Summary
Background
Oral rotavirus vaccines have lower effectiveness in high child mortality settings. We evaluated the impact of additional dose(s) schedules of rotavirus vaccine on vaccine immunogenicity and reduction in episodes of gastroenteritis.
Methods
We searched Medline (via PubMed), Cochrane databases and ClinicalTrials.gov for randomised controlled trials from 1973 to February 2022, evaluating the immunological and clinical impact of additional dose vs standard dose oral rotavirus vaccine schedules. We extracted immunogenicity – proportion of children with evidence of anti-rotavirus IgA seroresponse, and clinical – proportion of children with at least one episode of severe rotavirus gastroenteritis, outcome data and used random effects meta-analysis where appropriate. We assessed the methodological quality of the studies using the Cochrane risk of bias tool. The study protocol was registered in PROSPERO (CRD42021261058).
Findings
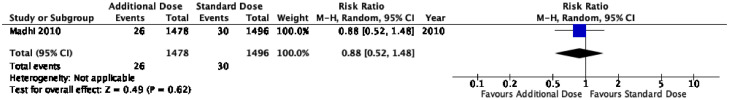
We screened 536 items and included 7 clinical trials. Our results suggest moderate to high level evidence that an additional dose rotavirus vaccine schedule improves IgA vaccine immune response, including additional doses administered as a booster dose schedule >6 months old; IgA vaccine seroresponse 74·3% additional dose schedule vs 56·1% standard dose schedule RR 1·3 (95%CI, 1·15 – 1·48), and when administered to children who were seronegative at baseline; IgA vaccine seroresponse 48.2% additional dose schedule vs 29.6% standard dose schedule RR 1.86 (95%CI 1.27 to 2.72). Only one study evaluated reduction in gastroenteritis episodes and found little benefit in first year of life, 1·8% vs 2·0% RR 0·88 (95% CI, 0·52 to 1·48), or second year of life, 1·7% vs 2·9% RR 0·62 (95%CI, 0·31 – 1·23).
Interpretation
Administering an additional dose of oral rotavirus vaccines is likely to result in an improved vaccine immune response, including when administered as a booster dose to older children. Evidence of an impact on diarrhoeal disease is needed before additional dose rotavirus vaccine schedules can be recommended as vaccine policy.
Funding
BM was funded by the National Health and Medical Research Council, the Royal Australasian College of Physicians Paediatrics and Child Health Division, and the Australian Academy of Science.
Keywords: Rotavirus, Rotavirus vaccines, Schedule, Immunogenicity, Diarrhoea
Research in context.
Evidence before this study
Oral rotavirus vaccines have been responsible for a significant reduction in the global burden of rotavirus gastroenteritis. However, vaccine effectiveness has varied across settings. A recent systematic review reported vaccine efficacy in Asia and Africa to be just 48 to 57% in the first year following vaccination, and 29% to 54% in the second year. Two previous reviews have evaluated the immunological and clinical impact of scheduling an additional dose of oral rotavirus vaccine. Both reviews evaluated schedules where the additional dose of oral rotavirus vaccine was administered early as part of an extended primary course (6, 10, 14 wks vs either 6, 10 wks or 10, 14 wks) and reported weak evidence that an ’additional dose’ schedule resulted in higher rates of vaccine seroconversion. We searched Medline (via Pubmed), Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Central & Infectious Disease Group Specialised Register, Cochrane Database of Systematic Reviews and ClincialTrials.gov covering the period from 1973 until February 2022, using the MESH terms ‘rotavirus’ and ‘rotavirus vaccines’. We identified nine articles, reporting seven randomised clinical trials, that compared an additional dose oral rotavirus vaccine schedule with a standard dose schedule. All seven clinical trials compared the proportion of children with evidence of anti-rotavirus IgA seroresponse following the additional dose vs standard dose schedule. Only one clinical trial evaluated reduction in the number of episodes of severe rotavirus gastroenteritis.
Added value of this study
Our review is the first to include data from studies where the additional dose of oral rotavirus vaccine was administered as a ‘booster dose’ in the second six months of life. Our evaluation of 7 clinical trials involving over 4000 children < 2 years old, suggests that an additional dose of oral rotavirus vaccine improves vaccine seroresponse compared to a standard rotavirus schedule. An improved vaccine seroresonse was observed when the additional rotavirus vaccine dose was administered as a booster dose in the second six months of life (vaccine seroresponse in an additional 168 children per 1000 vaccinated compared to the standard schedule; 95%CI 84 to 269), and among infants who were seronegative at baseline (vaccine seroresponse in an additional 255 per 1000 vaccinated children compared to the standard schedule; 95%CI 81 to 510). Only one clinical trial evaluated the impact of an additional dose schedule on reduction in episodes of severe rotavirus gastroenteritis and found little evidence of benefit from an additional dose schedule in either the first or second year of life.
