Abstract
Background
Human papillomavirus (HPV) infection is a common sexually transmitted disease, characterised by persistent infection with high-risk strains leading to malignant conditions such as cervical cancer. The HPV vaccine is a well-known primary preventive measure for HPV infections. Previous studies have shown that medical doctors’ vaccine recommendation is one of the key strategies in improving HPV vaccine uptake. In 2019, Zambia rolled out the free national HPV vaccination program targeting 14-year-old girls. However, the annual coverage for HPV vaccination is variable, with rates as low as 33% for 2021.
Materials and Methods
We conducted a cross-sectional study between September and December 2020 at the University Teaching Hospitals in Lusaka, Zambia. We used analysis of variance to assess the mean differences in the overall scores for knowledge, attitude and practices towards the HPV vaccine. In addition, we used structural equation modelling (SEM) to test the traditional education theory as medical doctors’ HPV vaccine knowledge, attitude, and practices cover several facets, and SEM can model latent variables.
Results
We enrolled 121 medical doctors, of whom 67 (44.6%) were male. The majority, 76 (62.8%), were registrars and 79 (65.3%) had more than ten years of clinical experience. The overall mean knowledge, attitude, and practice score of the HPV vaccine mean (SD) were 70.2 (15.1), 72.1 (18.5) and 77.1 (28.9), respectively. More than half of the medical doctors would advise anyone eligible to take the HPV vaccine 66 (54.6%). There was a positive correlation between attitude and practice towards the HPV vaccine (β = .03, P = .017). Conversely, there was no evidence of a correlation between overall HPV knowledge and attitude (β = .01, P = .670) and rank of the medical doctors (β = −7.87, P = .355).
Conclusion
Knowledge was high with good attitudes and practices among medical doctors, which are vital in vaccine recommendation and subsequent uptake.
Keywords: Zambia, sub-Saharan Africa, cervical cancer prevention, structural equation modelling, COVID-19, vaccine recommendation
Background
Human papillomavirus (HPV) infection is the most common sexually transmitted disease worldwide.1 Most sexually active people will get HPV infection in their lifetime, but the body’s immune system usually clears this off.2 Nevertheless, about 20% of infections persist with a long latency period which may lead to malignancies, including genital tract cancers, with cervical cancer being the commonest.3 HPV infections are highly prevalent; in a worldwide meta-analysis among women with normal cervical cytology, the prevalence was 10.4%. A regional analysis showed that Africa had the highest prevalence at 22.1%.4 HPV co-infection with HIV, which is also highly prevalent in sub-Saharan Africa (SSA), worsens the prognostic effects of HPV infection.5 HIV-positive women are up to six times more likely to develop cervical cancer than their HIV-negative counterparts.6,7 In Zambia, HIV infection is disproportionately distributed with a higher prevalence among females within the reproductive age group (15-49 years) than male counterparts,8 contributing to the high incidence of cervical cancer (66.4/100 000 women-years).9 Cervical cancer remains highly prevalent in Zambia, even though the country is one of the pioneers within the region in cervical cancer control.10 Zambia has a free national cervical cancer screening program since 2006 and is currently available in all the provinces of the country; however, the program faces many challenges at the individual and system levels, contributing to late presentation and delayed access to adequate treatment.10,11
The HPV vaccine is one of the greatest innovations in cervical cancer prevention, prequalified by the World Health Organisation (WHO) in 2006. Most high-income countries have successfully implemented HPV vaccination programs and are already reaping the benefits. For example, a meta-analysis including fourteen high-income countries reported a reduction in the prevalence of HPV types 16 and 18 by 83% among girls aged 13-19 years and by 66% among women aged 20-24 years with significant cross-protection from HPV 31, 33 and 45.12 Sadly, populations with the highest HPV incidence such as low and middle-income countries (LMICs) remain largely unprotected. In another instance, a global HPV vaccine coverage estimate, only 1% of the estimated 118 million women targeted through these programmes were from LMICs.13 Therefore, various strategies must be implemented to ensure that HPV vaccine coverage increases to acceptable levels capable of achieving herd immunity within the population.
