Abstract
Introduction
A precise knowledge of the possible Adverse Events (AEs) related to spinal surgical procedures is crucial in clinical practice.
Research Question
Purposes of this study are: to determine the prevalence and severity of perioperative AEs associated with pediatric and adult spine surgery in a high volume center; to estimate the impact of perioperative AEs on length of hospital stay (LOS).
Material and Methods
This is a prospective, observational, monocenter study, including 346 consecutive patients (294 adults and 52 pediatrics). The SAVES-V2 questionnaire was used to record AEs. The form was updated by the medical staff every time an adverse event was recorded during hospitalization.
Results
21,2% of pediatric patients and 20,7% of adults had at least 1 perioperative AEs. In adults, dural tear (3.1%) and neuropathic pain (4,8%), were the most frequent intraoperative and postoperative AE, respectively. In pediatric patients, neurologic deterioration was the most frequent postoperative AE. A diagnosis of deformity (p=0.01), an ASA grade equal or superior to 3 (p=0.023) and the procedure ‘Posterior Spinal Fusion’ (p=0.001) were associated with a higher frequency of AEs. AEs required prolonged LOS in 40 cases, 7 (70%) pediatric patients and 33 (65%) adults.
Discussion and Conclusion
The overall prevalence of AEs is 20.8%, and, although the distribution is almost equal between adult and pediatric patients, their severity is related to age, being higher in pediatric patients. Deformities, deformity correction, revision surgery and AP surgery are the most impactful factors. AEs seriously affect hospitalization, with prolonged LOS (mean 6 days).
Keywords: Spine surgery, Adverse events, Epidemiology, Patient's Safety, Deformity
Highlights
-
•
The 21,2% of pediatric patients and 20,7% of adults had at least 1 perioperative Adverse Event.
-
•
In adults, dural tears and neuropathic pain were the most frequent AEs.
-
•
In pediatric patients, neurologic deterioration was the most frequent postoperative AE.
-
•
A diagnosis of deformity was associated with a higher frequency of AEs.
-
•
The severity of AEs is related to age, being higher in pediatric patients.
1. Introduction
Spinal surgery is a rapidly growing surgical field, mainly due to the introduction of new techniques, approaches and instrumentation and therefore of increased indications for surgical treatments (Machado et al., 2017; Raad et al., 2018). In this situation, a more precise knowledge of the possible Adverse Events (AEs) related to surgical procedures and affecting patient's outcomes has become crucial in clinical practice. This should allow the patient to have all the necessary informations to provide a more precise informed consent, as well as a useful basis for surgeons to develop predictive analytics and measures to reduce the risks, with the ultimate goal to improve patient care and outcomes.
Overall, major spinal surgery is typically perceived as a risky procedure. This perception was reinforced over time by literature data that showed a high incidence of complications during or following spinal surgery (Lee et al., 2012; Nasser et al., 2010; Nohara et al., 2004; Rampersaud et al., 2006). However, a comprehensive knowledge of all AEs in spinal surgery is far from being reached. The main issue that limit progression in this field is the lack of standardized definition of AE: terms such as ‘AE’, ‘complication’, ‘harm’ and ‘adverse occurrence’ have been used interchangeably and there is a general inconsistent methodology of data collection (Elder and Dovey, 2002; Bruce et al., 2001). Moreover, the vast majority of reports on AEs are based on retrospective cohort studies or analysis of large registries, that could significantly underestimate the risk of complications (Rampersaud et al., 2006; Mirza et al., 2006; Calland et al., 2002).
Based on these considerations, some authors have recommended how to properly report AEs in spinal surgery: data collection should be prospective, ideally based on a simple recording form; AEs should be defined before their collection, and timing of occurrence and severity should be always reported (Rampersaud et al., 2006). On this prespective, the Spine Adverse Events Severity System version 2 (SAVES-V2) was developed (Rampersaud et al., 2016). it is a simple validated form to collect and report AEs related to spinal surgery. In this form, specific AEs are defined, either as intraoperative and as postoperative: Moreover, the surgeon can grade their severity in a simple and reproducible way directly on the form. The use of the SAVES-V2 has been shown to improve AEs detection, compared with other patient chart analysis, and has reached an excellent interobserver reliability (Rampersaud et al., 2016; Karstensen et al., 2016).
Given the premises above, the objectives of the present study are: (1) To determine the prevalence and severity of perioperative AEs associated with pediatric and adult spine surgery in a high volume, tertiary center. (2) To estimate the impact of perioperative AEs on length of hospital stay (LOS).
2. Methods
The study was designed according to the STROBE statements as a prospective, observational, monocenter study, to precisely describe the prevalence and severity of perioperative AEs in spine surgery. Each patient admitted to our clinic from November 2014 to November 2016 was included in this study, with no exclusion criteria other than the unwillingness of the patient to participate. 346 consecutive patients were eventually included, with no patient withdrawal. Except for 3 (0.9%) patients that had emergency admission for implant revision, each patient was scheduled for elective spinal surgery at our Institution. All patients gave their preliminary informed consent and the study was authorized by our institutional EC.
2.1. Data collection
Clinical data of the patients were collected during hospitalization.
The study involved adults (age ≥18 years old) and pediatric patients (age <18 years old); a preliminary categorization was done between first surgery and revision cases and patients were categorized in subgroups according to diagnosis and age: adults were divided into 4 subgroups (deformity, degenerative disorders, pseudoarthrosis and ‘other’) while pediatrics patients into 2 subgroups (deformity and ‘other’).
