Abstract
Purpose
To compare the outcomes of arthroscopic anterior Bankart repair with and without associated postero-inferior capsulolabral repair as treatment of anterior glenohumeral instabiliy at minimun 10 year follow-up.
Methods
A retrospective comparative study including patients who underwent arthroscopic anterior Bankart repair to treat anterior glenohumeral instability with glenoid bone-loss < 15% between January 2000 and February 2010 was performed. Outcomes were reported as recurrence rate, type of recurrence (dislocation or subluxation), need for revision surgery, range of motion, complications, and functional status. Outcomes were compared depending on whether a postero-inferior capsulolabral repair was added to the anterior Bankart repair.
Results
70 shoulders [59 males, mean age 28.2 (range 14–56), mean follow-up 146.1 (range 120–208) months] were included. Recurrence occurred in 9 cases (12.8%), including 3 dislocations and 6 subluxations. Revision surgery was needed in 8 (11.4%). Mean Rowe score improved from 29.7 (11.6) preoperatively to 87.1 (12.3) postoperatively. 83.3% returned to previous sports activities. Mean forward flexion changed from 173.5° (19.2) to 168.4º(10.4) (P < 0.01), external rotation from 81.4° (18) to 75.7° (10.5) (P < 0.01), and internal rotation decreased from 66.2% reaching T12 to 14.1% (P < 0.01). Addition of postero-inferior capsulolabral repair did not influence any of the outcomes significantly.
Conclusion
Postero-inferior capsulolabral repair added to anterior Bankart repair as treatment of anterior glenohumeral instability in abscence of significant glenoid bone-loss did not influence the outcomes in terms of recurrence, range of motion, return to sports, or functional status, compared to isolated anterior Bankart repair at 12.2 year follow-up.
Level of Evidence
Level III.
Keywords: Arthroscopy, Bankart repair, Shoulder instability, Redislocation, Outcomes, Posterior plication
Introduction
Anterior shoulder instability is a common and potentially disabling injury. Surgical treatment is often recommended, specially in young active patients. In recent years, arthroscopic repair of the anterior labrum-capsule complex (also known as Bankart repair) has emerged as the procedure of choice to treat anterior instability in absence of glenoid bone-loss in more than 85% of the cases [1, 2].
Arthroscopic Bankart repair using suture anchors has shown similar outcomes compared to open Bankart repair in terms of recurrence and functional recovery, with a lower rate of complications [3–5]. Studies with more than 10 year follow-up confirm that arthroscopic Bankart repair is safe and yields good functional results [6–10]. However, failure rates remain high, ranging from 18 to 35% [11]. This finding might be secondary to several reasons: less-developed techniques when the procedure started to be implemented, surgeons less familiarized with the technique, or less-precise indications for Bankart repair. In an attempt to improve the outcomes, other soft-tissue-repairing procedures associated with the arthroscopic anterior Bankart repair, like rotator interval closures [12]; infraspinatus myo-tenodesis to the Hill-Sachs defect [13]; or postero-inferior capsular plications [7], have been described.
The rationale of repairing the postero-inferior labrum-capsule complex in an isolated anterior instability is that, attending to the “circle injury” concept, a tear of the labrum and the capsuloligamentous complex at the anterior glenoid rim might be accompanied by injuries on the opposite site of the shoulder [14]. These injuries may comprise a progressive deformity of the joint capsule. As a consequence, posterior capsular plications and labrum repairs have been proposed by several authors as an adjacent procedure to anterior Bankart repair in an attempt to repair all the injured structures [15, 16], although the data about its efectiveness at long-term are scarce.
The goal of this study is to compare the outcomes of the arthroscopic anterior Bankart repair with and without associated postero-inferior capsulolabral repair as treatment of isolated anterior instabiliy in terms of recurrence, functional status, return to sports, and range of motion, at minimun 10 year follow-up. The null-hypothesis is that outcomes would be similar between both groups.
Materials and Methods
For the current study, a total of 121 consecutive patients subjected to arthroscopic Bankart repair between January 2000 and February 2010 were reviewed. Data regarding preoperative clinical history and surgical procedure were obtained from an electronic database. Sports involvement, type of sports, and competitive level was achieved.
