Abstract
Simple Summary
Despite an initial response to therapy, many lung cancer patients inevitably develop resistance to therapy leading to decreased duration of response and success of treatment. Recent research aims to elucidate mechanisms of resistance in order to improve drug response and treatment outcomes. By utilizing multidisciplinary approaches that target various resistance mechanism, it may be possible to delay development of treatment resistance or even resensitize cancers. This review aims to discuss novel approaches to improve clinical outcomes, delay the occurrence of resistance, and overcome resistance.
Abstract
Lung cancer is one of the leading causes of cancer-related deaths worldwide with a 5-year survival rate of less than 18%. Current treatment modalities include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Despite advances in therapeutic options, resistance to therapy remains a major obstacle to the effectiveness of long-term treatment, eventually leading to therapeutic insensitivity, poor progression-free survival, and disease relapse. Resistance mechanisms stem from genetic mutations and/or epigenetic changes, unregulated drug efflux, tumor hypoxia, alterations in the tumor microenvironment, and several other cellular and molecular alterations. A better understanding of these mechanisms is crucial for targeting factors involved in therapeutic resistance, establishing novel antitumor targets, and developing therapeutic strategies to resensitize cancer cells towards treatment. In this review, we summarize diverse mechanisms driving resistance to chemotherapy, radiotherapy, targeted therapy, and immunotherapy, and promising strategies to help overcome this therapeutic resistance.
Keywords: lung cancer, therapeutic resistance, chemotherapy, radiotherapy, targeted therapy, immunotherapy, tumor microenvironment, hypoxia
1. Introduction
Lung cancer is one of the leading causes of cancer deaths globally, with an approximately 1.8 million deaths per year [1]. It is a molecularly heterogeneous disease and can be divided into two major subtypes: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC is further subdivided into histological subtype lung adenocarcinoma (LUAD), lung squamous cell carcinoma (LUSC), and large cell lung carcinoma (LCLC), which together account for 85% of all lung cancer cases. The remaining 15% of lung cancer is constituted by SCLC [2,3,4,5]. Widespread inter and intratumoral heterogeneity and transdifferentiation afford multiple mechanisms by which treatment resistance may develop and thus pose threats to the treatment of lung cancer [6]. Accurate subtyping is remarkably important for the treatment of lung cancer as major treatment options are determined based on histological examination performed by molecular pathology or immunohistochemistry.
Although cigarette smoking is a major risk factor, environmental pollution and genetic factors also contribute to the development of lung cancer. Cancer driver genes found in LUAD include Kirsten rat sarcoma viral oncogene homolog (KRAS), epidermal growth factor receptor (EGFR), tumor protein p53 (TP53 or p53), kelch-like ECH-associated protein 1 (KEAP1), serine threonine kinase 11 (STK11) also named as LKB1, and neurofibromatosis type 1 (NF1) [7]. Commonly mutated genes in LUSC are TP53, a tumor suppressor gene that is present in more than 90% of tumors, and cyclin dependent kinase inhibitor 2A (CDKN2A). Retinoblastoma (RB1) and p53 are genes usually mutated in SCLC [7,8]. The amplification of MYC family genes (MYC, MYCL, and MYCN), which are proto-oncogenes, is also observed in a subset of SCLC tumors [9]. Efforts towards classifying lung cancers based on genetic lesions have greatly helped to guide targeted therapies and improve clinical practice [10].
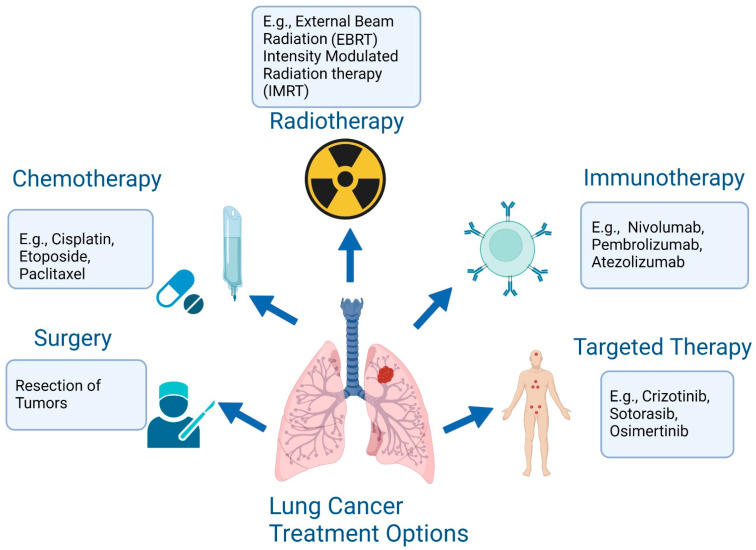
The treatment of lung cancer includes surgical resection, chemotherapy, immunotherapy, radiotherapy, and targeted therapy (Figure 1) [11,12]. There has been significant advancement in the treatment of lung cancer over the past two decades. The recent introduction of immune checkpoint inhibitors (ICIs), also named immune checkpoint blockades (ICBs), to target immune checkpoint proteins (ICPs) in the treatment of lung cancer patients, offers new promises [13]. Despite these advanced therapies, including immunotherapies, radiotherapies, and a combination of chemo-immunotherapies, resistance poses a challenge to clinical outcomes. Therapeutic resistance results in cancer recurrence and metastasis, and decreases patients’ lifespans [14]. Therefore, understanding the molecular mechanisms of therapeutic resistance is important in developing novel strategies to improve the overall survival (OS) rate of lung cancer patients. In this review, we discuss the mechanisms underlying the acquisition of resistance to different lines of therapy and potential strategies that can help overcome resistance.
Figure 1.
The treatment options for lung cancer are surgery, chemotherapy, radiotherapy, immunotherapy, and targeted therapy (created with BioRender.com (accessed on 1 September 2022).
2. Mechanism of Chemoresistance and Potential Therapeutic Inhibitors
Despite the growing interest in non-cytotoxic therapeutic agents, chemotherapy remains the standard treatment option for patients with advanced, unresectable NSCLC and first- and second-line management of SCLC [15,16,17]. There are four broad categories of chemotherapeutic drugs: (1) alkylating agents (e.g., platinum compounds such as cisplatin and carboplatin); (2) microtubule-targeting drugs (e.g., paclitaxel, docetaxel, and vinorelbine); (3) antimetabolites (e.g., pemetrexed and gemcitabine); and (4) topoisomerase inhibitors (e.g., etoposide) [18,19,20,21]. Despite the initial responsiveness of tumors to chemotherapies, lung cancer patients rapidly develop chemoresistance leading to disease progression.
Various factors contributing to chemoresistance (Table 1) include changes in drug influx and efflux, drug target alteration or inactivation, compartmentalization, epigenetic changes, and DNA damage. The blockade of cell-cycle arrest and apoptosis, the interaction of tumor microenvironments (TMEs), the acquisition of epithelial–mesenchymal evolution and cancer stem cell (CSC)-like phenotypes, unregulated microRNAs (miRNAs) expression, and metastasis are also responsible for chemoresistance [22,23,24,25,26]. TME is comprised of tumor and stromal cells such as fibroblasts, endothelial cells, and immune cells surrounded by a non-cellular component and vascular network. Cross-talk between the various components of the TME promotes tumor progression and therapeutic resistance by triggering hypoxia, a deficiency in nutrient supply, and vascular viscosity [27,28,29].
Table 1.
Summary of mechanism of chemotherapeutic resistance in lung cancer.
| Mode of Action | Target Entity | Chemotherapeutic Agent | References |
|---|---|---|---|
| DNA repair system | Upregulation of: ERCC1 DNA Polymerase |
Platinum compounds | [94,95] |
| Drug efflux | Upregulation of ABC family transporters: ABCC1/MRP1 ABCC3/MRP3 ABCB1/MDR1 ABCC10/MRP7 ABCB1/MDR1/p-glycoprotein ABCC6/MRP6 ABCC11/MRP8 |
Platinum compounds Microtubule-targeted compounds Etoposide Gemcitabine Pemetrexed |
[33,34,35,36,37,38] |
| Prosurvival signaling | Upregulation of: EGFR PI3K/Akt MAPK Calpain Sphk1 |
Platinum compounds Microtubule-targeted compounds Pemetrexed |
[42,43,44] |
| Cell cycle arrest | Upregulation of: Bcl-2 Bcl-XL Autophagy |
Platinum compounds Gemcitabine Microtubule-targeted compounds |
[46,47,96] |
| Epigenetic regulation | Promoter methylation of IGFBP3 and FOXF1 Upregulation of KDM3B Deregulation of circadian rhythm |
Platinum compounds | [67,97,98,99] |
| MicroRNA | Upregulation of: miR-106a, miR- 31, miR-15b, miR-27a, miR-223, miR-205, miR-92b, miR-224, miR-34c-5p, miR-181a, miR-135a, miR 197-3p, miR-222-3p downregulation of: miR-101-3p, miR-181, miR-589, miR-1244, miR-29c, miR-630, and miR-197 miR-16, miR-17-5p, miR-216b, miR-200b, miR-363-3p |
Platinum compounds Microtubule-targeted compounds Etoposide Gemcitabine |
[16,84,85,86,87] |
| EMT/CSC | Upregulation of: EMT phenotype Notch signaling Wnt signaling Shh signaling |
Platinum compounds Microtubule-targeted compounds Etoposide Pemetrexed |
[100,101] |
| Tumor microenvironment | Upregulation of: Hypoxia CAF PDL-1 |
Platinum compounds | [102,103,104] |
| Cancer metabolism | Upregulation of: PGC1α and glutamine metabolism Downregulation of: OXPHOS and glycolysis |
Platinum compounds | [90,105] |
Studies show that upregulation of the DNA repair pathway mediates resistance to platinum-based chemotherapeutic agents. Platinum-induced DNA damage is repaired by two main pathways: nucleotide excision repair (NER) and homologous recombination (HR). Excision Repair Cross Complementing-1 (ERCC1) is a pivotal component of NER, whose expression is associated with cisplatin resistance in NSCLC [16,30,31].
The transportation of drugs is a controlled process that is mediated by the ATP-binding cassette (ABC) transporter family of proteins. Expression of the ABC superfamily of transport proteins, such as MRP1/ABCC1 and MRP3/ABCC3, was found to be correlated with cisplatin resistance [32]. Upregulated expression of ABCB1/MDR1/p-glycoprotein, ABCC3/MRP3, and ABCC10/MRP7 was observed in paclitaxel-, docetaxel-, or vinorelbine-resistant NSCLC cells [33,34,35,36,37,38].
Glutathione S-transferase (GST) isozymes, glutathione S-transferase pi 1 (GSTP1), and glutathione S-transferase alpha 1 (GSTA1) are predominantly overexpressed in cancer cells and play a significant role in the detoxification and inactivation of platinum drugs, followed by resistance to chemotherapy [22,39,40]. Upregulation of GSTP1 is linked with a poor response to anticancer drugs such as cisplatin. Glutathione S-transferase alpha 1 (GSTA1-1) overexpression appears to undermine the doxorubicin-dependent reduction in glutathione, particularly in the H69 SCLC cell line, by reducing lipid peroxidation [22,39,41]. Another research shows that inhibition of GSTP expression, through antisense cDNA, increases the cancer cell sensitivity to doxorubicin, cisplatin, and etoposide by reducing the detoxification of the drugs [22,39].
Associated with resistance to chemotherapy is the activation of signal transduction pathways such as EGFR and its downstream facilitators, which include the PI3K/Akt and mitogen-activated protein kinase (MAPK) signaling pathways, nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), and signal transducers and activators of transcription 3 (STAT3) [42,43,44]. Ataxia-telangiectasia-mutated (ATM) is a member of the phosphatidylinositol 3-kinase- (PI3K) family of Ser/Thr protein kinases. NSCLC cells with acquired cisplatin resistance displayed an upregulation of ATM, phosphorylation/activation of its downstream effectors CHK2 and p53, and the overexpression of antiapoptotic proteins Bcl-2 and Bcl-XL. [45,46,47]. Pharmacological or genomic targeting of ATM, either alone or in combination with Mcl-1 (myeloid cell leukemia 1), which targets the B cell lymphoma 2 (Bcl-2) by acting as an antiapoptotic member of the Bcl-2 family of apoptosis-regulating proteins, restored sensitivity to cisplatin treatment in cisplatin-resistant cells [45,48]. Notably, Bcl-2 overexpression makes lung cancer cells resistant to apoptosis caused by DNA damage. Recent studies have shown that targeting Bcl-2-like proteins increases the effectiveness of platinum-based drugs, by eliminating cancer stem cells (CSCs) [49] as well as apoptosis-resistant cells [50,51,52,53]. As competitive inhibitors, antiapoptotic bcl-2 proteins [54] are currently under various clinical and preclinical stages of development for lung cancer treatment [53,55].
Downregulated expression of schlafen family member 11 (SLFN11), a member of the S-phase checkpoint, was found in the patient-derived xenograft (PDX) resistance model of SCLC [56,57]. SLFN11 is a relevant predictive biomarker of sensitivity to poly-ADP ribose polymerase (PARP) inhibitor monotherapy in SCLC, and its targeting can be a promising strategy to overcome resistance [57]. Inhibition of the cell cycle checkpoint kinase 1 (CHK1) was determined to have efficacy in platinum-resistant SCLC cells in vitro and in vivo [58,59]. Notch signaling is another important neuroendocrine stem cell signaling pathway. Cells with amplified Notch signaling are more chemoresistant than those undergoing more rapid expansion, suggesting notch signaling could enhance chemoresistance [60,61]. In a preclinical model, the inhibition of notch signaling in combination with chemotherapy increased the apoptosis of SCLC cells [60].
Geisslinger et al. demonstrated that lysosomal function interference might be an auspicious tactic in enabling sensitization to chemotherapy. Lysosomal function inhibition could target P-glycoprotein-driven chemoresistance, which might give rise to lysosome-targeted adjuvants in the future [62]. Zhan and colleagues successfully developed a new autophagy inhibitor, alpha-hederin, that changes lysosomal pH and inhibits the lysosomal maturation of cathepsin D [22]. The buildup of undigested material leads to the accumulation of reactive oxygen species (ROS), consequently enhancing its killing effect on tumor cells [22,63]. These mechanisms make alpha-hederin an effective agent in overcoming resistance to paclitaxel in NSCLC [64]. Additionally, the induction of sphingosine kinase-1 (SphK1) by insulin-like growth factor 1 (IGF1) was found to increase the tolerance of NSCLC cells to paclitaxel treatment, while pharmacological suppression of SphK1 restored paclitaxel sensitivity [65]. Similarly, epigenetic modifications play an important role in the regulation of DNA-mediated events, including transcription, DNA repair, and replication [66]. Aberrant regulation of such events promotes tumor formation, progression, and chemotherapy resistance. For example, the hypermethylation of the IGFBP3 promoter, and upregulation of forkhead box F1 (FOXF1) expression was found to trigger resistance to cisplatin and the acquisition of cancer stem cell (CSC)-like phenotypes in NSCLC cells [67].
Furthermore, increased expression and activation of WNT/b-catenin signaling was found to cause chemoresistance [68,69,70,71,72]. One in vitro study demonstrated that a protein kinase c (PKC) inhibitor, GF109203X, inhibits WNT5A-induced cell migration, invasion, and clonogenicity in A549 and A549/DDP (diammine dichloro platinum) lung cancer cells. This signifies the role of WNT5A in promoting lung cancer cell movement through WNT/PKC non-canonical pathway activation [73,74]. Gardner et. al. reported that the gene coding for twist family transcriptional factor (TWIST1) was upregulated in chemoresistant cells [75]. This enhanced TWIST1 expression is correlated with acquired drug resistance, epithelial-to-mesenchymal transition (EMT), metastasis, and stemness [76,77,78,79]. TWIST1 is a WNT-inducible transcription factor that relates to the dysregulation of WNT signaling detected in clinical samples and SCLC cell lines [80]. Therefore, targeting molecules involved in the WNT pathway could be a promising strategy to overcome chemotherapy resistance. Cisplatin or cis-diamminedichloroplatinum(II) (CDDP) resistance can be stimulated by variations in numerous intracellular pathways involving miRNAs. MiRNAs are a family of non-coding RNAs that regulate gene expression via sequence-specific targeting of mRNAs [81,82]. During the process of lung cancer development, miRNAs can operate as tumor suppressor genes or oncogenes. Hua and his colleagues found that overexpression of one such miRNA, miR-1, improved CDDP sensitivity of NSCLC cells through ATG3-mediated autophagy inhibition, providing a possible therapeutic target for reducing chemoresistance [83]. miR-106a, miR-31, miR-15b, miR-27a, miR-223, miR-205, miR-92b, and miR-224 promote resistance to cisplatin by downregulating the expression of adenosine triphosphate-binding cassette transporter A1 (ABCA1), adenosine triphosphate-binding cassette subfamily B member 9 (ABCB9), phosphatidylethanolamine-binding protein 4 (PEBP4), Raf kinase inhibitory protein (RKIP), F-box/WD repeat-containing protein 7 (FBXW7), phosphatase and tensin homolog (PTEN), and p21, respectively [84,85,86,87]. Altogether, studies show that targeting dysregulated miRNAs may be a promising strategy for enhancing therapeutic effectiveness, or overcoming drug resistance in lung cancer patients [88,89]. Other mechanisms of chemoresistance include metabolic reprogramming, communication between tumor cells and the surrounding TME, and the alteration of microtubules [38,90,91,92,93]. A better understanding of interactions mediating chemotherapy resistance will allow the discovery of novel targets to delay resistance onset and/or resensitize tumors to existing treatments.
3. Mechanism of Radiotherapy Resistance in Lung Cancer
Radiotherapy (RT) is one of the main lung cancer treatments and is effective for almost half of all cancer patients [106,107]. RT includes internal radiation therapy (brachytherapy) and external beam radiation therapy (EBRT). EBRT includes 3-D conformal radiation therapy (3-D CRT), stereotactic body radiation therapy (SBRT), proton therapy, prophylactic cranial irradiation (PCI), hypofractionated radiation therapy, and intensity-modulated radiation therapy (IMRT) [108,109,110,111,112,113,114,115,116]. Despite the use of RT for lung cancer treatment, unfortunately, the therapeutic outcomes are not always satisfactory, and tumor radioresistance can lead to the reduction in the efficiency of RT, resulting in tumor recurrence and metastasis [106,117]. Thus, it is necessary to investigate the molecular and cellular mechanisms responsible for the loss of radiosensitivity and discover potential therapeutic targets that might help overcome radioresistance.
3.1. Targeting Signaling Pathways Associated with Radioresistance and Potential Strategies for Radiosensitization in Lung Cancer
Diverse pro-survival and metastatic signaling pathways mediate cancer cells’ survival [117]. Genetic alterations of the PI3K, AKT, PTEN, EGFR, and KRAS genes, MET amplification, and EML4-ALK rearrangements are associated with lung cancer progression [118]. Moreover, radiation is linked to the dysregulation of these pathways such as the hyperactivation of PI3K/AKT, which induces RAC expression and activity, increases levels of EMT markers, and promotes invasive phenotypes and metastasis [117,119]. Furthermore, AKT may also contribute to radioresistance by promoting double-strand DNA break (DSB) repair [119]. Additionally, upregulation of gelsolin, a protein involved in cytoskeleton remodeling, is associated with the activation of PI3K/AKT signaling and promotion of radioresistance in NSCLC cells. Cancer cells overexpressing gelsolin showed reduced apoptosis, and decreased levels of cleaved caspase-3 and PARP after irradiation [120]. Diverse studies have focused on targeting these signaling pathways to overcome radioresistance. For example, downregulation of AKT and ERK via vascular endothelial growth factor receptor 2 (VEGFR2) inhibition can enhance radiosensitivity by increasing radiation-induced G2/M phase arrest and inhibiting radiation-induced DSB repair in NSCLC cells [121]. mTOR-dependent expression of hypoxia inducible factor 1 α (HIF1-α) was also linked to proliferation and cancer cell survival under hypoxic conditions. Inhibition of mTOR can decrease HIF1-α expression and restore radiation sensitivity in lung adenocarcinoma cells [122]. In addition, inhibiting RAC1, PI3K, MEK, and AKT overexpression can enhance radiation sensitivity by blocking DSB repair [117,119].