Each specific surgical procedure was recorded: i.e., if both a posterior spinal fusion (PSF) and an anterior lumbar interbody fusion (ALIF) were performed, two procedures were recorded for that patient. Therefore, the overall number of ‘Procedures’ is higher than the number of ‘Patients’. This choice allowed us to make specific subgroup analysis to determine whether a specific ‘Procedure’ is related to an increased risk of AEs. Detailed informations for adult and pediatric population's surgeries are given in Fig. 1. ASA score was collected as well. Each surgery included in the present study was performed by Surgeons with at least 5 years of experience in Spinal Surgery (see Fig. 2).
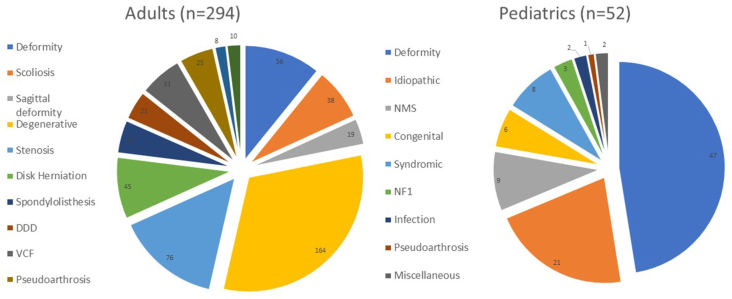
Fig. 1.
Graphical representation of Diagnostic Subgroups for the Adult (left) and Pediatric (Right) Population. Data are reported as Number. DDD, Degenerative Disk Disease; VCF, Vertebral Compression Fracture; NMS, Neuromuscular Scoliosis; NF1, Neurofibromatosis Type 1.
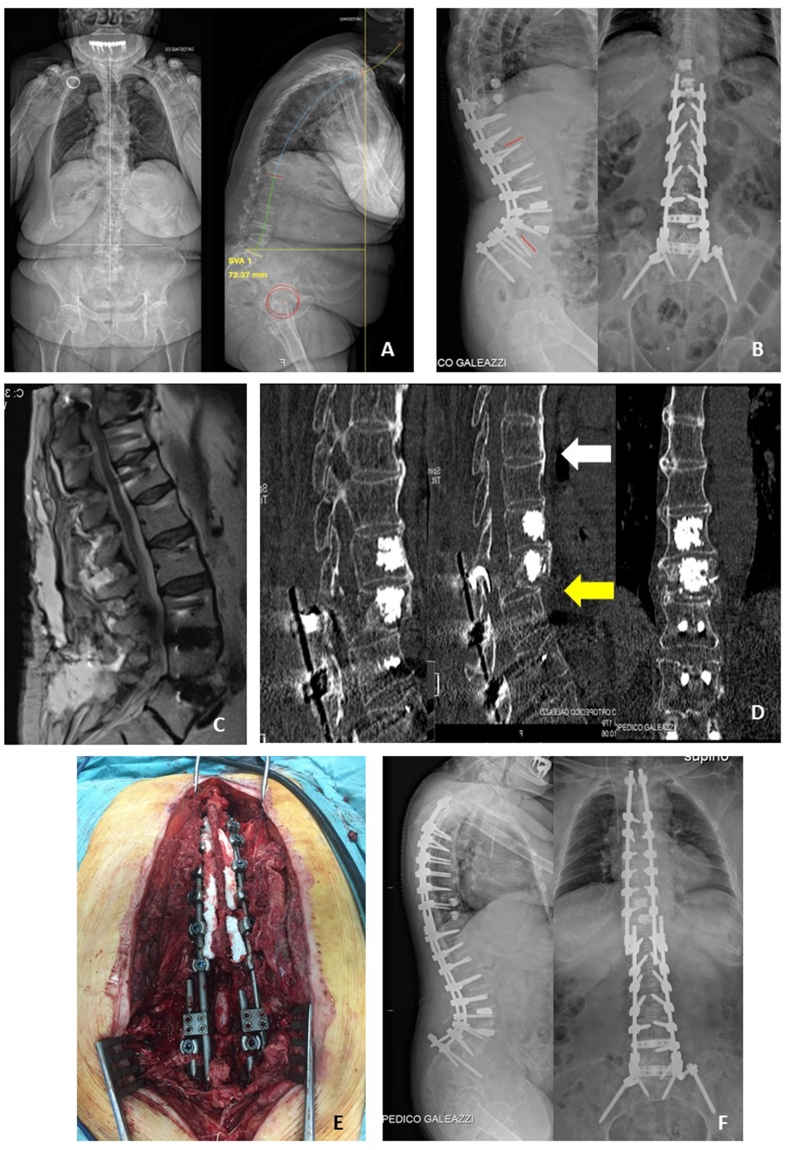
Fig. 2.
Case example of a perioperative AE: a 75 yo female was evaluated for severe back pain (VAS back 8, ODI 56). Full spine X-Rays shows a sagittal imbalance (PI-LL 41°, SVA 73 mm) (Panel A). The patient was therefore operated for deformity correction with a two stage surgery: first, extreme lateral interbody fusion (XLIF) was performed at L3-L4 and L4-L5; second, a posterior fusion from T10 to pelvis was done, with prophylactic vertebroplasty (VP) at T9 and T10 (Panel B). Seven days after surgery the patient complained of low back pain of sudden onset, so an MRI was performed (Panel C), without any pathological finding. Three days later, the patient developed paraplegya: a whole spine CT scan was performed (Panel D), that showed a fracture of T10 (Chance Fracture, AO B1) (Yellow Arrow); the fracture happened because of the complete ossification of the ALL starting from the level above the end of the instrumentation (White Arrow), thus leaving T10 in between two rigid segments; furthermore, the VP needles could have weakened the pedicles, increasing the risk of a Chance Fracture. The patient underwent emergency surgery with posterior decompression and extension of the instrumentation to T2 (Panel E, F). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The SAVES-V2 form was included in the clinical documentation of each patient, and updated by the medical staff every time an adverse event was recorded during hospitalization.
