Abstract
Background:
Squamous cell carcinoma (SCC) is a common cancer of the oral cavity. It mainly affects patients aged over 50 with male-to-female ratio 2:1. Most of the cases of oral SCC are linked to tobacco and alcohol use.
Objective:
In this report, we present a case of a 67-year-old male with a mass on the posterior-lateral border of the tongue.
Case report:
In this report, we present a case of a 67-yearold male with a mass on the posterior-lateral border of the tongue. Being heavy smoker and alcoholic since a young age, he was at high-risk of developing oral cancer. After thorough clinical, histopathological, and imaging assessments a poorly differentiated stage III (T3, N1, M0) SCC was confirmed. He underwent left hemiglossectomy with marginal mandibulectomy and radical neck dissection followed by radiation therapy.
Conclusion:
SCCs of the tongue can be often asymptomatic and identified at advanced phase leading to a poor prognosis. Therefore, their early diagnosis/management, and regular postoperative follow-ups are mandatory for better treatment outcome and recurrence prevention.
Keywords: Cancer, oral, squamous cell carcinoma, tongue, floor of the mouth
1. BACKGROUND
Squamous cell carcinoma (SCC) is a malignant epithelium-derived neoplasm occurring all over the body, but mostly in the skin and oral cavity (1); it represents up to 90% of all oral cancers (2, 3). Generally, it affects patients aged over 50, with history of high tobacco and alcohol consumption (4). SCCs of the tongue, frequently located at the lateral border, account for 25 to 40% of these neoplasms and are responsible along with SCCs of the floor of the mouth for more than 50% of the intraoral carcinomas (5). Survival rate at five years of SCC of the tongue varies between 40 and 50% (6-8).
Diagnosis of SCC of the tongue needs thorough clinical, radiological, and histological evaluations. Clinically, it may present as: a) an ulcerative swelling with fissuring or raised hard exophytic margins, b) a red lesion (erythroplakia), or c) a white or mixed white and red lesion (9).
Radiologically, computed tomography (CT) and magnetic resonance imaging (MRI), are of great importance for assessing this complex region. Their major advantage resides in their capability to identify the extent of the lesion, depth of invasion, involvement of tongue muscles, and importantly the nodal number, size, location, contour, and necrosis (10, 11).
Histologically, the lesion starts as an epithelial dysplasia with altered proliferation of dysplastic squamous cells on the surface of the epithelium, which consequently degrades the sub-epithelial basement membrane resulting in local destruction and distant invasion via metastasis (12).
Management of SCC of the tongue is mostly surgical, with radical neck dissection in the case of lymph node involvement. Radiotherapy and chemotherapy are considered as extra-postoperative treatments for advanced stages of cancer (1).
2. OBJECTIVE
In this report, we present a case of a 67-year-old male with a mass on the posterior-lateral border of the tongue. Being heavy smoker and alcoholic since a young age, he was at high-risk of developing oral cancer.
3. CASE PRESENTATION
A 67-year-old male was referred by his dentist to our specialized oral medicine clinic for evaluation of a mass on the posterior-lateral border of the tongue. Medical history was unremarkable and physical examination revealed no extra-oral abnormal findings. Intraorally, the patient presented a bilateral posterior edentulous in both jaws. Additionally, he complained of occasional bleeding from the lesion without pain or any other symptoms such as speech disturbance, difficulty in opening his mouth etc. He was a heavy smoker and excessive alcohol user for more than 30 years.
The lesion was firm and had an ulcerative exophytic white surface with ill-defined indurated margins. It was fixed to the underlying tissues, reaching inferiorly the floor of the mouth and the alveolar ridge of the mandible. Antero-posteriorly, it extended from the premolar region to the 2nd molar region (Figure 1). On neck palpation, there were enlarged, non-tender, and firm left cervical lymph nodes.
Figure 1. Ulcero-proliferative mass located in the left lateral border of the tongue extending inferiorly to the floor of the mouth and the alveolar ridge of the mandible.
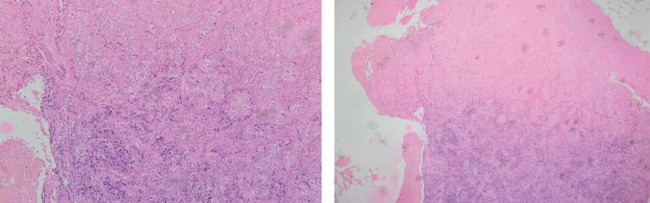
A biopsy of the lesion was performed and sent for histopathological assessment. Microscopic examination showed a neoplastic keratinized proliferation consisting of poorly differentiated squamous cells arranged in trabeculae of variable size ulcerating the epithelium and infiltrating the underlying lamina propria (Figure 2). The histological diagnosis of poorly differentiated SCC was made.
