Abstract
Background
Sierra Leone is one of the countries with poor health outcomes. The country has made some progress in the uptake of maternal health services. Despite improvements in the national coverage rates, there is no evidence of how equal these improvements have been.
Objective
To estimate inequalities in maternal healthcare use in Sierra Leone.
Methods
Using cross-sectional study data from 2008, 2013, and 2019 Demographic and Health Surveys (DHS), we study inequalities in maternal health services by computing rate ratios, and concentration indices (as well as concentration curves) using selected inequality stratifiers such as household wealth index, maternal education, and rural/urban place of residence.
Results
We found that considerable progress has been made in increasing the uptake of maternal health services as well as reducing inequalities over time. We also found that inequalities in the selected health indicators favoured women from wealthy households, educated women, as well as women from urban areas. Although inequalities declined over time, the use of delivery services was highly unequal. However, of the selected health interventions, the use of four or more antenatal visits was almost at perfect equality in 2013 and 2019.
Conclusion
Although efforts have been made to increase the use of maternal healthcare services among women with a lower socioeconomic status, the use of maternal health services remains favourable to women with a higher socioeconomic standing. Therefore, policy initiatives need to prioritise women of lower socioeconomic status through projects aimed at increasing women’s educational levels as well as focusing on poverty reduction.
Introduction
The improvement of women’s sexual and reproductive health and rights remains important in the fight to reduce child and maternal mortality. Low- and middle-income countries (LMIC), often have maternal mortality ratios (MMR) due to childbirth-related complications. Estimates show that the Sub-Saharan Africa region has a soaring MMR of 542 per 100000 live births [1]. Three countries made the largest contribution to the MMR in the region; these include South Sudan (1150 maternal deaths per 100000 live births), Chad (1140 maternal deaths per 100000 live births) and Sierra Leone (1120 maternal deaths per 100000 live births) [1]. These high rates are partially due to various challenges which tend to intensify them such as lack of access to and provision of healthcare services, lack of or inadequate use of family planning services, malnutrition, and other issues [2–5]. Many countries have made significant strides toward meeting their Millennium Development Goals (MDG) targets, especially when it comes to the use of maternal health services [6]. However, the progress made at the national level tends to hide the inequalities that still exist at lower levels of geography (i.e., districts and chiefdoms). The level of maternal health service use differs between different socioeconomic groups within a country. It remains to be seen if the Sustainable Development Goals (SDGs) will build on the MDGs in increasing the use of maternal health services while reducing inequalities between socioeconomic groups.
Sierra Leone has had challenges trying to reduce the MMR and improve maternal health service provision. After years of struggles in dealing with high maternal mortality levels and poor uptake and provision of maternal health services (i.e., home birth deliveries) due to unaffordability, the government introduced the Free Health Care Initiative (FHCI) around 2010 as a way of improving the use of maternal and child healthcare [7,8]. In poor communities, out-of-pocket (OOP) expenditure on health becomes unrealistic. The FHCI removed user fees for women and young children needing to use healthcare services [9]. This led to some improvements in the update of life-saving maternal health services. The percentage of births that were delivered at home decreased over time in the country from 71.8% in 2008, 24.4% in 2013, and 16.4% in 2019 [10–12]. High financial costs often become a barrier to healthcare use, especially in rural areas where women are expected to travel long distance and pay more for transport to reach health services, especially in rural areas [13–15]. However, there is evidence of the existence of health inequalities in the country despite many improvements in maternal healthcare use. Studies show the existence of wealth-based health inequalities in some parts of the country [16,17].
To analyse inequalities in maternal healthcare, we adopted the framework developed by the Commission on Social Determinants of Health (CSDH). The CSDH framework argues that social position is an important determinant of health inequities [18]. The framework considers different elements of inequality such as socioeconomic status, education, race and geographic location as well as other elements [18–20]. In this study, we included maternal education, and household wealth index as the structural determinants of health; we also include the place of residence in the analysis. The structural determinants are part of the social and economic context of individuals and these are often regarded as the actual social determinants of health [18]. Inequalities in healthcare, especially in LMIC have drawn a lot of attention in recent times [21]. Addressing the health needs of the populations in lower socioeconomic positions is crucial in improving the overall health of the entire population. Although a few studies on healthcare inequalities have been conducted in Sierra Leone, many have focused on different aspects of healthcare inequality, and have used other measures and datasets, than those considered in this study [16,17,22,23]. This study aims to explore the extent of health inequalities in maternal healthcare as well as possible changes in these inequalities in Sierra Leone.
Methods
Data sources
We used cross-sectional data from the 2008, 2013, and 2019 Demographic and Health Surveys (SLDHS). The DHS collects nationally representative data on various health-related interventions. This data is publicly available for download upon request. The DHS data are among the widely used sources of data for analysis of health-related inequalities. The DHS conducted in Sierra Leone sampled 7 758 households in 2008, 13 006 households in 2013, and 13 793 households in 2019, with a response rate of 97.6%, 99.3%, and 99.5% respectively [10–12]. For all data collection points, women of reproductive age (WRA) who were either usual household members or women present in the household on the night before the survey were eligible for interviews. We indicate the study sample in Table 1.
