Key features.
The Lifelines Cohort (Lifelines) is a large population-based multi- disciplinary dynamic cohort and biobank which facilitates FAIR (findable, accessible, interoperable and reusable) research on healthy ageing. Over 167 000 participants were included at baseline, with the aim to follow up for at least 30 years.
To questionnaires, new dimensions in work, health status, lifestyle, stress and psychosocial parameters were added. New collected samples included hair, feces, cord blood, placental tissue and breast milk. New measurements for cognition, eye function and vitamin status were added. Brain MRI (magnetic resonance imaging) and lung CT (computed tomography) were performed. Linkage with noise and air pollution exposure and various other registries is made possible. Finally, the number of participants with GWAS (genome-wide association studies) data is largely extended.
More than 70% participated in both the baseline and the second assessment.
Lifelines is open to researchers worldwide and provides easy access to data and samples [www.lifelines.nl/researcher].
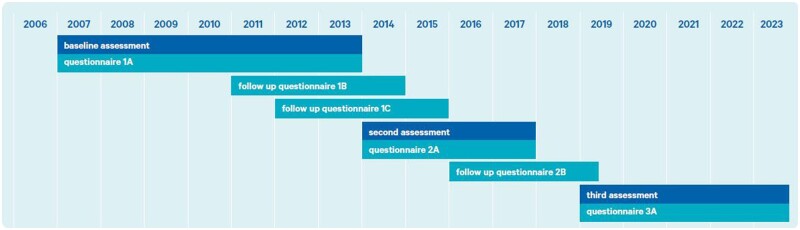
The original cohort
The Lifelines Cohort (Lifelines) is a large population-based multidisciplinary dynamic cohort and biobank designed to unravel the determinants of healthy ageing. Lifelines continuously generates deep pheno- and genotypic data to enable research on the development of chronic and rare diseases and their risk factors with the ultimate goal to contribute to healthy ageing, public health and precision medicine. Between 2006 and 2013, 10% (around 167 000) of the northern population of The Netherlands aged 0 to 93 years was enrolled using a three-generation recruitment design, as described previously.1 Data are collected through questionnaires (all ages) and measurements (age 8 years and older) on physical and mental health, lifestyle and the exposome. Furthermore, the Lifelines biobank has samples (blood, plasma, serum, hair, urine and feces) stored in a freezer warehouse (from age 8 years and older). Lifelines allows analyses at multiple levels, ranging from genetic and molecular domains through clinical, psychosocial and environmental determinants of health and disease, which allows for analyses within specific domains and also inter- and multidisciplinary analyses. All participants are invited for follow-up assessments every 5 years including a comprehensive questionnaire, and will be followed for at least 30 years (Figure 1). In between assessments, follow-up questionnaires are completed approximately once every 1.5–2.5 years.
Figure 1.
Timeline of Lifelines data collections
What is the reason for the new data collection?
The protocol of the study waves is largely fixed to enable longitudinal analyses into changes in health over the life course. However, there is flexibility in additions to the protocol to adapt to societal developments of public health importance, which resulted in new data on, for example, vaccinations, prevention programmes and COVID-19.
What will be the new areas of research?
Lifelines additionally started collecting hair and fecal samples to research the influence of cortisol and the microbiome, respectively, on healthy ageing. Furthermore Cogstate,2 a test to monitor cognitive change, was introduced and a jump height measurement was added to study physical strength (Table 1). Furthermore, new topics were added to the questionnaires over time; more details can be found in Table 2. Finally, the number of participants with available genome-wide data increased from 15 000 to 51 000 within the UMCG (University Medical Center Groningen) Genetics Lifelines Initiative (UGLI), and we are under way to increase this number to 110 000 participants.
Table 1.
