Abstract
Foreign bodies in the intraconal space are unusual, and lodgment at the orbital apex was even more unusual. High-velocity object injuries, such as gunshots or industrial accidents, are the common causes of intraorbital foreign bodies. It is difficult for surgeons to retrieve foreign bodies from the orbital apex as it is a deep, narrow space with critical surrounding structures. The use of an image-guided navigation system improves the accuracy of transnasal endoscopic surgery and causes less damage. We present a case in which a bullet became lodged in the orbital apex and was successfully removed using transnasal endoscopic surgery with the collaboration of otolaryngologists and ophthalmologists. To summarize, orbital apex foreign bodies are harmful, and prompt removal with a personalized multidisciplinary approach is critical.
Keywords: Bullet, transnasal endoscopic approach, navigation system, orbital apex, orbit
Introduction
Intraorbital foreign bodies are commonly caused by high-velocity objects injuries such as gunshots or industrial accidents.[1] Intraorbital foreign bodies would cause damage to surrounding structures such as extraocular muscles, bones, or the optic nerve, leading to complications such as limited extraocular movement, vision loss, or severe inflammation and infection.[1,2] As a result, the complete removal of the intraorbital foreign body has become the crucial issue for the better prognosis.
Intraorbital foreign bodies are uncommon, and foreign bodies in the orbital apex are even rarer, making removal difficult due to the deep, small, and confined space.[1,3,4] Conventional external approaches to the intraconal area from transconjunctival, transcranial, or transcutaneous of eyelid have been reported and commonly used.[4] Minimally invasive surgery is becoming more popular as technology and imaging systems improve.[1,5] This case report presented a 20-year-old male injured by an air gunshot with a metallic bullet confined at the orbital apex. The metallic bullet was extracted using an endoscopic transnasal approach and a surgical navigation system without causing any damage to the surrounding structures.
Case Report
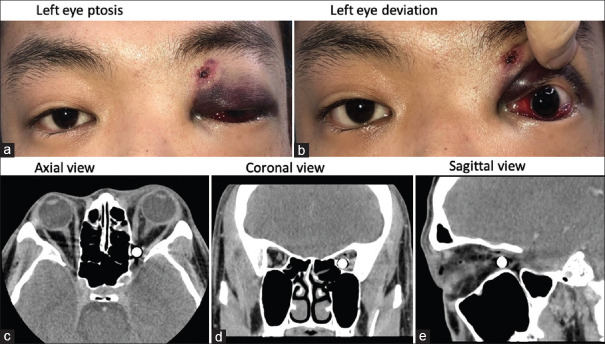
A 20-year-old male with the underlying disease of major depression disorder and arrhythmia under oral medication control presented to our emergency department with sudden-onset vision loss in the left eye after being shot by an air gun with a metal bullet. When his left eye was examined, one small penetration wound at the upper eyelid was discovered, along with ecchymosis and complete ptosis [Figure 1a and b]. The visual acuity was found no light perception in the left eye. The pupil was 6 mm and nonreponsive to light, with the positive reverse relative afferent pupillary defect. His left eye's ocular movements were limited to abduction and downward gaze. In the left eye, intraocular pressure and the results of a slit-lamp examination of other structures were normal. The computed tomography (CT) scan discovered a round metallic foreign body located at the left orbital apex [Figure 1c-e].
Figure 1.
(a) Clinical image of the patient demonstrating an entry wound located superomedially of the left upper eyelid with eyelid ecchymosis, complete ptosis, and hemorrhagic chemosis, (b) left exotropia in primary gaze position, (c) axial, (d) coronal, and (e) sagittal view of computed tomography scan image demonstrating round-shaped, metallic foreign body (bullet) at the left orbital apex area
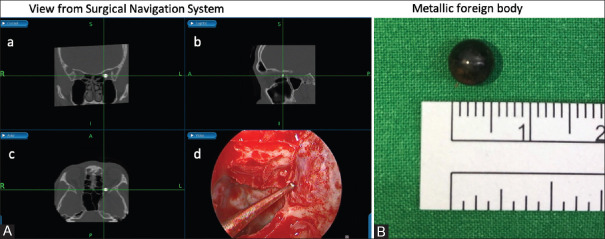
He was later diagnosed with the left intraconal foreign body complicated by traumatic optic neuropathy. Endoscopic transnasal removal was performed in assistance with a surgical navigation system (Medtronic StealthStation S8 Surgical Navigation System). The otolaryngologist started by performing an ethmoidectomy, removing a lamina papyracea 1.5 cm × 1.5 cm in size, and opening the adjacent periorbita with a crescent knife after localizing the bullet with the assistance of the navigation system [Figure 2a]. Then, the ophthalmologist dissected the orbital fat and exposed the medial rectus in the orbital apex. The medial rectus was gently elevated by a surgical elevator, and the bullet popped out into the nasal cavity when the surgeon gently compressed the eyeball. The bullet was eventually extracted with minimal damage to the surrounding tissues [Figure 2b]. No intraorbital bleeding was noted during the operation. The ocular movement continued to improve on the postoperative day 1 and throughout the hospitalization period. However, the visual acuity remained compromised. Although there was no discernible improvement in visual acuity after a 3-month follow-up, no postoperative complications or adjunctive tissue damage were observed during the follow-up period.
