Abstract
Background
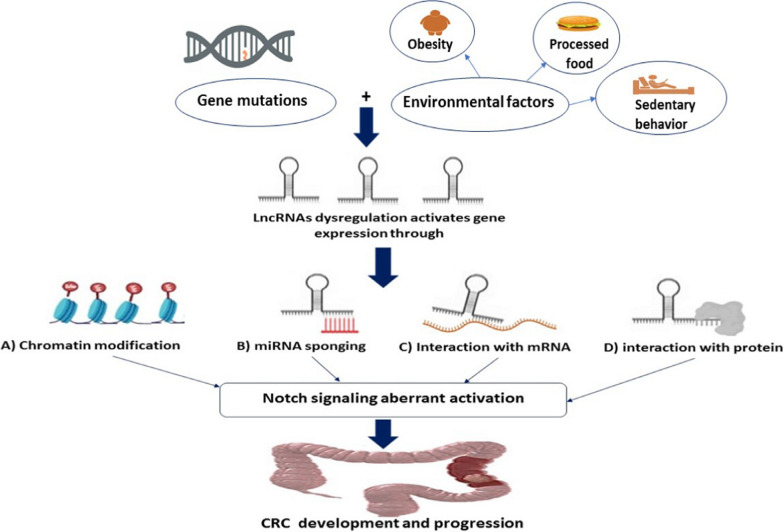
Colorectal cancer (CRC) is one of the most prevalent digestive cancers, ranking the 2nd cause of cancer-related fatality worldwide. The worldwide burden of CRC is predicted to rise by 60% by 2030. Environmental factors drive, first, inflammation and hence, cancer incidence increase.
Main
The Notch-signaling system is an evolutionarily conserved cascade, has role in the biological normal developmental processes as well as malignancies. Long non-coding RNAs (LncRNAs) have become major contributors in the advancement of cancer by serving as signal pathways regulators. They can control gene expression through post-translational changes, interactions with micro-RNAs or down-stream effector proteins. Recent emerging evidence has emphasized the role of lncRNAs in controlling Notch-signaling activity, regulating development of several cancers including CRC.
Conclusion
Notch-associated lncRNAs might be useful prognostic biomarkers or promising potential therapeutic targets for CRC treatment.
Therefore, here-in we will focus on the role of “Notch-associated lncRNAs in CRC” highlighting “the impact of Notch-associated lncRNAs as player for cancer induction and/or progression.”
Graphical Abstract
Keywords: Epigenetics, lncRNAs, Notch, Colorectal cancer, Inflammation, Micro-RNAs, Hallmarks of cancer
Introduction
Background
CRC is the third most ubiquitous malignancy as well as the second major cause of cancer-correlated death worldwide [1]. Surprisingly, CRC is now becoming more common among adolescents and young adults under the age of 45, who frequently come with advanced disease [2]. the prevalence of CRC is globally estimated to grow, environmental factors, such as increased sedentary behavior and obesity or processed food are thought to be one of the driving risk factors to this increase [3]. Even after surgical resection, chemotherapy/radiotherapy, using immunotherapy or the state-of-the-art targeted therapy, but, unfortunately, the 5-year survival rate remains low [2]. Cancer recurrence and distant metastases are the cause for these poor outcomes, especially for more advanced stage CRC [4].
CRC develops, throughout time, like other cancer types, as a result of a cascade of epigenetic alterations, mostly, affecting the genetic component, driving the normal colonic mucosa conversion into malignant tumor [5]. This interconversion is generated from alterations occurring within polyps, mostly adenomas [6]. Recent evidence shows that aberrant Notch cascade is crucial for CRC evolution.
Notch gene was discovered in 1917 by Morgan et al. in mutant Drosophila. The gene is known as 'Notch' because it causes a “breach” in the wings of Drosophila [7]. Notch cascade is conserved, among species, to control variety of biological activities as cell proliferation, differentiation as well as regulating cell fate decisions [8, 9].
Deregulation of Notch pathway is related to the development of hematological and solid malignancies, via pro-tumorigenic effect [10–13]. In the intestine, Notch pathway controls the homeostatic self-renewal processes and can cause ulcerative colitis, if the Notch pathway was dysregulated [14], which would cause the tumorigenic transformation of epithelia [15].
Notch pathway is a key player in CRC from initiation to resistance and metastasis, driving CRC progression and/or poor overall survival (OS) [16–19]. Positive association has been shown between the Notch receptor, Notch1, expression and deeper invasion of tumor-lymph node-metastasis (TNM) in CRC [20]. Patients with Notch1-positive malignancies had a worse OS rate than those with Notch1-negative ones [20]. Moreover, Notch-signaling is an ultimate regulator of epithelial-mesenchymal transition (EMT) process [21]. Notch-induced-EMT is a fundamental factor in CRC stemness and aggressiveness [22]. Also, increased expression of Notch as well as its target genes was shown to contribute to CRC chemoresistance [23–26].
Epigenetics-influenced activation of the Notch pathway would be led by non-protein coding RNAs (ncRNAs) expression dysregulation [27, 28]. LncRNAs are non-protein producing transcripts, performing a crucial role in the epigenetic regulation(s) affecting gene expression [29]. LncRNAs can control Notch-activation through regulation of Notch receptors or Notch ligands expression, either on transcriptional or post-transcriptional levels [30]. On the other hand, some lncRNAs are Notch-signaling downstream targets [31]. Several studies have showed that dysregulated lncRNAs have implications in CRC development, progression, metastasis as well as developing chemoresistance affecting the disease clinical outcomes [32–34].
Therefore, the interest in this review is to focus on the “Impact of the Notch-associated lncRNAs in CRC”. The review first aims to briefly discuss lncRNAs', Notch-signaling pathway and Notch-associated-lncRNAs mechanism(s) profiling in cancer. LncRNAs interacting with the Notch-cascade contributing to the development of various tumors are presented in the review. Second, we will highlight the role of Notch-associated lncRNAs as a player in cancer induction and progression, after defining specifically CRC types. Moreover, describing “Notch-associated lncRNAs impact on CRC clinical outcomes” and the “Notch-associated lncRNAs relationship to multidrug resistance (MDR), metastasis or recurrence.”
Non-protein coding RNA
Non-protein coding (non-coding) regions of the genome, generates numerous families of ncRNAs [35, 36], that controls gene expression and function. ncRNAs are classified based on their length, location and function into micro-RNAs (miRNAs), lncRNAs, small nucleolar RNAs (snoRNAs), small nuclear RNAs (snRNAs), small interfering RNAs (siRNAs) and PIWI-interacting RNAs (piRNAs) [37–39].
Long non-coding RNA
LncRNA are molecules with a length of more than 200 nucleotides [40]. LncRBase; The lncRNA sequence database; LncRBase is freely available at http://www.lncRbase.org
LncRNAs were originally described in mice through large-scale sequencing of entire cDNA libraries [41].
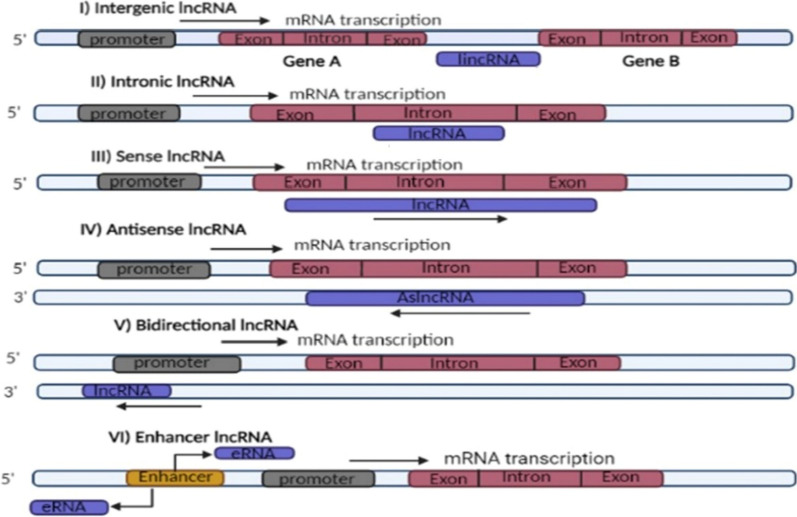
LncRNAs are named after their biogenesis locations in relation to the coding genes [42], which is illustrated in Fig. 1. LncRNAs can be intergenic (lincRNAs) which are derived from gaps between genes, usually placed between protein-coding genes, intronic-lncRNAs which originate from a protein-coding genes' intronic regions, sense-lncRNAs which are produced from same strand and direction of neighboring protein-coding genes. On the other hand, the antisense-lncRNAs (aslncRNA) called natural antisense transcripts (NATs) are generated from transcription of complementary strands of protein-coding genes. Likewise, the bidirectional-lncRNAs which are derived from sequences that are close to protein-coding genes' transcription start sites, but from reverse strand also. Enhancer RNAs (eRNAs) which are generated from protein-coding genes' upstream enhancer and promoter regions [38, 43, 44].
Fig. 1.
LncRNAs' classification based on their biogenesis site in relation to the coding genes. Depending on the biogenesis location, lncRNAs are classified into, intergenic which is transcribed from gaps between genes. Intronic which is transcribed from intronic regions of protein coding genes, sense which is transcribed in same direction and on same strand of neighboring coding genes; Both exonic and intronic sense lncRNAs are possible. Antisense which can be multiple exonic and intronic also but is transcribed from the reverse strand of neighboring coding gene. Bidirectional which is transcribed from region near to promoter of neighboring coding gene but from opposite strand. Enhancer which is transcribed from coding gene's enhancer region
LncRNA structure
The biogenesis of lncRNAs is mediated by RNA polymerase II, similar to that of messenger RNA (mRNA) [45]. As a result, many lncRNAs have caps on the 5′ end and poly(A) tails on the 3′ end [46]. The majority of lncRNAs are thought to have more than two exons, as well as secondary and tertiary structures [47]. For each transcriptional start of a given lncRNA, nearly two distinct 3′ ends can be detected. Alternate cleavage and polyadenylation are the two processes that contribute to alternative 3′ ends, resulting in generation of different isoforms of lncRNAs from the same site, which can be increased even more by alternative splicing events [48, 49]. On the other hand, there is an exception in some lncRNAs which can be un-polyadenylated [38].
LncRNA-encoding genes generally have their own promoters, transcription factors (TFs) and distinctive DNA motifs, suggesting that transcription of lncRNAs may be an independent epigenetic modification [47]. Moreover, other epigenetic factors as DNA methylation can regulate lncRNAs transcription [47]. LncRNAs can be found in the nucleus, cytoplasm, as well as body vesicles such as exosomes and mitochondria [50]. More than half of the expressed lncRNAs are cytoplasmic, where they relate to polysome fractions, regulating mRNAs stability and translation [51].
LncRNAs as epigenetic regulators
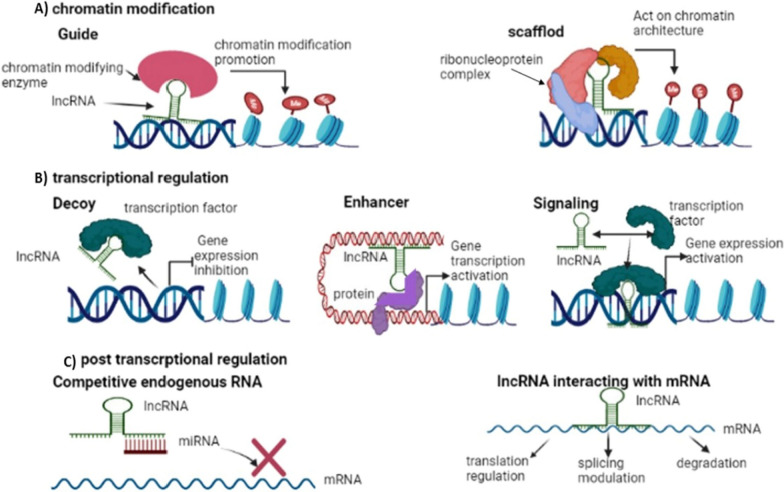
LncRNAs have the capacity to regulate several biological processes in both the normal and the disease states [52, 53]. LncRNAs play a key role in regulation of gene expression (54), which is clarified in Fig. 2.
Fig. 2.
LncRNAs as epigenetic regulators. In A lncRNA can control gene expression via modfying chromatin architecture; guide lncRNA interacts with chromatin modfying enzyme firstly, then guiding it to specfic gene locus. While scaffold serves as platfrom for developing of RNP complexes through interaction with ribonucleoproteins. In B lncRNA can control gene transcription, Decoy lncRNA inhibits transcription by trapping TFs; while enhancer or signal lncRNAs activate transcription by acting as TF or TF activator respectively. In C lncRNAs can post transcriptionally control gene expression by acting as ceRNA which sponges other regulatory ncRNAs, miRNAs, preventing their interaction with target mRNA or via lncRNA direct interaction with mRNA
LncRNAs can act as chromatin modifiers as guide lncRNA, interacting with chromatin-modifying-enzymes, mediating epigenetic modification by recruiting the developed chromatin remodeler complex to a specific gene locus [45]. On the other hand, scaffold lncRNA can assist in ribonucleoprotein (RNP) complexes assembly by interacting and placing proteins close to each other [29], Fig. 2A. And, depending on the proteins and RNAs present, transcriptional activation or repression is the result, once the complexes have been wholly developed [55].
LncRNAs can act as transcriptional regulators, including decoy lncRNA which repress transcription of its neighboring coding gene by trapping regulatory factors including TFs [56]. Enhancer lncRNA which can function as a transcription factor-like molecule or enhancer, to boost gene expression [57]. Moreover, signal lncRNAs act as a molecular signal to control transcription in response to diverse stimuli [55]. As a result, its presence and synthesis can be used as a measure of transcriptional activity [55], Fig. 2B.
LncRNAs can act as post-transcriptional regulators, including competitive endogenous RNA (ceRNA) acting as sponge for miRNAs and hence, silencing its target mRNA [58] or lncRNAs-mRNA direct interaction via recognizing complimentary sequences, with an overall regulation of capping, splicing and mRNA stability [54], Fig. 2C.
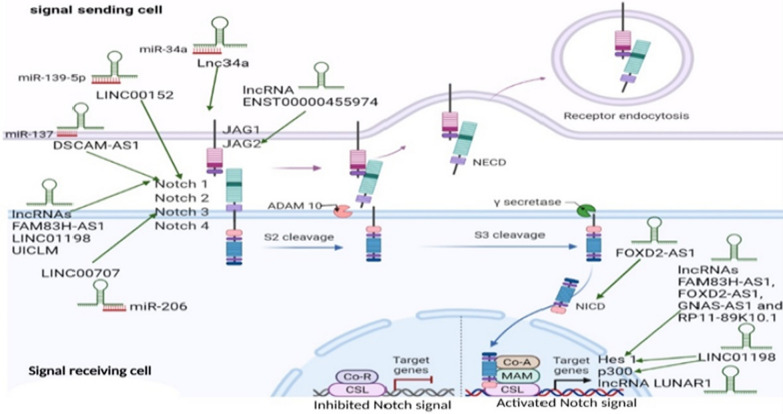
Notch-signaling mechanism (Fig. 3)
Fig. 3.
Notch-signaling and Notch-activation pathways in cancer, in relation to Notch associated-lncRNAs target genes. Notch receptors; Notch1, Notch2, Notch3, Notch4, Notch ligands; DLL; Delta-like ligand DLL1, DLL3, DLL4, and JAG, Jagged; JAG1, JAG2, ADAM; A Disintigrin and metalloproteases,, Co-R; co-repressors, co-A; co-activators, CSL transcription factor; (CBF1 Suppressor of Hairless, Lag-1), Hes1 hairy and enhancer of split-1, MAM mastermind proteins, NICD Notch intracellular domain, NECD Notch extracellular domain, Ƴ secretase gamma secretase. Notch signaling mechanism can be reinforced in cancer cells by lncRNAs, which can directly engage the Notch signal genes, boosting their expression, or disrupt miRNAs implicated in Notch signal suppression at specific stage
The binding of Notch ligand on one cell's membrane to a Notch receptor (Notch1, Notch2, Notch3) on the contacting cell's membrane initiates Notch signaling [59]. A two-step proteolysis cleavage process of Notch receptors starts once the ligand binds to them on the cell surface [60]. The ADAM enzymes (a disintegrin and metalloproteinase) catalyze the initial cleavage, resulting in the loss of the Notch's extracellular domain (NECD), which is then released by endocytosis [61]. While, the second cleavage is triggered by gamma-secretase, leading to release of the active Notch intracellular domain (NICD) [62, 63]. NICD enters the cell nucleus and interacts with the transcription factor CSL (CBF1, Suppressor of Hairless, Lag-1) and co-A activators mastermind (co-A MAM), all forming CSL-Notch-Mastermind transcription factor complex [62, 64], which is responsible for activating the Notch-target molecules transcription, like hairy and enhancer of split-1 (Hes1) and p300 [65]. Hes and Hey families' members are the most well-known Notch targets, which contribute to control many gene expression features related to cell fate regulation such as proliferation, differentiation and apoptosis [61]. The Hes family of transcription factors, specifically Hes1 in the gut, are the best identified Notch targets [66].