Number of participants with specific examination data from general Lifelines visits
| Baseline | 2nd assessment | 3rd assessment | |||
|---|---|---|---|---|---|
| Year | 2006–13 | 2014–17 | 2019–23 | ||
| Age | 8–17 | 18+ | 8–17 | 18+ | |
| Total n (visit) | 9500 | 152 500 | 6500 | 112 000 | Ongoing |
| Anthropometrya | 9500 | 152 500 | 6500 | 112 000 | Ongoing |
| Blood pressure | 9500 | 152 500 | 6500 | 112 000 | Ongoing |
| Lung function | 9500 | 113 000 | – | 32 000 | Ongoing |
| ECG | 1500 | 152 500 | – | 112 000 | Ongoing |
| RFFT | – | 87 500 | – | – | Ongoing |
| MINI (depression/anxiety) | – | 149 000 | – | 91 500 | Ongoing |
| MMSE | – | 13 000b | – | – | Ongoing |
| AGE reader | – | 83 000 | – | – | – |
| Cogstate | – | – | 2000c | 66 500 | Ongoing |
| Jump height | – | 5500 | 26 500 | – | |
Numbers are rounded down to the nearest 500.
AGE, advanced glycation end products; ECG, electrocardiogram; MINI, mini international neuropsychiatric interview (anxiety and depression); MMSE, mini mental state examination; RFFT, Ruff figural fluency test.
Height, weight, waist and hip circumference.
Age 65+.
Age 13–17 years.
Table 2.
Overview of the content of the questionnaires for adults
| Topic | Original dimensions | New dimensions |
|---|---|---|
| General information | ||
| Demographics | Marital status, household composition, nationality | Ethnicity, twins, parental divorce, language |
| Family composition | Date of birth, date of death father and mother, children | |
| Work | Employment, function, income, absences | Postal code, work history, work functioning, work environment, informal care, voluntary work, shift work |
| Education | Highest level of education | |
| Health | ||
| Health status | History and prevalence of diseases, disabilities and symptoms | Allergies, hearing, joint problems, bodily pain, fatigue, gastrointestinal conditions, skin conditions, oral health, ocular health, family health, acne, attention-deficit hyperactivity disorder, COVID-19, autistic traits, depression, psychosis |
| Medication use | Current prescription, doses | |
| Health care use | Contact with health care professionals, receiving informal care | Functionality quantified self-devices |
| Questions for females | Number of pregnancies, age at menopause and age at menarche | |
| Birth and development | Birthweight, birth defects, breastfeeding | Early life factors |
| Body weight | Highest and lowest body weight in past 5 years, unwanted weight loss | |
| Lifestyle and environment | ||
| Physical activity | Physical activity | |
| Nutrition | Nutrition intake, alcohol use | Alcohol dependence |
| Smoking | Current and past active and passive smoking behaviour | Nicotine dependence |
| Daytime | Sleeping, activities, volunteer work | |
| Physical environment | Type of floor covering at home, domestic animals | Perceived environment, local earthquakes |
| Sedentary behaviour | Sedentary behaviour | |
| Participation in prevention programmes | Participation in vaccinations, (combined) personal lifestyle programmes, national health screenings | |
| Screen time/internet use | Internet use, blue light | |
| Psychosocial parameters | ||
| Quality of life, well-being | Quality of life, emotional affect | Life satisfaction |
| Personality | Neuroticism, extroversion, openness, personality, anxiety | |
| Stress | Threatening experiences, long-term difficulties | Childhood trauma |
| Social support, independence | Social well-being, frailty, health care needs | Self-management ability, negative social interactions, independence, social patterns |
| Health anxiety | Health anxiety | |
Beside the regular study waves, Lifelines allows researchers to collect additional in-depth data in (a subcohort of) the Lifelines population. A complete overview of these embedded data collection projects can be found on the Lifelines wiki page [https://wiki-lifelines.web.rug.nl/doku.php?id=additional_assessments]. Five examples are highlighted as follows.
Lifelines NEXT, a birth cohort; 1500 pregnant women; 2016—still running; the origin of chronic diseases at a very early stage of life can be studied. Samples and information (from mother, father and baby) are collected.3
VESPER: diversity in sperm quality; 2019–21; 200 men; analyses on sperm and data from questionnaires are collected; generates control values in fertility research, for example on cancer-related infertility.
