Abstract
Introduction
Modern technologies are increasingly applied in neurosurgical resident training. To date, no data are available regarding how frequently these are used in the training of neurosurgeons, and what the perceived value of this technology is.
Research question
The aim was to benchmark the objective as well as subjective experience with modern- and conventional training technologies.
Material and methods
The EANS Young Neurosurgeons Committee designed a 12-item survey. It was distributed to neurosurgical residents and board-certified neurosurgeons between 6th of February and April 13, 2022.
Results
We considered 543 survey responses for analysis. Most participants (67%) indicated not having gained any training experience with modern technology. Most (40.7%) indicated lack of any modern or conventional training technology. Cadaver training was available to 27.6% while all modern training technology to <10%. Participants from countries with high gross domestic product per capita had more access to modern training technologies (p < 0.001). The perceived value of the different technologies was highest for hands-on OR training, followed by cadaver lab. The value of these was rated higher, compared to all modern technologies (p < 0.001).
Discussion and conclusion
Our survey reveals that cadaver labs are used more frequently than modern technologies for today's neurosurgical training. Hands-on training in the operating room (OR) was rated significantly more valuable than any conventional and modern training technology. Our data hence suggest that while modern technologies are well perceived and can surely add to the training of neurosurgeons, it remains critical to ensure sufficient OR exposure.
Keywords: EANS, Survey, Neurosurgery, Training, AR/VR, Simulation
Highlights
-
•
Survey on current use of modern technology in neurosurgical training.
-
•
Evaluation of modern and conventional training technologies.
-
•
Cadaver labs used more often than modern technologies for neurosurgical training.
-
•
It remains critical to ensure sufficient operating room exposure.
Abbreviation
- AR
augmented reality
- CI
confidence interval
- EANS
European Association of Neurosurgical Societies
- FLANC
Federación Latinoamericana de Sociedades de Neurocirugía
- GDP
Gross domestic product
- OR
operating room, odds ratio
- SD
standard deviation
- USD
US Dollar
- VR
virtual reality
- YNC
Young Neurosurgeons Committee
- YNN
Young Neurosurgeons Network
1. Introduction
Recently, modern techniques like augmented reality (AR), virtual reality (VR) and other simulator-based models, are being increasingly applied in the highly technologized field of neurosurgery. These products have found their use not only in operative planning and execution of surgery (Tabrizi and Mahvash, 2015; Hussain et al., 2020; Kockro et al., 2000; Yan et al., 2021), but also increasingly in the context of training and teaching of residents (Lohre et al., 2020; Shuhaiber, 2004; Bernardo, 2017; Zoli et al., 2022; Zoia et al., 2020). The use of new technologies in neurosurgery offers immense potential. However, financial factors on the developer side also play an essential role. As a result, the market supply of products based on these technologies is increasing without the benefits being fully understood. For surgery in general – and neurosurgery in particular – this always means examining the clinical benefit and necessity of the new technology. To date, no data are available regarding the clinical utility of these technologies, also due to their current ongoing development and validation process (Ghaednia et al., 2021; Petrone et al., 2022).
The use of new technology should have a positive influence on the current surgical workflow and ultimately on the treatment of the patient in terms of quality, efficiency, and safety. Moreover, the use of the technology should ideally help improve patient outcome. On the other hand, the use of new equipment or technology must not be a gimmick that distracts from the actual task at hand. In the regional context, the relationship between availability of resources and the resulting benefit must also be specifically considered. The market currently offers an increasing number of technologies and devices, especially intended for neurosurgical training. For example, AR and VR offer the possibility to simulate and train surgical procedures in a safe environment. These products and others such as artificial simulator-based models for the head and spine are intended to represent as real a scenario as possible. This would allow training with continuous uninterrupted availability and at a lower cost compared to conventional methods like cadaver training. Still, these training technologies are limited for neurosurgery by their restricted simulation of physical sensibility and correlation to the real scenario in the operating room (OR) (Ghaednia et al., 2021).
Currently, there is no data in the literature on how often such technologies are used in neurosurgical training. Likewise, it is unclear how valuable these technologies are considered in comparison to cadaver training or classical “hands-on training” in the OR. To answer these questions, the EANS Young Neurosurgeons Committee (YNC) initiated a 12-item survey, directed at neurosurgical residents and board-certified neurosurgeons.
2. Methods
2.1. Web-based survey and distribution
A 12-item web-based survey was designed using the SurveyMonkey platform (https://www.surveymonkey.com). Participants were asked to fill in 12 questions, of which the first questions contained demographic information of the participants. Five questions addressed the frequency and applicability of different training methods and technologies, as well as the subjective evaluation of each technology. The complete survey can be found as Supplemental Table 1. Survey results were checked for duplicates and missing data.