In trying to reduce the number of cervical cancer cases, the Cervical Cancer Prevention Program was launched in Zambia in the year 2006 and initially targeted the highest risk HIV-infected women then later included the non-HIV population, this programme utilised the various screening methods. In 2019, Zambia rolled out a free National HPV vaccination program for girls aged 14 years14 to reduce the high morbidity and mortality from cervical cancer.15 Vaccines are delivered through schools, health facilities and community outreach posts.16 During the inaugural year, the coverage was 75%, dropping steeply in 2021 to 33%. The drop was due to multiple factors, including; myths and misconceptions around the HPV vaccine, particularly with regards to infertility; fear of the unknown and possible side effects and lack of knowledge; lack of prior desensitisation to resolve cultural barriers before vaccination rollout, and this was further worsened by the closure of schools due to the COVID-19 pandemic.16 These figures fall short if the country has to remain on course with the World Health Organisation-WHO accelerated elimination strategy of cervical cancer strategy of having at least 90% of 15-year-old girls fully vaccinated by 2030.17
Among the strategies to increase HPV vaccine uptake is active medical doctors’ recommendation which is an essential driver of parental decisions about vaccination.18 As an exemplar, a study among women attending an antenatal clinic in Johannesburg found that the doctor’s recommendation was the most critical aspect when deciding to have their children vaccinated.19 Further, studies done in the USA review that doctors recommendations are among the most important predictors of HPV vaccine uptake among both girls20 and boys.21 A systematic review on barriers to HPV vaccination among US adolescents reported parents consistently citing health care professional recommendations as most important in their decision to vaccinate their children. Therefore, medical doctors ought to be knowledgeable to confidently recommend the HPV vaccine to their clients.22 Knowledge plays a key factor in nurturing doctor-patient relationships.23 Previous literature shows that variation in knowledge levels among doctors negatively affects their vaccine recommendations.24,25 However, there is limited information regarding HPV vaccination knowledge and recommendations among medical doctors in Zambia. Therefore, this study aimed to assess medical doctors’ knowledge, attitudes, and practices toward the HPV vaccine. We hypothesised that good knowledge and attitude would lead to good practices toward HPV vaccine recommendation, which is critical in the HPV vaccine uptake.
Materials and Methods
A cross-sectional study was conducted between September and December 2020 at the University Teaching Hospitals (UTH) in Lusaka, the largest referral hospital in Zambia, with a bed capacity of 1650 and about 600 Medical doctors. The hospital is divided into five specialist hospitals, namely: (i) Adult and Emergency Hospital, (ii) Women and Newborn Hospital, (iii) Cancer Diseases Hospital, (iv) Children’s Hospital and (v) Eye Hospital. The study population consisted of different ranks of medical doctors, i.e Junior resident medical officers (JRMO), Registrars and Consultants. A JRMO is a medical doctor interning and is within the first two years of graduating from medical school, working under supervision before working independently at primary healthcare facilities. A registrar is a medical doctor pursuing a master of medicine in any of the medical specialities, once they graduate, they work as specialists in general or district hospitals across the country in both clinical and administrative positions. A specialist consultant is a medical doctor who has served for a minimum of two years since graduating as a specialist and plays a supervisory role.
We used a single proportion formula to determine the number of medical doctors participating in the study. We assumed the prevalence of HPV knowledge by medical doctors of 84% from a similar study25 with a 5% margin of error, 95% confidence intervals and a design effect of one. After adjusting for a finite population assumption, the final sample size of 154 was arrived at. We did not stratify the sample among the different ranks of medical doctors since we assumed that the variables assessed were equal.
We contacted potential participants via the bulk email system of the Zambia Medical Association, informed them about the study’s nature, and invited them to participate. The questionnaires were sent out every two weeks up to 3 times for participants who were not responding to increase the response rate.
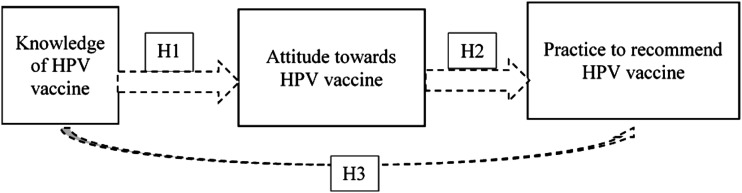
Using the traditional education theory, we hypothesised that the doctor’s knowledge of the HPV vaccine would influence their attitude towards it and ultimately lead to positive behaviour change. We made several assumptions (Figure 1). Firstly, we assumed that the expected covariance matrix in the traditional education theory does not differ from our sample covariance matrix. Secondly, knowledge regarding the HPV vaccine directly and positively influences both the attitude toward the HPV vaccine (H1 > 0) and the practice of recommending the vaccine to patients (H3 > 0). In addition, attitude directly and positively affects practice to recommend HPV vaccine (H2 > 0) and finally, knowledge indirectly affects practice to recommend HPV vaccine significantly and positively through attitude (H1+H2 > 0).
Figure 1.
Conceptual model of knowledge, attitude and practice towards HPV vaccine among medical doctors, Lusaka, Zambia.