Notch-associated-lncRNAs mechanism(s) profiling in cancer
Physiologically, several lncRNAs have been found to have a positive or negative association with the Notch-signaling pathway as well as micro-RNAs or mRNA as the Notch-related molecules [30]. In cancer generally, and colorectal specifically, activation of Notch-signaling can be influenced by several dysregulated lncRNAs, on the other hand, Notch-activation controls the expression of same or other lncRNAs, as depicted in Fig. 3. A list of lncRNAs interacting with the Notch-cascade contributing to various tumors development are presented in Tables 1 and 2.
Table 1.
List of down and upregulated lncRNAs expressions in different cancers and their Notch-target gene(s)
| Expression | LncRNA | Cancer type | Notch-target gene(s) | Refs. |
|---|---|---|---|---|
| Downregulated | LET | Non-small cell lung cancer (NSCLC) | Notch1 intracellular domain | [67] |
| NBR2 | NSCLC & Osteosarcoma | Notch1 | [68, 69] | |
| MEG3 | Endometrial | Notch 1, Hes1 | [70] | |
| MIR22HG | Gastric | Notch2 signaling | [71] | |
| LincRNA-p21 | Hepatocellular | Hes1 and NICD | [72] | |
| LINC00261 | Hepatocellular | Notch1 and Hes1 | [73] | |
| CEBPA-AS1 | Osteosarcoma | Hes1 and RBPJ | [74] | |
| RAMP2-AS1 | Glioblastoma | Notch3 | [75] | |
| HCG18 | Bladder | Notch1 | [76] | |
| PAUPAR | Uveal melanoma | Hes1 | [77] | |
| Upregulated | Xist | NSCLC & Pancreatic | Notch1 via sponging miR-137 | [78, 79] |
| Lbx2-as1 | NSCLC | Notch1, p21, Hes1 | [80] | |
| PVT 1 | NSCLC | Notch1, NICD and HES1 via YAP1 activation | [81] | |
| LINC01783 | NSCLC | DLL-1 via targeting miR-432-5p | [82] | |
| NALT1 | Gastric & Leukemia | Notch 1 | [83, 84] | |
| SNHG1 | Gastric | Notch1 via sponging miR-15b | [85] | |
| Linc01555 | Gastric | Notch1, Notch2, DLL3 and Hes1 | [86] | |
| DLEU2 |
Gastric Cervical |
Notch2 via sponging miR-23b-3p Notch1 and RBPJ through impeding p53 expression |
[87] [88] |
|
| SRA | Cervical | Notch1, Hes1 and p300 | [89] | |
| DARS-AS1 | Cervical | JAG1 via sponging miR-628-5p | [90] | |
| HOTAIR |
Retinoblastoma Cervical Pancreatic |
Notch1 and JAG1 Notch1, Hes1and P300 Notch3 via sponging miR-613 |
[91] [92] [93] |
|
| ROR |
Retinoblastoma Endometrial |
Notch1 via sponging miR-32 Notch1 via regulating miR34a expression |
[94] [95] |
|
| GHET1 | Prostate | Notch1, HIF-1α via negative regulation of KLF2 | [96] | |
| FEZF1-AS1 |
Prostate NSCLC & Glioblastoma |
Notch1, p21 and Hes1 Notch1 via sponging miR-34a |
[97] |
|
| DANCR | Prostate | JAG1 via sponging miR-34a-5p | [99] | |
| Linc-OIP5 |
Glioma Breast |
Jag1, Notch1 and Hes1 JAG1 |
[100] [101] |
|
| ZFAS1 | Glioma | Hes-1 and NICD | [102] | |
| LINC01152 | Glioblastoma | Notch-pathway via MAML2 + ve regulation | [103] | |
| PlncRNA-1 | Glioma | Notch1, JAG1 and Hes1 | [104] | |
| LINC01410 | Glioma | Notch2 | [105] | |
| SNHG3 | Breast | Notch; competitively binding miR-154-3p | [28] | |
| SNHG7 | Breast | Notch 1 via sponging miR-34a | [106] | |
| SNHG12 |
Osteosarcoma Nasopharyngeal |
Notch2 via sponging miR195-5p Notch pathway |
[107] [108] |
|
| CRNDE | Osteosarcoma | Notch1, JAG1 and EMT related proteins | [109] | |
| RP11–567G11.1 |
Pancreatic Renal |
Jagged1, Hes1, Hes5 and Math1 Jagged1, Hes5 and Hey1 |
[110] [111] |
|
| HCG11 | Pancreatic | NICD and Hes1 via sponging miR-579-3p | [112] | |
| LNCRNA00673 | Hepatocellular | Notch1 and Notch3 | [113] | |
| UCA1 | Tongue | JAG1 and Notch1 via sponging miR-124 | [114] | |
| MALAT1 | Ovarian | Notch1 pathway | [115] | |
| DLX6-AS1 | Epithelial ovarian | Notch1, p21 and Hes1 | [116] | |
| LncND | Neuroblastoma | Notch1 & Notch2 via sponging miR-143-3p | [117] | |
| HNF1A-AS1 | Oral squamous cell | Notch1, Hes1 | [118] | |
| CCAL | Papillary thyroid | Notch1 signaling | [119] | |
| LINC01123 | Lung adenocarcinoma | Notch1 via sponging miR-449b-5p | [120] | |
| BANCR | Melanoma | Notch2 via sponging miR‑204 | [121] | |
| Linc00152 | Infantile hemangioma | Notch1, Hes1 and Hey1 | [122] | |
| MEG8 | Hemangioma | Notch2 via sponging miR-497-5p | [123] | |
| HOXA-AS2 | Cervical | NICD | [124] |
Table 2.
List of cancer types with lncRNAs expressions down and upregulated and their Notch-target gene(s)
| Cancer | LncRNA | Expression | Notch-target gene(s) | Refs. |
|---|---|---|---|---|
| NSCLC |
LET NBR2 |
Downregulated |
Notch1 intracellular domain Notch1 |
[67] [69] |
|
Xist Lbx2-as1 PVT1 LINC01783 FEZF1-AS1 |
Upregulated |
Notch1 via sponging miR-137 Notch1, p21 and Hes1 Notch1, NICD and Hes1 via YAP1 activation DLL-1 via targeting miR-432-5p Notch1 via sponging miR-34a |
[79] [80] [81] [82] [27] |
|
| Lung adenocarcinoma | LINC01123 | Upregulated | Notch1 via sponging miR-449b-5p | [120] |
| Osteosarcoma |
NBR2 CEBPA-AS1 |
Downregulated |
Notch1 Hes1 and RBPJ |
[68] [74] |
|
SNHG12 CRNDE |
Upregulated |
Notch2 via sponging miR195-5p Notch1, JAG1 and EMT related proteins |
[107] [109] |
|
| Endometrial | MEG3 | Downregulated | Notch1, Hes1 | [70] |
| ROR | Upregulated | Notch1 via regulating expression of miR34a | [95] | |
| Gastric | MIR22HG | Downregulated | Notch2 signaling | [71] |
|
NALT1 SNHG1 Linc01555 DLEU2 |
Upregulated |
Notch1 Notch1 via sponging miR-15b Notch1, Notch2, DLL3 and Hes1 Notch2 |
[83] [85] [86] [87] |
|
| Hepatocellular |
LincRNA-p21 LINC00261 |
Downregulated |
NICD and Hes1 Notch1 and Hes1 |
[72] [73] |
| LNCRNA00673 | Upregulated | Notch1 and Notch3 | [113] | |
| Glioma | RAMP2-AS1 | Downregulated | Notch3 | [75] |
|
FEZF1-AS1 Linc-OIP5 ZFAS1 LINC01152 PlncRNA-1 LINC01410 |
Upregulated |
Notch1via sponging miR-34a JAG1, Notch1 and Hes1 Hes1 and NICD Notch pathway Notch1, JAG1 and Hes1 Notch2 |
[98] [100] [102] [103] [104] [105] |
|
| Bladder | HCG18 | Downregulated | Notch1 | [76] |
| Pancreatic |
Xist HOTAIR RP11-567G11.1 HCG11 |
Upregulated |
Notch1 via sponging miR-137 Notch3 via sponging miR-613 JAG1, hes1, hes5 and MATH1 NICD and Hes1 via sponging miR-579-3p |
[78] [93] [110] [112] |
| Melanoma | PAUPAR | Downregulated | Hes1 | [77] |
| BANCR | Upregulated | Notch2 via sponging miR-204 | [121] | |
| Cervical |
DLEU2 SRA DARS-AS1 HOTAIR HOXA-AS2 |
Upregulated |
Notch1 and RBPJ through impeding p53 expression Notch1, Hes1 and p300 JAG1 via sponging miR-628-5p Notch1, Hes1 and p300 NICD |
[88] [89] [90] [92] [124] |
| CRC |
FOXD2-AS1 FAM83H‑AS1 LINC00152 DSCAM-AS1 LINC01198 LINC00707 ENST00000455974 GNAS-AS1 & RP11-89K10.1 Lnc34a UICLM |
Upregulated |
NICD, Hes1 Notch1 and Hes1 Notch1 via sponging miR-139-5p Notch1 via sponging miR-137 Notch1, p300 and Hes1 Notch3 & TM4SF1via sponging miR-206 JAG2 Hes1 Notch pathway via sponging miR-34a Notch1 |
[125] [126] [127] [128] [129] [130] [131] [132] [135] |
| Breast |
Linc-OIP5 SNHG3 SNHG7 |
Upregulated |
JAG1 Notch by binding to miR-154-3p Notch1via sponging miR-34a |
[101] [28] [106] |
| Retinoblastoma |
HOTAIR ROR |
Upregulated |
Notch1, JAG1 Notch1 via sponging miR-32 |
[91] [94] |
| Prostate |
GHET1 FEZF1-AS1 DANCR |
Upregulated |
Notch1 and HIF-1 α via negative regulation of KLF2 Notch1, p21 and Hes1 JAG1 via sponging miR-34a-5p |
[96] [97] [99] |
| Tongue | UCA1 | Upregulated | JAG1 and Notch1 via sponging miR-124 | [114] |
| Ovarian |
MALAT1 DLX6-AS1 |
Upregulated |
Notch1 pathway Notch1, p21 and Hes1 |
[115] [116] |
| Renal | RP11-567G11.1 | Upregulated | JAG1, hes5 and Hey1 | [111] |
| Acute leukemia | NALT1 | Upregulated | Notch1 | [84] |
| Nasopharyngeal | SNHG12 | Upregulated | Notch pathway | [108] |
| Neuroblastoma | LncND | Upregulated | Notch1&Notch2 via sponging miR-143-3P | [117] |
| Oral squamous | HNF1A-AS1 | Upregulated | Notch1 and hes1 | [118] |
|
Hemangioma (infantile) |
MEG8 Linc00152 |
Upregulated |
Notch2 via sponging miR-497-5p Notch1, Hes1 and hey1 |
[123] [122] |
| Papillary thyroid | CCAL | Upregulated | Notch1 signal | [119] |
LncRNA-low expression in tumor (lncRNA-LET) a newly discovered lncRNA, was detected on chromosome 15q24.1 [136]. In NSCLC, LET demonstrated a tumor-suppressive effect; its overexpression in cells decreased NICD1 level [67]. As well, Neighbor of BRCA1 gene 2 (NBR2) is lncRNA that is encoded from the gene which locates near to the tumor suppressor gene BRCA1 [137]. NBR2 acts as tumor suppressor by inhibiting Notch1 expression in NSCLC and osteosarcoma [68, 69]. Additionally, Maternally expressed gene 3 (MEG3) is an imprinted gene in humans locating on chromosome 14q32.3, encodes lncRNA MEG3 [138]. lncRNA MEG3 inhibits endometrial tumor growth by negatively regulating Notch1 and Hes1 levels [70].
Human miR-22 host gene (MIR22HG) is a tumor suppressor lncRNA stimulating the expression of miR-22 [139]. MIR22HG suppresses Notch2 signaling, inhibiting progression of gastric cancer [71]. Likewise, LincRNA-p21 is 15 kb upstream from p21 gene, that can control both mRNA translation as well as protein stability [140]. LincRNA-p21 enhanced level reduces expression of Notch proteins, Hes1 and NICD, inhibiting hepatocellular carcinoma invasion and metastasis [72]. Moreover, CCAAT Enhancer Binding Protein Alpha (CEBPA) is a transcription factor that can regulate cell cycle with oncogenic functions [141]. CEBPA-AS1 is the CEBPA antisense RNA1 [142]. CEBPA-AS1 attenuates osteosarcoma progression via inhibiting Notch pathway members, Hes1 and RBPJ [74].
Receptor activity modifying protein 2 (RAMP2) is a single-transmembrane domain protein that plays key role in endothelial homeostasis. lncRNA RAMP2-AS1 is transcribed from RAMP2 antisense [143]. RAMP2-AS1 overexpression in cells represses Notch3 expression, impeding glioblastoma progression [75]. Besides, PAX6 upstream antisense RNA (PAUPAR) is lncRNA that could control expression of its adjacent gene Pax6, a transcription factor which controls neuronal differentiation [144]. PAUPAR serves as tumor suppressor in uveal melanoma via negatively regulation of Hes1 expression [77].
Xist (X inactive specific transcript) is the key regulator of X chromosome inactivation, which results in the stable and reliable one X chromosome silencing in somatic cells of female mammals in early development stages [145]. Xist acts as oncogenic lncRNA in NSCLC & pancreatic cancer via sponging miR-137, promoting Notch1 expression [78, 79]. Additionally, Ladybird-like homeobox gene 2 (LBX2) is a transcription factor encoding gene located on chromosome 2p13.1, involved in regulation of heart development as well as tumorigenesis of CRC [146]. LBX2-AS1, LBX2 antisense1 is lncRNA transcribed from an intron of the same chromosome [147]. In NSCLC, LBX2-AS1 functions as tumor promoter that positively regulates Notch signal markers, Notch1, p21 and Hes1, expressions [80].
Plasmacytoma variant translocation 1 (PVT1) lncRNA was firstly discovered in murine leukemia virus-induced T lymphomas as a ubiquitous retroviral integration site; PVT1 acts as oncogenic lncRNA in many cancers [148]. Upregulation of PVT1 promotes NSCLC progression through Yes-associated protein 1 (YAP1) mediated Notch pathway activation, boosting Notch1, NICD and Hes1 levels [81]. Likewise, Notch 1 associated lncRNA in T cell acute lymphoblastic leukemia1 (NALT1) is identified to cis-regulate its neighboring gene, Notch1, supposing that NALT1 actions is relayed on Notch signaling [83]. NALT1 overexpression activates Notch 1 expression in both gastric cancer and pediatric T cell acute lymphoblastic leukemia [83, 84].
Small nucleolar host gene 1 (SNHG1) is host for 8 small nucleolar RNAs, which contributes to ribosomal RNA modifications [149]. Overexpressed SNHG1 positively regulates Notch 1 and Doublecortin-like kinase 1 (DCLK1) expressions via modulation of miR-15b, inducing EMT in gastric cancer [85]. Besides, Deleted in Lymphocytic Leukemia 2 (DLEU2) is an RNA gene which is firstly discovered in chromosome 13q14 genomic region, a region that is usually eliminated in B-cell chronic lymphocytic leukemia [150]. DLEU2 promotes gastric cancer progression via serving as ceRNA for miR-23b-3p enhancing Notch2 expression [87]. While, upregulated DLEU2 induces cervical cancer proliferation by inhibition Notch pathway activity, Notch1 and RBPJ, through impeding p53 expression [88].
Steroid receptor RNA activator (SRA) is lncRNA that can activate transcriptional activity of steroid receptor [151]. SRA upregulation contributes to cervical tumorigenesis through enhancing Notch signal, promoting Notch1, Hes1 and p300 levels [89]. Additionally, lncRNA DARS antisense RNA 1 (DARS-AS1) that can also regulate its neighboring gene DARS (aspartyl-tRNA synthetase) is identified as tumor enhancer in various cancers [152]. DARS-AS1 enhanced expression positively regulates JAG1 through sponging miR-628-5p, inducing cervical tumorigenesis via Notch activation [90].
HOX transcript antisense RNA (HOTAIR) is lncRNA, transcribed from antisense strand of Homeobox C (HOXC) cluster gene; HOX genes encode essential embryonic development regulators. HOTAIR is a crucial regulator of chromatin structure and organization that controls expression of HOXD cluster genes [153, 154]. HOTAIR serves as tumor promoter, increasing Notch1 and JAG1 expressions in retinoblastoma [91]. Also, HOTAIR overexpression increases Notch markers levels, Notch1, Hes1 and P300, enhancing cervical carcinogenesis [92]. Moreover, HOTAIR positively regulates Notch 3 through serving as ceRNA for miR-613 in pancreatic cancer [93].
