Abstract
Many governments aim to mitigate health risks by attacking nutritional failures. In this article, we exploit a unique natural experiment, the COVID-19 pandemic as an exogenous public health shock, to estimate the learning effects of intensive health information campaigns on nutrient intake during the pandemic. Using data from nearly-one million food purchases in China, our empirical findings strongly support the learning effect in explaining improvements in nutrient intake in the post-COVID-19 period. We conclude that when public health shocks occur, policy makers can boost relevant learning mechanisms by promoting information and education to improve individuals’ awareness of preventive health behaviors of a more permanent nature, which can lead to health improvements in a society.
Keywords: Health behavior, COVID-19, Nutrition, Diet quality, Learning
1. Introduction
Many governments aim to mitigate health risks by attacking nutritional failures. To achieve such a goal, economists have often advocated the use of pricing mechanisms, such as obesity and junk food taxes or subsidies for healthy foods, but the effectiveness of these policies in promoting health outcomes remains controversial (see Alston et al., 2016, for a review). Alternatively, non-price policies, such as health information provision, including nutrition education programs; effective nutrition labeling on food packages; and health campaigns, have shown great potential to encourage improved nutrient intake through learning effects. Although the impact of health information provision on inattentive individuals is shown to be limited because of its salient features (e.g., Cawley and Ruhm, 2012), these findings shed light on when health information provision could effectively trigger a learning mechanism. For example, Agüero and Beleche (2017) show that the H1N1 pandemic, rather than seasonal flu, significantly altered long-run health behaviors in Mexico.
In this article, we use food purchases in China to illustrate the learning effect on health behaviors, specifically improvement in nutrient intake, during the COVID-19 pandemic and after if came under control. When the nation announced the first large-scale outbreak of COVID-19 on January 23, 2020 (the date of the Wuhan lockdown), the government and society experienced great pressures from the pandemic due to limited knowledge about the new virus. Chinese health authorities’ first response was to start intensive, nationwide information campaigns about adopting health behaviors to limit the spread of the virus, such as handwashing, wearing masks, sanitizing, and following a healthier diet to build strong immune systems. The novel virus was soon discovered to be highly transmittable and lethal, providing surprising changes in the state of nature that may effectively have triggered learning mechanisms to improve health behaviors.
Although we find a deterioration of nutrient intake during the active periods of COVID-19 infections, when we extend our analysis to the period when infections were under control, we observe a sharp increase in the consumption of good nutrients and a decrease in bad nutrients relative to before or during the COVID-19 active period. Specifically, COVID-19 infections increased the daily consumption of “bad” nutrients (sugar, sodium, and fat) by 0.1 to 1 percent and decreased consumption of “good” nutrients (fiber and protein) by 0.1 to 0.6 percent. When infections were under control, we find an increase of almost 1 and 8 percent for fiber and protein and a decrease of 7 to 16 percent in fat, sugar, and sodium. These increases are more substantial when compared to the COVID-19 active period.
Our findings contribute to the literature that seeks to better understand the adoption of health behaviors to improve public health (Allcott et al., 2020, Agüero and Beleche, 2017, Hanna et al., 2016). The results emphasize the importance of understanding nutrient intake during the COVID-19 pandemic, which has been largely overlooked even though the U.S. Centers for Disease Control and Prevention (2020), the World Health Organization (2020), and others have identified obesity as one of the co-morbidities that poses increased risk of severe illness or death from COVID-19. Our results support the ongoing policy debates highlighting the importance of a healthy diet in combatting or mitigating severe illness from the COVID-19 virus and the role public health institutions can play (Di Renzo et al., 2020, Naja and Hamadeh, 2020, Zimmer, 2020).
This article contributes to the growing body of research on the importance of behavioral mechanisms when individuals make decisions about nutrient intake. For instance, Smith, 2012, Staudigel, 2016 document emotional eating behaviors stemming from adverse economic conditions. Salience is also broadly discussed for other health issues, ranging from hospital rankings (Cutler et al., 2004, Pope, 2009) to restaurant hygiene alerts (Jin and Leslie, 2003, Dai and Luca, 2020). Similar to our work, Bennett et al., 2015, Agüero and Beleche, 2017 discuss the learning effect from public health shocks such as SARSs and H1N1.
Finally, this article also contributes to the handful of economic studies using a detailed account of nutrition information to capture the healthfulness of meals (i.e., Anderson et al., 2018; Zhu et al., 2016), in contrast to most studies, which use dummy variables like nutrition program enrollment (Belot and James, 2011, Chakraborty and Jayaraman, 2019) or indirect measures such as children’s heights (Thomsen et al., 2016), or that classify products into broad food groups (Oster, 2018).
2. Data and empirical strategy
2.1. Data on food purchases
The two main datasets used consists of: (1) daily COVID-19 case counts collected from local city and national health committee websites; and (2) 966,193 transactions for food delivery drawn from a confidential proprietary dataset from a restaurant conglomerate in China. In 2019, the conglomerate’s total food delivery sales reached 154 million RMB (around 18 million U.S. dollars), or 2.4 percent of China’s food delivery market in the restaurant industry. To meet the 30- to 60-minute time requirement for delivery and to minimize transportation costs, dishes in delivery transactions are usually prepared at the restaurants instead of centralized factories. The conglomerate owns four different chains, and we utilize the transaction data for food delivery from 72 restaurant locations in its largest chain, which potentially covers 138 million people in 10 cities across China.4 In 2019, the total market size for food deliveries in China reached 603.5 billion RMB (around 86 billion USD). Most food delivery transactions are submitted through the two largest online delivery platforms, Meituan-Dianping and Ele.me (like Yelp and TripAdvisor). To strip out the impact of COVID-19 from other factors, we truncate the sample from January 1 through May 31, 2020, because the second outbreak in China occurred in early June 2020.
2.2. Measurements of nutrient intake
The dependent variable used in the empirical models is the average nutritional content per transaction. To construct the nutrition measure, we first use the chain’s recipe data to collect the names and amounts of ingredients used for all dishes and then convert the ingredient amounts to nutrients using the China Food Composition Tables (Chinese Center for Disease Control and Prevention, 2019). We then calculate the average nutritional content per transaction by dividing the sum of the nutrients scaled by the energy content, adjusting for portion sizes. The nutrients included in the analysis are both nutrients-to-limit or “bad” nutrients (fat, sugar, and sodium) and nutrients-to-encourage or “good” nutrients (fiber and protein).5 In total, we utilize nine nutrients. The food is prepared following standard recipes and any changes are recorded. Updates of recipes are not frequent, and most updates only focus on one dish.6
In addition to individual nutrients, we also utilize two summary indices of nutrition. To this end, we calculate Nutrient Rich Food (NRF) scores using individual nutrient information per transaction. NRF scores have been compared extensively to other methods and have been validated with respect to measuring a healthy diet.7 Finally, we explore the robustness of our results by utilizing the Nutrient Profiling Index (NPI) system developed by the Food Standards Agency of the U.K. Department of Health in 2004–2005. NPI uses a scoring system to balance the contribution made by beneficial nutrients with nutrients that should be eaten less (U.K. Department of Health, 2011).8 We normalize NPI to range between 0 and 100, with higher values representing healthier nutritional choices.
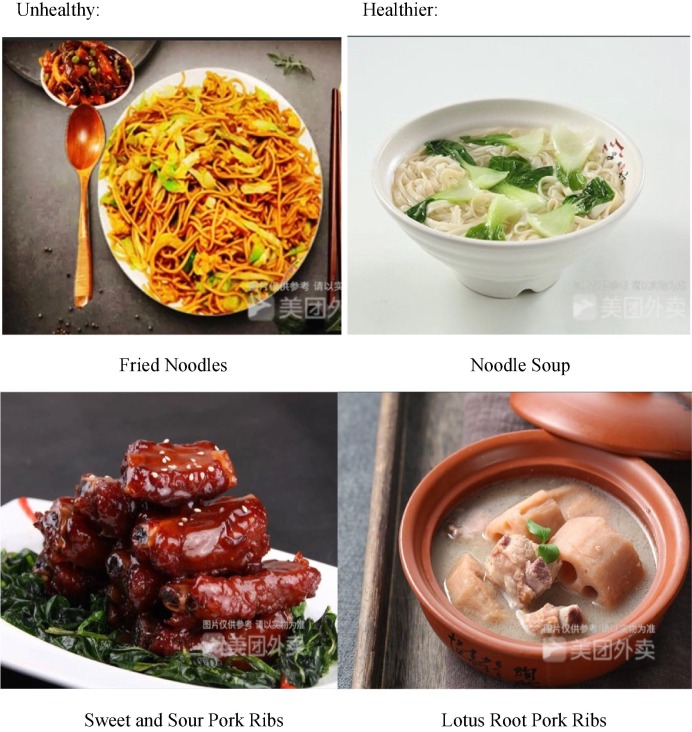
One potential issue is an individual’s lack of knowledge of the nutrient content of the various dishes. This is unlikely to occur in our study because customers are mainly from the middle-income population in China, which have relative high levels of educational attainment. In addition, in China there is also common about the nutritional characteristics of different cooking methods. For example, steamed dishes are healthier than deep-fried ones. Consider four popular dishes in our sample, which are displayed in Fig. 2. Fried noodles contain more oil and saturated fat than noodle soup, and sweet and sour pork ribs are less healthy than lotus root pork ribs soup because of more added sugars. In addition, healthfulness of animal protein dishes is familiar to most people through traditional Chinese wisdom, such as “no-legged meat [fish] is healthier than two-legged meat [chicken]; two-legged is healthier than four-legged [pork].”
Fig. 2.
Illustration of the Heathfulness of Popular Dishes by Tupe of Cooking.
2.3. COVID-19 data and other control variables
We use two variables to account for the contemporaneous presence of COVID-19 when the dish orders are placed: (1) daily city-level infection counts, and (2) daily national-level infection counts, both of which are collected from the Chinese Health Committee websites. We match the daily COVID data with daily food purchases. We eliminate data from February 12, 2020, as it is an obvious outlier.9 We also exclude new infections among international travelers because our sampled city governments required them to undergo centralized quarantine beginning in early March, and, as a result, they are unlikely to have an impact on local individuals’ nutritional decisions.
Control variables to account for other factors include the average price per dish, the discount rate, the portion size per transaction, proxies for demographic variables, and population mobility indexes. The average price per dish is calculated by dividing a transaction’s expenditure by the number of dishes. For the discount rate, we divide the revenue realized per transaction by the sum of menu prices multiplied by the number of dishes in this transaction.10 We use portion size to control for the number of people that the dishes serve, which is calculated by summing of the weight of all ingredients.11 We also control for restaurant fixed effects to account for time-invariant regional impact and use a set of time fixed effects, including the time when the transaction was received, day of the week, and a month dummy, to account for seasonal changes.
We do not directly observe demographics associated with transactions, raising a concern is the potential for omitted variable bias on the demand side.12 To address this, we employ several data strategies. First, we use two proxies for income: daily automobile traffic (denoted as income1) and monthly foot traffic within a three-kilometer radius of each of the 72 restaurant locations in our sample (denoted as income2).13 Second, we also use city-month interactions to account for potential time-varying variations in demographics such as income. Third, we also utilize unsupervised machine learning techniques that have performed favorably in the estimation of demand without demographics and geographic variables (Blumberg and Thompson, 2021).
We also use a population mobility index to account for the impact of mobility restrictions implemented by China’s government during the pandemic. Mobility data tracks people’s movement between cities. Gao-de offers location-based service (LBS), based on the global positioning system (GPS), IP addresses, locations of signaling towers, Wi-Fi for online searching and mapping, and a large variety of apps and software on mobile devices (Lai et al., 2020) to construct the mobility index. The index is classified as population inflows and outflows.