Cancer cells maintain a high redox level reflected by an increased ROS production and an activated antioxidant defense system equilibrium, which promotes neoplastic growth. Low and moderate levels of ROS can induce cancer cells’ proliferation and survival by post-transcriptional modifications of diverse proteins and kinases [123]. RT anticancer effects depend on the promotion of ROS accumulation, which causes cytotoxic oxidative stress [124]. However, radiation exposure may increase ROS and mitochondrial dysfunction, which are associated with pro-survival pathways and radio-adaptive resistance. Thus, ROS can mediate the cytotoxic effect of RT but also regulate the pro-survival adaptive response and induce radioresistance mainly due to the redox compensatory mechanisms in cancer cells. While ROS-mediated RT may eliminate the majority of cancer cells, the enhanced antioxidant capacity of cancer cells may allow some of them to survive the elevated ROS environment and induce cancer relapse and progression [124,125]. Low-dose ionizing-radiation can promote elevated ROS production inducing autophagy and activation of the Nrf2-HO-1 antioxidant pathway in lung adenocarcinoma cells [126]. Moreover, mutations in Keap1 are associated with Nrf2 constitutive activation in cancer cells and radioresistance. Nrf2 is also involved by redirecting glucose and glutamine to the serine, glutathione, and purine nucleotides synthesis pathways [127]. Thus, targeting glutaminase inhibition can radiosensitize KEAP1 mutant cells [128]. Furthermore, several studies have focused on plant-derived compounds due to their antineoplastic potential and low toxicity. For instance, ferulic acid was reported for its antioxidant and anti-inflammatory activities, and for its protective effect against gamma radiation-induced DNA damage. Ferulic acid treatment prior to gamma radiation increased already elevated ROS levels, inhibited the ROS-PI3K/Akt-p38 MAPK-NF-kB-MMP-9 pathway, and supported mitochondrial apoptotic pathway activation and cell cycle progression inhibition in cancer cells promoting their radiosensitization [123]. Therefore, targeting ROS can constitute a potential strategy to overcome radioresistance in lung cancer.
Lung cancer cells can acquire radioresistance through a mechanism of EMT [129]. Transcription factors Snail, Slug, and twist-related protein 1 (TWIST1) are frequently upregulated during the transition, with associated changes to EMT-related biomarkers such as E-cadherin, N-cadherin, and vimentin [78,130,131,132]. Cadherins such as E-cadherin and N-cadherin are components of adherens junctions between cells, along with catenins such as β-catenin. During EMT, the expression of N-cadherin in place of E-cadherin, along with the increased expression of intermediate filament protein vimentin, results in decreased cell–cell adhesion and changes in adhesion to the extracellular matrix, altering regulatory pathways such as contact inhibition and aiding in migration [133]. Understanding the underlying regulatory mechanisms of the EMT offers promising new targets to prevent or reverse its effects and overcome radioresistance. For example, β-Elemene, an inhibitor of the Prx-1/NF-kB/iNOS signaling pathway, radio-sensitized radioresistant NSCLC cells, decreased expression of N-cadherin and vimentin, and increased E-cadherin expression [134,135]. In another study, inhibition of chemokine (C-X-C motif) receptor 4 (CXCR4) in NSCLC decreased radioresistance, while overexpression increased it [136]. CXCR4 interacted with STAT3, an activator of Slug [136,137]. Inhibition of tescalcin (TESC), a protein in the TESC/c-Src/IGF1R signaling pathway, interfered with EMT and radio-sensitized NSCLC [138]. TESC may increase the expression of aldehyde dehydrogenase isoform 1 (ALDH1) via the activation of STAT3 [138]. RAD001, an inhibitor of the mTORC1 signaling pathway, inhibited EMT and radio-sensitized NSCLC [139]. E-cadherin expression levels increased while the expression of vimentin decreased when mTORC1 signaling was inhibited [139]. Treatment with EG00229, an inhibitor of neuropilin 1 (NRP1) binding to VEGF, radio-sensitized adenocarcinoma cell lines and reduced N-cadherin and vimentin, while NRP1 overexpression increased them. NRP1′s effect on EMT could result from the PI3K/AKT/mTOR, IL6/STAT3, or SDF-1/CXRC4 signaling pathways [140]. The silencing of C2 domain-containing phosphoprotein (CDP138) overcame radioresistance in NSCLC, and targeting growth differentiation factor 15 (GDF15) signaling, which may alter TGF-β/Smad signaling, resulting in increased Snail expression and EMT [141]. TWIST1 expression made NSCLC more resistant to radiation, while treatment with F-Box and Leucine Rich Repeat Protein 14 (FBXL14) destabilized TWIST1, radio-sensitizing the treated cells. FBXL14 expression levels had a negative correlation with EMT markers [142]. Taken together these studies suggest that targeting regulatory pathways associated with Snail, Slug, and TWIST1 to interfere with EMT could prevent radioresistance.
3.2. miRNAs in Radioresistant Lung Cancer Cells
miRNAs participate in many cellular function and is associated with radiotherapy process [143,144]. However, the deregulation of miRNAs expression can promote radioresistance in NSCLC by inhibiting the essential functional proteins involved in the radiation treatment response [145,146]. In recent studies focused on the role of miRNAs in lung cancer radioresistance, miR-145 was found to enhance radiosensitivity in NSCLC by targeting TMOD3 mRNA. Overexpression of miR-145 [147] was suggested as a potential strategy to increase the effectiveness of RT and sensitize radioresistance in lung cancer cells. Similarly, overexpressing miRNA-9 and miR-328-3p can enhance the sensitivity to RT in NSCLC cells [148,149]. Likewise, upregulation of miRNA-320a acts as an inhibitor of radioresistance in NSCLC by suppressing HIF1α and increasing PTEN methylation [144].
A study conducted in 2021 by Xue et al. clarified that miR-129-5p transfection into NSCLCs induces apoptosis, cell cycle arrest, and DNA injury, and can radio-sensitize NSCLCs by targeting SOX4 and RUNX1 [150]. Overexpressed FOXO3 is the target for miR-182 to increase radioresistance. Therefore, knocking down miR-182 can result in cell cycle arrest without changing the DNA damage repair system [151]. In addition, knocking down oncomiRNA, miR-410, can reduce DNA damage repair by targeting PTEN/PI3K/mTOR [152]. Overall, targeting different miRNAs in lung cancer appears to be a promising approach to overcome radioresistance.
3.3. DNA Damage Associated with Radioresistance in Lung Cancer
DNA damage is one of the major causes of radioresistance in lung cancer [153]. Ubiquitin-specific protease 14 (USP14) acts as a regulator [154] in double strand breaks (DSBs), which affects both non-homologous end-joining (NHEJ) and HR [155,156]. Knocking down USP14 by using short hairpin RNA (shRNA) showed a notable increase in the radiosensitivity of NSCLCs [154].
In another study, upregulation of serine proteinase inhibitor clade E member 2 (SERPINE2) and Sirtuin 3 acts as a regulator of radiosensitivity in lung cancer and is directly involved in the DNA repair mechanism by facilitating the phosphorylation of HR-mediated DSBs’ repair. Knocking down SERPINE2 in radioresistant cells made them more radiosensitive [157,158]. Moreover, knocking down Sirt3 can arrest the cell cycle and activate the ATM-Chk2 pathway over irradiation [158]. Transfecting an integrin beta-1 (ITGB1) short hairpin RNA (shRNA) increased radiation-induced DNA damage and arresting of the G2/M phase. The downstream effector of ITGB, Yes-associated protein 1 (YAP1), is suppressed by ITGB and it can induce radioresistance by affecting DNA repair, while inhibiting ITGB1 can help with radiosensitivity [159]. Moreover, activation of the A2B receptor promotes the recovery of irradiated lung cancer cells from DNA damage by the mediation of the γ-radiation-induced translocation of EGFR and phosphorylation of src and EGFR, while A2B inhibition is a therapeutic approach to make cancer cells radiosensitive [160]. Therefore, learning more about DNA damage-related mechanisms and pharmacologically inhibiting them can be a potential strategy to overcome radioresistance in lung cancer cell lines.
4. Targeted Therapy Resistance in Lung cancer and Overcoming Strategies
Targeting oncogenic driver alterations remains a potent and effective therapeutic approach, especially for patients with NSCLC subtypes [161,162]. EGFR and ALK inhibitors have become the mainstays of treatment in lung cancer therapy, while in recent years a new class of drugs has been able to target the once “un-druggable” KRAS mutation [163,164,165]. While targeted therapies might initially be effective for patients, chronic drug exposure leading to further alterations in these oncogenic drivers significantly reduces treatment efficacy [166]. In this section, we will discuss common resistance mechanisms to targeted therapies and strategies to overcome treatment resistance.
4.1. Overcoming EGFR TKI Resistance
More than 30% of all NSCLC patients have EGFR positive tumors, and patients with EGFR positive tumors are overwhelmingly female, non-smokers, and Asian [167]. Tyrosine kinase inhibitors (TKIs) that target EGFR mutations are, at least initially, an effective treatment for these patients. These include the first-generation reversible EGFR TKIs gefitinib and erlotinib, the second-generation irreversible TKIs afatinib and dacomitinib, and the third-generation irreversible TKI osimertinib [168].
Resistance to EGFR TKIs can be on-target (also known as EGFR-dependent) or off-target (also known as EGFR-independent) [169]. The most common acquired resistance mechanism following first-line treatment with first- or second-generation EGFR TKIs is the T790M mutation [170]. However, the T790M mutation does not affect responsiveness to osimertinib, a third-generation TKI [170]. Interestingly, osimertinib is effective both as a second-line treatment for previously treated EGFR positive tumors with acquired T790M mutation and as a first-line treatment for EGFR positive, advanced NSCLC [171]. The most common resistance mechanism to osimertinib is acquired C797S mutation [172], which spells the end of effective treatment with available EGFR TKIs for patients.
Notably, allosteric kinase inhibitors represent a fourth generation of EGFR TKIs that can overcome osimertinib resistance. JBJ-04-125-02, an allosteric kinase inhibitor, is a L858R-specific mutant-selective allosteric EGFR inhibitor that shows efficacy against EGFR positive C797S mutant NSCLCs as a single-agent in both in vitro and in vivo models [173]. The use of JBJ-04-125-02 in combination with osimertinib enhanced the binding ability of JBJ-04-125-02 and increased antitumor efficacy in mouse models [173]. This combination limited EGFR-dependent resistance mechanisms and delayed therapeutic resistance in vitro and in vivo [173]. JBJ-04-125-02 is among a new class of allosteric inhibitors that hold promise for overcoming C797S mutants [173].
Novel mechanisms by which EGFR resistance may be delayed and/or EGFR mutants may be resensitized to TKIs have also been explored. Targeting GRB2, an EGFR-binding adaptor protein, alongside the use of the EGFR TKI, icotinib, has been shown to delay resistance to EGFR TKIs in cancer cell lines and mouse models. Lymecycline, a derivative of the antibiotic tetracycline, was shown to target GRB2 and reverse resistance to icotinib in NSCLC cell lines. In mouse models, the addition of lymecycline to icotinib treatment produced a synergistic effect with no significant increase in toxicity [174]. Additionally, the enzymatic activity and expression of EHMT2 are upregulated in NSCLC cells [175]. The inhibition of EHMT2, a histone lysine methyltransferase, was shown to restore erlotinib sensitivity in resistant cancer cells. Combination of an EHMT2 inhibitor and erlotinib further enhanced antitumor effects in an EGFR TKI-resistant NSCLC mouse model [175].
EGFR-independent resistance includes MET amplification and HER2 amplification [169]. Normally expressed by stem and progenitor cells, MET amplification correlates with poor prognosis. HER2, also a common biomarker for breast cancer, is part of the EGFR family and can mediate resistance to TKIs as well. The HIF-1 inhibitor YC-1 was shown to resensitize the human LUAD cell line (HCC827) with acquired resistance with MET amplification to gefitinib, a first-generation EGFR TKI. The HIF-1 pathway allows cancer cells to survive in hypoxic conditions through transcriptional activation of the genes needed for survival and growth [176].
Additionally, insights into the emergence of EGFR TKI resistance present possible therapeutic targets. Heme levels were found to be elevated in osimertinib-resistant EGFR-mutant NSCLC cell lines and in the blood plasma of osimertinib-treated EGFR-mutant NSCLC patients [177]. Notably, plasma heme levels were most elevated in patients experiencing progression-free survival (PFS) of less than 15 months, as opposed to those having PFS > 15 months [177]. Our lab has previously shown that elevated heme synthesis and import underpin tumorigenic functions, and that heme sequestration effectively suppresses tumor growth and progression in NSCLC mouse models [178,179,180]. Thus, it is possible that heme plays a role in EGFR-dependent resistance pathways and targeting heme can be a viable strategy to overcome this resistance.
4.2. Overcoming ALK Drug Resistance
Anaplastic lymphoma kinase (ALK) gene rearrangements are a major hallmark of lung cancer. Aberrations in this gene, which codes for a protein tyrosine kinase, promote cancer proliferation and survival. The fusion of ALK with echinoderm microtubule-associated protein like-4 (EML4) gene creates the fusion gene EML4-ALK, which is the most observed ALK fusion in lung cancer [181,182]. ALK mutations are mutually exclusive with EGFR and KRAS mutations in many patients, positioning ALK as the primary target for treatment in ALK-positive lung cancers [183].
ALK inhibitors posed a breakthrough advancement in NSCLC treatment, as the standard first-line treatment was systemic chemotherapy before advancements in ALK inhibitors [184]. The first generation ALK inhibitor crizotinib, receiving accelerated approval by the FDA in 2011 for metastatic NSCLC, showed a median of 7.7 months PFS versus 3.0 months in chemotherapy controls pemetrexed or docetaxel in a phase III clinic trial A8081007 [185,186]. While this posed a major improvement in the treatment of ALK-positive tumors, most patients went on to develop resistance 1–2 years after treatment [187]. Primary resistance is characterized as a refractory response to initial treatment, likely attributed to different fusion variants [187]. Secondary resistance, or acquired resistance, falls into ALK dominant and ALK non-dominant categories. In ALK dominant secondary resistance, there is a mutation that prevents inhibition of the targeted tyrosine kinase. In ALK non-dominant resistance, there is a development of other mutations, such as EGFR, KRAS, or KIT amplification, which bypasses ALK [187].
The second generation ALK inhibitor ceritinib was developed as an oral ALK inhibitor 20 times more potent than crizotinib [188]. Ceritinib is effective for patients with developed resistance against crizotinib and was thus first approved for refractory NSCLC after crizotinib treatment [187]. Another second-generation ALK inhibitor, alectinib, displayed activity against L1196M mutations, which leads to resistance against crizotinib [189]. It was also approved for patients with progression on or after crizotinib. Similarly, brigatinib was developed as an additional second-generation ALK inhibitor with similar efficacy against L1196M mutations, as well as EGFR T790M mutations [187].
However, resistance soon emerged against these next generation TKIs, so third-generation lorlatinib was developed as an ALK and ROS1-inhibitor designed to target the driver mutations of crizotinib and second-generation ALK inhibitors [184]. In clinical trials, lorlatinib displayed greater PFS compared to crizotinib, positioning itself as a preferred first-line treatment against ALK-positive NSCLC [190,191]. Ensartinib, a second-generation small molecule ALK inhibitor, was created to target central nervous system (CNS) metastases [192,193]. Entrectinib, approved for neurotrophic tyrosine receptor kinase (NTRK) and ROS-1 NSCLC in 2019, targets ALK aberrations and can additionally cross the blood–brain barrier [192].
While second- and third-generation ALK inhibitors helped to overcome single mutation ALK resistance, double mutant ALK resistance seems inevitable [194]. Fourth-generation ALK TKIs are being developed that target double ALK-resistant mutations to help overcome drug resistance. Even so, double and triple mutation may develop against 4G ALK TKIs, but would still likely achieve a minimum of 35–40 months of PFS [194]. Off-target resistance mechanisms such as EGFR TKIs, including parallel bypass mechanisms such as MET amplification or RET rearrangement, or downstream signaling pathways such as BRAF fusions and MAP2K1 mutations, among several others, may occur [195]. Other off-target resistance mechanisms such as histological transformations to SCLC or EMT have also been observed after treatment with both EGFR and ALK TKIs, although the exact molecular mechanisms are unclear [195].
4.3. Strategies to Overcome Resistance to KRAS G12C Inhibitors
KRAS is the most common genetic alternation in NSCLC, occurring in 20–40% of LUADs [196]. KRAS is part of the RAS family of GTPases that play important roles in cell proliferation and survival, with KRAS being the most common RAS mutation in cancer constituting 85% of RAS mutations in cancer [197]. While KRAS has been an attractive target for anticancer therapies, it has remained elusive as attempts to inhibit KRAS have been hindered by the high affinity of RAS to bind GTP as well as a smooth structure with no obvious pockets for inhibitor binding. After many failures, two KRAS inhibitors have shown exciting results against the G12C KRAS variant, which occurs in nearly half of NSCLC KRAS mutations: sotorasib (Amgen) and adagrasib (Mirati Therapeutics). KRAS G12C inhibitors bind in the switch II pocket, locking KRAS into the inactivated state [198]. In clinical trial “KRYSTAL-1” in NSCLC, adagrasib showed a median 12.6-month OS, indicating strong clinical efficacy, with similar results observed for sotorasib in the “CodeBreaK100” study showing a median OS of 12.5 months [199,200].
The emergence of resistance is inevitable, as seen by preclinical and clinical data, due to high inter and intratumoral heterogeneity in lung cancer [201]. There are three main molecular mechanisms of resistance: on-target mechanisms, off-target mechanisms, and histological transformation [202]. Treatment with adagrasib was shown to increase acquired KRAS mutations or amplify bypass mechanisms such as MET amplification. In NSCLC, RAS-MAPK activation is a bypass mechanism due to mutations in the RAS-RAF-MEK-ERK pathway [202]. Another possible strategy for acquired resistance to KRAS G12C inhibitors could be to switch between sotorasib or adagrasib, although this may be ineffective for Y96D and Y96S mutations [202]. Cell line studies in BA/F3 cells showed that using BI-3406, a SOS1 inhibitor, or TNO 155, a SPH2 inhibitor, could overcome resistance against these mutations when used with KRAS G12C inhibitors [202].
Mitochondrial targeting could additionally serve as a strategy to overcome KRAS resistance. Apoptosis-inducing factor (AIF) deletion in KRAS G12D mouse lung cancer has been shown to lead to increased survival by leading to decreased oxidative phosphorylation (OXPHOS) and increased glycolytic activity [203]. This evidence is corroborated in human NSCLC patients where AIF expression has been shown to be associated with worse outcomes, as well as other studies showing the importance of mitochondrial activity and OXPHOS in both NSCLC and SCLC tumor progression [180]. In KRAS-driven colorectal cancers, mitochondrial inhibitors, such as tigecycline, have been shown to reduce tumor growth in vivo, which suggests that this combination may yield positive results in lung cancers [204]. This evidence suggests that co-targeting of mitochondria may be an effective strategy in overcoming KRAS resistance.