Inclusion/Exclusion Criteria
Patients with recurrent (at least 2 episodes), postraumatic unidirectional antero-inferior glenohumeral instability, subjected to arthroscopic Bankart repair were included in the study protocol.
Exclusion criteria were considered the following: posterior or multidirectional (defined as instability in more than one direction) shoulder instability, concomitant rotator cuff tears, glenoid bone-loss ≥ 15%, large Hill–Sachs injuries requiring additional procedures like remplissage, or an intact posterior capsulolabral complex. Patients subjected to open Bankart repair or bone-grafting procedures were also excluded. A previous Bankart repair, as well as concomitant SLAP tears were not considered as exclusion criteria.
Surgical Procedure
Surgery was performed in every case by the senior surgeon. Patients were placed in lateral decubitus position with the arm sustained by a longitudinal traction device at approximatelly 70° of abduction and 10° of forward flexion. A posterior portal was used to explore the glenohumeral joint. Two portals located at the rotator interval were then placed and used as viewing and working portals. First, postero-inferior labrum injuries were evaluated from the anterior portals, and repaired when considered necessary with XCEL (Stryker Endoscopy, Kalamazoo, MI) suture anchors. Posterior repair was performed at the discretion of the surgeon based mainly on preoperative clinical findings and training/philosophy in management. First, posterior anchor was placed at 7 o’clock on right shoulders and was tightened first. Posterior repair progressed proximal if more extensive lessions were noticed. Anterior Bankart repair was then performed using XCEL suture anchors placed on the anterior glenoid rim. At least 3 anchors were routinely placed. Capsular plications were always added to the anterior Bankart repair. A mean of 4.5 anchors (range 3–7) was used. Patients who required concomitant SLAP repairs (n = 19) were those who needed 5 or more anchors.
Rehabilitation Protocol
All shoulders were placed on a sling after surgery for 4 weeks. Pendular exercises were recommended twice a-day after thorough teaching of the exercise. At the fifth week, the sling was removed to begin with passive forward flexion. At the eighth week, passive rotation in adduction was initiated and active motion was allowed depending on the evolution. Patients returned to sports after at least 6 months from surgery.
Outcomes Measurements
A new physical exam was carried out in all patients by an independent orthopedic surgeon. Clinical data regarding outcomes were obtained at out-patient visit. Recurrence of instability included new dislocation events or subluxations, defined as feeling of loosening or popping of the joint, withouth need of manual reduction by thirds. The etiology of the recurrent events and the time from surgery were also recorded. The functional evaluation was assessed by the Rowe Score for Instability [17]. Active range of motion was presented as degrees of forward flexion and external rotation with the arm in adduction. Internal rotation was classified using a four level-scale, depending on the position reached by the dorsal aspect of the hand when the patient was asked to take it to his back [i.e., greater trochanter (1); buttock (2); L5 (3); and D12 (4)]. The need for further revision surgery, its cause, type of surgery, time from index surgery, and postoperative complications were also recorded.
Statistical Method
The statistical analysis was performed using SPSS 22.0 (IBM Corp. 2013, Armonk, NY: IBM Corp.). The sample was divided into two groups: patients with or without postero-inferior labrum repair and capsular plication added to the anterior Bankart repair. Outcomes were compared within groups. Differences between groups were analyzed using either Student’s t test o Mann–Whitney U for numeric variables. The Chi-square test was used on binary variables. A P value < 0.05 was considered significant.
Results
70 patients were included in the study, consisting on 59 males and 11 females, with a mean age of 28.2 (range 14–56) and mean follow-up of 146.1 (range 120–208) months. Patients’ baseline variables are presented in Table 1.
Table 1.