Implications of all the available evidence
It is important to find pragmatic strategies to improve the impact of rotavirus vaccines in settings where the burden of rotavirus remains unacceptably high. Administering an additional dose of oral rotavirus vaccines is likely to result in an improved vaccine immune response, including when administered as a booster dose to older children. However, evidence of an impact diarrhoeal disease is needed before additional dose rotavirus vaccine schedules can be recommended as vaccine policy
Alt-text: Unlabelled box
Introduction
Rotavirus remains a leading cause of diarrhoea-related morbidity and mortality in young children worldwide.1 Oral rotavirus vaccines have resulted in a significant reduction in the global burden of rotavirus disease. However, the effectiveness has varied across settings with high effectiveness observed in countries with low child mortality, and more modest effectiveness observed in countries with high mortality.2 A recent systematic review of the performance of four oral rotavirus vaccines in high child mortality settings in Asia and Africa reported that vaccine efficacy was only 48 to 57% in the first year following vaccination and 29% to 54% in the second year.1
The reasons for the lower effectiveness of oral rotavirus vaccines in high mortality settings are not well understood, but are likely to include high force of infection and factors believed to impair immunogenicity including high levels of maternal-derived vaccine-neutralising antibodies, intestinal microbiota dysbiosis/ environmental enteropathy, high prevalence of comorbid infections, poor nutrition, virus strain heterogeneity, and prevalent genetic determinants of vaccine responses or susceptibility to different rotavirus genotypes.3 Delayed or incomplete schedule adherence are exacerbated by age restrictions which are unique to rotavirus vaccines and these may also negatively impact on the vaccine programme. An earlier tetravalent rhesus-human rotavirus vaccine was associated with an increased risk of intussusception, with the highest attributable risk observed among infants >3 months old.4 As a result, manufacturers of the new generation oral rotavirus vaccines have recommended upper age limits for administration, which reduce the opportunity to catch up missed vaccines in later infancy.
There is a strong global health imperative to find effective and practical strategies to further reduce deaths and morbidity from severe rotavirus disease among young children. We hypothesise that administering additional dose(s) of oral rotavirus vaccine, either as an extended primary course or as a booster dose administered after the current recommended upper age limits of vaccine administration, may lead to improved immune responses and improved clinical protection against severe rotavirus gastroenteritis.
This review aims to address whether administering an additional dose of oral rotavirus vaccine improves the immune response to the vaccine and whether it reduces the risk of diarrhoeal disease among children <5 years old, compared to a routine rotavirus vaccine schedule. Where possible, we aimed to assess the effect of additional doses of rotavirus vaccine on safety outcomes, including intussusception.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines for this review. The protocol is available at www.crd.york.ac.uk/PROSPERO, CRD42021261058.
PICO – population, intervention, comparison, outcome
Our primary objective was to compare the effect of an extended schedule of oral rotavirus vaccine products on immunogenicity and/or reduction in diarrhoeal disease among children <5 years old, compared to a routine schedule.
A routine or ‘standard dose schedule’ was defined as two doses of Rotarix vaccine (GlaxoSmithKline), or three doses of RotaTeq vaccine (Merck), Rotasiil vaccine (Serum Institute of India) or Rotavac vaccine (Bharat Biotech). The comparator, an extended or ‘additional dose schedule’, was defined as more than two doses of Rotarix vaccine or more than three doses of RotaTeq, Rotasill or Rotavac vaccine. Where individual studies compared more than one standard schedule as per the above definition – typically Rotarix at 6, 10 and 14 wks vs at 6 and 10 wks or at 10 and 14 wks, the Rotarix 6 and 10wks schedule was selected as the standard schedule as this is consistent with the recommended age of oral rotavirus vaccine administration in the WHO Expanded Programme on Immunization.
The primary immunogenicity outcome was measured as the absolute difference in proportion of children with evidence of anti-rotavirus IgA seroresponse following all doses in the additional dose versus standard dose schedule. Seroresponse was defined as anti-rotavirus IgA ≥ 20IU/ml. To be consistent, where studies reported both seroresponse (IgA ≥ 20 IU/ml) and seroconversion (from pre-vaccine IgA < 20 IU/ml to post-vaccine IgA ≥ 20 IU/ml), seroresponse was selected as the primary outcome. Where studies reported seroresponse data at multiple time points, seroresponse approximately four weeks following the last administered dose of rotavirus vaccine/ placebo was selected as the primary outcome.
The primary clinical outcome was measured as reduction in diarrhoeal disease; difference in the proportion of children having one or more episodes of severe rotavirus gastroenteritis (severe RVGE) for children receiving an additional dose vs standard dose schedule. This was assessed for the time periods up to one year, two years and five years old. Severe gastroenteritis was defined as episodes of gastroenteritis requiring hospitalisation or episodes with a high Vesikari score – a validated assessment tool rating severity and duration of clinical symptoms including diarrhoea, vomiting, fever, dehydration, and clinical treatment required, where a score ≥ 11/20 has been considered to reflect severe symptoms.5 Where possible, we also assessed the difference in episodes of any rotavirus gastroenteritis (any RVGE), severe all-cause gastroenteritis (severe GE), and all-cause gastroenteritis (GE).
Safety outcomes were measured as the difference in risk of severe adverse events, intussusception, and death, among children receiving the additional vs standard dose schedule.
Inclusion and exclusion criteria
We included any identified randomised trials comparing an additional dose oral rotavirus vaccine schedule with a standard dose schedule. We excluded non-randomised studies, trials evaluating mixed rotavirus vaccine schedules, trials evaluating vaccines that have not been WHO prequalified (Rotavin-M1, Vietnam; and Lanzhou Lamb Rotavirus Vaccine, China) and trials comparing an additional dose rotavirus vaccine schedule with a non-standard rotavirus vaccine schedule (for example, comparing 3-dose Rotarix to 3-dose placebo, or comparing 3-dose Rotarix to 5-dose Rotarix). There was no exclusion based on study setting, as studies from low-mortality countries may have provided insight into oral vaccine performance among children in different mortality settings.6
Search strategy and study selection
We searched Medline (via PubMed), Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Central & Infectious Disease Group Specialised Register, Cochrane Database of Systematic Reviews, and ClinicalTrials.gov in June 2021, with weekly updates until February 2022, using the MESH terms ‘rotavirus’ and ‘rotavirus vaccines’. Databases were searched from 1973 until present with no restriction on language of publication. We examined the reference list of included studies and relevant review articles, reviewed the World Health Organization Clinical Trials Registry Platform (WHO ICTRP), and consulted experts in the field to identify studies missed by the above search strategy.