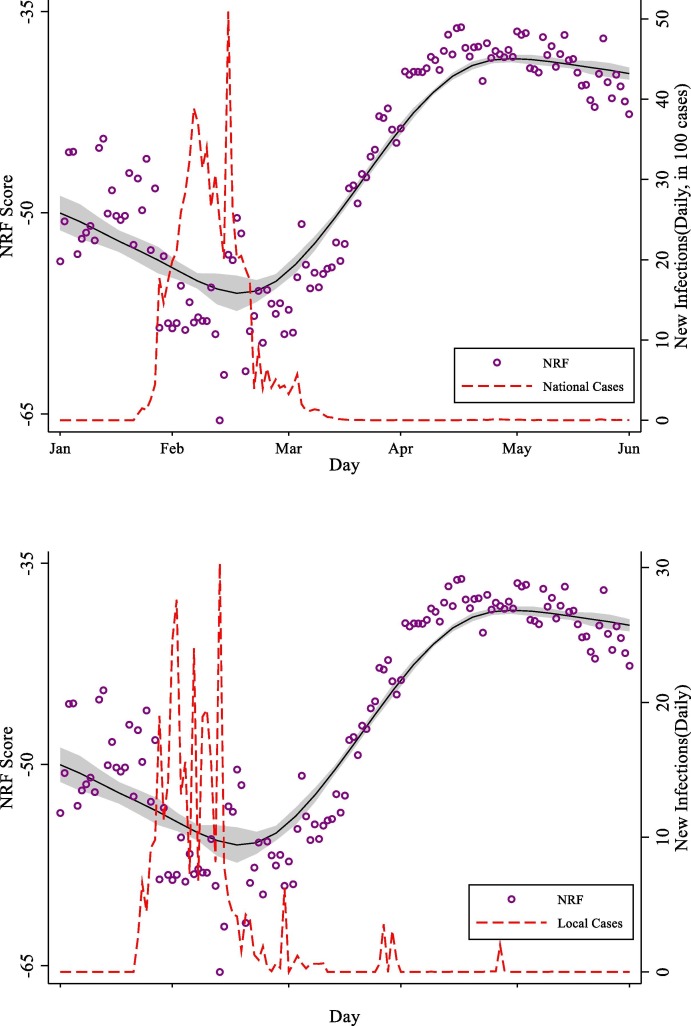
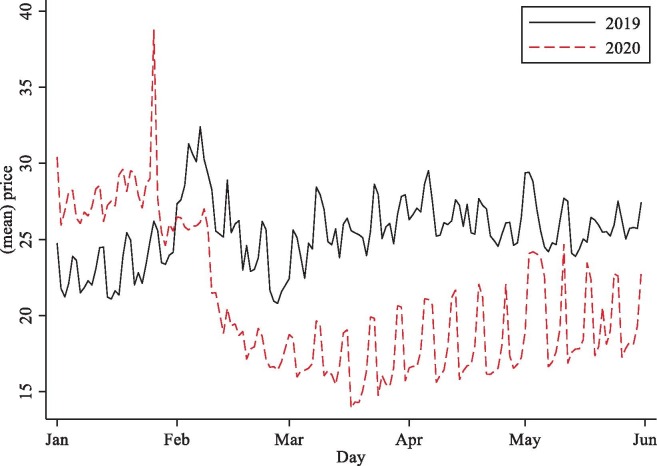
Table 1 presents a summary of the definitions and statistics of the variables used in the empirical analysis. Fig. 1 illustrates the trends in average NRF scores and the number of daily COVID-19 infections between January and June 2020. The upper panel shows that overall nutrition intake deteriorates up to March 2020, after which it appears to improve, reaching levels higher than those preceding the pandemic. The upper panel also suggests an inverse relationship between the number of infections and nutrient intake. To further illustrate this point, the lower panel plots the average NRF scores vs the number of infections regardless of dates, and it indicates a negative association between the two variables.
Table 1.
Summary of Variable Definitions and Statistics.
| Category | Variable Name | Variable Definition | Observations | Mean | Std. Dev |
|---|---|---|---|---|---|
| Nutrition Measures | Fiber | Avg. fiber contents per transaction (grams) | 966,193 | 1.66 | 1.386 |
| Fat | Avg. fat contents per transaction (grams) | 966,193 | 16.23 | 9.816 | |
| Sugar | Avg. sugar contents per transaction (grams) | 966,193 | 21.55 | 13.29 | |
| Sodium | Avg. sodium contents per transaction (mg) | 966,193 | 568.547 | 490.182 | |
| Protein | Avg. sodium contents per transaction (grams) | 966,193 | 8.504 | 4.453 | |
| NRF | Nutrition-Rich-Food score | 966,193 | −39.04 | 50.78 | |
| NPI | Nutrition Profile index | 966,193 | 41.57 | 12.92 | |
| COVID-19 | National | Daily number of infections at national level divided by 100 | 388,094 | 1.271 | 5.31 |
| Local | Daily number of infections at local level | 388,094 | 0.721 | 3.19 | |
| Income Proxies | Income1 | Daily traffic flow (restaurant-level) | 4,641 | 20.941 | 4.877 |
| Income2 | Monthly population flow (restaurant-level) | 4,641 | 0.257 | 0.246 | |
| Baseline Controls | Price | Average price per dish in a transaction | 966,193 | 23.02 | 12.331 |
| Discount | Discount rate per transaction | 966,193 | 0.748 | 0.159 | |
| Portion size | Total portion size per transaction (grams) | 966,193 | 688.932 | 600.065 | |
| Number of transactions | Daily number of transactions in a restaurant | 966,193 | 81.16 | 55.913 | |
| move_out | Gaode Index for population move-out | 1,820 | 31.12 | 24.00 | |
| move_in | Gaode Index for population move-in | 1,820 | 33.99 | 22.81 | |
| City-month | Interaction term between city and month dummies | 966,193 | 0.033 | 0.180 | |
| Post1 | Dummy = 1 for period Mar 19-May 31, 2020; =0 for Jan 1 to Jan 22, 2020 | 317,921 | 0.768 | 0.422 | |
| Post2 | Dummy = 1 for period Mar 19-May 31, 2020; =0 for Jan 23 to Mar 18, 2020 | 314,223 | 0.777 | 0.416 | |
| No. of Obs.: | 966,193 |
All values reported are means of transaction-level observations for both periods from January 1-May 31 for the years 2019 and 2020. The number of observations is 388,094 in the 2019 sample and 578,099 in the 2020 sample. Instead of reporting all dummy variables, we report only city-month interactions. In total, we have 18 interactions after multiplying nine city dummies by month dummies. Other fixed effects included in the regressions are restaurant dummies, city dummies, day-of-week dummies, hour dummies (which hour in a day that the transaction happens), and month dummies.
Fig. 1.
COVID-19 Infections and Nutrition.
2.4. Estimation strategy
To investigate the impact of the COVID-19 pandemic more formally on nutrient intake, based on transaction-level food deliveries, we propose the following model:
| (1) |
where is the individual nutrient content or nutrition index (NRF or NPI) contained in food delivery i from restaurant j in city c on day t. is the number of infections in city c on day t, and is the number of infections throughout China on day t. Other control variables are denoted by . and denote restaurant, city, and month fixed effects. is the unobserved term. We estimate equation (1) for the benchmark results using weighted least squares, with food delivery transactions in restaurant on day t used as the weight.
Given that we do not observe individual household demographics, the main identification concern using equation (1) is the omitted demographic variables contained in the error term . That is,
| (2) |
where is the i.i.d distributed error, are the time-invariant demographics, and are the time-variant demographics. are likely to affect nutrient intake, but they are not correlated with the pandemic because they are time-invariant. are the time-variant demographics that may affect diet choices and correlate with COVID-19 case counts. In this case, the estimates of COVID-19 may be biased by absorbing the impact of changes in unobserved demographics during the pandemic. We address this issue in the following ways.
First, are unlikely to be substantial for an individual who orders deliveries from the restaurants in our sample. The restaurants are more frequently visited by middle- and high-income groups, given the average spending per transaction.14 As shown by Chetty et al. (2020), income variations led by the COVID-19 pandemic in the U.S. are mainly incurred by the low-income population, while income decreases modestly for the middle- and high-income populations. A similar trend is also found in China (Qian and Fan, 2020). If income variations for middle- and high-income groups remain, both correlate with COVID-19 and the nutrition variable in our sample, and we use a crude approach by including the restaurant fixed effects () and city-month interactions ( as proxy variables for unobserved time-invariant and time-varying demographics in equation (1).
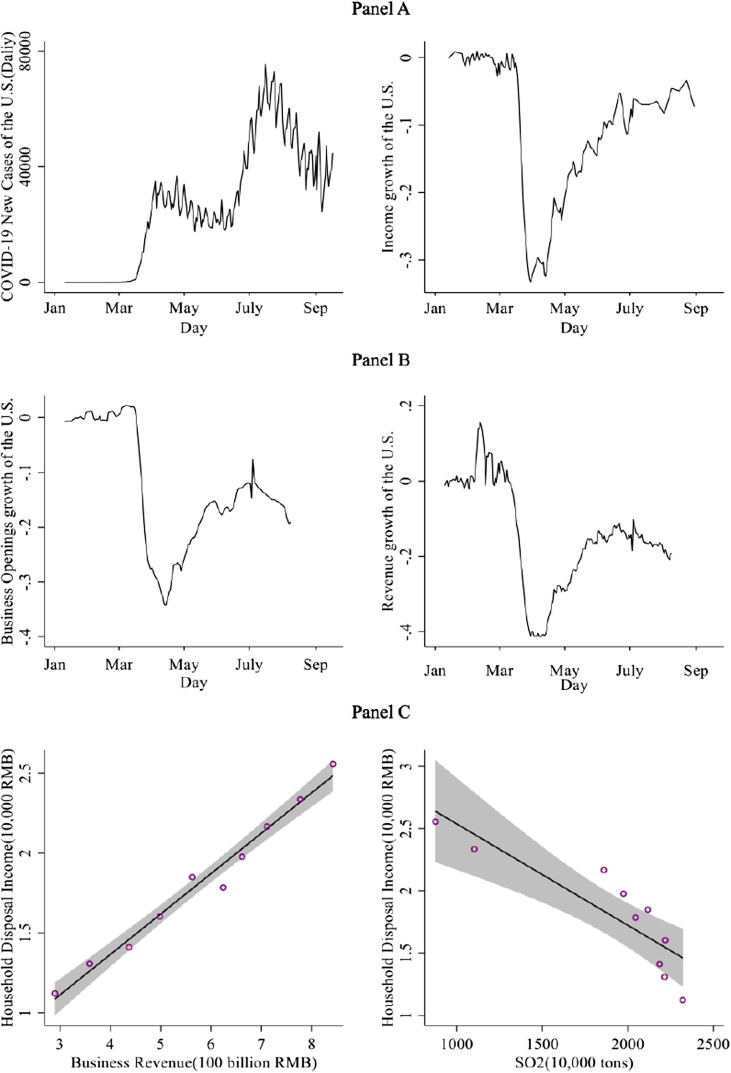
To further address this issue, we also estimate alternative models using income proxy variables for in equation (2). Given limited access to income data in China, Data for the U.S. from Chetty et. al (2020) indicate that business activities are more closely related to income variations than to the COVID-19 pandemic in the U.S, as shown in Fig. 3 . To examine whether the above relationships also apply to China, we collected yearly household income and business revenue for China from 2008 to 2018. Panel C in Fig. 3 shows that he 11-year trend of household income is significantly and positively correlated with business activities in China. Based on this, we propose two proxy variables for business activity in our sample: daily automobile traffic flow at the restaurant-level (income 1) and monthly foot traffic (income2), both within a three-kilometer radius of each of the 72 restaurant locations. The data are provided by the GIS DaaS Database from Tsinghua University.