Preoperative clinical features
| Patient data | Patients (n = 70) |
|---|---|
| Gender | |
| Male | 59 (84.3) |
| Female | 11 (15.7) |
| Age at presentation (years) | 28.2 (9.0) |
| < 20 | 15 (21.4) |
| 20–25 | 12 (17.1) |
| 25–30 | 20 (28.6) |
| > 30 | 23 (32.8) |
| Follow-up (months) | 146.1 ± 19.2 |
| Dominant arm | 41 (57.7) |
| Number of dislocations | 4.7 ± 6.5 |
| Practiced sports | |
| Yes | 42 (60) |
| No | 28 (40) |
| Competition sports | |
| Yes | 20 (47.6) |
| No | 22 (52.4) |
| Throwing sports | |
| Yes | 5 (11.9) |
| No | 37 (88.1) |
Data are presented as No. (%) or mean (standard deviation)
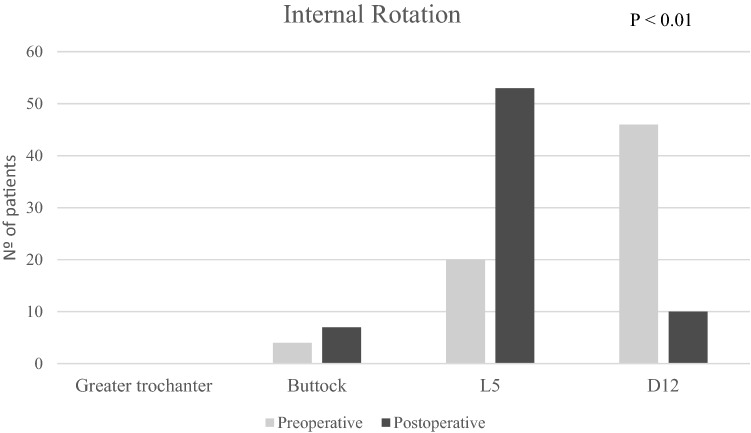
The outcomes of the arthroscopic anterior Bankart repair are visible at Table 2. Recurrence of instability occurred in 9 shoulders (12.8%) [3 dislocations (33%) and 6 subluxations (66%)], at a median of 17 (range 8–132) months of follow-up. Five events (55.6%) occurred within the first 24 months after surgery and 5 (55.6%) resulted from a new trauma. A total of 3 (4.2%) complications were reported during follow-up: 2 cases of persistent pain located on the anterior aspect of the shoulder and 1 case of transient neuroapraxia of the axillary nerve. One of the cases with residual pain and the neuroapraxia resolved with conservative treatment. In the other case of persistent pain, a protuding anchor was observed. Revision surgery was needed in 8 (11.4%) patients: 7 (87.5%) due to recurrent instability and 1 (12.5%) due to the anchor protuding into the joint. Revisions secondary to recurrent instability were subjected to revision Bankart in 5 cases (71.4%), open Latarjet in 1 case (14.3%) and an inferior glenohumeral ligament reconstruction using an artifical graft [18] in 1 case (14.3%). Median time to revision surgery was 23.5 (12–133) months. Mean Rowe score improved significantly after surgery at final follow-up. Flexion and external rotation showed a significant though clinically-not relevant decrease. Internal rotation decreased significantly [47 cases (66.2%) reached T12 preoperatively, where as 10 (14.1%) postoperatively] (Fig. 1).
Table 2.
Clinical outcomes after arthroscopic anterior Bankart repair
| Outcome measure | Patients (n = 70) |
P value | |
|---|---|---|---|
| Preoperative | Postoperative | ||
| Rowe score | 29.7 (11.6) | 87.1 (12.3) | < 0.01 |
| Forward flexion | 173.5° (19.2) | 168.4° (10.4) | < 0.01 |
| External rotation | 81.4° (18.0) | 75.7° (10.5) | < 0.01 |
| Return to sports | 35 (83.3) | ||
| Return to competitive sports | 17 (85) | ||
| Return to throwing sports | 4 (80) | ||
| Recurrence of instability | 9 (12.8) | ||
| Revision surgery | 8 (11.4) | ||
Data are presented as No. (%) or mean (standard deviation)
Fig. 1.
Global variation on internal rotation
Repair of postero-inferior labrum and posterior capsular plication was performed in 34 patients (48.6%). Table 3 shows demographics of both groups and Table 4 and Fig. 2 show the comparison of outcomes. No significant differences were observed on recurrence rate, need for revision surgery, functional status, range of motion, or return to sports.
Table 3.