Regulator of reprogramming (ROR) is promoter lncRNA for reprogramming of pluripotent stem cells. ROR is a key player in human embryonic stem cells self-renewal and differentiation [155]. ROR higher levels activates Notch1 expression via negative regulation of miR-32, stimulating EMT in retinoblastoma [94]. While ROR enhances Notch1 expression in endometrial cancer via regulating of miR34a [95]. As well, gastric carcinoma highly expressed transcript 1 (GHET1) is a confirmed oncogene lncRNA in multiple tumors [156]. Upregulated GHET1 increases prostate cancer proliferation through inducing HIF-1α and Notch 1 signal via negative regulation of Kruppel-like factor 2 (KLF2) [96].
FEZF1-AS1 is FEZ family Zinc Finger 1-Antisense RNA 1, a novel oncogenic lncRNA in various tumors [157]. FEZF1-AS1 is a tumor promoter in prostate cancer via Notch signal activation, overexpressed FEZF1-AS1 contributes to higher levels of Notch1, p21 and Hes1 [97]. On the other hand, FEZF1-AS1 upregulates Notch1 in NSCLC and glioblastoma via negative regulation of miR-34a [27, 98]. Besides, Differentiation antagonizing non-protein coding RNA (DANCR) is a lncRNA prevents differentiation of epidermal progenitor cells into osteoblasts [158]. DANCR overexpression positively regulates JAG1 via targeting miR-34a-5p, aggravating prostatic cancer resistance to docetaxel [99].
Linc-OIP5 (opa interacting protein5) is identified to regulate neurogenesis [159]. Linc-OIP5 overexpression enhances glioma tumorigenesis through Notch activation, upregulating JAG1, Notch-1 and Hes1 expressions [100]. Also, Linc-OIP5 knockdown in breast cancer cells was highly associated with JAG1 expression downregulation [101]. On the other hand, Zinc Finger NFX1-Type Containing 1 (ZNFX1) antisense RNA (ZFAS1) is an lncRNA transcribed from antisense strand next to ZNFX1 protein coding gene; ZFAS1 is identified as a regulator of alveolar and epithelial cell development in the mammary gland [160]. ZFAS1 serves as tumor promoter in glioma cells through upregulating of Notch pathway, enhancing Hes-1 and NICD levels [102]. Likewise, Prostate cancer-up-regulated RNA 1 (PlncRNA-1) is lncRNA transcript that is firstly recognized to be overexpressed in prostate cancer [161]. PlncRNA-1 overexpression induces glioma progression through boosting expressions of Notch1, JAG1 and Hes1, stimulating Notch signal [104].
Colorectal Neoplasia Differentially Expressed (CRNDE) lncRNA exhibits tissue-specific and time-specific expression patterns, is firstly discovered with its upregulated expression in colorectal adenomas and carcinomas [162]. overexpressed CRNDE lncRNA functions as oncogene in osteosarcoma cells via upregulation of Notch1, JAG1 and EMT related proteins [109]. Additionally, Urothelial carcinoma associated 1 (UCA1) is a lncRNA that is primarily discovered from cell lines of bladder cancer [163]. UCA1 elevated level positively regulates JAG1 and Notch1 through targeting miR-124, promoting tongue carcinoma [114].
Metastasis associated in lung adenocarcinoma transcript 1 (MALAT1) lnRNA is originally recognized in non-small-cell lung cancer (NSCLC) primary stages study, so was given that name. MALAT1 clinical relevance is related to metastasis prediction and survival in NSCLC early stages [164]. By blocking the Notch1 signalling pathway, MALAT-1 knockdown increased the chemosensitivity of ovarian cancer cells to cisplatin [115]. Besides, Distal-less homeobox 6 antisense 1 (DLX6-AS1) is a lncRNA expressed in normal brain tissue [165]. Upregulated DLX6-AS1 is epithelial ovarian tumor enhancer through modulating of Notch signal, DLX6-AS1 silencing was highly associated with decreasing levels of Notch1, p21, and Hes1 [116].
LncRNA for neurodevelopment (LncND) is linked to a neuro-developmental diseases in humans [117]. LncND overexpression upregulates Notch1 & Notch2 in neuroblastoma cells through inhibiting of miR-143-3p [117]. On the other hand, Hepatocyte nuclear factor-1 homeobox A (HNF1A) antisense RNA 1 (HNF1A-AS1) lncRNA is transcribed in the reverse direction of the HNF1A gene [166]. HNF1A-AS1 increased expression stimulates Notch pathway in oral squamous cell carcinoma; suppression of HNF1A-AS1 inhibits the expression of Notch1 and Hes1 [118].
Colorectal cancer-associated lncRNA (CCAL) has a verified oncogenic functions in CRC cells [167]. Upregulated CCAL activates Notch1 pathway, which aided in the progression of papillary thyroid cancer [119]. Additionally, BRAF-activated non-coding RNA (BANCR) is lncRNA discovered in melanoma cells at first, then its aberrant expression was verified in several cancers including CRC [168]. In melanoma, BANCR is a tumor promoter, negatively targets miR‑204, enhancing Notch 2 expression [121].
HOXA cluster antisense RNA2 (HOXA-AS2) lncRNA is transcribed from region between HOXA3 and HOXA4 regions [169]. In cervical cancer cells, HOXA-AS2 triggers Notch signal, downregulation of HOXA-AS2 contributes to decreased NICD protein level as well as significantly reducing interaction between NICD and the transcription factor RBP-JK [124].
Molecular mechanisms driving CRC in relation to Notch-Signaling
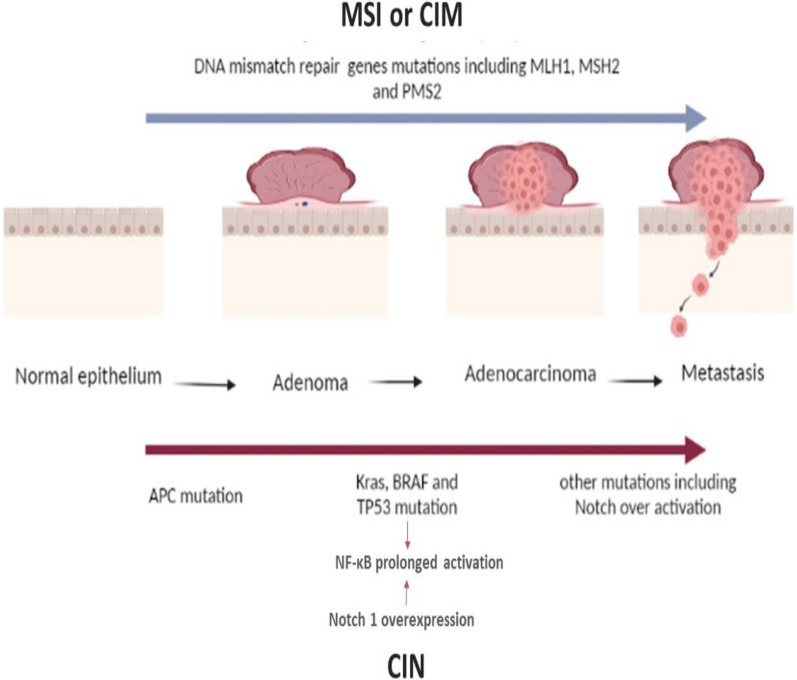
Mechanisms accompanied by oncogene(s) activation and inhibition of tumor suppressors expression [5], though driving CRC formation as in Fig. 4 are chromosomal instability (CIN), CpG island methylation (CIM), and microsatellite instability (MSI) [170].
The conventional chromosomal instability mechanism is characterized by the accumulation of mutations that are initiated after mutational inactivation in the adenomatous polyposis coli (APC), accompanied by oncogenes activations including ki-ras2 Kirsten rat sarcoma viral oncogene homolog (Kras), cyclooxygenase-2 (COX2) and v-raf murine sarcoma viral oncogene homolog B1 (BRAF), tumor suppressor genes silencing including TP53, Deleted in colon cancer/Deleted in pancreatic cancer locus4 (DCC/DPC4) and loss of heterozygosity of chromosome 18 [171, 172].
Microsatellite instability is caused by faulty or inactive DNA mismatch repair genes (MMR). Mutations in MMR genes create genetic abnormalities in other tumor suppressor genes that are associated with growth control [171]. Hereditary non-polyposis CRC syndrome and Lynch syndrome are characterized by microsatellite instability, resulting from one of MMR genes hereditary mutations such as MLH1, MSH2, and PMS2 [170, 173].
CpG island methylation pathway is identified by hypermethylation of CpG islands in gene promotors, contributing to transcriptional inhibition of varies tumor suppressor genes including MMR genes [173].
It is noteworthy to mention that inflammation-driven CRC promoted by a mutant version of the tumor protein 53 (p53(, is mediated via the nuclear factor kappa B cell (NF-κB) prolonged activation [174]. NF-κB activation is enhanced by Notch1 overexpression, which upregulates the transcriptional activity of NF-kappa-B p65 subunit [175]. Furthermore, inactivation of TP53 enhances the progression of Notch-induced invasive adenocarcinoma (in the glandular tissue) with EMT characteristics [176]. In other words, we can infer that combination of Notch1 hyperactivity with oncogenic Kras activation and TP53 inactivation promotes high rates of metastasis of intestinal adenocarcinoma [17] (Fig. 4).
Fig. 4.
Molecular mechanisms driving CRC in relation to Notch-signaling. APC adenomatous polyposis coli, BRAF v-raf murine sarcoma viral oncogene homolog B1, CIM CpG island methylation, CIN Chromosomal instability, Kras Ki-ras2 Kirsten rat sarcoma viral oncogene homolog, MSI microsatellite instability, NF-κB nuclear factor kappa B cell, TP53 tumor protein p53
Notch signaling as a regulator of CRC immune response
Substantial evidence supports the critical function of the Notch pathway in the immune system [177]. Notch signal controls the activation of, CD8+ cytotoxic T cell, which is the key player in the anti-tumor immunological function [178]. Additionally, the crosstalk between tumor cells and dendritic cells, which is necessary for the generation and proliferation of T regulatory (Treg) cells in the TME, is significantly influenced by JAG1-induced Notch activation [179]. JAG1-Notch3 signal activation has been revealed to be crucial for Treg generation and expansion driven by OX40 ligand [180]. Besides, JAG1-mediated maturation of dendritic cells encourages Treg survival and proliferation [181].
In CRC, both peripheral blood samples and tissues showed increased Notch1, Hes1 and Hes5 mRNA expressions in CD8+ T cells, while Notch2 mainly displayed enhanced level in tissue specimens [182]. Notch signal has potential immunosuppressive effect, which inhibits CD8+ T lymphocytes' cytolytic and noncytolytic activities by inducing programmed cell death protein-1 (PD-1). Silencing the Notch pathway enhances the cytotoxicity of tumor-infiltrating CD8+ T cells via increasing their production of pro-inflammatory cytokines such as interferon gamma (IFN-γ), interleukin-1β (IL-1β), IL-6, IL-8, tumor necrosis factor alpha (TNF-α), and vascular endothelial growth factor (VEGF) as well as reducing their PD-1 expression [182]. Likewise, it was showed that mutations in the Notch system were related with a rise in amount of tumor CD8+ T cells and a decline in Treg cells, with increasing expressions of immune checkpoints, chemokines and some effector molecules [183]. Notch mutation- induced immune checkpoints upregulation can stimulate better anti-tumor immunological response, suggesting that patients with these mutations may be more responsive to immune checkpoint blockades, which is a promising therapeutic approach intended to restore anticancer immune responses [183, 184].
Moreover, over activation of Notch1 signal drives metastasis in CRC in neutrophil-dependent manner via promoting chemokine CXCL5 (C-X-C Motif Chemokine Ligand 5) and transforming Growth Factor β (TGF-β) productions, triggering an inhibitory strategy to suppress T cell responses in the TME and create an immune-suppressed environment [17]. Additionally, accumulation of myeloid derived CD11b expressing cells in regions, where cells experienced EMT, requires Jag2 expression stimulating Notch signal and EMT [185]. Furthermore, it has been shown that measuring the proportion of circulating CD11b-Jag2 cells in patients may provide a sign of CRC development into a metastatic state [185].
Mechanism(s) by which upregulated-Notch-associated lncRNAs cause CRC (Table 3)
Table 3.
Mechanisms by which upregulated-Notch-associated lncRNAs cause CRC
| Notch-associated lncRNA | Mechanism(s) driving CRC | Refs. |
|---|---|---|
| LINC00152 | promotes cell proliferation, growth, invasion & migration & progression | [127] |
| LINC00707 | [130] | |
| DSCAM-AS1 | [128] | |
| FOXD2-AS1 | [125] | |
| ENST00000455974 | [131] | |
| GNAS-AS1 & RP11-89K10.1 | [132] | |
| UICLM | promotes CRC proliferation, growth, invasion, migration & regulates stemness | [135] |
| Lnc34a | promotes cancer stem cells self-renewal & CRC progression | [133, 134] |
| FAM83H‑AS1 |
promotes cell cycle progression, cell proliferation, invasion, migration & inhibits apoptosis |
[126] |
| LINC01198 | [129] | |
| LUNAR1 | [188] |
LINC00152 named cytoskeleton regulator (CYTOR) was an overexpressed lncRNA in CRC tissues, acting via sponging miR-139-5p, leading to positive regulation of Notch1 expression. knockdown of Notch1 expression was shown to effectively inhibit CRC cell growth caused by LINC00152 upregulation, proving evidence that activities of LINC00152 are relayed on Notch1 activation [127].
Likewise, LINC00707 expression was highly elevated in CRC tissues, to sponge miR-206 and regulate expression of its target molecules, Notch3 and transmembrane 4 L six family member 1 (TM4SF1) [130].
Additionally, lncRNA Down syndrome cell adhesion molecule Antisense RNA 1 (DSCAM-AS1) is a tumor promoter that is upregulated in CRC tissues. DSCAM-AS1 positively regulates Notch1 through targeting miR-137. Where, the inhibitory effects caused by silencing of DSCAM-AS1 in CRC cells, could be reversed by Notch1 overexpression or miR-137 suppression [128].
Besides, LncRNA FOXD2 adjacent opposite strand RNA 1 (FOXD2-AS1) was significantly overexpressed in CRC tissues. Inhibition of FOXD2-AS1 expression in CRC cells resulted in an enhancement of E-cadherin protein expression, decreasing the expression of N-cadherin and the Snail protein as well as significant decrement in the Notch-related proteins (NICD and Hes-1) expression, suggesting that FOXD2-AS1 promoted CRC progression through regulation of EMT and Notch pathway [125].
In addition, ENST00000455974 is an upregulated lncRNA in DNA mismatch repair-proficient colon cancer tissues. ENST00000455974 can regulate both mRNA and the Notch-signaling ligand JAG2 protein expression [131].
Moreover, Yuqin Zhang et al., verified that lncRNAs GNAS Antisense RNA 1 (GNAS-AS1) and RP11-465L10.10 expressions were significantly elevated in CRC tissues, being involved in CRC development through direct binding to the Notch downstream target Hes1132. Hes1 is involved in CRC stem cells self-renewal and tumorgenicity, promoting cell proliferation and migration [186, 187].
Furthermore, the expression of up-regulated in CRC liver metastasis (UICLM) lncRNA was elevated in CRC tissues, when being silenced, contributing to the downregulation of essential stemness-related-genes, including Notch1 [135].
In addition, the lncRNA-34a (Lnc34a) is increased in CRC and epigenetically suppresses miR-34a expression [133].
Besides, the expression of lncRNA FAM83H antisense RNA1 (FAM83H‑AS1) was enhanced in CRC tissues, and when was knocked down in CRC cell lines, resulted in suppression in both mRNA and Notch1 and Hes1 protein levels, countered through the Notch-signal activator JAG1 [126].
LINC01198 was an another upregulated lncRNA in CRC tissues that regulates Notch-pathway markers, namely, Notch1, p300 and Hes1 [129].
Moreover, Leukemia-Associated Non-Coding IGF1R Activator RNA 1 (LUNAR1), a novel Notch-regulated lncRNA, was recently reported to be significantly upregulated in CRC tissues [188, 189], induced by Notch1 activation, enhancing CRC progression through sustaining insulin-like growth factor 1 receptor (IGF-1R) expression [188].
Notch-associated lncRNAs impact on CRC clinical outcome (Table 4).
Table 4.