The SAVES-V2 is a form for recording, reporting and grading clinical severity of AEs in spinal surgery. It includes 14 specific intraoperative AEs, both related to anesthesia (e.g. hypotension, allergic reactions) orto the surgical procedures (e.g. dural tears, implant malpositioning etc); 22 specific postoperative AEs and a generic category named “other”. For each AE recorded, the compiler (a member of the medical staff) is required to estimate the clinical impact of the AE [by grading it from 1 (no treatment and no adverse effect) to 6 (death)], as well as to estimate the effect of the AE on the hospital LOS compared to our institution standard LOS for each type of procedure (six responses are possible: no difference, 1–2 days, 3–7 days, 8–14 days, 15–28 days, and more than 28 days).
In case of multiple AEs occurred simultaneously or in proximity, the most significant were reported. Conversely, the cumulative effect was presented, when temporally distinct events occurred.
For each patient the SAVES-V2 form was collected at discharge and used for the statistical analysis.
2.2. Statistical analysis
Descriptive statistics were used to summarize patient features and AEs incidence. This includes mean and standard deviation (SD) or median with the interquartile range (IQR) for continuous variables, and counts/percentages for categorical variables. Summary statistics were reported with maximum of 2 decimals, as appropriate. Comparison for continuous variables was performed by means of the T-test in case of normal distribution or with the nonparametric Wilcoxon rank sum test elsewhere. For comparison of categorical variables the Pearson Chi-square or Fisher's exact test was used. Statistical analysis was performed using STATA 14.1 (StataCorp LP, College Station, TX, USA). Statistical tests were based on a two-sided significance level of 0.01.
3. Results
3.1. Population and surgical procedures
Data were available for 346 (99.4%) patients out of 348; of those, 294 were adults (60.5% females, 39.5% males, mean age 48 ± 22 years old), and 52 were pediatric patients (75% females, 25% males, mean age 14 ± 3 years old). Patients were classified according to the diagnostic subgroups: in our adult population, the two most common subcohort were degenerative disorders (164 patients, 55.8%) and deformity, including adult scoliosis and sagittal imbalance (56 patients, 19%), whilst in our pediatric population, 49 (94,8%) patients underwent surgery for deformity correction, with the remaining two that underwent revision for infection [Fig. 1].
In Adults, 22.1% of patients were classified as ASA 1, 56.5% as ASA 2, 20.1 as ASA 3, and 1.4% as ASA 4; among pediatric patients, 21.2% were ASA 1, 23.1% ASA 2, 50% ASA 3 and 5.8% ASA 4.
505 surgical procedures were recorded on adults, of which 365 (72.3%) were performed as first surgery and 140 (27.7%) as revision surgery [Table 1]. Of the primary procedures, 105 (28.8%) were Posterior Spinal Fusions, with 58 short fusions (≤4 levels) and 47 long fusions (>4 levels). with Among pediatric patients, 117 overall procedures were recorded, of which 93 (79.5%) as first surgery and 24 (20.5%) as revision surgery; of those, the 41.7% occurred in cases with a diagnosis of secondary scoliosis (neuromuscular or congenital); among those with Idiopathic Scoliosis, 4 (28.6%) revision procedures were planned Growing Rods lengthening in Early Onset Scoliosis. [Table 2].
Table 1.
Overall Surgical Procedures recorded in Adult population, categorized in 1st Surgery and Revisions. PSF, Posterior Spinal Fusion; ALIF, Anterior Lumbar Interbody Fusion; TLIF Transforaminal Lumbar Interbody Fusion; XLIF Extreme Lateral Lumbar Interbody Fusion; TDA, Total Disk Arthroplasty; ACDF, Anterior Cervical Diskectomy and Fusion; PSO, Pedicle Subtraction Osteotomy.
| ADULTS (N = 294) | OVERALL PROCEDURES | C | L, LS | TL, TLS | T |
|---|---|---|---|---|---|
| Overall procedures | 505 | 16 | 305 | 52 | 17 |
| 1° SURGERY, n (%) | 365 (72.3%) | 15 | 214 | 43 | 10 |
| PSF | 105 (28.8%) | 58 (27.1%) | 43 (100%) | 4 (40%) | |
| ALIF | 17 (4.7%) | 17 (7.9%) | |||
| TLIF | 20 (5.5%) | 20 (9.3%) | |||
| XLIF | 11 (3.0%) | 11 (5.1%) | |||
| Microdiscectomy | 40 (11.0%) | 40 (18.7%) | |||
| Decompression | 68 (18.6%) | 66 (30.8%) | 2 (20%) | ||
| TDA | 2 (0.6%) | 2 (1%) | |||
| ACDF | 15 (4.1%) | 15 (100%) | |||
| Vertebroplasty | 27 (7.4%) | ||||
| Ant. Release | 3 (0.8%) | 3 (30%) | |||
| Ant. Spinal Fusion | 1 (0.3%) | 1 (10%) | |||
| Deformity correction, n (%) | 56 (15.3%) | ||||
|
| |||||
| REVISION, n (%) | 140 (27.7%) | 1 | 91 | 9 | 7 |
| PSF | 50 (35.7%) | 36 (39.6%) | 8 (88.9%) | 6 (85.7%) | |
| ALIF | 17 (12.1%) | 17 (18.7%) | |||
| TLIF | 7 (5%) | 7 (7.7%) | |||
| XLIF | 14 (10%) | 14 (15.4%) | |||
| Microdiscectomy | 1 (0.7%) | 1 (1.1%) | |||
| Decompression | 11 (7.9%) | 9 (9.9%) | 1 (11.1%) | 1 (14.3%) | |
| PSO | 7 (5%) | 7 (7.7%) | |||
| ACDF | 1 (0.7%) | 1 (100%) | |||
| Toilette | 9 (6.4%) | ||||
| Implant removal | 23 (16.4%) | ||||
| Deformity correction | 3 (2.1%) | ||||
Table 2.