5. Mechanism of Immunotherapeutic Resistance and Overcoming Strategies
Cancer immunotherapy is one of the most attractive therapeutic options over traditional therapies including chemotherapy, targeted therapy, and RT because of its promising clinical responses [205]. It targets the host immune system to make it fight against cancer cells and possesses promise to restore antitumor immunity [206]. Currently, various types of immunotherapies including adoptive T-cell therapy, cancer vaccine, ICIs, and cytokine modulators are approved by the Food and Drug Administration (FDA) against different types of cancer [207,208]. The use of ICIs directed against ICPs has showna stable response, long-term survival benefits, and increased PFS [209,210,211] in NSCLC patients. It is now considered as the first line of treatment alone or in combination with surgery, chemotherapy, and RT in patients with NSCLCs [212]. The FDA has approved immunotherapeutic drugs named as nivolumab, pembrolizumab, atezolizumab, and durvalumab to treat NSCLC patients [213]. These drugs, known as ICIs, inhibit PD-1 expression on the surface of T cells and PD-L1 overexpression on tumor cells, preventing the binding between PD-1/PD-L1, and restoring antitumor immunity [213]. However, resistance to ICIs either as primary or acquired resistance is commonly found in many patients [214,215] based on PD-L1 expression, where patients do not show any response to ICIs or develop resistance after 8–10 months of clinical benefit, respectively. Unfortunately, reduced expression of PD-L1 and major histocompatibility complex (MHC) proteins, lower levels of effector T cells, and a higher number of immune suppressor cells represent limited antitumor responses to ICIs in SCLC patients [216]. Therefore, it is necessary to study and target these resistance mechanisms that are summarized in Table 2 to resensitize cancer cells to immunotherapy and develop novel approaches for overcoming immunotherapeutic resistance.
Table 2.
Summary of mechanism of immunotherapeutic resistance and prospective targets in lung cancer.
| Resistance Mode | Action | Target | References |
|---|---|---|---|
| Gene mutations | a. Modify the expression of PD-1, PD-L1, and CTLA-4 proteins b. Deregulate PD-1/PD-L1 signaling pathways |
ALK, EGFR, HER-2, CDK2NA, STK11 (LKB1); TP53; KRAS | [219,221,226,227] |
| Dysregulation of cellular and molecular pathways | a. Promote primary and adaptive resistance to anti-CTLA-4 and anti-PD-1 b. Enhance cancer cell proliferation and metastasis |
Wnt/B-catenin, JAK/STAT3, PI3K-Akt, JAK1/2 mutations, IFN-γ signaling pathways | [215,222,224] |
| Neo-angiogenesis | a. Inhibit the infiltration of effector immune cells b. Upregulate the expression of PD-L1 c. Recruit Treg, TAM, and MDSC cells d. Impair the delivery of therapeutic agents to tumor cells e. Reduce adhesion molecules into TME |
Hypoxia, HIF1-A, VEGFA, VEGFR, Angiopoietin-2 (ANG2) | [228,229] |
| High oxidative metabolism | a. Trigger hypoxia b. Promote cancer cell growth, proliferation, and metastasis c. Create immunosuppressive TME d. Affect effector T cells |
OXPHOS complexes, heme, HIF1-A, VEGFA, VEGFR | [179,180,230,231,232] |
| Immunosuppressive TME | a. Recruit immunosuppressive cells (Tregs, Bregs, MDSCs, TAM, and CAF) b. Inhibit the infiltration of the effector immune cells c. Release of proinflammatory molecules d. Upregulate immune checkpoint proteins (ICPs) e. Affect antitumor immunity |
Alternative ICPs, immunosuppressive molecules, proinflammatory molecules, VEGFA, HIF1-A | [228,233,234] |
| Upregulation of alternative immune checkpoints | a. Modulate TME and show adaptive resistance to anti-PD-1 | LAG-3, TIGIT, TIM3, and TIM-1 | [228,234] |
| Deregulated epigenetics | a. Modify the expression of immune related genes b. Triggers T-cell dysfunction |
DNA methyl transferase; histone methyl transferase; histone deacetylase | [215,218] |
| Dysregulated circRNAs | a. Upregulate PD-L1 b. Recruit inflammatory molecules c. Inhibit the CD8+ T cells’ infiltration into tumorigenic regions |
hsa_circ_0000190, hsa_circ_0079587, circFGFR1, circUSP7 | [235,236,237,238,239] |
| Modified gut microbiota | a. Reduce effector T cells b. Increase regulatory T cells c. Affect antitumor responses |
Gut microbiota composition; gut bacteria | [240] |
Targeting Immunoresistance Mechanism to Resensitize Lung Cancer Cells to Immunotherapy
Gene mutations, modified TME, tumor mutational burden (TMB), the DNA mismatch repair (MMR) pathway, and altered epigenetics are reported as major drivers for modifying immunotherapeutics (Table 2) and promoting immunotherapy resistance [215,217,218]. Inadequate tumor immunogenicity associated with a low TMB, gene mutation, the lack of antigen presentation and PD-L1 expression, and mutations in the PI3K-Akt, IFN, and Wnt/B-catenin signaling pathways are considered as tumor intrinsic immunoresistance mechanisms, while immunosuppressive TME, epigenetic modifications, and the expression of alternative immunocheckpoints are associated with tumor extrinsic immunoresistance mechanisms [215].
It has been found that mutations in cancer driver genes, KRAS, EGFR, ALK, human epidermal growth factor receptor 2 (HER2), STK11, CDKN2A, TP53, etc. [7], dysregulate the expression of the PD-1 and PD-L1 and PD-1/PD-L1 signaling pathways, which are associated with resistance in immunotherapy [219,220,221]. The reversing of [219] STK11 mutations by knocking down the STAT3 gene was shown to improve the anti-PD-L1 and anti-cytotoxic T-lymphocyte-associated antigen (CTLA-4) resistance in NSCLCs. Different types of mutated signaling pathways including Wnt/B-catenin, JAK/STAT3, PI3K-Akt, interferon gamma (IFN-γ) signaling pathways, and mutations in Janus kinase (JAK1/2) accelerate resistance to anti-PD-1 [222], RT plus anti-CTLA4 [223], anti-CTLA4 [224], and anti-PD-1 [225] therapy, respectively, which are essentially needed to be considered for overcoming resistance to ICIs [215]. The upregulated PI3K-Akt signaling pathway reduces the function of CD8+ T cells by promoting the recruitment of immunosuppressive cells into TME, the expression of VEGF, and PD-L1 expression [215].
Alterations in the MMR system lead to the formation of microsatellite instability (MSI), short tandem repeat sequences, which are highly immunogenic and display high TMB neoantigen [241]. TMB, which is defined as the total number of somatic mutations found in the genome of cancer cells, works as an independent predictor for analyzing the outcome of the treatment to ICIs [242]. According to FDA, TMB ≥ 10 is considered—a good predictor of the immunotherapy response. A higher mutation burden in the genome of cancer cells leads to the increased possibility of producing neoantigens that can be targeted by ICIs to neutralize tumor cells [242]. CD8+ tumor-infiltrating lymphocytes (TIL) are reported to be elevated in MMR-deficient (dMMR) cancer and this dMMR shows a positive impact such as a stable response, OS, and PFS on immunotherapy [241,243]. This positive correlation was also observed between dMMR and the response to ICIs from a retrospective analysis conducted in NSCLC patients treated with nivolumab, which suggests the analysis of the MMR system improves immunotherapy [244].
Various cells found in TME such as tumor-associated macrophages (TAMs), regulatory T cells (Tregs), B regulatory cells (Bregs), cancer-associated fibroblasts (CAFs), and myeloid-derived suppressor cells (MDSCs) suppress immune responses and exhibit resistance to immunotherapy in many ways [228]. For instance, these cells block the activity of effector CD4+ and CD8+ T cells and release immunosuppressive molecules and angiogenic factors, such as transforming growth factor beta (TGF-β), interleukin 10 (IL-10), prostaglandin E2, and VEGF, respectively. These cells upregulate the expression of ICPs such as PD-1, PD-L1, and CTLA-4 as well as the expression of alternative ICPs, lymphocyte-activation gene 3 (LAG-3), and T-cell immunoglobulin mucin-3 (TIM-3). These events consequently trigger immunotherapeutic resistance [228,233,234] by turning immunosupportive TME into immunosuppressive TME.
Neo-angiogenesis, the formation of new blood vessels by tumor cells, is one of the hallmarks of cancer that enhances cancer cell growth, proliferation, and metastasis. The emergence of tumor vasculature from existing blood vessels affects regular blood flow, oxygen levels, and nutrient levels in TME [245]. This neo-vasculature induces the expression of angiogenic factors and VEGF, creates hypoxia, and recruits immunosuppressive cells (Treg, MDSC, CAF, and TAM) into TME, which causes immunosuppressive TME [246]. It has been found that angiogenic factors upregulate downstream signaling pathways involved in cancer cell proliferation, reduce adhesion molecules leading to the inhibition of the infiltration of effector T cells into TME, and impair the delivery of therapeutic agents into tumor cells [229]. Thus, the inhibition of neo-angiogenesis is promising to amplify the efficacy of immunotherapeutic agents.
Notably, cancer cells depend on enhanced mitochondrial energetic metabolism for ensuring high energy and oxygen to support their growth, proliferation, and metastasis [247]. High oxidative metabolism accompanied with oxygen consumption [247] creates hypoxia, which, in turn, activates HIF-1 signaling pathways, affects vasculature by triggering the release of VEGF, increases immunosuppressive cells, and reduces effector T cells [231]. All these events triggered by hypoxia modify TME, reduce immunotherapeutic efficacy, and trigger resistance to ICIs [231,232]. Huang et al. targeted mitochondria using atovaquone, which inhibited the expression of OXPHOS genes and lowered granulocytic-MDSCs and Treg cells [230]. This approach increased the number of tumor infiltrating CD4+ T cells and accelerated responses to anti-PD-1 therapy in lung cancer. Interestingly, heme sequestering peptide 2 (HeSP2) was shown to reduce OXPHOS levels and angiogenesis and improve hypoxia by normalizing HIF1A, VEGFA, and VEGFR1 in in vivo mouse models [179,180]. Therefore, targeting high oxidative phosphorylation and hypoxia might be a potential strategy for overcoming immunotherapeutic resistance.
Deregulated epigenetics promote immunotherapeutic resistance through modifying the expression of immune related genes and triggering immune suppressive phenotypes and dysfunctional T cells [215,218]. In a study conducted in NSCLC patients with cancer progression, the combination of Entinostat (ENT), a histone deacetylase inhibitor, and pembrolizumab showed synergistic and antitumor effects in phase II trials compared to anti-PD-1 treatment alone [248]. Therefore, using epigenetic inhibitors in combination with ICIs could be promising strategies for overcoming limitations in immunotherapy in lung cancer.
Multiple types of circular RNAs (circRNAs), for instance, hsa_circ_0000190 [236], hsa_circ_0079587 [237], circFGFR1 [238], circUSP7 [239], etc., have been found to be associated with promoting tumor progression, metastasis, immune evasion, and immunotherapy resistance [235]. These circRNAs provoke resistance to anti-PD-1 therapy by upregulating PD-L1 expression, targeting CXCR4, and inhibiting the infiltration of CD8+ T cells, which supports the necessity of targeting circRNAs to resensitize tumor cells to immunotherapy.
Gut microbiota composition is one of the factors that affect responses to immunotherapy and make tumor cells resistant to ICIs [249,250]. It worked as a good predictor to analyze the immunotherapeutic efficacy towards anti-PD-1 treatment in a study conducted on Chinese NSCLC patients [251]. Lung cancer patients, having low levels of the bacterium Akkermansia muciniphila in the gut due to antibiotic consumption, showed resistance to anti PD-1 treatment [240,249]. Huang et al., used ginseng polysaccharides (GPs), which is an extract of Panax ginseng, in combination with αPD-1 monoclonal antibody (mAb) to target gut microbiota in lung cancer mice models. They found that this combination significantly enhanced effector T cells and reduced Foxp3+ regulatory T cells, resulting in an improved antitumor response [240]. Therefore, targeting gut microbiota and analyzing its composition could be a promising approach for enhancing the efficacy of anti-PD-1/anti-PDL1 and overcoming resistance to immunotherapy in lung cancer cells.
6. Combination Approaches for Improving Therapeutic Resistance and Future Prospects
Although there have been many improvements in the treatment options for lung cancer, the evolution of resistance in therapy challenges the clinical outcomes of patients and reduces OS [16]. Recent advances in immunotherapy have revolutionized the landscape of clinical therapy in NSCLC. The FDA has already approved ICIs, anti–PD-1 and anti–PD-L1 antibodies, for the treatment of NSCLC. Despite the advancement in clinical outcomes, patients eventually fail to respond to immunotherapy due to the emergence of primary or secondary resistance. Therefore, combinations of immunotherapy with chemotherapy drugs or treatment combinations with radio and targeted therapy have been explored for better treatment outcomes, which are mentioned in Table 3. Given that immunotherapy drugs, targeted therapy drugs, and chemotherapy drugs act on different targets and cells, synergistic or combined treatment of these therapies or irradiation may achieve greater therapeutic effects at the cost of lower or similar side effects (Figure 2). Currently, a rising number of clinical trials are in progress to further explore new regimens as monotherapy or in the combination of chemotherapy with molecular targeted therapies, including first-, second-, and third-generation EGFR-TKI and ICIs [15,104].
Table 3.
An outline of clinical trials following combination approaches in lung cancer patients.
| Drug Combination | Phases/Study | Treatment Outcome | References |
|---|---|---|---|
| Platinum + pemetrexed + pembrolizumab | Phase III (Keynote 189) | median OS—22.0 months; median PFS—9.0 months |
[256] |
| Carboplatin + (nab)-paclitaxel + pembrolizumab | Phase III (Keynote 407) | median OS—15.9 months; median PFS—6.4 month |
[257] |
| Carboplatin + nab-paclitaxel + atezolizumab | Phase III (Impower 130) | median OS—18.6 months; median PFS—7.0 months |
[258] |
| Carboplatin + paclitaxel + bevacizumab + atezolizumab | Phase III (Impower 150) | median OS—19.2; median PFS—8.3 months |
[253] |
| Pembrolizumab + platinum + pemetrexed | Phase III | median OS—12 months; median PFS—8.8 months | [255] |
| Nivolumab + ipilimumab + two cycles of chemotherapy | Phase III (CheckMate 9LA) | median OS—15.6 months; | [259] |
| Avelumab + axitinib | Phase II (Javelin Medley VEGF) | ORR—31.7%; median PFS—5.5 months | [260] |
| Nivolumab + ipilimumab | Phase III (CheckMate 227) | median OS—17.1 months | [261] |
| Pembrolizumab + stereotactic body radiation therapy (SBRT) | Phase II (PEMBRO-RT) | median OS—15.9 months; median PFS—6.6 months | [262] |
Abbreviations: OS—overall survival; PFS—progression-free survival; ORR—objective response rate.
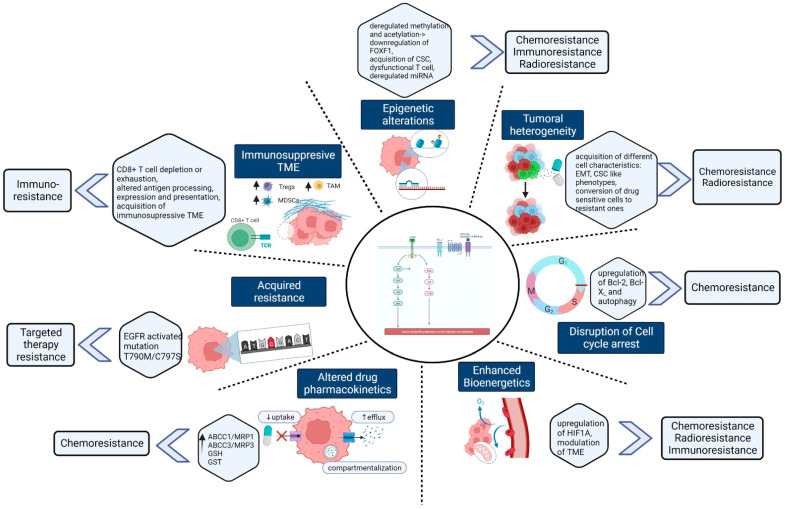
Figure 2.
Different mechanisms inducing therapeutic resistance in lung cancer: Therapeutic resistance against chemotherapy, radiotherapy, targeted therapy, and immunotherapy in lung cancer is caused by different types of mechanism. For instance, tumor heterogeneity, alteration in drug influx and efflux, compartmentalization, epigenetic changes, hypoxia, or reduced autophagy stimulate chemoresistance in lung cancer. Radioresistance is found to happen by epithelial and mesenchymal transition, DNA damage, dysregulated miRNA, and changes in various signaling pathways. Mutations in EGFR or KRAS genes and targets as well as alterations in drug sensitivity lead to mutations at T790M that cause primary and acquired resistance for targeted therapy. Mutations in cancer driver genes, immunosuppressive TME, modified epigenetics, and high bioenergetic are mainly responsible for triggering immunoresistance in lung cancer (created with BioRender.com (accessed on 15 September 2022).
Chemotherapy resistance can be overcome by following combination approaches with other therapies. Studies manifest that the addition of pembrolizumab to chemotherapy (carboplatin and paclitaxel or nab-paclitaxel) extends life expectancy in metastatic squamous NSCLC patients [252]. In one of the clinical trials of NSCLC, the IMpower150 trial, the addition of atezolizumab to bevacizumab plus chemotherapy significantly improved PFS and OS among patients with metastatic NSCLC, regardless of PD-L1 expression and EGFR or ALK genetic alteration status [253].
Immunotherapy-resistant lung cancers can be resensitized through combinations of ICIs and chemotherapeutic drugs. Cytotoxic chemotherapy drugs induce cell death and cause changes in the TME, enhancing antigen presentation, Tregs’ and MDSCs’ activity abrogation, and increasing T-cell activation and infiltration [254], etc. In a phase 3 trial involving metastatic NSCLC, a combination of anti-PD-1, pembrolizumab, and chemotherapy drugs, pemetrexed and cisplatin/carboplatin, resulted in an OS of 69.2% compared to the placebo–chemotherapy combination’s OS of 49.4% at the 12-month mark [255].
Combinations between ICIs and anti-angiogenesis agents are another potential approach, serving to simultaneously target an immunosuppressive TME and tumor neo-angiogenesis, to potentiate immunotherapy [214]. As mentioned earlier, neo-angiogenesis or tumor vasculature is an extrinsic resistance mechanism in immunotherapy-resistant cancers that plays a significant role in promoting an immunosuppressive TME and preventing the delivery of immunotherapeutic agents [228]. In a phase II clinical trial involving a combination of anti-PD-1 (avelumab), and the receptor kinase inhibitor drug (axitinib) targeting VEGFR showed an objective response rate (ORR) of 31.7% in chemotherapy-resistant and recurrent NSCLC [260]. Therefore, targeting VEGF and ICPs, following combination approaches, could serve as an effective strategy to overcome immunotherapy resistance in lung cancer.
One of the promising strategies for overcoming primary and acquired immunotherapy resistance is through the synergistic effects of PD-1/PD-L1 and CTLA-4 inhibitors. These synergistic effects are due to anti-PD-1/anti-PD-L1 acting on the early phases of immune activation, while anti-CTLA-4 acts on the later phases, in the peripheral tissues [263]. For instance, in combination between anti-PD-1 (nivolumab) and anti-CTLA-4 (ipilimumab), the OS rate increased, compared to nivolumab monotherapy alone [261]. These combinations help in the regulation of T-cell priming and activation [254] to overcome resistance. Furthermore, alternative ICPs such as LAG-3, TIM-3, and T-cell immunoglobulin and ITIM domain (TGIT) are upregulated due to ICI inhibition, leading to T-cell exhaustion and eventually adaptive resistance [228]. Combinations between common ICI’s and alternative checkpoint inhibitors have been shown to cause resensitization.