Notch-associated lncRNAs impact on CRC clinical outcome
| Notch-associated lncRNA |
CRC clinical outcome | Refs. | |||
|---|---|---|---|---|---|
| Size, TNM; Tumor stage | Disease-free survival/ OS | Recurrence/ Metastasis |
Hazard ratio (HR) | ||
| FOXD2-AS1 | – | Poor OS | – | 2.245 | [190] |
| FAM83H‑AS1 |
Larger size ≥ 5 cm, advanced stage III-IV |
Poor OS | – | 1.542; 95% confidence interval (CI) (1.115–2.135) | [126, 192] |
| LINC00152 | advanced stage III-IV | Poor disease-free survival & OS | Recurrence in Oxaliplatin-receiving patients | 3.825; 95%(CI) (1.723–8.493) | [127, 194] |
| LINC00707 |
Larger size ≥ 5 cm, advanced stage III-IV |
Poor OS | Lymphatic metastasis & distant metastasis |
4.255; 95%(CI) (1.560–11.610) |
[130, 196] |
| DSCAM-AS1 | Advanced stage III-IV | Poor OS | Metastasis | – | [128] |
| ENST00000455974 | – | Poor progression free survival |
14.404; 95% (CI) (1.785, 116.242) |
[131] | |
| UICLM |
Larger size, advanced stage III-IV |
Worse progression free survival | Liver metastasis |
2.13; 95%(CI) (1.77–3.06) |
[135] |
| LUNAR1 | Advanced stage III-IV | Unfavorable disease-free survival & OS | TNM | 3.25; 95%(CI) (1.98–5.31) | [188] |
Upregulation of FOXD2-AS1 is a predictor for poor survival in CRC, where FOXD2-AS1 higher expression was associated with clinical lower survival rate [190]. Furthermore, 12-year follow-up study after surgery, the survival rate analysis showed patients with enhanced FOXD2-AS1 expression, significantly exhibited 6-year survival rate, not 12-year, relative to those with lower expression [191].
FAM83H‑AS1 is an independent prognostic indicator in colon cancer. Where, patients with greater level of FAM83H‑AS1 had shorter OS time compared to patients with lower level [192]. Furthermore, FAM83H‑AS1 higher levels were significantly associated with larger tumor size and advanced tumor stage [126].
Additionally, overexpression of LINC00152 was associated with poor CRC prognosis, advanced tumor stage and worse OS as well as disease-free survival [127, 193]. Moreover, Linc00152 can be used as predictor for response of Oxaliplatin-receiving-patients, after radical colectomy, where high Linc00152 expression in Oxaliplatin-receiving-patients was associated with an increased N stage, recurrence, shorter OS and recurrence-free survival in comparison to patients with lower expression [194].
Likewise, LINC00707 and DSCAM-AS1 elevated levels are associated with poor patients' prognosis, shorter OS relative to those with lower expression [128, 195, 196]. LINC00707 enhanced expression was positively correlated with larger tumor size, advanced TNM stage, lymphatic metastasis and distant metastasis [130, 196].
DSCAM-AS1 upregulation was correlated to advanced clinical stage and metastasis status [128].
Besides, patients with higher levels of ENST00000455974 or UICLM had worse progression-free survival [131, 135]. Higher levels of UICLM were significantly correlated with CRC larger tumor size, advanced tumor stage as well as liver metastasis [135].
Again, LUNAR1 upregulation is associated with aggressive CRC, advanced tumor stage, poor differentiation status (high grade and stage), deeper tumor invasion and TNM, being attributed to unfavorable disease-free survival as well as OS [188].
Notch-associated lncRNAs in relation to multi-drug resistance (MDR) in CRC (Table 5)
Table 5.
Notch-associated lncRNAs in relation to multi-drug resistance in CRC
| Notch-associated lncRNA |
Multi-drug resistance in CRC | Refs. | |||
|---|---|---|---|---|---|
| Chemotherapy used | miR sponged | Target protein(s) | Effect on apoptosis | ||
| LINC00152 | Oxaliplatin |
miR-193a-3p miR-139-5p |
-ERBB4 with AKT signal activation -Notch1 which induces upregulating of MRP-1 and BcL-2 |
Suppressed | [25, 127, 194] |
| LINC00707 |
5-FU topotecan, cisplatin & Astragaloside IV |
miR-206 |
- Bcl-2 -Notch3 |
Lower apoptosis rate | [130, 199–201] |
| DSCAM-AS1 | Oxaliplatin | miR-137 |
-YBX1 - Notch1 which induces upregulating MRP-1 and BcL-2 |
Inhibition of cytotoxicity | [25, 128, 203] |
| Lnc34a | 5-FU | miR-34a | Lactate dehydrogenase | Inhibited | [133, 204] |
| ENST00000455974 |
Doxorubicin, 5-FU, Oxaliplatin |
– | JAG2 | Decreased apoptosis | [131, 205] |
| FAM83H‑AS1 | 5-FU | – |
-Notch1 which induces upregulating MRP-1 & BcL-2 -Hes1 which induces upregulating ABCC1, ABCC2, P-gp1 & N-cadherin & suppressing of E-cadherin |
Inhibited | [23, 25, 126] |
| UICLM | 5-FU | – | Notch1 which induces upregulating MRP-1 & BcL-2 | Inhibited | [25, 135] |
| FOXD2-AS1 | 5-FU | – | Hes1 which induces upregulating ABCC1, ABCC2, P-gp1 & N-cadherin & suppressing of E-cadherin | [23, 125] | |
|
GNAS-AS1 RP11-89K10.1 |
5-FU | – | Hes1 which induces upregulating ABCC1, ABCC2, P-gp1 & N-cadherin & suppressing of E-cadherin | [23, 132] | |
| LINC01198 | 5-FU |
-Notch1 which induces upregulating MRP-1 and BcL-2 -Hes1 which induces upregulating ABCC1, ABCC2, P-gp1 & N-cadherin &suppressing of E-cadherin |
Inhibited | [23, 25, 129] | |
| LUNAR1 | 5-FU | IGF-1R | Inhibited | [188, 210] | |
Cancer cells' adaptation reaction, to a diversity of cytotoxic drugs, is MDR, an obstacle to achieve effective chemotherapy [197].
Overexpression of linc00152 promoted colon cancer resistance to oxaliplatin-induced apoptosis. Linc00152 mediates drug resistance, through modulating erb-b2 receptor tyrosine kinase 4 (ERBB4) expression, by functioning as ceRNA negatively regulating miR-193a-3p expression with AKT (Protein kinase B) signaling activation [194]. Additionally, linc00152 overexpression inhibits 5-fluorouracil (5-FU) induced cell death in CRC, through activation of Notch1 and sponging miR-139-5p [127].
LINC00707 acts as ceRNA targeting miR-206 and inhibiting its expression, promoting its target Notch3 expression [130, 198]. MiR-206 downregulation, enhances resistance towards 5-FU by positively regulating B-cell lymphoma-2 (Bcl-2) protein level in CRC [199]. Additionally, downregulation of Notch3 in CRC cells was shown to improve the cells' chemosensitivity to topotecan as well as cisplatin with astragaloside IV coadministration [200, 201]. Therefore, LINC00707 may contribute to MDR through regulation of miR-206/Notch3 axis.
Likewise, DSCAM-AS1 targets miR-137 and negatively regulates its expression in CRC and breast cancer [128, 202]. Hence, downregulation of miR-137, promotes oxaliplatin-resistance via targeting Y-Box Binding Protein 1 (YBX1) [203].
Also, Lnc34a acts as ceRNA negatively regulating miR-34a expression [133]. miR-34a downregulation was shown to be associated with 5-FU resistance in colon cancer cells, via upregulation of its target protein levels lactate dehydrogenase [204].
Besides, ENST00000455974 positively regulates JAG2 expression. In CRC, JAG2 increased expression was shown to enhance chemoresistance to doxorubicin-induced cytotoxicity. Silencing JAG2, induced CRC cells apoptosis via suppression of p21 expression [205]. Additionally, knockdown of JAG2 expression was found to increase CRC cells chemosensitivity to 5-FU and oxaliplatin [205].
Moreover, studies identified that Notch1 could regulate MDR related genes multidrug resistance protein 1 (MRP1)/ ATP binding cassette subfamily C member 1 (ABCC1) and BcL-2 in cancer cells [206, 207]. In CRC, Notch1 overexpression is contributed to 5-FU resistance, Notch1 suppression via miR-139-5p overexpression increases 5-FU sensitization in CRC cells, depending on Notch1 downstream targets MRP-1 and BcL-2 downregulation [25]. Likewise, downregulation of Notch1 by miR-139-5p overexpression was associated with increasing drug sensitivity in MDR related to non-kinase transmembrane glycoprotein (CD44+) and CD133+ (prominin-1) CRC cells [208].
Furthermore, Hes1 elevated expression induces 5-FU resistance in CRC via enhancing EMT and ATP-binding cassette (ABC) transporters. Hes1 increased levels in CRC cells were highly associated with N-cadherin increasing expression, and E-cadherin suppressing expression which promote EMT [23]. Additionally, overexpression of Hes1 was contributed to upregulation of several ABC transporters, ABCC1, ABCC2 and p-glycoprotein 1 (P-gp1) which are crucial components in the metabolism of drugs [23]. ABC transporters are regarded as primary cause of treatment failure via reducing drug uptake and accumulation in cells. Resistance to a wide spectrum of anticancer medicines is conferred by overexpression of the ABCC1 transporter [23, 209].
In addition, LUNAR1 may be involved in conferring 5-FU resistance, being positively regulator of IGF-1R expression [188]. In human CRC cells, IGF-1R suppression could improve 5-FU-induced cell apoptosis and viability inhibition [210].
Notch-associated lncRNAs in relation to metastasis or recurrence in CRC (Table 6)
Table 6.
Notch-associated lncRNAs in relation to metastasis or recurrence in CRC
| Notch-associated lncRNA |
CRC | Refs. | |||
|---|---|---|---|---|---|
| Notch regulated | miR sponged | Target protein | Recurrence ± | ||
| UICLM | – | miR-215 | ZEB2 | Liver metastasis | [135] |
| DSCAM-AS1 | – | miR-216b | Higher levels are associated with metastasis | [128, 213] | |
| LINC00152 | – | miR-185-3p and miR-632 |
-FSCN1 -E-cadherin & mesenchymal markers vimentin & N-cadherin through interacting with β-catenin |
Promotes colon cancer cells invasion & metastasis |
[215] [217] |
| LINC00707 | Notch3 | – | – | Recurrence | [130, 218] |
UICLM increased level promotes liver metastasis in CRC through positively regulation of zinc finger E-box binding homeobox 2 (ZEB2) expression by sponging miR-215 [135]. ZEB2 is an E-cadherin transcriptional repressor regulates EMT [211, 212]. Additionally, expression of DSCAM-AS1 was significantly increased in patients with tumor metastasis compared to non-metastasis patients [128, 213]. DSCAM-AS1 induces invasion and migration of CRC cells through negative regulation of miR-216b [213].
Moreover, LINC00152 upregulation promotes CRC metastasis through positively regulation of Fascin actin-bundling protein 1 (FSCN1) expression via sponging miR-185-3p and miR-632. Fascin plays an important role in creating actin-based cellular protrusions, promoting motility and migration of CRC cells [214–216]. LINC00152 silencing in colon cancer cells was associated with increased E-cadherin level and decreased levels of mesenchymal markers vimentin and N-cadherin [217]. LINC00152 overexpression consistently contributed to epithelial properties loss and the development of mesenchymal traits in colon cells, promoting colon cancer cellular invasion and metastasis through interacting with β-catenin [217]. Beside, LINC00707 positively regulates Notch3 expression [130]. Notch3 increased nuclear expression has been attributed to tumor recurrence and could be used as a potential predictor in recurrent stages II and III CRC [218].
Notch activation to facilitate CRC metastasis, mediated via EMT process
EMT has contributed to a crosstalk between Notch receptors and their ligands in CRC [219] (Fig. 5A and 5B).
Fig. 5.
A Notch signaling induced EMT in CRC. MMP matrix metalloproteinases, SLUG snail family transcriptional repressor 2, Smad-3; SMAD family member 3, TGF β Transforming Growth Factor β. B Notch signaling induced EMT in CRC
Prolonged Notch1 activation in the epithelial cells cause a senescence-like state, allowing tumor cells to trans-migrate from the main tumor and recruitment to distant locations [21]. Notch1 overexpression enhances Snail expression and inhibits E-cadherin expression in the immortalized endothelium cells, with induction of EMT and malignant transformation [220]. Activation of Notch-signaling contributes to hypoxia induced tumor cells invasion and migration [221].
In CRC, Notch1-signal enhances EMT, due to its interaction with transcription factor controlling EMT and TGF-β, promoting more TME driving metastasis [16]. Likewise, Fender et al., showed that higher level of the EMT-related proteins CD44, snail family transcriptional repressor 2 (SLUG), and SMAD family member 3(Smad-3), as well as phenotypic alterations in CRC cells, emerged from constitutive activation of NICD1 in CRC cells [22].
Activity of Jagged-1 is regulated by Notch1, which then activates Notch3, leading to an increased production of SLUG and CD44 [22].
Sonoshita et al., showed that inhibition of Notch-signal causes suppression in CRC tumor invasion and intravasation activated by knockdown of Amino-terminal enhancer of split (Aes) gene in ApcΔ716mice intestinal polyposis, pointing out to Notch-signal inhibition as a potential player during CRC metastasis prevention and treatment [222].
The Notch-related protein, Hes1, enhances CRC metastasis through induction of EMT; Upregulation of Hes1 contributed to loss of cell adhesion via repressing E-cadherin expression and enhancing N-cadherin, vimentin as well as the EMT inducer Twist-1 expressions [223]. Moreover, Hes1 overexpression was associated with an increased matrix metalloproteinases members (MMP2 and MMP9) mRNA levels in CRC cells, promoting tumor invasion [223]. Furthermore, Hes1 increases invasion via positively regulating MMP14 expression, mediated through STAT3 activity upregulation [224]. Therefore, patients with an increased Hes1 in stage II CRC, would have a higher recurrence rate chances after treatment [23].
Conclusion and prospective
CRC has recognized as a dominant public health issue due to its high frequency and fatality rates [1]. Patients' prognosis remains poor despite substantial advancements in its treatments. Additionally, post-surgical relapse and metastases occur frequently [2, 4, 225]. Therefore, it is crucial to consider attentively the developments of novel biomarkers for CRC prognosis and treatment. Since the disruption of molecular pathways is a distinct characteristic of CRC, a variety of evaluations have suggested that pathways could be used as CRC treatment targets [226].
Recent studies have confirmed the major role of Notch signal in CRC progress. Notch signaling is capable of controlling both the homeostatic self-renewal and tumorigenic transformation of intestinal epithelial cells [15]. Additionally, epigenetic modifications have been shown to greatly contribute to occurrence and progression of inflammation enhanced CRC, and understanding of these alterations will aid to novel therapeutic alternatives detection [227]. The interplay of lncRNAs and Notch signal introduces innovative suggestion for CRC medication development.
In this review, we illustrated that Notch-associated lncRNAs displayed pivotal epigenetic regulatory role among cancer different aspects (growth, resistance, recurrence, and metastasis). The review summarized these regulatory control/involvement to come to a clearer understanding of Notch-related lncRNAs and their mechanisms upon cancer cells and the reverse, in CRC or other various cancer types. We enumerated a list of lncRNAs, described to influence, or are influenced by Notch-signaling activation, leading to colorectal tumorigenesis. Dysregulation of Notch-associated lncRNAs revealed to be highly associated with CRC progression/recurrence or conferring MDR as well as being involved in CRC metastasis. Thence, Notch-associated lncRNAs might be useful prognostic biomarkers or promising potential therapeutic targets for CRC treatment.
However, the impact of Notch associated lncRNAs in CRC, Few studies are available about lncRNAs GNAS-AS1 and RP11-89K10.1 and their impact on CRC clinical outcomes is still unknown, and their function(s) in CRC require further identification. The direct interaction between lnc34a and Notch-signaling is not fully elucidated. Additionally, other transcriptional regulators as histone modification, chromatin remodeling, and X chromosome inactivation to be addressed in another review.
Abbreviations
- ABC
ATP-binding cassette
- ADAM
A disintegrin and metalloproteinase
- Aes
Amino-terminal enhancer of split
- APC
Adenomatous polyposis coli
- AKT
Protein kinase B
- Bcl-2
B-cell lymphoma-2
- BRAF
V-raf murine sarcoma viral oncogene homolog B1
- CD133
Prominin-1
- ceRNA
Competitive endogenous RNA
- CRC
Colorectal cancer
- CSL
CBF1, Suppressor of Hairless, Lag-1
- Co-A MAM
Co-A activators mastermind
- CIN
Chromosomal instability
- CIM
CpG island methylation
- COX2
Cyclooxygenase-2
- CXCL5
C-X-C Motif Chemokine Ligand 5
- DCLK1
Doublecortin-like kinase 1
- EMT
Epithelial-mesenchymal transition
- eRNAs
Enhancer RNAs
- ERBB4
Erb-b2 receptor tyrosine kinase 4
- FSCN1
Fascin actin-bundling protein 1
- 5-FU
5-Fluorouracil
- Hes1
Hairy and enhancer of split-1
- HCG11
18; Human leucocyte antigen complex group 11, 18
- HEY1
Hairy/enhancer-of-split related with YRPW motif protein1
- HIF1α
Hypoxia-inducible factor 1α
- IGF-1R
Insulin-like growth factor 1 receptor
- IFN-γ
Interferon gamma
- IL-1β
Interleukin-1β
- Kras
Ki-ras2 Kirsten rat sarcoma viral oncogene homolog
- KLF2
Kruppel-like factor 2
- LncRNAs
Long non-coding RNAs
- LINC00261
Long Intergenic Non-Protein Coding RNA 261
- MAML
Mastermind like transcriptional coactivator
- MATH1
A mouse homolog of the Drosophila proneural gene atonal
- MDR
Multidrug resistance
- MiRNAs
Micro-RNAs
- MSI
Microsatellite instability
- MMR
Mismatch repair genes
- MMP
Matrix metalloproteinases
- MLH1
mutL homolog 1
- MSH2
mutS homolog 2
- NATs
Natural antisense transcripts
- NcRNAs
Non-protein coding RNAs
- NECD
Notch extracellular domain
- NICD
Notch intracellular domain
- NSCLC
Non-small cell lung cancer
- OS
Overall survival
- PD-1
Programmed cell death protein-1
- P-gp1
P-glycoprotein 1
- PMS2
PMS1 homolog 2
- RBPJ transcription factor
Recombination signal binding protein for immunoglobulin kappa J region
- RNP
Ribonucleoprotein
- SLUG
Snail family transcriptional repressor 2
- Smad3
SMAD family member 3
- SNHG3
7, 12, Small nucleolar RNA host gene 3, 7, 12
- Stat3
Signal transducer and activator of transcription 3
- TFs
Transcription factors
- TGF β
Transforming Growth Factor β
- TNF-α
Tumor necrosis factor alpha
- TNM
Tumor-lymph node-metastasis
- TM4SF1
Transmembrane 4 L six family member 1
- TP53 or p53
Tumor protein p53
- VEGF
Vascular endothelial growth factor
- YAP1
Yes-associated protein 1
- YBX1
Y-Box Binding Protein 1
- ZEB2
Zinc finger E-box binding homeobox 2
Author contributions
EO data curation, original draft preparation and rewriting, figures and tables construction, FE editing, rewriting, figures and tables revision, HNM conceptualization, supervision, tables and figures idea creation and revision, editing, rewriting, reviewing from submission till acceptance.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publications
All authors have read the manuscript and agreed to publish.