The survey was distributed between February 6, 2022 and April 13, 2022 via Email to all registered EANS members, as well as to registered FLANC members. Moreover, we used our personal networks to colleagues, friends, and national societies to promote the survey among the neurosurgical community.
2.2. Statistical analysis
All statistical analyses and generation of all graphs were performed using StataSE 15 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC). For the analysis as a function of gross domestic product (GDP) per capita for each country, we use the International Monetary Fund's database from April 2022 (International Monetary Fund, 2022). Descriptive statistics were employed, describing the responses as count (percent) and mean [standard deviation (SD)]. Graphical illustrations of results were used to explore relationships. We used logistic regression to analyze influence of co-variables on dichotomous questions. To compare the subjective value of different training technologies against the “gold standard” (hands-on training in the OR) and against each other, we used paired-sample t-tests. For purpose of analysis, AR/VR-based or simulation-based training methods are referred to as “modern training methods”, while cadaveric training is referred to as “conventional training method”. Results were considered significant at p-values < 0.05.
3. Results
3.1. Survey responses
The estimated number of neurosurgeons who were invited to respond to the survey were 7148. We received 556 responses (response rate = 8%), of which one was excluded for missing relevant data, and twelve were removed as duplicate. Finally, a total of 543 survey responses ere considered for analysis.
3.2. Demographics and characteristics of participants
All demographic data are summarized in Table 1. The mean age of participants was 37.5 years (SD 9.7, range: 23–76). The female (n = 121) to male (n = 421) ratio was 1:3. The majority of participants were from one of the EANS member states (n = 398, 73%). The countries with highest response rates were Mexico (n = 96, 18%), followed by Italy (n = 78, 14%), Spain (n = 60, 11%), Germany (n = 31, 6%), Romania (n = 26, 5%) and Switzerland (n = 24, 4%). Responses derived from 207 residents (38%) and 335 board-certified neurosurgeons (62%). The participant's average year of (intended) board-certification was 2017 (SD 8.4; range 1977–2031). Most participants indicated working at a university (academic) hospital (n = 384; 71%), followed by non-university hospital (n = 105; 19%) and private practice (n = 52; 10%).
Table 1.
Demographic data of n = 543 survey responders. Results are expressed as count (percent) or mean (standard deviation). ∗ Missing data in 4 participants (0.7%). ∗∗ Achieved or expected. ∗∗∗ A detailed list of participating countries is provided in the appendix, but most responses came from Mexico (n = 96, 18%), Italy (n = 78, 14%), Spain (n = 60, 11%), Germany (n = 31, 6%), Romania (n = 26, 5%) and Switzerland (n = 24, 4%).
| Age in years∗ | 37.5 (9.7) |
|---|---|
| Sex | |
| Female | 121 (22.3%) |
| Male | 421 (77.6%) |
| Missing | 1 (0.2%) |
| Year of board-certification∗∗ | |
| 1977–1999 | 27 (5.0%) |
| 2000–2004 | 19 (3.5%) |
| 2005–2009 | 27 (5.0%) |
| 2010–2014 | 68 (12.5%) |
| 2015–2019 | 109 (20.1%) |
| 2020–2024 | 198 (36.5%) |
| >2025 | 75 (13.8%) |
| Missing | 20 (3.7%) |
| Continent∗∗∗ | |
| Europe | 398 (73.3%) |
| North America | 5 (0.9%) |
| Latin America | 120 (22.1%) |
| Asia | 11 (2.0%) |
| Africa | 6 (1.1%) |
| Missing | 3 (0.6%) |
| Position | |
| Resident in neurosurgery | 207 (28.1%) |
| Board-certified neurosurgeon | 335 (61.7%) |
| Missing | 1 (0.2%) |
| Type of hospital | |
| University hospital | 384 (70.7%) |
| Non-university public hospital | 105 (19.3%) |
| Private hospital | 52 (9.6%) |
| Missing | 2 (0.4%) |
| Total: | N=543 (100%) |
3.3. Current application of modern training technologies
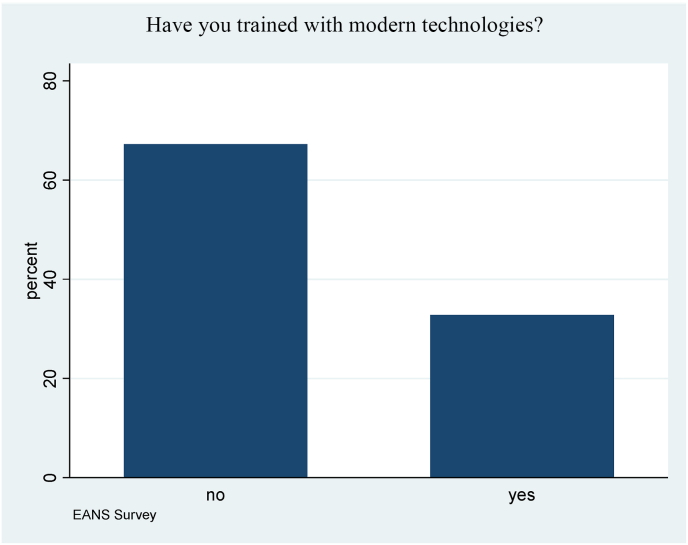
Fig. 1 illustrates that the majority (n = 365, 67%) of survey participants indicated not having gained any training experience with modern technology, such as AR, VR or surgical simulators. The rates of participants that were trained using modern training technologies were 30% for the categories of board-certification between 1977 and 1999, 42% between 2000 and 2004, 30% between 2005 and 2009, 26% between 2010 and 2014, 35% between 2015 and 2019, 37% between 2020 and 2024 and 25% > 2025. Neither the participant's age (OR 0.99, 95% CI 0.97–1.01, p = 0.26) nor the year of (intended) board-certification (OR 0.99, 95% CI 0.89–1.11, p = 0.970) were significantly associated with an affirmative answer to this question.
