Abstract
Introduction
Neurological disorders are one of the leading causes of death and disability adjusted life years (DALYs). Efforts have been made to increase the neurosurgical workforce in an attempt to address the global disease burden. Despite these efforts, there continues to be a shortage of neurosurgeons in both high-income countries (HICs) and low-and middle-income countries (LMICs).
Research question
The aim of the study was to identify the barriers to neurosurgical training in LMICs and HICs.
Materials and methods
We administered an electronic survey targeting medical students, neurosurgery residents, and recent neurosurgery graduates from 69 countries in both HICs and LMICs. Questions were framed to assess barriers to training.
Results
Of the 198 responses received (31.3% response rate), 72% identified as male, 27% female, and 0.5% as non-binary gender. 33 respondents were from HICs and 165 were from LMICs. 70.1% of respondents reported no availability of dissection labs in their home institutions. There was a significant difference in availability of subspecialty training between LMICs and HMICs (p = 0.001) but no significance was seen for competitiveness of programs (p = 0.473).
Discussion and conclusion
There are limitations to our study: it is not comprehensive of training programs globally, there is sampling bias, especially among LMICs, and the accuracy of responses is unclear. Nonetheless, our results highlight the need for a deliberate focus on designing and implementing both short and long term goals in tackling barriers to access to neurosurgical training, with a conscientious effort to involve interested stakeholders and governments to invest in the training and education of their neurosurgical workforce.
Keywords: Neurosurgery, Low- and middle-income countries (LMICs), High-income countries (HICs)
Highlights
-
•
In comparing LMICs to HICs, there was no significant difference found in ranked competitiveness for entering neurosurgical training.
-
•
A significant difference was found in weekly work hours (p = 0.016) and subspecialty training availability (p = 0.001) between LMICs and HMICs.
-
•
54.4% of countries represented in our study did not have neurosurgical subspecialty training available.
-
•
A significant number of our respondents (70.1%) reported no availability of dissection and surgical skills labs in their home institutions.
1. Introduction
Neurological disorders are one of the leading causes of death and disability worldwide (GBD, 2016 Neurology Collaborators, 2019). Each year, 22.6 million patients suffer from neurological disorders or injuries, 13.8 million of whom require surgical care. In order to address this need, an estimated 23,300 additional neurosurgeons are needed around the world to provide the essential surgical care (Dewan et al., 2018). Despite these reports, there continues to exist a wide gap in the provision of equitable access to neurosurgical care worldwide, with low- and middle-income countries (LMICs) bearing the brunt of the deficit, and large geographic treatment gaps particularly in Africa and Southeast Asia (Dewan et al., 2018). One of the critical key factors contributing to this wide gap is the lack of sufficient surgical workforce density. Many studies have supported the call to increase the neurosurgical workforce capacity, particularly in LMICs, and have called on the global neurosurgery community to assist in increasing the number of training programs, recruiting interested medical students and young physicians early into the field, and retaining existing trainees within their home countries (Dewan et al., 2018; Punchak et al., 2018).
Within high-income countries (HICs) in Europe and North America, neurosurgical training is usually standardized (Burkhardt et al., 2010a). The rigorous training requires medical school graduates and aspiring trainees to complete four or more years of medical school, followed by standard licensing, after which they commit to several years of residency training either via a direct route or after completion of a required general surgery training. This length of time varies depending on the specific program and country of training. Despite efforts to harmonize training in the European Union, there still exists significant variability in trainee access to educational materials and experiences such as hands-on surgical skills and simulation labs (Stienen et al., 2016a). In LMICs, there is even greater variability in training, with many countries lacking a uniform curriculum, varying training lengths, and different routes to training with differing certifications, or even no certification at all (Kato et al., 2020). This has led some to advocate for global standardized training in order to facilitate collaboration between training centers (Burkhardt et al., 2010a). Some of these efforts have met with success, such as in the multi-country training model of the College of Surgeons of East, Central, and Southern Africa (COSECSA). (Henderson et al., 2020).
As part of these efforts to increase and improve neurosurgical training, there must be a collaborative and conscientious effort to address the multitude of barriers students and trainees face in their pursuit to become neurosurgeons. Despite the increased momentum behind training neurosurgeons worldwide, there remain several barriers to accessing and completing accredited neurosurgical training programs, especially for medical school graduates in LMICs. Beyond the complete absence of any neurosurgical training in some countries, several barriers to easy accessibility to neurosurgical training have been reported in the literature for both HICs and LMICs that have training programs (Dias et al., 2013; Gnanakumar et al., 2020). Examples include lack of dissection and surgical skills labs, sustainable and cost-effective training modules or curricula, insufficient health research capacity to address local disease burden, and a paucity of mentors (Liang et al., 2016; Qayumi, 2010; Franzen et al., 2017; Lescano et al., 2019). These barriers; however, are significantly more pronounced in LMICs due to lack of standardized training, poor government investment in healthcare infrastructure, and more specifically, a lack of prioritization of surgical subspecialties. Studies from organizations such as the World Health Organization (WHO) have attributed this lack of investment in LMICs to a focus on communicable and non-communicable diseases such as heart disease over surgical disorders and injuries (Debas et al., 2015).
In this study, we assess the barriers to access to neurosurgical training for medical students seeking to enter training and for trainees in accessing resources to further their training, both in LMICs and HICs globally. Moreover, we explore the data to understand the similarities and differences in both settings, and seek sustainable long-term solutions for stakeholders to actively assist in breaking down these barriers.
2. Methods
This study was a collaborative effort by members of the Harvard Program in Global Surgery and Social Change, World Federation of Neurosurgical Societies Global Neurosurgery Committee, and the Ribat Neurospine Center, Ribat University Hospital of Sudan. The study was approved by the Harvard Medical School Institutional Review Board (IRB20-1372).
2.1. Survey design
Utilizing the EQUATOR checklist (Kelley et al., 2003), we developed a 12 to 23-question survey to assess the current neurosurgical training capacity and barriers to training around the world, with a particular focus on LMICs. Questionnaire length varied based on participant responses to initial questions. The survey was targeted at applicants to neurosurgical training, current trainees, and recent graduates from neurosurgical training programs within the past four years. All participants were asked questions regarding access and applying to neurosurgical training, while only current trainees and recent graduates were asked regarding resources and characteristics of training. The questionnaire was developed by one author (AA) and underwent review and revisions by the research team, which included members from the United States and Sudan, both neurosurgical trainees and medical students, until consensus was achieved.