Data was collected using a questionnaire sent electronically via Google forms platform@ due to COVID-19 preventative regulations to avoid physical contact and reduce the spread of the virus. We adapted the questionnaire from a previously developed and validated tool used among Israeli medical doctors.26 We first circulated the questionnaire to experts from the University of Zambia (UNZA), who carried out content and face validation. The resultant questionnaire was pre-tested on 12 medical doctors, who were later excluded from the study. It consisted of four sections with 27 questions distributed as follows; 5 social demographic questions, 13 HPV knowledge questions, six attitude questions and three practice questions. The Knowledge section had multiple choice questions with one or more correct answers to which participants had to choose the right choice, while the attitude and practice questions had yes/no options for responses. A score of one point was given if the respondent gave the correct answer for knowledge questions or chose “yes” to the questions on attitude and practice. We assigned a score of zero if any other response option was selected. The HPV knowledge, attitude and practice scores were calculated as continuous variables by adding the participant’s number of appropriate responses. The percentage HPV knowledge, attitude and practice scores were calculated by dividing the participant’s score by the maximum score of each outcome and multiplying by 100. We determined the internal validity of the questions by using Cronbach’s alpha score of not less than .70 and dropped any questions that had less than .70 scores. We de-identified all participant details. The STROBE checklist guided the manuscript writing.27
Ethics Approval
We received ethics approval from the University of Zambia School of Medicine Undergraduate Research Ethics Committee (UNZASOMUREC). Additional permission was obtained from the University Teaching Hospital (UTH) Director of clinical care and Diagnostics, and respective Senior Medical Superintendents before the research was carried out. We got participant informed consent online with a statement, “Choosing to proceed and complete the survey was considered consent to participate.” This statement only appeared after potential respondents read the information and consent forms linked to the questionnaire.
Statistical Analysis
We used Stata 16.1 (Stata Corp, College Station, Texas, USA) to analyse the data. Descriptive data were presented using frequencies with percentages and mean scores with standard deviation (SD). The Shapiro – Wilk test and quantile-quantile plots were used to confirm the normality of continuous data. The analysis of variance (ANOVA) test assessed the mean differences in the overall scores for knowledge, practice and attitude towards the HPV vaccine among medical doctors. ANOVA was followed by the Bonferroni posthoc test to assess pairwise comparison. Finally, we compared the proportions of correct responses between the medical doctors using the Pearson Chi-square test or Fisher’s exact test.
Structural Equation Modelling (SEM) was used to test the traditional education theory hypothesis as medical doctors HPV knowledge, attitude, and practices cover several facets. SEM can model several explanatory variables and multiple outcome variables. We used direct variables (questions on HPV knowledge, practices and attitude) to estimate the latent variables (knowledge, attitude and practices). For the goodness of fit for the model, we used the Tucker-Lewis Index (TLI) and the Comparative Fit Index (CFI), which were greater than .90 and .80 and Root Mean Standard Error of Association (RMSEA) was less than .05, suggesting a good fit.26 We considered path coefficients as the primary outcomes of SEM, which quantify the presumed relationships in the SEM.28 We standardised the path coefficient values and ranged from −1 to +1. A P-value of <.05 was considered statistically significant at a 95% confidence level for all statistical analyses.
Results
Baseline Characteristics
The study enrolled 121 participants, of whom 67 (44.6%) were male. The majority, 76 (62.8%) of respondents were registrars, 79 (65.3%) had more than ten years of clinical experience, and 68 (56.2%) were from Emergency and Adult hospitals. Nearly a third of the participants, 26 (24.8%), specialised in obstetrics and gynaecology (Table 1).
Table 1.
Baseline characteristics of respondents (N = 121).
| Characteristics | Frequency | Percentage |
|---|---|---|
| Sex | ||
| Female | 54 | 44.63 |
| Male | 67 | 55.37 |
| Rank | ||
| JRMO | 17 | 14.05 |
| Registrar | 76 | 62.81 |
| Consultant | 28 | 23.14 |
| Hospital/department | ||
| Cancer diseases | 4 | 3.31 |
| Paediatrics | 18 | 14.88 |
| Emergency and Adult (surgical and medical) | 68 | 56.20 |
| Women and Newborn | 31 | 25.62 |
| Years of practice | ||
| <1 | 14 | 11.57 |
| 1 – 5 | 18 | 14.88 |
| 6 – 10 | 10 | 8.26 |
| >10 | 79 | 65.29 |
| Speciality | ||
| Internal medicine | 24 | 19.83 |
| Obstetrics and gynaecology | 26 | 21.48 |
| Paediatrics | 18 | 14.88 |
| Surgery | 24 | 19.83 |
| Other | 29 | 23.97 |
Abbreviation: JRMO, Junior Resident Medical Officer.
Knowledge Scores Toward HPV-Vaccine
The overall knowledge mean (SD) score of the HPV vaccine among medical doctors was 70.2 (15.1). The mean score for JRMOs was 66.5 (15.4), registrars 68.01 (15.43) and consultants 78.4 (12.8). The majority of the medical doctors correctly identified the causative agent for cervical cancer 116 (95.9%). However, just under a third of the medical doctors, 29 (23.9%), correctly reported the incidence of cervical cancer in Zambia at the time of data collection. We noted that cervical cancer’s correct responses’ regarding the incidence rate was significantly different among the different specialities (P = .006). In addition, there was evidence of a difference in the overall HPV vaccine knowledge score among the medical doctors. On average, consultants had the highest scores for HPV vaccine knowledge compared to JRMOs and registrars (P = .004) (Table 2).