Demographics features of patients with/without posterior repair
| Patient data | No posterior repair (n = 36) |
Posterior repair (n = 34) |
P value |
|---|---|---|---|
| Gender | |||
| Male | 26 (72.2) | 33 (97.0) | 0.004* |
| Female | 10 (27.8) | 1(2.9) | |
| Age at presentation (years) | 27.1 ± 8.9 | 29.1 ± 9.3 | 0.353 |
| Follow-up (months) | 147.5 ± 22.6 | 144.6 ± 14.6 | 0.519 |
| Dominant arm | 20 (55.6) | 21 (61.8) | 0.388 |
| Number of dislocations | 5.6 ± 8.8 | 3.5 ± 2.2 | 0.196 |
| Practiced sports | |||
| Yes | 16 (44.4) | 24 (70.6) | 0.024* |
| No | 20 (55.6) | 10 (29.4) | |
| Competition sports | |||
| Yes | 11 (30.6) | 9 (26.5) | 0.042* |
| No | 25 (69.4) | 26 (73.5) | |
| Throwing sports | |||
| Yes | 2 (5.6) | 3 (8.8) | 0.586 |
| No | 34 (94.4) | 31 (91.1) | |
Data are presented as No. (%) or mean ± standard deviation
*P < 0.05
Table 4.
Comparison of outcomes when posterior repair was added
| Outcome | No Posterior repair (n = 36) |
Posterior repair (n = 34) |
P value |
|---|---|---|---|
| Rowe score | |||
| Preoperative | 25.9 ± 9.0 | 33.7 ± 12.7 | 0.008* |
| Postoperative | 83.8 ± 14.1 | 89.4 ± 9.7 | 0.122 |
| External rotation | |||
| Preoperative | 80.5 ± 22.8 | 82.4 ± 13.0 | 0.972 |
| Postoperative | 74.8 ± 11.8 | 76.8 ± 9.4 | 0.606 |
| Flexion | |||
| Preoperative | 171.7 ± 26.2 | 175.6 ± 9.4 | 0.426 |
| Postoperative | 167.3 ± 12.4 | 169.9 ± 8.2 | 0.545 |
| Recurrence | |||
| No | 33 (91.7) | 28 (82.4) | 0.245 |
| Yes | 3 (8.3) | 6 (17.6) | |
| Revision surgery | |||
| No | 33 (91.7) | 29 (85.3) | 0.472 |
| Yes | 3 (8.3) | 5 (14.7) | |
| Surgical complications | |||
| No | 33 (91.7) | 34 (100.0) | 0.085 |
| Yes | 3 (8.3) | 0 (0.0) | |
| Return to sports | |||
| No | 3 (18.7) | 4 (16.7) | 0.865 |
| Yes | 13 (81.2) | 20 (83.3) | |
| Return to competition sports | |||
| No | 2 (18.2) | 1 (11.1) | 0.12 |
| Yes | 9 (81.8) | 8 (88.9) | |
| Return to throwing sports | |||
| No | 0 (0) | 1 (33.3) | 0.32 |
| Yes | 2 (100) | 2 (66.7) | |
Data are presented as No. (%) or mean ± standard deviation
*P < 0.05
Fig. 2.
Comparison of internal rotation when posterior repair was added
Discussion
The most important finding of this study was that postero-inferior repair of the labrum-capsule complex associated with an anterior Bankart repair as treatment of anterior glenohumeral instability did not influence the outcomes at 12.2 years follow-up. 12.8% of shoulders had a recurrent instability event, while functional status, flexion, and external rotation were very satisfactory. Internal rotation was significantly decreased. Revision surgery was needed in 11.4%.
The recurrence rate on this study was slightly lower compared with previously reported on long-term follow-up series. A recent systematic review of outcomes of anterior arthroscopic Bankart repair at minimun 10 year follow-up showed that recurrent dislocations and subluxations were found at 16% and 17% of the cases, respectively [11]. The study by Komnos et al.[19] showed a rate similar to ours (11.5%), although mean follow-up was shorter (105.4 months). They excluded from their series patients with glenoid bone-loss over 15%, as we did. Furthermore, in our series, patients with large Hill–Sachs injuries requiring additional procedures, like the remplissage, were also excluded to evaluate only the effect of the anterior Bankart repair and the posterior repair in abscence of bone-loss. This aspect may be crucial to explain the differences with respect to the other series, where a higher cut-off is applied, generally 25% or even 50% of glenoid bone-loss [9, 20]. Assessing exclusion criteria regarding glenoid or humeral bone-loss is critical when reviewing the outcomes of arthroscopic Bankart repair.