Table 1. Sample used in the study.
| Survey year | 4+ ANC visits | Skilled ANC | Facility births | SBA |
|---|---|---|---|---|
| 2008 SLDHS | 3 380 | 4 103 | 5 651 | 5 811 |
| 2013 SLDHS | 7 532 | 8 647 | 12 079 | 12 198 |
| 2019 SLDHS | 6 448 | 7 326 | 9 771 | 9 771 |
| Total | 17 361 | 20 076 | 27 501 | 27 781 |
Note: The samples excluded “missing” and/or “do not know” cases.
Maternal health indicators
This section presents the maternal health indicators used in the study. We selected the following indicators: (i) four or more antenatal visits, (ii) skilled antenatal care providers, (iii) births assisted by a skilled birth attendant (SBA), and (iv) births delivered in a facility. We defined four or more antenatal care visits as women who had at least four or more antenatal care visits for their most recent pregnancy; this definition has been used elsewhere [24,25]. We defined skilled antenatal care providers as women whose antenatal visits (for the most recent birth) were attended by a skilled provider. We defined births delivered in a facility as births that were delivered in a health facility; the health facilities included a government hospital, government health centre, government health post, other public sector, private hospital/clinic, and other private sector. We also defined births assisted by a skilled birth attendant (SBA) as births that were assisted by a skilled birth attendant (i.e. skilled provider). A skilled provider included a doctor, nurse/midwife, or auxiliary midwife. We dichotomised the selected indicator variables and we coded them as 0 = no and 1 = yes. Inequality stratifiers and measures
This study used three stratifiers to measure health-related inequality (maternal education, household wealth index, and place of residence). The household wealth index was computed for each household [using the Principal Components Analysis (PCA) method] to disaggregate the sample into equal-sized quintiles (i.e. poorest to richest) [26]. We measured the prevalence of four maternal health indicators for each of the data points considered in this study. We used rate ratios to measure absolute differences in inequalities using the selected inequality stratifiers. The rate ratios provide a general description of the extent of inequalities. The rate ratios for the wealth index were measured in terms of highest versus lowest household wealth quintile (RRhhwi = Rhighest quintile ÷ Rlowest quintile). The rate ratios for maternal education were measured in terms of highest versus none (RReduc = Rhigher ÷ Rnone). The rate ratios for residence were measured in terms of urban vs rural (RRur = Rurban ÷ Rrural). The main limitation of the measures above is that they provide a basic picture of inequalities and ignore the differentials that often exist between all the categories of the inequality stratifier. For instance, in computing the rate ratios for the household wealth index, only two extremes are considered (richest quintile to poorest quintile) and not the rest of the quintiles.
To remedy this, we used the concentration index. The concentration index is the most used measure of health inequalities in public health studies. It shows the magnitude of health-related inequalities and whether these inequalities are concentrated among those with low socioeconomic status or those with high socioeconomic status. The index value becomes negative when the health intervention is concentrated among the poor and positive when it is concentrated among the rich [27]. If the concentration index is negative, then the health indicator is said to be concentrated among individuals with low socioeconomic status, while a positive concentration index shows that the health indicator is concentrated among individuals with a high socioeconomic status [28]. Therefore, to further quantify inequalities in the selected indicators, we employed the concentration index. Specifically, we employed the Erreygers corrected concentration index.
where bh and ah refer to the maximum and minimum bounds of the binary health indicator, μ refers to the mean of the health indicator, and C(h) refers to the concentration index [29]. The Erreygers corrected concentration index is recommended for use when the variable is binary [30]. The concentration curve is used to visualise the extent of inequalities in terms of the concentration index and the inequality stratifier is ranked across the x-axis and the cumulated fraction of the health intervention is plotted on the y-axis, and a diagonal line represents the line of equality [27]. Where the health intervention lies below the equity line, then it is said that there are pro-rich inequalities in that society, and when it lies above the equity line, then it is said there are pro-poor inequalities. We used the conindex command in Stata to estimate the corrected concentration index [31]. Various studies have used DHS data and applied similar methods to analyse the trends, determinants, and inequalities in maternal, child, and reproductive health interventions as well as service coverage [4,28,32–34].
Complex samples
For all the data points, the SLDHS used a two-stage cluster sampling approach to select respondents for the surveys [10–12]. As such, we needed to adjust for data representation in our analysis; therefore, we used the Stata svyset command to account for the under- and over-sampling of certain enumeration areas. An alpha (α) level of 0.05 was considered statistically significant. We used Stata version 14.2 [35] and Microsoft Excel for all analyses of this study.
Ethical considerations
We conducted all analyses using publicly available data from the SLDHS. The Institutional Review Board of Macro International, Inc. reviewed and approved the collection of data for all periods of the SLDHS data used in this study. Permission was granted to the authors by the DHS program to use this data for this study. For more information on the ethical review processes used by the DHS program. See more details on the ethical considerations in DHS data here: http://goo.gl/ny8T6X.