Survey variables were designed to collect data on participant demographics, geographic location, training level, and barriers to access to training. Specific questions were constructed to assess the presence and size of training programs, length of training, cost of entry and training, workload, and caseload. Additionally, data was collected on participant perceptions of competitiveness, availability of mentorship, and research opportunities. The details of the survey questionnaire are included in the supplementary Appendix 1.
2.2. Identification of participants
We sought the perspective of applicants to neurosurgical training, current trainees, and recent graduates from neurosurgical training programs within the past four years. Efforts were made to include respondents who were representative of all WHO regions with a focus on LMICs. In order to achieve this, our recruitment efforts were focused on international groups that contained our target groups. We advertised our study with the Global Surgery Student Alliance, Young African Neurosurgeons, and the Neurosurgery Cocktail Facebook group, utilizing email, social media platforms such as Twitter and Facebook, and messaging apps such as Telegram and WhatsApp. Requests were also made for word-of-mouth advertisement and through personal contacts of the study authors.
2.3. Survey distribution
Participants consented to receive an invitation to the survey by signing up via a Google Forms (Google, Mountainview, CA) request. Study data were collected and managed using REDCap electronic data capture tools hosted at Harvard Medical School (Harris et al., 2009). REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing: 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources. The survey was administered in English. Responses were collected from September 7th to November 10th, 2020. In order to improve response rate, biweekly reminder emails were sent out during this period to all invited participants who had not yet responded to the survey, for a total of three reminders (Hoddinott and Bass, 1986). A total of 633 people were invited to participate in the survey with a goal response rate of approximately 33% (Nulty, 2008).
2.4. Data analysis
Results were exported from the REDCap system into Microsoft Excel© 2016, and analyzed using SPSS (SPSS Inc. Released, 2009. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc.). Mean, mode, and frequency distributions were determined for respective variables in each country. When more than one mode was found for a variable, clarification was obtained by searching the literature or contacting neurosurgical society representatives for the respective country. When an answer was not able to be found, consensus was obtained amongst the authors as to which answer to select, and was then consistently applied to all relevant answers for a variable. Data was then analyzed at both a global and country-specific level. Countries were also grouped into high-income (HIC) and low- and middle-income (LMIC) classifications using the World Bank income classification. (The World Bank) Nonparametric comparison of the means using the Mann-Whitney U test was performed, comparing the HIC to LMIC group.
3. Results
3.1. Respondent demographics
We received a total of 198 responses out of 633 people invited to complete the survey, giving a 31.3% response rate. Of 198 responses from 69 different countries, 33 (16.70%) were from HICs and 165 (83.30%) were from LMICs (Fig. 1). 143 respondents identified as male (72%), 54 as female (27%), and 1 as non-binary gender (0.5%). Aspiring neurosurgeons, current neurosurgery trainees and recent neurosurgery graduates comprised 37%, 36%, and 27% of respondents, respectively (Table 1). The mean year in training for the neurosurgery trainees was 3.6 ± 1.7. The mean age of respondents was 32.5 ± 8.4 years. 33 respondents, only one of whom was from a HIC, attended medical school in a country different from that of their country of origin; 15 respondents - 4 from HIC medical schools - then underwent neurosurgical training in a country different from where they attended medical school.
Fig. 1.
Map view of country representation. Each blue-filled country had at least one respondent from that country. Number of respondents from each country is not shown here. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Table 1.
Respondent demographics with number of respondents for each category listed and percentage of respondents in parentheses.
| Amount (Percentage) | |
|---|---|
| Country-Income Group | |
| HIC | 33 (16.7%) |
| LMIC | 165 (83.3%) |
| Gender | |
| Male | 143 (72%) |
| Female | 54 (27%) |
| Non-binary | 1 (0.5%) |
| Training Level | |
| Aspiring Neurosurgeon | 70 (37%) |
| Neurosurgery Trainee | 68 (36%) |
| Recent Neurosurgery Graduate | 51 (27%) |
3.2. Global statistics
Measures of competitiveness for entering neurosurgical training and availability of mentorship were collected from all respondents. Globally, the mean competitiveness on a scale of 1–10 was ranked as 7.8 ± 2.5. The mean mentorship availability on a scale of 1–10 was ranked as 4.8 ± 2.6.
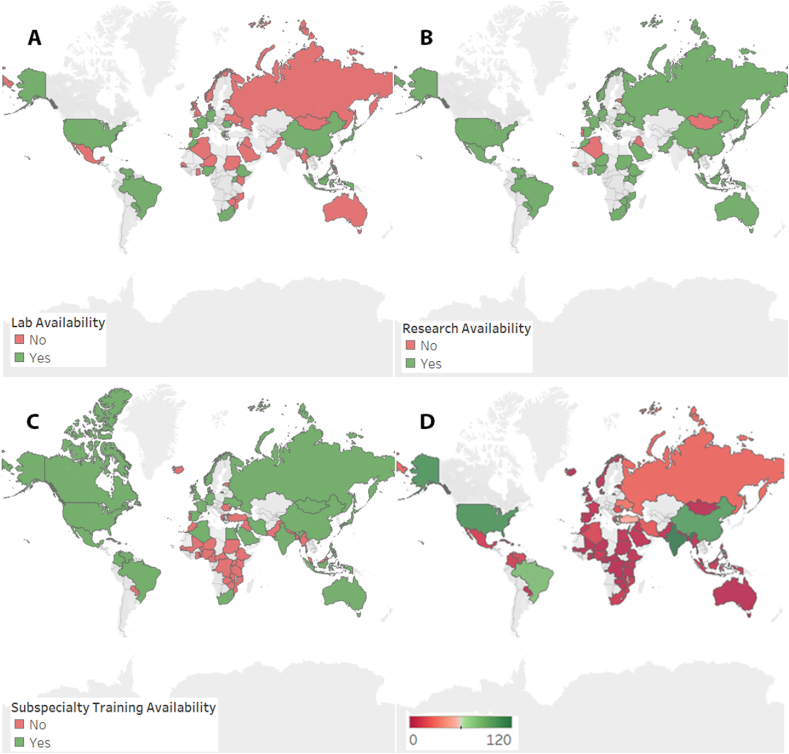
Data on research opportunities during training, availability of surgical skill or dissection labs, weekly work hours, and annual procedures were collected from participants who identified as neurosurgery trainees or recent graduates. 70.1% of survey respondents reported no availability of dissection and surgical skills labs in their home institutions. In regards to research, however, 76.9% of respondents reported that they did have research opportunities available to them. There was no apparent geographic distribution for the availability of dissection labs or research opportunities (Fig. 2). Of the countries represented, 45.6% were reported to have neurosurgical subspecialty training available. The majority of countries without subspecialty training were located in sub-Saharan Africa.