Items identified in the search were downloaded and assembled in an EndnoteX9 library and imported into Covidence software (covidence.org) where duplicates were removed. Two review authors (BM, PF) independently screened titles and abstracts and assessed the eligibility of full-text articles against PICO criteria. Disagreements were resolved through discussion and adjudication from additional review authors (PM, TS).
Data extraction
Two review authors (BM, PF) independently extracted data into a pre-piloted data extraction form in Covidence (based on the Cochrane Good Practice Data Extraction Form).7 Where a single study provided data at multiple time points or for multiple similar outcomes, all data were recorded but only the most relevant data was included in the analysis. Where multiple publications reported data from the same clinical trial, care was taken to extract the most comprehensive and relevant data, and to ensure it was only used once. One study author was contacted for missing information8 and additional data for the same clinical trial8, 9, 10 were obtained from an online repository provided by a consortium of clinical study sponsors (ClinicalStudyDataRequest.com).
Where possible, data were also collected on secondary outcomes including intussusception (as per Brighton criteria),11 death and serious adverse events.
Data synthesis and statistical analysis
To analyse the effect of an extended dose rotavirus vaccine schedule on immunogenicity and diarrhoeal disease, we included all children who were randomised and received an additional dose or standard dose rotavirus vaccine schedule. For the immunogenicity outcome, we included all children who had anti-rotavirus IgA seroresponse results available following administration of the final dose of oral rotavirus vaccine in the allocated schedule. For the clinical outcome we included all children who completed active surveillance through weekly visits to parents or guardians to collect diary cards and through the collection of data from health clinics.
We assessed the effect of an additional dose rotavirus vaccine schedule on vaccine seroresponse and reduction in diarrhoea episodes with a random-effects meta-analysis, generating summary relative risk (RR) estimates and 95% confidence intervals. We examined heterogeneity between studies visually and using the I2 statistic and investigated publication bias by visually inspecting funnel plots. We also estimated the risk differences to assist with interpreting the public health impact of the intervention. Analyses were carried out in RevMan 5.4.1 and GRADEPro.
Pre-specified subgroup analyses were undertaken where the additional dose was administered as part of an extended primary schedule and before the current recommended upper age limit of rotavirus vaccine administration (typically 6/10/14wks vs 6/10wks or 10/14wks) or administered as a booster dose in the second six months of life after the current recommended upper age limit of rotavirus vaccine administration (at approximately 9 months, 9-11 months, or 6 – 11 months old).
Risk of bias was assessed independently by two authors (BM, PF) using a Risk of Bias assessment tool considering the process for randomisation (sequence generation/allocation concealment), deviations from intended interventions (blinding of participants/personnel), missing outcome data, bias in outcome measurement (blinding of outcome assessors), and selective reporting (clinical trial registration before data analysis).7 The role of funding bodies in analysis of data and reporting of results was also observed. Discrepancies were adjudicated by a third author (PM).
A summary of findings table was created to present both relative and anticipated absolute effects of the most clinically relevant outcomes – IgA seroresponse and prevention of episodes of severe RVGE in the first and second year of life. Seroresponse rate and number of episodes of severe RVGE for the standard dose vaccine schedule were calculated using the standard dose results from included studies (GRADEPro). We assessed quality of evidence for each clinically important outcome using Grading of Recommendations, Assessment, Development and Evaluation (GRADE) by considering risk of bias, inconsistency, imprecision, indirectness, and publication bias.7
Role of funding
The funders had no role in the study design, collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication. All authors had full access to all the data in the study and responsibility for the decision to submit for publication.
Results
Our initial search identified 766 items; 536 titles and abstracts were screened, and 19 items progressed to full text review. Of these, a further ten items were excluded because they evaluated mixed dose schedules or non-prequalified vaccines, used non-standard comparators, were not randomised controlled trials, or were duplicates. One additional study was identified through correspondence with domain experts and was subsequently located in the Pan African Clinical Trial Registry, however results had not been reported at the time of our review. Thus, nine articles representing seven unique clinical trials met the inclusion criteria for this review (see Figure 1).
Figure 1.
PRISMA diagram.
* One additional study identified by domain expert and subsequently found in Pan African Clinical Trial Registry; data for this study was not available at the time of our review so the study was excluded.
Study characteristics
Of the seven clinical trials, four studied an additional dose of oral rotavirus vaccine administered in the first six months of life as part of the primary schedule (typically 6/10/14wks vs either 6/10wks or 10/14wks)9,12, 13, 14 and three studied the additional dose administered as a booster dose in the second six months of life (at approximately 9 months, 9 – 11 months, or 6 – 11 months old).15, 16, 17 Six studies evaluated an additional dose schedule for Rotarix,9,12, 13, 14,16,17 and one study for RotaTeq.15 No studies evaluated additional dose schedules for Rotavac or Rotasiil. Six trials were conducted in high mortality countries,9,12, 13, 14, 15,17 and one trial was conducted among Australian Indigenous children (see Table One).16
The results of a single clinical trial comparing 3-dose vs 2-dose Rotarix in South Africa and Malawi were reported in three separate publications. The first publication presented combined clinical outcome data at the end of the first year for both countries.9 The second and third publications reported two-year extended efficacy evaluation clinical outcome data for Malawi and South Africa separately.8,10 Additional immunogenicity data for this clinical trial was obtained from an online data repository (ClinicalStudyDataRequest.com).