Results
Prevalence and rate ratios
Table 2 shows the ratios of education-related inequalities among WRA between those with no education and those with higher levels of education. There was an increase in the use of maternal health services over the three periods. The use of delivery care services (facility-based delivery and skilled birth attendance) doubled between 2008 and 2019. The ratios for the selected maternal health indicators indicate the existence of inequalities that favour women with higher levels of education. Moreover, there was a decrease in inequalities between women with no education and those with higher levels of education from 2008 to 2019 as shown by the decrease in ratios.
Table 2. Maternal health indicators by maternal education in 2008, 2013 and 2019.
| Maternal education | |||||||
|---|---|---|---|---|---|---|---|
| Health indicator | Survey year | None | Primary | Secondary | Higher | Total | Ratio |
| 4+ ANC visits | 2008 | 64.2 | 75.2 | 83.2 | 97.2 | 68.1 | 1.51 |
| 2013 | 85.9 | 86.8 | 91.6 | 97.2 | 87.3 | 1.13 | |
| 2019 | 88.7 | 89.1 | 90.6 | 93.8 | 89.5 | 1.06 | |
| Skilled ANC | 2008 | 84.5 | 92.7 | 94.6 | 98.5 | 86.9 | 1.17 |
| 2013 | 96.3 | 98.0 | 99.3 | 98.7 | 97.1 | 1.02 | |
| 2019 | 97.6 | 98.3 | 98.4 | 97.6 | 97.9 | 1.00 | |
| Facility births | 2008 | 20.5 | 34.5 | 44.9 | 70.7 | 25.3 | 3.45 |
| 2013 | 49.9 | 58.2 | 71.1 | 87.6 | 54.9 | 1.76 | |
| 2019 | 79.6 | 84.3 | 89.1 | 95.3 | 83.4 | 1.20 | |
| SBA | 2008 | 35.7 | 55.9 | 70.9 | 94.4 | 42.4 | 2.64 |
| 2013 | 54.2 | 63.0 | 78.4 | 90.8 | 59.7 | 1.68 | |
| 2019 | 83.3 | 86.7 | 93.2 | 97.3 | 86.9 | 1.17 | |
Note: 4+ ANC visits = four or more antenatal care visits; skilled ANC = skilled antenatal care provider; facility births = births delivered in a facility; SBA = births assisted by a skilled birth attendant.
Table 3 examines the prevalence of maternal healthcare use as well as the wealth-based inequality ratios for the selected maternal health indicators. The use of maternal health services increased with socioeconomic status, where there was a higher use of these services among women from the richest households. In terms of the ratios, the findings showed that inequalities favoured women from the richest households. The ratios showed a decline between 2008 and 2019, indicating a decrease in pro-rich maternal health inequalities.
Table 3. Maternal health indicators by household wealth quintile in 2008, 2013 and 2019.
| Household wealth | ||||||||
|---|---|---|---|---|---|---|---|---|
| Health indicator | Survey year | Poorest | Poorer | Middle | Rich | Richest | Total | Ratio |
| 4+ ANC visits | 2008 | 59.1 | 62.5 | 66.1 | 70.8 | 87.2 | 68.1 | 1.48 |
| 2013 | 83.9 | 86.3 | 87.2 | 87.8 | 92.5 | 87.3 | 1.10 | |
| 2019 | 88.1 | 90.9 | 90.8 | 92.0 | 84.6 | 89.5 | 0.96 | |
| Skilled ANC | 2008 | 82.1 | 83.2 | 85.9 | 89.4 | 96.1 | 86.9 | 1.17 |
| 2013 | 96.0 | 96.7 | 96.7 | 98.1 | 98.3 | 97.1 | 1.02 | |
| 2019 | 98.3 | 98.5 | 99.0 | 98.5 | 94.9 | 97.9 | 0.97 | |
| Facility births | 2008 | 17.4 | 21.8 | 23.9 | 28.4 | 40.5 | 25.3 | 2.33 |
| 2013 | 48.9 | 50.3 | 49.7 | 60.6 | 71.0 | 54.9 | 1.45 | |
| 2019 | 78.6 | 80.5 | 83.6 | 86.1 | 91.5 | 83.4 | 1.16 | |
| SBA | 2008 | 28.1 | 35.4 | 38.6 | 49.0 | 71.4 | 42.4 | 2.54 |
| 2013 | 50.9 | 52.0 | 53.2 | 67.4 | 83.7 | 59.7 | 1.64 | |
| 2019 | 82.3 | 82.4 | 86.1 | 91.8 | 95.9 | 86.9 | 1.17 | |
Note: 4+ ANC visits = four or more antenatal care visits; skilled ANC = skilled antenatal care provider; facility births = births delivered in a facility; SBA = births assisted by a skilled birth attendant.
Table 4 shows the prevalence of maternal healthcare use by urban-rural residence and ratios of urban to rural inequalities. The use of maternal health services was higher among women from urban areas than those from rural areas, except for the use of antenatal services in 2019. The ratios for antenatal services in 2019 indicated that inequalities slightly favoured women from rural areas. In general, the ratios in 2008 and 2013 showed that inequalities favoured women from urban areas for all indicators.