Fig. 1.
Shows a bar chart with the answers to the question whether the participants have already trained with modern technologies such as virtual reality, augmented reality or simulators. Of all respondents (n = 543), 33% answered “yes” to this question, 67% answered “no”.
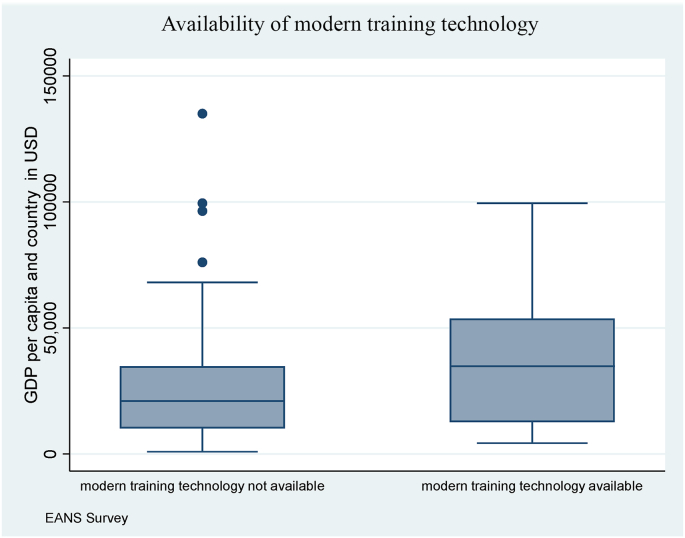
The relationship of the availability of modern training technologies and the GDP per capita available in each country was evaluated using paired t-test. Fig. 2 shows a mean GDP of 43371 USD (SD 31555) for the availability of advanced training technologies. Without the availability of modern technologies, the mean GDP was 28700 USD (SD 24237; p < 0.001). Of note, higher GDP per capita was also significantly correlated to the availability of cadaver training (p < 0.05).
Fig. 2.
Box plots represent the evaluation of the relationship between the availability of modern training technologies in each hospital and GDP per capita for each country. Paired t-test analysis revealed a highly significant (p < 0.001) association of high GDP per capita as a positive predictor of the availability of advanced training modalities. The figures display the median with 25th and 75th percentile (box) of GDP per capita of countries, the upper and lower adjacent values (whiskers) and outliners (dots). T (538) = -5.40, p < 0.001; n = 540.
Table 2 contains the available in-house training technologies. N = 221 (40.7%) participants indicated having no training technologies, n = 150 (27.6%) cadaver training, and less than 10 or 5% any modern type of training technology.
Table 2.
Responses to the question, which techniques are offered in-house for training (multiple responses were possible). Results are presented as count (percent). ∗ A detailed list of other training modalities is provided in the appendix.
