Among the imaging-based biomarkers that have been evaluated for detecting and staging liver fibrosis, liver tissue stiffness has emerged as the most reliable. MRI- and ultrasound-based quantitative elastography techniques have become widely available, and MR elastography (MRE) has emerged as the technique with highest performance.
Regulatory-approved MRE packages are available from the manufacturers of more than 90% of MRI systems worldwide, and all use the same standardized acquisition methods, shear-wave driver devices, and processing algorithms that provide a model-free measurement of the magnitude of the complex shear modulus, resulting in a high degree of cross-platform reproducibility [1]. In contrast, ultrasound elastography systems (i.e., vibration-controlled transient elastography [VCTE], point shear-wave elastography [pSWE], and 2D shear-wave elastography [2D SWE]) vary in technical implementation, shear-wave generation method, shear-wave spectra, and processing. Stiffness is reported in Young’s modulus, shear modulus, or shear-wave speed, depending on the manufacturer. Ultrasound-based measurements obtained by different systems generally cannot be compared reliably, and measurements of a uniform material can vary substantially with depth due to the effects of dispersion.
Precision is an important factor in longitudinal diagnostic testing. Multiple studies have shown that the repeatability of MRE (coefficient of variation [COV], ≈ 11%) is superior to that of VCTE (COV, ≈ 40%), the most commonly used ultrasound elastography technique [2].
The introduction of spin-echo echo-planar imaging (SE-EPI) MRE sequences more than 5 years ago for 3-T MRI systems established the technical success rate for MRE to be approximately 98% [3]. References suggesting that MRE frequently fails due to iron overload are no longer correct. Technical success of MRE is not affected by high body mass index (BMI) or ascites. Technical failures in VCTE are reported to be in the range of 10–15% and are often related to high BMI, ascites, and acoustic window limitations.
Accumulated evidence indicates that MRE has the highest diagnostic performance among all noninvasive techniques for detecting and staging liver fibrosis. A recent large meta-analysis compared MRE with VCTE, pSWE, and 2D SWE techniques [4]. MRE had high diagnostic performance (AUC = 0.91 for diagnosing clinically significant fibrosis; AUC = 0.92 for diagnosing advanced fibrosis). The diagnostic performance of the ultrasound-based techniques was lower, with AUCs ranging from 0.75 to 0.86 for clinically significant fibrosis and from 0.72 to 0.89 for advanced fibrosis. The AUC for detecting cirrhosis was approximately 0.90 for all techniques; however, several studies have shown that the PPV of MRE for detecting cirrhosis is usually higher than that for ultrasound-based elastography [5].