Table 4. Maternal health indicators by place of residence in 2008, 2013 and 2019.
| Place of residence | |||||
|---|---|---|---|---|---|
| Health indicator | Survey year | Urban | Rural | Total | Ratio |
| 4+ ANC visits | 2008 | 81.6 | 62.8 | 68.1 | 1.30 |
| 2013 | 91.0 | 85.8 | 87.3 | 1.06 | |
| 2019 | 89.0 | 89.7 | 89.5 | 0.99 | |
| Skilled ANC | 2008 | 93.9 | 84.1 | 86.9 | 1.12 |
| 2013 | 98.2 | 96.7 | 97.1 | 1.02 | |
| 2019 | 97.0 | 98.5 | 97.9 | 0.98 | |
| Facility births | 2008 | 40.6 | 19.6 | 25.3 | 2.07 |
| 2013 | 69.0 | 50.1 | 54.9 | 1.38 | |
| 2019 | 88.9 | 80.5 | 83.4 | 1.10 | |
| SBA | 2008 | 66.9 | 33.2 | 42.4 | 2.02 |
| 2013 | 78.9 | 53.2 | 59.7 | 1.48 | |
| 2019 | 94.1 | 83.1 | 86.9 | 1.13 | |
Note: 4+ ANC visits = four or more antenatal care visits; skilled ANC = skilled antenatal care provider; facility births = births delivered in a facility; SBA = births assisted by a skilled birth attendant.
Concentration curves
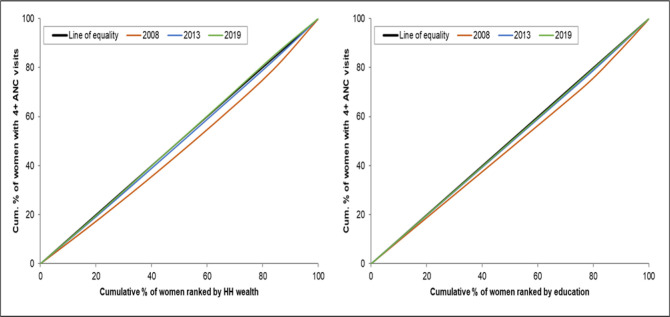
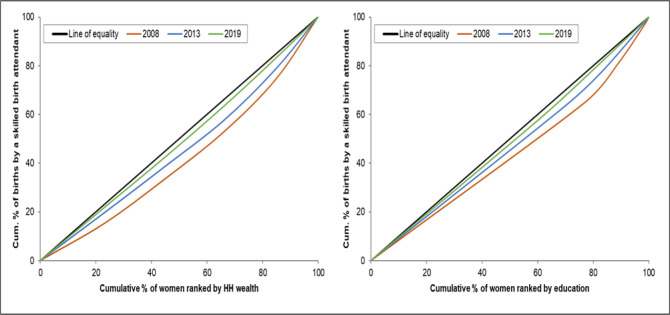
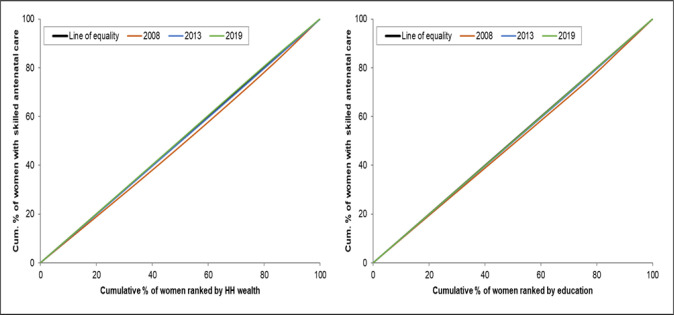
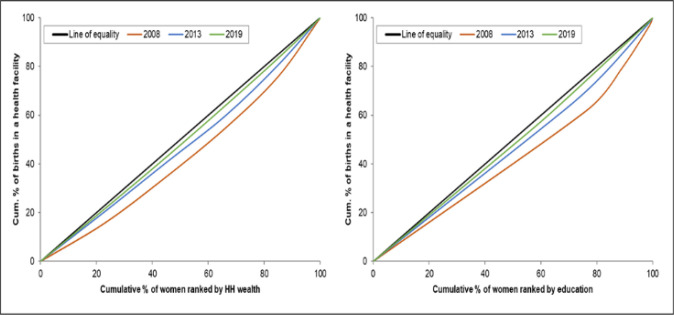
The concentration curves show that there are inequalities in the use of maternal health services favouring those with a higher socioeconomic position (women with higher levels of education and women from the richest households). There is a higher use of maternal health interventions by wealthier women than by poorer women (Figs 1–4). The inequalities decreased over time, as portrayed by the narrowing of the curves, particularly in the use of antenatal services. Figs 1 and 2 shows that the inequality gap has decreased over time. Moreover, by 2013 and 2019, the inequality gap had almost closed in terms of the use of antenatal services. Furthermore, the findings show that there is high inequality in the use of health facilities for delivery, and skilled birth attendants, as shown by the wide curves.