Fig. 2.
Geographic heatmaps demonstrating countries for which respondents reported the availability of dissection and surgical skills labs (A), availability of research opportunities (B), and availability of subspecialty neurosurgical training (C). The number of training programs per country is demonstrated in panel D, ranging from 0 (dark red) to 120 (dark green). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The number of weekly hours varied widely across countries with 43.1% of respondents reporting working >80 h per week (Table 2). The number of annual procedures performed at training programs also varied widely, with the greatest number of respondents (34.5%) reporting more than 500 procedures performed (Table 3).
Table 2.
Distribution of respondents who reported working the respective number of hours per week.
| Weekly Work Hours | Percent of Respondents |
|---|---|
| 0–10 | 0.9 |
| 10–20 | 3.4 |
| 20–30 | 0 |
| 30–40 | 2.6 |
| 40–50 | 11.2 |
| 50–60 | 14.7 |
| 60–70 | 12.1 |
| 70–80 | 12.1 |
| >80 | 43.1 |
Table 3.
Distribution of respondents who reported the respective number of annual procedures being performed at their training institution.
| Number of Annual Procedures | Percent of Respondents |
|---|---|
| <50 | 2.7 |
| 50–100 | 6.2 |
| 100–200 | 16.8 |
| 200–300 | 15 |
| 300–400 | 13.3 |
| 400–500 | 4.4 |
| >500 | 34.5 |
| Unsure | 7.1 |
3.3. Country statistics
Country specific data on the number of training programs, availability of subspecialty training, neurosurgery training length in years, number of trainees in a training program, gender demographics, average weekly work hours for trainees, average number of annual neurosurgical procedures performed at a training institution, availability of research opportunities, availability of dissection or surgical skills labs, competitiveness for entering neurosurgical training, and neurosurgical mentorship availability are reported in Table 4. The number of training programs in a country varied widely, from none to 120. Sub-Saharan Africa and South-East Asia had the fewest number of training programs per country (Fig. 2). Training length varied from 1 to 10 years, with the most common duration being 5 years. The size of training programs also varied widely, ranging from 2 to 70 trainees in a program. Men mostly outnumbered women in gender breakdown of trainees, with a mean percentage of 75% men to 25% women. Algeria and Spain were reported to have more women than men in their training programs, however.
Table 4.
Country specific data on number of training programs, availability of subspecialty training, neurosurgery training length in years, number of trainees in a training program (size), gender demographics, average weekly work hours for trainees, average number of annual neurosurgical procedures performed at a training institution, availability of research opportunities, availability of dissection or surgical skills labs, competitiveness for entering neurosurgical training on a scale of 1–10, and neurosurgical mentorship availability on a scale of 1–10. Some countries have more than one training pathway; different lengths of training are separated by a comma. Program size varied by program within a country, so presented values denote a range where more than one value was reported. LIC = low-income country; LMIC = lower-middle income country; UMIC = upper-middle income country; HIC = high-income country; SD = standard deviation.
| Country | Country Income Group | Number of Training Programs | Subspecialty Training Availability | Training Length | Program Size | Male:Female Ratio | Weekly Work Hours | Number of Annual Procedures | Research Availability | Lab Availability | Competitiveness (Mean ± SD) | Mentorship availability (Mean ± SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Algeria | LMIC | 13 | Yes | 5 | 3–9 | 1:3.5 | 50–60 | 200–300 | No | No | 2.7 ± 2.1 | 6.3 ± 1.2 |
| Australia | HIC | 1 | Yes | 6 | 70–80 | 200–300 | Yes | No | 10 | 6.5 ± 0.7 | ||
| Bangladesh | LMIC | 2 | No | 5 | >80 | 50–100 | No | No | 10 | 9 | ||
| Barbados | HIC | 0 | No | |||||||||
| Benin | LMIC | 0 | No | |||||||||
| Brazil | UMIC | 82 | Yes | 5 | 70–80 | >500 | Yes | Yes | 9.3 ± 0.6 | 5 ± 1 | ||
| Cameroon | LMIC | 1 | No | 7 ± 3.1 | 4.5 ± 3.7 | |||||||
| Canada | HIC | Yes | ||||||||||
| Cape Verde | LMIC | 0 | No | |||||||||
| Central African Republic | LIC | 0 | No | |||||||||
| China | UMIC | 100 | Yes | 4, 7 | 40 | 1:0.18 | 40–50 | >500 | Yes | Yes | 6 ± 1.4 | 6 ± 5.7 |
| Colombia | UMIC | 10 | Yes | 10 | 1 | |||||||
| Cuba | UMIC | 9 | Yes | 6 | 9 | |||||||
| Denmark | HIC | 4 | Yes | 5 | 4 | 1:0 | 30–40 | 100–200 | Yes | No | 9.5 ± 0.7 | 5 |
| DR Congo | LIC | 0 | No | 9.5 ± 0.7 | 2.3 ± 1.2 | |||||||
| Egypt | LMIC | 3 | Yes | 5 ± 5.7 | 7.5 ± 0.7 | |||||||