Three subcohorts focused on gastrointestinal health (‘DArm Gezondheid’): Lifelines DEEP (DAG1), DAG2 and DAG3; 1500, 100 and 9500 participants, respectively; 2012–16; gaining insight into the relationship between microbiome, genetic and metabolic variation and phenotype variation. Samples and information from questionnaires were collected. Genome-wide transcriptomics and methylation data were generated, metabolites and biomarkers have been measured and the gut microbiome has been assessed.4
ImaLife; 12 000 participants; 2017—still running; low-dose CT; very early indicators of chronic obstructive lung diseases, coronary artery diseases and lung cancer can be studied.5
COVID-19 project; 77 000 participants with at least one questionnaire; 2020–21; a series of at least 25 questionnaires; risk factors of COVID-19 and psychological and societal impacts can be studied.6
Record linkage
Air quality,7 noise registries7 and distance to local sports facilities and retail facilities (LISA) are examples of available environmental data linked to participants’ residential geocodes. Lifelines is also a member of the Geoscience and health cohort consortium (GECCO).8 Other registries that were linked at an individual level, are: CBS (Statistics Netherlands) with cause of death and sociodemographic factors; IADB (Dutch prescription medication database); PALGA (Dutch pathology/anatomy archive); PERINED (Dutch perinatal registry); and NCR (Netherlands Cancer Registry). Linkage with general practitioners and COVID-19 PCR testing are in preparation.
Who is in the cohort?
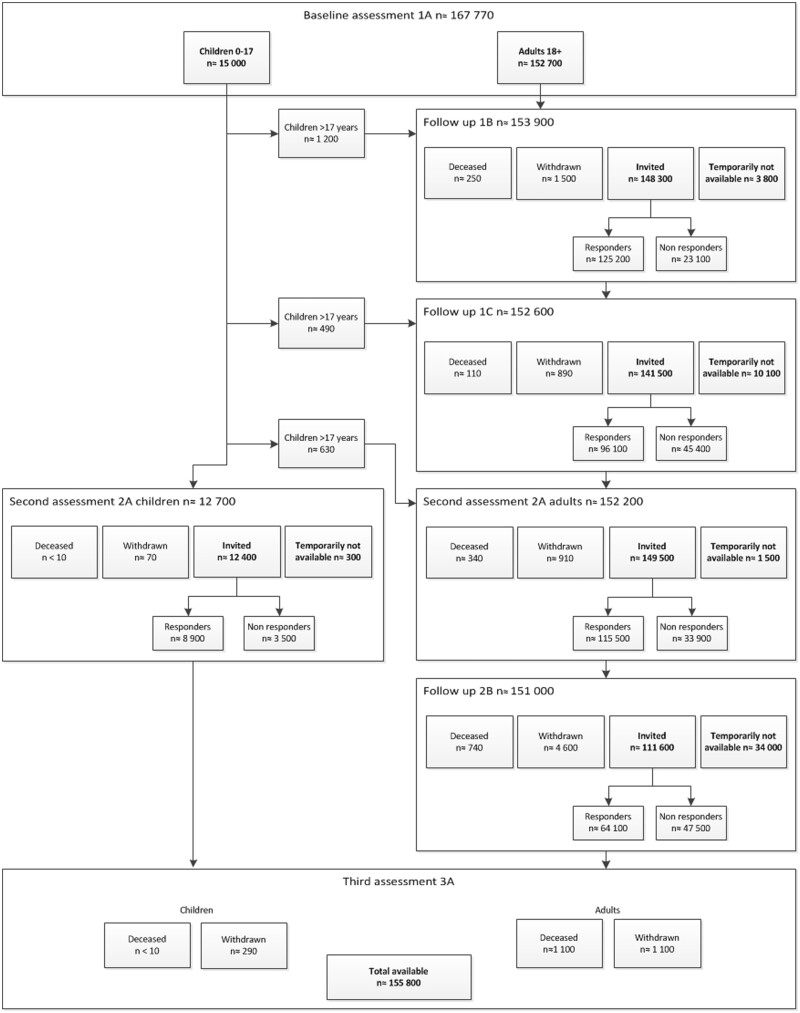
At baseline 167 729 participants were enrolled into the cohort, aged 0 to 93 years, with a mean age of 41 years. During follow-up, mean age of the population increased to 49 years at the start of the third research round. Lifelines has a stable group of active participants: approximately 71% took part in both the baseline and the second assessment (Figure 2). Over a decade later, 120 000 participants are expected to participate in the third wave for study centre visits and completing questionnaires.