Fig 1. Concentration curves showing wealth-and-education-based inequality in the use of four or more antenatal visits in Sierra Leone, 2008, 2013 and 2019.
Fig 4. Concentration curves showing wealth-and-education-based inequality in the use of skilled birth attendants in Sierra Leone, 2008, 2013 and 2019.
Fig 2. Concentration curves showing wealth-and-education-based inequality in the use of skilled antenatal services in Sierra Leone, 2008, 2013 and 2019.
Fig 3. Concentration curves showing wealth-and-education-based inequality in the use of health facilities for delivery in Sierra Leone, 2008, 2013 and 2019.
Concentration indices
The wealth-based and maternal-education-based concentration indices show that there have been improvements (as shown by the decreasing levels over time) in inequality in the use of maternal healthcare use for about eleven years, from 2008–2019 (Tables 5 and 6). The biggest decrease in the concentration index was for the use of births assisted by a skilled birth attendant, which decreased from 0.330 to 0.113 for wealth-based inequalities and 0.230 to 0.095 for education-based inequalities (Tables 5 and 6). Conversely, there was high inequality in the use of delivery care services (births delivered in a facility and births assisted by a skilled birth attendant), in both 2008 and 2013.
Table 5. Concentration indices showing wealth-based inequality in the use of maternal health services in Sierra Leone, 2008, 2013 and 2019.
| Health indicator | Survey year | Conc. Index (CI) | SE (CI) | 95% CI | |
|---|---|---|---|---|---|
| Low | High | ||||
| 4+ ANC visits | 2008 | 0.197* | 0.023 | 0.152 | 0.243 |
| 2013 | 0.052* | 0.013 | 0.026 | 0.077 | |
| 2019 | 0.016 | 0.013 | -0.010 | 0.042 | |
| Skilled ANC | 2008 | 0.104* | 0.017 | 0.070 | 0.138 |
| 2013 | 0.022* | 0.005 | 0.012 | 0.032 | |
| 2019 | -0.007 | 0.007 | -0.021 | 0.008 | |
| Facility births | 2008 | 0.202* | 0.024 | 0.155 | 0.249 |
| 2013 | 0.196* | 0.024 | 0.148 | 0.244 | |
| 2019 | 0.109* | 0.019 | 0.072 | 0.147 | |
| SBA | 2008 | 0.330* | 0.026 | 0.279 | 0.382 |
| 2013 | 0.250* | 0.023 | 0.206 | 0.295 | |
| 2019 | 0.113* | 0.016 | 0.081 | 0.145 | |
Note: * = p<0.001
** = p<0.01; 4+ ANC visits = four or more antenatal care visits; skilled ANC = skilled antenatal care provider; facility births = births delivered in a facility; SBA = births assisted by a skilled birth attendant.
Table 6. Concentration indices showing education-based inequality in the use of maternal health services in Sierra Leone, 2008, 2013 and 2019.
| Health indicator | Survey year | Conc. Index (CI) | SE (CI) | 95% CI | |
|---|---|---|---|---|---|
| Low | High | ||||
| 4+ ANC visits | 2008 | 0.128* | 0.015 | 0.099 | 0.157 |
| 2013 | 0.038* | 0.009 | 0.021 | 0.056 | |
| 2019 | 0.021** | 0.008 | 0.005 | 0.038 | |
| Skilled ANC | 2008 | 0.070* | 0.010 | 0.050 | 0.090 |
| 2013 | 0.026* | 0.004 | 0.018 | 0.034 | |
| 2019 | 0.010** | 0.004 | 0.003 | 0.017 | |
| Facility births | 2008 | 0.170* | 0.015 | 0.141 | 0.200 |
| 2013 | 0.160* | 0.013 | 0.135 | 0.185 | |
| 2019 | 0.097* | 0.012 | 0.072 | 0.121 | |
| SBA | 2008 | 0.230* | 0.016 | 0.199 | 0.261 |
| 2013 | 0.179* | 0.013 | 0.155 | 0.204 | |
| 2019 | 0.095* | 0.012 | 0.071 | 0.118 | |
Note: * = p<0.001
** = p<0.01; 4+ ANC visits = four or more antenatal care visits; skilled ANC = skilled antenatal care provider; facility births = births delivered in a facility; SBA = births assisted by a skilled birth attendant.
Discussion
This study aimed to explore health inequalities in maternal healthcare in Sierra Leone. The findings show that considerable progress has been made in the use of maternal health services; the measures employed in the study show that inequalities in maternal healthcare use have declined since 2008. Our findings suggest that maternal health inequalities favour women from wealthy households, educated women, as well as women from urban areas. This could be because women with better socioeconomic status (wealthy households and higher education) tend to live in urban areas and can better pay for use and the available health services compared to their counterparts [36,37]. Moreover, improvements in wealth and education-based inequality were evident in 2013 and 2019 for the use of antenatal services. Although inequality declined over time, the use of delivery care services remained highly unequal. Our findings are similar to other studies which found substantial inequalities in the use of delivery services; similar studies show that inequalities in delivery care services tend to favour wealthier and more educated women [3,34,37,38]. A study in Sierra Leone also found that maternal education made a considerable contribution to inequalities in institutional delivery [16]. The cultural aspects of the population as well as their perceptions of modern medicine and related health provision are critical in understanding the use of maternal healthcare services [16,39].
