Highlights
-
•
Preservation of LSAs is extremely important during resections of insular gliomas.
-
•
Navigated 3D-US power Doppler may enable intraoperative visualization of LSAs.
-
•
Quality of ultrasound scanner is important when LSAs should be visualized.
-
•
Reliability of LSAs depiction by 3D-US power Doppler is still investigated.
Keywords: Lenticulostriate arteries, Insula, Glioma, 3D-ultrasound, Power Doppler
Dear Editors,
We read with great interest the paper written by Bykanov et al. describing the sensitivity of three-dimensional (3D) time-of-flight (TOF) 3.0 T magnetic resonance angiography in visualizing the number and course of lenticulostriate arteries (LSAs) in patients with insular gliomas (Bykanov et al., 2021). We congratulate the authors for their important study. We agree that resection of insular gliomas is still challenging, predominantly due to the risk of iatrogenic injury to LSAs. Their finding, elucidating the informative value of preoperative 3D TOF angiography, may certainly help during surgical strategy planning.
However, we would like to comment on the authors' discussion concerning the possibility of intraoperative visualization of LSAs using ultrasound. Referring to our previous work (Šteňo et al., 2016), the authors describe their negative experience which is opposite to our finding that navigated 3D-ultrasound (3DUS) power Doppler mode may enable intraoperative visualization of LSAs. Additionally, Bykanov et al. stated that it is difficult to detect the intraparenchymatous segment of the LSAs 0.5–0.1 mm in diameter in the surgical wound during the final stages of tumor resection.
While we agree with the authors that the intraoperative identification of LSAs using ultrasound is non-trivial, we think that the method we presented is promising, and at least in some cases may help to prevent injury of LSAs during removal of insular gliomas. Of note, another ultrasound-based method of LSAs identification using audio signal of intraoperative micro-Doppler recordings has been reported by Yaşargil et al. (Yaşargil et al., 2002) years before we published the paper describing direct LSAs visualization by navigated 3D-US power Doppler mode.
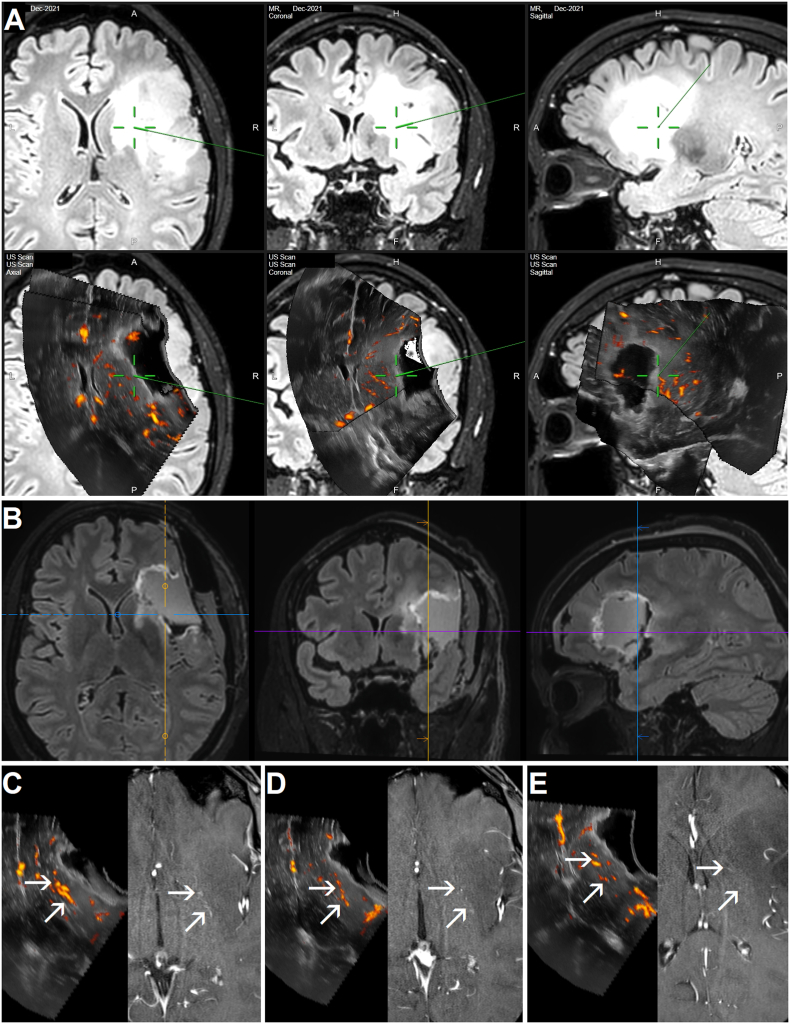
The quality of LSAs ultrasound imaging is currently being evaluated at our department in a prospective study. Hence, we would like to shortly present our last included patient operated in December 2021. As seen in Fig. 1, LSAs were clearly depicted, and not only before the resection, but also toward its end, when a relatively large resection cavity was present.