Combination therapy is also a promising strategy to overcome resistance to EGFR TKIs. This approach aims at evading drug resistance through a so-called bypass signaling mechanism by targeting other parallel pathways. Preclinical studies have demonstrated that upfront treatment of EML4-ALK-positive lung tumors with both an ALK inhibitor and a MAPK pathway inhibitor can substantially postpone or even inhibit the onset of resistance [264]. Similar findings were detected in EGFR-mutant lung adenocarcinoma preclinical models and individuals with BRAF V600E lung adenocarcinoma [265,266]. In mouse models, a combination of carboplatin chemotherapy and sotorasib in KRAS G12C lung cancer resulted in greater tumor regression than either monotherapy [267]. Adagrasib combination therapy with palbociclib, a CDK4/6 inhibitor, yielded similar results [268]. A combination of anti-PD-1 immunotherapy with both sotorasib and adagrasib showed complete tumor regression in mice with KRAS G12C tumors [267]. This may be due to the inhibition of KRAS leading to less immunosuppressive TME as KRAS signaling affects IL-10 and TGF-β [269].
Another resensitization method is through ICI and RT combinations. RT functions by causing DNA damage, which eventually leads to cell death. Irradiation creates an immune response through cyclic GMP–AMP synthase (cGAS) stimulation of interferon gene (STING) (cGAS-STING) pathway activation, upregulating the type 1 interferon [270], which causes resensitization through MHC I upregulation [271]. It leads to antigen visibility through T-cell priming, alteration to the TME, etc., [270]; however, it also upregulates PD-L1 expression [272]. A combination results in synergistic effects to potentially overcome immunotherapy resistance by enhancing the effects of immunotherapy through RT [270]. In PEMBRO-RT, treatment with anti-PD-1 (pembrolizumab) after stereotactic body RT showed an increase in ORR [262]. This trial indicates that a combination can be effective in overcoming resistance.
Cisplatin-resistant NSCLC cells display upregulation of peroxisome proliferator-activated receptor gamma (PPARγ) and coactivator-1 alpha (PGC-1α). PGC-1α is a transcription factor coactivator that promotes mitochondrial respiration, heme biosynthesis, angiogenesis [105], and OXPHOS with downregulation of glycolysis [273,274], causing hypoxia by inducing HIF-1α [103,275]. Similarly, hypoxic stress and changes in TME are known to cause radioresistance and effect immune effector cells such as CD8+ and CD4+ T cells [276,277]. Many studies have confirmed that some cancer cells depend on OXPHOS and targeting OXPHOS and mitochondrial respiration overcome their resistance [278,279,280,281]. The author’s lab extensively studies the relationship of heme with lung cancer and has generated HeSP2 that significantly alleviates tumor hypoxia and normalizes tumor vasculature, raising the possibility of their combination with chemotherapy drugs such as cisplatin or immune therapy assisting in improving antitumor efficacy [282].
To optimize the outcome of combination therapy, another strategy of nanotechnology-based co-encapsulation and co-delivery can be used. This will ensure equal spatial and sequential drug dissemination in the target tumor cells [283]. This method can help overcome resistance [284] as it will enhance drug stability by increasing concentrations of drug accumulation in tumor cells with lower side effects.
7. Conclusions
Drug resistance is a major issue in lung cancer that leads to treatment failure, tumor progression, and relapse. Recently, the significant improvement in understanding the complex landscape of therapeutic resistance has changed the treatment paradigm of lung cancer. For instance, platinum-based drug treatment in combination with first-, second-, and third-generation EGFR TKI (erlotinib, afatinib, and osimertinib, respectively), ALK TKIs (ceritinib), or ICIs (pembrolizumab, nivolumab, and atezolizumab) has improved the clinical benefits and patients’ lifespan. Although the initial response is remarkable, the patient ultimately develops resistance. Hence, targeting multiple mechanisms such as deregulated TME, hypoxia, upregulation of alternative ICPs, immunosuppressive TME, deregulated autophagy, DNA damage, and EMT could work as a promising strategy to overcome therapeutic resistance and to improve clinical outcomes in lung cancer patients.
Altogether, combination therapy that targets multidisciplinary approaches, is a great strategy to delay the onset of resistance. However, optimal doses and timings of the administration of such combinations alongside toxicity levels are yet to be determined. Although there are several ongoing clinical trials, many exhibit optimistic results, while others are inconclusive, such as the results found in the PEMBRO-RT phase 2 randomized clinical trial. [262]. In this regard, translational research is important alongside defining the immune patterns of patients, or screening for TME characteristics, tumor cell immune phenotypes, specific mutations, and the host’s immune status. It will also help in developing the best strategies in terms of dose, timing, duration, and sequence of administration, thus reducing toxicity. Therefore, the identification of novel therapeutic methods that target the potential markers, mediators, or pathways triggering therapeutic resistance is necessary to develop precision medicine to reduce lung cancer progression, increase OS, and prevent the occurrence of resistance.
Author Contributions
Conceptualization, A.A., Z.A. and L.Z.; literature survey: A.A., Z.A., P.M. (Pouya Modareszadeh), P.M. (Parsa Modareszadeh), E.B., P.S.A., M.d.C.C.C. and A.R.D.; writing—original draft preparation, A.A., Z.A., P.M. (Pouya Modareszadeh), P.M. (Parsa Modareszadeh), E.B., P.S.A., M.d.C.C.C. and A.R.D.; writing—review and editing, A.A. and Z.A.; visualization, A.A. and P.M. (Parsa Modareszadeh); supervision, L.Z.; funding acquisition, L.Z. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Research in the Zhang lab is supported by the Cancer Prevention and Research Institute of Texas, grant number RP200021.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Thandra K.C., Barsouk A., Saginala K., Aluru J.S., Barsouk A. Epidemiology of lung cancer. Współczesna Onkol. 2021;25:45–52. doi: 10.5114/wo.2021.103829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Sousa V.M.L., Carvalho L. Heterogeneity in Lung Cancer. Pathobiology. 2018;85:96–107. doi: 10.1159/000487440. [DOI] [PubMed] [Google Scholar]
- 3.Hua X., Zhao W., Pesatori A.C., Consonni D., Caporaso N.E., Zhang T., Zhu B., Wang M., Jones K., Hicks B., et al. Genetic and epigenetic intratumor heterogeneity impacts prognosis of lung adenocarcinoma. Nat. Commun. 2020;11:2459. doi: 10.1038/s41467-020-16295-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marino F.Z., Bianco R., Accardo M., Ronchi A., Cozzolino I., Morgillo F., Rossi G., Franco R. Molecular heterogeneity in lung cancer: From mechanisms of origin to clinical implications. Int. J. Med. Sci. 2019;16:981–989. doi: 10.7150/ijms.34739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bade B.C., Dela Cruz C.S. Lung Cancer 2020: Epidemiology, Etiology, and Prevention. Clin. Chest Med. 2020;41:1–24. doi: 10.1016/j.ccm.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Jamal-Hanjani M., Wilson G.A., McGranahan N., Birkbak N.J., Watkins T.B.K., Veeriah S., Shafi S., Johnson D.H., Mitter R., Rosenthal R., et al. Tracking the Evolution of Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017;376:2109–2121. doi: 10.1056/NEJMoa1616288. [DOI] [PubMed] [Google Scholar]
- 7.Pao W., Hutchinson K.E. Chipping away at the lung cancer genome. Nat. Med. 2012;18:349–351. doi: 10.1038/nm.2697. [DOI] [PubMed] [Google Scholar]
- 8.Skoulidis F., Heymach J.V. Co-occurring genomic alterations in non-small-cell lung cancer biology and therapy. Nat. Rev. Cancer. 2019;19:495–509. doi: 10.1038/s41568-019-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saab S., Zalzale H., Rahal Z., Khalifeh Y., Sinjab A., Kadara H. Insights Into Lung Cancer Immune-Based Biology, Prevention, and Treatment. Front. Immunol. 2020;11:159. doi: 10.3389/fimmu.2020.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hung Y.P., Chirieac L.R. How should molecular findings be integrated in the classification for lung cancer? Transl. Lung Cancer Res. 2020;9:2245–2254. doi: 10.21037/tlcr-20-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou J., Huang Q., Huang Z., Li J. Combining immunotherapy and radiotherapy in lung cancer: A promising future? J. Thorac. Dis. 2020;12:4498–4503. doi: 10.21037/JTD-2019-ITM-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lemjabbar-Alaoui H., Hassan O.U., Yang Y.-W., Buchanan P. Lung cancer: Biology and treatment options. Biochim. Biophys. Acta Rev. Cancer. 2015;1856:189–210. doi: 10.1016/j.bbcan.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain P., Jain C., Velcheti V. Role of immune-checkpoint inhibitors in lung cancer. Ther. Adv. Respir. Dis. 2018;12:175346581775007. doi: 10.1177/1753465817750075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vasan N., Baselga J., Hyman D.M. A view on drug resistance in cancer. Nature. 2019;575:299–309. doi: 10.1038/s41586-019-1730-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuan M., Huang L.-L., Chen J.-H., Wu J., Xu Q. The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal Transduct. Target. Ther. 2019;4:61. doi: 10.1038/s41392-019-0099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Min H.-Y., Lee H.-Y. Mechanisms of resistance to chemotherapy in non-small cell lung cancer. Arch. Pharmacal Res. 2021;44:146–164. doi: 10.1007/s12272-021-01312-y. [DOI] [PubMed] [Google Scholar]
- 17.Janet W.-T., Elizabeth H.-B. Drug Resistance Mechanisms in Non-Small Cell Lung Carcinoma. J. Cancer Res. Updates. 2013;2:265. doi: 10.6000/1929-2279.2013.02.04.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Konstantinov S.M., Berger M.R. Alkylating Agents. In: Offermanns S., Rosenthal W., editors. Encyclopedia of Molecular Pharmacology. Springer; Berlin/Heidelberg, Germany: 2008. pp. 53–57. [Google Scholar]
- 19.Olaussen K.A., Postel-Vinay S. Predictors of chemotherapy efficacy in non-small-cell lung cancer: A challenging landscape. Ann. Oncol. 2016;27:2004–2016. doi: 10.1093/annonc/mdw321. [DOI] [PubMed] [Google Scholar]
- 20.Jordan M.A., Wilson L. Microtubules as a target for anticancer drugs. Nat. Rev. Cancer. 2004;4:253–265. doi: 10.1038/nrc1317. [DOI] [PubMed] [Google Scholar]
- 21.Scagliotti G.V., Selvaggi G. Antimetabolites and cancer: Emerging data with a focus on antifolates. Expert Opin. Ther. Pat. 2006;16:189–200. doi: 10.1517/13543776.16.2.189. [DOI] [PubMed] [Google Scholar]
- 22.Riganti C., Contino M. New Strategies to Overcome Resistance to Chemotherapy and Immune System in Cancer. Int. J. Mol. Sci. 2019;20:4783. doi: 10.3390/ijms20194783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Assaraf Y.G., Brozovic A., Gonçalves A.C., Jurkovicova D., Linē A., Machuqueiro M., Saponara S., Sarmento-Ribeiro A.B., Xavier C.P.R., Vasconcelos M.H. The multi-factorial nature of clinical multidrug resistance in cancer. Drug Resist. Updates. 2019;46:100645. doi: 10.1016/j.drup.2019.100645. [DOI] [PubMed] [Google Scholar]
- 24.Holohan C., Van Schaeybroeck S., Longley D.B., Johnston P.G. Cancer drug resistance: An evolving paradigm. Nat. Rev. Cancer. 2013;13:714–726. doi: 10.1038/nrc3599. [DOI] [PubMed] [Google Scholar]
- 25.Bukowski K., Kciuk M., Kontek R. Mechanisms of Multidrug Resistance in Cancer Chemotherapy. Int. J. Mol. Sci. 2020;21:3233. doi: 10.3390/ijms21093233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Housman G., Byler S., Heerboth S., Lapinska K., Longacre M., Snyder N., Sarkar S. Drug Resistance in Cancer: An Overview. Cancers. 2014;6:1769–1792. doi: 10.3390/cancers6031769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen P., Kuang P., Wang L., Li W., Chen B., Liu Y., Wang H., Zhao S., Ye L., Yu F., et al. Mechanisms of drugs-resistance in small cell lung cancer: DNA-related, RNA-related, apoptosis-related, drug accumulation and metabolism procedure. Transl. Lung Cancer Res. 2020;9:768–786. doi: 10.21037/tlcr-19-547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramos A., Sadeghi S., Tabatabaeian H. Battling Chemoresistance in Cancer: Root Causes and Strategies to Uproot Them. Int. J. Mol. Sci. 2021;22:9451. doi: 10.3390/ijms22179451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim J.-Y., Lee J.-Y. Targeting Tumor Adaption to Chronic Hypoxia: Implications for Drug Resistance, and How It Can Be Overcome. Int. J. Mol. Sci. 2017;18:1854. doi: 10.3390/ijms18091854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin L.P., Hamilton T.C., Schilder R.J. Platinum Resistance: The Role of DNA Repair Pathways. Clin. Cancer Res. 2008;14:1291–1295. doi: 10.1158/1078-0432.CCR-07-2238. [DOI] [PubMed] [Google Scholar]
- 31.Vilmar A., Sørensen J.B. Excision repair cross-complementation group 1 (ERCC1) in platinum-based treatment of non-small cell lung cancer with special emphasis on carboplatin: A review of current literature. Lung Cancer. 2009;64:131–139. doi: 10.1016/j.lungcan.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 32.Young L.C., Campling B.G., Cole S.P., Deeley R.G., Gerlach J.H. Multidrug resistance proteins MRP3, MRP1, and MRP2 in lung cancer: Correlation of protein levels with drug response and messenger RNA levels. Clin. Cancer Res. 2001;7:1798–1804. [PubMed] [Google Scholar]
- 33.Oguri T., Ozasa H., Uemura T., Bessho Y., Miyazaki M., Maeno K., Maeda H., Sato S., Ueda R. MRP7/ABCC10 expression is a predictive biomarker for the resistance to paclitaxel in non-small cell lung cancer. Mol. Cancer Ther. 2008;7:1150–1155. doi: 10.1158/1535-7163.MCT-07-2088. [DOI] [PubMed] [Google Scholar]
- 34.Bessho Y., Oguri T., Ozasa H., Uemura T., Sakamoto H., Miyazaki M., Maeno K., Sato S., Ueda R. ABCC10/MRP7 is associated with vinorelbine resistance in non-small cell lung cancer. Oncol. Rep. 2009;21:263–268. [PubMed] [Google Scholar]
- 35.Shimomura M., Yaoi T., Itoh K., Kato D., Terauchi K., Shimada J., Fushiki S. Drug resistance to paclitaxel is not only associated with ABCB1 mRNA expression but also with drug accumulation in intracellular compartments in human lung cancer cell lines. Int. J. Oncol. 2012;40:995–1004. doi: 10.3892/ijo.2011.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao Y., Lu H., Yan A., Yang Y., Meng Q., Sun L., Pang H., Li C., Dong X., Cai L. ABCC3 as a marker for multidrug resistance in non-small cell lung cancer. Sci. Rep. 2013;3:3120. doi: 10.1038/srep03120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shen W., Pang H., Liu J., Zhou J., Zhang F., Liu L., Ma N., Zhang N., Zhang H., Liu L. Epithelial-mesenchymal transition contributes to docetaxel resistance in human non-small cell lung cancer. Oncol. Res. 2014;22:47–55. doi: 10.3727/096504014X14098532393473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cui H., Arnst K., Miller D.D., Li W. Recent Advances in Elucidating Paclitaxel Resistance Mechanisms in Non-small Cell Lung Cancer and Strategies to Overcome Drug Resistance. Curr. Med. Chem. 2020;27:6573–6595. doi: 10.2174/0929867326666191016113631. [DOI] [PubMed] [Google Scholar]
- 39.Pljesa-Ercegovac M., Savic-Radojevic A., Matic M., Coric V., Djukic T., Radic T., Simic T. Glutathione Transferases: Potential Targets to Overcome Chemoresistance in Solid Tumors. Int. J. Mol. Sci. 2018;19:3785. doi: 10.3390/ijms19123785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Townsend D.M., Tew K.D. The role of glutathione-S-transferase in anti-cancer drug resistance. Oncogene. 2003;22:7369–7375. doi: 10.1038/sj.onc.1206940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharma A., Patrick B., Li J., Sharma R., Jeyabal P.V., Reddy P.M., Awasthi S., Awasthi Y.C. Glutathione S-transferases as antioxidant enzymes: Small cell lung cancer (H69) cells transfected with hGSTA1 resist doxorubicin-induced apoptosis. Arch. Biochem. Biophys. 2006;452:165–173. doi: 10.1016/j.abb.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 42.Sun C.-Y., Nie J., Huang J.-P., Zheng G.-J., Feng B. Targeting STAT3 inhibition to reverse cisplatin resistance. Biomed. Pharmacother. 2019;117:109135. doi: 10.1016/j.biopha.2019.109135. [DOI] [PubMed] [Google Scholar]