Overall Surgical Procedures recorded in Pediatric population, categorized in 1st Surgery and Revisions. PSF, Posterior Spinal Fusion; TLIF, Transforaminal Lumbar Interbody Fusion; GR, Growing Rods; ACDF Anterior Cervical Diskectomy and Fusion.
| PEDIATRICS (N = 52) | OVERALL PROCEDURES | C∗ | L, LS∗ | TL, TLS∗ | T∗ | |
|---|---|---|---|---|---|---|
| Overall procedures, n (%) | 117 | 2 | 6 | 43 | 6 | |
| 1° SURGERY, n (%) | 93 (79.5%) | 2 | 5 | 39 | 3 | |
| PSF | 36 (38.7%) | 1 (50%) | 3 (60%) | 32 (82.1%) | ||
| TLIF | 1 (1.1%) | 1 (20%) | ||||
| GR Insertion | 1 (1.1%) | 1 (2.6%) | ||||
| SHILLA | 6 (6.5%) | 6 (15.4%) | ||||
| ACDF | 1 (1.1%) | 1 (50%) | ||||
| Release + HALO | 4 (4.3%) | |||||
| Anterior | 3 (3.2%) | 1 (20%) | 2 (66.6%) | |||
| Posterior | 1 (1.1%) | 1 (33.3%) | ||||
| Deformity Correction | 40 (47%) | |||||
| REVISION | 24 (20.5%) | 0 | 1 | 4 | 3 | |
| Toilette | 1 (4.1%) | 1 (25%) | ||||
| PSF rev. | 5 (20.8%) | 1 | 3 (75%) | 1 (33.3%) | ||
| Anterior Spinal Fusion | 1 (4.1%) | 1 (33.3%) | ||||
| Anterior Release | 1 (4.1%) | 1 (33.3%) | ||||
| GR Lengthening | 6 (25%) | |||||
| Implant Removal | 3 (12.5%) | |||||
| Deformity Correction | 7 (29.2%) | |||||
3.2. 1AEs distribution and surgical variables association
Overall, 77 AEs occurred in 72 patients (20.8%). In particular, 13 AEs occurred in 11 (21.5%) pediatrics patients and 64 AEs occurred in 61 (17.6%) adults. Distribution and type of AEs are reported in Table 3. Among adults, dural tears (3.1%) and postoperative neuropathic pain (4.8%) were the most common intra and perioperative AEs, respectively. Among pediatric patients, the most common AE was the presence of postoperative neurological deficit (3 cases, 5,8%; two of those were transitory and resolved in the first week, while the remaining one had a postoperative spinal cord lesion with paraplegia).
Table 3.
Overall AEs recorded in the whole population, categorized in intra and postoperative.
| INTRAOPERATIVE | Overall | Ped | Adults |
|---|---|---|---|
| Total intraoperative, n (%) | 24 (6.9%) | 4 (7.7%) | 20 (6.8%) |
| Allergic reaction, n (%) | 3 (0.9%) | 1 (1.9%) | |
| Cord injury, n (%) | 1 (0.3%) | 1 (1.9%) | |
| Dural tear, n (%) | 9 (2.6%) | 9 (3.1%) | |
| Hardware malp. requiring revision, n (%) | 4 (1.2%) | 1 (1.9%) | 3 (1.0%) |
| Hypotension, n (%) | 1 (0.3%) | 1 (1.9%) | |
| Massive blood loss, n (%) | 4 (1.2%) | 1 (1.9%) | 3 (1.0%) |
| Vascular injury, n (%) | 2 (0.6%) | 2 (0.7%) | |
| Airway/ventilation, n (%) | 1 (0.3%) | 1 (1.9%) | |
| Other, n (%) |
2 (0.6%) |
2 (0.7%) |
|
| POSTOPERATIVE | Overall | Ped | Adults |
| Total postoperative, n (%) | 48 (13.9%) | 7 (13.5%) | 41 (13.9%) |
| Cardiac arrest/failure/arrhythmia, n (%) | 3 (0.9%) | 3 (1.0%) | |
| Construct failure with loss of correc., n (%) | 3 (0.9%) | 3 (1.0%) | |
| CSF leak/meningocele, n (%) | 1 (0.3%) | 1 (0.3%) | |
| Deep wound infection, n (%) | 3 (0.9%) | 3 (1.0%) | |
| Dysphagia, n (%) | 1 (0.3%) | 1 (0.3%) | |
| Hematoma, n (%) | 1 (0.3%) | 1 (0.3%) | |
| Neurologic det. ≥ 1 motor grade, n (%) | 10 (2.9%) | 3 (5.8%) | 7 (2.4%) |
| Postop. neuropathic pain, n (%) | 14 (4.0%) | 14 (4.8%) | |
| Wound dehiscence, n (%) | 1 (0.3%) | 1 (0.3%) | |
| Other, n (%) | 15 (4.3%) | 4 (7.7%) | 11 (3.7%) |
No association was found between demographic data (age, gender) and the frequency of AEs. Conversely, when analyzing the diagnostic subgroups, results are reported in Table 4; overall, patients with a diagnosis of deformity (p = 0.01) have more often AEs than the others. ASA grade equal or superior to 3 was associated with a higher frequency of AEs (p = 0.023).