Fig. 1.
Visualization of LSAs during right-sided insular glioma resection using 3D-US power Doppler mode. A: Intraoperative neuronavigation screenshot. Upper row: Preoperative 3D Fluid attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) sequence showing a large, right-sided infiltrative fronto-insular grade II glioma. Lower row: 3D-US image scanned after some resection, rendered in axial, coronal and sagittal planes and fused with the preoperative navigation FLAIR MRI sequence; the ultrasound image consists of two stacked ultrasound scans, the power Doppler scan is superficial. The LSAs visualized by 3D-US power Doppler are localized a few millimeters under the resection cavity bottom, which is touched by the tip of the pointer (end of the green line – center of the green cross) in order to evaluate the distance to the nearest perforator. B: Postoperative 3D FLAIR MRI sequence performed 24 hours after the surgery showing a subtotal resection. Note residual tumor infiltration in the anterior limb of the internal capsule, also in the area of presumed fronto-striatal tract location, and a thin layer lateral to the striatum (close to LSAs, which are not visible on the FLAIR sequence). C – E: Intraoperative 3D-US power-Doppler images rendered in axial planes (left) and corresponding preoperative contrast-enhanced 3 T 3D TOF MRI sequence (right). Note the intraparenchymatous segments of LSAs (arrows) are visualized by both modalities: at the level just above their origin from M1 segment of middle cerebral artery (C), at the level of the insular apex (D), and at the level of the upper part of the superior periinsular sulcus (E). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
We hypothesize several reasons why Bykanov et al. have not been successful in ultrasound visualization of LSAs.
First, the quality of ultrasound scanner is not negligible when delicate structures, such as submillimeter LSAs, should be visualized. The ultrasound system the authors used during their study was introduced almost 15 years ago; more sensitive ultrasound scanners providing higher image quality are currently available. Notably, one of the main reasons why we cancelled our first prospective study on 3D-US power Doppler visualization of LSAs in 2016 was the fact that the navigated 3D-US system we had at that time (SonoWand Invite, SONOWAND AS, Trondheim, Norway) was equipped with an out-of-date ultrasound scanner. A new study on the same topics has been started at our department in 2021, after we obtained a high-end 3D-US system (ultrasound bk5000, BK Medical Aps, Herlev, Denmark integrated with neuronavigation Curve, Brainlab AG, Munich, Germany), better at depicting vascular structures (Šteňo et al., 2021).
Second, Bykanov et al. most likely did not use 3D-US during their study; to the best of our knowledge, the combination of neuronavigation and ultrasound system used by the authors does not enable 3D rendering of ultrasound images. However, ultrasound imaging in standard axial, coronal and sagittal planes rendered by 3D-US systems makes anatomical identification of various structures much less challenging compared to 2D ultrasound; recognition of LSAs is most probably not an exemption.