| None | 221 (40.7%) |
| Augmented or virtual reality (AR/VR; e.g., Surgical Theater, HoloLens, etc.) | 54 (9.9%) |
| Virtual reality (VR)-based simulators (e.g., Dextroscope, Neurotouch, etc.) | 26 (4.8%) |
| Spinal model-based simulators (e.g., Realspine, etc.) | 41 (7.6%) |
| Cranial model-based simulators (e.g., Brainbox, etc.) | 53 (9.8%) |
| Cadaver training | 150 (27.6%) |
| Others∗ | 32 (5.9%) |
| Total: | N=543 (100%) |
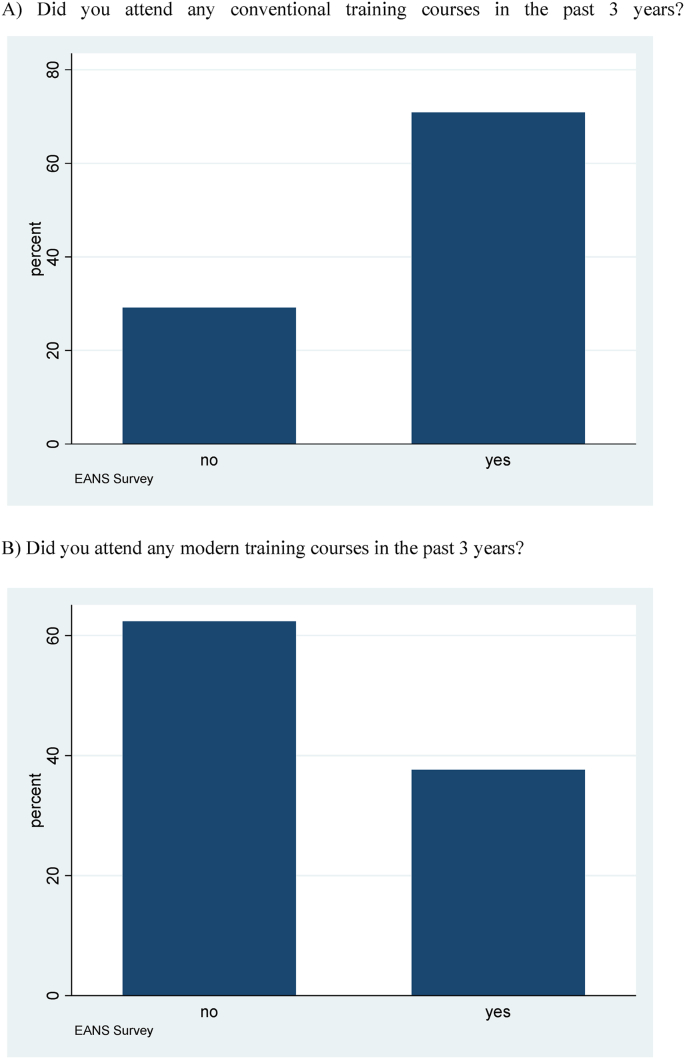
Fig. 3A and B depict the rate of participation in training courses within the last three years, either as trainee or faculty. Note that most (71%, n = 384) reported having attended a training course using “conventional methods”, while the minority (38%, n = 204) attended courses using “modern training technologies”.
Fig. 3.
A: Bar graphs, illustrating that 71% (n = 384/543) of the survey respondents have participated in a training course using conventional training methods (such as cadaver training) within the last three years, either as participants or faculty. Fig. 2B: However, only the minority (n = 204, 38%) participated in a training course that employed modern training methods (such as VR/AR-based or simulator-based models). There was one respondent with missing data for both questions. VR: virtual reality; AR: augmented reality.
3.4. Subjective evaluation of modern training technologies
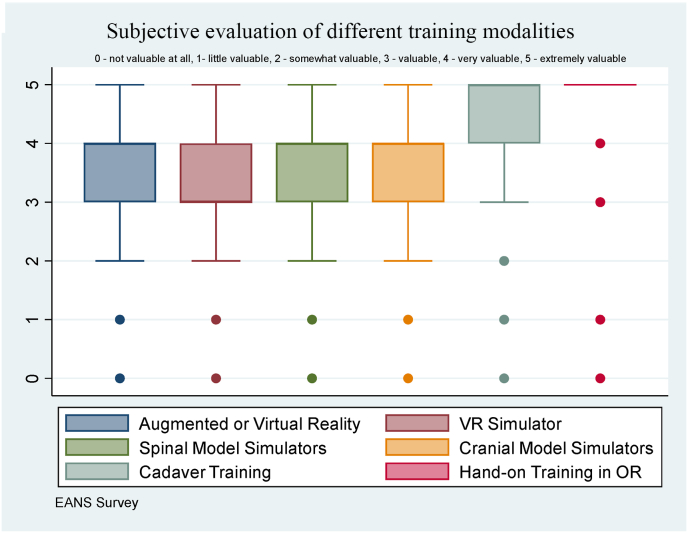
On a scale from 0 - not valuable at all, 1 - little valuable, 2 - somewhat valuable, 3 - valuable, 4 - very valuable, to 5 - extremely valuable, participants considered “hands-on” training in the operation room (OR) as most valuable (mean 4.74, SD 0.66), followed by cadaver training (mean 4.47, SD 0.84), cranial model simulator (mean 3.59, SD 1.11), spinal model simulator (mean 3.68, SD 1.14), AR and VR (mean 3.51, SD 1.08), and VR simulator (mean 3.40, SD 1.12) (Fig. 4). Compared to the “gold standard” hands-on training in the OR, all training technologies scored lower (p < 0.001). There were also highly significant differences, when comparing each of the modern training technologies to the conventional cadaver training (p < 0.001).