- 43.Jin L., Chun J., Pan C., Li D., Lin R., Alesi G.N., Wang X., Kang H.B., Song L., Wang D., et al. MAST1 Drives Cisplatin Resistance in Human Cancers by Rewiring cRaf-Independent MEK Activation. Cancer Cell. 2018;34:315–330.e7. doi: 10.1016/j.ccell.2018.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stewart D.J. Mechanisms of resistance to cisplatin and carboplatin. Crit. Rev. Oncol./Hematol. 2007;63:12–31. doi: 10.1016/j.critrevonc.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 45.Zhang F., Shen M., Yang L., Yang X., Tsai Y., Keng P.C., Chen Y., Lee S.O., Chen Y. Simultaneous targeting of ATM and Mcl-1 increases cisplatin sensitivity of cisplatin-resistant non-small cell lung cancer. Cancer Biol. Ther. 2017;18:606–615. doi: 10.1080/15384047.2017.1345391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Horibe S., Matsuda A., Tanahashi T., Inoue J., Kawauchi S., Mizuno S., Ueno M., Takahashi K., Maeda Y., Maegouchi T., et al. Cisplatin resistance in human lung cancer cells is linked with dysregulation of cell cycle associated proteins. Life Sci. 2015;124:31–40. doi: 10.1016/j.lfs.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 47.Sarin N., Engel F., Kalayda G.V., Mannewitz M., Cinatl J., Jr., Rothweiler F., Michaelis M., Saafan H., Ritter C.A., Jaehde U., et al. Cisplatin resistance in non-small cell lung cancer cells is associated with an abrogation of cisplatin-induced G2/M cell cycle arrest. PLoS ONE. 2017;12:e0181081. doi: 10.1371/journal.pone.0181081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shen M., Xu Z., Xu W., Jiang K., Zhang F., Ding Q., Xu Z., Chen Y. Inhibition of ATM reverses EMT and decreases metastatic potential of cisplatin-resistant lung cancer cells through JAK/STAT3/PD-L1 pathway. J. Exp. Clin. Cancer Res. 2019;38:149. doi: 10.1186/s13046-019-1161-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hu Y., Yagüe E., Zhao J., Wang L., Bai J., Yang Q., Pan T., Zhao H., Liu J., Zhang J. Sabutoclax, pan-active BCL-2 protein family antagonist, overcomes drug resistance and eliminates cancer stem cells in breast cancer. Cancer Lett. 2018;423:47–59. doi: 10.1016/j.canlet.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 50.D’Aguanno S., Del Bufalo D. Inhibition of Anti-Apoptotic Bcl-2 Proteins in Preclinical and Clinical Studies: Current Overview in Cancer. Cells. 2020;9:1287. doi: 10.3390/cells9051287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mukherjee N., Almeida A., Partyka K.A., Lu Y., Schwan J.V., Lambert K., Rogers M., Robinson W.A., Robinson S.E., Applegate A.J., et al. Combining a GSI and BCL-2 inhibitor to overcome melanoma’s resistance to current treatments. Oncotarget. 2016;7:84594–84607. doi: 10.18632/oncotarget.13141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ni Chonghaile T., Letai A. Mimicking the BH3 domain to kill cancer cells. Oncogene. 2008;27((Suppl. S1)):S149–S157. doi: 10.1038/onc.2009.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thomas S., Quinn B.A., Das S.K., Dash R., Emdad L., Dasgupta S., Wang X.Y., Dent P., Reed J.C., Pellecchia M., et al. Targeting the Bcl-2 family for cancer therapy. Expert Opin. Targets. 2013;17:61–75. doi: 10.1517/14728222.2013.733001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bodur C., Basaga H. Bcl-2 inhibitors: Emerging drugs in cancer therapy. Curr. Med. Chem. 2012;19:1804–1820. doi: 10.2174/092986712800099839. [DOI] [PubMed] [Google Scholar]
- 55.Maji S., Panda S., Samal S.K., Shriwas O., Rath R., Pellecchia M., Emdad L., Das S.K., Fisher P.B., Dash R. Chapter Three—Bcl-2 Antiapoptotic Family Proteins and Chemoresistance in Cancer. In: Tew K.D., Fisher P.B., editors. Advances in Cancer Research. Volume 137. Academic Press; Cambridge, MA, USA: 2018. pp. 37–75. [DOI] [PubMed] [Google Scholar]
- 56.Inno A., Stagno A., Gori S. Schlafen-11 (SLFN11): A step forward towards personalized medicine in small-cell lung cancer? Transl. Lung Cancer Res. 2018;7((Suppl. S4)):S341–S345. doi: 10.21037/tlcr.2018.11.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lok B.H., Gardner E.E., Schneeberger V.E., Ni A., Desmeules P., Rekhtman N., de Stanchina E., Teicher B.A., Riaz N., Powell S.N., et al. PARP Inhibitor Activity Correlates with SLFN11 Expression and Demonstrates Synergy with Temozolomide in Small Cell Lung Cancer. Clin. Cancer Res. 2017;23:523–535. doi: 10.1158/1078-0432.CCR-16-1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sen T., Tong P., Diao L., Li L., Fan Y., Hoff J., Heymach J.V., Wang J., Byers L.A. Targeting AXL and mTOR Pathway Overcomes Primary and Acquired Resistance to WEE1 Inhibition in Small-Cell Lung Cancer. Clin. Cancer Res. 2017;23:6239–6253. doi: 10.1158/1078-0432.CCR-17-1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hsu W.-H., Zhao X., Zhu J., Kim I.-K., Rao G., McCutcheon J., Hsu S.-T., Teicher B., Kallakury B., Dowlati A., et al. Checkpoint Kinase 1 Inhibition Enhances Cisplatin Cytotoxicity and Overcomes Cisplatin Resistance in SCLC by Promoting Mitotic Cell Death. J. Thorac. Oncol. 2019;14:1032–1045. doi: 10.1016/j.jtho.2019.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sosa Iglesias V., Giuranno L., Dubois L.J., Theys J., Vooijs M. Drug Resistance in Non-Small Cell Lung Cancer: A Potential for NOTCH Targeting? Front. Oncol. 2018;8:267. doi: 10.3389/fonc.2018.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Leonetti A., Facchinetti F., Minari R., Cortellini A., Rolfo C.D., Giovannetti E., Tiseo M. Notch pathway in small-cell lung cancer: From preclinical evidence to therapeutic challenges. Cell Oncol. 2019;42:261–273. doi: 10.1007/s13402-019-00441-3. [DOI] [PubMed] [Google Scholar]
- 62.Geisslinger F., Müller M., Vollmar A.M., Bartel K. Targeting Lysosomes in Cancer as Promising Strategy to Overcome Chemoresistance-A Mini Review. Front. Oncol. 2020;10:1156. doi: 10.3389/fonc.2020.01156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Perillo B., Di Donato M., Pezone A., Di Zazzo E., Giovannelli P., Galasso G., Castoria G., Migliaccio A. ROS in cancer therapy: The bright side of the moon. Exp. Mol. Med. 2020;52:192–203. doi: 10.1038/s12276-020-0384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhan Y., Wang K., Li Q., Zou Y., Chen B., Gong Q., Ho H.I., Yin T., Zhang F., Lu Y., et al. The Novel Autophagy Inhibitor Alpha-Hederin Promoted Paclitaxel Cytotoxicity by Increasing Reactive Oxygen Species Accumulation in Non-Small Cell Lung Cancer Cells. Int. J. Mol. Sci. 2018;19:3221. doi: 10.3390/ijms19103221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu X., Wu Q., Zhou X., Huang J. SphK1 functions downstream of IGF-1 to modulate IGF-1-induced EMT, migration and paclitaxel resistance of A549 cells: A preliminary in vitro study. J. Cancer. 2019;10:4264–4269. doi: 10.7150/jca.32646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dawson M.A., Kouzarides T. Cancer epigenetics: From mechanism to therapy. Cell. 2012;150:12–27. doi: 10.1016/j.cell.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 67.Zhao J., Xue X., Fu W., Dai L., Jiang Z., Zhong S., Deng B., Yin J. Epigenetic activation of FOXF1 confers cancer stem cell properties to cisplatin-resistant non-small cell lung cancer. Int. J. Oncol. 2020;56:1083–1092. doi: 10.3892/ijo.2020.5003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu R., Chen Y., Liu G., Li C., Song Y., Cao Z., Li W., Hu J., Lu C., Liu Y. PI3K/AKT pathway as a key link modulates the multidrug resistance of cancers. Cell Death Dis. 2020;11:797. doi: 10.1038/s41419-020-02998-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Reshma P.L., Unnikrishnan B.S., Preethi G.U., Syama H.P., Archana M.G., Remya K., Shiji R., Sreekutty J., Sreelekha T.T. Overcoming drug-resistance in lung cancer cells by paclitaxel loaded galactoxyloglucan nanoparticles. Int. J. Biol. Macromol. 2019;136:266–274. doi: 10.1016/j.ijbiomac.2019.06.075. [DOI] [PubMed] [Google Scholar]
- 70.Pearce M.C., Gamble J.T., Kopparapu P.R., O’Donnell E.F., Mueller M.J., Jang H.S., Greenwood J.A., Satterthwait A.C., Tanguay R.L., Zhang X.-K., et al. Induction of apoptosis and suppression of tumor growth by Nur77-derived Bcl-2 converting peptide in chemoresistant lung cancer cells. Oncotarget. 2018;9:26072–26085. doi: 10.18632/oncotarget.25437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sun Y., Hu B., Wang Q., Ye M., Qiu Q., Zhou Y., Zeng F., Zhang X., Guo Y., Guo L. Long non-coding RNA HOTTIP promotes BCL-2 expression and induces chemoresistance in small cell lung cancer by sponging miR-216a. Cell Death Dis. 2018;9:85. doi: 10.1038/s41419-017-0113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhou Y., Liu H., Xue R., Tang W., Zhang S. BH3 Mimetic ABT-199 Enhances the Sensitivity of Gemcitabine in Pancreatic Cancer in vitro and in vivo. Dig. Dis. Sci. 2018;63:3367–3375. doi: 10.1007/s10620-018-5253-7. [DOI] [PubMed] [Google Scholar]
- 73.Yang J., Zhang K., Wu J., Shi J., Xue J., Li J., Chen J., Zhu Y., Wei J., He J., et al. Wnt5a Increases Properties of Lung Cancer Stem Cells and Resistance to Cisplatin through Activation of Wnt5a/PKC Signaling Pathway. Stem Cells Int. 2016;2016:1690896. doi: 10.1155/2016/1690896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang Y., Wang X. Targeting the Wnt/β-catenin signaling pathway in cancer. J. Hematol. Oncol. 2020;13:165. doi: 10.1186/s13045-020-00990-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gardner E.E., Lok B.H., Schneeberger V.E., Desmeules P., Miles L.A., Arnold P.K., Ni A., Khodos I., De Stanchina E., Nguyen T., et al. Chemosensitive Relapse in Small Cell Lung Cancer Proceeds through an EZH2-SLFN11 Axis. Cancer Cell. 2017;31:286–299. doi: 10.1016/j.ccell.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Beck B., Lapouge G., Rorive S., Drogat B., Desaedelaere K., Delafaille S., Dubois C., Salmon I., Willekens K., Marine J.-C., et al. Different Levels of Twist1 Regulate Skin Tumor Initiation, Stemness, and Progression. Cell Stem Cell. 2015;16:67–79. doi: 10.1016/j.stem.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 77.Schmidt J.M., Panzilius E., Bartsch H.S., Irmler M., Beckers J., Kari V., Linnemann J.R., Dragoi D., Hirschi B., Kloos U.J., et al. Stem-cell-like properties and epithelial plasticity arise as stable traits after transient Twist1 activation. Cell Rep. 2015;10:131–139. doi: 10.1016/j.celrep.2014.12.032. [DOI] [PubMed] [Google Scholar]
- 78.Yang J., Mani S.A., Donaher J.L., Ramaswamy S., Itzykson R.A., Come C., Savagner P., Gitelman I., Richardson A., Weinberg R.A. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004;117:927–939. doi: 10.1016/j.cell.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 79.Yang W.-H., Lan H.-Y., Huang C.-H., Tai S.-K., Tzeng C.-H., Kao S.-Y., Wu K.-J., Hung M.-C., Yang M.-H. RAC1 activation mediates Twist1-induced cancer cell migration. Nat. Cell Biol. 2012;14:366–374. doi: 10.1038/ncb2455. [DOI] [PubMed] [Google Scholar]
- 80.Herzog B.H., Devarakonda S., Govindan R. Overcoming Chemotherapy Resistance in SCLC. J. Thorac. Oncol. 2021;16:2002–2015. doi: 10.1016/j.jtho.2021.07.018. [DOI] [PubMed] [Google Scholar]
- 81.Feng X., Wang Z., Fillmore R., Xi Y. MiR-200, a new star miRNA in human cancer. Cancer Lett. 2014;344:166–173. doi: 10.1016/j.canlet.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen Y., Gao D.-Y., Huang L. In vivo delivery of miRNAs for cancer therapy: Challenges and strategies. Adv. Drug Deliv. Rev. 2015;81:128–141. doi: 10.1016/j.addr.2014.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hua L., Zhu G., Wei J. MicroRNA-1 overexpression increases chemosensitivity of non-small cell lung cancer cells by inhibiting autophagy related 3-mediated autophagy. Cell Biol. Int. 2018;42:1240–1249. doi: 10.1002/cbin.10995. [DOI] [PubMed] [Google Scholar]
- 84.Ansari J., Shackelford R.E., El-Osta H. Epigenetics in non-small cell lung cancer: From basics to therapeutics. Transl. Lung Cancer Res. 2016;5:155–171. doi: 10.21037/tlcr.2016.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zagryazhskaya A., Zhivotovsky B. miRNAs in lung cancer: A link to aging. Ageing Res. Rev. 2014;17:54–67. doi: 10.1016/j.arr.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 86.Si W., Shen J., Zheng H., Fan W. The role and mechanisms of action of microRNAs in cancer drug resistance. Clin. Epigenet. 2019;11:25. doi: 10.1186/s13148-018-0587-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang H., Chen J., Zhang S., Zheng X., Xie S., Mao J., Cai Y., Lu X., Hu L., Shen J., et al. MiR-223 regulates autophagy associated with cisplatin resistance by targeting FBXW7 in human non-small cell lung cancer. Cancer Cell Int. 2020;20:258. doi: 10.1186/s12935-020-01284-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.MacDonagh L., Gray S.G., Finn S.P., Cuffe S., O’Byrne K.J., Barr M.P. The emerging role of microRNAs in resistance to lung cancer treatments. Cancer Treat. Rev. 2015;41:160–169. doi: 10.1016/j.ctrv.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 89.Lujambio A., Lowe S.W. The microcosmos of cancer. Nature. 2012;482:347–355. doi: 10.1038/nature10888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cruz-Bermúdez A., Laza-Briviesca R., Vicente-Blanco R.J., García-Grande A., Coronado M.J., Laine-Menéndez S., Palacios-Zambrano S., Moreno-Villa M.R., Ruiz-Valdepeñas A.M., Lendinez C., et al. Cisplatin resistance involves a metabolic reprogramming through ROS and PGC-1α in NSCLC which can be overcome by OXPHOS inhibition. Free Radic. Biol. Med. 2019;135:167–181. doi: 10.1016/j.freeradbiomed.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 91.Obrist F., Michels J., Durand S., Chery A., Pol J., Levesque S., Joseph A., Astesana V., Pietrocola F., Wu G.S., et al. Metabolic vulnerability of cisplatin-resistant cancers. EMBO J. 2018;37:e98597. doi: 10.15252/embj.201798597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen S.-H., Chang J.-Y. New Insights into Mechanisms of Cisplatin Resistance: From Tumor Cell to Microenvironment. Int. J. Mol. Sci. 2019;20:4136. doi: 10.3390/ijms20174136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Qu Y., Dou B., Tan H., Feng Y., Wang N., Wang D. Tumor microenvironment-driven non-cell-autonomous resistance to antineoplastic treatment. Mol. Cancer. 2019;18:69. doi: 10.1186/s12943-019-0992-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Amiri-Kordestani L., Basseville A., Kurdziel K., Fojo A.T., Bates S.E. Targeting MDR in breast and lung cancer: Discriminating its potential importance from the failure of drug resistance reversal studies. Drug Resist. Updates. 2012;15:50–61. doi: 10.1016/j.drup.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.El-Awady R., Saleh E., Hashim A., Soliman N., Dallah A., Elrasheed A., Elakraa G. The Role of Eukaryotic and Prokaryotic ABC Transporter Family in Failure of Chemotherapy. Front. Pharm. 2016;7:535. doi: 10.3389/fphar.2016.00535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xu X., Jin S., Ma Y., Fan Z., Yan Z., Li W., Song Q., You W., Lyu Z., Song Y., et al. miR-30a-5p enhances paclitaxel sensitivity in non-small cell lung cancer through targeting BCL-2 expression. J. Mol. Med. 2017;95:861–871. doi: 10.1007/s00109-017-1539-z. [DOI] [PubMed] [Google Scholar]
- 97.Ibanez de Caceres I., Cortes-Sempere M., Moratilla C., Machado-Pinilla R., Rodriguez-Fanjul V., Manguán-García C., Cejas P., López-Ríos F., Paz-Ares L., de CastroCarpeño J., et al. IGFBP-3 hypermethylation-derived deficiency mediates cisplatin resistance in non-small-cell lung cancer. Oncogene. 2010;29:1681–1690. doi: 10.1038/onc.2009.454. [DOI] [PubMed] [Google Scholar]
- 98.Dalvi M.P., Wang L., Zhong R., Kollipara R.K., Park H., Bayo J., Yenerall P., Zhou Y., Timmons B.C., Rodriguez-Canales J., et al. Taxane-Platin-Resistant Lung Cancers Co-develop Hypersensitivity to JumonjiC Demethylase Inhibitors. Cell Rep. 2017;19:1669–1684. doi: 10.1016/j.celrep.2017.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen B., Tan Y., Liang Y., Li Y., Chen L., Wu S., Xu W., Wang Y., Zhao W., Wu J. Per2 participates in AKT-mediated drug resistance in A549/DDP lung adenocarcinoma cells. Oncol. Lett. 2017;13:423–428. doi: 10.3892/ol.2016.5430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang Y., Xu W., Guo H., Zhang Y., He Y., Lee S.H., Song X., Li X., Guo Y., Zhao Y., et al. NOTCH1 Signaling Regulates Self-Renewal and Platinum Chemoresistance of Cancer Stem–like Cells in Human Non–Small Cell Lung Cancer. Cancer Res. 2017;77:3082–3091. doi: 10.1158/0008-5472.CAN-16-1633. [DOI] [PubMed] [Google Scholar]
- 101.Ahmad A., Maitah M.i.Y., Ginnebaugh K.R., Li Y., Bao B., Gadgeel S.M., Sarkar F.H. Inhibition of Hedgehog signaling sensitizes NSCLC cells to standard therapies through modulation of EMT-regulating miRNAs. J. Hematol. Oncol. 2013;6:77. doi: 10.1186/1756-8722-6-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wu H.-M., Jiang Z.-F., Ding P.-S., Shao L.-J., Liu R.-Y. Hypoxia-induced autophagy mediates cisplatin resistance in lung cancer cells. Sci. Rep. 2015;5:12291. doi: 10.1038/srep12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Guo Q., Lan F., Yan X., Xiao Z., Wu Y., Zhang Q. Hypoxia exposure induced cisplatin resistance partially via activating p53 and hypoxia inducible factor-1α in non-small cell lung cancer A549 cells. Oncol. Lett. 2018;16:801–808. doi: 10.3892/ol.2018.8767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen J., Jiang C.C., Jin L., Zhang X.D. Regulation of PD-L1: A novel role of pro-survival signalling in cancer. Ann. Oncol. 2016;27:409–416. doi: 10.1093/annonc/mdv615. [DOI] [PubMed] [Google Scholar]
- 105.Tan Z., Luo X., Xiao L., Tang M., Bode A.M., Dong Z., Cao Y. The Role of PGC1α in Cancer Metabolism and its Therapeutic Implications. Mol. Cancer Ther. 2016;15:774–782. doi: 10.1158/1535-7163.MCT-15-0621. [DOI] [PubMed] [Google Scholar]
- 106.Gomez-Casal R., Epperly M.W., Wang H., Proia D.A., Greenberger J.S., Levina V. Radioresistant human lung adenocarcinoma cells that survived multiple fractions of ionizing radiation are sensitive to HSP90 inhibition. Oncotarget. 2015;6:44306–44322. doi: 10.18632/oncotarget.6248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yang W.-C., Hsu F.-M., Yang P.-C. Precision radiotherapy for non-small cell lung cancer. J. Biomed. Sci. 2020;27:82. doi: 10.1186/s12929-020-00676-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chen M., Yang J., Liao Z., Chen J., Xu C., He X., Zhang X., Zhu R.X., Li H. Anatomic change over the course of treatment for non–small cell lung cancer patients and its impact on intensity-modulated radiation therapy and passive-scattering proton therapy deliveries. Radiat. Oncol. 2020;15:55. doi: 10.1186/s13014-020-01503-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim N., Noh J.M., Lee W., Park B., Pyo H. Clinical Outcomes of Pencil Beam Scanning Proton Therapy in Locally Advanced Non-Small Cell Lung Cancer: Propensity Score Analysis. Cancers. 2021;13:3497. doi: 10.3390/cancers13143497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Skliarenko J., Barry A. Clinical and practical applications of radiation therapy: When should radiation therapy be considered for my patient? Medicine. 2020;48:84–89. doi: 10.1016/j.mpmed.2019.11.004. [DOI] [Google Scholar]