Figure 2.
Image-guidance navigation system reconstruction computed tomography image in (A-a) coronal, (A-b) sagittal, and (A-c) axial views revealed the orbital apex metallic foreign body in all three planes, and (A-d) real-time surgical view at the orbital apex. The rounded bullet was shown at the orbital apex after a small area of the lamina papyracea was removed and the periorbita incision was made; the bullet was delivered by a surgical instrument penetrated near the orbital apex. (B) The metallic foreign body was 6.0 mm in diameter
Discussion
Foreign bodies confined at the orbital apex are uncommon but usually associated with devastating orbital injury.[1,3,5] Loss of vision was a common symptom of globe rupture or traumatic optic neuropathy.[1] Furthermore, retained intraorbital foreign body can cause immediate or delayed complications, such as orbital inflammation, cellulitis, or infection. Although a few cases of well-tolerated retained orbital foreign body[6] were reported, surgical removal was still recommended to avoid those immediate and delayed complications.[1,2]
An appropriate imaging study should be done before the surgery to detect the location, the size, and the material of the foreign bodies.[3] For metallic foreign bodies, the standard diagnostic test would be a CT scan, which is quick, noninvasive, and safe. Furthermore, a CT scan of the head-and-neck area with an orbital thin cut can benefit the surgeon through three-dimensional reconstruction and application in the navigation system.[7]
There are several different methods for removing foreign bodies lodged in the orbital cavity. Due to the confined and narrow space as well as the small surgical field, it is a difficult technique.[8] Several methods are reported for removing intraconal objects, including the transconjunctival,[9,10] transmaxillary,[11] transcranial,[12] and eyelid.[13]
The abovementioned approaches will be limited by the location of the foreign body and may result in a scar after the operation. These approaches may be time-consuming and challenging in precisely localizing the foreign body.[4,14] Furthermore, the structures at the orbital apex, with different anatomies, and abundant vessels and nerves, are difficult to dissect and approach. Transnasal endoscopic surgery, on the other hand, is gaining acceptance and application as a novel and safe technique for approaching the medial intraconal space with a better surgical view and less scar formation. Besides, combining endoscopic surgery and image navigation system could allow the surgeons to personalized design the surgical methods and routes.[5,7,15] With the rapid advancement of science and technology, computer-aided navigation systems have become widely used in craniomaxillofacial field to guide the surgical instrument for a safer approach to the delicate and vulnerable structures in the small surgical field. From former review study, navigation technology not merely improves safety intraoperatively but also improves health outcomes in the wide range of craniomaxillofacial procedures.[16] As a result, the navigation system is critical in transnasal endoscopic surgery, allowing for accurate foreign-body localization and avoiding unnecessary tissue dissection.[16,17]
Transnasal endoscopic removal of bullet around the orbital apex was first described by Muhammad Khyani et al., who delivered the bullet through transnasal endoscopic surgery uneventfully without the image navigation system. According to this report, the bullet entered the orbital apex through the lateral nasal wall. The destruction of the lamina papyracea wound provided a clue and a route to localize the bullet through transnasal endoscopic approach.[18] According to the various entering route of the foreign body, the lateral orbitotomy approach had been reported as well. The patient in our case got the gunshot through his eyebrow area, which was not directly penetration at the septum of the nose. As a result of the lack of visibility in the confined space, endoscopic transnasal surgery with the navigation system provided a better surgical view and accurate localization.[7,19] Koo et al.[7] described a case in which an orbital apex foreign body (a ballpoint pen nib) was successfully removed entirely by transnasal endoscopic surgery and an image-guidance navigation system. Furthermore, Promsopa and Prapaisit[20] reported a similar case with a chronic metal bullet at the nasal lower of the orbital cone for 8 months and retrieved the bullet using endoscopic transnasal surgery and a navigation system without causing damage to her visual acuity or surrounding structures. To sum up, with the enhancement of the navigation system and technique, the surgeon is not only able to accurately locate the object but also has a better surgical view throughout the operation to minimize the damage to surrounding vital structures. What's more, the collaboration of both specialties bridges the gap between intranasal and intraorbital dissection.