Table 2.
Cross-tabulation: Knowledge of HPV and HPV vaccine average scores by doctors rank.
| Knowledge Questions | Total n = 121 (%) | JRMO n = 17 (%) | Registrar n = 76 (%) | Consultant n = 28 (%) | P-Value |
|---|---|---|---|---|---|
| Which is the causative agent for cervical cancer? | 116 (95.9) | 16 (94.1) | 72 (94.7) | 28 (100) | .453a |
| Which is/are the risk factor/s for cervical cancer? | 108 (89.2) | 15 (88.2) | 67 (88.2) | 26 (92.9) | .782a |
| What is the incidence rate of cervical cancer in Zambia? | 29 (23.9) | 3 (17.7) | 13 (17.1) | 13 (46.4) | .006b |
| According to your knowledge, is the HPV vaccine available in Zambia? | 114 (94.2) | 15 (88.2) | 71 (93.4) | 28 (100) | .232a |
| What is the standardised WHO age range recommended for HPV vaccination? | 102 (86.4) | 14 (82.4) | 63 (85.1) | 25 (92.6) | .543 |
| Is HPV vaccination recommended for pregnant women? | 69 (57.02) | 9 (52.9) | 39 (51.3) | 21 (75.0) | .090b |
| According to WHO, catch-up vaccination is up to which age? | 87 (71.9) | 10 (58.8) | 53 (69.7) | 24 (85.7) | .119b |
| What is the route of administration of the HPV vaccine? | 75 (61.9) | 10 (58.8) | 43 (56.6) | 22 (78.6) | .117b |
| What is the protection rate (percentage) with the HPV vaccine? | 44 (36.4) | 7 (41.2) | 23 (30.3) | 14 (50.0) | .162b |
| When is the HPV vaccine most effective? | 91 (75.2) | 12 (70.6) | 54 (71.1) | 25 (89.3) | .144a |
| What is the screening technique for cervical cancer? | 116 (95.9) | 17 (100) | 74 (97.4) | 25 (89.3) | .121a |
| According to WHO, what is the recommended number of HPV vaccine doses that should be given? | 47 (38.8) | 4 (23.5) | 33 (43.4) | 10 (35.7) | .292b |
| Can someone who has had HPV vaccine develop cervical cancer? | 105 (86.8) | 15 (88.2) | 66 (86.8) | 24 (85.7) | .971a |
| Overall score mean (SD) | 70.2 (15.1) | 66.5 (15.4) | 68.0 (15.4) | 78.4 (12.8) | .004c |
aFisher’s exact test.
bPearson chi-square test.
coneway analysis of variance (ANOVA), values are percentage mean scores.
Attitude Scores Toward HPV Vaccine
The overall mean (SD) score for attitudes was 72.1 (18.5). It was highest among consultants, 75.7 (19.1), and lowest among JRMOs, 68.2 (17.4), although random chance finding could not be ruled out (P = .397). The majority, 117 (96.7%) of the doctors, agreed that screening women for cervical cancer even after being vaccinated was necessary, and nearly everyone, 114 (94.2%), agreed that the vaccine could prevent cervical cancer. However, about one third, 31 (25.6%) of the medical doctors disagreed that the vaccine could work once infected with the HPV virus. We noted a significant association between the ranks of the medical doctor and the question of HPV vaccine safety (P = .019) (Table 3).
Table 3.
Cross-tabulations: Attitude average scores towards HPV vaccine by doctors ranks.
| Attitude Questions | Total n=121 (%) | JRMO n=17 (%) | Registrar n=76 (%) | Consultant n=28 (%) | P-Value |
|---|---|---|---|---|---|
| Do you think the vaccine against HPV can prevent cervical cancer? | 114 (94.2) | 15 (88.2) | 72 (94.7) | 27 (96.4) | .523a |
| What do you think, once infected with HPV can the vaccine still work? | 31 (25.6) | 5 (29.4) | 20 (26.3) | 6 (21.4) | .829a |
| Do you think the vaccine should also be offered to men/boys? | 84 (69.4) | 13 (76.5) | 49 (64.5) | 22 (78.6) | .304b |
| Once vaccinated, is it necessary to screen that person for cervical cancer? | 117 (96.7) | 17 (100) | 73 (96.1) | 27 (96.4) | .710a |
| According to you, is the vaccine safe? | 90 (74.4) | 8 (47.1) | 58 (76.3) | 24 (85.7) | .019a |
| Could you accept being vaccinated if you were eligible? | 99 (81.8) | 16 (94.1) | 60 (78.9) | 23 (82.1) | .382a |
| Overall score mean (SD) | 72.1 (18.5) | 68.2 (17.4) | 71.6 (18.6) | 75.7 (19.1) | .397c |
aFisher’s exact test.
bPearson chi-square test.
coneway analysis of variance (ANOVA), values are percentage mean scores.