- 111.Cao C., Wang D., Chung C., Tian D., Rimner A., Huang J., Jones D.R. A systematic review and meta-analysis of stereotactic body radiation therapy versus surgery for patients with non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2019;157:362–373.e8. doi: 10.1016/j.jtcvs.2018.08.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yin X., Yan D., Qiu M., Huang L., Yan S.-X. Prophylactic cranial irradiation in small cell lung cancer: A systematic review and meta-analysis. BMC Cancer. 2019;19:95. doi: 10.1186/s12885-018-5251-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chun S.G., Hu C., Choy H., Komaki R.U., Timmerman R.D., Schild S.E., Bogart J.A., Dobelbower M.C., Bosch W., Galvin J.M., et al. Impact of Intensity-Modulated Radiation Therapy Technique for Locally Advanced Non-Small-Cell Lung Cancer: A Secondary Analysis of the NRG Oncology RTOG 0617 Randomized Clinical Trial. J. Clin. Oncol. 2017;35:56–62. doi: 10.1200/JCO.2016.69.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gjyshi O., Liao Z. Proton therapy for locally advanced non-small cell lung cancer. Br. J. Radiol. 2020;93:20190378. doi: 10.1259/bjr.20190378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Iocolano M., Wild A.T., Hannum M., Zhang Z., Simone C.B., 2nd, Gelblum D., Wu A.J., Rimner A., Shepherd A.F. Hypofractionated vs. conventional radiation therapy for stage III non-small cell lung cancer treated without chemotherapy. Acta Oncol. 2020;59:164–170. doi: 10.1080/0284186X.2019.1675907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yin L., Xue J., Li R., Zhou L., Deng L., Chen L., Zhang Y., Li Y., Zhang X., Xiu W., et al. Effect of Low-Dose Radiation Therapy on Abscopal Responses to Hypofractionated Radiation Therapy and Anti-PD1 in Mice and Patients With Non-Small Cell Lung Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2020;108:212–224. doi: 10.1016/j.ijrobp.2020.05.002. [DOI] [PubMed] [Google Scholar]
- 117.Tan S., Yi P., Wang H., Xia L., Han Y., Wang H., Zeng B., Tang L., Pan Q., Tian Y., et al. RAC1 Involves in the Radioresistance by Mediating Epithelial-Mesenchymal Transition in Lung Cancer. Front. Oncol. 2020;10:649. doi: 10.3389/fonc.2020.00649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jiang N., Dai Q., Su X., Fu J., Feng X., Peng J. Role of PI3K/AKT pathway in cancer: The framework of malignant behavior. Mol. Biol. Rep. 2020;47:4587–4629. doi: 10.1007/s11033-020-05435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Toulany M., Iida M., Keinath S., Iyi F.F., Mueck K., Fehrenbacher B., Mansour W.Y., Schaller M., Wheeler D.L., Rodemann H.P. Dual targeting of PI3K and MEK enhances the radiation response of K-RAS mutated non-small cell lung cancer. Oncotarget. 2016;7:43746–43761. doi: 10.18632/oncotarget.9670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhao R.S., Wang W., Li J.P., Liu C.M., He L. Gelsolin Promotes Radioresistance in Non-Small Cell Lung Cancer Cells Through Activation of Phosphoinositide 3-Kinase/Akt Signaling. Technol. Cancer Res. Treat. 2017;16:512–518. doi: 10.1177/1533034616643884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Li L., Li Y., Zou H. A novel role for apatinib in enhancing radiosensitivity in non-small cell lung cancer cells by suppressing the AKT and ERK pathways. PeerJ. 2021;9:e12356. doi: 10.7717/peerj.12356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ushijima H., Suzuki Y., Oike T., Komachi M., Yoshimoto Y., Ando K., Okonogi N., Sato H., Noda S.E., Saito J., et al. Radio-sensitization effect of an mTOR inhibitor, temsirolimus, on lung adenocarcinoma A549 cells under normoxic and hypoxic conditions. J. Radiat. Res. 2015;56:663–668. doi: 10.1093/jrr/rrv021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Das U., Manna K., Adhikary A., Mishra S., Saha K.D., Sharma R.D., Majumder B., Dey S. Ferulic acid enhances the radiation sensitivity of lung and liver carcinoma cells by collapsing redox homeostasis: Mechanistic involvement of Akt/p38 MAPK signalling pathway. Free Radic. Res. 2019;53:944–967. doi: 10.1080/10715762.2019.1655559. [DOI] [PubMed] [Google Scholar]
- 124.Shah M.A., Rogoff H.A. Implications of reactive oxygen species on cancer formation and its treatment. Semin. Oncol. 2021;48:238–245. doi: 10.1053/j.seminoncol.2021.05.002. [DOI] [PubMed] [Google Scholar]
- 125.Kim T.W., Hong D.W., Kang C.M., Hong S.H. A novel PPARɣ ligand, PPZ023, overcomes radioresistance via ER stress and cell death in human non-small-cell lung cancer cells. Exp. Mol. Med. 2020;52:1730–1743. doi: 10.1038/s12276-020-00511-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chen N., Wu L., Yuan H., Wang J. ROS/Autophagy/Nrf2 Pathway Mediated Low-Dose Radiation Induced Radio-Resistance in Human Lung Adenocarcinoma A549 Cell. Int. J. Biol. Sci. 2015;11:833–844. doi: 10.7150/ijbs.10564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mikac S., Rychłowski M., Dziadosz A., Szabelska-Beresewicz A., Fahraeus R., Hupp T., Sznarkowska A. Identification of a Stable, Non-Canonically Regulated Nrf2 Form in Lung Cancer Cells. Antioxidants. 2021;10:786. doi: 10.3390/antiox10050786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Binkley M.S., Jeon Y.J., Nesselbush M., Moding E.J., Nabet B.Y., Almanza D., Kunder C., Stehr H., Yoo C.H., Rhee S., et al. KEAP1/NFE2L2 Mutations Predict Lung Cancer Radiation Resistance That Can Be Targeted by Glutaminase Inhibition. Cancer Discov. 2020;10:1826–1841. doi: 10.1158/2159-8290.CD-20-0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhou S., Zhang M., Zhou C., Wang W., Yang H., Ye W. The role of epithelial-mesenchymal transition in regulating radioresistance. Crit. Rev. Oncol. Hematol. 2020;150:102961. doi: 10.1016/j.critrevonc.2020.102961. [DOI] [PubMed] [Google Scholar]
- 130.Cano A., Pérez-Moreno M.A., Rodrigo I., Locascio A., Blanco M.J., del Barrio M.G., Portillo F., Nieto M.A. The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat. Cell Biol. 2000;2:76–83. doi: 10.1038/35000025. [DOI] [PubMed] [Google Scholar]
- 131.Moreno-Bueno G., Cubillo E., Sarrió D., Peinado H., Rodríguez-Pinilla S.M., Villa S., Bolós V., Jordá M., Fabra A., Portillo F., et al. Genetic profiling of epithelial cells expressing E-cadherin repressors reveals a distinct role for Snail, Slug, and E47 factors in epithelial-mesenchymal transition. Cancer Res. 2006;66:9543–9556. doi: 10.1158/0008-5472.CAN-06-0479. [DOI] [PubMed] [Google Scholar]
- 132.Hui L., Zhang S., Dong X., Tian D., Cui Z., Qiu X. Prognostic significance of twist and N-cadherin expression in NSCLC. PLoS ONE. 2013;8:e62171. doi: 10.1371/journal.pone.0062171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Menju T., Date H. Lung cancer and epithelial-mesenchymal transition. Gen. Thorac. Cardiovasc. Surg. 2021;69:781–789. doi: 10.1007/s11748-021-01595-4. [DOI] [PubMed] [Google Scholar]
- 134.Kumar M., Allison D.F., Baranova N.N., Wamsley J.J., Katz A.J., Bekiranov S., Jones D.R., Mayo M.W. NF-κB regulates mesenchymal transition for the induction of non-small cell lung cancer initiating cells. PLoS ONE. 2013;8:e68597. doi: 10.1371/journal.pone.0068597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zou K., Li Z., Zhang Y., Mu L., Chen M., Wang R., Deng W., Zou L., Liu J. β-Elemene enhances radiosensitivity in non-small-cell lung cancer by inhibiting epithelial-mesenchymal transition and cancer stem cell traits via Prx-1/NF-kB/iNOS signaling pathway. Aging. 2020;13:2575–2592. doi: 10.18632/aging.202291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kim J.Y., Kim H.J., Jung C.W., Lee T.S., Kim E.H., Park M.J. CXCR4 uses STAT3-mediated slug expression to maintain radioresistance of non-small cell lung cancer cells: Emerges as a potential prognostic biomarker for lung cancer. Cell Death Dis. 2021;12:48. doi: 10.1038/s41419-020-03280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Shih P.C., Mei K.C. Role of STAT3 signaling transduction pathways in cancer stem cell-associated chemoresistance. Drug Discov. Today. 2021;26:1450–1458. doi: 10.1016/j.drudis.2020.11.032. [DOI] [PubMed] [Google Scholar]
- 138.Lee J.H., Choi S.I., Kim R.K., Cho E.W., Kim I.G. Tescalcin/c-Src/IGF1Rβ-mediated STAT3 activation enhances cancer stemness and radioresistant properties through ALDH1. Sci. Rep. 2018;8:10711. doi: 10.1038/s41598-018-29142-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen Y., Li W.W., Peng P., Zhao W.H., Tian Y.J., Huang Y., Xia S., Chen Y. mTORC1 inhibitor RAD001 (everolimus) enhances non-small cell lung cancer cell radiosensitivity in vitro via suppressing epithelial-mesenchymal transition. Acta Pharm. Sin. 2019;40:1085–1094. doi: 10.1038/s41401-019-0215-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Cong L., Yi J., Qiu S., Wang R., Jin S., Jiang R., Cong X. Effect of EG00229 on Radiation Resistance of Lung Adenocarcinoma Cells. J. Cancer. 2021;12:6105–6117. doi: 10.7150/jca.56123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lu Y., Ma J., Li Y., Huang J., Zhang S., Yin Z., Ren J., Huang K., Wu G., Yang K., et al. CDP138 silencing inhibits TGF-β/Smad signaling to impair radioresistance and metastasis via GDF15 in lung cancer. Cell Death Dis. 2017;8:e3036. doi: 10.1038/cddis.2017.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Cui Y.H., Kang J.H., Suh Y., Zhao Y., Yi J.M., Bae I.H., Lee H.J., Park D.W., Kim M.J., Lee S.J. Loss of FBXL14 promotes mesenchymal shift and radioresistance of non-small cell lung cancer by TWIST1 stabilization. Signal Transduct. Target. 2021;6:272. doi: 10.1038/s41392-021-00599-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lu J., Zhan Y., Feng J., Luo J., Fan S. MicroRNAs associated with therapy of non-small cell lung cancer. Int. J. Biol. Sci. 2018;14:390–397. doi: 10.7150/ijbs.22243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Xu L.M., Yu H., Yuan Y.J., Zhang J., Ma Y., Cao X.C., Wang J., Zhao L.J., Wang P. Overcoming of Radioresistance in Non-small Cell Lung Cancer by microRNA-320a Through HIF1α-Suppression Mediated Methylation of PTEN. Front. Cell Dev. Biol. 2020;8:553733. doi: 10.3389/fcell.2020.553733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Arechaga-Ocampo E., Lopez-Camarillo C., Villegas-Sepulveda N., Gonzalez-De la Rosa C.H., Perez-Añorve I.X., Roldan-Perez R., Flores-Perez A., Peña-Curiel O., Angeles-Zaragoza O., Rangel Corona R., et al. Tumor suppressor miR-29c regulates radioresistance in lung cancer cells. Tumour Biol. 2017;39:1010428317695010. doi: 10.1177/1010428317695010. [DOI] [PubMed] [Google Scholar]
- 146.Cellini F., Morganti A.G., Genovesi D., Silvestris N., Valentini V. Role of microRNA in response to ionizing radiations: Evidences and potential impact on clinical practice for radiotherapy. Molecules. 2014;19:5379–5401. doi: 10.3390/molecules19045379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Li H., Zhao S., Chen X., Feng G., Chen Z., Fan S. MiR-145 modulates the radiosensitivity of non-small cell lung cancer cells by suppression of TMOD3. Carcinogenesis. 2022;43:288–296. doi: 10.1093/carcin/bgab121. [DOI] [PubMed] [Google Scholar]
- 148.Wei W., Dong Z., Gao H., Zhang Y.-Y., Shao L.-H., Jin L.-L., Lv Y.-H., Zhao G., Shen Y.-N., Jin S.-Z. MicroRNA-9 enhanced radiosensitivity and its mechanism of DNA methylation in non-small cell lung cancer. Gene. 2019;710:178–185. doi: 10.1016/j.gene.2019.05.050. [DOI] [PubMed] [Google Scholar]
- 149.Ma W., Ma C.N., Zhou N.N., Li X.D., Zhang Y.J. Up- regulation of miR-328-3p sensitizes non-small cell lung cancer to radiotherapy. Sci. Rep. 2016;6:31651. doi: 10.1038/srep31651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Xue T., Yin G., Yang W., Chen X., Liu C., Yang W., Zhu J. MiR-129-5p Promotes Radio-sensitivity of NSCLC Cells by Targeting SOX4 and RUNX1. Curr. Cancer Drug Targets. 2021;21:702–712. doi: 10.2174/1568009621666210415094350. [DOI] [PubMed] [Google Scholar]
- 151.Chen G., Yu L., Dong H., Liu Z., Sun Y. MiR-182 enhances radioresistance in non-small cell lung cancer cells by regulating FOXO3. Clin. Exp. Pharmacol. Physiol. 2019;46:137–143. doi: 10.1111/1440-1681.13041. [DOI] [PubMed] [Google Scholar]
- 152.Yuan Y., Liao H., Pu Q., Ke X., Hu X., Ma Y., Luo X., Jiang Q., Gong Y., Wu M., et al. miR-410 induces both epithelial–mesenchymal transition and radioresistance through activation of the PI3K/mTOR pathway in non-small cell lung cancer. Signal Transduct. Target. Ther. 2020;5:85. doi: 10.1038/s41392-020-0182-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Li L., Zhu T., Gao Y.F., Zheng W., Wang C.J., Xiao L., Huang M.S., Yin J.Y., Zhou H.H., Liu Z.Q. Targeting DNA Damage Response in the Radio(Chemo)therapy of Non-Small Cell Lung Cancer. Int. J. Mol. Sci. 2016;17:839. doi: 10.3390/ijms17060839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sharma A., Almasan A. USP14 Regulates DNA Damage Response and Is a Target for Radiosensitization in Non-Small Cell Lung Cancer. Int. J. Mol. Sci. 2020;21:6383. doi: 10.3390/ijms21176383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.da Silva M.S. DNA Double-Strand Breaks: A Double-Edged Sword for Trypanosomatids. Front. Cell Dev. Biol. 2021;9:669041. doi: 10.3389/fcell.2021.669041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Rahimian E., Amini A., Alikarami F., Pezeshki S.M.S., Saki N., Safa M. DNA repair pathways as guardians of the genome: Therapeutic potential and possible prognostic role in hematologic neoplasms. DNA Repair. 2020;96:102951. doi: 10.1016/j.dnarep.2020.102951. [DOI] [PubMed] [Google Scholar]
- 157.Zhang J., Wu Q., Zhu L., Xie S., Tu L., Yang Y., Wu K., Zhao Y., Wang Y., Xu Y., et al. SERPINE2/PN-1 regulates the DNA damage response and radioresistance by activating ATM in lung cancer. Cancer Lett. 2022;524:268–283. doi: 10.1016/j.canlet.2021.10.001. [DOI] [PubMed] [Google Scholar]
- 158.Cao K., Chen Y., Zhao S., Huang Y., Liu T., Liu H., Li B., Cui J., Cai J., Bai C., et al. Sirt3 Promoted DNA Damage Repair and Radioresistance Through ATM-Chk2 in Non-small Cell Lung Cancer Cells. J. Cancer. 2021;12:5464–5472. doi: 10.7150/jca.53173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Li Y., Sun C., Tan Y., Zhang H., Li Y., Zou H. ITGB1 enhances the Radioresistance of human Non-small Cell Lung Cancer Cells by modulating the DNA damage response and YAP1-induced Epithelial-mesenchymal Transition. Int. J. Biol. Sci. 2021;17:635–650. doi: 10.7150/ijbs.52319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kitabatake K., Yoshida E., Kaji T., Tsukimoto M. Involvement of adenosine A2B receptor in radiation-induced translocation of epidermal growth factor receptor and DNA damage response leading to radioresistance in human lung cancer cells. Biochim. Et Biophys. Acta Gen. Subj. 2020;1864:129457. doi: 10.1016/j.bbagen.2019.129457. [DOI] [PubMed] [Google Scholar]
- 161.Ai X., Guo X., Wang J., Stancu A.L., Joslin P.M.N., Zhang D., Zhu S. Targeted therapies for advanced non-small cell lung cancer. Oncotarget. 2018;9:37589–37607. doi: 10.18632/oncotarget.26428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Howlader N., Forjaz G., Mooradian M.J., Meza R., Kong C.Y., Cronin K.A., Mariotto A.B., Lowy D.R., Feuer E.J. The Effect of Advances in Lung-Cancer Treatment on Population Mortality. N. Engl. J. Med. 2020;383:640–649. doi: 10.1056/NEJMoa1916623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Díaz-Serrano A., Gella P., Jiménez E., Zugazagoitia J., Paz-Ares Rodríguez L. Targeting EGFR in Lung Cancer: Current Standards and Developments. Drugs. 2018;78:893–911. doi: 10.1007/s40265-018-0916-4. [DOI] [PubMed] [Google Scholar]
- 164.Roskoski R. Anaplastic lymphoma kinase (ALK) inhibitors in the treatment of ALK-driven lung cancers. Pharmacol. Res. 2017;117:343–356. doi: 10.1016/j.phrs.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 165.Drosten M., Barbacid M. Targeting KRAS mutant lung cancer: Light at the end of the tunnel. Mol. Oncol. 2022;16:1057–1071. doi: 10.1002/1878-0261.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wu S.-G., Shih J.-Y. Management of acquired resistance to EGFR TKI–targeted therapy in advanced non-small cell lung cancer. Mol. Cancer. 2018;17:38. doi: 10.1186/s12943-018-0777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Zhang Y.-L., Yuan J.-Q., Wang K.-F., Fu X.-H., Han X.-R., Threapleton D., Yang Z.-Y., Mao C., Tang J.-L. The prevalence of EGFR mutation in patients with non-small cell lung cancer: A systematic review and meta-analysis. Oncotarget. 2016;7:78985–78993. doi: 10.18632/oncotarget.12587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ayati A., Moghimi S., Salarinejad S., Safavi M., Pouramiri B., Foroumadi A. A review on progression of epidermal growth factor receptor (EGFR) inhibitors as an efficient approach in cancer targeted therapy. Bioorg. Chem. 2020;99:103811. doi: 10.1016/j.bioorg.2020.103811. [DOI] [PubMed] [Google Scholar]
- 169.Passaro A., Jänne P.A., Mok T., Peters S. Overcoming therapy resistance in EGFR-mutant lung cancer. Nat. Cancer. 2021;2:377–391. doi: 10.1038/s43018-021-00195-8. [DOI] [PubMed] [Google Scholar]