However, there are still some disadvantages to this novel approach. First, postoperative crust formation obstructing the nasal cavity, epistaxis, and nasal discharge is common during the early postoperative period, but these symptoms generally improve with supportive care.[21,22] Second, longer operative time was required compared with the traditional method. Finally, due to orbital anatomy, the transnasal approach has some limitations. Technically, the medial and inferior sides are easier to approach with this transnasal method, but the other sides are more challenging.[22,23] With adding the navigation system, we can not only avoid and alleviate the adjunctive tissue damage through the nostril and the nasal cavity but also have accurate localization. Despite limitations, transnasal endoscopic procedures combined with a navigation system remained a novel technique for more complex lesions extending from the orbital apex to the intracranial space.
To our knowledge, there were few reported cases in the literature reporting an orbital apex bullet that was removed in an entirely transnasal endoscopic procedure. We presented a unique case of an orbital apex bullet with a favorable surgical outcome.
Conclusion
Foreign bodies located at the orbital apex are detrimental to visual function and difficult to be removed. By emphasizing the benefits of a personalized multidisciplinary approach, we improve surgical success and reduce complications.
Institutional review board statement
The protocol has been reviewed by the Research Ethics Committee D of the National Taiwan University Hospital and complies the categories of exempt in accordance with the governmental laws and regulations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Yi-Hsuan Wei, an editorial board member at Taiwan Journal of Ophthalmology, had no role in the peer review process of or decision to publish this article. The other authors decalared no conflicts of interest in writing this paper.
References
- 1.Fulcher TP, McNab AA, Sullivan TJ. Clinical features and management of intraorbital foreign bodies. Ophthalmology. 2002;109:494–500. doi: 10.1016/s0161-6420(01)00982-4. [DOI] [PubMed] [Google Scholar]
- 2.Shetty NR, Panjiyar MM. Transnasal endoscopic removal of intra-orbital metallic foreign body. Int J Orl Head Neck Surg. 2019;5:1. [Google Scholar]
- 3.Al-Mujaini A, Al-Senawi R, Ganesh A, Al-Zuhaibi S, Al-Dhuhli H. Intraorbital foreign body: Clinical presentation, radiological appearance and management. Sultan Qaboos Univ Med J. 2008;8:69–74. [PMC free article] [PubMed] [Google Scholar]
- 4.Das D, Kuberappa RG, Agrawal S, Modaboyina S. Fragmented pellet in the orbital apex: A dilemma to remove or not. BMJ Case Rep. 2020;13:e237280. doi: 10.1136/bcr-2020-237280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feichtinger M, Zemann W, Kärcher H. Removal of a pellet from the left orbital cavity by image-guided endoscopic navigation. Int J Oral Maxillofac Surg. 2007;36:358–61. doi: 10.1016/j.ijom.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Ho VH, Wilson MW, Fleming JC, Haik BG. Retained intraorbital metallic foreign bodies. Ophthalmic Plast Reconstr Surg. 2004;20:232–6. doi: 10.1097/01.iop.0000129014.94384.e6. [DOI] [PubMed] [Google Scholar]
- 7.Koo Ng NK, Jaberoo MC, Pulido M, Olver JM, Saleh HA. Image guidance removal of a foreign body in the orbital apex. Orbit. 2009;28:404–7. doi: 10.3109/01676830903074087. [DOI] [PubMed] [Google Scholar]
- 8.Teh D, Mohamad NF, Lim E, Zulkiflee AB, Narayanan P, Kamalden TA. Endoscopic transnasal removal of an intraconal foreign body using an image-guided surgical system. Comput Assist Surg (Abingdon) 2016;21:25–8. doi: 10.3109/24699322.2016.1170884. [DOI] [PubMed] [Google Scholar]