Competing interests
Authors declare there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Omnia Emam, Email: omneya.emam@pharma.asu.edu.eg.
Eman F. Wasfey, Email: eman_wasfey@pharma.asu.edu.eg
Nadia M. Hamdy, Email: nadia_hamdy@pharma.asu.edu.eg
References
- 1.Bray F, Ferlay J, Soerjomataram I. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Tang XJ, Wang W, Hann SS. Interactions among lncRNAs, miRNAs and mRNA in colorectal cancer. Biochimie. 2019;163:58–72. doi: 10.1016/j.biochi.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89–103. doi: 10.5114/pg.2018.81072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheng H, Wei X, Mao M, He J, Luo T, Lu S, et al. Adenocarcinoma with mixed subtypes is a rare but aggressive histologic subtype in colorectal cancer. BMC Cancer. 2019;19(1):1–11. doi: 10.1186/s12885-019-6245-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He J, Wu F, Han Z, Hu M, Lin W, Li Y, et al. Biomarkers (mRNAs and non-coding RNAs) for the diagnosis and prognosis of colorectal cancer—from the body fluid to tissue level. Front Oncol. 2021;11(April):1–14. doi: 10.3389/fonc.2021.632834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simon K. Colorectal cancer development and advances in screening. Clin Interv Aging. 2016;11:967–976. doi: 10.2147/CIA.S109285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morgan TH. The theory of the gene. Am Nat. 1917;51(609):513–544. doi: 10.1086/279629. [DOI] [Google Scholar]
- 8.Luo Z, Shang X, Zhang H, Wang G, Massey PA, Barton SR, et al. Notch signaling in osteogenesis, osteoclastogenesis, and angiogenesis. Am J Pathol. 2019;189(8):1495–1500. doi: 10.1016/j.ajpath.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai EC. Notch signaling: control of cell communication and cell fate. Development. 2004;131(5):965–973. doi: 10.1242/dev.01074. [DOI] [PubMed] [Google Scholar]
- 10.Weng AP, Ferrando AA, Lee W, Morris JP, Silverman LB, Sanchez-Irizarry C, et al. Activating mutations of NOTCH1 in human T cell acute lymphoblastic leukemia. Science (80-) 2004;306(5694):269–271. doi: 10.1126/science.1102160. [DOI] [PubMed] [Google Scholar]
- 11.McCarter AC, Wang Q, Chiang M. Notch in leukemia. In: Borggrefe T, Giaimo BD, editors. Molecular mechanisms of notch signaling. Cham: Springer International Publishing; 2018. pp. 355–394. [Google Scholar]
- 12.Zou B, Zhou X, Lai S, Liu J. Notch signaling and non-small cell lung cancer (Review) Oncol Lett. 2018;15(3):3415–3421. doi: 10.3892/ol.2018.7738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brzozowa-Zasada M, Piecuch A, Dittfeld A, Mielańczyk Ł, Michalski M, Wyrobiec G, et al. Notch signalling pathway as an oncogenic factor involved in cancer development. Contemp Oncol (Poznan, Poland) 2016;20(4):267–272. doi: 10.5114/wo.2016.61845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghorbaninejad M, Heydari R, Mohammadi P, Shahrokh S, Haghazali M, Khanabadi B, et al. Contribution of NOTCH signaling pathway along with TNF-α in the intestinal inflammation of ulcerative colitis. Gastroenterol Hepatol from Bed to Bench. 2019;12(Suppl1):S80–S86. [PMC free article] [PubMed] [Google Scholar]
- 15.Radtke F, Clevers H. Self-renewal and cancer of the gut: two sides of a coin. Science (80-). 2005;307(5717):1904–1909. doi: 10.1126/science.1104815. [DOI] [PubMed] [Google Scholar]
- 16.Jackstadt R, van Hooff SR, Leach JD, Cortes-Lavaud X, Lohuis JO, Ridgway RA, et al. Epithelial NOTCH signaling rewires the tumor microenvironment of colorectal cancer to drive poor-prognosis subtypes and metastasis. Cancer Cell. 2019;36(3):319–336.e7. doi: 10.1016/j.ccell.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruland J. Colon cancer: epithelial notch signaling recruits neutrophils to drive metastasis. Cancer Cell. 2019;36(3):213–214. doi: 10.1016/j.ccell.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Li B, Ji ZZ, Zheng PS. Notch1 regulates the growth of human colon cancers. Cancer. 2010;116(22):5207–5218. doi: 10.1002/cncr.25449. [DOI] [PubMed] [Google Scholar]
- 19.Shaik JP, Alanazi IO, Pathan AAK, Parine NR, Almadi MA, Azzam NA, et al. Frequent activation of notch signaling pathway in colorectal cancers and its implication in patient survival outcome. Buyukhatipoglu H, editor. J Oncol 2020;2020:6768942. 10.1155/2020/6768942 [DOI] [PMC free article] [PubMed]
- 20.Chu D, Li Y, Wang W, Zhao Q, Li J, Lu Y, et al. High level of notch1 protein is associated with poor overall survival in colorectal cancer. Ann Surg Oncol. 2010;17(5):1337–1342. doi: 10.1245/s10434-009-0893-7. [DOI] [PubMed] [Google Scholar]
- 21.Wieland E, Rodriguez-Vita J, Liebler SS, Mogler C, Moll I, Herberich SE, et al. Endothelial notch1 activity facilitates metastasis. Cancer Cell. 2017;31(3):355–367. doi: 10.1016/j.ccell.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Fender AW, Nutter JM, Fitzgerald TL, Bertrand FE, Sigounas G. Notch-1 promotes stemness and epithelial to mesenchymal transition in colorectal cancer. J Cell Biochem. 2015;116(11):2517–2527. doi: 10.1002/jcb.25196. [DOI] [PubMed] [Google Scholar]
- 23.Sun L, Ke J, He Z, Chen Z, Huang Q, Ai W, et al. HES1 promotes colorectal cancer cell resistance to 5-Fu by inducing Of EMT and ABC transporter proteins. J Cancer. 2017;8(14):2802–2808. doi: 10.7150/jca.19142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jin Y, Wang M, Hu H, Huang Q, Chen Y, Wang G. Overcoming stemness and chemoresistance in colorectal cancer through miR-195–5p-modulated inhibition of notch signaling. Int J Biol Macromol. 2018;117:445–453. doi: 10.1016/j.ijbiomac.2018.05.151. [DOI] [PubMed] [Google Scholar]
- 25.Liu H, Yin Y, Hu Y, Feng Y, Bian Z, Yao S, et al. miR-139–5p sensitizes colorectal cancer cells to 5-fluorouracil by targeting NOTCH-1. Pathol Res Pract. 2016;212(7):643–649. doi: 10.1016/j.prp.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Zhao Q, Zhuang K, Han K, Tang H, Wang Y, Si W, et al. Silencing DVL3 defeats MTX resistance and attenuates stemness via Notch Signaling Pathway in colorectal cancer. Pathol Res Pract. 2020;216(8):152964. doi: 10.1016/j.prp.2020.152964. [DOI] [PubMed] [Google Scholar]
- 27.Huang S, Li C, Huang J, Luo P, Mo D, Wang H. LncRNA FEZF1-AS1 promotes non-small lung cancer cell migration and invasion through the up-regulation of NOTCH1 by serving as a sponge of miR-34a. BMC Pulm Med. 2020;20(1):110. doi: 10.1186/s12890-020-1154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang H, Li X, Wang W, Dong H. Long non-coding RNA SNHG3 promotes breast cancer cell proliferation and metastasis by binding to microRNA-154–3p and activating the notch signaling pathway. BMC Cancer. 2020;20(1):838. doi: 10.1186/s12885-020-07275-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang C, Wang L, Ding Y, Lu X, Zhang G, Yang J, et al. LncRNA structural characteristics in epigenetic regulation. Int J Mol Sci. 2017;18(12):2659. doi: 10.3390/ijms18122659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reicher A, Foßelteder J, Kwong LN, Pichler M. Crosstalk between the Notch signaling pathway and long non-coding RNAs. Cancer Lett. 2018;420:91–96. doi: 10.1016/j.canlet.2018.01.070. [DOI] [PubMed] [Google Scholar]
- 31.Trimarchi T, Bilal E, Ntziachristos P, Fabbri G, Dalla-Favera R, Tsirigos A, et al. Genome-wide mapping and characterization of notch-regulated long noncoding RNAs in acute leukemia. Cell. 2014;158(3):593–606. doi: 10.1016/j.cell.2014.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bian Z, Jin L, Zhang J, Yin Y, Quan C, Hu Y, et al. LncRNA - UCA1 enhances cell proliferation and 5-fluorouracil resistance in colorectal cancer by inhibiting MIR-204-5p. Sci Rep. 2016;6(March):1–12. doi: 10.1038/srep23892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luo J, Qu J, Wu D-K, Lu Z-L, Sun Y-S, Qu Q. Long non-coding RNAs: a rising biotarget in colorectal cancer. Oncotarget. 2017;8(13):22187–22202. doi: 10.18632/oncotarget.14728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhu Y, Li B, Liu Z, Jiang L, Wang G, Lv M, et al. Up-regulation of lncRNA SNHG1 indicates poor prognosis and promotes cell proliferation and metastasis of colorectal cancer by activation of the Wnt/β-catenin signaling pathway. Oncotarget. 2017;8(67):111715–111727. doi: 10.18632/oncotarget.22903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yao RW, Wang Y, Chen LL. Cellular functions of long noncoding RNAs. Nat Cell Biol. 2019;21(5):542–551. doi: 10.1038/s41556-019-0311-8. [DOI] [PubMed] [Google Scholar]
- 36.Mahmoud MM, Sanad EF, Hamdy NM. MicroRNAs’ role in the environment-related non-communicable diseases and link to multidrug resistance, regulation, or alteration. Environ Sci Pollut Res. 2021;28(28):36984–37000. doi: 10.1007/s11356-021-14550-w. [DOI] [PubMed] [Google Scholar]
- 37.Rinn JL, Chang HY. Genome regulation by long noncoding RNAs. Annu Rev Biochem. 2012;81(1):145–166. doi: 10.1146/annurev-biochem-051410-092902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernandes JCR, Acuña SM, Aoki JI, Floeter-Winter LM, Muxel SM. Long non-coding RNAs in the regulation of gene expression: Physiology and disease. Vol. 5, Non-coding RNA. 2019. p. 17. [DOI] [PMC free article] [PubMed]
- 39.Ulitsky I, Bartel DP. LincRNAs: genomics, evolution, and mechanisms. Cell. 2013;154(1):26. doi: 10.1016/j.cell.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karlsson O, Baccarelli AA. Environmental health and long non-coding RNAs. Curr Environ Heal Rep. 2016;3(3):178–187. doi: 10.1007/s40572-016-0092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okazaki Y, Furuno M, Kasukawa T, Adachi J, Bono H, Kondo S, et al. Analysis of the mouse transcriptome based on functional annotation of 60,770 full-length cDNAs. Nature. 2002;420(6915):563–573. doi: 10.1038/nature01266. [DOI] [PubMed] [Google Scholar]
- 42.Salviano-Silva A, Lobo-Alves SC, de Almeida RC, Malheiros D, Petzl-Erler ML. Besides pathology: long non-coding RNA in cell and tissue homeostasis. Non-coding RNA. 2018;4(1):3. doi: 10.3390/ncrna4010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khandelwal A, Bacolla A, Vasquez KM, Jain A. Long non-coding RNA: a new paradigm for lung cancer. Mol Carcinog. 2015;54(11):1235–1251. doi: 10.1002/mc.22362. [DOI] [PubMed] [Google Scholar]
- 44.Hermans-Beijnsberger S, van Bilsen M, Schroen B. Long non-coding RNAs in the failing heart and vasculature. Non-coding RNA Res. 2018;3(3):118–130. doi: 10.1016/j.ncrna.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morlando M, Fatica A. Alteration of epigenetic regulation by long noncoding RNAs in cancer. Int J Mol Sci. 2018;19(2):570. doi: 10.3390/ijms19020570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Quinn JJ, Chang HY. Unique features of long non-coding RNA biogenesis and function. Nat Rev Genet. 2016;17(1):47–62. doi: 10.1038/nrg.2015.10. [DOI] [PubMed] [Google Scholar]
- 47.Dempsey JL, Cui JY. Long non-coding RNAs: A novel paradigm for toxicology. Toxicol Sci. 2017;155(1):3–21. doi: 10.1093/toxsci/kfw203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kawaji H, Severin J, Lizio M, Waterhouse A, Katayama S, Irvine KM, et al. The FANTOM web resource: from mammalian transcriptional landscape to its dynamic regulation. Genome Biol. 2009;10(4):R40. doi: 10.1186/gb-2009-10-4-r40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ziegler C, Kretz M. The more the Merrier-Complexity in long non-coding RNA loci. Vol. 8, Frontiers in endocrinology. 2017. p. 1–6. [DOI] [PMC free article] [PubMed]
- 50.Statello L, Guo CJ, Chen LL, Huarte M. Gene regulation by long non-coding RNAs and its biological functions. Nat Rev Mol Cell Biol. 2021;22(2):96–118. doi: 10.1038/s41580-020-00315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carlevaro-Fita J, Rahim A, Guigó R, Vardy LA, Johnson R. Cytoplasmic long noncoding RNAs are frequently bound to and degraded at ribosomes in human cells. RNA. 2016;22(6):867–882. doi: 10.1261/rna.053561.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dahariya S, Paddibhatla I, Kumar S, Raghuwanshi S, Pallepati A, Gutti RK. Long non-coding RNA: classification, biogenesis and functions in blood cells. Mol Immunol. 2019;112(May):82–92. doi: 10.1016/j.molimm.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 53.AbdelHamid SG, Refaat AA, Benjamin AM, Elmawardy LA, Elgendy LA, Manolly MM, et al. Deciphering epigenetic(s) role in modulating susceptibility to and severity of COVID-19 infection and/or outcome: a systematic rapid review. Environ Sci Pollut Res. 2021;28(39):54209–54221. doi: 10.1007/s11356-021-15588-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bhat SA, Ahmad SM, Mumtaz PT, Malik AA, Dar MA, Urwat U, et al. Long non-coding RNAs: mechanism of action and functional utility. Non-coding RNA Res. 2016;1(1):43–50. doi: 10.1016/j.ncrna.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fang Y, Fullwood MJ. Roles, functions, and mechanisms of long non-coding RNAs in cancer. Genom Proteom Bioinform. 2016;14(1):42–54. doi: 10.1016/j.gpb.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li X, Wu Z, Fu X, Han W. LncRNAs: Insights into their function and mechanics in underlying disorders. Mutat Res Rev Mutat Res. 2014;762:1–21. doi: 10.1016/j.mrrev.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 57.O’Brien SJ, Bishop C, Hallion J, Fiechter C, Scheurlen K, Paas M, et al. Long non-coding RNA (lncRNA) and epithelial-mesenchymal transition (EMT) in colorectal cancer: a systematic review. Cancer Biol Ther. 2020;21(9):769–781. doi: 10.1080/15384047.2020.1794239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mahmoud MM, Sanad EF, Elshimy RAA, Hamdy NM. Competitive endogenous role of the LINC00511/miR-185–3p axis and miR-301a-3p from liquid biopsy as molecular markers for breast cancer diagnosis. Front Oncol. 2021 doi: 10.3389/fonc.2021.749753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Andersson ER, Sandberg R, Lendahl U. Notch signaling: simplicity in design, versatility in function. Development. 2011;138(17):3593–3612. doi: 10.1242/dev.063610. [DOI] [PubMed] [Google Scholar]
- 60.Brou C, Logeat F, Gupta N, Bessia C, LeBail O, Doedens JR, et al. A novel proteolytic cleavage involved in notch signaling: the role of the disintegrin-metalloprotease TACE. Mol Cell. 2000;5(2):207–216. doi: 10.1016/s1097-2765(00)80417-7. [DOI] [PubMed] [Google Scholar]