Additionally, the findings show that there is some degree of inequality favouring populations in urban areas; this supports the literature which argues women in urban areas tend to have greater access to maternal health services compared to women in rural areas [40,41]. These findings speak to the rural-urban gap in the provision of healthcare services between rural and urban areas as well as the related barriers, such as costs and distance, disproportionally faced by women in rural areas [13–15,42]. The introduction of the FHCI and the removal of user fees might have contributed to the increase in the use of maternal health services as well as the reduction of inequality in the use of these services. Witter and colleagues have conducted numerous studies, which monitored and evaluated the main pillars of the FHCI concerning how these pillars have been implemented on the ground [43,44]. The authors argue that the use of maternal health services in the country has increased, and this increase could be attributed to the implementation of the FHCI [43,45,46]. It is difficult to pinpoint the exact contribution of the FHCI to increasing the use of health services since some of these health services had high uptake rates before the implementation of the FHCI [46]. Although the FHCI may have contributed to an increase in the use of maternal healthcare services, there is still some level of inequality that exists in the use of maternal healthcare services in the period highlighted in this study. A comprehensive analysis of the impact of this initiative (and other related initiatives) on the use of maternal health services and related inequalities in the country will be important for future research.
Strengths and limitations
The main strength of this study is that we used nationally representative datasets from three collection periods to better estimate inequalities in maternal healthcare use. The study uses cross-sectional data, as such, the data cannot serve as the basis for establishing causality among variables. There may be recall bias because of the longer recall time, where respondents are required to report on past occurrences of the use of certain healthcare services.
Conclusion
Our findings show that despite efforts by the government to increase the use of maternal healthcare services among women with a lower socioeconomic status, the use of these services remains favourable to those with a higher socioeconomic status. To ensure balance among the different socioeconomic groups, policy initiatives need to prioritise women with lower socioeconomic status (those with the most unequal maternal health services) through projects aimed at reducing poverty and increasing their educational levels, especially among women from rural areas. Moreover, further studies are necessary to study the specific impact of the FHCI and similar initiatives on the use of maternal healthcare services in the country, and what impact these initiatives have had on the reduction of health inequalities.
Acknowledgments
The authors would like to thank Ms. Anisha Panchia (Statistics South Africa), Dr. Lutendo Malisha (Statistics South Africa), and Mr. Amos Moto (Statistics South Africa), for their valuable assistance during the draft and editing phases of this paper. We would also like to thank the DHS for making the data used in this study available.
Abbreviations
- DHS
Demographic and Health Survey
- FHCI
Free Health Care Initiative
- MMR
Maternal Mortality Ratios
- MDGs
Millennium Development Goals
- PCA
Principal Components Analysis
- SBA
Skilled Birth Attendant
- SDGs
Sustainable Development Goals
Data Availability
The dataset is freely available for download and use upon registration on the Demographic and Health Survey Program website (https://dhsprogram.com/data/new-user-registration.cfm).
Funding Statement
This study forms part of MT’s PhD research, which was funded by the National Research Foundation (http://www.nrf.ac.za), under the scarce skills doctoral scholarship. The grant reference number is SFH14061268912. The funders played no role in study design, data collation and analysis, the decision to publish, or the preparation of the manuscript.
