Abstract
The risk factors for recurrence of hemorrhagic or ischemic stroke in patients with intracranial hemorrhage (ICH) are inconclusive. This study was designed to investigate the risk factors for stroke recurrence and the impact of antiplatelet on stroke recurrence in patients with ICH. This population-based case-cohort study analyzed the data obtained from a randomized sample of 2 million subjects in the Taiwan National Health Insurance Research Database. The survival of patients with hemorrhagic stroke from January 1, 2000, to December 31, 2013, was included in the study. During the 5-year follow-up period, the recurrence rate of stroke was 13.1% (7.01% hemorrhagic stroke, and 6.12% ischemic stroke). The recurrence rate of stroke was 13.3% in the without antiplatelet group and 12.6% in the antiplatelet group. The risk factor for hemorrhagic stroke was hypertension (OR 1.87). The risk factors for ischemic stroke were age (OR 2.99), diabetes mellitus (OR 1.28), hypertension (OR 2.68), atrial fibrillation (OR 1.97), cardiovascular disease (OR 1.42), and ischemic stroke history (OR 1.68). Antiplatelet may decrease risk of hemorrhagic stroke (OR 0.53). The risk of stroke recurrence is high in patients with ICH. Hypertension is a risk factor for ischemic and hemorrhagic stroke recurrence. Antiplatelet therapy does not decrease risk of ischemic stroke recurrence but may reduce recurrence of hemorrhagic stroke.
Subject terms: Diseases, Medical research, Neurology, Risk factors
Introduction
Though the incidence and mortality rates of stroke with intracranial hemorrhage (ICH) declined gradually1, hemorrhagic stroke still accounts for 10–20% of patients with stroke2–4. The global burden of hemorrhagic stroke is gradually increasing. Risk factors for ICH included hypertension and warfarin use5–7. The survival outcomes after hemorrhagic stroke include mortality, functional impairment, quality of life impairment, intracerebral hemorrhage recurrence, ischemic stroke, cognitive impairment, psychiatric diseases, and epilepsy8. The annual rate of stroke recurrence after ICH was approximately 5–10%9,10. However, the report on the type of recurrent stroke after the patients with ICH is inconclusive. Studies have reported that patients with ICH have a higher risk of hemorrhage recurrence than those with ischemic stroke11,12. Some studies have reported that patients with deep ICH have a higher risk of ischemic stroke recurrence than those with hemorrhagic stroke and those with lobar hemorrhage have an increased risk of hemorrhagic stroke recurrence10. However, some studies have found that the type of recurrent stroke was not significantly different between patients with lobar hemorrhage and those with deep hemorrhage stroke9,13. Murthy et al. have found that compared with individuals without ICH, patients with ICH have an increased risk of ischemic stroke with a hazard ratio (HR) of 3.114.
A study has shown that inadequate blood pressure control increases the probability of ICH recurrence15. In patients with ICH who received antiplatelet drugs, the rate of ICH recurrence and hemorrhage volume did not increase16,17. In contrast, Biffi et al. have found that the use of antiplatelet drugs may increase the risk of ICH recurrence in patients with lobar hemorrhage15.
Stroke recurrence may increase mortality and impair daily activity and function. Presently, the risk factors for ischemic and hemorrhagic stroke recurrence remain inconclusive. Therefore, this study was designed to determine and investigate the risk factors for ischemic or hemorrhagic stroke recurrence and the impact of antiplatelet on stroke recurrence in patients with ICH in Taiwan.
Methods
Data source and ethics approval
This population-based case-cohort study used data from the Taiwan National Health Insurance Research Database (NHIRD) that comprises data obtained from 2 million individuals. The National Health Insurance (NHI) program in Taiwan has been operating since 1995. The NHIRD is a research database developed by the NHI Research Institute and contains patient healthcare data from hospitals, outpatient clinics, and community pharmacies. NHI encompasses more than 99% of 23 million individuals and 95% of the hospitals in Taiwan. The NHI Research Institute provides the database to researchers after anonymizing all personal information. This study included data retrieved from the “Longitudinal Health Insurance Database” (LHID 2005) from a random sample of 2 million individuals within the NHIRD, with linked longitudinal data available from 2000 to 2013. The randomized data (LHID 2005) represent all beneficiaries as no significant differences in sex, age, and premium rate are found between individuals in the LHID 2005 and the original NHIRD datasets. The codes of the International Classification of Diseases, Ninth Revision (ICD-9) were used to define diseases. This study was approved by the Institutional Review Board of Ditmanson Medical Foundation Chiayi Christian Hospital, Taiwan (CYCH-IRB: 2020131). Due to the anonymity of the NHIRD, the requirement for informed consent from each patients was waived by the IRB of Ditmanson Medical Foundation Chiayi Christian Hospital.