Figure 2.
Flowchart of number of participants until the start of the third assessment
In between waves (1A and 2A in Figure 2), participants received follow-up questionnaires. The response rates were 84%, 68% and 58% for the follow-up questionnaires 1B, 1C and 2B, respectively (Figure 2).
Finally, participants were invited to participate in additional studies initiated by external researchers. Response rates on additional studies varied between 10% and 50%, depending on the topic.
Table 3 shows the baseline characteristics of participants. In total, 8900 participants (5.9%) withdrew from participating and 2500 (1.7%) died. On average, this group of withdrawn participants were older, more often female and overweight, had more often a low educational level, no paid job and a medium-to-bad perceived health and were more likely to smoke.
Table 3.
Baseline characteristics of adult participants according to different participation categories
| All included at baseline | Activea | Withdrawna | Deceaseda | |
|---|---|---|---|---|
| n b | 152 700 | 141 200 | 8900 | 2500 |
| Age (mean ± SD) | 44.6 ± 13.1 | 44.1 ± 12.8 | 47.9 ± 14.0 | 61.6 ± 13.8 |
| % Male | 41.5 | 41.4 | 39.2 | 55.9 |
| % Low educational level | 16.6 | 15.7 | 27.2 | 32.0 |
| % No paid jobc | 10.7 | 10.2 | 16.6 | 17.6 |
| % Medium/bad perceived health | 9.7 | 9.3 | 14.0 | 18.1 |
| % Smoking | 21.4 | 21.3 | 23.4 | 25.1 |
| % Overweight (BMI >=25) | 55.3 | 54.6 | 61.0 | 68.6 |
SD, standard deviation; BMI, body mass index.
Participation status at the end of 2020.
Rounded to the nearest hundred.
Excluding students and retirement.
Reasons for withdrawal were diverse: participating is too time consuming, lost interest, lost trust in big data/negative media attention, moved outside the region or entered regular health care programme based on health-related complaints. Because Lifelines aims to retain as many participants as possible, the following options for withdrawal are presented to the participants (percentages of total Lifelines population): (i) no invitations for study centre visits, only for questionnaires (1.8%); (ii) no invitations for questionnaires, only for visits (0.8%); (iii) withdrawal, with permission to continue using previously collected data and biomaterial (5.7%); (iv) complete withdrawal, all collected materials will be destroyed (0.1%).
What has been measured?
Data and samples
Data and samples from the general assessments
Measurements taken during the general study visits are shown in Table 1. In addition to the measurements, participants collected urine, fasting blood samples were taken and questionnaires were filled out. Immediately after blood draw, one of the blood and one of the urine samples were sent to the laboratory for analysis of a selected list of parameters. Parameters measured from EDTA Sysmex and NaF (sodium fluoride) tubes where comparable between all three assessments.1 From heparin gel tubes: sodium, potassium, urea (only third assessment), creatinine, eGFR (estimated glomerular filtration rate), triglyceride, cholesterol, HDL(high-density lipoprotein)-cholesterol, LDL(low-density lipoprotein)-cholesterol were repeated and chloride was additionally measured compared with baseline assessment. From urine only creatinine from 24-h urine was repeated compared with baseline assessment.
