Abstract
Introduction
We present a case of a 60-year-old female that underwent surgery for clipping a right vertebrobasilar junction aneurysm (VBJA) in a hybrid operation room.
Research question
Does the retrograde suction technique with a proximal balloon is safe and effective as an adjuvant technique in surgery of VBJA?
Material and methods
After an extended retrosigmoid approach was performed, a 6F Neuron catheter with an intermediate multipurpose catheter were navigated to the right vertebral artery (VA) through a 6-French sheath, which caused a severe catheter-induced vasospasm in the right VA. The aneurysm was then deflated and clipped. After the withdrawal of the catheter the vasospasm was resolved.
Results
The patient had a good recovery, with VI cranial nerve palsy and mild dysphagia due to mild right vocal cord palsy, both improving at 1-month follow-up and fully recovered at 6-month follow-up.
Discussion and conclusion
The combination of endovascular procedures and microsurgery at the same hybrid operation room in that case resulted in a safe and effective technique. It is an interesting tool that could help neurosurgeons deal with certain selected cases of VBJA. Intraoperative angiography offers the possibility to reposition a misplaced clip in the same surgery. Good collaboration between interventional neuroradiologists and vascular neurosurgeons helps in achieving good results in such difficult cases.
Keywords: Vertebrobasilar junction aneurysm, Aneurysm clipping, Endovascular assisted, Hybrid operation room
Abbreviations: VBJA, Vertebrobasilar Junction Aneurysm; DSA, Digital Subtraction Angiography; PICA, Posterior Inferior Cerebellar Artery; IONM, Intraoperative Neurophysiologic Monitoring; CN, Cranial Nerves; VA, Vertebral Artery; ICG, Indocianine Green Fluorescence; AICA, Anterior Inferior Cerebellar Artery
Highlights
-
•
Endovascular assisted surgery could add safety and efficacy to the treatment of certain selected cases of VBJA.
-
•
Proximal balloon occlusion and retrograde suction minimize cranial nerve manipulation for achieving proximal control.
-
•
Collaboration between Interventional Neuroradiologists and Vascular Neurosurgeons is of utmost importance.
-
•
Intraoperative angiography offers the chance to reposition a misplaced clip in the same surgery.
-
•
A hybrid operation room is a useful tool for the treatment of some particular neurovascular malformations.
1. Introduction
Proximal control is key in aneurysm surgery helping to soften aneurysm sac and preventing uncontrolled aneurysm bleeding during its dissection. In some particular cases such as paraclinoid and vertebrobasilar junction (VBJA) aneurysms, proximal control requires certain maneuvers that add extra dissection and could jeopardize vascular and/or neural structures like cranial nerves and brain stem perforators or approaches like carotid artery neck exposure. Endovascular assisted procedures (in a hybrid operation room) to gain proximal control have already been successfully used in certain centers.
Since 1990, when Batjer et al. (Batjer and Samson, 1990) described a technique to gain proximal control and deflate paraclinoid aneurysms (also known as “Dallas technique”) through an angiocatheter directly inserted in the internal carotid artery, this technique has evolved through some modifications of the initial procedure (Shucart et al., 1990) towards a truly/purely endovascular approach, therefore, avoiding surgical exposure of the carotid artery in the neck. The endovascular proximal occlusion with a balloon catheter and retrograde aspiration has been widely reported as a useful adjuvant technique for the clipping of paraclinoid aneurysms (Skrap et al., 2010; Chen et al., 2011; Ng et al., 2000; Flores et al., 2019). Likewise, intraoperative temporary balloon occlusion as proximal control has also been described in the treatment of basilar aneurysms (Shucart et al., 1990). This approach/technique minimizes dangerous manipulation of noble structures in attempting proximal control, making it faster and safer, and depending on the location of the aneurysm sparing a cervical incision and dissection.
The recent introduction of hybrid operation rooms has facilitated the performance of combined neurovascular procedures, such as the aforementioned endovascular proximal control, and represents an opportunity to refine/optimize these mixed techniques.