Three studies,12,13,16 had moderately high attrition rate (20% – 30%), but overall the studies were deemed high quality and low risk of bias, with the exception of one study where the process of randomisation sequence generation was unclear17 (see Supplementary Materials). A funnel plot was used to assess publication bias and none was observed (see Supplementary Materials).
Immunogenicity results
All seven clinical trials evaluated the effect of an additional dose rotavirus vaccine schedule on immunogenicity. On pooling the results from all seven studies, 1343 of 2194 (61·2%) children receiving an additional dose schedule had a seroresponse vs 1235 of 2205 (56·0%) children receiving standard dose schedule. The RR of anti-rotavirus IgA seroresponse was 1·25 (95%CI 1·04 to 1·49) but with considerable heterogeneity between studies (I2 = 89%) (see Figure 2). The estimated increase in vaccine seroresponse was an additional 140 per 1000 vaccinated children (95%CI, 22 to 275 per 1000 children) (see Table Two).
Figure 2.
IgA seroresponse – IgA > 20IU/ml following last dose of oral rotavirus vaccine administered in the additional dose vs standard dose schedule.
In the four studies where the additional dose was administered as part of the primary schedule (6/10/14wks vs 6/10wks or 10/14wks),9,12, 13, 14 there was weak evidence of increased seroresponse with 889 of 1583 (56·2%) children receiving additional dose seroresponding vs 889 of 1588 (56·0%) children receiving standard dose schedule, RR 1·21 (95%CI, 0·90 to 1·65) but with evidence of high heterogeneity (I2 = 85%) (see Supplementary Materials). In contrast, in the three studies where the additional dose was administered as a booster dose in the second six months of life (at 9 months, 9–11 months, and 6 – 11 months old),15, 16, 17 there was moderate evidence of increased seroresponse with 454 of 611 (74·3%) children receiving additional dose seroresponding vs 346 of 617 (56·1%) children receiving standard dose schedule, RR: 1·3 (95%CI, 1·15 to 1·48) with moderate evidence of heterogeneity (I2 = 56%) (see Supplementary Materials). This corresponds to an estimated 168 additional vaccine seroresponses per 1000 vaccinated children (95%CI, 84 to 269 per 1000 children) (see Table Two).
Three studies only included children proven to be seronegative (IgA < 20 IU/ml) at baseline in their primary per-protocol analysis.12, 13, 14 A post-hoc sensitivity analysis was undertaken evaluating seroconversion results only (i.e. excluding children with anti-rotavirus IgA ≥ 20 IU/ml at baseline from all seven studies). There was evidence of seroconversion for 412 of 854 (48·2%) children receiving an additional dose vs 252 of 850 (29·6%) children receiving standard dose schedule; RR 1·86 (95%CI 1·27 to 2·72) but with evidence of high heterogeneity across studies (I2 = 88%) (see Supplementary Materials). This is equivalent to an estimated 255 additional vaccine seroconversions per 1000 vaccinated seronegative children (95%CI, 81 to 510 per 1000 children); Table 2.
Table 1.
Clinical trials comparing an additional dose oral rotavirus vaccine schedule with a standard dose oral rotavirus vaccine schedule.
| Author | Country | Participantsa | Vaccine | Schedule | Immunological Follow-Up | Clinical Follow-Up |
|---|---|---|---|---|---|---|
| Steele 2010 12 | South Africa | 264 | Rotarix | 6/10/14 wks vs 10/14 wksc | 8 weeks | not reported |
| Madhi 2010 9,b | South Africa & Malawi | 2,298 | one year | |||
| Cunliffe 2012 8,b | Malawi | 652 | Rotarix | 6/10/14 wks vs 10/14 wksc | 4 weeks | one & two years |
| Madhi 2012 10,b | South Africa | 1646 | one & two years | |||
| Ali 2014 13 | Pakistan | 324 | Rotarix | 6/10/14 wks vs 6/10 wksd | 4 weekse | not reported |
| Armah 2016 14 | Ghana | 285 | Rotarix | 6/10/14 wks vs 6/10 wksd | 4 weekse | not reported |
| Zaman 2016 17 | Bangladesh | 466 | Rotarix | 6/10 wks/ 9 mths vs 6/10 wks | 8 weeks | not reported |
| Haidara 2018 15 | Mali | 584 | RotaTeq | 6/10/14 wks/ 9-11 mths vs 6/10/14 wks | 4 weeks | not reported |
| Middleton 2022 16 | Australia | 178 | Rotarix | 2 mths/4 mths/ 6- 12 mths vs 2 mths/ 4 mths | 4 – 8 weeks | not reported |
number of children randomised with anti-rotavirus IgA seroresponse results available following administration of the final dose of oral rotavirus vaccine in the additional and standard dose schedules.
Madhi 2010/ Cunliffe 2012/ Madhi 2012 present data from the same clinical trial (NCT00241644)
Steele 2010 and Madhi 2010/ Cunliffe 2012/ Madhi 2012 present data for three rotavirus vaccine schedules – 6/10 wks, 6/10/14 wks, three-dose placebo – we evaluated 6/10 wks vs 6/10/14 wks (discounted placebo data).
Ali 2014/ Armah 2016 present data for three rotavirus vaccine schedules – 6/10 wks, 10/14 wks, 6/10/14 wks – the 6/10wk schedule was selected as the ‘standard schedule’ as consistent with EPI.