Plasma, serum, buffy coat and lymphocytes were stored. From adults, 24-h urine and morning urine were stored; from children (8–17 years), timed overnight urine was stored. During the second assessment, in addition to blood and urine, also scalp hair and fecal samples were collected in a subcohort of the participants. Stored samples are available for researchers worldwide.
Data and samples from subcohorts
Next to the general Lifelines measurements, in subcohorts of Lifelines additional data and samples were collected or analysed. Samples of cord blood, placental tissue and breast milk were collected and stored (NEXT).3 And samples from nose (nasal brush), breath4 and semen (VESPER) were analysed. Furthermore plasma testosterone (VESPER), vascular function (ImaLife5), folic acid and the vitamins B6, B12, D, A, E and K (MINUTHE9) were or are going to be determined. Eye measurements including refraction, intraocular pressure, visual field, structural layers of the eye, fundus photograph and eye dryness are being collected (EyeLife). MRI (magnetic resonance imaging) of the heart and of the brain and a CT of the lungs were or will be available (ImaLife). Finally measurement of social interaction by smartphone is planned.
Questionnaire data
The questionnaires completed during the regular study waves generated around 8000 variables and cover a broad range of topics (Table 2). For detailed information about the available data, please visit our Lifelines Wiki [http://wiki-lifelines.web.rug.nl] or catalogue [https://data-catalogue.lifelines.nl].
Genomic data
Genomic data have been collected in subcohorts of the Lifelines cohort population. Whole genome sequencing is available for 165 participants. The Infinium Global Screening Array® (GSA) MultiEthnic Disease Version was used for SNP (single nucleotide polymorphism) genotyping of 38 000 participants. In combination with 15 400 samples already genotyped on the Cytochip GWAS (genome-wide association study), Illumnia CytoSNP-12v2), a single quality controlled GWAS dataset of n ≈ 50 000 subjects is available. In the near future the availability of GWAS data of all participants is planned.
What has it found? Key findings and publications
Lifelines data are used in diverse research disciplines, from social sciences to biomedical sciences, and have led to a considerable scientific contribution. To date, a total of about 600 proposals have been approved: over 500 papers are published; and more than 125 researchers currently work with Lifelines data from all over the world. A complete overview of the publications can be found at the Lifelines website [www.lifelines.nl/researcher/publications].
Some highlights
Almost 25% of the participants who had electrocardiographic evidence of a myocardial infarction (MI) where unaware of it (silent MI).10 These participants do not have the increased risk of anxiety disorders that was found in participants with a recognized MI.11
Food patterns were strongly regionally defined.12
A diet with relative high percentage of proteins, and high part plant-based proteins compared with animal-based protein, was associated with a lower HbA1 score and a better kidney function.13
A combination of 16 volatile organic compounds from breath samples can accurately distinguish irritable bowel syndrome patients from healthy controls.14
The gut microbiome is related to the risk of cardiovascular diseases, independent of dietary patterns or inflammatory markers.15
Occupational exposure to pesticides is genome-wide associated with differential DNA methylation.16
Use of corticosteroids was associated with metabolic syndrome,17 reduced executive cognitive functioning and a higher likelihood of mood and anxiety disorders.18
Family structures have no influence on the effects of body mass index on physical and mental quality of life.19
It has been claimed that functional somatic syndromes, like irritable bowel syndrome, chronic fatigue syndrome and fibromyalgia, share a common aetiology, but predictors of these new-onset syndromes were more often syndrome-specific.20
Low social economic status is a risk factor for vitamin deficiencies (B6, B12 and folic acid), partly explained by diet quality (Lifelines-MINUTHE study9).
What are the main strengths and weaknesses?