Table 4.
Association Between presence of AE and each diagnostic subgroup in the whole Population. Data reported as Number (Percentage).
| No AEs (n = 238; 81.0%) | AEs (n = 56; 19.1%) | p-value | |
|---|---|---|---|
| Diagnostic Subgroups | |||
| Deformity | 78 (28%) | 29 (43.3%) | 0.015 |
| Degenerative | 143 (51.3%) | 21 (31.3%) | ns |
| Vertebral Fracture | 24 (8.6%) | 7 (10.4%) | ns |
| Pseudoarthrosis | 27 (9.7%) | 7 (10.4%) | ns |
| Others | 8 (2.9%) | 4 (6%) | ns |
When evaluating the association between type of surgical procedure and AEs for the whole population, PSF was associated with a significantly higher frequency of AEs (p = 0.001). A borderline significant association was found also for ALIF (p = 0,013), XLIF (p = 0.029), decompression only (p = 0.021) and association between an anterior and posterior approach (PSF + ALIF or PSF + XLIF) on the same patient (p = 0.035). Concerning the spinal region of surgery, patients who were operated with long thoracolumbar fusion had a higher number of AEs (p = 0.008), as well as revision surgeries were associated with more AEs (p = 0.004).
Subgroup analysis of association between surgical procedures and AEs for adults and pediatric patients are reported in Table 5, Table 6, respectively. For pediatric patients, only the anterior release reaches a borderline significant association (p = 0.047). Conversely, in adults the deformity correction (p = 0.008) and long fusions including both the Lumbar and Thoracic Spine (p = 0.0001) are strongly associated with an increased frequency of AEs.
Table 5.
Association Between presence of AE, each procedure recorded and the level of the procedure in Adult Population. Data reported as Number (Percentage).
| No AEs (n = 238; 81.0%) | AEs (n = 56; 19.1%) | p-value | |
|---|---|---|---|
| Procedure | |||
| PSF | 112 (47.1%) | 42 (75.0%) | 0.000 |
| ALIF | 23 (9.7%) | 12 (21.4%) | 0.014 |
| TLIF | 21 (8.8%) | 6 (10.7%) | 0.659 |
| XLIF | 17 (7.1%) | 9 (16.1%) | 0.034 |
| Microdiscectomy | 39 (16.4%) | 3 (5.4%) | 0.034 |
| Decompression | 71 (29.8%) | 8 (14.3%) | 0.018 |
| PSO | 4 (1.7%) | 3 (5.4%) | 0.104 |
| TDA | 2 (0.8%) | 0 (0.0%) | 0.491 |
| ACDF | 16 (6.7%) | 1 (1.8%) | 0.154 |
| Vertebroplasty | 23 (9.7%) | 4 (7.1%) | 0.557 |
| Posterior relase | 1 (0.4%) | 0 (0.0%) | 0.627 |
| Anterior release | 2 (0.8%) | 0 (0.0%) | 0.491 |
| Toilette | 6 (2.5%) | 3 (5.4%) | 0.268 |
| Rods lengthened | |||
| Implant removal | 19 (8.0%) | 5 (8.9%) | 0.816 |
| Deformity correction | 24 (10.1%) | 13 (23.2%) | 0.008 |
| Revision required | 49 (20.6%) | 18 (32.1%) | 0.064 |
| Level | |||
| Cervical | 36 (15.1%) | 6 (10.7%) | 0.396 |
| Lumbar | 170 (71.4%) | 38 (67.9%) | 0.597 |
| Thoraco-lumbar | 34 (14.3%) | 19 (33.9%) | 0.001 |
| Thoracic | 27 (11.3%) | 6 (10.7%) | 0.893 |
Table 6.
Association Between presence of AE, each procedure recorded and the level of the procedure in Pediatric Population. Data reported as Number (Percentage).
| No AEs (n = 41; 78.8%) | AEs (n = 11; 21.1%) | p-value | |
|---|---|---|---|
| Procedure | |||
| PSF | 35 (85.4%) | 8 (72.7%) | 0.325 |
| TLIF | 1 (2.4%) | 0 (0.0%) | 0.601 |
| ACDF | 1 (2.4%) | 0 (0.0%) | 0.601 |
| Posterior relase | 0 (0.0%) | 1 (9.1%) | 0.051 |
| Anterior release | 1 (2.4%) | 2 (18.2%) | 0.047 |
| Toilette | 0 (0.0%) | 1 (9.1%) | 0.051 |
| Rods lengthened | 5 (12.2%) | 1 (9.1%) | 0.775 |
| Implant removal | 3 (7.3%) | 0 (0.0%) | 0.355 |
| Deformity correction | 30 (73.2%) | 6 (54.6%) | 0.235 |
| Revision required | 8 (19.5%) | 3 (27.3%) | 0.576 |
| Level | |||
| Cervical | 4 (9.8%) | 0 (0.0%) | 0.281 |
| Lumbar | 6 (14.6%) | 1 (9.1%) | 0.632 |
| Thoraco-lumbar | 30 (73.2%) | 7 (63.6%) | 0.535 |
| Thoracic | 3 (7.3%) | 0 (0.0%) | 0.355 |
3.3. Severity of AEs and LOS
Severity of AEs is detailed in Table 7: Severe AEs (Grade 3, 4 and 5) occurred more frequently in pediatric patients than in adults.
Table 7.