- 9.Kiratli H, Bulur B, Bilgiç S. Transconjunctival approach for retrobulbar intraconal orbital cavernous hemangiomas. Orbital surgeon's perspective. Surg Neurol. 2005;64:71–4. doi: 10.1016/j.surneu.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 10.Pillai P, Lubow M, Ortega A, Ammirati M. Endoscopic transconjunctival surgical approach to the optic nerve and medial intraconal space: A cadaver study. Neurosurgery. 2008;63:204–8. doi: 10.1227/01.NEU.0000327026.01816.E5. [DOI] [PubMed] [Google Scholar]
- 11.Lyson T, Sieskiewicz A, Rogowski M, Mariak Z. The transmaxillary endoscopic approach to the inferior part of the orbit: How I do it. Acta Neurochir (Wien) 2015;157:625–8. doi: 10.1007/s00701-015-2359-y. [DOI] [PubMed] [Google Scholar]
- 12.Abuzayed B, Kucukyuruk B, Tanriover N, Sanus GZ, Canbaz B, Akar Z, et al. Transcranial superior orbitotomy for the treatment of intraorbital intraconal tumors: Surgical technique and long-term results in single institute. Neurosurg Rev. 2012;35:573–82. doi: 10.1007/s10143-012-0393-2. [DOI] [PubMed] [Google Scholar]
- 13.Pelton RW, Patel BC. Superomedial lid crease approach to the medial intraconal space: A new technique for access to the optic nerve and central space. Ophthalmic Plast Reconstr Surg. 2001;17:241–53. doi: 10.1097/00002341-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Purgason PA, Hornblass A. Complications of surgery for orbital tumors. Ophthalmic Plast Reconstr Surg. 1992;8:88–93. doi: 10.1097/00002341-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Khan-Lim D, Ellis J, Saleh H, Ram B. Endoscopic transnasal removal of orbital foreign body. Eye (Lond) 1999;13:667–8. doi: 10.1038/eye.1999.181. [DOI] [PubMed] [Google Scholar]
- 16.Klimek L, Wenzel M, Mösges R. Computer-assisted orbital surgery. Ophthalmic Surg. 1993;24:411–7. [PubMed] [Google Scholar]
- 17.Ewers R, Schicho K, Undt G, Wanschitz F, Truppe M, Seemann R, et al. Basic research and 12 years of clinical experience in computer-assisted navigation technology: A review. Int J Oral Maxillofac Surg. 2005;34:1–8. doi: 10.1016/j.ijom.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 18.Muhammad Khyani IA, Hafeez A, Farooq MU, Alam J. Endoscopic removal of bullet from orbital apex. J Coll Physicians Surg Pak. 2008;18:646–8. doi: 10.2008/JCPSP.646648. [DOI] [PubMed] [Google Scholar]
- 19.Levin B, Goh ES, Ng YH, Sethi DS. Endoscopic removal of a foreign body in the orbital apex abutting the optic nerve. Singapore Med J. 2019;60:265–6. doi: 10.11622/smedj.2019045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Promsopa C, Prapaisit U. Removal of intraconal bullet through endoscopic transnasal surgery with image-guided navigation system 8 months after injury: A case report. J Med Case Rep. 2019;13:65. doi: 10.1186/s13256-019-2007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Battaglia P, Lambertoni A, Castelnuovo P. Transnasal endoscopic surgery: Surgical techniques and complications. Adv Otorhinolaryngol. 2020;84:46–55. doi: 10.1159/000457924. [DOI] [PubMed] [Google Scholar]
- 22.El Rassi E, Adappa ND, Battaglia P, Castelnuovo P, Dallan I, Freitag SK, et al. Development of the international orbital Cavernous Hemangioma Exclusively Endonasal Resection (CHEER) staging system. Int Forum Allergy Rhinol. 2019;9:804–12. doi: 10.1002/alr.22316. [DOI] [PubMed] [Google Scholar]
- 23.Melder K, Zwagerman N, Gardner PA, Wang EW. Endoscopic endonasal approach for intra- and extraconal orbital pathologies. J Neurol Surg B Skull Base. 2020;81:442–9. doi: 10.1055/s-0040-1713940. [DOI] [PMC free article] [PubMed] [Google Scholar]