To the best of our knowledge this technique hasn't yet been described for the treatment of a VBJA. Even though it might not be necessary in all cases, and it was not first described for this type of aneurysms, we think it is an interesting tool to take into account in dealing with some particular cases of VBJA.
2. Case presentation
A 60-year-old female presented with sudden diplopia secondary to VI cranial nerve palsy. Workout studies, including CT and CTA, showed no signs of hemorrhage but a right verteborbasilar junction aneurysm. Consequently, a digital subtraction angiography (DSA) was performed and confirmed the presence of a right vertebrobasilar junction aneurysm (VBJA). The dome measured 7.72 × 7.68mm and the neck, 5.85mm.
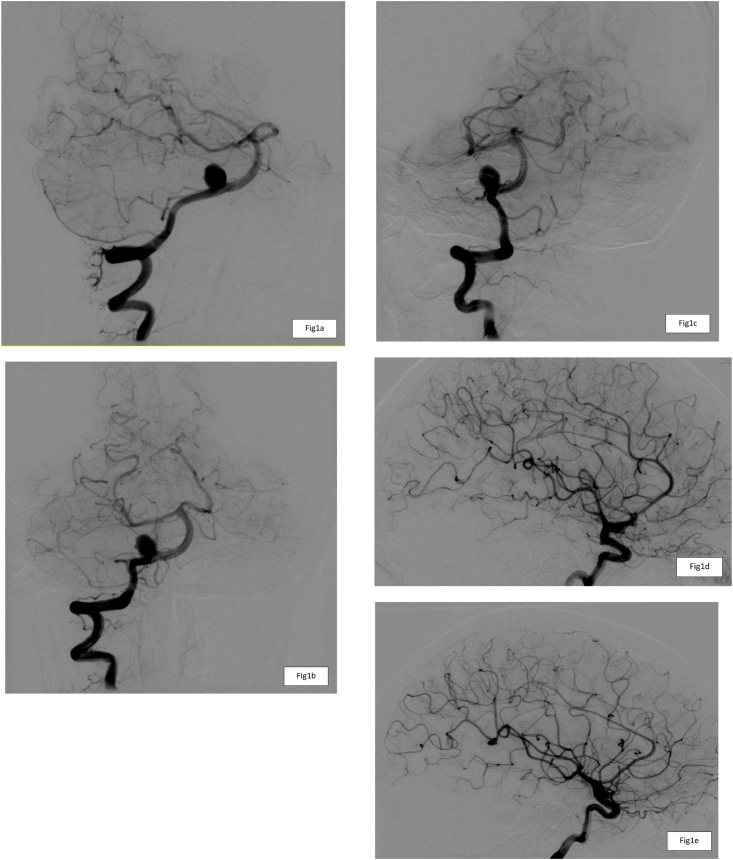
The posterior inferior cerebellar artery (PICA) had its origin just adjacent to the neck of the aneurysm (Fig. 1).
Fig. 1.
a: Anteroposterior, b: lateral and c: oblique projections of the preoperative DSA depicting a right vertebrobasilar junction aneurysm. d: Right internal carotid artery and e: left internal carotid artery, both showing little opacification of Posterior Communicating Arteries.
The patient was selected for microsurgery in the hybrid operation room. The aim was to use an endovascular balloon catheter for proximal temporal occlusion and retrograde aspiration as an adjuvant technique for neck clipping.
The patient underwent general anesthesia with propofol. No gases could be used as they interfere with intraoperative neurophysiologic monitoring (IONM). The IONM electrodes were placed. With the patient in the supine position, the anesthesiologist catheterized the radial artery while the neurosurgeon introduced a 6-French sheath into the femoral artery. The sheath was continuously perfused with heparinized saline (2000UI/L).