The diagnostic performance of MRE benefits from the large volume of liver evaluated (Fig. 1). VCTE and pSWE assess approximately 0.1% of total liver volume, and 2D SWE assesses approximately 2%. In comparison, MRE typically assesses a region representing approximately 20% of the total liver volume.
Fig. 1—
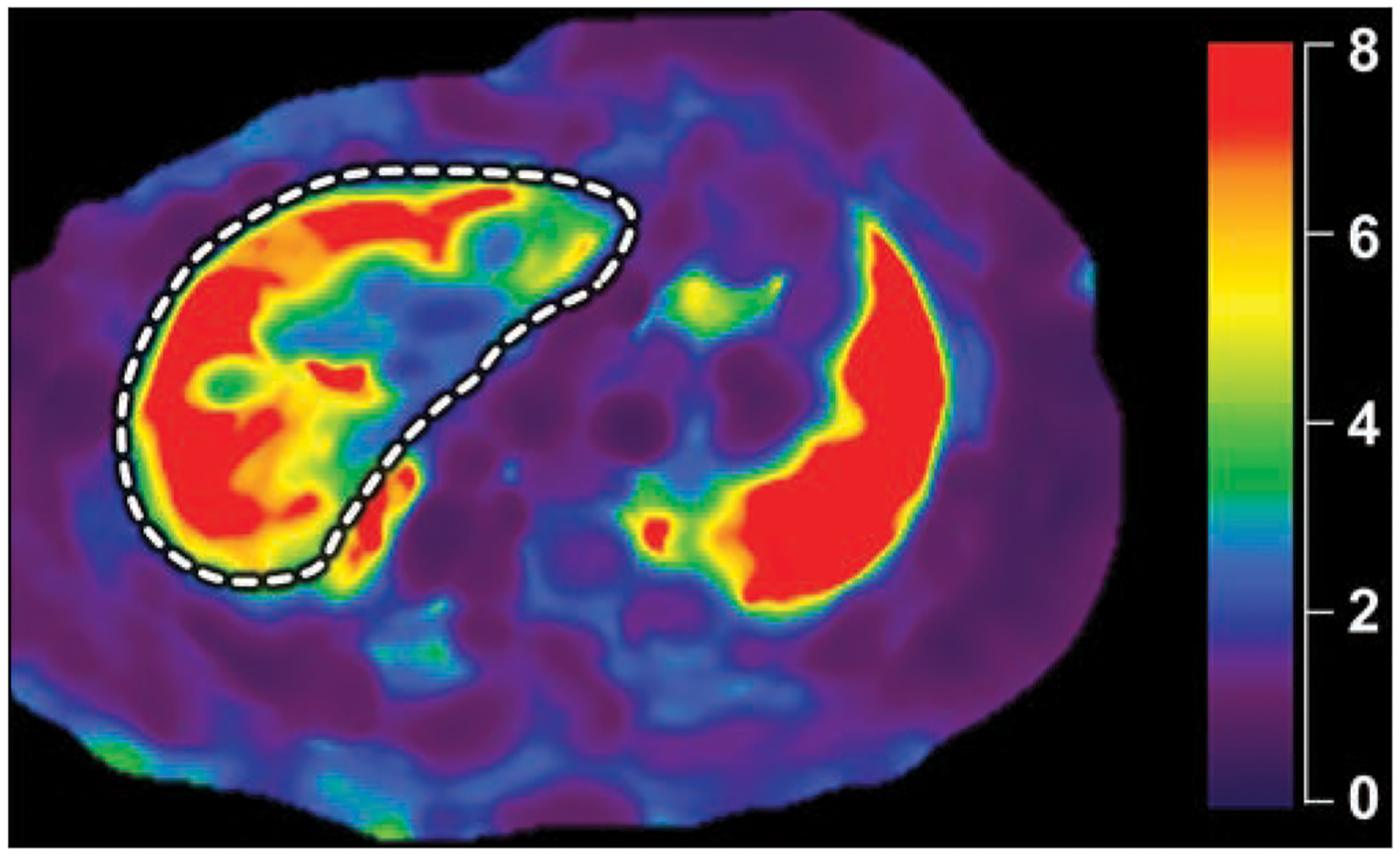
22-year-old woman with suspected primary sclerosing cholangitis. MR elastography shows heterogeneously increased liver stiffness with peripheral distribution. Mean stiffness of liver (dashed line) tissue is 5.3 kPa. Biopsy showed stage IV fibrosis. Scale shows liver stiffness values in kilopascals.
Elastography is a rapid examination. A standard four-section MRE acquisition can be obtained in a single breath-hold and can easily be combined with a single breath-hold acquisition that quantifies steatosis and iron to provide a comprehensive assessment of diffuse liver disease in as few as two breath-holds. Ultrasound elastography typically requires 10 measurements, each obtained during suspended respiration. Most reviews have concluded that MRE is considerably less operator-dependent than ultrasound-based elastography.
MRE-based measurements of liver stiffness are not confounded by the presence of elevated liver fat. Ultrasound-based elastography measurements have been reported to be systematically biased by the effects of steatosis, probably resulting from dispersion effects and the wider bandwidth of shear waves used with these techniques.
Cost and availability are often raised as differentiating factors in the context of elastography. The cost of adding MRE capability to an existing MRI system is comparable to or lower than the cost of a VCTE unit. The U.S. Medicare reimbursement for an MRE examination (Current Procedural Terminology [CPT] code 76391) is approximately $220. The reimbursement for SWE (CPT code 76981) is approximately $122. Cost-efficacy studies are highly dependent on cost assumptions. In one analysis, VCTE was found to be only slightly more cost-effective than MRE ($690 vs $781, respectively, in terms of cost per relevant diagnosis), albeit with lower accuracy [6]. Yet this analysis was constructed using the full abdominal MRI cost rather than the stand-alone MRE cost [6], which means that MRE would likely have been found to be more cost-effective than VCTE if the cost had been assigned appropriately.