Ali 2014/ Armah 2016 measure immunogenicity at both 4 wks and 8 wks post standard schedule– we selected 4wk immunogenicity for our analysis.
Table 2.
Summary of findings.
| Additional Dose vs Standard Schedule Oral Rotavirus Vaccine to Improve Immunogenicity & Prevent Episodes of Gastroenteritis | |||||
|---|---|---|---|---|---|
| Population: children < 5 years | |||||
| Intervention: extended dose rotavirus vaccine schedule (more than two doses of Rotarix or more than three doses of RotaTeq/ Rotavac/ Rotasiil) | |||||
| Comparison: standard dose rotavirus vaccine schedule (two doses of Rotarix or three doses of RotaTeq/ Rotavac/ Rotasiil) | |||||
| Outcomes | No of Participants | Relative Effect (95% CI) | Anticipated Absolute Effects |
Quality of Evidence (Grade) | |
| Standard Dose | Additional Dose | ||||
| IgA Seroresponse (all studies)a | 4399 (7 RCTs) | RR 1.25 (1·04 to 1·49) | 560 per 1000 | 700 per 1000 (582 to 835) | Moderatec |
| IgA Seroresponse – additional dose schedule completed before 6 months of agea | 3171 (4 RCTs) | RR 1.21 (0·90 to 1·65) | 560 per 1000 | 678 per 1000 (504 to 924) | Moderatec |
| IgA Seroresponse – additional dose schedule completed after 6 months of agea | 1228 (3 RCTs) | RR 1.30 (1·15 to 1·48) | 561 per 1000 | 729 per 1000 (645 to 830) | High |
| IgA Seroconversion (seronegative at baseline)a | 1704 (7 studies) | RR 1.86 (1·27 to 2·72) | 296 per 1000 | 551 per 1000 (377 to 806) | Moderatec |
| Prevention of at least one episode of severe RVGE in the first year of lifeb | 2974 (1 RCT) | RR 0.88 (0·52 to 1·48) | 20 per 1000 | 18 per 1000 (10 to 30) | Moderated |
| Prevention of at least one episode of severe RVGE in the second year of lifeb | 1500 (1 RCT*) | RR 0.62 (0·31 to 1·23) | 29 per 1000 | 18 per 1000 (9 to 36) | Moderated |
IgA seroresponse/ seroconversion measured four to eight weeks following the last administered dose of oral rotavirus vaccine in the schedule.
Severity defined as Vesikari score ≥ 11.
Downgraded one level due to high heterogeneity among studies.
Downgraded one level due to imprecision due to the confidence intervals indicating a potential increase or decrease in diarrhoea episodes with an extended vs standard dose schedule.
Clinical results
Only one clinical trial (reported in three publications)8, 9, 10 evaluated the number of episodes of severe RVGE. In this randomised controlled trial of 2974 participants in South Africa and Malawi, the additional dose of oral Rotarix was administered early or ‘before’ the standard schedule (6/10/14 wks vs 10/14 wks). The primary outcome was severe rotavirus gastroenteritis defined as episodes of gastroenteritis with a Vesikari score ≥ 11.5 No hospitalisation data was reported for the 3-dose vs 2-dose schedule. In total, 26 of 1478 (1·8%, 95% CI 1·2 to 2·6%) children were reported to have at least one episode of severe RVGE in the 3-dose Rotarix group in the first year of life, compared to 30 of 1496 (2·0%, 95%CI 1·4 to 2.9%) in the 2-dose Rotarix group. This corresponds to RR 0·88, 95% CI, 0·52 to 1·48 (risk difference = 0·2%) (see Figure 3). At least one episode of gastroenteritis in the second year of life was reported for 13 of 746 children in the 3-dose Rotarix group vs 22 of 754 children in the 2-dose group, for the combined South Africa and Malawi cohorts. This corresponds to a combined RR 0·62, 95%CI, 0·31 to 1·23 (risk difference = 1·2%) (see Figure 4), an estimated reduction in the risk of at least one episode of severe rotavirus gastroenteritis for 9 per 1000 vaccinated children (95%CI, 20 fewer to 7 more children with at least one episode of severe gastroenteritis per 1000 children) (see Table Two).
Figure 3.
Proportion of children with at least one episode of severe rotavirus gastroenteritis in additional dose vs standard dose schedule; first year of life.
Figure 4.
Proportion of children with at least one episode of severe rotavirus gastroenteritis in additional dose vs standard dose schedule; second year of life.
Additional results from the same clinical trial for any-severity RVGE and severe all-cause GE are provided in the Supplementary Materials. There was no data available on all-cause gastroenteritis and no data up to five years old.