Fig. 4.
Box plots containing the subjective evaluation of the different training modalities (Augmented or Virtual Reality, VR Simulator, Spine Model Simulators, Cranial Model Simulators, Cadaver Training, Hands-on Training in OR). The rating is ordinally distributed (from 0 - not valuable at all, 1 - little valuable, 2 - somewhat valuable, 3 - valuable, 4 - very valuable, to 5 - extremely valuable). Respondents rated “hands-on” OR training highest compared to all other modalities (p < 0.001), and cadaver training scored higher than all other modern training modalities (p < 0.001; paired t-tests). The figures display the median with the 25th–75th percentile (box), the upper and lower adjacent values (whiskers) and outliers (dots).
4. Discussion
New technologies in the field of VR and AR as well as simulator-based models are becoming increasingly used in surgery, not only for surgical planning and execution but also for training and education (Bernardo, 2017; Rehder et al., 2016; Cannizzaro et al., 2022). This survey maps the current use of modern training technologies in neurosurgery with comparison to conventional training technologies. Strikingly, our survey reveals that no in-house training opportunities are available at all in about 41% of survey participants. Secondly, the use of conventional training technologies such as cadaver training still seems to dominate for both in-house training and training at courses. Third, participants consider “hands-on” training in the OR as considerably more valuable than any other type of conventional or modern training technology – and the modern training technologies are evaluated less favorably, compared to conventional cadaver training.
We were surprised to see that the expected steep increase in use of modern training technologies among younger (vs. older) colleagues or those with recent & future board-certification was not evident from our data. Besides the progressive development of new training technology, there is some literature supporting the notion that due to several factors – among them working time restrictions and distribution of departmental caseload across more trainees in the past decade (Stienen et al., 2016a, 2016b) - trainees’ exposure to live surgery decreases, while the use of modern training technologies increases in parallel (Stienen et al., 2020). This development is likely to result in less well-trained future surgeons, with the development and implementation of modern technology in neurosurgical training supported to compensate or at least attenuate this effect (Stienen et al., 2016c). Considering the overall low use of, and hence limited experience with these – partially very advanced and sophisticated technologies – in neurosurgery today, maybe the true value was not well visible from our data. It would have required an even larger survey sample, including more responses from higher income countries with the available financial resources to afford these modern training technologies, to truly estimate their value in training.
Modern training technology is usually integrated in training courses first, where trainees and faculty alike can gain experience with the technology and appreciate its value, before eventually considering purchasing for in-house training at their own department. According to our survey, almost 40% have gained experiences with modern training technology over the past 3 years, a rate which is still 30% lower when compared to conventional cadaver training. To date, comprehensive data on the frequency of use of modern technologies in surgical training are not available, which also applies to other surgical disciplines. In literature, especially concerning orthopedics and general surgery, the focus is on the evaluation of safety and quality as well as the benefit of different training technologies (Chen et al., 2020; Bresler et al., 2020; Passman et al., 2007; Huri et al., 2021; Vaughan et al., 2016; Mabrey et al., 2010; Müller and Bockholt, 1998; Skertich et al., 2021; Verhey et al., 2020; Sankaranarayanan et al., 2021). According to the data from our survey, modern training technology still seems to be used much less compared to conventional training methods. Nevertheless, our data do not give us the possibility of comparison to other surgical specialties and hence make generalization difficult. The fact that most modern training technologies are relatively new, while in a rapidly progressing developmental process and sometimes even more expensive than dedicated cadaver preparations, possibly accounting for their currently low frequency of use. For the international comparison, especially between countries with high and low financial resources, we tested the correlation of GDP per capita of the respective countries with the availability of modern training methods. A high GDP was found to be a positive predictor for the availability of modern training technologies. This result is not surprising if we consider the high initial costs of the modern training technologies. In contrast, whether the respondent had participated in a course with modern training technologies in the last 3 years or had been trained with modern training technology did not demonstrate any statistical association to the GDP. On the other hand, there was also a significant association (p < 0.05) between the GDP per capita and the availability of cadaver training in the respective hospitals. Even though the relationship between the GDP per capita and availability of cadaver training was less impressive than with the modern training technologies, the effect of a country's financial resources on the ability to train residents outside the OR is evident. However, the frequency of use does not answer whether a training technology is relevant or not.