Practice Scores Toward HPV Vaccine
The majority of the doctors would recommend the HPV vaccine to their family members, 104 (85.9%) and other people, 110 (90.9%). More than half of the doctors would advise anyone to take the HPV vaccine 66 (54.6%). There was evidence of an association between the doctor’s rank and the question about advising anyone to take the vaccine (P = .023) (Table 4).
Table 4.
Cross-tabulation:Practice average scores towards HPV vaccine by doctors rank.
| Practices Questions | Total n=121 (%) | JRMO n=17 (%) | Registrar n=76 (%) | Consultant n=28 (%) | P-Value |
|---|---|---|---|---|---|
| Have you ever advised anyone to take the HPV vaccine? | 66 (54.6) | 5 (29.4) | 41 (53.9) | 20 (71.4) | .023a |
| Can you recommend the vaccine to your family members? | 104 (85.9) | 16 (94.1) | 62 (81.6) | 26 (92.9) | .621b |
| Can you recommend the vaccine to other people? | 110 (90.9) | 17 (100) | 67 (88.2) | 26 (92.9) | .653b |
| Overall score mean (SD) | 77.1 (28.9) | 74.5 (18.7) | 74.6 (30.7) | 85.7 (27.9) | .201c |
bFisher’s exact test.
aPearson chi-square test.
coneway analysis of variance (ANOVA), values are percentage mean scores.
Correlations between HPV knowledge, attitudes and practices
We applied the SEM to assess correlations between HPV knowledge, attitude, and practices results, shown in Figure 2. The goodness of fit for the final model was assessed using: RMSEA = .042; TLI = .889; and CFI = .903.
Figure 2.
Structural Equation Model (SEM) on HPV knowledge, attitude and practices among medical doctors in Lusaka, Zambia. Key: K1 – K13 are questions on HPV knowledge, A1 – Q6 are questions on attitude, p1-p3 are questions on practices, RMSEA-root mean square error of approximation, CFI-comparative fit index, Tucker-Lewis index, positioncat (medical doctors categorised as, junior resident medical officer, registrar and consultant).
There was no evidence of a correlation between overall HPV vaccine knowledge and attitude (β = .01, P = .670) and rank of the medical doctors (β = −7.87, P = .355). However, knowledge question 4 (on knowledge of vaccine availability on the Zambian market) significantly correlated with attitude question 2 (whether or not a vaccine can work once infected) (β = .01, P = .001). There was a positive correlation between attitude and practice. Medical doctors with high attitudes scores were more likely to have high practice scores (β= .03, P=.017). Additionally, a consultant or registrar, compared to JRMOs, was more likely to have high attitude scores toward vaccine safety (β = .06, P = .002). Medical doctors who knew the causative agent for cervical cancer were more likely to recommend the vaccine to family members than those who did not (β= .03, P=.001) (Figure 2).
Discussion
The present study examined medical doctors’ knowledge, attitude and practices toward the HPV vaccine. To the best of our knowledge, this is the first study in Zambia conducted during the HPV vaccination campaign national rollout. Most participants were registrars and were most likely to be in a position to discuss with patients about getting the HPV vaccine. These were adequately represented at 62.81% of the study sample. Generally, we found high average scores of knowledge, attitudes and practices towards the HPV vaccine. The knowledge of the HPV vaccine was not associated with the practice; however, medical doctors who reported high average scores for attitude were more likely to score highly on the practice of the HPV vaccine. Further, among the medical doctors' ranks, consultants reported the highest average scores on HPV knowledge than the JRMOs and registrars.
The overall average knowledge score reported in this study is not similar to what Hogue and colleagues found among South African medical doctors: the average knowledge score was 5 out of 11 items translating to less than 50%.24 This could be plausible due to the increase in knowledge and dissemination over time as the study was conducted eight years ago, physicians could be now well informed hence the difference in findings. Varied knowledge levels have been reported elsewhere. For instance, HPV vaccine knowledge among healthcare workers, as seen in a study in Saudi Arabia, was 61%, with over 90% of medical doctors aware of the link between HPV and cervical cancer, similar to our study findings.25 However, a study done among healthcare workers in Nigeria showed that despite more than 90% being aware of the HPV, 44% were unaware of the HPV vaccine; further, this study included nurses and found that they were the least aware of the HPV vaccine.29
Consultants were more knowledgeable than JRMOs, a finding consistent with the findings of AlMansoori and others,30 where doctors with more than ten years of service were more likely to have higher knowledge of HPV vaccine than those with less than ten years of service. The probable reason is that for one to be at a specialist consultant level, they are subject experts with much exposure to HPV-related conditions. Additionally, the Zambia HPV vaccination pilot program, which was highly publicised, took place in 2013 and 2014 in Lusaka province, where our study site is domiciled.31 Most JRMOs included in this study may have been medical students in the period when the vaccine rollout was introduced in the Zambian healthcare. Therefore, this could explain why we found high average knowledge levels among consultants who could have been working during the period for the vaccine national rollout program.