Figure 2. Microscopic features of the lesion.
Subsequently, a CT scan of the head and neck along with a total-body positron emission tomography (PET)/CT scan were performed. Consequently, the final diagnosis of SCC stage III (T3, N1, M0) was confirmed.
The patient was referred to a head and neck oncologist and underwent left hemiglossectomy with marginal mandibulectomy and left radical neck dissection followed by radiation therapy. Currently, after one year of the surgery he is clinically normal and under regular follow-up.
4. DISCUSSION
SCC is the most common cancer of the oral cavity with male-to-female ratio 2:1. The tongue, oropharynx, and floor of the mouth are the most affected sites. SCC of the gingiva and lips are less reported (1, 10, 13). Most of the cases of oral SCC are linked to tobacco and alcohol use. Moreover, a study conducted by Hashibe et al. confirmed that the joint effect between tobacco and alcohol use makes the head and neck cancer risk even higher (14). Additionally, many other factors such as ultraviolet light, human papillomavirus (HPV), Candida infections, radiation, genetic factors, malnourishment, diet, and chemical exposures to betel quit and areca nut have also been proposed as risk factors (2, 15). Before progressing to the malignant stage, many of oral cavity SCC cases develop from premalignant lesions like leukoplakia and erythroplakia, histologically characterized by degrees of dysplasia and clinically asymptomatic (1, 15). Oral SCCs are often misdiagnosed or identified at a late phase (in stages III or IV), leading to significant deterioration in patient quality of life and noticeably decreasing the survival chances due to the delay in delivering prompt and adequate treatment (12, 16).
Our patient was at high-risk for developing oral cancer given his history of concomitant heavy smoking and alcohol addiction since a young age. Also, his initial lesion of the posterior-lateral border of the tongue might have been ignored or underestimated during previous oral exams.
Histopathological assessment of SCC determines the tumor grading by identifying the abnormal cells differentiation. Poorly differentiated SCCs are habitually considered more aggressive, and in many cases presenting worse prognosis (15). As for the staging, it is usually based on the American Joint Committee for Cancer (AJCC) – TNM classification where 3 main parameters are assessed clinically, radiologically, and histopathologically: (T) tumor size, (N) tumor cell spread to draining lymph nodes, and (M) tumor cells spread to distant parts of the body as metastasis (15, 17). Another staging system AJCC/UICC (Union for International Cancer Control) is worldwide used. Among other features, it describes the lesion at presentation prior to treatment (clinical staging, cTNM), after surgical treatment (pathological staging, pTNM), and at disease recurrence (rTNM). In our case, the lesion was poorly differentiated with a cancer staging of AJCC Stage III–T3, N1, M0 given the size and the presence of palpable lymph nodes.
It is usually accepted that better prognosis is related to early oral SCCs, especially those that are well-differentiated and not metastasized. Unfortunately, most oral SCCs are diagnosed at a late stage of the disease leading to five year survival rates not exceeding 12% of the cases (9). In 2020, the International Agency for Research on Cancer (IARC) released the GLOBOCAN which is an online database providing global cancer statistics and estimation of incidence and mortality in 185 countries for 36 types of cancer. Accordingly, the GLOBOCAN reports 377,713 new cases of lip and oral cavity cancers worldwide and 177,757 resultant new deaths (18).
Our patient presented an advanced case, consequently he was treated surgically (hemiglossectomy with marginal mandibulectomy) and with radiation therapy. Furthermore, because of the lymph nodes involvement a radical neck dissection was performed.
5. CONCLUSION
Like the majority of oral cancers, SCCs of the tongue can be often asymptomatic and identified at advanced phase leading to a poor prognosis. Hence, their early diagnosis/management, and regular postoperative follow-ups are mandatory for optimum treatment outcome and recurrence prevention.
Patient’s Consent Form:
Written informed consent was obtained from the patient for publication of this case report.
Conflicts of interest:
The authors declare that they have no conflicts of interests.
Financial disclosure:
No funding was received.