Overall, no great deficits on range of motion have been reported at long-term follow-up after anterior Bankart repairs. Different series have reported mild deficits on internal and external rotation after surgery, not reaching clinical relevance in any case [7, 8, 21, 22]. Similar findings were observed in our series except on internal rotation, which showed a notable postoperative deficit, as 66.2% of patientes reached at least D12 preoperatively, while only 14.1% postoperatively. Nevertheless, functional outcomes remained satisfactory as the majority of these cases were still able to reach the L5 level (76%).
Good-to-excellent functional results after anterior arthroscopic Bankart repair can be expected at long-term. Mean postoperative Rowe score has been reported to be over 87 points by Murphy et al. [11] and overall return to sports rate was 77.6%. Comparable findings were shown by Komnos et al. [19] and Aboalata et al. [6], with return to sport rates over 75% in both series. In our study, 83.3% of patients could return to sports practice after surgery, 85% returned to a competitive level, and 80% to throwing sports.
Adding soft-tissue procedures to anterior Bankart repair to restore shoulder stability is controversial. Attending to the “circle injury” concept, the essential lesion of anterior shoulder instability is a tear of the labrum and the capsuloligamentous complex from the anterior glenoid rim, which might be accompanied by injuries on the opposite site of the shoulder [14]. However, there are no long-term clinical data supporting the effectiveness of repairing posterior injuries in the setting of isolated anterior instability. Westerheide et al. added postero-inferior capsular plications to anterior arthroscopic Bankart repairs to treat 71 shoulders with anterior shoulder instability, and observed a recurrence rate of 7% and a satisfaction rate of 100%, with 90% of patients returning to their previous sports level at a mean of 33.3 month follow-up [16]. Though, there was no control group. Castagna et al. conducted a randomized trial comparing an arthroscopic anterior Bankart repair adding a postero-inferior plication stitch with an arthroscopic anterior Bankart repair alone at 2 years of follow-up. No significant differences regarding recurrence rates, UCLA scores, and ASES scores were observed, while improvements in Constant score were greater in the plication group. In addition, no differences were found between groups in external or internal rotation, and a slight deficit on forward flexion was observed in the plication group [15]. Chiang et al. reported a 6.6% recurrence rate on their series at 5 year follow-up, adding a rotator interval closure and postero-inferior capsular plications to an anterior Bankart repair, with excellent clinical outcomes and range of motion [23]. An interesting finding of this study was that the mean glenoid bone-loss measured intraoperatively was 17.5%, a relatively high value that did not seem to affect the outcomes, specially the recurrence rate. However, there was no control group to determine the effect of the postero-inferior plication and the rotator interval closure solely. In our series, the addition of postero-inferior labrum repair with capsular plications to an anterior Bankart repair did not have any influence on the outcomes. Indeed, recurrence rate was more than double when it was added (8.3% versus 17.6%), although the differences were not statistically significant. To our knowledge, this is the only work published evaluating this surgical gesture in a long-term follow-up series. Additional research including randomized controlled trials will be needed to confirm this observation.
This study has several limitations. First, baseline characteristics and surgical records were obtained from a retrospective database. Second, at the time the surgeries were performed, no clear guidelines were available on literature to decide when a posterior capsulolabral repair added to the anterior Bankart repair could be optimal to each case, leaving the decision of when to perform these procedures depending exclusively on surgeon’s criteria. To compensate this, very strict inclusion and exclusion criteria were applied, i.e., glenoid or humeral bone-loss cut-off, to evaluate solely the effect of labrum repairs in absence of any confounding factors. Third, recurrence is reported as redislocation and subluxation, while residual apprehension was not assessed, which could have lead to an underestimation of the recurrence rate. To compensate this possible bias, other outcomes, such as need for revision surgery, were also analyzed.
Conclusion
The addition of postero-inferior capsulolabral repair to anterior Bankart repair as treatment of anterior glenohumeral instability did not influence the outcomes in terms of recurrence, range of motion, return to sports, or functional status, compared to isolated anterior Bankart repair at long-term follow-up.