Overall, the medical doctors reported above-average attitude scores towards the HPV vaccine. This is in tandem with what was reported in an earlier study where about 86% of the medical doctors agreed that the HPV vaccine is safe, although about a third of the participants were uncertain of the acceptance of the vaccine by parents.30 A study done in the UK with more than ten years of National HPV vaccination showed that about 93.8% of physicians agreed or strongly agreed to recommend the HPV vaccine, with those unsure if they would recommend the HPV vaccine citing lack of knowledge and narrow spectrum of protection among other reasons.32 Similarly, a systematic review done in Iran showed positive attitudes among medical students and female nurses despite having low levels of knowledge.33
The study results show that the practices of medical doctors regarding the HPV vaccine were above average. Similar to our results, Hoque and others24 found that most medical doctors in South Africa would highly recommend the HPV vaccine to their patients, specifically those who mentioned that they would comply with HPV vaccination. Further, Yu and others34 explored the factors influencing doctors’ recommendation of HPV vaccine in China and found that medical staff had a higher willingness to recommend HPV vaccine than students, despite having low levels of knowledge. The duration in service and the ability to recommend the HPV vaccine have yielded variable results worldwide; for example, a systematic review based on studies conducted in the USA showed mixed results, with some studies showing no effect of years in practice on vaccine recommendation.35 However, a modest association was found in a systematic review on the level of practice and ability to recommend the vaccine.36 Therefore, our findings are in tandem with the prevailing trends of medical doctors’ willingness to recommend the vaccine.
Furthermore, the practice scores found in our study mean that doctors are willing to encourage screening of cervical cancer and HPV vaccination among parents seeking services from the hospitals. The plausible explanation is that those aware of the HPV, HPV vaccine and preventive strategies take a keen interest and play a vital role in preventing the negative messages around the vaccine. Therefore, the rolled-out HPV vaccination in Zambia should utilise the medical doctors to increase vaccine uptake among the populace. The high scores on attitude towards HPV vaccine mean that medical doctors would be key in the drive to address the myths and misconceptions about vaccination. Furthermore, implementation strategies targeting medical doctors may benefit by concentrating on the link between attitude and practice as the two are associated in this population instead of knowledge. On the other hand, considering that Zambia has a school-based HPV vaccination program, it is imperative that other important stakeholders in the community such as teachers, community leaders and parents are also actively involved in order to help facilitate HPV vaccine acceptability and ultimate uptake through strengthening collaboration with the health sector.37
Strengths and Limitations
This study has some limitations. It was conducted at a tertiary hospital; hence results may not be generalisable to lower levels of care; however, the study findings give an insight into the general outlook of the HPV vaccination program. In addition, we used an online mode of data collection necessitated by COVID-19, which could have affected the response rate. Further, the sample had more registrars than other ranks, so the overall parameter estimates should be interpreted with caution. Finally, the calculated sample size could not be achieved given the finite eligible population. Therefore, the results should be interpreted with caution; however, we believe the findings can still give an idea of the knowledge, attitude and practice towards the HPV vaccination in Zambia.
Nevertheless, the present study has some strengths worth noting. Firstly, we used a robust SEM for latent variables to test the traditional education theory assumptions compared to similar studies. Secondly, the study was done during the period when the HPV vaccination was rolled out in Zambia, despite witnessing high vaccine hesitance and mortality due to cervical cancer making our finding very crucial for guidance on the development of implementation strategies
Conclusions
This study has demonstrated that medical doctors are generally knowledgeable about the HPV vaccine and willing to recommend it to eligible candidates despite the majority not knowing to what extent cervical cancer is ravaging the country. These findings are crucial because medical doctors have been shown to influence the parent’s willingness to accept the vaccination of their children. Therefore, their knowledge, attitudes and practices towards the HPV vaccine are key to successfully implementing the vaccination program. With Zambia’s free National HPV vaccination programme, strategies aimed at enlightening JRMOs on the HPV vaccine should be pursued and implemented in addition to other approaches to improve uptake. Finally, future studies in Zambia should identify implementation strategies to address the myths and misconceptions about the HPV vaccine through medical doctors since they have high knowledge, attitude and practice. This would potentially address the current low vaccine uptake in Zambia.
Acknowledgments
We would like to acknowledge the Senior Medical Superintendents of the University Teaching Hospitals and the medical doctors who participated in this study. MM and KML would like to acknowledge that some of their time is supported by the UNC-UNZA-Wits Partnership for HIV and Women’s Reproductive Health (grant number: D43 TW010558).
Footnotes
Author Contributions: MKL-Conceptualisation, proposal writing, original draft manuscript preparation; JCK & JCZN-proposal writing & data collection-MM formal data analysis & manuscript writing; Manuscript editing JCK. All authors have read the final version and agreed to publish the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: We received ethics approval from the University of Zambia School of Medicine Undergraduate Research Ethics Committee (UNZASOMUREC). Additional permission was obtained from the University Teaching Hospital (UTH) Director clinical care and Diagnostics and respective Senior Medical Superintendents before the research was carried out. Participant informed consent was obtained online with a statement, “Choosing to proceed and completion of the survey was considered as consent to participate.” This statement only appeared after potential respondents read the information and consent forms linked to the questionnaire.