Safety
One episode of intussusception was reported in the 7 clinical trials involving 4,399 children. This episode occurred 11 weeks after administration of a final dose of oral rotavirus vaccine in a child receiving an extended schedule and was assessed to be ‘not temporarily related’.9 Three deaths were reported in the same study (one in the extended schedule and two in the standard schedule); all three deaths occurred more than 42 days after administration of the last dose of oral rotavirus vaccine and none were assessed as vaccine related.9
GRADE assessment
A GRADE assessment was completed for pre-specified clinically important outcomes. The quality of evidence for immunogenicity outcomes was deemed moderate, after being downgraded one level due to high heterogeneity of included studies. An exception was the ‘booster-dose’ subgroup analysis where the results were more similar (moderate heterogeneity, I2 = 56%) and the quality of evidence remained high (see Table Two). The quality of evidence for reduction in diarrhoea outcome was deemed moderate downgraded one level for imprecision due to the confidence intervals around both relative and absolute estimates of vaccine effect including either a potential increase or decrease in the number of vaccinated children with an episode of diarrhoea (see Table Two).18
Discussion
Our review of seven clinical trials involving over 4000 children aged <2 years old suggests that extended or additional dose oral rotavirus vaccine schedules improve rotavirus vaccine immune responses compared to routine or standard schedules, with an estimated 140 additional children per 1000 vaccinated (95%CI, 22 to 275 children) demonstrating evidence of IgA seroresponse, albeit with moderate to high heterogeneity across trials. Point estimates of vaccine immune response were higher when the additional rotavirus vaccine dose was administered as a booster dose in the second six months of life (168 additional children per 1000 vaccinated; 95%CI, 84 to 269 per 1000 children) rather than as an extended primary course (118 additional children per 1000 vaccinated; 95%CI, 56 fewer to 364 more per 1000 children), but the confidence intervals were wide and overlapping. Likewise, point estimates of the vaccine immune response were also higher among infants who were seronegative at baseline (255 additional children per 1000 vaccinated; 95%CI, 81 to 510 per 1000 children), although it is not feasible to routinely test for serostatus prior to vaccination. The overall certainty of evidence is assessed as moderate, downgraded one level due to the high heterogeneity in results among the included studies.
There is very little clinical information from randomised trials available on the effect of an extended or additional dose oral rotavirus vaccine schedule on the frequency of diarrhoeal disease. In this review, only one study was found to evaluate and report on this clinical outcome with insufficient data to conclude whether there was any clinical benefit or not. It should be noted that this clinical trial was conducted with three study arms – extended dose schedule (3-doses) vs standard schedule (2-doses) vs placebo, and none of the groups had high rates of rotavirus diarrhoea. The results suggested that for populations with similar rates of disease, an extended schedule is unlikely to reduce the risk of severe rotavirus disease by more than 2% in the first or second year. The overall certainty of the evidence is moderate, downgraded one level due to imprecision.
Our results are consistent with two previous systematic reviews which found weak evidence of increased immune responses when the additional rotavirus vaccine dose was administered in the first six months of life as part of the primary schedule.6,19 However, our review is the first to include data on ‘booster dose’ studies where the additional dose is administered in the second six months of life. We hypothesise that declining levels of circulating maternal antibodies and maturation of the infant's immune system contribute to the greater effectiveness of additional doses administered to infants >6 months old.
Importantly, given the increased risk of intussusception observed with Rotashield (a rhesus derived rotavirus vaccine licensed in the 1990s),4 in our review only one episode of intussusception was reported among more than 4000 clinical trial participants. This episode occurred more than 11 weeks after the last administered dose of oral rotavirus vaccine in a child receiving an extended schedule which is likely to be outside the aetiologic window for vaccine-induced intussusception. It should be noted, however, that the pathogenic mechanisms involved in intussusception following rotavirus vaccination remain uncertain and intussusception incidence, ascertainment and fatality rate varies widely between populations, being highly dependent upon access to medical treatment among other factors.22 While vaccine-associated intussusception is typically defined as occurring within 21 days of receipt of rotavirus vaccine23 and all included studies followed participants for a minimum of 28 days, caution is warranted when applying these findings to other settings.
Data on pre-specified outcomes was available for all seven studies. Most data was for oral Rotarix rotavirus vaccine. Only one of the included studies evaluated an additional dose of RotaTeq rotavirus vaccine (though results were consistent) and no studies evaluated additional doses of Rotasiil or Rotavac. The RotaTeq study reported a 3-fold rise in IgA titre as the primary outcome. However, the study also reported anti-rotavirus IgA levels < and ≥ 20IU/ml following the additional vs standard dose schedule, and these values were used in the meta-analysis to enable direct comparison with the Rotarix studies.
One potentially relevant study was identified in the screening process through correspondence with domain experts and located in the Pan African Clinical Trial Registry. This randomised study of 214 children in Zambia will evaluate the immunological effect of a two-dose Rotarix schedule (6wks, 10wks) vs three-dose Rotarix schedule (6wks, 10wks, 9mths); data for this study was not available at the time of our review. Two additional dose studies were excluded after ‘full text review’ as per our protocol because they compared additional dose schedules to other ‘non-standard’ schedules. One of these studies compared 3-doses vs 5-doses of Rotarix among 90 children in southern India. This study reported vaccine seroresponses (anti-rotavirus IgA ≥ 20IU/ml) in 36 of 44 children who received 3-doses of Rotarix vs 32 of 44 children who received 5-doses of Rotarix.20 The authors concluded no added benefit from the 5-dose vs 3-dose schedule, but the sample size was small. The second study compared 3-doses of Rotarix vs 3-doses of placebo among 100 HIV positive children in South Africa. Among children who were seronegative at baseline, this study reported IgA ≥ 20 IU/ml among 57·1% (95%CI 34% to 78·2%) of 25 children in the 3-dose Rotarix group, and among 18·2% (95%CI 5·2% to 40·3%) of 25 children in the placebo group.21 Episodes of rotavirus gastroenteritis were reported in 4 children in the 3-dose Rotarix group and 4 children in the placebo group.21
We limited this review by excluding studies which evaluated mixed rotavirus vaccine schedules, additional dose schedules of non-WHO prequalified rotavirus vaccines, and studies comparing additional dose schedules to other non-standard schedules. We therefore cannot draw any conclusions about these alternative vaccine strategies. Currently these approaches are not recommended by the World Health Organisation Strategic Advisory Group of Experts, but this may change in future years.