| Estonia | HIC | 1 | No | 5 | 50–60 | 300–400 | No | No | 4 | 7 | ||
| Ethiopia | LIC | 3 | No | 5 | 15 | 1:0.15 | 70–80 | >500 | Yes | Yes | 9.3 ± 1.2 | 4.3 ± 3.2 |
| France | HIC | 5 | Yes | 5 | 0–10 | >500 | Yes | Yes | 6.5 ± 5 | 7 | ||
| Germany | HIC | Yes | 7 | 40–50 | 50–100 | Yes | Yes | 4.5 ± 5 | 3 ± 2.8 | |||
| Ghana | LMIC | 2 | No | 4, 7, 8 | 5–6 | 1:0.22 | 60–70 | 100–200 | Yes | No | 7.4 ± 1.7 | 4 ± 1.9 |
| Greece | HIC | 18 | No | 9 | 60–70 | 100–200 | Yes | Yes | 1 | 3.5 ± 2.1 | ||
| Haiti | LIC | 1 | Yes | 10 | 2 | |||||||
| Hungary | HIC | |||||||||||
| Iceland | HIC | 0 | No | |||||||||
| India | LMIC | 120 | Yes | 9.7 ± 0.6 | 4.3 ± 2.9 | |||||||
| Indonesia | UMIC | 8 | Yes | 5, 6 | 9–50 | 1:0.12 | >80 | 100–200 | Yes | Yes | 7.7 ± 2 | 6.5 ± 2.5 |
| Iran | UMIC | 20 | Yes | 8 | 10 | |||||||
| Iraq | UMIC | 3 | No | 5 | 15 | 10–20 | >500 | No | No | 2.1 | 1.4 | |
| Israel | HIC | 10 | Yes | 6 | 11 | 1:0.37 | >80 | Yes | No | 9 | 6 | |
| Japan | HIC | Yes | 5 | 50–60 | Yes | Yes | ||||||
| Kenya | LMIC | 2 | No | 6 | 4 | 1:0 | >80 | 200–300 | Yes | No | 7.4 ± 3.4 | 3.8 ± 1.9 |
| Lebanon | UMIC | 5 | Yes | |||||||||
| Malaysia | UMIC | 1 | No | 4 | >80 | 100–200 | Yes | Yes | 9.3 ± 1 | 4.5 ± 2.6 | ||
| Mali | LIC | 1 | No | |||||||||
| Malta | HIC | 0 | No | |||||||||
| Mauritius | HIC | 0 | No | |||||||||
| Mexico | UMIC | 10 | Yes | 6 | 10–20 | 200–300 | Yes | No | 8 | 5.5 ± 2.1 | ||
| Mongolia | LMIC | 1 | Yes | 1 | 60–70 | 300–400 | No | No | 3.3 ± 2.1 | 4.7 ± 2.5 | ||
| Montserrat | HIC | 0 | No | |||||||||
| Morocco | LMIC | 5 | No | 5 | 27 | 1:0.35 | 70–80 | 400–500 | Yes | Yes | 8.5 ± 2.1 | 5 ± 4.2 |
| Mozambique | LIC | 7 | No | 5 | 6 | 1:0.2 | 60–70 | >500 | Yes | No | 5 | 5 |
| Myanmar | LMIC | 3 | No | 8 | 70 | 1:0.37 | >80 | 200–300 | Yes | No | 5 | 1 |
| Nepal | LMIC | 2 | No | |||||||||
| Niger | LIC | 1 | No | 5 | 11 | 1:0.22 | 50–60 | 50–100 | Yes | No | 6 | 8 |
| Nigeria | LMIC | 6 | No | 4, 6, 7, 10 | 6–17 | 1:0.06 | >80 | 300–400 | Yes | Yes | 9 ± 1.3 | 3.8 ± 1.7 |
| Norway | HIC | 4 | Yes | 6 | 9 | 1:0.5 | 50–60 | 200–300 | Yes | No | 8 | 4 |
| Pakistan | LMIC | 2 | No | 3, 5 | 2–16 | 1:0.22 | >80 | >500 | Yes | No | 7.1 ± 2.3 | 3.6 ± 2.2 |
| Paraguay | UMIC | 3 | No | 5 | 50–60 | 300–400 | Yes | Yes | 6 | 3 | ||
| Philippines | LMIC | 10 | Yes | 5, 6 | 3–12 | 1:0.5 | >80 | >500 | Yes | No | 9.4 ± 1.2 | 5.3 ± 2.6 |
| Portugal | HIC | 11 | No | 6 | 7 | 1:0.75 | 60–70 | >500 | No | No | 8 | 8 |
| Romania | HIC | 15 | No | 6 | 50–60 | <50 | Yes | Yes | 6.3 ± 1.5 | 3 ± 1.7 | ||
| Russia | UMIC | 25 | Yes | 2, 5 | 30–40 | 100–200 | Yes | No | 6.8 ± 2.4 | 3.6 ± 1.7 | ||
| Rwanda | LIC | 1 | Yes | |||||||||
| Saudi Arabia | HIC | 3 | Yes | 6 | 39 | 60–70 | 50–100 | Yes | No | 7 | 4 | |
| Senegal | LMIC | 1 | No | 1, 5 | 42 | 1:0.27 | 60–70 | 100–200 | No | No | 3 ± 2.8 | 2.5 ± 2.1 |
| South Africa | UMIC | 7 | Yes | 5 | 50–60 | 300–400 | Yes | Yes | 9 ± 1.4 | 5.5 ± 0.7 | ||
| Spain | HIC | 1 | Yes | 5 | 5 | 1:1.5 | 40–50 | 200–300 | Yes | Yes | 10 | 4 |
| Sudan | LIC | 1 | No | 6 | 25–36 | 1:0.64 | >80 | 300–400 | Yes | No | 8.2 ± 1.6 | 4.2 ± 2.1 |
| Tanzania | LMIC | 1 | No | |||||||||
| Togo | LIC | 0 | No | |||||||||
| Turkey | UMIC | 50 | No | 3 | 9 | |||||||
| Uganda | LIC | 2 | No | 4, 7 | 3–13 | 1:0.14 | 10–20 | >500 | Yes | Yes | 9 ± 2 | 4 ± 4.2 |
| UK | HIC | 1 | Yes | 8 | 40–50 | 200–300 | Yes | No | 9.3 ± 1.2 | 5.7 ± 2.1 | ||
| Ukraine | LMIC | 30 | Yes | 6 | 5 | 1:0.67 | 50–60 | >500 | Yes | No | 8.7 ± 2.3 | 3 ± 1.7 |
| USA | HIC | 105 | Yes | 7 | 3–11 | 1:0.2 | >80 | >500 | Yes | Yes | 9.6 ± 0.5 | 6.9 ± 2 |
| Venezuela | UMIC | 13 | Yes | 5 | >80 | >500 | Yes | Yes | 9 | 1 | ||
| Zambia | LMIC | 1 | No | |||||||||
| Zimbabwe | LMIC | 1 | No | 5 | 40–50 | Yes | No | 9 | 9 |
3.4. Comparative analysis
In comparing LMICs to HICs, there was no significant difference found in ranked competitiveness for entering neurosurgical training, with a mean of 7.8 on a scale of 1–10 amongst both LMIC and HIC respondents (p = 0.473). There was also no significant difference in ranked availability of mentorship, with LMIC respondents reporting a mean of 4.7 on a scale of 1–10 compared to 5.4 reported amongst HIC respondents (p = 0.162). In addition, no significant difference was found between LMIC and HIC respondents for annual number of procedures (p = 0.122), availability of research opportunities (p = 0.692), or availability of surgical skill or dissection labs (p = 0.262) (Table 5). A significant difference was found in weekly work hours (p = 0.016) and subspecialty training availability (p = 0.001) between LMICs and HMICs. HIC respondents reported on average fewer weekly work hours than LMIC respondents. Subspecialty training was reported to be available more often by HIC respondents than LMIC respondents.