Fig. 3.
Proxies for Income Variations. The figure shows that income variations do not closely follow the spread of COVID-19. Instead, air pollution and business openings and revenues are two sets of plausible proxy variables for income given their relationship graphed here. Panels A and B show the number of new cases, income growth rate, business openings rate, and business revenue growth rate in the U.S. against time. The data is from Chetty et. al (2020) using spending growth as a proxy of income variations. Panel C graphs the relationship between business revenue and (vertical axes) and household disposal income (horizontal axis) in China for 2008–2018. The relationship also indicates that both variables are closely related with income v.
However, demographic variables may not be good proxies to control for consumer heterogeneity in taste when consumers who fall into the same income category have different taste in dishes.15 As capturing variations in taste is equivalent to segmenting consumers with different utility functions, we implement the Generalized Axiom of Revealed Preference (GARP) method and the K-means algorithm proposed by Blumberg and Thompson (2021), who conclude that both methods work better than demographics to describe differences in taste. The GARP algorithm needs to compare pairs of expenditure and quantity, which is computationally intensive given a standard personal computer without GPU. We solve this problem by using 1, 5, and 10 percent of the sample randomly drawn from the full sample, following the computer science literature for manipulating big data (for recent examples, see Danaf et. al 2019; Ruiz et. al 2020). Performing K-means is less intensive, so we clustered the whole sample according to the quantity and expenditure into 500, 1000 and 1500 clusters. We report the results of sampling GARP and K-means for 500 clusters in Table 5, Table 6.16
Table 5.
Estimated COVID-19 Effects with Heterogenous Tastes by Revealed Preference Method.
| Variables | NRF | NPI | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.155* | −0.575* | −0.177*** | −0.177** | −0.013* | −0.040* | −0.050** | −0.047* |
| (0.072) | (0.281) | (0.042) | (0.070) | (0.007) | (0.022) | (0.016) | (0.023) | |
| Local Cases | −0.131** | −1.085*** | −0.571*** | −0.406*** | −0.017** | −0.108*** | −0.060** | −0.045* |
| (0.046) | (0.116) | (0.078) | (0.036) | (0.006) | (0.030) | (0.022) | (0.021) | |
| GARP 1 % | Yes | Yes | ||||||
| GARP 5 % | Yes | Yes | ||||||
| GARP 10 % | Yes | Yes | ||||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 1,456 | 7,218 | 14,498 | 144,044 | 1,456 | 7,218 | 14,498 |
| R-squared | 0.030 | 0.402 | 0.287 | 0.253 | 0.042 | 0.453 | 0.353 | 0.345 |
Table 6.
Estimated COVID-19 Effects with Heterogenous Tastes by K-means Clustering.
| Variables | NRF | NPI | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.155* | −0.158*** | −0.176*** | −0.218*** | −0.013* | −0.046*** | −0.030** | −0.070*** |
| (0.072) | (0.030) | (0.028) | (0.055) | (0.007) | (0.007) | (0.011) | (0.019) | |
| Local Cases | −0.131** | −0.281*** | −0.279*** | −0.331*** | −0.017** | −0.030*** | −0.033** | −0.023** |
| (0.046) | (0.047) | (0.031) | (0.044) | (0.006) | (0.008) | (0.011) | (0.010) | |
| K-means 500 | Yes | Yes | ||||||
| K-means 1000 | Yes | Yes | ||||||
| K-means 1500 | Yes | Yes | ||||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 |
| R-squared | 0.030 | 0.180 | 0.190 | 0.203 | 0.042 | 0.260 | 0.269 | 0.276 |
To investigate the longer run effects of COVID-19 on nutrient intake, we split the sample into three periods: (1) January 1 through January 22, 2020, as the pre-pandemic period; (2) January 23 through March 18, 2020, as the middle-pandemic period; and (3) March 19 through May 31, 2020, as the post-COVID-19 period. January 23, 2020 is the date when the central government imposed a lockdown in Wuhan and other cities in Hubei province. March 18th is a critical date for the pandemic’s being well-controlled, as on that day new domestic infections in China reached zero for the first time and stayed at or nearly that level for the remaining period. We conduct pair-wide comparisons of model (1) using a dummy variable for the post-pandemic period (Post = 1; 0 for other periods), in lieu of COVID infections. We retain all other control variables of the baseline model (1). The parameter estimates for the baseline and alternative empirical models are presented below.
3. Empirical results
3.1. Impacts of COVID-19 on nutrient intakes
Table 2 presents parameter estimates for individual nutrient intakes based on equation (1) from January 1 through March 18, 2020 (excluding the post-COVID period, i.e., post March 18, 2020). For each nutrient, we present results for four alternative model specifications for control variables. Regardless of the model specification, the number of COVID-19 cases significantly and positively impacts the intake of fat, sugar, and sodium (nutrients-to-limit) and negatively impacts the intake of protein and fiber (the nutrients-to-encourage), indicating an overall decline in the quality of nutrient intake. These results also show that local infections have a stronger effect than do national infections.
Table 2.
Results for Individual Nutrient Intake.
| Variable | Fat | Sugar | Sodium | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | |
| National Cases | 0.032*** | 0.023*** | 0.063*** | 0.031** | 0.092*** | 0.160*** | 1.402*** | 1.197*** | ||
| (0.006) | (0.006) | (0.004) | (0.011) | (0.012) | (0.014) | (0.280) | (0.338) | |||
| Local Cases | 0.099*** | 0.093*** | 0.108*** | 0.100*** | 0.156*** | 0.217*** | 2.316*** | 2.311*** | ||
| (0.009) | (0.007) | (0.006) | (0.012) | (0.011) | (0.011) | (0.268) | (0.273) | |||
| Discount | −4.816*** | −4.759*** | −4.843*** | 13.519*** | 13.615*** | 13.409*** | −356.641*** | |||
| (0.892) | (0.843) | (0.896) | (0.860) | (0.902) | (0.859) | (38.794) | ||||
| Price | 0.097*** | 0.099*** | 0.098*** | −0.425*** | −0.422*** | −0.421*** | 3.081*** | |||
| (0.010) | (0.009) | (0.009) | (0.011) | (0.012) | (0.012) | (0.717) | ||||
| Portion Size | −0.004*** | −0.004*** | −0.004*** | −0.009*** | −0.009*** | −0.009*** | −0.131*** | |||
| (0.001) | (0.001) | (0.001) | (0.001) | (0.001) | (0.001) | (0.007) | ||||
| Move_out | −0.022** | −0.033*** | −0.025** | −0.010 | −0.029** | −0.021** | −0.527 | |||
| (0.009) | (0.008) | (0.011) | (0.009) | (0.009) | (0.009) | (0.295) | ||||
| Move_in | −0.001 | −0.007 | −0.003 | −0.029* | −0.037* | −0.034* | −0.945* | |||
| (0.012) | (0.011) | (0.012) | (0.014) | (0.018) | (0.015) | (0.502) | ||||
| Constant | 6.071*** | 9.263*** | 9.697*** | 9.270*** | 38.070*** | 36.725*** | 37.453*** | 36.750*** | 642.543*** | 865.530*** |
| (0.216) | (0.318) | (0.411) | (0.298) | (0.164) | (0.539) | (0.574) | (0.629) | (11.091) | (33.688) | |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 |
| R-squared | 0.040 | 0.075 | 0.072 | 0.075 | 0.049 | 0.312 | 0.308 | 0.310 | 0.031 | 0.054 |
| Variable | Sodium | Protein | Fiber | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (11) | (12) | (13) | (14) | (15) | (16) | (17) | (18) | (19) | (20) | |
| National Cases | 2.203*** | −0.008*** | −0.019*** | −0.027*** | −0.004*** | −0.003*** | −0.006*** | |||
| (0.301) | (0.002) | (0.003) | (0.002) | (0.001) | (0.001) | (0.001) | ||||
| Local Cases | 3.105*** | −0.011** | −0.019*** | −0.032*** | −0.008*** | −0.006*** | −0.009*** | |||
| (0.306) | (0.004) | (0.002) | (0.002) | (0.000) | (0.001) | (0.001) | ||||
| Discount | −355.210*** | −358.064*** | −2.855*** | −2.867*** | −2.832*** | −0.570*** | −0.574*** | −0.566*** | ||
| (39.530) | (38.426) | (0.530) | (0.521) | (0.535) | (0.110) | (0.113) | (0.108) | |||
| Price | 3.124*** | 3.134*** | 0.084*** | 0.084*** | 0.083*** | −0.004*** | −0.004*** | −0.004*** | ||
| (0.731) | (0.722) | (0.013) | (0.013) | (0.013) | (0.001) | (0.001) | (0.001) | |||
| Portion Size | −0.131*** | −0.131*** | 0.001*** | 0.001*** | 0.001*** | 0.000*** | 0.000*** | 0.000*** | ||
| (0.007) | (0.007) | (0.000) | (0.000) | (0.000) | (0.000) | (0.000) | (0.000) | |||
| Move_out | 0.003 | 0.006** | 0.005*** | 0.003** | 0.003*** | 0.003*** | ||||
| (0.002) | (0.002) | (0.002) | (0.001) | (0.001) | (0.001) | |||||
| Move_in | 0.008*** | 0.009*** | 0.009*** | 0.002 | 0.002 | 0.002 | ||||
| (0.002) | (0.001) | (0.003) | (0.002) | (0.003) | (0.002) | |||||
| Constant | −0.795** | −0.660* | 4.861*** | 5.209*** | 5.118*** | 5.204*** | 3.166*** | 3.275*** | 3.246*** | 3.274*** |
| (0.301) | (0.309) | (0.060) | (0.287) | (0.265) | (0.306) | (0.012) | (0.088) | (0.097) | (0.085) | |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 |
| R-squared | 0.054 | 0.054 | 0.026 | 0.110 | 0.110 | 0.110 | 0.017 | 0.028 | 0.028 | 0.028 |
Model specification follows equation (1) using transaction-level data from January 1-March 18, 2020, using individual nutrients as dependent variables. The regressions are estimated using weighted least squares, where the weight is the daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
To quantify, the results indicate that for every 100 new COVID-19 infections at the national level, there is a decrease of protein and fiber intake of 0.008–0.027 g and 0.004–0.006 g per transaction, and an increase in fat, sugar, and sodium consumption of 0.032–063 g, 0.03–0.16 g, and 1.2–2.2 mg per transaction.17 Using the mean of each nutrient intake in the 2020 sample, these results translate into a 0.1 to 0.7 percent increase in nutrients-to-limit and a 0.1 to 0.4 percent decrease in nutrients-to-encourage per transaction. The changes in nutrients stemming from local COVID-19 infections are more significant than those for an equivalent number of national infections. For every single increase in local infections,18 there were increases in fat, sugar, and sodium intake of about 0.093–0.108 g, 0.100–0.217 g, and 2.311–3.105 mg, respectively, and decreases protein and fiber intake of 0.011–0.032 g and 0.006–0.009 g per transaction.19 This accounts for a 0.4 to 1 percent increase in sodium, fat, and sugar (nutrients-to-limit) and a 0.1 to 0.6 percent decrease in fiber and protein (nutrients-to-encourage) per transaction.