REFERENCES
- 1.Abraham S, Mallika B, Reshma A, Kassim RM. An atypical case of oral squamous cell carcinoma of mandibular alveolus. Case Rep Dent. 2019;2019:2521685. doi: 10.1155/2019/2521685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson NW, Jayasekara P, Amarasinghe AA. Squamous cell carcinoma and precursor lesions of the oral cavity: epidemiology and aetiology. Periodontol. 2000. 2011;57:19–37. doi: 10.1111/j.1600-0757.2011.00401.x. [DOI] [PubMed] [Google Scholar]
- 3.Pontes FS, Carneiro JT, Jr, Fonseca FP, da Silva TS, Pontes HA, Pinto Ddos S., Jr. Squamous cell carcinoma of the tongue and floor of the mouth: analysis of survival rate and independent prognostic factors in the Amazon region. J Craniofac Surg. 2011;22:925–930. doi: 10.1097/SCS.0b013e31820fe1cb. [DOI] [PubMed] [Google Scholar]
- 4.González-Guevara MB, Linares-Vieyra C, Castro-García ME, Muñiz-Lino MA, Abaroa-Chauvet C, Bello-Torrejón F. Carcinoma escamocelular bucal. Caso clínico y revisión de la literatura [Oral squamous cell carcinoma. Case report and review of literature] Rev Med Inst Mex Seguro Soc. 2022;60:85–90. [PMC free article] [PubMed] [Google Scholar]
- 5.Ion Ciucă Mărăşescu FI, Marasescu PC, Matei M, Florescu AM, Margaritescu C, Petrescu SMS, et al. Epidemiological and histopathological aspects of tongue squamous cell carcinomas-retrospective study. Curr Health Sci J. 2018;44(3):211–224. doi: 10.12865/CHSJ.44.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sano D, Myers JN. Metastasis of squamous cell carcinoma of the oral tongue. Cancer Metastasis Rev. 2007;26:645–662. doi: 10.1007/s10555-007-9082-y. [DOI] [PubMed] [Google Scholar]
- 7.Jehn P, Dittmann J, Zimmerer R, Stier R, Jehn M, Gellrich NC, et al. Survival rates according to tumour location in patients with surgically treated oral and oropharyngeal squamous cell carcinoma. Anticancer Res. 2019;39(5):2527–2533. doi: 10.21873/anticanres.13374. [DOI] [PubMed] [Google Scholar]
- 8.Zini A, Czerninski R, Sgan-Cohen HD. Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med. 2010;39:299–305. doi: 10.1111/j.1600-0714.2009.00845.x. [DOI] [PubMed] [Google Scholar]
- 9.Markopoulos AK. Current aspects on oral squamous cell carcinoma. Open Dent J. 2012;6:126–130. doi: 10.2174/1874210601206010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagale G, Pradhan SR, Basnet A. Tongue cancer in a young male. Cureus. 2021;13:e17702. doi: 10.7759/cureus.17702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sigal R, Zagdanski AM, Schwaab G, Bosq J, Auperin A, Laplanche A, et al. CT and MR imaging of squamous cell carcinoma of the tongue and floor of the mouth. Radiographics. 1996;16(4):787–810. doi: 10.1148/radiographics.16.4.8835972. [DOI] [PubMed] [Google Scholar]
- 12.Rivera C, Venegas B. Histological and molecular aspects of oral squamous cell carcinoma (Review) Oncol Lett. 2014;8:7–11. doi: 10.3892/ol.2014.2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Effiom OA, Adeyemo WL, Omitola OG, Ajayi OF, Emmanuel MM, Gbotolorun OM. Oral squamous cell carcinoma: a clinicopathologic review of 233 cases in Lagos, Nigeria. J Oral Maxillofac Surg. 2008;66:1595–1599. doi: 10.1016/j.joms.2007.12.025. [DOI] [PubMed] [Google Scholar]
- 14.Hashibe M, Brennan P, Chuang SC, Boccia S, Castellsague X, Chen C, et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol Biomarkers Prev. 2009;18(2):541–550. doi: 10.1158/1055-9965.EPI-08-0347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patton LL, Glick M. 2nd. Hoboken, New Jersey: John Wiley and Sons; 2016. The ADA Practical guide to patients with medical conditions; pp. 81–88. [Google Scholar]
- 16.Jung DW, Che ZM, Kim J, Kim K, Kim KY, Williams D, et al. Tumor-stromal crosstalk in invasion of oral squamous cell carcinoma: a pivotal role of CCL7. Int J Cancer. 2010;127(2):332–344. doi: 10.1002/ijc.25060. [DOI] [PubMed] [Google Scholar]
- 17.Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67(2):93–99. doi: 10.3322/caac.21388. [DOI] [PubMed] [Google Scholar]
- 18.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]