Therefore, we designed the next part of the survey to be a subjective evaluation of the respective training methods. Unsurprisingly, practical training on a patient in the OR was indicated as the most valuable method, and a large body of pro- and retrospective data supports that “hands-on” neurosurgical training for many basic and advanced procedures is safe (Stienen et al., 2014, 2015; Joswig et al., 2016a, 2016b, 2017a, 2017b; Maldaner et al., 2018; Vasella et al., 2019; Ebner et al., 2010). Coming closest to the goal of the “real OR scenario” and most authentic training situation influences the perceived value of a training method. On average, the conventional training method “cadaver lab” received the second highest rating. Differences between the gold-standard (training in the OR) and all other training methods were highly statistically significant (p < 0.001). Interestingly, respondents also considered the conventional cadaver lab training as superior to all modern training technologies. An objective and comparable evaluation of the different training technologies in terms of performance and gain of surgical skill is still pending. Despite the subordinate average evaluation compared to the gold-standard, individual consideration of the modern training technologies indicated high degrees of value for many respondents. Considering the technology-related limitations, specific advantages of the respective techniques also become apparent. Despite the mediocre ratings in this survey, modern training technologies will surely be important components of future neurosurgical training.
4.1. Strengths and limitations
This survey provides the first figures on the frequency of use of various modern and conventional training technologies. The data can serve as a reference for further studies and questions in this context. Furthermore, the survey gives a first impression of the subjective evaluation of the different training technologies, which can be compared to the gold standard of training in the OR. The results are relevant for the industry, for residency program directors and those involved in health politics.
The limitations of this work relate mainly to the nature of data collection. In this type of survey, voluntary, non-incentivized participation and subjective evaluation lead to bias. Furthermore, a low survey response rate in general and relatively low participation from high GDP countries leads to methodologically limited assessability and bias in the results. The low response rate from North America, Asia and Africa also complicates the analysis in an international comparison and does not allow generalization to these regions.
5. Conclusions
This EANS Young Neurosurgeons survey reveals that cadaver labs are still used more frequently than AR/VR or other surgical simulators available for neurosurgical training. Hands-on training in the OR was rated significantly more valuable than any conventional or any modern training technology. Our data suggests that while different training technologies are well perceived and can surely add to the training of neurosurgeons, for neurosurgeons and residents alike, it remains critical to ensure sufficient OR exposure.
Authors’ contributions
Each author made substantial contributions to this article. Conception and design: all authors. Acquisition of data: all authors. Statistical analysis: Stengel and Stienen. Analysis and interpretation of data: Stengel and Stienen. Drafting the article: Stengel and Stienen. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript: all authors. Administrative/technical/material support: all authors. Study supervision: Stienen.
Funding
No funding was received for this research. No financial support was received for this study.
Disclosures
The authors declare that they have no competing interests.
Acknowledgements
The authors sincerely thank all collaborators of the study for participation in the survey.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bas.2022.100929.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Bernardo A. Virtual reality and simulation in neurosurgical training. World Neurosurg. 2017 Oct;106:1015–1029. doi: 10.1016/j.wneu.2017.06.140. [DOI] [PubMed] [Google Scholar]
- Bresler L., Perez M., Hubert J., Henry J.P., Perrenot C. Residency training in robotic surgery: the role of simulation. J. Vis. Surg. 2020 Jun;157(3 Suppl. 2):S123–S129. doi: 10.1016/j.jviscsurg.2020.03.006. [DOI] [PubMed] [Google Scholar]
- Cannizzaro D., Zaed I., Safa A., Jelmoni A.J.M., Composto A., Bisoglio A., et al. Augmented reality in neurosurgery, state of art and future projections. A systematic review. Front. Surg. 2022;9 doi: 10.3389/fsurg.2022.864792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Rodrigues Armijo P., Krause C., SAGES Robotic Task Force. Siu K.-C., Oleynikov D. A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg. Endosc. 2020 Jan;34(1):361–367. doi: 10.1007/s00464-019-06775-1. [DOI] [PubMed] [Google Scholar]