Table 3 presents parameter estimates for equation (1) using NRF scores and NPI as dependent variables. These results corroborate the main finding of the results for individual nutrients: that is, nutrient intake deteriorates during the pandemic. The impacts of COVID-19 under the two summary indexes are of similar magnitude and statistical significance. Using NRF scores, we estimate that for every 100 increases in national infections, there was a 0.16–1.39 g/kal decrease in the NRF index, while a similar increase in local COVID-19 infections led to a 0.13–0.44 g/kal decrease in the NRF index, which results in a 0.3 to 3.6 percent decrease relative to the NRF scores in our sample. The pattern for changes in NPI is similar.
Table 3.
Results for Nutrition Summary Indexes.
| Variable | NRF | NPI | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.155* | −0.280*** | −0.388*** | −0.013* | −0.049*** | −0.073*** | ||
| (0.072) | (0.061) | (0.042) | (0.007) | (0.008) | (0.004) | |||
| Local Cases | −0.131** | −0.249*** | −0.435*** | −0.017** | −0.055*** | −0.088*** | ||
| (0.046) | (0.060) | (0.016) | (0.006) | (0.009) | (0.007) | |||
| Other Control Variables | No | Yes | Yes | Yes | No | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 |
| R-squared | 0.030 | 0.121 | 0.121 | 0.120 | 0.042 | 0.206 | 0.206 | 0.206 |
Model specification follows equation (1) using transaction-level data from January 1-March 18, 2020, using nutrition summary metrics (NRF and NPI) as dependent variables. The regressions are estimated using weighted least squares, using as weight the daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
3.2. Robustness checks
We conduct several additional robustness checks. First, we check for using alternative income proxies: car and foot traffic. The results for the estimated COVID-19 coefficients, presented in Table 4 , are robust to the specifications using these alternative income proxies and support the baseline model. These results also mitigate concerns over omission of income variations at the individual level. Along the same lines, Tables 5 and report the results of NRF and NPI from GARP and K-means clustering to account for consumers’ heterogenous tastes instead of using income proxies. Columns (1) and (5) in both tables are results without controlling tastes. Table 5 shows that the impact of national and local cases on the nutrition index are not just significantly negative for 1 %, 5 % and 10 % samples to perform GARP, but also more significant than without controlling the tastes. The results for Table 6 show a similar pattern as those in the baseline results.
Table 4.
Estimated COVID-19 Effects Under Alternative Income Proxies.
| Variable | NRF | |||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.388*** | −0.397*** | −0.388*** | −0.396*** | ||||
| (0.042) | (0.040) | (0.042) | (0.040) | |||||
| Local Cases | −0.435*** | −0.470*** | −0.434*** | −0.470*** | ||||
| (0.016) | (0.021) | (0.015) | (0.020) | |||||
| Income1 | 0.218 | 0.224 | 0.453* | 0.460** | ||||
| (0.205) | (0.190) | (0.220) | (0.203) | |||||
| Income2 | 9.790 | 9.837 | 9.781 | 9.873 | ||||
| (5.491) | (5.548) | (5.420) | (5.553) | |||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 |
| R-squared | 0.121 | 0.121 | 0.121 | 0.121 | 0.120 | 0.120 | 0.120 | 0.120 |
| Variable | NPI | |||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.073*** | −0.067*** | −0.073*** | −0.067*** | ||||
| (0.004) | (0.005) | (0.004) | (0.005) | |||||
| Local Cases | −0.088*** | −0.078*** | −0.088*** | −0.078*** | ||||
| (0.007) | (0.005) | (0.007) | (0.005) | |||||
| Income1 | −0.159*** | −0.158*** | −0.121*** | −0.120*** | ||||
| (0.038) | (0.036) | (0.032) | (0.031) | |||||
| Income2 | 1.688** | 1.655** | 1.685** | 1.661** | ||||
| (0.639) | (0.586) | (0.617) | (0.581) | |||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 |
| R-squared | 0.206 | 0.206 | 0.206 | 0.206 | 0.206 | 0.206 | 0.206 | 0.206 |
| Variable | NRF | NPI | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.280*** | −0.283*** | −0.280*** | −0.283*** | −0.049*** | −0.049*** | −0.049*** | −0.049*** |
| (0.061) | (0.058) | (0.061) | (0.058) | (0.008) | (0.007) | (0.008) | (0.007) | |
| Local Cases | −0.249*** | −0.285*** | −0.249*** | −0.285*** | −0.055*** | −0.047*** | −0.055*** | −0.047*** |
| (0.060) | (0.072) | (0.061) | (0.072) | (0.009) | (0.007) | (0.009) | (0.007) | |
| Income1 | 0.490* | 0.497* | −0.115** | −0.114*** | ||||
| (0.248) | (0.231) | (0.036) | (0.034) | |||||
| Income2 | 9.754 | 9.853 | 1.680** | 1.658** | ||||
| (5.426) | (5.566) | (0.619) | (0.584) | |||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 | 144,044 |
| R-squared | 0.121 | 0.121 | 0.121 | 0.122 | 0.206 | 0.207 | 0.206 | 0.207 |
Results are at the transaction level from January 1-March 18, 2020. Note that the COVID-19 coefficients in columns (1a) and (1b) and (4a) and (4b) are from the same model, but the national and local COVID-19 coefficients are presented in different columns. Except where noted, all specifications are estimated with other control variables. Note that *, **, and *** indicate significance at the 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
The second set of robustness checks focuses on the potentially unobserved regional effects that are correlated with COVID-19 and nutrient intake. That is, although we control for city fixed effects, the impact of COVID-19 infections may spill over to other regions. Following Chang et al. (2018), we use COVID-19 case counts from other cities to proxy unobserved local factors that may correlate with a particular city’s COVID-19 prevalence and nutrition decisions and then rerun the regression including COVID-19 infections in the nearest city. The results, presented in Table 7 , show that the COVID-19 infections in neighboring cities did not have a discernable impact on nutrient intake in our baseline results and that their omission likely did not significantly bias the results.
Table 7.
Robustness Check for Regional Spillovers and Pre-trends.
| Variables | Impact of Infected Cases from Neighboring Cities | Test for Pre-existing Trends from January 1–22, 2019 | ||||||
|---|---|---|---|---|---|---|---|---|
| NRF | NPI | NRF | NPI | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National | −0.140*** | −0.160*** | −0.042*** | −0.046*** | −2.652 | −1.636 | −0.541 | −0.156 |
| (0.041) | (0.031) | (0.008) | (0.007) | (1.768) | (2.193) | (0.447) | (0.409) | |
| Local | −0.301*** | −0.283*** | −0.036*** | −0.029** | 0.456 | 0.374 | 0.045 | 0.021 |
| (0.035) | (0.049) | (0.008) | (0.010) | (0.483) | (0.504) | (0.107) | (0.100) | |
| Neighbor | −0.001 | 0.024 | −0.015 | −0.013 | ||||
| (0.106) | (0.099) | (0.037) | (0.035) | |||||
| K-means 500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Control Variables | No | Yes | No | Yes | No | Yes | No | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 118,207 | 118,207 | 118,207 | 118,207 |
| R-squared | 0.030 | 0.121 | 0.042 | 0.207 | 0.022 | 0.057 | 0.036 | 0.229 |
| Variables | Test for Pre-existing Trends from January 23– March 18, 2019 | Test for Pre-existing Trends from March 19-May 31, 2019 | ||||||
|---|---|---|---|---|---|---|---|---|
| NRF | NPI | NRF | NPI | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National | −0.043 | −1.044 | 0.254 | 0.563 | 4.058 | 1.719 | 1.549 | 1.358 |
| (0.469) | (1.529) | (0.216) | (0.529) | (3.535) | (5.353) | (0.970) | (1.858) | |
| Local | −0.008 | −0.011 | −0.013 | −0.015 | −0.062 | −0.017 | −0.013 | 0.013 |
| (0.064) | (0.052) | (0.014) | (0.009) | (0.116) | (0.103) | (0.027) | (0.027) | |
| K-means 500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Control Variables | No | Yes | No | Yes | No | Yes | No | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 188,251 | 188,251 | 188,251 | 188,251 | 271,641 | 271,641 | 271,641 | 271,641 |
| R-squared | 0.162 | 0.215 | 0.179 | 0.331 | 0.036 | 0.167 | 0.037 | 0.213 |
The regressions are estimated using weighted least squares, using as weight the daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% levels of confidence. All errors are clustered at the city level.
The third set of robustness checks focused on whether the impacts are driven in part by pre-pandemic trends that may arise with seasonal or other time-dependent effects or by other effects that cause spurious correlation with 2020 COVID impacts, that is, in terms of our sample, by a similar trend for the same period in 2019. To this end, we run the baseline model with the same dates (January 1 through March 18) and the same control variables and restaurant orders for 2019.20 Columns (5)-(8) of Table 5 report the results for the two nutrition summary indexes. None of the estimates are significantly different from zero, showing no similar trend in nutrition decisions in our 2019 sample. Thus, no discernable pre-pandemic city or time differences are evident in our sample.21
3.3. Post-Pandemic effects
Panels A-C in Table 8 presents the results for the pre-, middle, and post-pandemic periods, as defined previously. Panel A that compares the pre- and post-COVID-19 periods shows a significant increase in the consumption of nutrients-to-encourage in the post-COVID-19 period relative to the pre-COVID period. On average, these results show an increase of 0.135 g and 0.080 g for fiber and protein—almost an 8 percent and 1 percent increase, given the mean values of fiber and protein intake in the sample. At the same time, the results show significant decreases in the amount of nutrients-to-limit: on average, a decrease of 1.628 g, 3.431 g, and 40.988 mg in fat, sugar, and sodium, respectively, accounting for 7 to 16 percent decreases relative to the sample means. The nutrient results are also supported by corresponding NRF scores and NPI increases of 11 and 1.4 percent, indicating an overall increase in the healthiness of the diet. Panel B that with the results for the middle v. the post-COVID-19 periods, shows that the impacts on nutrient intake are starker than those in Panel A. That is, we find even stronger evidence of nutritional improvement when the post-COVID period is compared to the most active period of the pandemic. Panel C simply compares the 2020 and the 2019 March 19-May 31 periods (post-COVID) and finds evidence of diet improvement in 2020 relative to the same period in 2019.
Table 8.
Results at Different Stages of the Pandemic.
| Variable | PANEL A: Post = 1 for Post-COVID period (March 19-May 31, 2020) vs Pre-COVID Period (January 1–22, 2020) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Post | −1.628*** | −3.431*** | −40.988*** | 0.080*** | 0.135*** | 4.413*** | 0.602* |
| (0.378) | (0.121) | (12.260) | (0.004) | (0.031) | (1.436) | (0.326) | |
| K-means 500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 |
| R-squared | 0.141 | 0.298 | 0.032 | 0.139 | 0.103 | 0.105 | 0.212 |
| Variable | PANEL B: Post=1 for Post-COVID Period (March 19-May 31, 2020) vs COVID Period (January 23-March 18, 2020) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (8) | (9) | (10) | (11) | (12) | (13) | (14) | |
| Post | −0.763** | −5.755*** | −75.491*** | 0.739** | 0.727*** | 5.619*** | 3.900*** |
| (0.261) | (0.355) | (16.528) | (0.243) | (0.055) | (0.949) | (0.558) | |
| K-means 500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 |
| R-squared | 0.129 | 0.299 | 0.060 | 0.150 | 0.141 | 0.095 | 0.239 |
| Variable | PANEL C: Post=1 for Post-Covid Period (March 19-May 31, 2020) vs year 2019 (March 19-May 31, 2019) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (8) | (9) | (10) | (11) | (12) | (13) | (14) | |
| Post | −3.155*** | −1.891** | –32.654*** | 1.581*** | 0.136*** | 5.607*** | 1.094* |
| (0.294) | (0.582) | (2.176) | (0.228) | (0.015) | (1.617) | (0.590) | |
| K-means 500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 |
| R-squared | 0.239 | 0.370 | 0.168 | 0.253 | 0.130 | 0.187 | 0.282 |
The regressions are estimated using weighted least squares. The dependent variable is the weighted daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
4. Potential mechanisms
4.1. An intertemporal model of nutrient intake
We develop a simple intertemporal choice model that focuses on the behavioral motivation aspects regarding the healthfulness of nutritional choices to link the COVID-19 pandemic to improvements in nutrient intake. Consider an individual who decides on the healthfulness of their diet at time 0. We summarize the healthfulness using a single quantity . At time 0, the individual opts for nutrient intake and obtains an experienced utility of , which captures their hedonic experience of eating. Given the fact that “bad” nutrients such as sweets, starches, and fats could generate higher level of comfort, we assume that is a decreasing function on , as a healthier diet is associated with a lower hedonic experience from a reduction in consumption of “bad” nutrients that generate comfort and immediate rewards from eating (Laitinen et al., 2002, Oliver and Wardle, 1999, Smith, 2012).