Table 5.
Comparison between LMICs & HICs. Competitiveness and mentorship availability were graded on a scale of 1–10 with increasing values denoting increasing competitiveness and mentorship availability. Weekly work hours was an ordinal variable with the following values: 1 = 0–10, 2 = 10–20, 3 = 20–30, 4 = 30–40, 5 = 40–50, 6 = 50–60, 7 = 60–70, 8 = 70–80, 9=>80. Number of annual procedures was an ordinal variable with the following values: 1=<50, 2 = 50–100, 3 = 100–200, 4 = 200–300, 5 = 300–400, 6 = 400–500, 7=>500. Research availability, dissection lab availability, and subspecialty training availability were all categorical variables with 1 = yes and 2 = no.
| Variable | Income Group | Mean (SD) | Mean Rank | Sum of Ranks | Mann-Whitney U | p-value |
|---|---|---|---|---|---|---|
| Competitiveness | LMIC | 7.8 (2.4) | 92.8 | 14568 | 2165 | 0.473 |
| HIC | 7.8 (3.0) | 100.3 | 3010 | |||
| Mentorship Availability | LMIC | 4.7 (2.6) | 91.2 | 14408 | 1847 | 0.162 |
| HIC | 5.4 (2.2) | 106.5 | 2983 | |||
| Weekly Work Hours | LMIC | 7.5 (1.9) | 61.8 | 5931 | 645 | 0.016 |
| HIC | 6.5 (2) | 42.8 | 855 | |||
| Number of Annual Procedures | LMIC | 5.3 (1.9) | 59 | 5659.5 | 628.5 | 0.122 |
| HIC | 4.4 (2.3) | 46 | 781.5 | |||
| Research Availability | LMIC | 1.3 (0.5) | 59.4 | 5763 | 930 | 0.692 |
| HIC | 1.2 (0.4) | 57 | 1140 | |||
| Dissection Lab Availability | LMIC | 1.8 (0.5) | 60.3 | 5846.5 | 846.5 | 0.262 |
| HIC | 1.7 (0.6) | 52.8 | 1056.5 | |||
| Subspecialty Training Availability | LMIC | 1.8 (0.7) | 104 | 16946.5 | 1798.5 | 0.001 |
| HIC | 1.3 (0.5) | 71.5 | 2359.5 |
4. Discussion
Neurosurgical training continues to be a competitive and difficult undertaking around the world. The long training duration, immense library of knowledge, and technical expertise necessary to become a neurosurgeon already stand as barriers to increasing the neurosurgical workforce. These standards of excellence cannot be diminished, but there exist a multitude of other addressable barriers that limit the equitable training of neurosurgeons. Our study provides a snapshot of the unmet needs in neurosurgical training around the world and can inform efforts to improve equitable access to training in order to address the global neurosurgical workforce shortage.
4.1. Availability of neurosurgical training
Although our study is not a comprehensive accounting of all neurosurgical training programs around the world, we found an unsurprising lack of neurosurgical training programs in LMICs and smaller island nations, including Iceland. Sub-Saharan Africa and South-East Asia had the fewest number of training programs per country. Due to this dearth of training opportunities, many survey respondents, most from LMICs, reported travelling to other countries both for medical school education and neurosurgical training. We did not assess the various reasons for this finding in our study; however, even if training programs are present in LMICs, training positions in HICs are still highly sought after, contributing to brain drain (Scheitler et al., 2020).
In addition, we found that 54.4% of countries represented in our study did not have neurosurgical subspecialty training available. LMICs were less likely than HICs to have subspecialty training available (p = 0.001), with the largest deficit in sub-Saharan Africa. This finding is consistent with a recent study where 40% of respondents from LMICs reported lack of adequate subspecialty exposure (Deora et al., 2020). The field of neurosurgery has witnessed an increase in subspecialization due to advanced technology, need for more expertise, and advances in minimally invasive procedures. In LMICs, the low workforce density and lack of necessary equipment can make it difficult to have subspecialty practices; however, studies have shown that the majority of the unmet neurosurgical needs in these countries are head injuries (Dewan et al., 2018). Subsequently, the scale up of the neurosurgical workforce and the skill-set they should possess should match the disease burden. These countries may want to develop two tracks for training - a shorter and more limited training focused on neurotrauma and general neurosurgical skills to manage the most urgent and common conditions, and a longer and more specialized training in the care of more complex conditions, scaled up to match the capabilities and the capacities of the neurosurgical system of the country.
This finding underscores the importance of strategic investment in neurosurgical health system development by local governments, supplemented by country-led north-south (between HICs and LMICs) and south-south (between LMICs) collaborations for specialized training of the neurosurgical workforce (Fuller et al., 2015). One confounding factor in these findings is that advanced neurosurgical training in LMICs can often focus on technical skills such as endoscopic training rather than the traditional Western subspecialty categories. These advanced training opportunities may not have been captured by our survey. They also encompass a training dynamic that must be thoroughly understood when developing training partnerships.
4.2. Operative volume
Sufficient surgical volume and experience is also critical for neurosurgical training. The COVID-19 pandemic demonstrated the importance of this as many institutions were forced to cancel elective surgeries and restructure training (Aljuboori et al., 2021; Wittayanakorn et al., 2020). In our study, there was no difference between HICs and LMICs in regards to the annual number of procedures their institutions performed, with only 34.5% of respondents reporting more than 500 procedures annually. Previous research has suggested 250–300 cases per year per trainee for proper training (Reulen and Marz, 1998), suggesting that approximately ⅔ of respondents were in programs that could not support more than two total trainees. Based on these recommendations accreditation protocols often require training centers to have a minimum of 200 cases per year; however, approximately ¼ of our respondents reported less than 200 cases per year being performed at their institutions. This can be a significant barrier to increasing training as neurosurgical capacity as case volume must first be increased; this requires investment in not just neurosurgeons and operative equipment but multiple other facets such as radiology, anesthesiology, and critical care (WFNS Foundation, 2020). It is important to note that the COVID-19 pandemic may have affected these numbers depending on which years the respondents were basing their data.