Our review suggests that an extended or additional dose schedule of oral rotavirus vaccines incrementally improves vaccine immune responses compared to a routine or standard dose schedule. However, while measures of increased immunogenicity tend to broadly reflect improved oral vaccine performance,6 protection against wild-type rotavirus infection is mediated by both humoral and cellular components of the immune system22 and anti-rotavirus IgA is a weak correlate of protection.24 Vaccine-induced anti rotavirus IgA titres may be influenced by exposure to natural infection, and the age at which children are first exposed to rotavirus may vary between populations; the median age of rotavirus positive hospital admissions is reported to be 38 weeks (IQR, 25 – 58 weeks) in countries with very high child mortality, compared to 65 weeks (IQR, 40 – 107 weeks in countries with low child mortality.25 Similarly, although all four WHO prequalified oral rotavirus vaccines are live attenuated vaccines and serum anti-rotavirus IgA antibody responses have been used as a measure of immunogenicity for all products,22 few studies have directly compared the immune response between rotavirus vaccines26,27 limiting the ability to generalise our immunological results to Rotasiil or Rotavac. For these reasons, evidence of increased vaccine seroresponse is insufficient to change vaccine policy or clinical practice.
Only one study,8, 9, 10 evaluated the effect of additional vaccine doses on the frequency of diarrhoeal disease. However, this study reported low rates of rotavirus disease and gave the additional Rotarix dose ‘early’ at six weeks old when vaccine responses might be impaired by high levels of maternal-derived vaccine-neutralising antibodies and immature infant immune function.3 This trial also reported diarrhoea severity as per Vesikari score rather than as per hospitalisation.5 Despite the evidence of improved immune responses, clinical trials to assess and quantify the clinical benefit of adding a dose of oral rotavirus vaccine against severe disease are warranted before any strategy can be implemented in settings with high residual burden of disease. In settings where it is highly feasible to deliver vaccines after 6 months old, there is biological rationale for delaying such a dose, although the evidence favouring a later versus earlier dose remains weak.
In conclusion, it is important to find pragmatic strategies to improve the impact of rotavirus vaccines in settings where the burden of rotavirus infection remains unacceptably high. Our systematic review found moderate to high level of evidence that administration of additional doses of oral rotavirus vaccines as part of an extended schedule is likely to result in improved vaccine immune responses, including when the additional doses are administered as a booster dose to children older than 6-months old. However, further research is needed to evaluate whether there is a meaningful impact on diarrhoeal disease before additional dose rotavirus vaccine schedules can be recommended as vaccine policy.
Contributors
BFM wrote the first draft of the report with input from PF, TLS and PM. BFM and TLS conceived the study. BFM, PF, TLS, PM contributed to the study protocol. BFM and PF screened all titles and abstracts, and independently extracted data. BFM completed the analysis under the supervision of PM. All authors had full access to all the data in the study, contributed to the manuscript and had final responsibility for the decision to submit for publication. All authors meet the requirements for authorship inclusion and have seen and approved the final version of the manuscript.
Data sharing statement
All aggregated data used in the meta-analysis will be accessible under request by contacting the corresponding author: Bianca Middleton (bianca.middleton@menzies.edu.au).
Declaration of interests
The authors declare no competing interests.
Acknowledgement
BM is supported by an NHMRC Postgraduate Scholarship (1134095), a RACP P&CHD NHMRC Scholarship and a Douglas and Lola Douglas Scholarship in Medical Science, Australian Academy of Science.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101687.
Appendix. Supplementary materials
References
- 1.Henschke N, Bergman H, Hungerford D, et al. The efficacy and safety of rotavirus vaccines in countries in Africa and Asia with high child mortality. Vaccine. 2022;40(12):1707–1711. doi: 10.1016/j.vaccine.2022.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burnett E, Parashar UD, Tate JE. Real-world effectiveness of rotavirus vaccines, 2006-19: a literature review and meta-analysis. Lancet Glob Health. 2020;8(9):e1195–e1202. doi: 10.1016/S2214-109X(20)30262-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Velasquez DE, Parashar UD, Jiang B. Decreased performance of live attenuated, oral rotavirus vaccines in low-income settings: causes and contributing factors. Expert Rev Vaccines. 2018;17(2):145–161. doi: 10.1080/14760584.2018.1418665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organisation Rotavirus vaccines: WHO position paper - January 2013. Wkly Epidemiol Rec. 2013;31(52):6170–6171. [Google Scholar]
- 5.Ruuska T, Vesikari T. Rotavirus disease in Finnish children: use of numerical scores for clinical severity of diarrhoeal episodes. Scand J Infect Dis. 1990;22(3):259–267. doi: 10.3109/00365549009027046. [DOI] [PubMed] [Google Scholar]