Next, the choice of at time 0 also influences the individual’s health-related utility at time 1, . Assume that to some extent the individual is aware of the existence of relationship between at time 0 and at time 1 but does not know the exact quantitative relationship. Let and denote two possible states of that an individual believes about the health-diet relationship: (1) , which is a constant indicating no relationship between healthfulness of diet at time 0 and utility at time 1; and (2) , indicating a higher utility at time 1 with a healthier diet at time 0. Let and denote the subjective probabilities that an individual believes the true state to be and respectively. Consequently, the health-related utility in time 1 takes an expected utility form for and . Finally, let denote the individual discount rate between the experienced and the expected utility.
An individual chooses h by maximizing their net expected utility:
| (3) |
The first order condition for the maximization of (1) yields.
| (4) |
Equation (4) suggests that the degree of healthfulness of the diet is determined by an individual’s compounded valuation of experienced utility as well as their beliefs about the connection between nutrient intake and health.
4.2. Potential explanations of changes in nutrition
Following the behavioral economics literature, we explore three explanations of how COVID-19 works by affecting nutrient intake based on changes in and stemming from the shock of the COVID-19 pandemic. The details are shown in Appendix A.
4.2.1. Emotional eating
It is widely documented that health and economic insecurities cause stress and that individuals under stress tend to value an immediately realized utility more than an expected later one (Koppel et al., 2017, Delaney et al., 2014). For instance, stress induced by economic insecurity triggers unhealthy eating behavior by increasing sugar intake (Staudigel, 2016). By the same token, we expect that the COVID-19 pandemic causes stress and that individuals become more focused on their immediate experienced utility rather than a deliberation about a nutrition-health utility in the future. Thus, this causes to decrease, resulting in a lower h or nutrient intake relative to before the pandemic. Yet the impact of stress is temporary, as stress vanishes when the pandemic is well controlled.
4.2.2. Salience
Even if individuals were inattentive to the true relation between nutrition and health prior to the pandemic because the relationship nutrition-health was not salient, the pandemic could suddenly make this relationship salient by bringing about a greater focus on the expected utility of health rather than on experienced utility. In contrast to emotional eating, salience increases as an individual puts more weight on their expected health-related utility, resulting in a healthier diet during the COVID-19 period. Like emotional eating, salience is a temporary behavioral driving force, indicating that increases in are temporary and that the impact of salience on nutrient intake vanishes in the post-pandemic period.
4.2.3. Learning
The pandemic stimulated a worldwide boom in health information provision from both public and private media. As an important component of the response to the pandemic, information about the relationship among eating a healthier diet, chronic diseases, and COVID-19-associated health risks can be found in the web pages of public health authorities and is widely discussed in social media. This fact may initiate extensive learning from health information as well as increases in an individual’s beliefs about . That is, learning induces an increase in and resulting in a higher h, or a healthier diet.22 Unlike the impacts of emotional eating and salience on , the learning effect on updating is rational and lasts over the long run. That is, once an individual learns that is more likely to be true than they believed before, they will tend to hold that belief even in the post-COVID-19 period. In essence, the learning effect leads to a long-run improvement even after the pandemic.
In summary, our finding that nutrition deteriorates during the COVID-19 active period is more consistent with the explanation of emotional eating while learning is more consistent with the period when the COVID-19 pandemic came under control.
5. Policy implications
From a policy perspective, our results show that policy makers’ efforts to decrease overall stress and worries during health shocks are necessary but have limited and short-run effects. Instead, we suggest that policy makers emphasize boosting learning mechanisms by promoting information and education to improve individuals’ awareness of preventive health behaviors of a more permanent nature, such as changes in nutrition and exercise behaviors. This, of course, is suggested in addition to encouraging such pandemic-specific behaviors as handwashing, mask-wearing, and social distancing. The long-run positive health impacts of adopting preventive health behaviors may mitigate the negative impact of health shocks in a society and are likely to outlive the pandemic itself.
Besides general public-health concerns for the entire population, a more specific but important policy implication concerns children’s health during COVID-19, as early-life exposure to malnutrition has long-term consequences for adult health, education, and labor market outcomes (Almond and Currie, 2011). Like the negative findings reported in Baron et al. (2020) for school closures during the pandemic, our findings imply that school closure may also have a negative nutritional impact on children who are eating at home during the period of an active pandemic when diet follows emotional eating. Thus, nutrition guidelines and health education should be provided to parents and students to mitigate negative effects of potential health shocks during the pandemic.
6. Conclusion
In this article, we examine the potential effects of the COVID-19 pandemic on nutrient intake, using this pandemic as a case study of a public health shock. The theoretical analysis proposes that emotional eating or salience temporarily induces negative changes in nutrient intake, while learning can improve it in the long run. To empirically tests these effects, we utilize data from approximately-one million restaurant transactions in 10 cities in China, and a battery of model specifications and robustness checks to identify the effects. To account for possible selection bias, even though we empirically use proxies for income that may well be valid instruments for income, there may be other consumer characteristics that may bias the results. One would be the selection of active users of food delivery apps during the pandemic. As noted by Statista (2022), in June 2020, about 31 % of the Chinese respondents ordered more from food delivery apps during the COVID-19 pandemic. However, 33 % ordered less through food apps, 19 % did not change their food-ordering habits, and 16 % stopped using apps. Given this mixed picture, it is not possible to speculate on the direction of the likely bias in our sample. In addition, we used city and restaurant fixed effects to capture fixed unobservable variables that could include the nature of the neighborhoods each restaurant is located. We also applied GARP and K-means to control for potential heterogeneities in Taste. Finally, we provide a conceptual analysis for potential behavioral mechanisms that can explain the outcomes observed, including learning.
Overall, we find that individuals eat less healthily as the number of COVID-19 infections increases. However, once the pandemic comes under control, the healthfulness of their nutrition improves significantly relative to the middle, early, and pre-pandemic periods, as indicated by changes in intake of individual nutrients as well as changes in Nutrient Rich Food (NRF) scores and the Nutrition Profile indexes. These findings are robust, and they empirically support our theoretical predictions for learning as a driving mechanism for nutrient-intake improvement stemming from the pandemic health shock. Thus, learning eventually not only overcomes the negative impact of emotional eating and economic insecurity on nutrient intake, but it also overtakes the negative forces on diet after the pandemic comes under control providing a silver lining. By utilizing the COVID-19 pandemic as a natural experiment of a public health shock, the findings fill a gap in the health policy literature concerning how and to what extent the learning effect from health shocks can lead to changes in nutritional choices. The pandemic not only generates a widespread and substantial learning effect that could be detected empirically, but it also allows us to distinguish the learning effects from other effects.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
The research is supported by Public Computing Cloud, Renmin University of China and funded by the Fundamental Research Funds for the Central Universities, the Research Funds of Renmin University of China (22XNA021), and the Richard DelFavero Fund for Agricultural and Resource Economics at the University of Connecticut. All errors are ours.
Due to confidentiality requirements, we are not allowed to publish specific information regarding the location of the restaurants by city, but, with the permission of the company, we can disclose the geographical distribution of the 10 cities in the responses. The 10 cities are Beijing, Shanghai, Nanjing, Tianjin, Guangzhou, Kunming, Hangzhou, Shenzhen, Shijiazhuang, and Suzhou. The samples cover the four first-tier metropolitan cities in China (Beijing, Shanghai, Guangzhou, and Shenzhen) and the remaining six cities are provincial capitals located in northeastern, eastern, southwestern, and southern areas of China, covering a population of 150 million and accounting for around 10 percent of the total population of China.
In the China Food Composition Tables, because there is no information about sugar content for each food, we use the carbohydrate content to proxy sugar in each food. The total sugar content used in the analysis includes the carbohydrates in each food as well as sugar added during cooking. Also note that although vitamins, calcium, and iron are included in the calculations of nutrition indexes, they are not included in the tables of results for individual nutrients.
The restaurants occasionally update their recipes in their computer system. In our sample, we account for sporadic changes in recipes by updating the nutrition information in real time.
The basic idea of the NRF scores is to define nutrient-rich foods rather than energy-dense ones, as encouraged by the 2005 Dietary Guidelines for Americans (U.S. Department of Health and Human Services, 2005). Following standard procedure, NRFs are computed as the sum of the percentage of daily values of nutrients-to-encourage minus the sum of the percentage of maximum recommended values of nutrients-to-limit. The formula for calculating the nutrition indexes is in Appendix B.
NPIs are used internationally to identify healthier foods via scores based on energy and individual nutrients, as well as amounts of healthy foods such as fruit and vegetables (U.K. Department of Health, 2011).
On February 12, 2020, the China National Health Committee switched the infection diagnosis procedure from molecular to clinical diagnosis, resulting in an abnormal—and the biggest—increase for that day, with 15,152 new cases. However, this spike was not observed again after February 20, 2020, when the government switched back to molecular diagnosis tests.
The price is usually determined by both demand and supply changes. One concern is the price may increase due to the supply constraints of the pandemic. In our data, we instead found the prices are declining. The trend of price changes would in principle reject the hypothesis of supply constraints or at least support the notion that declining demand forces were stronger than any supply constraints. One extension for this study is to control the supply changes as well when the supply chain data is more available.
Food delivery orders are submitted through mobile phone apps, and people usually neglect to type in the number of people who will share the dishes.
We are indebted to a reviewer who pointed out and encouraged more discussion on the potential omitted variables/selection bias from missing demographics, particularly in the context of active food app users during the pandemic.
The data is provided by the GIS DaaS Database at Tsinghua University. In general, restaurants deliver only to residents who live close by to ensure the guaranteed 30-minute delivery time. Cell phone data refers to the different cell phone number detected in the area per month.
The average expenditure per capita in the restaurants is around 89RMB (around 13USD) per transaction, and the total bill could be up to 400 RMB (around 57 USD) when four persons eat together (the normal size of groups that dine in the restaurants). Given that the average household yearly disposable income in China was around 30,733 RMB (around 4,390 USD) in 2019, and the Chinese tradition that only one person pays the entire bill when dining in restaurants, low-income people are unlikely to frequently visit restaurants because one meal would cost more than their one-month income.
This was pointed out by one of the reviewers, which prompted further analysis reported below.
We also conducted runs with 1,000 and 1,500 cluster fixed effects (reported in Appendix D), but the results were fundamentally like the ones reported in Table 5, Table 6 with 500 cluster fixed effects.
We use the average of the results of specifications (1), (2), and (3), which include national infections. Note that the impact of national infections is not significant for sugar and protein under model specification (3) in Table 2, which excludes control variables.
Note from Table 1 that national infections were measured in the one-hundreds while local infections are reported in actual numbers.
The impact of local infections is not significant for protein in the first model specification, which excludes all other control variables.