4.3. Work hours
There is significant controversy regarding the effect of work-hour restrictions on neurosurgical training and patient care (Norby et al., 2014). We found wide variability across countries in regards to trainee weekly work hours, with 43.1% of respondents working more than >80 h per week. A small cohort (6.9%) of respondents reported working less than 40 h a week, and 0.9% reported only 0–10 h; most contracts for service or training positions have a minimum 40–48 h work week, and so the explanation for these lower work hours is unclear. There was a significant difference in weekly work hours between LMICs and HMICs (p = 0.016), with LMIC trainees working on average more hours than their HIC counterparts. This may be due in part to the work hour restrictions of 80 and 48 h per week in the United States and Europe respectively. (Accreditation Council for Graduate Medical Education; Stienen et al., 2016b) With few support staff in hospitals across LMICs, trainees may spend the majority of their time on administrative and logistical responsibilities instead of their core neurosurgery training. Thus, the increased work hours do not necessarily translate to more educationally beneficial experiences. It will be important for future studies to assess more specific parameters such as case logs, number of cases performed independently, and hours spent in the neurosurgery clinic and operating room.
4.4. Access to mentorship
Mentors are critical to the personal and professional development of neurosurgery trainees, teaching both technical and non-technical skills (Akhigbe et al., 2017). Historically, surgical training has been based on apprenticeship (Halsted, 1904), but this model has diminished in use as neurosurgery has grown, making mentorship relations even more crucial for the development of trainees. Our study found that mentorship availability in neurosurgery was ranked as just average, with a mean score of 4.8 ± 2.6 out of 10 reported by respondents. This deficit in mentorship can be detrimental for overall workforce training as well as equitable representation of marginalized minorities within neurosurgery, as demonstrated by lack of female mentorship being a major obstacle to women choosing spine surgery as their specialty, as studies have shown that early mentorship is a key indicator that influences women to choose a surgical specialty (Falavigna et al., 2021; Hemal et al., 2021). Interestingly, we found no difference in reported availability of mentors in LMICs compared to HICs. Nonetheless, although there are efforts to improve mentorship availability in HICs, in many LMICs, small neurosurgical workforces can preclude these efforts. International partnerships can help ameliorate this deficit (Research EoH, 2014); however, differences in cultural and hierarchical structures can make these relationships difficult (Warner, 2002).
4.5. Dissection labs
A significant number of our respondents (70.1%) reported no availability of dissection and surgical skills labs in their home institutions, with no difference between HICs and LMICs. This is consistent with the findings of another recent global study that found only 17.8% of trainees had access to cadaveric training courses, and represents a significant barrier to neurosurgical training (Gnanakumar et al., 2020). With the increase in the utilization of simulation in surgical pre-operative planning and intraoperative lesion location, it has become imperative for training programs to develop surgical skills labs in order to equip trainees with the necessary tools to effectively hone their surgical skills and anatomical knowledge (Stienen et al., 2016c). While efforts have been made by many programs and organizations in HICs to incorporate a dissection curriculum (Harrop et al., 2013; Liu et al., 2015), the results are not similar in LMICs. While this finding might be due to lack of institutional funding and resource availability, LMICs institutions such as the All India Institute of Medical Sciences (AIIMS) have been able to develop simulation labs that have shown promising results using limited resources (Suri et al., 2014, 2016).
4.6. Research
Although research opportunities were reported to be much more accessible than dissection labs, nearly a quarter of survey participants reported not having access to research opportunities. This provides an opportunity for improvement, as locally led quality research output has been linked to successes in overcoming global health challenges (Dye et al., 2013). Although our study found no difference in the availability of research opportunities between HICs and LMICs, research capacity, output, and representation has been limited in LMICs, as they represent only 4.5% of neurosurgery research output globally despite comprising 46% of the global population (Servadei et al., 2019). These disparities between HICs and LMICs are perhaps due to a lack of investment in building local research capacity. While there is availability of research opportunities, there are still several challenges - limited experience, lack of infrastructure, and minimal funding. In addition, in those cases where HIC actors have developed research collaborations to help build research capacity, partnership and authorship in articles may not be equitable (Uthman et al., 2013). Thus, research capacity building efforts must focus on education and equitable partnerships between researchers from HICs and LMICs (Nthumba et al., 2021).
4.7. Women in neurosurgery
Our survey respondents’ gender demographics closely resembled the reported gender breakdown of training programs, with a mean percentage of 75% men and 25% women. This may simply be a reflection of the percentage of female respondents; however, this finding was similar to another recent study that found approximately 80% of trainees globally to be male without a significant difference between HICs and LMICs (Gnanakumar et al., 2020). This is a promising finding for equity, as the number of practicing neurosurgeons in the United States who are women was only 3% in 2008 (Burkhardt et al., 2010b). Variations will exist between countries and even different training centers within a country, but the overall trend is promising. This trend will likely only continue as more women in neurosurgery will lead to greater mentorship for female medical students and increase the likelihood that they will enter neurosurgical training (Hemal et al., 2021).
4.8. Limitations
Our study provides a snapshot of neurosurgical training around the world, with 69 different countries represented and 83% of responses from LMICs. There are multiple limitations to the study, however. Although we have a broad distribution and representation of countries around the world, the overall size of the study is small and it is not a complete picture. In addition, the number of respondents from each individual country was small, limiting the representativeness of the responses. Sampling bias exists as countries with no or limited neurosurgical training opportunities, especially among LMICs, were likely not captured. The barriers may be greater in these countries but are still likely similar to those we found in our sample population. In addition, we did not clarify with survey respondents whether they had applied for a training program unsuccessfully or were unable to pursue training for any reason. This contributes further to sampling bias, as we likely did not capture those applicants most affected by barriers.
It is unclear if participants were providing data from their country or from their own individual experience. In addition, as this is a survey study, the individual responses are the views of the respondents and the veracity of the reported findings is unclear. Although we attempted to clarify some contradicting responses, it is difficult to independently verify the responses. Furthermore, there was variability amongst respondents in their understanding of questions and their answers, such as the United Kingdom reported as having one training program due to the single national system for applying to residency, which limits the interpretability of the results.