- 61.Guruharsha KG, Kankel MW, Artavanis-Tsakonas S. The Notch signalling system: recent insights into the complexity of a conserved pathway. Nat Rev Genet. 2012;13(9):654–666. doi: 10.1038/nrg3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kopan R, Ilagan MXG. The canonical notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137(2):216–233. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schroeter EH, Kisslinger JA, Kopan R. Notch-1 signalling requires ligand-induced proteolytic release of intracellular domain. Nature. 1998;393(6683):382–386. doi: 10.1038/30756. [DOI] [PubMed] [Google Scholar]
- 64.Miele L. Notch signaling. Clin Cancer Res. 2006;12(4):1074–1079. doi: 10.1158/1078-0432.CCR-05-2570. [DOI] [PubMed] [Google Scholar]
- 65.Bray SJ. Notch signalling: a simple pathway becomes complex. Nat Rev Mol Cell Biol. 2006;7(9):678–689. doi: 10.1038/nrm2009. [DOI] [PubMed] [Google Scholar]
- 66.Sikandar SS, Pate KT, Anderson S, Dizon D, Edwards RA, Waterman ML, et al. NOTCH signaling is required for formation and self-renewal of tumor-initiating cells and for repression of secretory cell differentiation in colon cancer. Cancer Res. 2010;70(4):1469–1478. doi: 10.1158/0008-5472.CAN-09-2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li S, Zhao H, Li J, Zhang A, Wang H. Downregulation of long non-coding RNA LET predicts poor prognosis and increases Notch signaling in non-small cell lung cancer. Oncotarget. 2018;9(1):1156–1168. doi: 10.18632/oncotarget.23452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cai W, Wu B, Li Z, He P, Wang B, Cai A, et al. LncRNA NBR2 inhibits epithelial-mesenchymal transition by regulating Notch1 signaling in osteosarcoma cells. J Cell Biochem. 2019;120(2):2015–2027. doi: 10.1002/jcb.27508. [DOI] [PubMed] [Google Scholar]
- 69.Gao YP, Li Y, Li HJ, Zhao B. LncRNA NBR2 inhibits EMT progression by regulating Notch 1 pathway in NSCLC. Eur Rev Med Pharmacol Sci. 2019;23(18):7950–7958. doi: 10.26355/eurrev_201909_19011. [DOI] [PubMed] [Google Scholar]
- 70.Guo Q, Qian Z, Yan D, Li L, Huang L. LncRNA-MEG3 inhibits cell proliferation of endometrial carcinoma by repressing Notch signaling. Biomed Pharmacother. 2016;82:589–594. doi: 10.1016/j.biopha.2016.02.049. [DOI] [PubMed] [Google Scholar]
- 71.Li H, Wang Y. Long noncoding RNA (IncRNA) MIR22HG suppresses gastric cancer progression through attenuating NOTCH2 signaling. Med Sci Monit. 2019;25:656–665. doi: 10.12659/MSM.912813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jia M, Jiang L, Wang YD, Huang JZ, Yu M, Xue HZ. lincRNA-p21 inhibits invasion and metastasis of hepatocellular carcinoma through Notch signaling-induced epithelial–mesenchymal transition. Hepatol Res. 2016;46(11):1137–1144. doi: 10.1111/hepr.12659. [DOI] [PubMed] [Google Scholar]
- 73.Zhang H-F, Li W, Han Y-D. LINC00261 suppresses cell proliferation, invasion and Notch signaling pathway in hepatocellular carcinoma. Cancer Biomark. 2018;21:575–582. doi: 10.3233/CBM-170471. [DOI] [PubMed] [Google Scholar]
- 74.Xia P, Gu R, Zhang W, Sun YF. lncRNA CEBPA-AS1 overexpression inhibits proliferation and migration and stimulates apoptosis of OS cells via notch signaling. Mol Ther Nucleic Acids. 2020;6(19):1470–1481. doi: 10.1016/j.omtn.2019.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 75.Liu S, Mitra R, Zhao MM, Fan W, Eischen CM, Yin F, et al. The potential roles of long noncoding RNAs (lncRNA) in glioblastoma development. Mol Cancer Ther. 2016;15(12):2977–2986. doi: 10.1158/1535-7163.MCT-16-0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xu Z, Huang B, Zhang Q, He X, Wei H, Zhang D. NOTCH1 regulates the proliferation and migration of bladder cancer cells by cooperating with long non-coding RNA HCG18 and microRNA-34c-5p. J Cell Biochem. 2019;120(4):6596–6604. doi: 10.1002/jcb.27954. [DOI] [PubMed] [Google Scholar]
- 77.Ding X, Wang X, Lin M, Xing Y, Ge S, Jia R, et al. PAUPAR lncRNA suppresses tumourigenesis by H3K4 demethylation in uveal melanoma. FEBS Lett. 2016;590:1729–1738. doi: 10.1002/1873-3468.12220. [DOI] [PubMed] [Google Scholar]
- 78.Liu PJ, Pan YH, Wang DW, You D. Long non-coding RNA XIST promotes cell proliferation of pancreatic cancer through miR-137 and Notch1 pathway. Eur Rev Med Pharmacol Sci. 2020;24(23):12161–12170. doi: 10.26355/eurrev_202012_24005. [DOI] [PubMed] [Google Scholar]
- 79.Wang X, Zhang G, Cheng Z, Dai L, Jia L, Jing X, et al. Knockdown of LncRNA-XIST suppresses proliferation and TGF-β1-induced EMT in NSCLC through the Notch-1 pathway by regulation of miR-137. Genet Test Mol Biomarkers. 2018;22(6):333–342. doi: 10.1089/gtmb.2018.0026. [DOI] [PubMed] [Google Scholar]
- 80.Tang LX, Su SF, Wan Q, He P, Xhang Y, Cheng XM. Novel long non-coding RNA LBX2-AS1 indicates poor prognosis and promotes cell proliferation and metastasis through Notch signaling in non-small cell lung cancer. Eur Rev Med Pharmacol Sci. 2019;23(17):7419–7429. doi: 10.26355/eurrev_201909_18851. [DOI] [PubMed] [Google Scholar]
- 81.Zeng SG, Xie JH, Zeng QY, Dai SH, Wang Y, Wan XM, et al. lncRNA PVT1 promotes metastasis of non-small cell lung cancer through EZH2-mediated activation of Hippo/NOTCH1 signaling pathways. Cell J. 2021;23(1):21–31. doi: 10.22074/cellj.2021.7010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Deng Y, Zhang L, Luo R. LINC01783 facilitates cell proliferation, migration and invasion in non-small cell lung cancer by targeting miR-432-5p to activate the notch pathway. Cancer Cell Int. 2021;21(1):234. doi: 10.1186/s12935-021-01912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Piao HY, Guo S, Wang Y, Zhang J. Long noncoding RNA NALT1-induced gastric cancer invasion and metastasis via NOTCH signaling pathway. World J Gastroenterol. 2019;25(44):6508–6526. doi: 10.3748/wjg.v25.i44.6508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang Y, Wu P, Lin R, Rong L, Xue Y, Fang Y. LncRNA NALT interaction with NOTCH1 promoted cell proliferation in pediatric T cell acute lymphoblastic leukemia. Sci Rep. 2015;5(1):13749. doi: 10.1038/srep13749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu Z-Q, He W-F, Wu Y-J, Zhao S-L, Wang L, Ouyang Y-Y, et al. LncRNA SNHG1 promotes EMT process in gastric cancer cells through regulation of the miR-15b/DCLK1/Notch1 axis. BMC Gastroenterol. 2020;20(1):156. doi: 10.1186/s12876-020-01272-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhao X, Zhao Z. Linc01555 promotes proliferation, migration and invasion of gastric carcinoma cells by interacting with Notch signaling pathway. J BUON. 2020;25(2):1007–1012. [PubMed] [Google Scholar]
- 87.Li G, Zhang Z, Chen Z, Liu B, Wu H. LncRNA DLEU2 is activated by STAT1 and induces gastric cancer development via targeting miR-23b-3p/NOTCH2 axis and Notch signaling pathway. Life Sci. 2021;277(247):119419. doi: 10.1016/j.lfs.2021.119419. [DOI] [PubMed] [Google Scholar]
- 88.He M, Wang Y, Cai J, Xie Y, Tao C, Jiang Y, et al. LncRNA DLEU2 promotes cervical cancer cell proliferation by regulating cell cycle and NOTCH pathway. Exp Cell Res. 2021;402(1):112551. doi: 10.1016/j.yexcr.2021.112551. [DOI] [PubMed] [Google Scholar]
- 89.Eoh Jin K, Paek J, Kim Wun S, Kim Jung H, Lee Yeon H, Lee Kil S, et al. Long non-coding RNA, steroid receptor RNA activator (SRA), induces tumor proliferation and invasion through the NOTCH pathway in cervical cancer cell lines. Oncol Rep. 2017;38(6):3481–3488. doi: 10.3892/or.2017.6023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chen Y, Wu Q, Lin J, Wei J. DARS-AS1 accelerates the proliferation of cervical cancer cells via miR-628–5p/JAG1 axis to activate Notch pathway. Cancer Cell Int. 2020;20(1):535. doi: 10.1186/s12935-020-01592-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dong C, Liu S, Lv Y, Zhang C, Gao H, Tan L, et al. Long non-coding RNA HOTAIR regulates proliferation and invasion via activating Notch signalling pathway in retinoblastoma. J Biosci. 2016;41(4):677–687. doi: 10.1007/s12038-016-9636-7. [DOI] [PubMed] [Google Scholar]
- 92.Lee M, Kim HJ, Kim SW, Park SA, Chun KH, Cho NH, et al. The long non-coding RNA HOTAIR increases tumour growth and invasion in cervical cancer by targeting the Notch pathway. Oncotarget. 2016;7(28):44558–44571. doi: 10.18632/oncotarget.10065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cai H, Yao J, An Y, Chen X, Chen W, Wu D, et al. LncRNA HOTAIR acts a competing endogenous RNA to control the expression of notch3 via sponging miR-613 in pancreatic cancer. Oncotarget. 2017;8(20):32905–32917. doi: 10.18632/oncotarget.16462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gao Y, Luo X, Zhang J. LincRNA-ROR is activated by H3K27 acetylation and induces EMT in retinoblastoma by acting as a sponge of miR-32 to activate the Notch signaling pathway. Cancer Gene Ther. 2021;28(12):42–54. doi: 10.1038/s41417-020-0181-z. [DOI] [PubMed] [Google Scholar]
- 95.Zeng SY, Liu CQ, Zhuang Y, Chen Y, Gu LL, Shi SQ. LncRNA ROR promotes proliferation of endometrial cancer cells via regulating Notch1 pathway. Eur Rev Med Pharmacol Sci. 2020;24(11):5970–5978. doi: 10.26355/eurrev_202006_21490. [DOI] [PubMed] [Google Scholar]
- 96.Zhu Y, Tong Y, Wu J, Liu Y, Zhao M. Knockdown of LncRNA GHET1 suppresses prostate cancer cell proliferation by inhibiting HIF-1α/Notch-1 signaling pathway via KLF2. BioFactors. 2019;45(3):364–373. doi: 10.1002/biof.1486. [DOI] [PubMed] [Google Scholar]
- 97.Zhu LF, Song LD, Xu Q, Zhan JF. Highly expressed long non-coding RNA FEZF1-AS1 promotes cells proliferation and metastasis through Notch signaling in prostate cancer. Vol. 23, European review for medical and pharmacological sciences. 2019. p. 5122–32. [DOI] [PubMed]
- 98.Luo L, Zhang Y, He H, Chen C, Zhang B, Cai M. LncRNA FEZF1-AS1 sponges miR-34a to upregulate Notch-1 in glioblastoma. Cancer Manag Res. 2020;12:1827–1833. doi: 10.2147/CMAR.S240531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ma Y, Fan B, Ren Z, Liu B, Wang Y. Long noncoding RNA DANCR contributes to docetaxel resistance in prostate cancer through targeting the miR-34a-5p/JAG1 pathway. Onco Targets Ther. 2019;12:5485–5497. doi: 10.2147/OTT.S197009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hu G, Wu L, Kuang W, Chen Y, Zhu X, Guo H, et al. Knockdown of linc-OIP5 inhibits proliferation and migration of glioma cells through down-regulation of YAP-NOTCH signaling pathway. Gene. 2017;610:24–31. doi: 10.1016/j.gene.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 101.Zhu Q, Li J, Wu Q, Cheng Y, Zheng H, Zhan T, et al. Linc—OIP5 in the breast cancer cells regulates angiogenesis of human umbilical vein endothelial cells through YAP1 / Notch / NRP1 signaling circuit at a tumor microenvironment. Biol Res. 2020;53(1):1–12. doi: 10.1186/s40659-020-0273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gao K, Ji Z, She K, Yang Q, Shao L. Long non-coding RNA ZFAS1 is an unfavourable prognostic factor and promotes glioma cell progression by activation of the Notch signaling pathway. Biomed Pharmacother. 2017;87:555–560. doi: 10.1016/j.biopha.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 103.Wu J, Wang N, Yang Y, Jiang G, Zhan H, Li F. LINC01152 upregulates MAML2 expression to modulate the progression of glioblastoma multiforme via Notch signaling pathway. Cell Death Dis. 2021;12(1):115. doi: 10.1038/s41419-020-03163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wang X, Yan Y, Zhang C, Wei W, Ai X, Pang Y, et al. Upregulation of lncRNA PlncRNA-1 indicates the poor prognosis and promotes glioma progression by activation of Notch signal pathway. Biomed Pharmacother. 2018;103(5):216–221. doi: 10.1016/j.biopha.2018.03.150. [DOI] [PubMed] [Google Scholar]
- 105.Zhao X, Shen F, Yang B. LncRNA LINC01410 induced by MYC accelerates glioma progression via sponging miR-506–3p and modulating NOTCH2 expression to motivate Notch signaling pathway. Cell Mol Neurobiol. 2021 doi: 10.1007/s10571-021-01042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sun X, Huang T, Liu Z, Sun M, Luo S. LncRNA SNHG7 contributes to tumorigenesis and progression in breast cancer by interacting with miR-34a through EMT initiation and the Notch-1 pathway. Eur J Pharmacol. 2019;856(January):172407. doi: 10.1016/j.ejphar.2019.172407. [DOI] [PubMed] [Google Scholar]
- 107.Zhou S, Yu L, Xiong M, Dai G. Biochemical and biophysical research communications LncRNA SNHG12 promotes tumorigenesis and metastasis in osteosarcoma by upregulating Notch2 by sponging miR-195–5p. Biochem Biophys Res Commun. 2018;495(2):1822–1832. doi: 10.1016/j.bbrc.2017.12.047. [DOI] [PubMed] [Google Scholar]
- 108.Liu Z-B, Tang C, Jin X, Liu S-H, Pi W. Increased expression of lncRNA SNHG12 predicts a poor prognosis of nasopharyngeal carcinoma and regulates cell proliferation and metastasis by modulating Notch signal pathway. Cancer Biomark. 2018;23:603–613. doi: 10.3233/CBM-181873. [DOI] [PubMed] [Google Scholar]
- 109.Li Z, Tang Y, Xing W, Dong W, Wang Z. LncRNA, CRNDE promotes osteosarcoma cell proliferation, invasion and migration by regulating Notch1 signaling and epithelial-mesenchymal transition. Exp Mol Pathol. 2018;104(1):19–25. doi: 10.1016/j.yexmp.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 110.Huang R, Nie W, Yao K, Chou J. Depletion of the lncRNA RP11-567G11.1 inhibits pancreatic cancer progression. Biomed Pharmacother. 2019;112(138):108685. doi: 10.1016/j.biopha.2019.108685. [DOI] [PubMed] [Google Scholar]
- 111.Liu S, Liu WH, Diao ZL, Zhang AH, Guo W, Han X, et al. LncRNA RP11-567G11.1 accelerates the proliferation and invasion of renal cell carcinoma through activating the Notch pathway. Eur Rev Med Pharmacol Sci. 2020;24(9):4738–4744. doi: 10.26355/eurrev_202005_21162. [DOI] [PubMed] [Google Scholar]
- 112.Xu J, Xu W, Yang X, Liu Z, Sun Q. LncRNA HCG11/miR-579–3p/MDM2 axis modulates malignant biological properties in pancreatic carcinoma via Notch/Hes1 signaling pathway. Aging (Albany NY) 2021;13(12):16471–16484. doi: 10.18632/aging.203167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chen H, Liu JZ, Hu GJ, Shi LL, Lan T. Promotion of proliferation and metastasis of hepatocellular carcinoma by LncRNA00673 based on the targeted-regulation of notch signaling pathway. Eur Rev Med Pharmacol Sci. 2017;21(15):3412–3420. [PubMed] [Google Scholar]
- 114.Zhang TH, Liang LZ, Liu XL, Wu JN, Su K, Chen JY, et al. LncRNA UCA1/miR-124 axis modulates TGFβ1-induced epithelial-mesenchymal transition and invasion of tongue cancer cells through JAG1/Notch signaling. J Cell Biochem. 2019;120(6):10495–10504. doi: 10.1002/jcb.28334. [DOI] [PubMed] [Google Scholar]