We deleted the number of infections for February 29, 2020, as that date did not apply in 2019.
We also conducted regressions aggregating observations to the restaurant level and adding the number of transactions as a proxy for active users (the results are reported in Appendix C). The key results for the impacts on COVID on diet quality were substantially the same.
As evidence for the demand for health information associated with the pandemic, using data from Baidu searches (China’s Google search engine) and internet searches between January 1 to May 31, 2020, we observe a more than a 10-fold increase of internet searches for four keywords after January 23, 2020: (1) mask, (2) sanitize, (3) immunity, and (4) handwashing.
Appendix A. A choice model of nutrition intake
We build an intertemporal choice model to study individuals’ behaviors in both the COVID period and the post-pandemic period. At time , individuals obtain a utility of , which is considered to be an experienced utility that measures the hedonic quality gained from eating. Assume that reflects their utility gained from their future health outcomes, which are in turn dependent on nutrient intake at time 0. is defined as an individual’s health-related utility.
In the real world, individuals are likely to be aware that future health outcomes are to some degree connected to nutrient intake but unlikely to know the exact quantitative relationship. It is more natural to assume that individuals know that belongs to some subset of the set of all functions from to , and that they have some subjective belief about the likelihood of which is true. Put formally, we assume and, for the sake of simplicity, that is finite. An individual’s subjective belief is denoted by , where is the set of all probability measures on . Suppose there is some . We write , where is the individual’s subjective probability that is the true health-related utility function.
Hence, individuals optimize the following problem:
| (A1) |
where is their ex ante expected health-related utility, and is their time preferences about how they discount the future utility. A larger means that the individuals weight the expected future utility more.
We introduce the following assumptions to make the analysis reasonable and tractable:
Assumption 1
is continuous and twice differentiable, withand.
We also require, out of technical consideration, that , in order to make the absolute value a deceasing function and to simplify the mathematics.
Assumption 2
, whereis a constant function on, andis continuous and twice differentiable, withand.
Assumption 2 specifies individuals’ knowledge about the relationship between nutrient intake and health-related utility. Although we could encounter a spectrum of possible relations between health-related utility and nutrient intake, we only emphasize these two states as they are the most relevant to the considerations of this research.
Assumption 3. , .
Assumption 3 indicates that when the diet becomes extremely unhealthy, that is, when takes a small value in the domain , it is more beneficial for individuals to eat a little healthier. Since if is small, the marginal health-related utility of eating a little healthier is larger than the marginal experienced utility of eating unhealthier if the diet is already extremely unhealthy. When the diet is already extremely healthy, i.e., when takes a large value in the domain , it is more beneficial for individuals to eat a little unhealthier. Since if is large, the marginal experienced utility of eating a little unhealthier is larger than the marginal health-related utility of eating even healthier if the diet is already extremely healthy.
Note that, out of technical consideration (that is, to make the solution to the following first order condition (A.3) real, as will be shown below), we require , which is stronger than , since .
As Assumption 2 specifies to be a doubleton; we write and , where is the subjective probability that individuals believe the true relation between health-related utility and nutrient intake to be . Specifically, we can rewrite the optimization problem (A.opt01) as.
| (A2) |
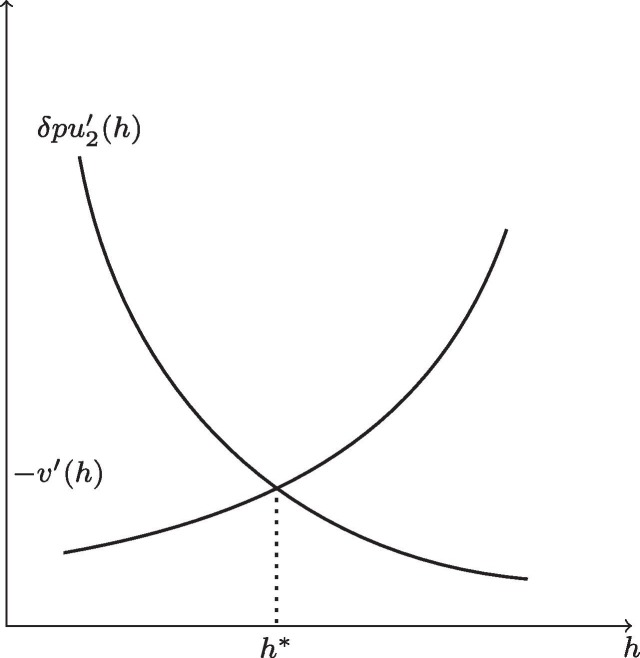
The first order condition of equation (A.2) is.
| (A3) |
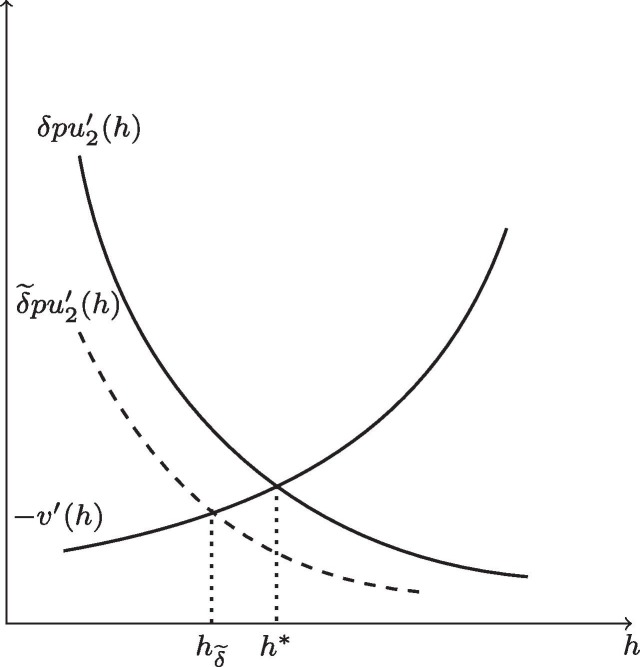
with being the optimal nutrient intake level. The optimal solution exists and is unique, since the curves of and intersect once and only once, according to Assumptions 1 to 3. See Fig. A1 for illustration.
Fig. A1.
Optimal Nutrient Intake Given by Equation (A.3).
(1) Stress and Time Preferences.
The first pathway through which COVID-19 affects diet is stress. For technical reasons we require that Assumption 3 still hold for .
As , we have , and is no longer the optimal choice of nutrient intake. The new optimal choice of nutrient intake is smaller than , because both and increase when gets smaller, according to Assumptions 1 and 2, and increases more quickly than , according to Assumption 3. Fig. A2 illustrates that by shifting to , pandemic-caused stress moves the curve downward to , giving rise to a smaller optimal solution . This shock is temporal, and its effect will start to vanish as the pandemic abates.
Fig. A2.
The Effect of Stress on the Optimal Healthiness of Diet.
(2) Salience.
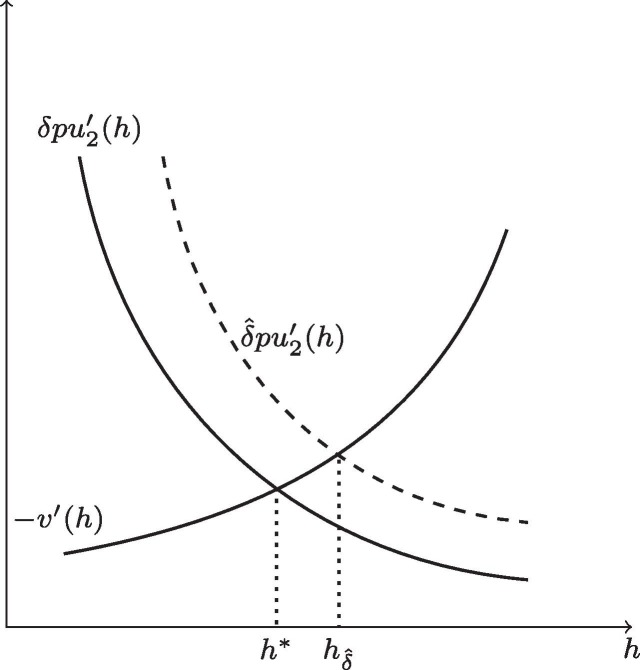
Like the stress-induced shocks, salience also brings about a shock to changes of time preferences . But by shifting to a larger , the shock of salience is positive, and it is reasonable to assume that the more salient the health considerations are, the larger is the weight that individuals put on their expected health-related utility. Contrary to the negative stressor shock (shifting to ), the positive shock of salience (shifting to drives the optimal choice of nutrient intake higher than , indicating a healthier diet during the COVID period. As with stressor shock, the positive shock of salience will vanish in post-COVID-19 period. Fig. A3 illustrates that by shifting to , salience moves the curve upward to , giving rise to a larger optimal solution . This effect is temporary and will decrease as the pandemic abates.
Fig. A3.
The Effect of Salience on Diet.
(3) Learning.
In contrast to stress and salience, learning is a rational mechanism through which individuals update their beliefs about the diet-health link during the pandemic. Although social media and medical studies have long documented that healthy eating habits are crucial to individuals’ healthiness, it is likely that many individuals are not fully aware of this fact. This unawareness may be due to inattentiveness or lack of information, which is modeled in our framework by an individual’s uncertainty between and . The outbreak of the COVID-19 pandemic stimulates information campaigns to provide enough medical information for individuals to learn more about the health behaviors, including eating a healthier diet, that could lead them to have more faith that is true.
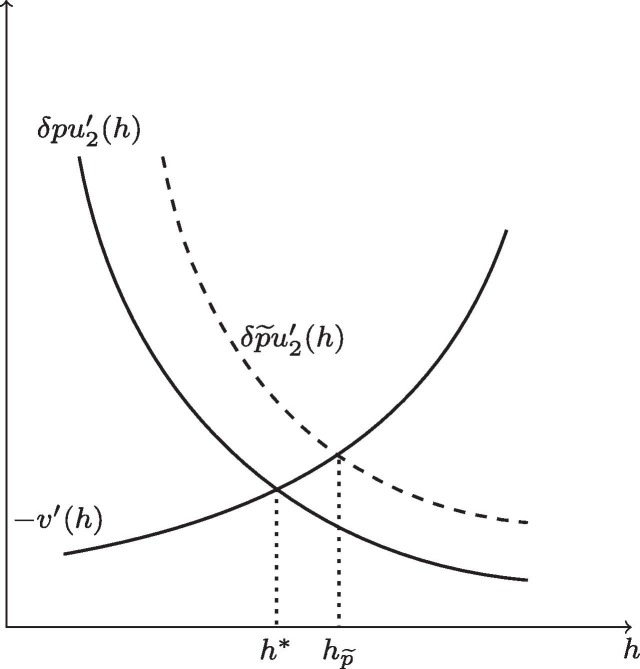
Formally, the learning mechanism is captured by the positive impact on , leading to a larger than . Unlike the stress-caused shock on , the learning effect lasts in the long run; that is, once individuals learn that is more likely to be true than they believed before, they will hold that belief even if the initial stimulus (e.g., the information campaign during the pandemic) has stopped. Similarly, we require that Assumption 3 still hold for . Since , we have . This makes no longer the optimal choice of nutrient intake. The new optimal choice of nutrient intake should be larger than , as both and decrease when gets larger, as implied in Assumptions 1 and 2, and decreases more slowly than , according to Assumption 3. Fig. A4 illustrates that by shifting to , learning moves the curve upward to , giving rise to a larger optimal solution . This learning effect will last even if the pandemic is under control.
Fig. A4.
The Effect of Learning on Diet.