Severity of AEs recorded.
| All∗ (n = 64) | Pediatrics (n = 11) | Adults (n = 53) | |
|---|---|---|---|
| Grade 1 | 22 (34.4%) | 2 (18.2%) | 20 (37.7%) |
| Grade 2 | 18 (28.1%) | 1 (9.1%) | 17 (32.1%) |
| Grade 3 | 17 (26.6%) | 4 (36.4%) | 13 (24.5%) |
| Grade 4 | 4 (6.3%) | 2 (18.2%) | 2 (3.8%) |
| Grade 5 | 3 (4.7%) | 2 (18.2%) | 1 (1.9%) |
Abbreviations: AEs, Adverse Events; LOS, Length of Hospital Stay; SAVES-V2, Spine Adverse Events Severity System version 2.
LOS for the whole population ranged from 1 to 75 days, with a median value of 6 days. AEs required prolonged LOS in 40 cases, 7 (70%) pediatric patients and 33 (65%) adults (p = 0.747): The presence of AEs was associated with longer LOS (6 ± 3.5 days vs 12,1 ± 11 days, p < 0.001), with a mean of 6 more days of hospitalization. Perioperative AEs have required a revision surgery in 4,9% (17) of patients.
4. Discussion
A comprehensive knowledge of AEs in spinal surgery is lacking. This is due to a high variability in defining, grading and reporting AEs, and because several studies are based on retrospective analysis that could easily underestimate their prevalence.
In a review by Nasser et al. that includes more than 100 papers, incidence of AEs ranged from 4.8% to 66% and a significant difference in the rate of reported complications, between prospective and retrospective studies, was detected (Nasser et al., 2010).
This data heterogeneity could creates confusion and uncertainty both for the surgeon and the patients, about a preoperative risk definition. Moreover, it makes unreliable a benchmark on surgical procedure's and PROMs analysis.
To overcome those limitations, the SAVES-V2 form has been proposed to be used in spinal surgery (Rampersaud et al., 2016). It was specifically developed to “capture” AEs and designed for a prospective data collection; it has been validated in various clinical settings and showed a good intra and interobserver reliability.
Using this tool, we conducted a prospective analysis of AEs in spinal surgery, evaluating prevalence, severity and impact on length of hospital stay in a high volume, referral center both on adults and pediatric patients. The first study to use the SAVES-V2 questionnaire to prospectively collect AEs in spinal surgery was published by Street et al. (2012): they described an incidence of perioperative AEs of 73.5%, similar to the 77% found by Karstensen et al. (2016). In both studies the incidence was much higher than the 12,4% we found in our population.
This difference could be explained by the fact that in these two studies some electrolyte imbalances and medication-related side effects were considered as AEs (in the “other” category); those two side-effects had the highest incidence in their studies.
Similarly to the approach used by Rampersaud et al. (2010), we decided not to consider the occurrence of a slight electrolyte imbalance as a perioperative AE; similarly, medication-related side effects were reported as AE only when serious enough to alter LOS.
Interestingly, with this approach the high differences in the reported incidence of postoperative AEs are due to 2 non-categorized AEs, therefore highlighting the importance of a strict definition of what is considered or not an AE.
Considering the clinical, diagnostic and surgical variables, we found in adult population that the diagnosis of “deformity” and the procedures “deformity correction and PSF”, as well as revision surgery were associated with a higher prevalence of AEs. The observation that an ASA Class ≥3 is associated with increased prevalence of AEs is consistent with most of the literature (Kwan et al., 2018; Somani et al., 2017; Onda et al., 2018), and highlights the importance of checking the overall status of the patient when planning a spinal procedure.
Surgery for adult spine deformity is usually perceived as more risky when compared with other kinds of procedures. A systematic review by the International Spine Study Group found a prevalence of perioperative AEs of 34.2% following surgery for adult spine deformity (Sciubba et al., 2015). However, these results are biased by the heterogeneous inclusion criteria, the retrospective nature of the majority of included studies (87%), and the lack of a standardized definition of AEs among studies. In a recent prospective, multicenter study by Kwan et al. the prevalence of non-neurologic perioperative AEs in adult spine deformity was found to be 43% (Kwan et al., 2018). In our study, the prevalence of AEs in adult deformity patient was 27.1%. This difference could explained by the different definition of AE, particularly concerning the “minor” AES included in other studies.
In our study, we have collected the same categories of AEs either in patients with deformity or without, and the significantly higher prevalence of AEs that we found in the former subgroup strengthen the issue that adult deformity surgery is more risky than surgery for degenerative conditions without deformity. Interestingly, in a study by Smith et al. regarding the deformity correction with three-column osteotomies, the same complications prevalence was found between cervical and thoracic procedures, thereby suggesting that correction of deformity itself is the risky procedure, irrespective of the site (Smith et al., 2017). Our findings confirmed this strong association between the “deformity correction” procedure and a higher prevalence of AEs.
Population-based studies reported higher risk of complication in instrumented surgery than in non-instrumented surgery (8), as confirmed in the prospective study by Campbell et al. that showed also increased complications in longer fusions (Campbell et al., 2011). These observations are consistent with our results: posterior instrumented surgery, as well as long fusions, were associated with higher AEs occurrences than other procedures.
In our study, revision surgeries were associated with an increased risk of AEs in agreement with other trials (3,10,11). Generally, they are technically demanding procedures, surgeon must often manage previous instrumentations, with coronal and/or sagittal malalignment and combined surgical approaches are often necessary.