References
- 1.World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary. Geneva: World Health Organization, 2019. 2019. Report No.: Contract No.: WHO/RHR/19.23. [Google Scholar]
- 2.Zere E, Kirigia JM, Duale S, Akazili J. Inequities in maternal and child health outcomes and interventions in Ghana. BMC Public Health. 2012;12(1):252. doi: 10.1186/1471-2458-12-252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Obiyan MO, Kumar A. Socioeconomic Inequalities in the Use of Maternal Health Care Services in Nigeria:Trends Between 1990 and 2008. SAGE Open. 2015;5(4):2158244015614070. doi: 10.1177/2158244015614070 [DOI] [Google Scholar]
- 4.Goli S, Nawal D, Rammohan A, Sekher TV, Singh D. Decomposing the socioeconomic inequality in utilization of maternal health care services in selected countries of south Asia and sub-Saharan Africa. J Biosoc Sci. 2018;50(6):749–69. Epub 2017/10/31. doi: 10.1017/S0021932017000530 . [DOI] [PubMed] [Google Scholar]
- 5.De La Torre A, Nikoloski Z, Mossialos E. Equity of access to maternal health interventions in Brazil and Colombia: a retrospective study. Int J Equity Health. 2018;17(1):43. Epub 2018/04/13. doi: 10.1186/s12939-018-0752-x ; PubMed Central PMCID: PMC5896161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations Department of Economic and Social Affairs. The Millennium Development Goals Report. 2015. [Google Scholar]
- 7.Bertone MP, Samai M, Edem-Hotah J, Witter S. A window of opportunity for reform in post-conflict settings? The case of Human Resources for Health policies in Sierra Leone, 2002–2012. Conflict and Health. 2014;8(1):11. doi: 10.1186/1752-1505-8-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edoka I, McPake B, Ensor T, Amara R, Edem-Hotah J. Changes in catastrophic health expenditure in post-conflict Sierra Leone: an Oaxaca-blinder decomposition analysis. International Journal for Equity in Health. 2017;16(1):166. doi: 10.1186/s12939-017-0661-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Duinen AJ, Westendorp J, Ashley T, Hagander L, Holmer H, Koroma AP, et al. Catastrophic expenditure and impoverishment after caesarean section in Sierra Leone: An evaluation of the free health care initiative. PLOS ONE. 2021;16(10):e0258532. doi: 10.1371/journal.pone.0258532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Statistics Sierra Leone—SSL, ICF International. Sierra Leone Demographic and Health Survey 2013. SSL and ICF International: Freetown, Sierra Leone, 2014. [Google Scholar]
- 11.Statistics Sierra Leone—SSL ICF Macro. Sierra Leone Demographic and Health Survey 2008. Calverton, Maryland, USA: SSL and ICF Macro, 2009. [Google Scholar]
- 12.Statistics Sierra Leone—StatsSL, ICF. Sierra Leone Demographic and Health Survey 2019. Freetown/Sierra Leone: StatsSL/ICF, 2020. [Google Scholar]
- 13.Harris B, Goudge J, Ataguba JE, McIntyre D, Nxumalo N, Jikwana S, et al. Inequities in access to health care in South Africa. Journal of Public Health Policy. 2011;32(1):S102–S23. doi: 10.1057/jphp.2011.35 [DOI] [PubMed] [Google Scholar]
- 14.Silal SP, Penn-Kekana L, Harris B, Birch S, McIntyre D. Exploring inequalities in access to and use of maternal health services in South Africa. BMC Health Services Research. 2012;12(1):120. doi: 10.1186/1472-6963-12-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samuel O, Zewotir T, North D. Decomposing the urban–rural inequalities in the utilisation of maternal health care services: evidence from 27 selected countries in Sub-Saharan Africa. Reproductive Health. 2021;18(1):216. doi: 10.1186/s12978-021-01268-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jalloh MB, Bah AJ, James PB, Sevalie S, Hann K, Shmueli A. Impact of the free healthcare initiative on wealth-related inequity in the utilization of maternal & child health services in Sierra Leone. BMC Health Services Research. 2019;19(1):352. doi: 10.1186/s12913-019-4181-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bognini JD, Samadoulougou S, Ouedraogo M, Kangoye TD, Van Malderen C, Tinto H, et al. Socioeconomic inequalities in curative healthcare-seeking for children under five before and after the free healthcare initiative in Sierra Leone: analysis of population-based survey data. International Journal for Equity in Health. 2021;20(1):124. doi: 10.1186/s12939-021-01474-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. A conceptual framework for action on the social determinants of health. Geneva: World Health Organization; 2010. [Google Scholar]
- 19.Zere E, Oluwole D, Kirigia JM, Mwikisa CN, Mbeeli T. Inequities in skilled attendance at birth in Namibia: A decomposition analysis. BMC Pregnancy and Childbirth. 2011;11(1):34. doi: 10.1186/1471-2393-11-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chapman AR. The social determinants of health, health equity, and human rights. Health Hum Rights. 2010;12(2):17–30. Epub 20101215. . [PubMed] [Google Scholar]
- 21.Regidor E. Measures of health inequalities: part 1. Journal of Epidemiology and Community Health. 2004;58(10):858. doi: 10.1136/jech.2003.015347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Witter S, Zou G, Diaconu K, Senesi RGB, Idriss A, Walley J, et al. Opportunities and challenges for delivering non-communicable disease management and services in fragile and post-conflict settings: perceptions of policy-makers and health providers in Sierra Leone. Conflict and Health. 2020;14(1):3. doi: 10.1186/s13031-019-0248-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsawe M, Susuman AS. Examining inequality of opportunity in the use of maternal and reproductive health interventions in Sierra Leone. Journal of Public Health. 2020;42(2):254–61. doi: 10.1093/pubmed/fdz023 [DOI] [PubMed] [Google Scholar]