Patient head was fixed with a radiolucent Mayfield clamp (Mayfield Skull Clamps, Integra Lifesciences Corporation, Plainsboro Township, New Jersey, USA) in supine position with the head turned 90° to the left. We use this position for retrosigmoid approaches instead of the park bench position as we have found that is more comfortable since the shoulder of the patient does not interfere with the surgical maneuvers and surgeon position, even though it is slightly elevated with a small pillow. Moreover, we think that with this position both vision angle and angle of attack are optimal.
Then an extended retrosigmoid approach was performed. The bone over the sigmoid sinus was carefully drilled. That maneuver allowed anterior retraction of the sinus, once the dura was opened, providing an extended anterior view (Quiñones-Hinojosa et al., 2006).
With the dura opened and the sigmoid sinus anteriorly retracted, dissection of the arachnoid was started, exposing the cranial nerves (CN) VI, VII, VIII, IX, X, XI, XII, the vertebral artery (VA) and the PICA. The aneurysm was found to be originated in the vertebrobasilar junction just adjacent to the origin of the PICA. Aneurysm dissection and exposition showed the right CN VI crossing over the aneurysm dome.
Using an integrated intraoperative angiography system (Philips Azurion 7, Amsterdam, The Netherlands) a 6F Neuron catheter, helped by an intermediate multipurpose catheter, was navigated into the right vertebral artery. The aim was to navigate a Scepter balloon (Microvention Terumo Inc, Aliso Viejo, California, USA) into the right VA gaining proximal control by inflating it under direct angiographic vision. If it was deemed necessary for a safer clipping, retrograde suction through the balloon catheter to deflate the aneurysm was also planned.
The arm of the angiography system was placed in an oblique position in such a way that allowed the surgeon to work with the microscope while keeping the same angiographic view and position, thus without interfering with the endovascular maneuvers and images (Fig. 2). The purpose was to avoid further ischemia time related to engine repositioning once the balloon was inflated. This way, as soon as the balloon was inflated, we could rapidly start to work on the aneurysm at the surgical site.
Fig. 2.
a, b, c, d, e, Picture of the hybrid operation room setting. The angiography arc must be placed in a way that the surgeon is able to perform the aneurysm clipping. During intraoperative control angiographic series, the surgical field is covered with sterile fluoroscopic protectors and caution must be taken in order not to collide with the Mayfield clamp.
With the Neuron catheter in place contrast injection showed a stop secondary to a severe catheter-induced vasospasm in the right VA. As a consequence of the vasospasm, we noticed under the microscope that the aneurysm was significantly deflated. It is difficult to ensure if we could have resolved the vasospasm sufficiently to place the balloon as planned, and therefore risking our surgical strategy. Thus, we decided to get profit of the situation and try to clip the aneurysm under this particular condition.
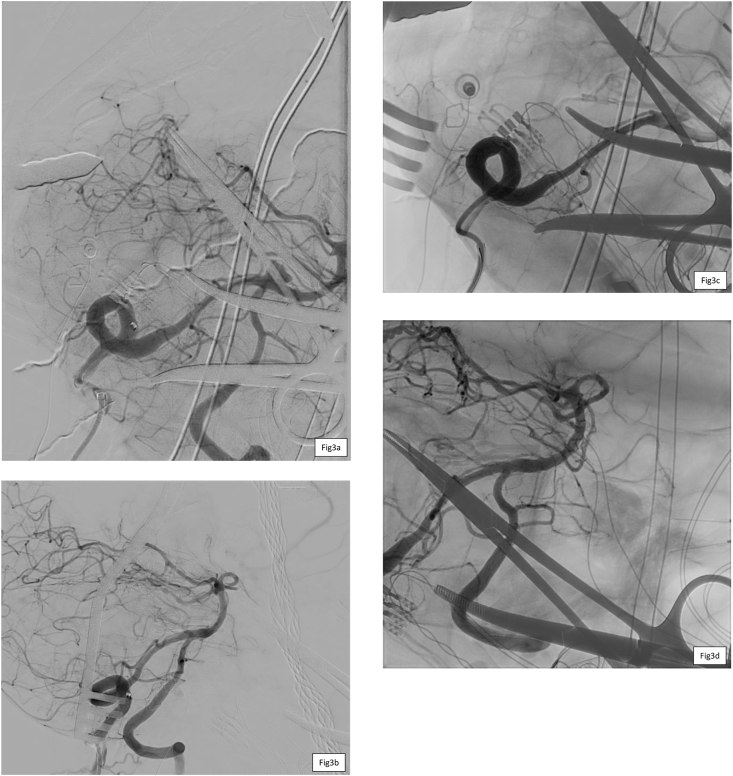