- Ebner F.H., Dimostheni A., Tatagiba M.S., Roser F. Step-by-step education of the retrosigmoid approach leads to low approach-related morbidity through young residents. Acta Neurochir. 2010 Jun;152(6):985–988. doi: 10.1007/s00701-010-0611-z. discussion 988. [DOI] [PubMed] [Google Scholar]
- Ghaednia H., Fourman M.S., Lans A., Detels K., Dijkstra H., Lloyd S., et al. Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J. 2021 Oct;21(10):1617–1625. doi: 10.1016/j.spinee.2021.03.018. [DOI] [PubMed] [Google Scholar]
- Huri G., Gülşen M.R., Karmış E.B., Karagüven D. Cadaver versus simulator based arthroscopic training in shoulder surgery. Turk. J. Med. Sci. 2021 Jun;51(3):1179–1190. doi: 10.3906/sag-2011-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain R., Lalande A., Guigou C., Bozorg-Grayeli A. Contribution of augmented reality to minimally invasive computer-assisted cranial base surgery. IEEE J. Biomed. Health Inf. 2020 Jul;24(7):2093–2106. doi: 10.1109/JBHI.2019.2954003. [DOI] [PubMed] [Google Scholar]
- International Monetary Fund . April 2022. World Economic Outlook Database.https://www.imf.org/en/Publications/WEO/weo-database/2022/April/weo-report?c=512,914,612,171,614,311,213,911,314,193,122,912,313,419,513,316,913,124,339,638,514,218,963,616,223,516,918,748,618,624,522,622,156,626,628,228,924,233,632,636,634,238,662,960,423,935,128,611,321,243,248,469,253,642,643,939,734,644,819,172,132,646,648,915,134,652,174,328,258,656,654,336,263,268,532,944,176,534,536,429,433,178,436,136,343,158,439,916,664,826,542,967,443,917,544,941,446,666,668,672,946,137,546,674,676,548,556,678,181,867,682,684,273,868,921,948,943,686,688,518,728,836,558,138,196,278,692,694,962,142,449,564,565,283,853,288,293,566,964,182,359,453,968,922,714,862,135,716,456,722,942,718,724,576,936,961,813,726,199,733,184,524,361,362,364,732,366,144,146,463,528,923,738,578,537,742,866,369,744,186,925,869,746,926,466,112,111,298,927,846,299,582,487,474,754,698,&s=PPPPC,&sy=2022&ey=2022&ssm=0&scsm=1&scc=0&ssd=1&ssc=0&sic=0&sort=country&ds=.&br=1 [Internet]. [cited 2022 May 26]. Available from: [Google Scholar]
- Joswig H., Hock C., Hildebrandt G., Schaller K., Stienen M.N. Microscopic lumbar spinal stenosis decompression: is surgical education safe? Acta Neurochir. 2016 Feb;158(2):357–366. doi: 10.1007/s00701-015-2667-2. [DOI] [PubMed] [Google Scholar]
- Joswig H., Gautschi O.P., El Rahal A., Sveikata L., Bartoli A., Hildebrandt G., et al. Cranioplasty: is surgical education safe? World Neurosurg. 2016 Jul;91:81–88. doi: 10.1016/j.wneu.2016.03.081. [DOI] [PubMed] [Google Scholar]
- Joswig H., Jucker D., Lavalley A., Sprenger L., Gautschi O.P., Hildebrandt G., et al. Shunts: is surgical education safe? World Neurosurg. 2017 Jun;102:117–122. doi: 10.1016/j.wneu.2017.02.128. [DOI] [PubMed] [Google Scholar]
- Joswig H., Haile S.R., Hildebrandt G., Stienen M.N. Residents' learning curve of lumbar transforaminal epidural steroid injections. J. Neurol. Surg. Cent. Eur. Neurosurg. 2017 Sep;78(5):460–466. doi: 10.1055/s-0037-1599056. [DOI] [PubMed] [Google Scholar]
- Kockro R.A., Serra L., Tseng-Tsai Y., Chan C., Yih-Yian S., Gim-Guan C., et al. Planning and simulation of neurosurgery in a virtual reality environment. Neurosurgery. 2000 Jan;46(1):118–135. ; discussion 135-137. [PubMed] [Google Scholar]
- Lohre R., Warner J.J.P., Athwal G.S., Goel D.P. The evolution of virtual reality in shoulder and elbow surgery. JSES INTL. 2020 Jun;4(2):215–223. doi: 10.1016/j.jseint.2020.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabrey J.D., Reinig K.D., Cannon W.D. Virtual reality in orthopaedics: is it a reality? Clin. Orthop. Relat. Res. 2010 Oct;468(10):2586–2591. doi: 10.1007/s11999-010-1426-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldaner N., Sosnova M., Sarnthein J., Bozinov O., Regli L., Stienen M.N. Burr hole trepanation for chronic subdural hematomas: is surgical education safe? Acta Neurochir. 2018 May;160(5):901–911. doi: 10.1007/s00701-017-3458-8. [DOI] [PubMed] [Google Scholar]
- Müller W., Bockholt U. The virtual reality arthroscopy training simulator. Stud. Health Technol. Inf. 1998;50:13–19. [PubMed] [Google Scholar]
- Passman M.A., Fleser P.S., Dattilo J.B., Guzman R.J., Naslund T.C. Should simulator-based endovascular training be integrated into general surgery residency programs? Am. J. Surg. 2007 Aug;194(2):212–219. doi: 10.1016/j.amjsurg.2006.11.029. [DOI] [PubMed] [Google Scholar]