Appendix B. Details on the calculations of nutrition scores
The basic idea of an NRF score is to define nutrient-rich foods rather than energy-dense ones, as encouraged by the 2005 Dietary Guidelines for Americans (U.S. Department of Health and Human Services, 2005). Following standard procedure, NRFs are computed as the sum of the percentage of daily values of nutrients-to-encourage minus the sum of the percentage of maximum recommended values of nutrients-to-limit (Drewnowski and Fulgoni, 2014, Drewnoski, 2009). In our analysis, we calculated NRF using the following formula:
NRF = (protein/50 + fiber/25 – saturated fat/20 – added sugars/50 –sodium/2400) *100/ED,
where the denominator in the parentheses is the reference daily values based on a 2000-kcal diet, the numerator is the the nutritional contents per gram, and ED is energy density calculated as kcal/100 g. A negative NRF could be interpreted as the dish containing more nutrients-to-limit than nutrients-to-encourage.
For NPI, according to the U.K. Department of Health (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216094/dh_123492.pdf), the original NPI is calculated as:
NPI_original = (points for energy) + (points for saturated fat) + (points for sugars) + (points for sodium) - (points for % fruit, vegetable & nut content) - (points for fiber) - (points for protein).
The relationship between points and nutrition contents is given by tables on page 5 of Nutrient Profiling Technical Guidance (U.K. Department of Health, 2011). The larger original NPI scores indicate less healthy. To be comparable with NRF, we normalize NPI according to the following formula:
NPI = (-NPI_original-Min(-NPI_original))/(Max(-NPI_original)-Min(-NPI_original))*100.
Appendix C. Results for dish prices and Restaurant-Level Data.
See Fig. D1 and Table C1, Table C2 .
Table C1.
COVID-19 Coefficients Under Alternative Income Proxies (Restaurant-Level Data).
| Variable | NRF | |||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.451*** | −0.409*** | −0.452*** | −0.411*** | ||||
| (0.089) | (0.117) | (0.088) | (0.114) | |||||
| Local Cases | −0.511*** | −0.455** | −0.511*** | −0.458** | ||||
| (0.128) | (0.143) | (0.128) | (0.142) | |||||
| Income1 | −1.449 | −1.401 | −1.299 | −1.250 | ||||
| (0.997) | (0.959) | (0.996) | (0.959) | |||||
| Income2 | 20.552 | 18.978 | 20.307 | 18.918 | ||||
| (16.330) | (15.553) | (16.256) | (15.481) | |||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 |
| R-squared | 0.267 | 0.271 | 0.269 | 0.272 | 0.268 | 0.271 | 0.270 | 0.272 |
| Variable | NPI | |||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.095*** | −0.090*** | −0.095*** | −0.091*** | ||||
| (0.017) | (0.014) | (0.017) | (0.014) | |||||
| Local Cases | −0.116** | −0.110*** | −0.116** | −0.111*** | ||||
| (0.037) | (0.029) | (0.037) | (0.029) | |||||
| Income1 | −0.176 | −0.164 | −0.130 | −0.118 | ||||
| (0.261) | (0.262) | (0.242) | (0.243) | |||||
| Income2 | 4.793 | 4.608 | 4.744 | 4.612 | ||||
| (2.786) | (3.009) | (2.807) | (3.000) | |||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 |
| R-squared | 0.350 | 0.351 | 0.352 | 0.352 | 0.352 | 0.353 | 0.354 | 0.354 |
| Variable | NRF | NPI | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National Cases | −0.310** | −0.292** | −0.311** | −0.294** | −0.061*** | −0.060*** | −0.062*** | −0.060*** |
| (0.102) | (0.115) | (0.100) | (0.112) | (0.014) | (0.015) | (0.014) | (0.015) | |
| Local Cases | −0.364** | −0.323* | −0.364** | −0.325* | −0.087** | −0.083** | −0.087** | −0.084** |
| (0.146) | (0.155) | (0.146) | (0.155) | (0.035) | (0.029) | (0.035) | (0.029) | |
| Income1 | −1.156 | −1.106 | −0.101 | −0.088 | ||||
| (1.045) | (1.007) | (0.245) | (0.246) | |||||
| Income2 | 20.537 | 19.296 | 4.789 | 4.690 | ||||
| (16.232) | (15.372) | (2.752) | (2.930) | |||||
| Other Control Variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 | 4,641 |
| R-squared | 0.273 | 0.275 | 0.274 | 0.276 | 0.356 | 0.356 | 0.358 | 0.358 |
Results are at the restaurant level from January 1-March 18, 2020. Note that the COVID-19 coefficients in columns (3a) and (3b) are from the same model, but the national COVID and local COVID coefficients are presented in different columns across all income specifications: column (3a) for the national infections and column (3b) for the local infections. The same holds for columns 6a and 6b. Except where noted, all specifications are estimated with other control variables, including city_month, discount, price, portion size, city dummies, DOW (day of week), and month dummies. Note that *, **, and *** indicate significance at the 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
Table C2.
Changes in Vegetable, Fish and Other Meat (Pork and Beef) Dish Ratios.
| Variable | Post = 1 for Post-COVID vs Pre-COVID | Post = 1 for Post-COVID vs COVID | ||||
|---|---|---|---|---|---|---|
| Vegetable | Fish | Pork & Beef | Vegetable | Fish | Pork & Beef | |
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Post | −0.006 | 0.014 | 0.008** | 0.011*** | −0.000 | 0.001 |
| (0.009) | (0.012) | (0.003) | (0.002) | (0.006) | (0.002) | |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 317,921 | 317,921 | 317,921 | 314,223 | 314,223 | 314,223 |
| R-squared | 0.055 | 0.294 | 0.182 | 0.050 | 0.290 | 0.154 |
The dependent variables are the ratios of vegetable, fish, and other meat (pork and beef) dishes to the total number of dishes ordered. Columns (1)-(3) report results by comparing changes during the post-COVID periods to pre-COVID periods. Columns (4)-(6) report results by comparing changes during the post-COVID periods to COVID periods. Note that *, **, *** indicate 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
Fig. D1.
Average Dish Prices for 2019 and 2020.
Appendix D. Results for revealed preference and K-Means
See Table D1, Table D2, Table D3, Table D4 .
Table D1.
Robustness Check for Regional Spillovers and Pre-trends with 1000 Clusters.
| Variables | Impact of Infections in Neighboring Cities | Test for Pre-existing Trends from January 1–22, 2019 | ||||||
|---|---|---|---|---|---|---|---|---|
| NRF | NPI | NRF | NPI | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National | −0.227*** | −0.176*** | −0.023*** | −0.009*** | −2.471 | −1.604 | −0.540 | −0.291 |
| (0.048) | (0.028) | (0.001) | (0.001) | (1.954) | (2.221) | (0.426) | (0.459) | |
| Local | −0.276*** | −0.280*** | −0.034* | −0.031** | 0.470 | 0.413 | 0.048 | 0.020 |
| (0.049) | (0.038) | (0.016) | (0.013) | (0.456) | (0.511) | (0.101) | (0.100) | |
| Neighbor | 0.043 | 0.002 | −0.003 | −0.021 | ||||
| (0.096) | (0.108) | (0.027) | (0.032) | |||||
| K-means 1000 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Control Variables | No | Yes | No | Yes | No | Yes | No | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 118,207 | 118,207 | 118,207 | 118,207 |
| R-squared | 0.111 | 0.190 | 0.129 | 0.269 | 0.490 | 0.550 | 0.227 | 0.359 |
| Variables | Test for Pre-existing Trends from January 23– March 18, 2019 | Test for Pre-existing Trends from March 19-May 31, 2019 | ||||||
|---|---|---|---|---|---|---|---|---|
| NRF | NPI | NRF | NPI | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National | −1.058 | −2.494 | 0.332 | 0.505 | 4.475 | 4.196 | 2.053 | 2.700 |
| (0.643) | (1.785) | (0.269) | (0.301) | (3.862) | (5.964) | (1.257) | (2.109) | |
| Local | 0.011 | 0.009 | −0.010 | −0.011 | 0.109 | 0.071 | 0.056 | 0.070 |
| (0.065) | (0.053) | (0.014) | (0.008) | (0.155) | (0.158) | (0.039) | (0.038) | |
| K-means 1000 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Control Variables | No | Yes | No | Yes | No | Yes | No | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 188,251 | 188,251 | 188,251 | 188,251 | 271,641 | 271,641 | 271,641 | 271,641 |
| R-squared | 0.492 | 0.548 | 0.345 | 0.450 | 0.205 | 0.296 | 0.210 | 0.342 |
The regressions are estimated using weighted least squares, using as weight the daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% levels of confidence. All errors are clustered at the city level.
Table D2.
Results at Different Stages of the Pandemic with 1000 Clusters.
| Variable | PANEL A: Post = 1 for Post-COVID period (March 19-May 31, 2020) vs Pre-COVID Period (January 1–22, 2020) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Post | −0.277*** | −2.038*** | −35.432** | 0.974*** | 0.421*** | 6.721*** | 2.860** |
| (0.008) | (0.344) | (11.313) | (0.102) | (0.128) | (2.031) | (0.924) | |
| K-means 1000 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 |
| R-squared | 0.238 | 0.359 | 0.143 | 0.233 | 0.209 | 0.178 | 0.274 |
| Variable | PANEL B: Post=1 for Post-COVID Period (March 19-May 31, 2020) vs COVID Period (January 23-March 18, 2020) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (8) | (9) | (10) | (11) | (12) | (13) | (14) | |
| Post | −0.523*** | −5.617*** | −37.014*** | 0.741*** | 0.701*** | 8.946*** | 3.677*** |
| (0.101) | (0.304) | (11.370) | (0.169) | (0.057) | (2.321) | (0.405) | |
| K-means 1000 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 |
| R-squared | 0.221 | 0.348 | 0.152 | 0.229 | 0.207 | 0.160 | 0.292 |
| Variable | PANEL C: Post=1 for Post-Covid Period (March 19-May 31, 2020) vs year 2019 (March 19-May 31, 2019) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (8) | (9) | (10) | (11) | (12) | (13) | (14) | |
| Post | −3.552*** | −1.853*** | −52.779** | 1.720*** | 0.222* | 4.831*** | 2.366*** |
| (0.727) | (0.409) | (22.279) | (0.164) | (0.100) | (0.188) | (0.402) | |
| K-means 1000 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 |
| R-squared | 0.257 | 0.384 | 0.192 | 0.266 | 0.158 | 0.206 | 0.298 |
The regressions are estimated using weighted least squares. The dependent variable is the weighted daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
Table D3.