5. Conclusion
Our study highlights the need for a deliberate focus on designing and implementing both short and long term strategic goals in tackling barriers to access to neurosurgical training. The appropriate provision of resources can provide aspiring and current trainees the tools needed to successfully matriculate into and complete a training program. In order to bridge the gap in the provision of equitable neurosurgical care across the globe, institutions and stakeholders need to develop collaborative efforts and invest in appropriate infrastructure to address these barriers to neurosurgical training and education.
Declaration of competing interest
We declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere.
There was no conflict of interest associated with this manuscript. As a corresponding author, I confirm that The manuscript has been read and approved for submission by all contributing authors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bas.2022.100900.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Accreditation Council for Graduate Medical Education: Report of the ACGME Work Group on Resident Duty Hours. Premier, Inc. https://www.premierinc.com/safety/safety-share/08-02_downloads/03_wkgreport_602.pdf.
- Akhigbe T., Zolnourian A., Bulters D. Mentoring models in neurosurgical training: review of literature. J. Clin. Neurosci. 2017;45:40–43. doi: 10.1016/j.jocn.2017.07.025. [DOI] [PubMed] [Google Scholar]
- Aljuboori Z.S., Young C.C., Srinivasan V.M., et al. Early effects of COVID-19 pandemic on neurosurgical training in the United States: a case volume Analysis of 8 programs. World Neurosurg. 2021;145:e202–e208. doi: 10.1016/j.wneu.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhardt J.K., Zinn P.O., Bozinov O., Colen R.R., Bertalanffy H., Kasper E.M. Neurosurgical education in Europe and the United States of America. Neurosurg. Rev. 2010;33(4):409–417. doi: 10.1007/s10143-010-0257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhardt J.K., Zinn P.O., Bozinov O., Colen R.R., Bertalanffy H., Kasper E.M. Neurosurgical education in Europe and the United States of America. Neurosurg. Rev. 2010;33(4):409–417. doi: 10.1007/s10143-010-0257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debas H.T., Donkor P., Gawande A., Jamison D.T., Kruk M.E., Mock C.N., editors. third ed. vol. 1. The International Bank for Reconstruction and Development/The World Bank; Washington (DC): April 2, 2015. (Essential Surgery: Disease Control Priorities). [PubMed] [Google Scholar]
- Deora H., Garg K., Tripathi M., Mishra S., Chaurasia B. Residency perception survey among neurosurgery residents in lower-middle-income countries: grassroots evaluation of neurosurgery education. Neurosurg. Focus. 2020 Mar 1;48(3):E11. doi: 10.3171/2019.12.FOCUS19852. 10.3171/2019.12.FOCUS19852. PMID: 32114547. [DOI] [PubMed] [Google Scholar]
- Dewan M.C., Rattani A., Fieggen G., et al. Global neurosurgery: the current capacity and deficit in the provision of essential neurosurgical care. Executive Summary of the Global Neurosurgery Initiative at the Program in Global Surgery and Social Change [published online ahead of print, 2018 Apr 1] J. Neurosurg. 2018:1–10. doi: 10.3171/2017.11.JNS171500. [DOI] [PubMed] [Google Scholar]
- Dias M.S., Sussman J.S., Durham S., Iantosca M.R. Perceived benefits and barriers to a career in pediatric neurosurgery: a survey of neurosurgical residents. J. Neurosurg. Pediatr. 2013;12(5):422–433. doi: 10.3171/2013.7.PEDS12597. [DOI] [PubMed] [Google Scholar]
- Dye C., Boerma T., Evans D., et al. World Health Organisation; Geneva: 2013. The World Health Report 2013: Research for Universal Health Coverage. [Google Scholar]
- Falavigna A., Ramos M.B., de Farias F.A.C., et al. Perception of gender discrimination among spine surgeons across Latin America: a web-based survey [published online ahead of print, 2021 Apr 11] Spine J. 2021;S1529–9430(21) doi: 10.1016/j.spinee.2021.04.009. 00182-0. [DOI] [PubMed] [Google Scholar]
- Franzen S.R., Chandler C., Lang T. Health research capacity development in low and middle income countries: reality or rhetoric? A systematic meta-narrative review of the qualitative literature. BMJ Open. 2017;7(1) doi: 10.1136/bmjopen-2016-012332. Published 2017 Jan 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller A., Tran T., Muhumuza M., Haglund M.M. Building neurosurgical capacity in low and middle income countries. eNeurologicalSci. 2015;3:1–6. doi: 10.1016/j.ensci.2015.10.003. Published 2015 Nov 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2016 Neurology Collaborators Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–480. doi: 10.1016/S1474-4422(18)30499-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnanakumar S., Abou El Ela Bourquin B., Robertson F.C., et al. The world federation of neurosurgical Societies young neurosurgeons survey (Part I): demographics, resources, and education. World Neurosurg X. 2020;8 doi: 10.1016/j.wnsx.2020.100083. Published 2020 May 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halsted W. The training of the surgeon. Bull. Johns Hopkins Hosp. 1904;15:267–275. [Google Scholar]
- Harris Paul A., Taylor Robert, Thielke Robert, Payne Jonathon, Gonzalez Nathaniel, Conde Jose G. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 2009 Apr;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrop J., Lobel D.A., Bendok B., Sharan A., Rezai A.R. Developing a neurosurgical simulation-based educational curriculum: an overview. Neurosurgery. 2013;73(Suppl. 1):25–29. doi: 10.1227/NEU.0000000000000101. [DOI] [PubMed] [Google Scholar]
- Hemal K., Reghunathan M., Newsom M., Davis G., Gosman A. Diversity and inclusion: a review of effective initiatives in surgery [published online ahead of print, 2021 Apr 17] J. Surg. Educ. 2021;S1931–7204(21) doi: 10.1016/j.jsurg.2021.03.010. 00063-5. [DOI] [PubMed] [Google Scholar]
- Henderson F., Jr., Abdifatah K., Qureshi M., et al. The College of surgeons of East, Central, and southern Africa: successes and challenges in standardizing neurosurgical training. World Neurosurg. 2020;136:172–177. doi: 10.1016/j.wneu.2020.01.084. [DOI] [PubMed] [Google Scholar]