- Petrone S., Cofano F., Nicolosi F., Spena G., Moschino M., Di Perna G., et al. Virtual-augmented reality and life-like neurosurgical simulator for training: first evaluation of a hands-on experience for residents. Front. Surg. 2022 May;9 doi: 10.3389/fsurg.2022.862948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehder R., Abd-El-Barr M., Hooten K., Weinstock P., Madsen J.R., Cohen A.R. The role of simulation in neurosurgery. Childs Nerv. Syst. 2016 Jan;32(1):43–54. doi: 10.1007/s00381-015-2923-z. [DOI] [PubMed] [Google Scholar]
- Sankaranarayanan G., Parker L., De S., Kapadia M., Fichera A. Simulation for colorectal surgery. J. Laparoendosc. Adv. Surg. Tech. 2021 May;31(5):566–569. doi: 10.1089/lap.2021.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuhaiber J.H. Augmented reality in surgery. Arch. Surg. 2004 Feb;139(2):170–174. doi: 10.1001/archsurg.139.2.170. [DOI] [PubMed] [Google Scholar]
- Skertich N.J., Schimpke S.W., Lee T., Wiegmann A.L., Pillai S., Rossini C., et al. Pediatric surgery simulation-based training for the general surgery resident. J. Surg. Res. 2021 Feb;258:339–344. doi: 10.1016/j.jss.2020.05.038. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Smoll N.R., Hildebrandt G., Schaller K., Gautschi O.P. Early surgical education of residents is safe for microscopic lumbar disc surgery. Acta Neurochir. 2014 Jun;156(6):1205–1214. doi: 10.1007/s00701-014-2070-4. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Joswig H., Jucker D., Hildebrandt G., Schaller K., Gautschi O.P. Anterior cervical discectomy and fusion: is surgical education safe? Acta Neurochir. 2015 Sep;157(8):1395–1404. doi: 10.1007/s00701-015-2396-6. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Netuka D., Demetriades A.K., Ringel F., Gautschi O.P., Gempt J., et al. Working time of neurosurgical residents in Europe--results of a multinational survey. Acta Neurochir. 2016 Jan;158(1):17–25. doi: 10.1007/s00701-015-2633-z. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Netuka D., Demetriades A.K., Ringel F., Gautschi O.P., Gempt J., et al. Neurosurgical resident education in Europe--results of a multinational survey. Acta Neurochir. 2016 Jan;158(1):3–15. doi: 10.1007/s00701-015-2632-0. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Netuka D., Demetriades A.K., Ringel F., Gautschi O.P., Gempt J., et al. Residency program trainee-satisfaction correlate with results of the European board examination in neurosurgery. Acta Neurochir. 2016 Oct;158(10):1823–1830. doi: 10.1007/s00701-016-2917-y. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Freyschlag C.F., Schaller K., Meling T., EANS Young Neurosurgeons and EANS Training Committee Procedures performed during neurosurgery residency in Europe. Acta Neurochir. 2020 Oct;162(10):2303–2311. doi: 10.1007/s00701-020-04513-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabrizi L.B., Mahvash M. Augmented reality–guided neurosurgery: accuracy and intraoperative application of an image projection technique. J. Neurosurg. 2015 Jul;123(1):206–211. doi: 10.3171/2014.9.JNS141001. [DOI] [PubMed] [Google Scholar]
- Vasella F., Velz J., Neidert M.C., Henzi S., Sarnthein J., Krayenbühl N., et al. Safety of resident training in the microsurgical resection of intracranial tumors: data from a prospective registry of complications and outcome. Sci. Rep. 2019 Jan;9(1):954. doi: 10.1038/s41598-018-37533-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan N., Dubey V.N., Wainwright T.W., Middleton R.G. A review of virtual reality based training simulators for orthopaedic surgery. Med. Eng. Phys. 2016 Feb;38(2):59–71. doi: 10.1016/j.medengphy.2015.11.021. [DOI] [PubMed] [Google Scholar]
- Verhey J.T., Haglin J.M., Verhey E.M., Hartigan D.E. Virtual, augmented, and mixed reality applications in orthopedic surgery. Int. J. Med. Robot. 2020 Apr;16(2) doi: 10.1002/rcs.2067. [DOI] [PubMed] [Google Scholar]
- Yan C., Wu T., Huang K., He J., Liu H., Hong Y., et al. The application of virtual reality in cervical spinal surgery: a review. World Neurosurg. 2021 Jan;145:108–113. doi: 10.1016/j.wneu.2020.09.040. [DOI] [PubMed] [Google Scholar]
- Zoia C., Raffa G., Somma T., Della Pepa G.M., La Rocca G., Zoli M., et al. COVID-19 and neurosurgical training and education: an Italian perspective. Acta Neurochir. 2020 Aug;162(8):1789–1794. doi: 10.1007/s00701-020-04460-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoli M., Bongetta D., Raffa G., Somma T., Zoia C., Della Pepa G.M. Young neurosurgeons and technology: survey of young neurosurgeons section of Italian society of neurosurgery (società italiana di Neurochirurgia, SINch) World Neurosurg. 2022 Mar;(22) doi: 10.1016/j.wneu.2022.03.022. S1878-8750. 00303-00305. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.