- 24.Mallick L, Dahiru T, MacQuarrie KLD. Trends in maternal health in Nigeria, 2003–2013. Rockville, Maryland, USA: ICF International, 2016. [Google Scholar]
- 25.Mallick L, Allen C, Hong R. Trends in maternal and child health in Cambodia, 2000–2014. Rockville, Maryland, USA: ICF, 2018. [Google Scholar]
- 26.Rutstein SO, Johnson K. The DHS wealth index. Calverton, Maryland, USA: ORC Macro, 2004. [Google Scholar]
- 27.World Health O. Handbook on health inequality monitoring with a special focus on low- and middle-income countries. Geneva: World Health Organization; 2013. 2013. [Google Scholar]
- 28.Makate M, Makate C. The evolution of socioeconomic status-related inequalities in maternal health care utilization: evidence from Zimbabwe, 1994–2011. Global health research and policy. 2017;2:1–. doi: 10.1186/s41256-016-0021-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Purohit BC. Inequity in Indian Health Care. Singapore: Springer; 2017. [Google Scholar]
- 30.Erreygers G. Correcting the Concentration Index. Journal of Health Economics. 2009;28(2):504–15. doi: 10.1016/j.jhealeco.2008.02.003 [DOI] [PubMed] [Google Scholar]
- 31.O’Donnell O O ’Neill S, Van Ourti T, Walsh B. conindex: Estimation of concentration indices. The Stata journal. 2016;16(1):112–38. . [PMC free article] [PubMed] [Google Scholar]
- 32.Boutayeb A, Helmert U. Social inequalities, regional disparities and health inequity in North African countries. International Journal for Equity in Health. 2011;10(1):23. doi: 10.1186/1475-9276-10-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bintabara D, Basinda N. Twelve-year persistence of inequalities in antenatal care utilisation among women in Tanzania: a decomposition analysis of population-based cross-sectional surveys. BMJ Open. 2021;11(4):e040450. doi: 10.1136/bmjopen-2020-040450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Novignon J, Ofori B, Tabiri KG, Pulok MH. Socioeconomic inequalities in maternal health care utilization in Ghana. International Journal for Equity in Health. 2019;18(1):141. doi: 10.1186/s12939-019-1043-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 36.Rashad AS, Sharaf MF. Who Benefits from Public Healthcare Subsidies in Egypt? Social Sciences. 2015;4(4):1162–76. doi: 10.3390/socsci4041162 [DOI] [Google Scholar]
- 37.Hajizadeh M, Alam N, Nandi A. Social inequalities in the utilization of maternal care in Bangladesh: Have they widened or narrowed in recent years? International Journal for Equity in Health. 2014;13(1):120. doi: 10.1186/s12939-014-0120-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Axelson H, Gerdtham U-G, Ekman B, Hoa DTP, Alfvén T. Inequalities in reproductive, maternal, newborn and child health in Vietnam: a retrospective study of survey data for 1997–2006. BMC Health Services Research. 2012;12(1):456. doi: 10.1186/1472-6963-12-456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higi AH, Debelew GT, Dadi LS. Perception and Experience of Health Extension Workers on Facilitators and Barriers to Maternal and Newborn Health Service Utilization in Ethiopia: A Qualitative Study. International Journal of Environmental Research and Public Health. 2021;18(19):10467. doi: 10.3390/ijerph181910467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Collin SM, Anwar I, Ronsmans C. A decade of inequality in maternity care: antenatal care, professional attendance at delivery, and caesarean section in Bangladesh (1991–2004). International Journal for Equity in Health. 2007;6(1):9. doi: 10.1186/1475-9276-6-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zere E, Tumusiime P, Walker O, Kirigia J, Mwikisa C, Mbeeli T. Inequities in utilization of maternal health interventions in Namibia: implications for progress towards MDG 5 targets. International journal for equity in health. 2010;9:16-. doi: 10.1186/1475-9276-9-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Habib SS, Jamal WZ, Zaidi SMA, Siddiqui J-U-R, Khan HM, Creswell J, et al. Barriers to Access of Healthcare Services for Rural Women—Applying Gender Lens on TB in a Rural District of Sindh, Pakistan. International Journal of Environmental Research and Public Health. 2021;18(19):10102. doi: 10.3390/ijerph181910102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Witter S, Brikci N, Harris T, Williams R, Keen S, Mujica A, et al. The free healthcare initiative in Sierra Leone: Evaluating a health system reform, 2010–2015. The International Journal of Health Planning and Management. 2018;33(2):434–48. doi: 10.1002/hpm.2484 [DOI] [PubMed] [Google Scholar]
- 44.Witter S, Wurie H, Bertone MP. The free health care initiative: how has it affected health workers in Sierra Leone? Health Policy and Planning. 2015;31(1):1–9. doi: 10.1093/heapol/czv006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sharkey A, Yansaneh A, Bangura PS, Kabano A, Brady E, Yumkella F, et al. Maternal and newborn care practices in Sierra Leone: a mixed methods study of four underserved districts. Health Policy and Planning. 2016;32(2):151–62. doi: 10.1093/heapol/czw104 [DOI] [PubMed] [Google Scholar]
- 46.Koroma MM, Kamara SS, Bangura EA, Kamara MA, Lokossou V, Keita N. The quality of free antenatal and delivery services in Northern Sierra Leone. Health research policy and systems. 2017;15(Suppl 1):49-. doi: 10.1186/s12961-017-0218-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset is freely available for download and use upon registration on the Demographic and Health Survey Program website (https://dhsprogram.com/data/new-user-registration.cfm).