Very few studies prospectively evaluated the incidence of AEs specifically in a pediatric population. In the study by Karstensen et al., 87 patients included were under 18 years of age, but no detailed analysis was performed (Karstensen et al., 2016). Smith et al. on 65 patients treated surgically for Early Onset Scoliosis, 59 have shown at least one AE, with the most common being instrumentation failures and infections. In a large, retrospective study on pediatric patients based on the SRS database, but limited to the diagnosis of spondylolisthesis, Fu et al. have found an overall incidence of major postoperative complications of 10.4% (Fu et al., 2011). In another study on the same database, conducted on the Adolescent Idiopathic Scoliosis surgery, the overall complication rate reported was the 3.9% (Lee et al., 2016). It should be noted, however, that the SRS Morbidity and mortality Database has less defined items compared to the SAVES-V2 used in this study (i.e. new neurologic deficit, infections, unintentional return to OR within 90 days, death). In our study the overall incidence of AEs in the pediatric population is 21.5%, thus similar to the adult population but with more severe AEs. This can be explained by the variety of procedures performed on pediatric patients: most of them were “deformity correction with PSF”, but we have treated also EOS patients with growing rods, that are often associated with a several complications (Teoh et al., 2016). This assumption is confirmed by our observation that an anterior release was associated with more AEs, being it generally required in most severe deformities, with more complex surgical approaches, thus at higher risk of complications.
Another significant finding of our study is that 70% of AEs in pediatric population and 65% in adult population were serious enough to prolong the LOS. We have observed a mean increase of 6 days, similar to what reported in other studies (Yadla et al., 2015; Culler et al., 2016), either in pediatric and adult population. Recently, Sultan et al. have found in AIS patients that perioperative complications have prolonged the LOS (Sultan et al., 2018).
Our study has some limitations: first, it reflects the experience of a single center, with the strength that surgeries were performed by the same team with consistent methodology, but reflecting only the range of spinal disorders treated by us, excluding spinal tumors or trauma. Second, the self collection of AEs could be seen as a bias with an underestimation effect; however, comparative studies have shown that the use of the SAVES-V2 intrinsically reduces such biases (Rampersaud et al., 2016). Third, although the total number of patients included is large, the subcohort for some procedures is quite limited. Finally, we did not evaluated the patient's specific outcomes for each patient included in this study; while this analysis goes beyond the scope of this paper, we nonetheless graded the severity of AEs according to the SAVES-V2 definition, and estimated the impact on the length of stay, to provide an overall understanding of their clinical relevance.
5. Conclusions
This study provides prospectively collected data on AEs in spinal surgery in a high-volume referral center using the SAVES-V2 form. The SAVES-V2 is a simple and reliable tool to identify and grade perioperative AEs in spinal surgery.
The main findings of our paper can be summarized as follows:
-
•
The overall prevalence of AEs found in this study (20.8%) is high if compared to retrospective analysis, but similar to what reported in prospective studies.
-
•
Although the distribution of AEs is almost equal between adult and pediatric patients, their severity is related to age, being higher in pediatric patients.
-
•
In Adults, a diagnosis of deformity, and the procedures of deformity correction, revision surgery and anterior-posterior surgery are the most ‘at risk’ for AEs occurrence.
-
•
In Pediatric Patients, Anterior Release is the most ‘at risk’ procedure for AEs occurrence
-
•
AEs seriously affect hospitalization, with prolonged LOS (mean of 6 days).
These data could be useful for clinicians to improve counseling of potential spine surgical patients and would be helpful to identify higher risk situations preoperatively.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
AL: Conceptualization, Data Collection, Writing – Review & Editing.
EG: Data Analysis, Writing – Draft.
FG: Data Analysis, Writing – Review & Editing.
AC: Data Analysis, Writing – Review & Editing.
FP: Project Management, Supervision.
GP: Supervision, Writing – Review & Editing.
MBB: Supervision, Writing – Review & Editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The Authors acknowledge the work of Andrea Luca MD, Lisa Babbi MD, Francesca Manfroni MD and Sara Razza MD for the help in data collection.
References
- Bruce J., Russell E.M., Mollison J., Krukowski Z.H. The measurement and monitoring of surgical adverse events. Health Technol. Assess. 2001;5:1–194. doi: 10.3310/hta5220. [DOI] [PubMed] [Google Scholar]
- Calland J.F., Adams R.B., Benjamin D.K.J., et al. Thirty-day postoperative death rate at an academic medical center. Ann. Surg. 2002;235:690–698. doi: 10.1097/00000658-200205000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell P.G., Yadla S., Malone J., et al. Complications related to instrumentation in spine surgery: a prospective analysis. Neurosurg. Focus. 2011;31:E10. doi: 10.3171/2011.7.FOCUS1134. [DOI] [PubMed] [Google Scholar]
- Culler S.D., Jevsevar D.S., Shea K.G., et al. Incremental hospital cost and length-of-stay associated with treating adverse events among medicare beneficiaries undergoing lumbar spinal fusion during fiscal year 2013. Spine (Phila Pa 1976) 2016;41:1613–1620. doi: 10.1097/BRS.0000000000001641. [DOI] [PubMed] [Google Scholar]