- 115.Bai L, Wang A, Zhang Y, Xu X, Zhang X. Knockdown of MALAT1 enhances chemosensitivity of ovarian cancer cells to cisplatin through inhibiting the Notch1 signaling pathway. Exp Cell Res. 2018;366(2):161–171. doi: 10.1016/j.yexcr.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 116.Zhao J, Liu HR. Down-regulation of long noncoding RNA DLX6-AS1 defines good prognosis and inhibits proliferation and metastasis in human epithelial ovarian cancer cells via Notch signaling pathway. Eur Rev Med Pharmacol Sci. 2019;23(8):3243–3252. doi: 10.26355/eurrev_201904_17684. [DOI] [PubMed] [Google Scholar]
- 117.Rani N, Nowakowski TJ, Zhou H, Godshalk SE, Lisi V, Kriegstein AR, et al. A primate lncRNA mediates Notch signaling during neuronal development by sequestering miRNA. Neuron. 2016;90(6):1174–1188. doi: 10.1016/j.neuron.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liu Z, Li H, Fan S, Lin H, Lian W. STAT3-induced upregulation of long noncoding RNA HNF1A-AS1 promotes the progression of oral squamous cell carcinoma via activating Notch signaling pathway. Cancer Biol Ther. 2019;20(4):444–453. doi: 10.1080/15384047.2018.1529119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ye Y, Song Y, Zhuang J, He S, Ni J, Xia W. Long noncoding RNA CCAL promotes papillary thyroid cancer progression by activation of NOTCH1 pathway. Oncol Res. 2018;26(9):1383–1390. doi: 10.3727/096504018X15188340975709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhang M, Han Y, Zheng Y, Zhang Y, Zhao X, Gao Z, et al. ZEB1-activated LINC01123 accelerates the malignancy in lung adenocarcinoma through NOTCH signaling pathway. Cell Death Dis. 2020;11(11):981. doi: 10.1038/s41419-020-03166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cai B, Zheng Y, Ma S, Xing Q, Wang X, Yang B, et al. BANCR contributes to the growth and invasion of melanoma by functioning as a competing endogenous RNA to upregulate Notch2 expression by sponging miR-204. Int J Oncol. 2017;51(6):1941–1951. doi: 10.3892/ijo.2017.4173. [DOI] [PubMed] [Google Scholar]
- 122.Wang Y, Li M, Dong C, Ma Y, Xiao L, Zuo S, et al. Linc00152 knockdown inactivates the Akt / mTOR and Notch1 pathways to exert its anti-hemangioma effect. Life Sci. 2019;223(February):22–28. doi: 10.1016/j.lfs.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 123.Ma Q, Dai X, Lu W, Qu X, Liu N, Zhu C. Biochemical and Biophysical Research Communications Silencing long non-coding RNA MEG8 inhibits the proliferation and induces the ferroptosis of hemangioma endothelial cells by regulating miR-497–5p / NOTCH2 axis. Biochem Biophys Res Commun. 2021;556:72–78. doi: 10.1016/j.bbrc.2021.03.132. [DOI] [PubMed] [Google Scholar]
- 124.Wu Q, Lu S, Zhang L, Zhao L. LncRNA HOXA-AS2 activates the notch pathway to promote cervical cancer cell proliferation and migration. Reprod Sci. 2021;28(10):3000–3009. doi: 10.1007/s43032-021-00626-y. [DOI] [PubMed] [Google Scholar]
- 125.Yang X, Duan B, Zhou X. Long non-coding RNA FOXD2-AS1 functions as a tumor promoter in colorectal cancer by regulating EMT and Notch signaling pathway. Eur Rev Med Pharmacol Sci. 2017;21(16):3586–3591. [PubMed] [Google Scholar]
- 126.Lu S, Dong W, Zhao P, Liu Z. LncRNA FAM83H-AS1 is associated with the prognosis of colorectal carcinoma and promotes cell proliferation by targeting the notch signaling pathway. Oncol Lett. 2018;15(2):1861–1868. doi: 10.3892/ol.2017.7520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bian Z, Zhang J, Li M, Feng Y, Yao S, Song M, et al. Long non-coding RNA LINC00152 promotes cell proliferation, metastasis, and confers 5-FU resistance in colorectal cancer by inhibiting miR-139-5p. Oncogenesis. 2017;6(11):395. doi: 10.1038/s41389-017-0008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Xu J, Wu G, Zhao Y, Han Y, Zhang S, Li C, et al. Long noncoding RNA DSCAM-AS1 facilitates colorectal cancer cell proliferation and migration via miR-137/notch1 axis. J Cancer. 2020;11(22):6623–6632. doi: 10.7150/jca.46562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.D’Abbronzo G, Franco R. LINC01198 promotes colorectal cancer cell proliferation and inhibits apoptosis via notch signaling pathway. Eur Rev Med Pharmacol Sci. 2020;24(19):9776–9777. doi: 10.26355/eurrev_202010_23182. [DOI] [PubMed] [Google Scholar]
- 130.Zhu H, He G, Wang Y, Hu Y, Zhang Z, Qian X, et al. Long intergenic noncoding RNA 00707 promotes colorectal cancer cell proliferation and metastasis by sponging miR-206. Onco Targets Ther. 2019;12:4331–4340. doi: 10.2147/OTT.S198140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lao Y, Li Q, Li N, Liu H, Liu K, Jiang G, et al. Long noncoding RNA ENST00000455974 plays an oncogenic role through up-regulating JAG2 in human DNA mismatch repair-proficient colon cancer. Biochem Biophys Res Commun. 2019;508(2):339–347. doi: 10.1016/j.bbrc.2018.11.088. [DOI] [PubMed] [Google Scholar]
- 132.Zhang Y, Zheng L, Lao X, Wen M, Qian Z, Liu X, et al. Hes1 is associated with long non-coding RNAs in colorectal cancer. Ann Transl Med. 2019;7(18):459. doi: 10.21037/atm.2019.08.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang L, Bu P, Ai Y, Srinivasan T, Chen HJ, Xiang K, et al. A long non-coding RNA targets microRNA miR-34a to regulate colon cancer stem cell asymmetric division. Green MR, editor. Elife 2016;5:e14620. 10.7554/eLife.14620 [DOI] [PMC free article] [PubMed]
- 134.Bu P, Chen KY, Chen JH, Wang L, Walters J, Shin YJ, et al. A microRNA miR-34a-regulated bimodal switch targets notch in colon cancer stem cells. Cell Stem Cell. 2013;12(5):602–615. doi: 10.1016/j.stem.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chen DL, Lu YX, Zhang JX, Wei XL, Wang F, Zeng ZL, et al. Long non-coding RNA UICLM promotes colorectal cancer liver metastasis by acting as a ceRNA for microRNA-215 to regulate ZEB2 expression. Theranostics. 2017;7(19):4836–4849. doi: 10.7150/thno.20942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ye Z, Duan J, Wang L, Ji Y, Qiao B. LncRNA-LET inhibits cell growth of clear cell renal cell carcinoma by regulating miR-373-3p. Cancer Cell Int. 2019;19(1):311. doi: 10.1186/s12935-019-1008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Auriol E, Billard L-M, Magdinier F, Dante R. Specific binding of the methyl binding domain protein 2 at the BRCA1-NBR2 locus. Nucleic Acids Res. 2005;33(13):4243–4254. doi: 10.1093/nar/gki729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Jia H-Y, Zhang K, Lu W-J, Xu G-W, Zhang J-F, Tang Z-L. LncRNA MEG3 influences the proliferation and apoptosis of psoriasis epidermal cells by targeting miR-21/caspase-8. BMC Mol cell Biol. 2019;20(1):46. doi: 10.1186/s12860-019-0229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhang D-Y, Zou X-J, Cao C-H, Zhang T, Lei L, Qi X-L, et al. Identification and functional characterization of long non-coding RNA MIR22HG as a tumor suppressor for hepatocellular carcinoma. Theranostics. 2018;8(14):3751–3765. doi: 10.7150/thno.22493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hall JR, Messenger ZJ, Tam HW, Phillips SL, Recio L, Smart RC. Long noncoding RNA lincRNA-p21 is the major mediator of UVB-induced and p53-dependent apoptosis in keratinocytes. Cell Death Dis. 2015;6(3):e1700. doi: 10.1038/cddis.2015.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Szmajda D, Krygier A, Jamroziak K, Żebrowska-Nawrocka M, Balcerczak E. Expression level of CEBPA gene in acute lymphoblastic leukemia individuals. Sci Rep. 2019;9(1):15640. doi: 10.1038/s41598-019-52104-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ke D, Li H, Zhang Y, An Y, Fu H, Fang X, et al. The combination of circulating long noncoding RNAs AK001058, INHBA-AS1, MIR4435-2HG, and CEBPA-AS1 fragments in plasma serve as diagnostic markers for gastric cancer. Oncotarget 2017;8(13):21516–25. https://www.oncotarget.com/article/15628/text/ [DOI] [PMC free article] [PubMed]
- 143.Lai CH, Chen AT, Burns AB, Sriram K, Luo Y, Tang X, et al. RAMP2-AS1 regulates endothelial homeostasis and aging. Front Cell Dev. 2021 doi: 10.3389/fcell.2021.635307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Vance KW, Sansom SN, Lee S, Chalei V, Kong L, Cooper SE, et al. The long non-coding RNA paupar regulates the expression of both local and distal genes. EMBO J. 2014;33(4):296–311. doi: 10.1002/embj.201386225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Cerase A, Pintacuda G, Tattermusch A, Avner P. Xist localization and function: new insights from multiple levels. Genome Biol. 2015;16(1):166. doi: 10.1186/s13059-015-0733-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Huang X, Yang Y, Yang C, Li H, Cheng H, Zheng Y. Overexpression of LBX2 associated with tumor progression and poor prognosis in colorectal cancer. Oncol Lett. 2020;19(6):3751–3760. doi: 10.3892/ol.2020.11489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ma Y-N, Hong Y-G, Yu G-Y, Jiang S, Zhao B, Guo A, et al. LncRNA LBX2-AS1 promotes colorectal cancer progression and 5-fluorouracil resistance. Cancer Cell Int. 2021;21(1):501. doi: 10.1186/s12935-021-02209-y. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 148.Lu D, Luo P, Wang Q, Ye Y, Wang B. lncRNA PVT1 in cancer: a review and meta-analysis. Clin Chim Acta. 2017;474:1–7. doi: 10.1016/j.cca.2017.08.038. [DOI] [PubMed] [Google Scholar]
- 149.Thin KZ, Tu JC, Raveendran S. Long non-coding SNHG1 in cancer. Clin Chim Acta. 2019;494:38–47. doi: 10.1016/j.cca.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 150.Ghafouri-Fard S, Dashti S, Farsi M, Taheri M. Deleted in lymphocytic leukemia 2 (DLEU2): an lncRNA with dissimilar roles in different cancers. Biomed Pharmacother. 2021;133:111093. doi: 10.1016/j.biopha.2020.111093. [DOI] [PubMed] [Google Scholar]
- 151.Yan R, Wang K, Peng R, Wang S, Cao J, Wang P, et al. Genetic variants in lncRNA SRA and risk of breast cancer. Oncotarget. 2016;7(16):22486–22496. doi: 10.18632/oncotarget.7995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Jiao M, Guo H, Chen Y, Li L, Zhang L. DARS-AS1 promotes clear cell renal cell carcinoma by sequestering miR-194–5p to up-regulate DARS. Biomed Pharmacother. 2020;128:110323. doi: 10.1016/j.biopha.2020.110323. [DOI] [PubMed] [Google Scholar]
- 153.Rinn JL, Kertesz M, Wang JK, Squazzo SL, Xu X, Brugmann SA, et al. Functional demarcation of active and silent chromatin domains in human HOX loci by noncoding RNAs. Cell. 2007;129(7):1311–1323. doi: 10.1016/j.cell.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Woo CJ, Kingston RE. HOTAIR lifts noncoding RNAs to new levels. Cell. 2007;129(7):1257–1259. doi: 10.1016/j.cell.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 155.Pan Y, Li C, Chen J, Zhang K, Chu X, Wang R, et al. The emerging roles of long noncoding RNA ROR (lincRNA-ROR) and its possible mechanisms in human cancers. Cell Physiol Biochem. 2016;40(1–2):219–229. doi: 10.1159/000452539. [DOI] [PubMed] [Google Scholar]
- 156.Jiang YF, Zhang HY, Ke J, Shen H, Ou HB, Liu Y. Overexpression of LncRNA GHET1 predicts an unfavourable survival and clinical parameters of patients in various cancers. J Cell Mol Med. 2019;23(8):4891–4899. doi: 10.1111/jcmm.14486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Shi C, Sun L, Song Y. FEZF1-AS1: a novel vital oncogenic lncRNA in multiple human malignancies. Biosci Rep. 2019;39(6):BSR20191202. doi: 10.1042/BSR20191202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jin SJ, Jin MZ, Xia BR, Jin WL. Long non-coding RNA DANCR as an emerging therapeutic target in human cancers. Front Oncol. 2019;9:1225. doi: 10.3389/fonc.2019.01225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Ulitsky I, Shkumatava A, Jan CH, Sive H, Bartel DP. Conserved function of lincRNAs in vertebrate embryonic development despite rapid sequence evolution. Cell. 2011;147(7):1537–1550. doi: 10.1016/j.cell.2011.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Askarian-Amiri ME, Crawford J, French JD, Smart CE, Smith MA, Clark MB, et al. SNORD-host RNA Zfas1 is a regulator of mammary development and a potential marker for breast cancer. RNA. 2011;17(5):878–891. doi: 10.1261/rna.2528811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Cui Z, Ren S, Lu J, Wang F, Xu W, Sun Y, et al. The prostate cancer-up-regulated long noncoding RNA PlncRNA-1 modulates apoptosis and proliferation through reciprocal regulation of androgen receptor. Urol Oncol Semin Orig Investig. 2013;31(7):1117–1123. doi: 10.1016/j.urolonc.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 162.Ellis BC, Molloy PL, Graham LD. CRNDE: A long non-coding RNA involved in cancer neurobiology, and development. Front Genet. 2012;3:1–15. doi: 10.3389/fgene.2012.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wang X-S, Zhang Z, Wang H-C, Cai J-L, Xu Q-W, Li M-Q, et al. Rapid Identification of UCA1 as a very sensitive and specific unique marker for human bladder carcinoma. Clin Cancer Res. 2006;12(16):4851–4858. doi: 10.1158/1078-0432.CCR-06-0134. [DOI] [PubMed] [Google Scholar]
- 164.Ji P, Diederichs S, Wang W, Böing S, Metzger R, Schneider PM, et al. MALAT-1, a novel noncoding RNA, and thymosin β4 predict metastasis and survival in early-stage non-small cell lung cancer. Oncogene. 2003;22(39):8031–8041. doi: 10.1038/sj.onc.1206928. [DOI] [PubMed] [Google Scholar]
- 165.Alizadeh A, Jebelli A, Baradaran B, Amini M, Oroojalian F, Hashemzaei M, et al. Crosstalk between long non-coding RNA DLX6-AS1, microRNAs and signaling pathways: a pivotal molecular mechanism in human cancers. Gene. 2021;769:145224. doi: 10.1016/j.gene.2020.145224. [DOI] [PubMed] [Google Scholar]
- 166.Wu Y, Liu H, Shi X, Yao Y, Yang W, Song Y. The long non-coding RNA HNF1A-AS1 regulates proliferation and metastasis in lung adenocarcinoma. Oncotarget. 2015;6(11):9160–9172. doi: 10.18632/oncotarget.3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Deng X, Ruan H, Zhang X, Xu X, Zhu Y, Peng H, et al. Long noncoding RNA CCAL transferred from fibroblasts by exosomes promotes chemoresistance of colorectal cancer cells. Int J Cancer. 2020;146(6):1700–1716. doi: 10.1002/ijc.32608. [DOI] [PubMed] [Google Scholar]
- 168.Zhou T, Gao Y. Increased expression of LncRNA BANCR and its prognostic significance in human hepatocellular carcinoma. World J Surg Oncol. 2016;14(1):8. doi: 10.1186/s12957-015-0757-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wang J, Su Z, Lu S, Fu W, Liu Z, Jiang X, et al. LncRNA HOXA-AS2 and its molecular mechanisms in human cancer. Clin Chim Acta. 2018;485:229–233. doi: 10.1016/j.cca.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 170.Tariq K, Ghias K. Colorectal cancer carcinogenesis: a review of mechanisms. Cancer Biol Med. 2016;13(1):120–135. doi: 10.28092/j.issn.2095-3941.2015.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lizarbe MA, Calle-Espinosa J, Fernández-Lizarbe E, Fernández-Lizarbe S, Robles MÁ, Olmo N, et al. Colorectal cancer: from the genetic model to posttranscriptional regulation by noncoding RNAs. Linnebacher M, editor. Biomed Res Int 2017;2017:7354260. 10.1155/2017/7354260 [DOI] [PMC free article] [PubMed]