Author Contribution
PCMdS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. PCMdS participated on study concept and design, drafting the manuscript, and critical review. NZU participated on study concept and design and critical manuscript review. ITM participated on analysis and interpretation of data, and critical review. ÁCD was the surgeon of the cases presented and participating on critical review of the manuscript.
Data Availability
All data are available in the main text.
Compliance with ethical standards
Conflict of Interest
Pablo Carnero-Martín de Soto, Néstor Zurita-Uroz, Iskandar Tamimi Mariño, and Ángel Calvo Díaz declare that they have no conflict of interest.
Ethical Approval
The study protocol was approved by the Hospital Viamed Montecanal ethical committee (registry number 20201).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Research Involves Human and Animal Participants
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Pablo Carnero-Martín de Soto , Email: pablocarneromds@hotmail.com.
Néstor Zurita-Uroz, Email: ntzurita@gmail.com.
Iskandar Tamimi-Mariño, Email: Isktamimi80@yahoo.com.
References
- 1.Balke M, Shafizadeh S, Bouillon B, Banerjee M. Management of shoulder instability: The current state of treatment among German orthopaedic surgeons. Archives of Orthopaedic and Trauma Surgery. 2016;136:1717–1721. doi: 10.1007/s00402-016-2553-2. [DOI] [PubMed] [Google Scholar]
- 2.Owens BD, Harrast JJ, Hurwitz SR, Thompson TL, Wolf JM. Surgical trends in Bankart repair: An analysis of data from the American Board of Orthopaedic Surgery certification examination. American Journal of Sports Medicine. 2011;39:1865–1869. doi: 10.1177/0363546511406869. [DOI] [PubMed] [Google Scholar]
- 3.Chalmers PN, Mascarenhas R, Leroux T, Sayegh ET, Verma NN, Cole BJ, Romeo AA. Do arthroscopic and open stabilization techniques restore equivalent stability to the shoulder in the setting of anterior glenohumeral instability? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:355–363. doi: 10.1016/j.arthro.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Harris JD, Gupta AK, Mall NA, Abrams GD, McCormick FM, Cole BJ, Bach BR, Romeo AA, Verma NN. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy. 2013;29:920–933. doi: 10.1016/j.arthro.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Lenters TR, Franta AK, Wolf FM, Leopold SS, Matsen FA. Arthroscopic compared with open repairs for recurrent anterior shoulder instability. A systematic review and meta-analysis of the literature. Journal of Bone and Joint Surgery. American Volume. 2007;89:244–254. doi: 10.2106/00004623-200702000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Aboalata M, Plath JE, Seppel G, Juretzko J, Vogt S, Imhoff AB. Results of arthroscopic Bankart repair for anterior-inferior shoulder instability at 13-year follow-up. American Journal of Sports Medicine. 2017;45:782–787. doi: 10.1177/0363546516675145. [DOI] [PubMed] [Google Scholar]
- 7.Castagna A, Markopoulos N, Conti M, Delle Rose G, Papadakou E, Garofalo R. Arthroscopic bankart suture-anchor repair: Radiological and clinical outcome at minimum 10 years of follow-up. American Journal of Sports Medicine. 2010;38:2012–2016. doi: 10.1177/0363546510372614. [DOI] [PubMed] [Google Scholar]
- 8.Chapus V, Rochcongar G, Pineau V, de Chou ÉS, Hulet C. Ten-year follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocation in young patients. Orthopaedics & Traumatology, Surgery & Research. 2015;101:889–893. doi: 10.1016/j.otsr.2015.09.029. [DOI] [PubMed] [Google Scholar]
- 9.Flinkkilä T, Knape R, Sirniö K, Ohtonen P, Leppilahti J. Long-term results of arthroscopic Bankart repair: Minimum 10 years of follow-up. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26:94–99. doi: 10.1007/s00167-017-4504-z. [DOI] [PubMed] [Google Scholar]
- 10.Yapp LZ, Nicholson JA, Robinson CM. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: Long-term follow-up of a randomized, double-blinded trial. Journal of Bone and Joint Surgery. American Volume. 2019;102:460–467. doi: 10.2106/JBJS.19.00858. [DOI] [PubMed] [Google Scholar]