- Hoddinott S.N., Bass M.J. The dillman total design survey method. Can. Fam. Physician. 1986;32:2366–2368. [PMC free article] [PubMed] [Google Scholar]
- Kato Y., Liew B.S., Sufianov A.A., et al. Review of global neurosurgery education: horizon of neurosurgery in the developing countries [published correction appears in Chin Neurosurg J. 2020 Aug 24;6:30] Chin Neurosurg J. 2020;6:19. doi: 10.1186/s41016-020-00194-1. Published 2020 May 19. doi:10.1186/s41016-020-00194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley K., Clark B., Brown V., Sitzia J. Good practice in the conduct and reporting of survey research. Int. J. Qual. Health Care. 2003;15(3):261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- Lescano A.G., Cohen C.R., Raj T., et al. Strengthening mentoring in low- and middle-income countries to advance global health research: an overview. Am. J. Trop. Med. Hyg. 2019;100(1_Suppl. l):3–8. doi: 10.4269/ajtmh.18-0556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang K.E., Bernstein I., Kato Y., Kawase T., Hodaie M. Enhancing neurosurgical education in low- and middle-income countries: current methods and new advances. Neurol. Med.-Chir. 2016;56(11):709–715. doi: 10.2176/nmc.ra.2016-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.K., Kshettry V.R., Recinos P.F., Kamian K., Schlenk R.P., Benzel E.C. Establishing a surgical skills laboratory and dissection curriculum for neurosurgical residency training. J. Neurosurg. 2015;123(5):1331–1338. doi: 10.3171/2014.11.JNS14902. [DOI] [PubMed] [Google Scholar]
- Norby K., Siddiq F., Adil M.M., Haines S.J. The effect of duty hour regulations on outcomes of neurological surgery in training hospitals in the United States: duty hour regulations and patient outcomes. J. Neurosurg. 2014;121(2):247–261. doi: 10.3171/2014.4.JNS131191. [DOI] [PubMed] [Google Scholar]
- Nthumba P.M., Newton M.W., Gathuya Z. Global surgery in the 21st century: the voice from Africa - we need a new model. Paediatr. Anaesth. 2021;31(5):510–512. doi: 10.1111/pan.14162. [DOI] [PubMed] [Google Scholar]
- Nulty D.D. The adequacy of response rates to online and paper surveys: what can be done? Assess Eval. High Educ. 2008;33(3):301–314. doi: 10.1080/02602930701293231. [DOI] [Google Scholar]
- Punchak M., Mukhopadhyay S., Sachdev S., et al. Neurosurgical care: availability and access in low-income and middle-income countries. World Neurosurg. 2018;112:e240–e254. doi: 10.1016/j.wneu.2018.01.029. [DOI] [PubMed] [Google Scholar]
- Qayumi K. Surgical skills lab: a hub for competency training. J. Invest. Surg. 2010;23(1):48–56. doi: 10.3109/08941930903469391. [DOI] [PubMed] [Google Scholar]
- Research EoH . 2014. Seven Principles for Strengthening Research Capacity in Low- and Middle Income Countries: Simple Ideas in a Complex World. TDR/ESSENCE/2.14. [Google Scholar]
- Reulen H.J., Marz U. 5 years' experience with a structured operative training programme for neurosurgical residents. Acta Neurochir. 1998;140:1197–1203. doi: 10.1007/s007010050237. [DOI] [PubMed] [Google Scholar]
- Scheitler K.M., Lu V.M., Carlstrom L.P., Graffeo C.S., Perry A., Daniels D.J., Meyer F.B. Geographic distribution of international medical graduate residents in U.S. Neurosurgery training programs. World Neurosurgery. 2020;137:e383–e388. doi: 10.1016/j.wneu.2020.01.201. [DOI] [PubMed] [Google Scholar]
- Servadei F., Tropeano M.P., Spaggiari R., et al. Footprint of reports from low- and low- to middle-income countries in the neurosurgical data: a study from 2015 to 2017. World Neurosurg. 2019;130:e822–e830. doi: 10.1016/j.wneu.2019.06.230. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Netuka D., Demetriades A.K., et al. Neurosurgical resident education in Europe--results of a multinational survey. Acta Neurochir. 2016;158(1):3–15. doi: 10.1007/s00701-015-2632-0. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Netuka D., Demetriades A.K., et al. Working time of neurosurgical residents in Europe--results of a multinational survey. Acta Neurochir. 2016;158(1):17–25. doi: 10.1007/s00701-015-2633-z. [DOI] [PubMed] [Google Scholar]
- Stienen M.N., Netuka D., Demetriades A.K., et al. Residency program trainee-satisfaction correlate with results of the European board examination in neurosurgery. Acta Neurochir. 2016;158(10):1823–1830. doi: 10.1007/s00701-016-2917-y. [DOI] [PubMed] [Google Scholar]
- Suri A., Roy T.S., Lalwani S., Deo R.C., Tripathi M., Dhingra R., Bhardwaj D.N., Sharma B.S. Practical guidelines for setting up neurosurgery skills training cadaver laboratory in India. Neurol. India. 2014;62:249–256. doi: 10.4103/0028-3886.136897. [DOI] [PubMed] [Google Scholar]
- Suri A., Patra D.P., Meena R.K. Simulation in neurosurgery: past, present, and future. Neurol. India. 2016;64(3):387–395. doi: 10.4103/0028-3886.181556. [DOI] [PubMed] [Google Scholar]
- The World Bank. Data: Country Classification, Low-Income Countries. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519.
- Uthman O.A., Okwundu C.I., Wiysonge C.S., Young T., Clarke A. Citation classics in systematic reviews and meta-analyses: who wrote the top 100 most cited articles? PLoS One. 2013;8(10) doi: 10.1371/journal.pone.0078517. Published 2013 Oct 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner N. Internationalization and Cultural Diversity Cultural Issues Related to HEI Administration and Hierarchy: an African Case Study. IEASA Conference. 2002. http://www.ushepia.uct.ac.za/sites/default/files/image_tool/images/322/Publications/About_USHEPiA/Cultural-Issues-related-to-Higher-Education-Institutions-Administration-and-Hierarchy-An-African-Case-StudyNan-Warner.pdf Available at: [Google Scholar]
- WFNS Foundation . World Federation of Neurosurgical Societies; 1 October 2020. Guideline for the Certification of Post-Graduate Training Centers.https://www.wfns.org/WFNSData/Document/Guideline-for-the-Certification-of-Post-Graduate-Training-Centers-08102020.pdf Available at: [Google Scholar]
- Wittayanakorn N., Nga V.D.W., Sobana M., Bahuri N.F.A., Baticulon R.E. Impact of COVID-19 on neurosurgical training in Southeast Asia. World Neurosurg. 2020;144:e164–e177. doi: 10.1016/j.wneu.2020.08.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.