- 172.Malki A, Elruz RA, Gupta I, Allouch A, Vranic S, Al Moustafa AE. Molecular mechanisms of colon cancer progression and metastasis: recent insights and advancements. Int J Mol Sci. 2021;22:1–24. doi: 10.3390/ijms22010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Arends MJ. Pathways of colorectal carcinogenesis. Appl Immunohistochem Mol Morphol 2013;21(2):97–102. https://journals.lww.com/appliedimmunohist/Fulltext/2013/03000/Pathways_of_Colorectal_Carcinogenesis.1.aspx [DOI] [PubMed]
- 174.Cooks T, Pateras IS, Tarcic O, Solomon H, Schetter AJ, Wilder S, et al. Mutant p53 prolongs NF-κB activation and promotes chronic inflammation and inflammation-associated colorectal cancer. Cancer Cell. 2013;23(5):634–646. doi: 10.1016/j.ccr.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Chu D, Zhou Y, Zhang Z, Li Y, Li J, Zheng J, et al. Notch1 expression, which is related to p65 status, is an independent predictor of prognosis in colorectal cancer. Clin Cancer Res. 2011;17(17):5686–5694. doi: 10.1158/1078-0432.CCR-10-3196. [DOI] [PubMed] [Google Scholar]
- 176.Nakayama M, Oshima M. Mutant p53 in colon cancer. J Mol Cell Biol. 2019;11(4):267–276. doi: 10.1093/jmcb/mjy075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Mathern DR, Laitman LE, Hovhannisyan Z, Dunkin D, Farsio S, Malik TJ, et al. Mouse and human Notch-1 regulate mucosal immune responses. Mucosal Immunol. 2014;7(4):995–1005. doi: 10.1038/mi.2013.118. [DOI] [PubMed] [Google Scholar]
- 178.Meurette O, Mehlen P. Notch signaling in the tumor microenvironment. Cancer Cell. 2018;34(4):536–548. doi: 10.1016/j.ccell.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 179.Li D, Masiero M, Banham AH, Harris AL. The notch ligand jagged1 as a target for anti-tumor therapy. Front Oncol. 2014 doi: 10.3389/fonc.2014.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Gopisetty A, Bhattacharya P, Haddad C, Bruno JC, Vasu C, Miele L, et al. OX40L/Jagged1 cosignaling by GM-CSF–induced bone marrow-derived dendritic cells is required for the expansion of functional regulatory T cells. J Immunol. 2013;190(11):5516–5525. doi: 10.4049/jimmunol.1202298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Bugeon L, Gardner LM, Rose A, Gentle M, Dallman MJ. Cutting edge: Notch signaling induces a distinct cytokine profile in dendritic cells that supports T cell-mediated regulation and IL-2-dependent IL-17 production. J Immunol. 2008;181(12):8189–8193. doi: 10.4049/jimmunol.181.12.8189. [DOI] [PubMed] [Google Scholar]
- 182.Yu W, Wang Y, Guo P. Notch signaling pathway dampens tumor-infiltrating CD8+ T cells activity in patients with colorectal carcinoma. Biomed Pharmacother. 2018;97:535–542. doi: 10.1016/j.biopha.2017.10.143. [DOI] [PubMed] [Google Scholar]
- 183.Wang F, Long J, Li L, Zhao Z, Wei F, Yao Y, et al. Mutations in the notch signalling pathway are associated with enhanced anti-tumour immunity in colorectal cancer. J Cell Mol Med. 2020;24(20):12176–12187. doi: 10.1111/jcmm.15867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kamal AM, Wasfey EF, Elghamry WR, Sabry OM, Elghobary HA, Radwan SM. Genetic signature of CTLA-4, BTLA, TIM-3 and LAG-3 molecular expression in colorectal cancer patients: Implications in diagnosis and survival outcomes. Clin Biochem. 2021;96:13–18. doi: 10.1016/j.clinbiochem.2021.06.007. [DOI] [PubMed] [Google Scholar]
- 185.Caiado F, Carvalho T, Rosa I, Remédio L, Costa A, Matos J, et al. Bone marrow-derived CD11b+ Jagged2+ cells promote epithelial-to-mesenchymal transition and metastasization in colorectal cancer. Cancer Res. 2013;73(14):4233–4246. doi: 10.1158/0008-5472.CAN-13-0085. [DOI] [PubMed] [Google Scholar]
- 186.Gao F, Huang W, Zhang YQ, Tang SH, Zheng L, Ma F, et al. Hes1 promotes cell proliferation and migration by activating Bmi-1 and PTEN/Akt/GSK3ß pathway in human colon cancer. Oncotarget. 2015;6(36):38667–38680. doi: 10.18632/oncotarget.5484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Gao F, Zhang Y, Wang S, Liu Y, Zheng L, Yang J, et al. Hes1 is involved in the self-renewal and tumourigenicity of stem-like cancer cells in colon cancer. Sci Rep. 2014;4(1):3963. doi: 10.1038/srep03963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Zhang Z, Li G, Qiu H, Yang J, Bu X, Zhu S, et al. The novel notch-induced long noncoding RNA LUNAR1 determines the proliferation and prognosis of colorectal cancer. Sci Rep. 2019;9(1):1–9. doi: 10.1038/s41598-019-56536-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Qian J, Garg A, Li F, Shen Q, Xiao K. LncRNA LUNAR1 accelerates colorectal cancer progression by targeting the miR-495-3p/MYCBP axis. Int J Oncol. 2020;57(5):1157–1168. doi: 10.3892/ijo.2020.5128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Zhang M, Jiang X, Jiang S, Guo Z, Zhou Q, He J. LncRNA FOXD2-AS1 regulates miR-25-3p/sema4c axis to promote the invasion and migration of colorectal cancer cells. Cancer Manag Res. 2019;11:10633–10639. doi: 10.2147/CMAR.S228628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Zhu Y, Qiao L, Zhou Y, Ma N, Wang C, Zhou J. Long non-coding RNA FOXD2-AS1 contributes to colorectal cancer proliferation through its interaction with microRNA-185-5p. Cancer Sci. 2018;109(7):2235–2242. doi: 10.1111/cas.13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Yang L, Cui J, Wang Y, Tan J. FAM83H-AS1 is upregulated and predicts poor prognosis in colon cancer. Biomed Pharmacother. 2019;118(August):109342. doi: 10.1016/j.biopha.2019.109342. [DOI] [PubMed] [Google Scholar]
- 193.Zhang J, Yin M, Huang J, Lv Z, Liang S, Miao X, et al. Long noncoding RNA LINC00152 as a novel predictor of lymph node metastasis and survival in human cancer: a systematic review and meta-analysis. Clin Chim Acta. 2018;483(March):25–32. doi: 10.1016/j.cca.2018.03.034. [DOI] [PubMed] [Google Scholar]
- 194.Yue B, Cai D, Liu C, Fang C, Yan D. Linc00152 functions as a competing endogenous RNA to confer oxaliplatin resistance and holds prognostic values in colon cancer. Mol Ther. 2016;24(12):2064–2077. doi: 10.1038/mt.2016.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Li B, Sun H, Zhang J. LncRNA DSCAM-AS1 promotes colorectal cancer progression by acting as a molecular sponge of miR-384 to modulate AKT3 expression. Aging (Albany NY) 2020;12(10):9781–9792. doi: 10.18632/aging.103243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wang H, Luan H, Zhan T, Liu X, Song J, Dai H. Long non-coding RNA LINC00707 acts as a competing endogenous RNA to enhance cell proliferation in colorectal cancer. Exp Ther Med. 2020;19(2):1439–1447. doi: 10.3892/etm.2019.8350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Palko-Łabuz A, Środa-Pomianek K, Wesołowska O, Kostrzewa-Susłow E, Uryga A, Michalak K. MDR reversal and pro-apoptotic effects of statins and statins combined with flavonoids in colon cancer cells. Biomed Pharmacother. 2018;2019(109):1511–1522. doi: 10.1016/j.biopha.2018.10.169. [DOI] [PubMed] [Google Scholar]
- 198.Shao HJ, Li Q, Shi T, Zhang GZ, Shao F. LINC00707 promotes cell proliferation and invasion of colorectal cancer via miR-206/FMNL2 axis. Eur Rev Med Pharmacol Sci. 2019;23(9):3749–3759. doi: 10.26355/eurrev_201905_17801. [DOI] [PubMed] [Google Scholar]
- 199.Meng X, Fu R. MiR-206 regulates 5-FU resistance by targeting Bcl-2 in colon cancer cells. Onco Targets Ther. 2018;11:1757–1765. doi: 10.2147/OTT.S159093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Xie T, Li Y, Li S-L, Luo H-F. Astragaloside IV enhances cisplatin chemosensitivity in human colorectal cancer via regulating NOTCH3. Oncol Res. 2016;24(6):447–453. doi: 10.3727/096504016X14685034103590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Yao J, Qian CJ. Notch3 siRNA enhances chemosensitivity of colon cancer cells to topotecan. Chin J Cancer Biother. 2009;16(6):604–608. [Google Scholar]
- 202.Ma Y, Bu D, Long J, Chai W, Dong J. LncRNA DSCAM-AS1 acts as a sponge of miR-137 to enhance Tamoxifen resistance in breast cancer. J Cell Physiol. 2019;234(3):2880–2894. doi: 10.1002/jcp.27105. [DOI] [PubMed] [Google Scholar]
- 203.Guo Y, Pang Y, Gao X, Zhao M, Zhang X, Zhang H, et al. MicroRNA-137 chemosensitizes colon cancer cells to the chemotherapeutic drug oxaliplatin (OXA) by targeting YBX1. Cancer Biomark. 2017;18:1–9. doi: 10.3233/CBM-160650. [DOI] [PubMed] [Google Scholar]
- 204.Li X, Zhao H, Zhou X, Song L. Inhibition of lactate dehydrogenase A by microRNA.34a resensitizes colon cancer cells to 5.fluorouracil. Mol Med Rep. 2015;11(1):577–582. doi: 10.3892/mmr.2014.2726. [DOI] [PubMed] [Google Scholar]
- 205.Vaish V, Kim J, Shim M. Jagged-2 (JAG2) enhances tumorigenicity and chemoresistance of colorectal cancer cells. Oncotarget. 2017;8(32):53262–53275. doi: 10.18632/oncotarget.18391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ferreira AC, Suriano G, Mendes N, Gomes B, Wen X, Carneiro F, et al. E-cadherin impairment increases cell survival through Notch-dependent upregulation of Bcl-2. Hum Mol Genet. 2012;21(2):334–343. doi: 10.1093/hmg/ddr469. [DOI] [PubMed] [Google Scholar]
- 207.Cho S, Lu M, He X, Ee PL-R, Bhat U, Schneider E, et al. Notch1 regulates the expression of the multidrug resistance gene ABCC1/MRP1 in cultured cancer cells. Proc Natl Acad Sci. 2011;108(51):20778–20783. doi: 10.1073/pnas.1019452108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Xu K, Shen K, Liang X, Li Y, Nagao N, Li J, et al. MiR-139-5p reverses CD44+/CD133+-associated multidrug resistance by downregulating NOTCH1 in colorectal carcinoma cells. Oncotarget. 2016;7(46):75118–75129. doi: 10.18632/oncotarget.12611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sodani K, Patel A, Kathawala RJ, Chen Z-S. Multidrug resistance associated proteins in multidrug resistance. Chin J Cancer. 2012;31(2):58–72. doi: 10.5732/cjc.011.10329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Liu N, Li J, Zhao Z, Han J, Jiang T, Chen Y, et al. MicroRNA-302a enhances 5-fluorouracil-induced cell death in human colon cancer cells. Oncol Rep. 2017;37(1):631–639. doi: 10.3892/or.2016.5237. [DOI] [PubMed] [Google Scholar]
- 211.Zheng Y-B, Luo H-P, Shi Q, Hao Z-N, Ding Y, Wang Q-S, et al. miR-132 inhibits colorectal cancer invasion and metastasis via directly targeting ZEB2. World J Gastroenterol. 2014;20(21):6515–6522. doi: 10.3748/wjg.v20.i21.6515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Sun ZF, Zhang Z, Liu Z, Qiu B, Liu K, Dong G. MicroRNA-335 inhibits invasion and metastasis of colorectal cancer by targeting ZEB2. Med Oncol. 2014;31(6):982. doi: 10.1007/s12032-014-0982-8. [DOI] [PubMed] [Google Scholar]
- 213.Liu F, Jia J, Sun L, Yu Q, Duan H, Jiao D, et al. lncRNA DSCAM-AS1 downregulates miR-216b to promote the migration and invasion of colorectal adenocarcinoma cells. Onco Targets Ther. 2019;12:6789–6795. doi: 10.2147/OTT.S213301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Kureishy N, Sapountzi V, Prag S, Anilkumar N, Adams JC. Fascins, and their roles in cell structure and function. BioEssays. 2002;24(4):350–361. doi: 10.1002/bies.10070. [DOI] [PubMed] [Google Scholar]
- 215.Ou C, Sun Z, He X, Li X, Fan S, Zheng X, et al. Targeting YAP1/LINC00152/FSCN1 signaling axis prevents the progression of colorectal cancer. Adv Sci. 2020;7(3):1901380. doi: 10.1002/advs.201901380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Adams JC. Roles of fascin in cell adhesion and motility. Curr Opin Cell Biol. 2004;16(5):590–596. doi: 10.1016/j.ceb.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 217.Yue B, Liu C, Sun H, Liu M, Song C, Cui R, et al. A positive feed-forward loop between LncRNA-CYTOR and Wnt/β-catenin signaling promotes metastasis of colon cancer. Mol Ther. 2018;26(5):1287–1298. doi: 10.1016/j.ymthe.2018.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ozawa T, Kazama S, Akiyoshi T, Murono K, Yoneyama S, Tanaka T, et al. Nuclear Notch3 expression is associated with tumor recurrence in patients with stage II and III colorectal cancer. Ann Surg Oncol. 2014;21(8):2650–2658. doi: 10.1245/s10434-014-3659-9. [DOI] [PubMed] [Google Scholar]
- 219.Tyagi A, Sharma AK, Damodaran C. A review on Notch signaling and colorectal cancer. Cells. 2020;9(6):1549. doi: 10.3390/cells9061549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Timmerman LA, Grego-Bessa J, Raya A, Bertrán E, Pérez-Pomares JM, Díez J, et al. Notch promotes epithelial-mesenchymal transition during cardiac development and oncogenic transformation. Genes Dev. 2004;18(1):99–115. doi: 10.1101/gad.276304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Sahlgren C, Gustafsson MV, Jin S, Poellinger L, Lendahl U. Notch signaling mediates hypoxia-induced tumor cell migration and invasion. Proc Natl Acad Sci U S A. 2008;105(17):6392–6397. doi: 10.1073/pnas.0802047105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Sonoshita M, Aoki M, Fuwa H, Aoki K, Hosogi H, Sakai Y, et al. Suppression of colon cancer metastasis by aes through inhibition of notch signaling. Cancer Cell. 2011;19(1):125–137. doi: 10.1016/j.ccr.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 223.Yuan R, Ke J, Sun L, He Z, Zou Y, He X, et al. HES1 promotes metastasis and predicts poor survival in patients with colorectal cancer. Clin Exp Metastasis. 2015;32(2):169–179. doi: 10.1007/s10585-015-9700-y. [DOI] [PubMed] [Google Scholar]
- 224.Weng MT, Tsao PN, Lin HL, Tung CC, Change MC, Chang YT, et al. Hes1 increases the invasion ability of colorectal cancer cells via the STAT3-MMP14 pathway. PLoS ONE. 2015;10(12):e0144322. doi: 10.1371/journal.pone.0144322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Rizk NI, Abulsoud AI, Kamal MM, Kassem DH, Hamdy NM. Exosomal-long non-coding RNAs journey in colorectal cancer: Evil and goodness faces of key players. Life Sci. 2022;292:120325. doi: 10.1016/j.lfs.2022.120325. [DOI] [PubMed] [Google Scholar]
- 226.Wan M, Wang Y, Zeng Z, Deng B, Zhu B, Cao T, et al. Colorectal cancer (CRC) as a multifactorial disease and its causal correlations with multiple signaling pathways. Biosci Rep. 2020;40(3):00265. doi: 10.1042/BSR20200265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Yang Z-H, Dang Y-Q, Ji G. Role of epigenetics in transformation of inflammation into colorectal cancer. World J Gastroenterol. 2019;25(23):2863. doi: 10.3748/wjg.v25.i23.2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.