MRE is now widely available, deployed on approximately 2000 MRI systems in radiology facilities worldwide. Reviews of the role of elastography in nonradiology journals often base availability in part on whether the test can be performed in a point-of-care clinic. Some publications have explicitly attributed the fact that MRE is performed by radiology facilities as a disadvantage, while still acknowledging that MRE has the best overall performance. Most ultrasound-based elastography capacity worldwide is in the form of VCTE units that are primarily deployed by self-referring clinicians in nonradiology facilities.
Multiple societies and payers have recognized the role of VCTE and MRE for assessing liver fibrosis. SWE techniques are still considered investigational and not medically necessary by most payers.
In summary, the published literature has established that the performance of MRE in staging liver fibrosis is superior to that of ultrasound-based elastography with respect to precision, accuracy, reproducibility, standardization, operator dependence, cross-vendor technical success rate, volume of liver evaluated, and influence of confounders. MRE is widely available and has the highest diagnostic performance among all noninvasive tests for detecting and staging liver fibrosis.
Given the nuanced nature of this discussion, we had some reluctance in accepting to write this Counterpoint. The availability of multiple modalities has always been a major asset for radiology. Regardless of the specific implementation, the innovative technologies discussed here provide patients with a safer, more comfortable, and much less expensive alternative to invasive liver biopsy for detecting and staging liver fibrosis. The clinical use of MRI-based and ultrasound-based elastography will evolve in the future, based on further advances in technology, changing practice patterns, levels of training, availability of new therapeutic options for chronic liver disease, and most important of all, the best interest of our patients.
Acknowledgments
Supported by grants from the NIH (R01 AA021171, R37 EB001981, R01 EB017197), U.S. Department of Defense (W81XWH-19-1-0583-01), and The Mayo Clinic.
Footnotes
M. Yin and The Mayo Clinic have intellectual property and a financial interest related to this research. The remaining author declares that there are no additional disclosures relevant to the subject matter of this article.
References
- 1.Yasar TK, Wagner M, Bane O, et al. Interplatform reproducibility of liver and spleen stiffness measured with MR elastography. J Magn Reson Imaging 2016; 43:1064–1072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harrison SA, Dennis A, Fiore MM, et al. Utility and variability of three non-invasive liver fibrosis imaging modalities to evaluate efficacy of GR-MD-02 in subjects with NASH and bridging fibrosis during a phase-2 randomized clinical trial. PLoS One 2018; 13:e0203054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim DW, Kim SY, Yoon HM, Kim KW, Byun JH. Comparison of technical failure of MR elastography for measuring liver stiffness between gradient-recalled echo and spin-echo echo-planar imaging: a systematic review and meta-analysis. J Magn Reson Imaging 2020; 51:1086–1102 [DOI] [PubMed] [Google Scholar]
- 4.Selvaraj EA, Mózes FE, Jayaswal ANA, et al. ; LITMUS Investigators. Diagnostic accuracy of elastography and magnetic resonance imaging in patients with NAFLD: a systematic review and meta-analysis. J Hepatol 2021; 75:770–785 [DOI] [PubMed] [Google Scholar]
- 5.Dong BT, Chen YP, Lyu GR, Wang HM, Lin GF, Gu JH. Diagnostic accuracy of two-dimensional shear wave elastography and magnetic resonance elastography for staging liver fibrosis in patients with chronic hepatitis B: a systematic review and meta-analysis. J Gastroenterol Hepatol 2021. May 12 [published online] [DOI] [PubMed] [Google Scholar]
- 6.Vilar-Gomez E, Lou Z, Kong N, Vuppalanchi R, Imperiale TF, Chalasani N. Cost effectiveness of different strategies for detecting cirrhosis in patients with nonalcoholic fatty liver disease based on United States health care system. Clin Gastroenterol Hepatol 2020; 18:2305–2314.e12 [DOI] [PubMed] [Google Scholar]