- Elder N.C., Dovey S.M. Classification of medical errors and preventable adverse events in primary care: a synthesis of the literature. J. Fam. Pract. 2002;51:927–932. [PubMed] [Google Scholar]
- Fu K.-M.G., Smith J.S., Polly D.W.J., et al. Morbidity and mortality in the surgical treatment of six hundred five pediatric patients with isthmic or dysplastic spondylolisthesis. Spine (Phila Pa. 2011;36:308–312. doi: 10.1097/BRS.0b013e3181cf3a1d. 1976. [DOI] [PubMed] [Google Scholar]
- Karstensen S., Bari T., Gehrchen M., et al. Morbidity and mortality of complex spine surgery: a prospective cohort study in 679 patients validating the Spine AdVerse Event Severity (SAVES) system in a European population. Spine J. 2016;16:146–153. doi: 10.1016/j.spinee.2015.09.051. [DOI] [PubMed] [Google Scholar]
- Kwan K.Y.H., Bow C., Samartzis D., et al. Non-neurologic adverse events after complex adult spinal deformity surgery: results from the prospective, multicenter Scoli-RISK-1 study. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2018 doi: 10.1007/s00586-018-5790-y. [DOI] [PubMed] [Google Scholar]
- Lee M.J., Konodi M.A., Cizik A.M., et al. Risk factors for medical complication after spine surgery: a multivariate analysis of 1,591 patients. Spine J. 2012;12:197–206. doi: 10.1016/j.spinee.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee N.J., Guzman J.Z., Kim J., et al. A comparative analysis among the SRS M&M, NIS, and KID databases for the adolescent idiopathic scoliosis. Spine Deform. 2016;4:420–424. doi: 10.1016/j.jspd.2016.05.005. [DOI] [PubMed] [Google Scholar]
- Machado G.C., Maher C.G., Ferreira P.H., et al. Trends, complications, and costs for hospital admission and surgery for lumbar spinal stenosis. Spine (Phila Pa 1976) 2017;42:1737–1743. doi: 10.1097/BRS.0000000000002207. [DOI] [PubMed] [Google Scholar]
- Mirza S.K., Deyo R.A., Heagerty P.J., et al. Towards standardized measurement of adverse events in spine surgery: conceptual model and pilot evaluation. BMC Muscoskel. Disord. 2006;7:53. doi: 10.1186/1471-2474-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasser R., Yadla S., Maltenfort M.G., et al. Complications in spine surgery. J. Neurosurg. Spine. 2010;13:144–157. doi: 10.3171/2010.3.SPINE09369. [DOI] [PubMed] [Google Scholar]
- Nohara Y., Taneichi H., Ueyama K., et al. Nationwide survey on complications of spine surgery in Japan. J. Orthop. Sci. 2004;9:424–433. doi: 10.1007/s00776-004-0802-7. [DOI] [PubMed] [Google Scholar]
- Onda S., Kanayama M., Hashimoto T., et al. Peri-operative complications of lumbar spine surgery in patients over eighty five years of age: a retrospective cohort study. Int. Orthop. 2018;42:1083–1089. doi: 10.1007/s00264-018-3875-1. [DOI] [PubMed] [Google Scholar]
- Raad M., Donaldson C.J., El Dafrawy M.H., et al. Trends in isolated lumbar spinal stenosis surgery among working US adults aged 40-64 years, 2010-2014. J. Neurosurg. Spine. 2018;29:169–175. doi: 10.3171/2018.1.SPINE17964. [DOI] [PubMed] [Google Scholar]
- Rampersaud Y.R., Moro E.R.P., Neary M.A., et al. Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine (Phila Pa 1976) 2006. 31:1503-1510. [DOI] [PubMed]
- Rampersaud Y.R., Neary M.A., White K. Spine adverse events severity system: content validation and interobserver reliability assessment. Spine (Phila Pa. 2010;35:790–795. doi: 10.1097/BRS.0b013e3181bf25a3. 1976. [DOI] [PubMed] [Google Scholar]
- Rampersaud Y.R., Anderson P.A., Dimar J.R., 2nd, Fisher C.G. Spinal Adverse Events Severity System, version 2 (SAVES-V2): inter- and intraobserver reliability assessment. J. Neurosurg. Spine. 2016;25:256–263. doi: 10.3171/2016.1.SPINE14808. [DOI] [PubMed] [Google Scholar]
- Sciubba D.M., Yurter A., Smith J.S., et al. A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform. 2015;3:575–594. doi: 10.1016/j.jspd.2015.04.005. [DOI] [PubMed] [Google Scholar]
- Smith J.S., Shaffrey C.I., Lafage R., et al. Three-column osteotomy for correction of cervical and cervicothoracic deformities: alignment changes and early complications in a multicenter prospective series of 23 patients. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2017;26:2128–2137. doi: 10.1007/s00586-017-5071-1. [DOI] [PubMed] [Google Scholar]
- Somani S., Capua J Di, Kim J.S., et al. ASA classification as a risk stratification tool in adult spinal deformity surgery: a study of 5805 patients. Glob. Spine J. 2017;7:719–726. doi: 10.1177/2192568217700106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street J.T., Lenehan B.J., DiPaola C.P., et al. Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients. Spine J. 2012;12:22–34. doi: 10.1016/j.spinee.2011.12.003. [DOI] [PubMed] [Google Scholar]
- Sultan A.A., Berger R.J., Cantrell W.A., et al. Predictors of extended length of hospital stay in adolescent idiopathic scoliosis patients undergoing posterior segmental instrumented fusion: an analysis of 407 surgeries performed at a large academic center. Spine (Phila Pa 1976) 2018 doi: 10.1097/BRS.0000000000002919. [DOI] [PubMed] [Google Scholar]
- Teoh K.H., Winson D.M.G., James S.H., et al. Do magnetic growing rods have lower complication rates compared with conventional growing rods? Spine J. 2016;16:S40–S44. doi: 10.1016/j.spinee.2015.12.099. [DOI] [PubMed] [Google Scholar]
- Yadla S., Ghobrial G.M., Campbell P.G., et al. Identification of complications that have a significant effect on length of stay after spine surgery and predictive value of 90-day readmission rate. J. Neurosurg. Spine. 2015;23:807–811. doi: 10.3171/2015.3.SPINE14318. [DOI] [PubMed] [Google Scholar]