The aneurysm was then clipped using one fenestrated clip (with the VI cranial nerve passing through the fenestration) and two straight clips. The Neuron catheter was then withdrawn few centimeters and an intraoperative angiography performed, showing resolution of the vasospasm and a small neck remnant. One of the straight clips was repositioned achieving complete aneurysm obliteration (Fig. 3). Two weeks after discharge she presented with Covid-19 disease and required 15 days of hospital admission. The patient had a good recovery with VI cranial nerve palsy and mild dysphagia due to mild right vocal cord palsy, both improving at 1-month follow-up and fully recovered at 6-month follow-up.
Fig. 3.
a: intraoperative DSA showing the aneurysm deflated due to a reactive vasospasm at the Vertebral Artery; b: intraoperative DSA after 2 clips were placed showing a small remnant of aneurismal sac; c: intraoperative DSA after the third clip was placed showing complete exclusion of the aneurysm, and vertebral artery vasospasm solved; d: intraoperative angiography showing complete exclusion of the aneurysm without subtraction so the clips can be seen.
3. Discussion
Since Batjer first described the “Dallas technique” (Batjer and Samson, 1990), some authors have reported their experience in combining endovascular procedures as an adjuvant technique for aneurysm clipping. In most of these papers, the catheter is either introduced in the angiosuite and then the patient transferred to the operation room or introduced in the operation room but using fluoroscopy, thus obtaining a worse image quality (Skrap et al., 2010; Chen et al., 2011; Ng et al., 2000; Flores et al., 2019).
With the recent improvement of technology, some neurosurgery departments have advocated for the implementation of new operation rooms that incorporate high image quality angiography systems. This endows the neurosurgeon with a great variety of options that helps in dealing with the management of vascular lesions.
3.1. Angiographic assessment and clip reposition
In the case exposed the clips had to be replaced because the intraoperative angiography showed a neck remnant. It is known that DSA is the gold standard to assess aneurysm complete exclusion with the added advantage of evaluation of proximal and distal arterial branches flow and permeability (Riva et al., 2018). We have routinely used indocianine green fluorescence (ICG) video-angiography under the microscope in many aneurysm cases. ICG video-angiography allows a rapid assessment of possible neck remnant and potential need for clip reposition. We usually use it before the definitive intraoperative DSA is performed as the latter requires selective catheterization and is more time consuming. In this case due to the desired position achieved with the microscope and the angiography system we did not perform ICG video-angiography and direct DSA assessment was obtained without wasting time. Intraoperative angiography offers the possibility to reposition a misplaced clip in the same surgery. It is important because in some cases, relying solely on video angiography could lead to overestimate the quality of clipping.
3.2. Proximal balloon occlusion and retrograde suction
Having a proximal control in that case without intraoperative DSA would have required placing a clip in the VA proximal to the aneurysm. Working between the narrow corridors that offer the lower cranial nerves, PICA and the anterior inferior cerebellar artery (AICA) is a challenging procedure which can be even more difficult with a proximal clip placed blocking the surgeon instruments. Furthermore, the balloon occlusion permits the retrograde suction if needed, deflating the aneurysm and making the dissection around the neck and dome easier, faster and safer.