Robustness Check for Regional Spillovers and Pre-trends with 1500 Clusters.
| Variables | Impact of Infections in Neighboring Cities | Test for Pre-existing Trends from January 1–22, 2019 | ||||||
|---|---|---|---|---|---|---|---|---|
| NRF | NPI | NRF | NPI | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National | −0.017*** | −0.110*** | −0.039*** | −0.070*** | −2.330 | −1.428 | −0.172 | 0.151 |
| (0.003) | (0.001) | (0.009) | (0.018) | (1.716) | (2.050) | (0.409) | (0.461) | |
| Local | −0.332*** | −0.334*** | −0.012*** | −0.010*** | 0.492 | 0.491 | 0.019 | 0.006 |
| (0.064) | (0.049) | (0.003) | (0.002) | (0.432) | (0.491) | (0.098) | (0.098) | |
| Neighbor | 0.098 | 0.043 | 0.015 | −0.009 | ||||
| (0.091) | (0.111) | (0.023) | (0.026) | |||||
| K-means 1500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Control Variables | No | Yes | No | Yes | No | Yes | No | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 144,044 | 144,044 | 144,044 | 144,044 | 118,207 | 118,207 | 118,207 | 118,207 |
| R-squared | 0.127 | 0.203 | 0.142 | 0.277 | 0.501 | 0.561 | 0.237 | 0.365 |
| Variables | Test for Pre-existing Trends from January 23– March 18, 2019 | Test for Pre-existing Trends from March 19-May 31, 2019 | ||||||
|---|---|---|---|---|---|---|---|---|
| NRF | NPI | NRF | NPI | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| National | −0.760 | −2.543 | 0.529 | 0.730 | −0.122 | −0.286 | 1.214 | 1.795 |
| (0.439) | (1.517) | (0.781) | (0.531) | (3.793) | (5.828) | (1.417) | (1.220) | |
| Local | 0.016 | 0.010 | −0.007 | −0.009 | 0.129 | 0.071 | 0.072 | 0.077 |
| (0.068) | (0.053) | (0.014) | (0.008) | (0.105) | (0.111) | (0.059) | (0.056) | |
| K-means 1500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Control Variables | No | Yes | No | Yes | No | Yes | No | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Restaurant FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Month FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 188,251 | 188,251 | 188,251 | 188,251 | 271,641 | 271,641 | 271,641 | 271,641 |
| R-squared | 0.499 | 0.555 | 0.350 | 0.454 | 0.209 | 0.299 | 0.220 | 0.350 |
The regressions are estimated using weighted least squares, using as weight the daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% levels of confidence. All errors are clustered at the city level.
Table D4.
Results at Different Stages of the Pandemic with 1500 Clusters.
| Variable | PANEL A: Post = 1 for Post-COVID period (March 19-May 31, 2020) vs Pre-COVID Period (January 1–22, 2020) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Post | −0.946*** | −1.983*** | −34.660*** | 0.240* | 0.197* | 4.464** | 1.497*** |
| (0.259) | (0.464) | (9.965) | (0.121) | (0.092) | (1.885) | (0.277) | |
| K-means 1500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 | 317,921 |
| R-squared | 0.254 | 0.367 | 0.160 | 0.246 | 0.222 | 0.169 | 0.284 |
| Variable | PANEL B: Post=1 for Post-COVID Period (March 19-May 31, 2020) vs COVID Period (January 23-March 18, 2020) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (8) | (9) | (10) | (11) | (12) | (13) | (14) | |
| Post | −0.241*** | −5.382*** | −30.545*** | 0.710** | 0.713*** | 9.420*** | 3.396*** |
| (0.007) | (0.396) | (6.074) | (0.270) | (0.055) | (1.884) | (0.415) | |
| K-means 1500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 | 314,223 |
| R-squared | 0.235 | 0.357 | 0.165 | 0.238 | 0.227 | 0.174 | 0.299 |
| Variable | PANEL C: Post=1 for Post-Covid Period (March 19-May 31, 2020) vs year 2019 (March 19-May 31, 2019) | ||||||
|---|---|---|---|---|---|---|---|
| Fat | Sugar | Sodium | Protein | Fiber | NRF | NPI | |
| (8) | (9) | (10) | (11) | (12) | (13) | (14) | |
| Post | −2.948*** | −1.220** | −37.868*** | 1.686*** | 0.085*** | 5.140*** | 1.594*** |
| (0.315) | (0.386) | (0.399) | (0.170) | (0.006) | (1.300) | (0.108) | |
| K-means 1500 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City-month | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chain FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| City FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day of the week FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hour FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Day FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 | 515,691 |
| R-squared | 0.267 | 0.389 | 0.200 | 0.273 | 0.175 | 0.215 | 0.306 |
The regressions are estimated using weighted least squares. The dependent variable is the weighted daily number of transactions in each restaurant. Note that *, **, *** indicate 90%, 95%, and 99% confidence intervals. All errors are clustered at the city level.
References
- Agüero J.M., Beleche T. Health shocks and their long-lasting impact on health behaviors: Evidence from the 2009 H1N1 pandemic in Mexico. J. Health Economics. 2017;54:40–55. doi: 10.1016/j.jhealeco.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allcott H., Boxell L., Conway J., Gentzkow M., Thaler M., Yang D. Polarization and public health: Partisan differences in social distancing during the Coronavirus pandemic. J. Public Economics. 2020;191:104254. doi: 10.1016/j.jpubeco.2020.104254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almond, D., & Currie, J. (2011). Chapter 15 - Human capital development before age five. In Handbook of Labor Economics. Chapter 15, Part B, vol. 4. Elsevier, pp. 1315–1486.
- Alston J.M., MacEwan J.P., Okrent A.M. The economics of obesity and related policy. Annual Review of Resource Economics. 2016;8(1):443–465. [Google Scholar]
- Anderson M.L., Gallagher J., Ritchie E.R. School meal quality and academic performance. J. Public Economics. 2018;168:81–93. [Google Scholar]
- Baron E.J., Goldstein E.G., Wallace C.T. Suffering in silence: How COVID-19 closures inhibit the reporting of child maltreatment. J. Public Economics. 2020;190(C): 104258:13 pages. doi: 10.1016/j.jpubeco.2020.104258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belot M., James J. Healthy school meals and educational outcomes. J. Health Economics. 2011;30(3):489–504. doi: 10.1016/j.jhealeco.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Bennett D., Chiang C.F., Malani A. Learning during a crisis: The SARS epidemic in Taiwan. J. Dev. Econ. 2015;112:1–18. doi: 10.1016/j.jdeveco.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg J., Thompson G. Nonparametric segmentation methods: Applications of unsupervised machine learning and revealed preferences. Am. J. Agric. Econ. 2021;104:976–998. [Google Scholar]
- Cawley, J., & Ruhm, C.J. (2012). The economics of risky health behaviors. In Handbook of Health Economics, Volume 2, Chapter 3, 97-199.
- Chakraborty T., Jayaraman R. School feeding and learning achievement: Evidence from India's midday meal program. J. Dev. Econ. 2019;139:249–265. [Google Scholar]
- Chang T.Y., Huang W., Wang Y. Something in the air: Pollution and the demand for health insurance. The Review of Economic Studies. 2018;85(3):1609–1634. [Google Scholar]
- Chetty, R., Friedman, J., Hendren, N., & Stepner, M. (2020). The economic impacts of COVID-19: Evidence from a new public database built from private sector data. Working paper. https://opportunityinsights. org/wp-content/uploads/2020/05/tracker_paper. pdf.
- Chinese Center for Disease Control and Prevention . 6th Edition. Peking University Publishing; Beijing: 2019. China Food Composition Tables. [Google Scholar]
- Cutler D.M., Huckman R.S., Landrum M.B. The role of information in medical markets: An analysis of publicly reported outcomes in cardiac surgery. American Economic Review. 2004;94(2):342–346. doi: 10.1257/0002828041301993. [DOI] [PubMed] [Google Scholar]
- Dai W., Luca M. Digitizing disclosure: The case of restaurant hygiene scores. American Economic Journal: Microeconomics. 2020;12(2):41–59. [Google Scholar]
- Danaf M., Becker F., Song X., Atasoy B., Ben-Akiva M. Online discrete choice models: Applications in personalized recommendations. Decis. Support Syst. 2019;119:35–45. [Google Scholar]
- Delaney, L., G. Fink, and C.P. Harmon. 2014. Effects of stress on economic decision-making: Evidence from laboratory experiments. Working Paper. IZA Discussion Paper No. 8060. Available at SSRN: https://ssrn.com/abstract=2420705.
- Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attina A., Cinelli G., Leggen C., Caparello G., Barrea L., Scerbo F., Esposito E., De Lorenzo A. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Translational Medicine. 2020;18(229):1–15. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnoski A. Defining nutrient density: Development and validation of the nutrient rich foods index. J. Am. Coll. Nutr. 2009;28(4):4215–4265. doi: 10.1080/07315724.2009.10718106. [DOI] [PubMed] [Google Scholar]
- Drewnowski A., Fulgoni V.L., III Nutrient density: principles and evaluation tools. The American J. clinical nutrition. 2014;99(5):1223S–1228S. doi: 10.3945/ajcn.113.073395. [DOI] [PubMed] [Google Scholar]
- Hanna R., Duflo E., Greenstone M. Up in smoke: The influence of household behavior on the long-run impact of improved cooking stoves. American Economic Journal: Economic Policy. 2016;8(1):80–114. [Google Scholar]
- Jin G.Z., Leslie P. The effect of information on product quality: Evidence from restaurant hygiene grade cards. Q. J. Econ. 2003;118(2):409–451. [Google Scholar]
- Koppel L., Andersson D., Posadzy K., Västfjäll D., Tinghög G. The effect of acute pain on risky and intertemporal choice. Experimental Economics. 2017;20(4):878–893. doi: 10.1007/s10683-017-9515-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, S., Bogoch, I.I., Ruktanonchai, N.W., Watts, A., Lu, X., Yang, W., Yu, Hongjie, Khan, K., & Tatem, A.J. (2020). Assessing spread risk of Wuhan novel coronavirus within and beyond China, January-April 2020: A travel network-based modeling study. MedRxIV, PMC7276059, March 9, 2020. Available at https://doi.org/10.1101/2020.02.04.20020479.
- Laitinen J., Ek E., Sovio U. Stress-related eating and drinking behavior and body mass index and predictors of this behavior. Prev. Med. 2002;34(1):29–39. doi: 10.1006/pmed.2001.0948. [DOI] [PubMed] [Google Scholar]
- Naja F., Hamadeh R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. European Review of Clinical Nutrition. 2020;74(8):1117–1121. doi: 10.1038/s41430-020-0634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver G., Wardle J. Perceived effects of stress on food choice. Physiol. Behav. 1999;66(3):511–515. doi: 10.1016/s0031-9384(98)00322-9. [DOI] [PubMed] [Google Scholar]
- Oster E. Diabetes and diet: Purchasing behavior change in response to health information. American Economic Journal: Applied Economics. 2018;10(4):308–348. doi: 10.1257/app.20160232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope D.G. Reacting to rankings: Evidence from “America's Best Hospitals”. J. Health Economics. 2009;28(6):1154–1165. doi: 10.1016/j.jhealeco.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Qian Y., Fan W. Who loses income during the COVID-19 outbreak? Evidence from China. Research in Social Stratification and Mobility. 2020;68:100522. [Google Scholar]
- Smith T.G. Economic stressors and the demand for “fattening” foods. Am. J. Agric. Econ. 2012;94(2):324–330. [Google Scholar]
- Staudigel M. A soft pillow for hard times? Economic insecurity, food intake and body weight in Russia. J. Health Economics. 2016;50:198–212. doi: 10.1016/j.jhealeco.2016.09.001. [DOI] [PubMed] [Google Scholar]
- Thomsen M.R., Nayga R.M., Jr, Alviola P.A., IV, Rouse H.L. The effect of food deserts on the body mass index of elementary school children. Am. J. Agric. Econ. 2016;98(1):1–18. [Google Scholar]
- U.K. Department of Health. (2011). Nutrient Profiling Technical Guidance. Accessed from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216094/dh_123492.pdf.
- U.S. Centers for Disease Control and Prevention (2020). Coronavirus Diseases 2019: People with Certain Medical Conditions, https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
- U.S. Department of Health and Human Services. (2005). 2005 Dietary Guidelines for Americans. https://health.gov/sites/default/files/2020-01/DGA2005.pdf.
- World Health Organization (2020), Connecting the World to Combat Coronavirus. https://www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---healthy-diet.
- Zhu C., Lopez R.A., Liu X. Information cost and consumer choices of healthy foods. Am. J. Agric. Econ. 2016;98(1):41–53. [Google Scholar]
- Zimmer, G. (2020). Our diets are changing because of the coronavirus pandemic. Is it for the better? Times, April 28, 2020.