- 170.Wagener-Ryczek S., Heydt C., Süptitz J., Michels S., Falk M., Alidousty C., Fassunke J., Ihle M.A., Tiemann M., Heukamp L., et al. Mutational spectrum of acquired resistance to reversible versus irreversible EGFR tyrosine kinase inhibitors. BMC Cancer. 2020;20:408. doi: 10.1186/s12885-020-06920-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lamb Y.N. Osimertinib: A Review in Previously Untreated, EGFR Mutation-Positive, Advanced NSCLC. Target. Oncol. 2021;16:687–695. doi: 10.1007/s11523-021-00839-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Oxnard G.R., Hu Y., Mileham K.F., Husain H., Costa D.B., Tracy P., Feeney N., Sholl L.M., Dahlberg S.E., Redig A.J., et al. Assessment of Resistance Mechanisms and Clinical Implications in Patients With EGFR T790M–Positive Lung Cancer and Acquired Resistance to Osimertinib. JAMA Oncol. 2018;4:1527–1534. doi: 10.1001/jamaoncol.2018.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.To C., Jang J., Chen T., Park E., Mushajiang M., De Clercq D.J.H., Xu M., Wang S., Cameron M.D., Heppner D.E., et al. Single and Dual Targeting of Mutant EGFR with an Allosteric Inhibitor. Cancer Discov. 2019;9:926–943. doi: 10.1158/2159-8290.CD-18-0903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chen Y., Wu J., Yan H., Cheng Y., Wang Y., Yang Y., Deng M., Che X., Hou K., Qu X., et al. Lymecycline reverses acquired EGFR-TKI resistance in non–small-cell lung cancer by targeting GRB2. Pharmacol. Res. 2020;159:105007. doi: 10.1016/j.phrs.2020.105007. [DOI] [PubMed] [Google Scholar]
- 175.Wang L., Dong X., Ren Y., Luo J., Liu P., Su D., Yang X. Targeting EHMT2 reverses EGFR-TKI resistance in NSCLC by epigenetically regulating the PTEN/AKT signaling pathway. Cell Death Dis. 2018;9:129. doi: 10.1038/s41419-017-0120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Jin Q., Zheng J., Chen M., Jiang N., Xu X., Huang F. HIF-1 Inhibitor YC-1 Reverses the Acquired Resistance of EGFR-Mutant HCC827 Cell Line with MET Amplification to Gefitinib. Oxid. Med. Cell. Longev. 2021;2021:6633867. doi: 10.1155/2021/6633867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Cai X., Miao J., Sun R., Wang S., Molina-Vila M.A., Chaib I., Rosell R., Cao P. Dihydroartemisinin overcomes the resistance to osimertinib in EGFR-mutant non-small-cell lung cancer. Pharmacol. Res. 2021;170:105701. doi: 10.1016/j.phrs.2021.105701. [DOI] [PubMed] [Google Scholar]
- 178.Sohoni S., Ghosh P., Wang T., Kalainayakan S.P., Vidal C., Dey S., Konduri P.C., Zhang L. Elevated Heme Synthesis and Uptake Underpin Intensified Oxidative Metabolism and Tumorigenic Functions in Non–Small Cell Lung Cancer Cells. Cancer Res. 2019;79:2511–2525. doi: 10.1158/0008-5472.CAN-18-2156. [DOI] [PubMed] [Google Scholar]
- 179.Dey S., Ashrafi A., Vidal C., Jain N., Kalainayakan S.P., Ghosh P., Alemi P.S., Salamat N., Konduri P.C., Kim J.W., et al. Heme Sequestration Effectively Suppresses the Development and Progression of Both Lung Adenocarcinoma and Squamous Cell Carcinoma. Mol. Cancer Res. 2022;20:139–149. doi: 10.1158/1541-7786.MCR-21-0385. [DOI] [PubMed] [Google Scholar]
- 180.Wang T., Ashrafi A., Konduri P.C., Ghosh P., Dey S., Modareszadeh P., Salamat N., Alemi P.S., Berisha E., Zhang L. Heme Sequestration as an Effective Strategy for the Suppression of Tumor Growth and Progression. Mol. Cancer Ther. 2021;20:2506–2518. doi: 10.1158/1535-7163.MCT-21-0033. [DOI] [PubMed] [Google Scholar]
- 181.Elliott J., Bai Z., Hsieh S.-C., Kelly S.E., Chen L., Skidmore B., Yousef S., Zheng C., Stewart D.J., Wells G.A. ALK inhibitors for non-small cell lung cancer: A systematic review and network meta-analysis. PLoS ONE. 2020;15:e0229179. doi: 10.1371/journal.pone.0229179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Camidge D.R., Dziadziuszko R., Peters S., Mok T., Noe J., Nowicka M., Gadgeel S.M., Cheema P., Pavlakis N., de Marinis F., et al. Updated Efficacy and Safety Data and Impact of the EML4-ALK Fusion Variant on the Efficacy of Alectinib in Untreated ALK-Positive Advanced Non–Small Cell Lung Cancer in the Global Phase III ALEX Study. J. Thorac. Oncol. 2019;14:1233–1243. doi: 10.1016/j.jtho.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 183.Gainor J.F., Varghese A.M., Ou S.H., Kabraji S., Awad M.M., Katayama R., Pawlak A., Mino-Kenudson M., Yeap B.Y., Riely G.J., et al. ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: An analysis of 1683 patients with non-small cell lung cancer. Clin. Cancer Res. 2013;19:4273–4281. doi: 10.1158/1078-0432.CCR-13-0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Gristina V., La Mantia M., Iacono F., Galvano A., Russo A., Bazan V. The Emerging Therapeutic Landscape of ALK Inhibitors in Non-Small Cell Lung Cancer. Pharmaceuticals. 2020;13:474. doi: 10.3390/ph13120474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kazandjian D., Blumenthal G.M., Chen H.-Y., He K., Patel M., Justice R., Keegan P., Pazdur R. FDA Approval Summary: Crizotinib for the Treatment of Metastatic Non-Small Cell Lung Cancer with Anaplastic Lymphoma Kinase Rearrangements. Oncologist. 2014;19:e5–e11. doi: 10.1634/theoncologist.2014-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Camidge D.R., Bang Y.J., Kwak E.L., Iafrate A.J., Varella-Garcia M., Fox S.B., Riely G.J., Solomon B., Ou S.H., Kim D.W., et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: Updated results from a phase 1 study. Lancet Oncol. 2012;13:1011–1019. doi: 10.1016/S1470-2045(12)70344-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wu J., Savooji J., Liu D. Second- and third-generation ALK inhibitors for non-small cell lung cancer. J. Hematol. Oncol. 2016;9:19. doi: 10.1186/s13045-016-0251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Tian W., Zhang P., Yuan Y., Deng X.H., Yue R., Ge X.Z. Efficacy and safety of ceritinib in anaplastic lymphoma kinase-rearranged non-small cell lung cancer: A systematic review and meta-analysis. J. Clin. Pharm. 2020;45:743–754. doi: 10.1111/jcpt.13157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Paik J., Dhillon S. Alectinib: A Review in Advanced, ALK-Positive NSCLC. Drugs. 2018;78:1247–1257. doi: 10.1007/s40265-018-0952-0. [DOI] [PubMed] [Google Scholar]
- 190.Shaw A.T., Bauer T.M., de Marinis F., Felip E., Goto Y., Liu G., Mazieres J., Kim D.-W., Mok T., Polli A., et al. First-Line Lorlatinib or Crizotinib in Advanced ALK-Positive Lung Cancer. N. Engl. J. Med. 2020;383:2018–2029. doi: 10.1056/NEJMoa2027187. [DOI] [PubMed] [Google Scholar]
- 191.Peng L., Lu D., Xia Y., Hong S., Selvaggi G., Stebbing J., Sun Y., Liang F. Efficacy and Safety of First-Line Treatment Strategies for Anaplastic Lymphoma Kinase-Positive Non-Small Cell Lung Cancer: A Bayesian Network Meta-Analysis. Front. Oncol. 2021;11:754768. doi: 10.3389/fonc.2021.754768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Rothenstein J.M., Chooback N. ALK Inhibitors, Resistance Development, Clinical Trials. Curr. Oncol. 2018;25:59–67. doi: 10.3747/co.25.3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Horn L., Wang Z., Wu G., Poddubskaya E., Mok T., Reck M., Wakelee H., Chiappori A.A., Lee D.H., Breder V., et al. Ensartinib vs Crizotinib for Patients With Anaplastic Lymphoma Kinase−Positive Non–Small Cell Lung Cancer: A Randomized Clinical Trial. JAMA Oncol. 2021;7:1617–1625. doi: 10.1001/jamaoncol.2021.3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ou S.-H.I., Nagasaka M., Brazel D., Hou Y., Zhu V.W. Will the clinical development of 4th-generation “double mutant active” ALK TKIs (TPX-0131 and NVL-655) change the future treatment paradigm of ALK+ NSCLC? Transl. Oncol. 2021;14:101191. doi: 10.1016/j.tranon.2021.101191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Cooper A.J., Sequist L.V., Lin J.J. Third-generation EGFR and ALK inhibitors: Mechanisms of resistance and management. Nat. Rev. Clin. Oncol. 2022;19:499–514. doi: 10.1038/s41571-022-00639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Adderley H., Blackhall F.H., Lindsay C.R. KRAS-mutant non-small cell lung cancer: Converging small molecules and immune checkpoint inhibition. EBioMedicine. 2019;41:711–716. doi: 10.1016/j.ebiom.2019.02.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Dunnett-Kane V., Nicola P., Blackhall F., Lindsay C. Mechanisms of Resistance to KRASG12C Inhibitors. Cancers. 2021;13:151. doi: 10.3390/cancers13010151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Liu J., Kang R., Tang D. The KRAS-G12C inhibitor: Activity and resistance. Cancer Gene Ther. 2021;29:875–878. doi: 10.1038/s41417-021-00383-9. [DOI] [PubMed] [Google Scholar]
- 199.Jänne P.A., Riely G.J., Gadgeel S.M., Heist R.S., Ou S.I., Pacheco J.M., Johnson M.L., Sabari J.K., Leventakos K., Yau E., et al. Adagrasib in Non-Small-Cell Lung Cancer Harboring a KRAS(G12C) Mutation. N. Engl. J. Med. 2022;387:120–131. doi: 10.1056/NEJMoa2204619. [DOI] [PubMed] [Google Scholar]
- 200.Skoulidis F., Li B.T., Dy G.K., Price T.J., Falchook G.S., Wolf J., Italiano A., Schuler M., Borghaei H., Barlesi F., et al. Sotorasib for Lung Cancers with KRAS p.G12C Mutation. N. Engl. J. Med. 2021;384:2371–2381. doi: 10.1056/NEJMoa2103695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Tanaka N., Lin J.J., Li C., Ryan M.B., Zhang J., Kiedrowski L.A., Michel A.G., Syed M.U., Fella K.A., Sakhi M., et al. Clinical Acquired Resistance to KRAS(G12C) Inhibition through a Novel KRAS Switch-II Pocket Mutation and Polyclonal Alterations Converging on RAS-MAPK Reactivation. Cancer Discov. 2021;11:1913–1922. doi: 10.1158/2159-8290.CD-21-0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Koga T., Suda K., Fujino T., Ohara S., Hamada A., Nishino M., Chiba M., Shimoji M., Takemoto T., Arita T., et al. KRAS Secondary Mutations That Confer Acquired Resistance to KRAS G12C Inhibitors, Sotorasib and Adagrasib, and Overcoming Strategies: Insights From In Vitro Experiments. J. Thorac. Oncol. 2021;16:1321–1332. doi: 10.1016/j.jtho.2021.04.015. [DOI] [PubMed] [Google Scholar]
- 203.Rao S., Mondragón L., Pranjic B., Hanada T., Stoll G., Köcher T., Zhang P., Jais A., Lercher A., Bergthaler A., et al. AIF-regulated oxidative phosphorylation supports lung cancer development. Cell Res. 2019;29:579–591. doi: 10.1038/s41422-019-0181-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Rebane-Klemm E., Truu L., Reinsalu L., Puurand M., Shevchuk I., Chekulayev V., Timohhina N., Tepp K., Bogovskaja J., Afanasjev V., et al. Mitochondrial Respiration in KRAS and BRAF Mutated Colorectal Tumors and Polyps. Cancers. 2020;12:815. doi: 10.3390/cancers12040815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Zhang H., Chen J. Current status and future directions of cancer immunotherapy. J. Cancer. 2018;9:1773–1781. doi: 10.7150/jca.24577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Sukari A., Nagasaka M., Al-Hadidi A., Lum L.G. Cancer Immunology and Immunotherapy. Anticancer Res. 2016;36:5593. doi: 10.21873/anticanres.11144. [DOI] [PubMed] [Google Scholar]
- 207.Murciano-Goroff Y.R., Warner A.B., Wolchok J.D. The future of cancer immunotherapy: Microenvironment-targeting combinations. Cell Res. 2020;30:507–519. doi: 10.1038/s41422-020-0337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Voena C., Chiarle R. Advances in cancer immunology and cancer immunotherapy. Discov. Med. 2016;21:125–133. [PubMed] [Google Scholar]
- 209.Herbst R.S., Baas P., Kim D.W., Felip E., Pérez-Gracia J.L., Han J.Y., Molina J., Kim J.H., Arvis C.D., Ahn M.J., et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): A randomised controlled trial. Lancet. 2016;387:1540–1550. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 210.Reck M., Rodríguez-Abreu D., Robinson A.G., Hui R., Csőszi T., Fülöp A., Gottfried M., Peled N., Tafreshi A., Cuffe S., et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2016;375:1823–1833. doi: 10.1056/NEJMoa1606774. [DOI] [PubMed] [Google Scholar]
- 211.Garon E.B., Hellmann M.D., Rizvi N.A., Carcereny E., Leighl N.B., Ahn M.J., Eder J.P., Balmanoukian A.S., Aggarwal C., Horn L., et al. Five-Year Overall Survival for Patients With Advanced Non-Small-Cell Lung Cancer Treated With Pembrolizumab: Results From the Phase I KEYNOTE-001 Study. J. Clin. Oncol. 2019;37:2518–2527. doi: 10.1200/JCO.19.00934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Bodor J.N., Kasireddy V., Borghaei H. First-Line Therapies for Metastatic Lung Adenocarcinoma Without a Driver Mutation. J. Oncol. Pract. 2018;14:529–535. doi: 10.1200/JOP.18.00250. [DOI] [PubMed] [Google Scholar]
- 213.Lee H.T., Lee J.Y., Lim H., Lee S.H., Moon Y.J., Pyo H.J., Ryu S.E., Shin W., Heo Y.S. Molecular mechanism of PD-1/PD-L1 blockade via anti-PD-L1 antibodies atezolizumab and durvalumab. Sci. Rep. 2017;7:5532. doi: 10.1038/s41598-017-06002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Fares C.M., Van Allen E.M., Drake C.G., Allison J.P., Hu-Lieskovan S. Mechanisms of Resistance to Immune Checkpoint Blockade: Why Does Checkpoint Inhibitor Immunotherapy Not Work for All Patients? Am. Soc. Clin. Oncol. Educ. Book. 2019;39:147–164. doi: 10.1200/EDBK_240837. [DOI] [PubMed] [Google Scholar]
- 215.Wang F., Wang S., Zhou Q. The Resistance Mechanisms of Lung Cancer Immunotherapy. Front. Oncol. 2020;10:568059. doi: 10.3389/fonc.2020.568059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Hamilton G., Rath B. Immunotherapy for small cell lung cancer: Mechanisms of resistance. Expert Opin. Biol. 2019;19:423–432. doi: 10.1080/14712598.2019.1592155. [DOI] [PubMed] [Google Scholar]
- 217.Bai R., Lv Z., Xu D., Cui J. Predictive biomarkers for cancer immunotherapy with immune checkpoint inhibitors. Biomark Res. 2020;8:34. doi: 10.1186/s40364-020-00209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Gkountakos A., Delfino P., Lawlor R.T., Scarpa A., Corbo V., Bria E. Harnessing the epigenome to boost immunotherapy response in non-small cell lung cancer patients. Adv. Med. Oncol. 2021;13:17588359211006947. doi: 10.1177/17588359211006947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Pore N., Wu S., Standifer N., Jure-Kunkel M., de Los Reyes M., Shrestha Y., Halpin R., Rothstein R., Mulgrew K., Blackmore S., et al. Resistance to Durvalumab and Durvalumab plus Tremelimumab Is Associated with Functional STK11 Mutations in Patients with Non-Small Cell Lung Cancer and Is Reversed by STAT3 Knockdown. Cancer Discov. 2021;11:2828–2845. doi: 10.1158/2159-8290.CD-20-1543. [DOI] [PubMed] [Google Scholar]
- 220.Skoulidis F., Goldberg M.E., Greenawalt D.M., Hellmann M.D., Awad M.M., Gainor J.F., Schrock A.B., Hartmaier R.J., Trabucco S.E., Gay L., et al. STK11/LKB1 Mutations and PD-1 Inhibitor Resistance in KRAS-Mutant Lung Adenocarcinoma. Cancer Discov. 2018;8:822–835. doi: 10.1158/2159-8290.CD-18-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Gutiontov S.I., Turchan W.T., Spurr L.F., Rouhani S.J., Chervin C.S., Steinhardt G., Lager A.M., Wanjari P., Malik R., Connell P.P., et al. CDKN2A loss-of-function predicts immunotherapy resistance in non-small cell lung cancer. Sci. Rep. 2021;11:20059. doi: 10.1038/s41598-021-99524-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Shayan G., Srivastava R., Li J., Schmitt N., Kane L.P., Ferris R.L. Adaptive resistance to anti-PD1 therapy by Tim-3 upregulation is mediated by the PI3K-Akt pathway in head and neck cancer. Oncoimmunology. 2017;6:e1261779. doi: 10.1080/2162402X.2016.1261779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Benci J.L., Xu B., Qiu Y., Wu T.J., Dada H., Twyman-Saint Victor C., Cucolo L., Lee D.S.M., Pauken K.E., Huang A.C., et al. Tumor Interferon Signaling Regulates a Multigenic Resistance Program to Immune Checkpoint Blockade. Cell. 2016;167:1540–1554.e12. doi: 10.1016/j.cell.2016.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Gao J., Shi L.Z., Zhao H., Chen J., Xiong L., He Q., Chen T., Roszik J., Bernatchez C., Woodman S.E., et al. Loss of IFN-γ Pathway Genes in Tumor Cells as a Mechanism of Resistance to Anti-CTLA-4 Therapy. Cell. 2016;167:397–404.e9. doi: 10.1016/j.cell.2016.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Shin D.S., Zaretsky J.M., Escuin-Ordinas H., Garcia-Diaz A., Hu-Lieskovan S., Kalbasi A., Grasso C.S., Hugo W., Sandoval S., Torrejon D.Y., et al. Primary Resistance to PD-1 Blockade Mediated by JAK1/2 Mutations. Cancer Discov. 2017;7:188–201. doi: 10.1158/2159-8290.CD-16-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Gainor J.F., Shaw A.T., Sequist L.V., Fu X., Azzoli C.G., Piotrowska Z., Huynh T.G., Zhao L., Fulton L., Schultz K.R., et al. EGFR Mutations and ALK Rearrangements Are Associated with Low Response Rates to PD-1 Pathway Blockade in Non-Small Cell Lung Cancer: A Retrospective Analysis. Clin. Cancer Res. 2016;22:4585–4593. doi: 10.1158/1078-0432.CCR-15-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Xia L., Yu Y., Lan F., Yan J., Li J., Li W., Xia Y. Case Report: Tumor Microenvironment Characteristics in a Patient With HER2 Mutant Lung Squamous Cell Carcinoma Harboring High PD-L1 Expression Who Presented Hyperprogressive Disease. Front. Oncol. 2021;11:760703. doi: 10.3389/fonc.2021.760703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Horvath L., Thienpont B., Zhao L., Wolf D., Pircher A. Overcoming immunotherapy resistance in non-small cell lung cancer (NSCLC)—Novel approaches and future outlook. Mol. Cancer. 2020;19:141. doi: 10.1186/s12943-020-01260-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Ren S., Xiong X., You H., Shen J., Zhou P. The Combination of Immune Checkpoint Blockade and Angiogenesis Inhibitors in the Treatment of Advanced Non-Small Cell Lung Cancer. Front. Immunol. 2021;12:689132. doi: 10.3389/fimmu.2021.689132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Huang M., Xiong D., Pan J., Zhang Q., Wang Y., Myers C.R., Johnson B.D., Hardy M., Kalyanaraman B., You M. Prevention of Tumor Growth and Dissemination by In Situ Vaccination with Mitochondria-Targeted Atovaquone. Adv. Sci. 2022;9:e2101267. doi: 10.1002/advs.202101267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Kopecka J., Salaroglio I.C., Perez-Ruiz E., Sarmento-Ribeiro A.B., Saponara S., De Las Rivas J., Riganti C. Hypoxia as a driver of resistance to immunotherapy. Drug Resist. Updat. 2021;59:100787. doi: 10.1016/j.drup.2021.100787. [DOI] [PubMed] [Google Scholar]