In the reported case, we were not able to inflate the balloon neither perform retrograde suction because we identified a catheter induced vasospasm. The VA is very sensitive and prone to vasospasm. The VA catheter induced vasospasm has already been reported as a temporary and reversible and even used as an adjuvant technique to diminish the VA blood flow (Kim et al., 2016). Even though our intention was to inflate a balloon instead, the induced vasospasm produced a similar effect on the aneurysm, deflating it and the choice was made to get profit of the situation and proceed with the aneurysm clipping. However, careful navigation of the catheter must be carried out because it could have been more difficult to resolve and lead to severe complications.
4. Conclusion
The combination of endovascular procedures and microsurgery at the same hybrid operation room in that case resulted in a safe and effective technique. It is an interesting tool that could help neurosurgeons deal with certain selected cases of VBJA. Intraoperative angiography offers the possibility to reposition a misplaced clip in the same surgery. Good collaboration between interventional neuroradiologists and vascular neurosurgeons helps in achieving good results in such difficult case.
Declaration of competing interest
The authors don't have any conflict of interests to declare.
References
- Batjer H.H., Samson D.S. Retrograde suction decompression of giant paraclinoidal aneurysms. Technical note. J. Neurosurg. 1990;73(2):305–306. doi: 10.3171/jns.1990.73.2.0305. [DOI] [PubMed] [Google Scholar]
- Chen S.F., Kato Y., Subramanian B., Kumar A., Watabe T., Imizu S., et al. Retrograde suction decompression assisted clipping of large and giant cerebral aneurysms: our experience. Minim. Invasive Neurosurg. 2011;54(1):1–4. doi: 10.1055/s-0030-1268479. [DOI] [PubMed] [Google Scholar]
- Flores B.C., White J.A., Hunt Batjer H., Samson D.S. The 25th anniversary of the retrograde suction decompression technique (Dallas technique) for the surgical management of paraclinoid aneurysms: historical background, systematic review, and pooled analysis of the literature. J. Neurosurg. 2019;130(3):902–916. doi: 10.3171/2017.11.JNS17546. [DOI] [PubMed] [Google Scholar]
- Kim S., Kang M., Choi J.H. Thrombectomy using a stent retriever with artificially induced vertebral artery vasospasm in a patient with acute basilar artery occlusion: a case report. NeuroRadiol. J. 2016;29(1):90–92. doi: 10.1177/1971400915620438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng P.Y., Huddle D., Gunel M., Awad I.A. Intraoperative endovascular treatment as an adjunct to microsurgical clipping of paraclinoid aneurysms. J. Neurosurg. 2000;93(4):554–560. doi: 10.3171/jns.2000.93.4.0554. [DOI] [PubMed] [Google Scholar]
- Quiñones-Hinojosa A., Chang E.F., Lawton M.T. vol. 58. Neurosurgery; 2006. (The Extended Retrosigmoid Approach: an Alternative to Radical Cranial Base Approaches for Posterior Fossa Lesions). [DOI] [PubMed] [Google Scholar]
- Riva M., Amin-Hanjani S., Giussani C., DeWitte O., Bruneau M. Indocyanine green videoangiography in aneurysm surgery: systematic review and meta-Analysis. Neurosurgery. 2018;83(2):166–179. doi: 10.1093/neuros/nyx387. [DOI] [PubMed] [Google Scholar]
- Shucart W.A., Kwan E.S., Heilman C.B. Temporary balloon occlusion of a proximal vessel as an aid to clipping aneurysms of the basilar and paraclinoid internal carotid Arteries: technical note. Neurosurgery. 1990 Jul 1;27(1):116–119. doi: 10.1097/00006123-199007000-00017. https://academic.oup.com/neurosurgery/article/27/1/116/2752401 [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- Skrap M., Petralia B., Toniato G. Temporary balloon occlusion during the surgical treatment of giant paraclinoid and vertebrobasilar aneurysms. Acta Neurochir. 2010;152(3):435–442. doi: 10.1007/s00701-009-0566-0. [DOI] [PubMed] [Google Scholar]