- 11.Murphy AI, Hurley ET, Hurley DJ, Pauzenberger L, Mullett H. Long-term outcomes of the arthroscopic Bankart repair: A systematic review of studies at 10-year follow-up. Journal of Shoulder and Elbow Surgery. 2019;28:2084–2089. doi: 10.1016/j.jse.2019.04.057. [DOI] [PubMed] [Google Scholar]
- 12.Calvo A, Martínez AA, Domingo J, Herrera A. Rotator interval closure after arthroscopic capsulolabral repair: A technical variation. Arthroscopy. 2005;21:765. doi: 10.1016/j.arthro.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 13.Cho NS, Yoo JH, Juh HS, Rhee YG. Anterior shoulder instability with engaging Hill-Sachs defects: A comparison of arthroscopic Bankart repair with and without posterior capsulodesis. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24:3801–3808. doi: 10.1007/s00167-015-3686-5. [DOI] [PubMed] [Google Scholar]
- 14.Cuéllar R, Ruiz-Ibán MA, Cuéllar A. Anatomy and biomechanics of the unstable shoulder. Open Orthop J. 2017;11:919–933. doi: 10.2174/1874325001711010919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castagna A, Borroni M, Delle Rose G, Markopoulos N, Conti M, Vinci E, Garofalo R. Effects of posterior-inferior capsular plications in range of motion in arthroscopic anterior Bankart repair: A prospective randomized clinical study. Knee Surgery, Sports Traumatology, Arthroscopy. 2009;17:188–194. doi: 10.1007/s00167-008-0650-7. [DOI] [PubMed] [Google Scholar]
- 16.Westerheide KJ, Dopirak RM, Snyder SJ. Arthroscopic anterior stabilization and posterior capsular plication for anterior glenohumeral instability: A report of 71 cases. Arthroscopy. 2006;22:539–547. doi: 10.1016/j.arthro.2005.12.033. [DOI] [PubMed] [Google Scholar]
- 17.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: A long-term end-result study. Journal of Bone and Joint Surgery. American Volume. 1978;60:1–16. doi: 10.2106/00004623-197860010-00001. [DOI] [PubMed] [Google Scholar]
- 18.Sánchez M, Cuéllar R, García A, Albillos J. Anterior stabilization of the shoulder by means of an artificial capsular reinforcement and arthroscopy—part I: Surgical technique. Journal of Long-Term Effects of Medical Implants. 2000;10:187–197. [Google Scholar]
- 19.Komnos GA, Banios K, Liantsis A, Alexiou K, Varitimidis S, Bareka M, Hantes ME. Results of arthroscopic Bankart repair in recreational athletes and laborers: A retrospective study with 5 to 14 years of follow-up. Orthopaedic Journal of Sports Medicine. 2019;7:2325967119881648. doi: 10.1177/2325967119881648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zimmermann SM, Scheyerer MJ, Farshad M, Catanzaro S, Rahm S, Gerber C. Long-term restoration of anterior shoulder stability: A retrospective analysis of arthroscopic Bankart repair versus open Latarjet procedure. Journal of Bone and Joint Surgery. American Volume. 2016;98:1954–1961. doi: 10.2106/JBJS.15.01398. [DOI] [PubMed] [Google Scholar]
- 21.Privitera DM, Bisson LJ, Marzo JM. Minimum 10-year follow-up of arthroscopic intra-articular Bankart repair using bioabsorbable tacks. American Journal of Sports Medicine. 2012;40:100–107. doi: 10.1177/0363546511425891. [DOI] [PubMed] [Google Scholar]
- 22.Plath JE, Aboalata M, Seppel G, Juretzko J, Waldt S, Vogt S, Imhoff AB. Prevalence of and risk factors for dislocation arthropathy: Radiological long-term outcome of arthroscopic Bankart repair in 100 shoulders at an average 13-year follow-up. American Journal of Sports Medicine. 2015;43:1084–1090. doi: 10.1177/0363546515570621. [DOI] [PubMed] [Google Scholar]
- 23.Chiang E-R, Wang J-P, Wang S-T, Hung S-C, Ma H-L, Liu C-L, Chen T-H. Arthroscopic posteroinferior capsular plication and rotator interval closure after Bankart repair in patients with traumatic anterior glenohumeral instability—a minimum follow-up of 5 years. Injury. 2010;41:1075–1078. doi: 10.1016/j.injury.2010.05.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available in the main text.