- 232.Boreel D.F., Span P.N., Heskamp S., Adema G.J., Bussink J. Targeting Oxidative Phosphorylation to Increase the Efficacy of Radio- and Immune-Combination Therapy. Clin. Cancer Res. 2021;27:2970–2978. doi: 10.1158/1078-0432.CCR-20-3913. [DOI] [PubMed] [Google Scholar]
- 233.Saleh R., Elkord E. Acquired resistance to cancer immunotherapy: Role of tumor-mediated immunosuppression. Semin. Cancer Biol. 2020;65:13–27. doi: 10.1016/j.semcancer.2019.07.017. [DOI] [PubMed] [Google Scholar]
- 234.Koyama S., Akbay E.A., Li Y.Y., Herter-Sprie G.S., Buczkowski K.A., Richards W.G., Gandhi L., Redig A.J., Rodig S.J., Asahina H., et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat. Commun. 2016;7:10501. doi: 10.1038/ncomms10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Wu J., Zhu M.X., Li K.S., Peng L., Zhang P.F. Circular RNA drives resistance to anti-PD-1 immunotherapy by regulating the miR-30a-5p/SOX4 axis in non-small cell lung cancer. Cancer Drug Resist. 2022;5:261–270. doi: 10.20517/cdr.2021.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Luo Y.H., Yang Y.P., Chien C.S., Yarmishyn A.A., Adekunle Ishola A., Chien Y., Chen Y.M., Tsai P.H., Lin T.W., Wang M.L., et al. Circular RNA hsa_circ_0000190 Facilitates the Tumorigenesis and Immune Evasion by Upregulating the Expression of Soluble PD-L1 in Non-Small-Cell Lung Cancer. Int. J. Mol. Sci. 2021;23:64. doi: 10.3390/ijms23010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Liu Z., Wang T., She Y., Wu K., Gu S., Li L., Dong C., Chen C., Zhou Y. N(6)-methyladenosine-modified circIGF2BP3 inhibits CD8(+) T-cell responses to facilitate tumor immune evasion by promoting the deubiquitination of PD-L1 in non-small cell lung cancer. Mol. Cancer. 2021;20:105. doi: 10.1186/s12943-021-01398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Zhang P.F., Pei X., Li K.S., Jin L.N., Wang F., Wu J., Zhang X.M. Circular RNA circFGFR1 promotes progression and anti-PD-1 resistance by sponging miR-381-3p in non-small cell lung cancer cells. Mol. Cancer. 2019;18:179. doi: 10.1186/s12943-019-1111-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Chen S.W., Zhu S.Q., Pei X., Qiu B.Q., Xiong D., Long X., Lin K., Lu F., Xu J.J., Wu Y.B. Cancer cell-derived exosomal circUSP7 induces CD8(+) T cell dysfunction and anti-PD1 resistance by regulating the miR-934/SHP2 axis in NSCLC. Mol. Cancer. 2021;20:144. doi: 10.1186/s12943-021-01448-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Huang J., Liu D., Wang Y., Liu L., Li J., Yuan J., Jiang Z., Jiang Z., Hsiao W.W., Liu H., et al. Ginseng polysaccharides alter the gut microbiota and kynurenine/tryptophan ratio, potentiating the antitumour effect of antiprogrammed cell death 1/programmed cell death ligand 1 (anti-PD-1/PD-L1) immunotherapy. Gut. 2022;71:734–745. doi: 10.1136/gutjnl-2020-321031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Maby P., Tougeron D., Hamieh M., Mlecnik B., Kora H., Bindea G., Angell H.K., Fredriksen T., Elie N., Fauquembergue E., et al. Correlation between Density of CD8+ T-cell Infiltrate in Microsatellite Unstable Colorectal Cancers and Frameshift Mutations: A Rationale for Personalized Immunotherapy. Cancer Res. 2015;75:3446–3455. doi: 10.1158/0008-5472.CAN-14-3051. [DOI] [PubMed] [Google Scholar]
- 242.Klempner S.J., Fabrizio D., Bane S., Reinhart M., Peoples T., Ali S.M., Sokol E.S., Frampton G., Schrock A.B., Anhorn R., et al. Tumor Mutational Burden as a Predictive Biomarker for Response to Immune Checkpoint Inhibitors: A Review of Current Evidence. Oncologist. 2020;25:e147–e159. doi: 10.1634/theoncologist.2019-0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Le D.T., Durham J.N., Smith K.N., Wang H., Bartlett B.R., Aulakh L.K., Lu S., Kemberling H., Wilt C., Luber B.S., et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–413. doi: 10.1126/science.aan6733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Olivares-Hernández A., Del Barco Morillo E., Parra Pérez C., Miramontes-González J.P., Figuero-Pérez L., Martín-Gómez T., Escala-Cornejo R., Bellido Hernández L., González Sarmiento R., Cruz-Hernández J.J., et al. Influence of DNA Mismatch Repair (MMR) System in Survival and Response to Immune Checkpoint Inhibitors (ICIs) in Non-Small Cell Lung Cancer (NSCLC): Retrospective Analysis. Biomedicines. 2022;10:360. doi: 10.3390/biomedicines10020360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Aggarwal C., Somaiah N., Simon G. Antiangiogenic agents in the management of non-small cell lung cancer: Where do we stand now and where are we headed? Cancer Biol. 2012;13:247–263. doi: 10.4161/cbt.19594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Voron T., Marcheteau E., Pernot S., Colussi O., Tartour E., Taieb J., Terme M. Control of the immune response by pro-angiogenic factors. Front. Oncol. 2014;4:70. doi: 10.3389/fonc.2014.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Sica V., Bravo-San Pedro J.M., Stoll G., Kroemer G. Oxidative phosphorylation as a potential therapeutic target for cancer therapy. Int. J. Cancer. 2020;146:10–17. doi: 10.1002/ijc.32616. [DOI] [PubMed] [Google Scholar]
- 248.Hellmann M., Jänne P., Opyrchal M., Hafez N., Raez L., Gabrilovich D., Wang F., Ordentlich P., Brouwer S., Sankoh S., et al. OA05.01 Efficacy/Safety of Entinostat (ENT) and Pembrolizumab (PEMBRO) in NSCLC Patients Previously Treated with Anti-PD-(L)1 Therapy. J. Thorac. Oncol. 2018;13:S330. doi: 10.1016/j.jtho.2018.08.257. [DOI] [Google Scholar]
- 249.Routy B., Le Chatelier E., Derosa L., Duong C.P.M., Alou M.T., Daillère R., Fluckiger A., Messaoudene M., Rauber C., Roberti M.P., et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359:91–97. doi: 10.1126/science.aan3706. [DOI] [PubMed] [Google Scholar]
- 250.He D., Li X., An R., Wang L., Wang Y., Zheng S., Chen X., Wang X. Response to PD-1-Based Immunotherapy for Non-Small Cell Lung Cancer Altered by Gut Microbiota. Oncol. Ther. 2021;9:647–657. doi: 10.1007/s40487-021-00171-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Fang C., Fang W., Xu L., Gao F., Hou Y., Zou H., Ma Y., Moll J.M., Yang Y., Wang D., et al. Distinct Functional Metagenomic Markers Predict the Responsiveness to Anti-PD-1 Therapy in Chinese Non-Small Cell Lung Cancer Patients. Front. Oncol. 2022;12:837525. doi: 10.3389/fonc.2022.837525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Insinga R.P., Feliciano J.L., Qiao N., Vandormael K., Zhang Y. Cost-effectiveness of pembrolizumab + chemotherapy versus chemotherapy and pembrolizumab monotherapy in first line treatment of NSCLC in the US—Updated analyses with additional trial follow-up. J. Med. Econ. 2021;24:792–805. doi: 10.1080/13696998.2021.1937188. [DOI] [PubMed] [Google Scholar]
- 253.Socinski M.A., Jotte R.M., Cappuzzo F., Orlandi F., Stroyakovskiy D., Nogami N., Rodríguez-Abreu D., Moro-Sibilot D., Thomas C.A., Barlesi F., et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N. Engl. J. Med. 2018;378:2288–2301. doi: 10.1056/NEJMoa1716948. [DOI] [PubMed] [Google Scholar]
- 254.Huang M.-Y., Jiang X.-M., Wang B.-L., Sun Y., Lu J.-J. Combination therapy with PD-1/PD-L1 blockade in non-small cell lung cancer: Strategies and mechanisms. Pharmacol. Ther. 2021;219:107694. doi: 10.1016/j.pharmthera.2020.107694. [DOI] [PubMed] [Google Scholar]
- 255.Gandhi L., Rodríguez-Abreu D., Gadgeel S., Esteban E., Felip E., De Angelis F., Domine M., Clingan P., Hochmair M.J., Powell S.F., et al. Pembrolizumab plus Chemotherapy in Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2018;378:2078–2092. doi: 10.1056/NEJMoa1801005. [DOI] [PubMed] [Google Scholar]
- 256.Gadgeel S., Rodríguez-Abreu D., Speranza G., Esteban E., Felip E., Dómine M., Hui R., Hochmair M.J., Clingan P., Powell S.F., et al. Updated Analysis From KEYNOTE-189: Pembrolizumab or Placebo Plus Pemetrexed and Platinum for Previously Untreated Metastatic Nonsquamous Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2020;38:1505–1517. doi: 10.1200/JCO.19.03136. [DOI] [PubMed] [Google Scholar]
- 257.Paz-Ares L., Luft A., Vicente D., Tafreshi A., Gümüş M., Mazières J., Hermes B., Çay Şenler F., Csőszi T., Fülöp A., et al. Pembrolizumab plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018;379:2040–2051. doi: 10.1056/NEJMoa1810865. [DOI] [PubMed] [Google Scholar]
- 258.West H., McCleod M., Hussein M., Morabito A., Rittmeyer A., Conter H.J., Kopp H.G., Daniel D., McCune S., Mekhail T., et al. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): A multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:924–937. doi: 10.1016/S1470-2045(19)30167-6. [DOI] [PubMed] [Google Scholar]
- 259.Reck M., Ciuleanu T.-E., Dols M.C., Schenker M., Zurawski B., Menezes J., Richardet E., Bennouna J., Felip E., Juan-Vidal O., et al. Nivolumab (NIVO) + ipilimumab (IPI) + 2 cycles of platinum-doublet chemotherapy (chemo) vs 4 cycles chemo as first-line (1L) treatment (tx) for stage IV/recurrent non-small cell lung cancer (NSCLC): CheckMate 9LA. J. Clin. Oncol. 2020;38:9501. doi: 10.1200/JCO.2020.38.15_suppl.9501. [DOI] [Google Scholar]
- 260.Galffy G., Lugowska I., Poddubskaya E., Cho B.C., Ahn M.-J., Han J.-Y., Su W.-C., Hauke R., Dyar S., Lee D.H., et al. 281 JAVELIN Medley VEGF: Phase 2 study of avelumab + axitinib in patients with previously treated non-small cell lung cancer (NSCLC) or treatment naive, cisplatin-ineligible urothelial cancer (UC) J. ImmunoTherapy Cancer. 2020;8:A171. doi: 10.1136/jitc-2020-SITC2020.0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Hellmann M.D., Paz-Ares L., Bernabe Caro R., Zurawski B., Kim S.-W., Carcereny Costa E., Park K., Alexandru A., Lupinacci L., de la Mora Jimenez E., et al. Nivolumab plus Ipilimumab in Advanced Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2019;381:2020–2031. doi: 10.1056/NEJMoa1910231. [DOI] [PubMed] [Google Scholar]
- 262.Theelen W.S.M.E., Peulen H.M.U., Lalezari F., van der Noort V., de Vries J.F., Aerts J.G.J.V., Dumoulin D.W., Bahce I., Niemeijer A.-L.N., de Langen A.J., et al. Effect of Pembrolizumab After Stereotactic Body Radiotherapy vs Pembrolizumab Alone on Tumor Response in Patients With Advanced Non–Small Cell Lung Cancer: Results of the PEMBRO-RT Phase 2 Randomized Clinical Trial. JAMA Oncol. 2019;5:1276–1282. doi: 10.1001/jamaoncol.2019.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Morganti S., Curigliano G. Combinations using checkpoint blockade to overcome resistance. Ecancermedicalscience. 2020;14:1148. doi: 10.3332/ecancer.2020.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Hrustanovic G., Olivas V., Pazarentzos E., Tulpule A., Asthana S., Blakely C.M., Okimoto R.A., Lin L., Neel D.S., Sabnis A., et al. RAS-MAPK dependence underlies a rational polytherapy strategy in EML4-ALK–positive lung cancer. Nat. Med. 2015;21:1038–1047. doi: 10.1038/nm.3930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Planchard D., Besse B., Groen H.J.M., Souquet P.-J., Quoix E., Baik C.S., Barlesi F., Kim T.M., Mazieres J., Novello S., et al. Dabrafenib plus trametinib in patients with previously treated BRAFV600E-mutant metastatic non-small cell lung cancer: An open-label, multicentre phase 2 trial. Lancet Oncol. 2016;17:984–993. doi: 10.1016/S1470-2045(16)30146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Tricker E.M., Xu C., Uddin S., Capelletti M., Ercan D., Ogino A., Pratilas C.A., Rosen N., Gray N.S., Wong K.-K., et al. Combined EGFR/MEK Inhibition Prevents the Emergence of Resistance in EGFR-Mutant Lung Cancer. Cancer Discov. 2015;5:960–971. doi: 10.1158/2159-8290.CD-15-0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Canon J., Rex K., Saiki A.Y., Mohr C., Cooke K., Bagal D., Gaida K., Holt T., Knutson C.G., Koppada N., et al. The clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumour immunity. Nature. 2019;575:217–223. doi: 10.1038/s41586-019-1694-1. [DOI] [PubMed] [Google Scholar]
- 268.Hallin J., Engstrom L.D., Hargis L., Calinisan A., Aranda R., Briere D.M., Sudhakar N., Bowcut V., Baer B.R., Ballard J.A., et al. The KRAS G12C Inhibitor MRTX849 Provides Insight toward Therapeutic Susceptibility of KRAS-Mutant Cancers in Mouse Models and Patients. Cancer Discov. 2020;10:54–71. doi: 10.1158/2159-8290.CD-19-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Jiao D., Yang S. Overcoming Resistance to Drugs Targeting KRAS Mutation. Innovation. 2020;1:100035. doi: 10.1016/j.xinn.2020.100035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Wang Y., Deng W., Li N., Neri S., Sharma A., Jiang W., Lin S.H. Combining Immunotherapy and Radiotherapy for Cancer Treatment: Current Challenges and Future Directions. Front. Pharm. 2018;9:185. doi: 10.3389/fphar.2018.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Schoenhals J.E., Seyedin S.N., Tang C., Cortez M.A., Niknam S., Tsouko E., Chang J.Y., Hahn S.M., Welsh J.W. Preclinical Rationale and Clinical Considerations for Radiotherapy Plus Immunotherapy: Going Beyond Local Control. Cancer J. 2016;22:130–137. doi: 10.1097/PPO.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 272.Gong X., Li X., Jiang T., Xie H., Zhu Z., Zhou F., Zhou C. Combined Radiotherapy and Anti-PD-L1 Antibody Synergistically Enhances Antitumor Effect in Non-Small Cell Lung Cancer. J. Thorac. Oncol. 2017;12:1085–1097. doi: 10.1016/j.jtho.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 273.Cruz-Bermúdez A., Laza-Briviesca R., Vicente-Blanco R.J., García-Grande A., Coronado M.J., Laine-Menéndez S., Alfaro C., Sanchez J.C., Franco F., Calvo V., et al. Cancer-associated fibroblasts modify lung cancer metabolism involving ROS and TGF-β signaling. Free Radic. Biol. Med. 2019;130:163–173. doi: 10.1016/j.freeradbiomed.2018.10.450. [DOI] [PubMed] [Google Scholar]
- 274.Chambers J.M., Wingert R.A. PGC-1α in Disease: Recent Renal Insights into a Versatile Metabolic Regulator. Cells. 2020;9:2234. doi: 10.3390/cells9102234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Paredes F., Sheldon K., Lassègue B., Williams H.C., Faidley E.A., Benavides G.A., Torres G., Sanhueza-Olivares F., Yeligar S.M., Griendling K.K., et al. Poldip2 is an oxygen-sensitive protein that controls PDH and αKGDH lipoylation and activation to support metabolic adaptation in hypoxia and cancer. Proc. Natl. Acad. Sci. USA. 2018;115:1789–1794. doi: 10.1073/pnas.1720693115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Palazon A., Goldrath A.W., Nizet V., Johnson R.S. HIF Transcription Factors, Inflammation, and Immunity. Immunity. 2014;41:518–528. doi: 10.1016/j.immuni.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Horsman M.R., Overgaard J. The impact of hypoxia and its modification of the outcome of radiotherapy. J. Radiat Res. 2016;57((Suppl. S1)):i90–i98. doi: 10.1093/jrr/rrw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Farge T., Saland E., de Toni F., Aroua N., Hosseini M., Perry R., Bosc C., Sugita M., Stuani L., Fraisse M., et al. Chemotherapy-Resistant Human Acute Myeloid Leukemia Cells Are Not Enriched for Leukemic Stem Cells but Require Oxidative Metabolism. Cancer Discov. 2017;7:716–735. doi: 10.1158/2159-8290.CD-16-0441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Kuntz E.M., Baquero P., Michie A.M., Dunn K., Tardito S., Holyoake T.L., Helgason G.V., Gottlieb E. Targeting mitochondrial oxidative phosphorylation eradicates therapy-resistant chronic myeloid leukemia stem cells. Nat. Med. 2017;23:1234–1240. doi: 10.1038/nm.4399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Navarro P., Bueno M.J., Zagorac I., Mondejar T., Sanchez J., Mourón S., Muñoz J., Gómez-López G., Jimenez-Renard V., Mulero F., et al. Targeting Tumor Mitochondrial Metabolism Overcomes Resistance to Antiangiogenics. Cell Rep. 2016;15:2705–2718. doi: 10.1016/j.celrep.2016.05.052. [DOI] [PubMed] [Google Scholar]
- 281.Zhang G., Frederick D.T., Wu L., Wei Z., Krepler C., Srinivasan S., Chae Y.C., Xu X., Choi H., Dimwamwa E., et al. Targeting mitochondrial biogenesis to overcome drug resistance to MAPK inhibitors. J. Clin. Investig. 2016;126:1834–1856. doi: 10.1172/JCI82661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Ghosh P., Guo Y., Ashrafi A., Chen J., Dey S., Zhong S., Liu J., Campbell J., Konduri P.C., Gerberich J., et al. Oxygen-Enhanced Optoacoustic Tomography Reveals the Effectiveness of Targeting Heme and Oxidative Phosphorylation at Normalizing Tumor Vascular Oxygenation. Cancer Res. 2020;80:3542–3555. doi: 10.1158/0008-5472.CAN-19-3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Tardi P., Johnstone S., Harasym N., Xie S., Harasym T., Zisman N., Harvie P., Bermudes D., Mayer L. In vivo maintenance of synergistic cytarabine:daunorubicin ratios greatly enhances therapeutic efficacy. Leuk. Res. 2009;33:129–139. doi: 10.1016/j.leukres.2008.06.028. [DOI] [PubMed] [Google Scholar]
- 284.Livney Y.D., Assaraf Y.G. Rationally designed nanovehicles to overcome cancer chemoresistance. Adv. Drug Deliv. Rev. 2013;65:1716–1730. doi: 10.1016/j.addr.2013.08.006. [DOI] [PubMed] [Google Scholar]