Lasty, the authors did not clarify which Doppler mode (color or power Doppler) they have negative experience with (Bykanov et al., 2021; Pitskhelauri and Bykanov, 2021). The methodology we presented is based on power Doppler mode (Šteňo et al., 2016), which is more sensitive for depicting flow in small vessels than the standard color Doppler (McDicken and Anderson, 2002).
Identification of LSAs using 3D-US power Doppler certainly has some limitations, which we will report after finalizing our ongoing prospective study. Because the reliability of LSAs depiction by 3D-US is yet uncertain, surgeons must still adhere to all standard precautions in order to prevent injury to LSAs. On the other hand, none of these techniques was proven to be fully reliable, especially when insular tumors incorporate LSAs. This is true also for the authors' previous findings, that the resection of medial tumor portion should stop when beige-colored putamen or lenticulostriate veins (referred also as inferior striate veins, Rhoton, 2002) were detected (Pitskhelauri and Bykanov, 2021). The importance of both aforementioned anatomical landmarks was reported before (Yaşargil et al., 2002), nevertheless, while undoubtedly helpful, anatomical landmarks are often insufficient for the exact location of the perforating arteries on their whole trajectory (Duffau, 2009).
In conclusion, in our opinion neurosurgeons should be aware that navigated 3D-US power Doppler may enable direct LSAs visualization, which may serve as a warning sign at least in some insular glioma cases.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the presented patient.
Availability of data and material (data transparency)
The datasets generated during and/or analyzed during the presented case are available from the corresponding author on reasonable request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
References
- Bykanov A.E., Pitskhelauri D.I., Batalov A.I., Young R., Trube M.A., Holodny A.I., Pronin I.N., Zagidullin T. Sensitivity of three-dimensional time-of-flight 3.0 T magnetic resonance angiography in visualizing the number and course of lenticulostriate arteries in patients with insular gliomas. Brain Spine. 2021;(2) doi: 10.1016/j.bas.2021.100856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffau H. A personal consecutive series of surgically treated 51 cases of insular WHO Grade II glioma: advances and limitations. J. Neurosurg. 2009;110:696–708. doi: 10.3171/2008.8.JNS08741. [DOI] [PubMed] [Google Scholar]
- McDicken W.N., Anderson T. The difference between colour Doppler velocity imaging and power Doppler imaging. Eur. J. Echocardiogr. 2002;(3):240–244. doi: 10.1053/euje.2002.0150. [DOI] [PubMed] [Google Scholar]
- Pitskhelauri D.I., Bykanov A.E. Complication avoidance: resection of the insular glioma complicated by iatrogenic injury to the lenticulostriate artery. Acta Neurochir. 2021;163(11):3093–3096. doi: 10.1007/s00701-021-04806-2. [DOI] [PubMed] [Google Scholar]
- Rhoton A.L., Jr. The cerebral veins. Neurosurgery. 2002;51(4 Suppl. l):S159–S205. doi: 10.1227/01.NEU.0000028228.51706.2D. 2002. [DOI] [PubMed] [Google Scholar]
- Šteňo A., Jezberová M., Hollý V., Timárová G., Šteňo J. Visualization of lenticulostriate arteries during insular low-grade glioma surgeries by navigated 3D ultrasound power Doppler: technical note. J. Neurosurg. 2016;125(4):1016–1023. doi: 10.3171/2015.10.JNS151907. [DOI] [PubMed] [Google Scholar]
- Šteňo A., Buvala J., Babková V., Kiss A., Toma D., Lysak A. Current limitations of intraoperative ultrasound in brain tumor surgery. Front. Oncol. 2021;11:659048. doi: 10.3389/fonc.2021.659048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaşargil M.G., Krisht A.F., Türe U., Al-Mefty O., Yaşargil D. Microsurgery of insular gliomas: Part IV: surgical treatment and outcome. Contemp. Neurosurg. 2002;(24):1–8. doi: 10.1097/01.CNE.0000527943.73058.68. [DOI] [Google Scholar]