ORCID iD
Mwansa Ketty Lubeya, MD https://orcid.org/0000-0002-8526-3410
References
- 1.World Health Organisation . Wkly Epidemiol Rec. 2009;84:50517-50532. https://www.who.int/wer/2009/wer8415.pdf [Google Scholar]
- 2.McBride AA. Human papillomaviruses: Diversity, infection and host interactions. Nat Rev Microbiol. 2021;20:1-14. doi: 10.1038/s41579-021-00617-5. [DOI] [PubMed] [Google Scholar]
- 3.Giuliano AR, Nyitray AG, Kreimer AR, et al. EUROGIN 2014 roadmap: differences in human papillomavirus infection natural history, transmission and human papillomavirus-related cancer incidence by gender and anatomic site of infection. Int J Cancer. 2015;136(12):2752-2760. doi: 10.1002/ijc.29082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Sanjosé S, Diaz M, Castellsagué X, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis. 2007;7(7):453-459. DOI: 10.1016/S1473-3099(07)70158-5. [DOI] [PubMed] [Google Scholar]
- 5.Harris TG, Burk RD, Palefsky JM, et al. Incidence of cervical squamous intraepithelial lesions associated with HIV serostatus, CD4 cell counts, and human papillomavirus test results. JAMA. 2005;293(12):1471-1476. doi: 10.1001/jama.293.12.1471. [DOI] [PubMed] [Google Scholar]
- 6.Stelzle D, Tanaka LF, Lee KK, et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet Global Health 2020; Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly H, Weiss HA, Benavente Y, et al. Association of antiretroviral therapy with high-risk human papillomavirus, cervical intraepithelial neoplasia, and invasive cervical cancer in women living with HIV: a systematic review and meta-analysis. The lancet HIV. 2018;5(1):e45-e58. doi: 10.1016/s2352-3018(17)30149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ministry of health Z. Zambia Population-Based HIV Impact Assessment (ZAMPHIA) 2016: Final Report. Lusaka; 2019. https://phia.icap.columbia.edu/wp-content/uploads/2019/02/ZAMPHIA-Final-Report__2.22.19.pdf [Google Scholar]
- 9.Nyambe A, Lubeya MK. Cervical cancer and HIV in Zambian women. Lancet Global Health. 2021;9(6):e734. doi: 10.1016/s2214-109x(21)00230-8. [DOI] [PubMed] [Google Scholar]
- 10.Mwanahamuntu MH, Sahasrabuddhe VV, Pfaendler KS, et al. Implementation of ‘see-and-treat’ cervical cancer prevention services linked to HIV care in Zambia. AIDS. 2009;23(6):N1-N5. doi: 10.1097/QAD.0b013e3283236e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mwamba MJ, Kasonka L, Basil OO, et al. Cervical cancer diagnosis and treatment delays in the developing world: Evidence from a hospital-based study in Zambia. Gynecologic Oncology Reports. 2021;37:100784. doi: 10.1016/j.gore.2021.100784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drolet M, É B, Pérez N, Brisson M. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet (London, England). 2019;394(10197):497-509. doi: 10.1016/S0140-6736(19)30298-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bruni L, Saura-Lázaro A, Montoliu A, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev Med. 2021;144:106399. doi: 10.1016/j.ypmed.2020.106399. [DOI] [PubMed] [Google Scholar]
- 14.Ministerial Statement on Human Papillomavirus Vaccine by the Hon. Minister Of Health, 2019. [accessed 15 March 2022]. Available at: https://www.parliament.gov.zm.publication.docs/MinisterialStatementonHPVVaccine.pdf [Google Scholar]
- 15.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2018;68(6):394-424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 16.Kayombo M. Zambia’s hurdles in cervical cancer fight. Zambia daily mail 2022 Mar 03 [accessed 2022 March 10 ].Available at: http://www.daily-mail.co.zm/zambias-hurdles-in-cervical-cancer-fight/http://www.daily-mail.co.zm/zambias-hurdles-in-cervical-cancer-fight/
- 17.World Health Organization Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. 2020. Report No.: ISBN 978-92-4-001410-7.[accessed on 2021 March 17].Available at: https://www.who.int/publications/i/item/9789240014107 [Google Scholar]