Strengths
The main strengths of the Lifelines cohort and biobank are its longitudinal study design, with repeated measures on a wide range of multidisciplinary topics along with the collection of a large variety of biological samples. Furthermore, the three-generation design (increasing to the fourth generation in the additional birth cohort Lifelines NEXT) is a unique feature providing excellent opportunities for genetic research and the influence of family culture and social environment on health. Another strength of the Lifelines cohort is that it is being conducted in a large and stable cohort in the sense that relatively few people move out of the area. Moreover, the response rate of participants to re-invitation and questionnaires is promising for future research rounds. Finally, several opportunities exist to obtain more detailed research data, by the collection of additional data in (sub)cohorts or by data linkage.
Weaknesses
Next to the strengths, also some weaknesses are present in Lifelines. Almost 30% of the population did not participate in the second research round and attrition was selective. For the third assessment, a clear goal is set to welcome at least 120 000 participants to the study centre. The study visits and completed questionnaires will be closely monitored to retain as many participants as possible in the cohort. In case of an unexpected drop in number, timely appropriate action will be taken, dependent on the reasons for this drop. Second, inherent in the population composition of the three northern provinces in The Netherlands, relatively few ethnic minorities participate in Lifelines.
Can I get hold of the data? Where can I find out more?
Lifelines provides researchers worldwide with easy and fast access to FAIR (findable, accessible, interoperable and reusable) data and samples for research on healthy ageing. A submitted application [www.lifelines.nl/researcher] will be reviewed within 2 weeks. After signing the offer and the DMTA (Data and/or Material Transfer Agreement), in general, data will be available within 2 weeks and samples within 6–12 weeks. For detailed information about the available data please take a visit to our Lifelines Wiki [https://wiki-lifelines.web.rug.nl] or catalogue [https://data-catalogue.lifelines.nl/]. Because Lifelines is a not-for-profit cohort and biobank, we charge only the cost price of release and linking materials for researchers of scientific and educational institutes. Lifelines can always be contacted for any information requests [research@lifelines.nl].
Ethics approval
The Lifelines study was approved by the ethics committee of the University Medical Center Groningen, document number METC UMCG METc 2007/152. Informed consent was obtained from all individuals included in the study.
Funding
The Lifelines initiative has been made possible by subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen, Groningen University and the provinces in the north of the Netherlands (Drenthe, Friesland, Groningen)
Author Contributions
A.S., J.R. and A.D. drafted the paper and were involved in reviewing the paper in detail. A.S. finalized writing the paper. P.H., G.N. and J.G.M.R. were involved as members of the Scientific Advisory Committee of Lifelines, and were involved in reviewing this paper in detail.
Conflict of interest
None declared.
Contributor Information
Anna Sijtsma, Lifelines Cohort Study, Roden, The Netherlands.
Johanna Rienks, Lifelines Cohort Study, Roden, The Netherlands.
Pim van der Harst, Department of Cardiology, University Medical Centre Utrecht, Utrecht, The Netherlands; Department of Cardiology, University Medical Center Groningen, Groningen, The Netherlands.
Gerjan Navis, Department of Nephrology, University Medical Center Groningen, Groningen, The Netherlands.
Judith G M Rosmalen, Departments of Psychiatry and Internal Medicine, University Medical Center Groningen, Groningen, The Netherlands.
Aafje Dotinga, Lifelines Cohort Study, Roden, The Netherlands.
