241–56. 10.1136/bmjqs-2015-004265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reid RJ, Fishman PA, Yu O, et al. Patient-Centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care 2009;15:e71–87. [PubMed] [Google Scholar]
- 34.Clair MCS, Sundberg G, Kram JJF. Incorporating home visits in a primary care residency clinic: the patient and physician experience. J Patient Cent Res Rev 2019;6:203–9. 10.17294/2330-0698.1701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allen J, Child A, Mertens S. The development of an end-to-end service solution to support lupus patients and improve their experience in clinical trials. Clin Trials 2019;16:71–80. 10.1177/1740774518811111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown EJ, Kangovi S, Sha C, et al. Exploring the patient and staff experience with the process of primary care. Ann Fam Med 2015;13:347–53. 10.1370/afm.1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bruton J, Norton C, Smyth N, et al. Nurse handover: patient and staff experiences. Br J Nurs 2016;25:386–93. 10.12968/bjon.2016.25.7.386 [DOI] [PubMed] [Google Scholar]
- 38.Hasson F, Muldrew D, Carduff E, et al. ‘Take more laxatives was their answer to everything’: a qualitative exploration of the patient, carer and healthcare professional experience of constipation in specialist palliative care. Palliat Med 2020;34:1057–66. 10.1177/0269216319891584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hull KL, Quann N, Glover S, et al. Evaluating the clinical experience of a regional in-center nocturnal hemodialysis program: the patient and staff perspective. Hemodial Int 2021;25:447–56. 10.1111/hdi.12953 [DOI] [PubMed] [Google Scholar]
- 40.Insua-Summerhays B, Hart A, Plummer E, et al. Staff and patient perspectives on therapeutic engagement during one-to-one observation. J Psychiatr Ment Health Nurs 2018;25:546–57. 10.1111/jpm.12497 [DOI] [PubMed] [Google Scholar]
- 41.Milosevic M, Brborovic H, Mustajbegovic J, et al. Patients and health care professionals: partners in health care in Croatia? Br J Health Psychol 2014;19:670–82. 10.1111/bjhp.12062 [DOI] [PubMed] [Google Scholar]
- 42.Morris R, Payne O, Lambert A. Patient, carer and staff experience of a hospital-based stroke service. Int J Qual Health Care 2007;19:105–12. 10.1093/intqhc/mzl073 [DOI] [PubMed] [Google Scholar]
- 43.Nightingale JM, Murphy F, Eaton C, et al. A qualitative analysis of staff-client interactions within a breast cancer assessment clinic. Radiography 2017;23:38–47. 10.1016/j.radi.2016.08.004 [DOI] [PubMed] [Google Scholar]
- 44.Tang CY, Turczyniak M, Sayner A, et al. Adopting a collaborative approach in developing a prehabilitation program for patients with prostate cancer utilising experience-based co-design methodology. Support Care Cancer 2020;28:5195–202. 10.1007/s00520-020-05341-z [DOI] [PubMed] [Google Scholar]
- 45.Togher FJ, Davy Z, Siriwardena AN. Patients’ and ambulance service clinicians’ experiences of prehospital care for acute myocardial infarction and stroke: a qualitative study. Emerg Med J 2013;30:942–8. 10.1136/emermed-2012-201507 [DOI] [PubMed] [Google Scholar]
- 46.Glidewell L, Boocock S, Pine K, et al. Using behavioural theories to optimise shared haemodialysis care: a qualitative intervention development study of patient and professional experience. Implement Sci 2013;8:118. 10.1186/1748-5908-8-118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Newbold A, Hardy G, Byng R. Staff and patient experience of improving access to psychological therapy group interventions for anxiety and depression. J Ment Health 2013;22:456–64. 10.3109/09638237.2013.815333 [DOI] [PubMed] [Google Scholar]
- 48.Leighton Y, Clegg A, Bee A. Evaluation of community matron services in a large metropolitan City in England. Qual Prim Care 2008;16:83–9. [PubMed] [Google Scholar]
- 49.Masters E, Weston C, Chisholm J, et al. Role of the advanced nurse practitioner within teenage and young adult oncology. What is the impact on patient and staff experience of a new nurse practitioner role to a teenage and young adult service? J Adolesc Young Adult Oncol 2019;8:668–73. 10.1089/jayao.2019.0020 [DOI] [PubMed] [Google Scholar]
- 50.Wand T, Collett G, Cutten A, et al. Patient and staff experience with a new model of emergency department based mental health nursing care implemented in two rural settings. Int Emerg Nurs 2021;57:101013. 10.1016/j.ienj.2021.101013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061155supp001.pdf (63.7KB, pdf)
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, MC, upon reasonable request.