- 18.Rosen BL, Shepard A, Kahn JA. US Health Care Clinicians’ Knowledge, Attitudes, and Practices Regarding Human Papillomavirus Vaccination: A Qualitative Systematic Review. Acad Pediatr. 2018;18(2s):S53-s65. doi: 10.1016/j.acap.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chipidza FE, Wallwork RS, Stern TA. Impact of the Doctor-Patient Relationship. Prim Care Companion CNS Disord. 2015;17(5):2015. doi: 10.4088/PCC.15f01840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brewer NT, Gottlieb SL, Reiter PL, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197-204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reiter PL, Gilkey MB, Brewer NT. HPV vaccination among adolescent males: results from the National Immunization Survey-Teen. Vaccine. 2013;31(26):2816-2821. doi: 10.1016/j.vaccine.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014;168:76PMC4538997. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Francis SA, Nelson J, Liverpool J, Soogun S, Mofammere N, Thorpe RJ, Jr. Examining attitudes and knowledge about HPV and cervical cancer risk among female clinic attendees in Johannesburg, South Africa. Vaccine. 2010;28(50):8026-8032. doi: 10.1016/j.vaccine.2010.08.090. [DOI] [PubMed] [Google Scholar]
- 24.Hoque ME. Factors influencing the recommendation of the Human Papillomavirus vaccine by South African doctors working in a tertiary hospital. Afr Health Sci. 2016;16(2):567-575. doi: 10.4314/ahs.v16i2.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Almazrou S, Saddik B, Jradi H. Knowledge, attitudes, and practices of Saudi physicians regarding cervical cancer and the human papillomavirus vaccine. J Infect Public Health. 2020;13(4):584-590. doi: 10.1016/j.jiph.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 26.Khamisy-Farah R, Adawi M, Jeries-Ghantous H, et al. Knowledge of Human Papillomavirus (HPV), Attitudes and Practices Towards Anti-HPV Vaccination Among Israeli Pediatricians, Gynecologists, and Internal Medicine Doctors: Development and Validation of an Ad Hoc Questionnaire. Vaccines. 2019;7(4):157. doi: 10.3390/vaccines7040157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573-577. (Note, you will probably need to renumber your references after this addition). [DOI] [PubMed] [Google Scholar]
- 28.Liu C, Wang D, Zhang X. Knowledge, Attitudes and Intentions to Prescribe Antibiotics: A Structural Equation Modeling Study of Primary Care Institutions in Hubei, China. Int J Environ Res Publ Health. 2019;16(13):2385. doi: 10.3390/ijerph16132385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Audu BM, Bukar M, Ibrahim AI, Swende TZ. Awareness and perception of human papillomavirus vaccine among healthcare professionals in Nigeria. J Obstet Gynaecol. 2014;34(8):714-717. doi: 10.3109/01443615.2014.925431. [DOI] [PubMed] [Google Scholar]
- 30.AlMansoori LS, AlKatheeri MS, AlHallami AA, AlMarzooqi MY, Al-Tatari M, L-Tatari HA. Physicians’ knowledge, attitude, and practices toward HPV disease and vaccination in Al Ain city, UAE. International Journal of Contemporary Research and Review. 2019;10(6):20741-20750. DOI: 10.15520/ijcrr.v10i06.706. [DOI] [Google Scholar]
- 31.Human Papillomavirus Vaccine Launched in Zambia. 2013. [Accessed] 15 May 2021. Available at: https://www.afro.who.int/news/human-papilloma-virus-hpv-vaccine-introduced-zambia [Google Scholar]
- 32.Sherman SM, Cohen CR, Denison HJ, Bromhead C, Patel H. A survey of knowledge, attitudes and awareness of the human papillomavirus among healthcare professionals across the UK. Eur J Publ Health. 2020;30(1):10-16. doi: 10.1093/eurpub/ckz113. [DOI] [PubMed] [Google Scholar]
- 33.Taebi M, Riazi H, Keshavarz Z, Afrakhteh M. Knowledge and Attitude Toward Human Papillomavirus and HPV Vaccination in Iranian Population: A Systematic Review. Asian Pac J Cancer Prev APJCP. 2019;20(7):1945-1949. doi: 10.31557/APJCP.2019.20.7.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu C, Chen L, Ruan G, An J, Sun P. Evaluation of Knowledge and Attitude Toward HPV and Vaccination Among Medical Staff, Medical Students, and Community Members in Fujian Province. Risk Manag Healthc Pol. 2020;13:989-997. doi: 10.2147/RMHP.S243048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gilkey MB, McRee A-L. Provider communication about HPV vaccination: A systematic review. Hum Vaccines Immunother. 2016;12(6):1454-1468. doi: 10.1080/21645515.2015.1129090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vadaparampil ST, Malo TL, Kahn JA, et al. Physicians’ Human Papillomavirus Vaccine Recommendations, 2009 and 2011. Am J Prev Med. 2014;46(1):80-84. DOI: 10.1016/j.amepre.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kucheba F, Mweemba O, Matenga TFL, Zulu JM. Acceptability of the human papillomavirus vaccine in schools in Lusaka in Zambia: Role of community and formal health system factors. Global Publ Health. 2021;16(3):378-389. doi: 10.1080/17441692.2020.1810734. [DOI] [PubMed] [Google Scholar]