References
- 1. Scholtens S, Smidt N, Swertz MA et al. Cohort Profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol 2015;44:1172–80. [DOI] [PubMed] [Google Scholar]
- 2. Fredrickson J, Maruff P, Woodward M et al. Evaluation of the usability of a brief computerized cognitive screening test in older people for epidemiological studies. Neuroepidemiology 2010;34:65–75. [DOI] [PubMed] [Google Scholar]
- 3. Warmink-Perdijk WDB, Peters LL, Tigchelaar EF et al. Lifelines NEXT: a prospective birth cohort adding the next generation to the three-generation Lifelines cohort study. Eur J Epidemiol 2020;35:157–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tigchelaar EF, Zhernakova A, Dekens JA et al. Cohort Profile: LifeLines DEEP, a prospective, general population cohort study in the northern Netherlands: study design and baseline characteristics. BMJ Open 2015;5:e006772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xia C, Rook M, Pelgrim GJ et al. Early imaging biomarkers of lung cancer, COPD and coronary artery disease in the general population: rationale and design of the ImaLife (Imaging in Lifelines) study. Eur J Epidemiol 2020;35:75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mc Intyre K, Lanting P, Deelen P et al. Lifelines COVID-19 cohort: investigating COVID-19 infection and its health and societal impacts in a Dutch population-based cohort. BMJ Open 2021;11:e044474044474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zijlema WL, Smidt N, Klijs B et al. The LifeLines Cohort Study: a resource providing new opportunities for environmental epidemiology. Arch Public Health 2016;74:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Timmermans EJ, Lakerveld J, Beulens JWJ et al. Cohort Profile: The Geoscience and Health Cohort Consortium (GECCO) in the Netherlands. BMJ Open 2018;8:e021597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhu Y, Minovic I, Dekker LH et al. Vitamin status and diet in elderly with low and high socioeconomic status: The Lifelines-MINUTHE study. Nutrients 2020;12:2659. 10.3390/nu12092659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van der Ende MY, Hartman MHT, Schurer RAJ et al. Prevalence of electrocardiographic unrecognized myocardial infarction and its association with mortality. Int J Cardiol 2017;243:34–39. [DOI] [PubMed] [Google Scholar]
- 11. Iozzia G, de Miranda Azevedo R, van der Harst P, Rosmalen JGM, de Jonge P, Roest AM. Association of recognized and unrecognized myocardial infarction with depressive and anxiety disorders in 125,988 individuals: a report of the Lifelines cohort study. Psychosom Med 2020;82:736–43. [DOI] [PubMed] [Google Scholar]
- 12. Dekker LH, Rijnks RH, Strijker D, Navis GJ. A spatial analysis of dietary patterns in a large representative population in the north of The Netherlands – the Lifelines cohort study. Int J Behav Nutr Phys Act 2017;14:166–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moller G, Sluik D, Ritz C et al. A protein diet score, including plant and animal protein, investigating the association with HbA1c and eGFR – The PREVIEW Project. Nutrients 2017;9:763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baranska A, Mujagic Z, Smolinska A et al. Volatile organic compounds in breath as markers for irritable bowel syndrome: a metabolomic approach. Aliment Pharmacol Ther 2016;44:45–56. [DOI] [PubMed] [Google Scholar]
- 15. Kurilshikov A, van den Munckhof ICL, Chen L et al. ; LifeLines DEEP Cohort Study, BBMRI Metabolomics Consortium. Gut microbial associations to plasma metabolites linked to cardiovascular phenotypes and risk. Circ Res 2019;124:1808–20. [DOI] [PubMed] [Google Scholar]
- 16. van der Plaat DA, de Jong K, de Vries M et al. ; Biobank-based Integrative Omics Study Consortium. Occupational exposure to pesticides is associated with differential DNA methylation. Occup Environ Med 2018;75:427–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Savas M, Muka T, Wester VL et al. Associations between systemic and local corticosteroid use with metabolic syndrome and body mass index. J Clin Endocrinol Metab 2017;102:3765–74. [DOI] [PubMed] [Google Scholar]
- 18. Savas M, Vinkers CH, Rosmalen JGM et al. Systemic and local corticosteroid use is associated with reduced executive cognition, and mood and anxiety disorders. Neuroendocrinology 2020;110:282–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Demetrashvili N, Smidt N, Snieder H, van den Heuvel ER, Wit EC. Variance components models for analysis of big family data of health outcomes in the Lifelines cohort study. Twin Res Hum Genet 2019;22:4–13. [DOI] [PubMed] [Google Scholar]
- 20. Monden R, Rosmalen JGM, Wardenaar KJ, Creed F. Predictors of new onsets of irritable bowel syndrome, chronic fatigue syndrome and fibromyalgia: the Lifelines study. Psychol Med 2020. doi: 10.1017/S0033291720001774. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]