- 6.Church J, Parker E, Kirkpatrick B, Grassly N, Prendergast AJ. Interventions to improve oral vaccine performance: a systematic review and meta-analysis. Lancet Infect Dis. 2019;19(2):203–214. doi: 10.1016/S1473-3099(18)30602-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins JPT, Thomas J, Chandler J, et al. 2nd ed. John Wiley & Sons; Chichester (UK): 2019. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- 8.Cunliffe NA, Witte D, Ngwira BM, et al. Efficacy of human rotavirus vaccine against severe gastroenteritis in Malawian children in the first two years of life: a randomized, double-blind, placebo controlled trial. Vaccine. 2012;30(suppl 1):A36–A43. doi: 10.1016/j.vaccine.2011.09.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madhi SA, Cunliffe NA, Steele D, et al. Effect of human rotavirus vaccine on severe diarrhea in African infants. NEngl J Med. 2010;362(4):289–298. doi: 10.1056/NEJMoa0904797. [DOI] [PubMed] [Google Scholar]
- 10.Madhi SA, Kirsten M, Louw C, et al. Efficacy and immunogenicity of two or three dose rotavirus-vaccine regimen in South African children over two consecutive rotavirus-seasons: a randomized, double-blind, placebo-controlled trial. Vaccine. 2012;30(suppl 1):A44–A51. doi: 10.1016/j.vaccine.2011.08.080. [DOI] [PubMed] [Google Scholar]
- 11.Bines JE, Kohl KS, Forster J, et al. Acute intussusception in infants and children as an adverse event following immunization: case definition and guidelines of data collection, analysis, and presentation. Vaccine. 2004;22(5-6):569–574. doi: 10.1016/j.vaccine.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Steele AD, Reynders J, Scholtz F, et al. Comparison of 2 different regimens for reactogenicity, safety, and immunogenicity of the live attenuated oral rotavirus vaccine RIX4414 coadministered with oral polio vaccine in South African infants. J Infect Dis. 2010;202(suppl):S93–100. doi: 10.1086/653550. [DOI] [PubMed] [Google Scholar]
- 13.Ali SA, Kazi A, Cortese MM, et al. Impact of different dosing schedules on the immunogenicity of the human rotavirus vaccine in infants in Pakistan: a randomized trial. J Infect Dis. 2014;210(11):1772–1779. doi: 10.1093/infdis/jiu335. [DOI] [PubMed] [Google Scholar]
- 14.Armah G, Lewis KD, Cortese MM. A randomized, controlled trial of the impact of alternative dosing schedules on the immune response to human rotavirus vaccine in rural Ghanaian infants. J Infect Dis. 2016;213(11):1678–1685. doi: 10.1093/infdis/jiw023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haidara C, Tapia MD, Sow SO, et al. Evaluation of a booster dose of pentavalent rotavirus vaccine coadministered with measles, yellow fever, and meningitis a vaccines in 9-month-old Malian infants. J Infect Dis. 2018;218(4):606–613. doi: 10.1093/infdis/jiy215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Middleton BF, Danchin M, Jones MA, et al. Immunogenicity of a third scheduled dose of rotarix in Australian indigenous infants: a phase IV, double-blind, randomised, placebo-controlled clinical trial. J Infect Dis. 2022;20:1–8. doi: 10.1093/infdis/jiac038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zaman K, Fleming JA, Victor JC, et al. Noninterference of rotavirus vaccine with measles-rubella vaccine at 9 months of age and improvements in antirotavirus immunity: a randomized trial. J Infect Dis. 2016;213(11):1686–1693. doi: 10.1093/infdis/jiw024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schunemann H, Brozek J, Gyatt G, Oxman H. GRADE Handbook. 2013. Extracted March 29, 2022. https://gdt.gradepro.org/app/handbook/handbook.html
- 19.Gruber JF, Gruber LM, Weber RP, Becker-Dreps S, Jonsson Funk M. Rotavirus vaccine schedules and vaccine response among infants in low- and middle-income countries: a systematic review. Open Forum Infect Dis. 2017;4(2):1–10. doi: 10.1093/ofid/ofx066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kompithra RZ, Paul A, Manoharan D, et al. Immunogenicity of a three dose and five dose oral human rotavirus vaccine (RIX4414) schedule in south Indian infants. Vaccine. 2014;32(suppl 1):A129–A133. doi: 10.1016/j.vaccine.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Steele AD, Madhi SA, Louw CE, et al. Safety, reactogenicity, and immunogenicity of human rotavirus vaccine RIX4414 in human immunodeficiency virus-positive infants in South Africa. Pediatr Infect Dis J. 2011;30(2):125–130. doi: 10.1097/INF.0b013e3181f42db9. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organisation Rotavirus: vaccines: WHO position paper – July 2021. Wkly Epidemiol Rec. 2021;96(28):301–319. [Google Scholar]
- 23.Sheel M, Wood N, Macartney K, et al. Severity of rotavirus-vaccine-associated intussusception: prospective hospital-based surveillance, Australia, 2007-2018. Pediatr Infect Dis J. 2022;41(6):507–513. doi: 10.1097/INF.0000000000003521. [DOI] [PubMed] [Google Scholar]
- 24.Lee B, Carmolli M, Dickson DM, et al. Rotavirus-specific immunoglobulin A responses are impaired and serve as a suboptimal correlate of protection among infants in Bangladesh. Clin Infect Dis. 2018;67(2):186–192. doi: 10.1093/cid/ciy076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Global Rotavirus Surveillance Network and Rotavirus Age Study Collaborators. Hasso-Agopsowicz M, Lavada CN, Lopman B, et al. Global review of the age distribution of rotavirus disease in children aged < 5 years before the introduction of rotavirus vaccination. Clin Infect Dis. 2019;69:1071–1078. doi: 10.1093/cid/ciz060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Libster R, McNeal M, Walter EB, et al. Safety and immunogenicity of sequential rotavirus vaccine schedules. Pediatrics. 2016;137(2) doi: 10.1542/peds.2015-2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Velasquez-Portocarrero DE, Wang X, Cortese MM, et al. Head-to-head comparison of the immunogenicity of RotaTeq and Rotarix rotavirus vaccines and factors associated with seroresponse in infants in Bangladesh: a randomised, controlled, open-label, parallel, phase 4 trial. Lancet Infect Dis. 2022 doi: 10.1016/S1473-3099(22)00368-1. online ahead of print on Aug 9, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.