Study subjects and definitions
Hemorrhagic stroke was defined as an episode of rapidly developing neurological deficit attributed to the focal collection of blood within the brain parenchyma or ventricular system (ICH) or due to subarachnoid bleeding (subarachnoid hemorrhage) not caused by trauma18. All hospitalized patients with the diagnosis of hemorrhagic stroke (ICD-9 codes: 430 and 431) between January 1, 2000 and December 31, 2013 were included in the study. Recurrent hemorrhagic stroke was defined as patient re-hospitalization with a discharge diagnosis of hemorrhagic stroke (ICD-9 codes: 430 and 431). Recurrent ischemic stroke was defined as patient re-hospitalization with a discharge diagnosis of ischemic stroke (ICD-9 codes, 433, 434, and 436). Stroke risk factors were defined as the following disease diagnosis during discharge in patients with hemorrhagic stroke: hypertension (ICD-9 code, 401, 405), diabetes mellitus (ICD-9 code, 250, 648), atrial fibrillation (ICD-9 code, 427), cardiovascular disease (ICD-9 code, 492, 648), congestive heart failure (ICD-9 code, 402, 404, 428), and dyslipidemia (ICD-9 code, 272). All patients underwent computed tomography or magnetic resonance imaging to confirm the occurrence of stroke. The exclusion criteria were as follows: (1) patients younger than 20 years; (2) those who had a history of hemorrhagic stroke; (3) those who continue to use antiplatelet drugs for more than 7 days 1 month before the onset of hemorrhagic stroke; (4) those with stroke recurrence within 1 month before hemorrhagic stroke onset; and (5) those who died within 1 month after stroke onset.
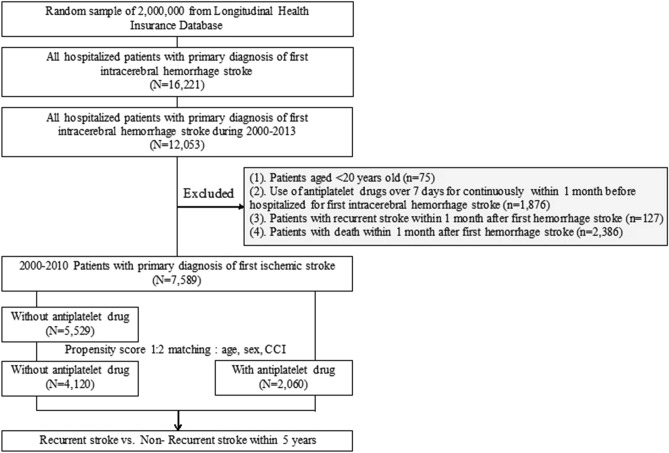
In total, 12,053 patients were hospitalized under the discharge diagnosis of hemorrhagic stroke. Among them, 75 patients were younger than 20 years, 1876 patients used antiplatelet drugs for more than 7 days within 1 month before stroke onset, 127 patients had stroke recurrence within 1 month after stroke onset, and 2386 patients died within 1 month after stroke onset, all of whom were excluded from this study. Finally, 7589 patients were included in the study (Fig. 1). The patients who continued to use one or two of the drugs—aspirin, ticlopidine, and clopidogrel—were classified in the use antiplatelet group.
Figure 1.
Flow chart of patient enrollment. CCI: clinical comorbidity index.
Separate propensity score matches were performed using a ratio of 1:2 to compare the risk of stroke recurrence between the groups with and without the use of antiplatelet drugs. All methods were performed in accordance with the relevant guidelines and regulations.
Outcome measure
The primary endpoint of this study was new-onset hemorrhagic or ischemic stroke.
Statistical analysis
In this study, we compared the rate of stroke recurrence between patients who used antiplatelet drugs and those who did not receive antiplatelet drugs using propensity score matching with a ratio of 1:2 to match the study patients based on age, sex, and clinical comorbidity index (CCI). The baseline characteristics of the patients as categorical variables were compared using the chi-square test. Continuous variables were compared using the t-test. Cox proportional hazards regression models were used to evaluate the HRs and 95% confidence intervals (CIs) for the recurrence of ischemic and hemorrhagic stroke in each risk factor. All statistical analyses were performed using SAS statistical software (version 9.4; SAS Institute, Inc, Cary, NC). P < 0.05 was considered statistically significant.
Results
From 2000 to 2013, 7589 patients fulfilled the inclusion criteria for this study. The characteristics of the 7589 patients are shown in Table 1. After 1:2 propensity score matching for sex, age, and CCI, 6180 patients were included in the analysis, including 4120 patients in the without antiplatelet group and 2060 patients in the antiplatelet group. The area under the curve of the propensity score was 0.544. After propensity score matching, age, sex, stroke severity, and ischemic stroke history were not significantly different between the without antiplatelet and antiplatelet groups. The probability of admission to the intensive care unit and hospitalization day longer than 9 days was higher in the without antiplatelet group. The rates of diabetes mellitus, hypertension, hyperlipidemia, atrial fibrillation, cardiovascular disease, and congestive heart failure were higher in the antiplatelet group (Table S1).
Table 1.
Characteristics of the patients with hemorrhagic stroke (n = 7589).
| Variables | Without antiplatelet (n = 5529) |
Antiplatelet (n = 2060) |
P |
|---|---|---|---|
| Age | |||
| 20–44 | 832 (15.05) | 138 (6.70) | < 0.0001 |
| 45–59 | 1960 (35.45) | 744 (36.12) | |
| ≥ 60 | 2737 (49.50) | 1178 (57.18) | |
| Mean ± SD | 60.09 ± 15.16 | 62.27 ± 12.31 | |
| Sex | |||
| Female | 2176 (39.36) | 802 (38.93) | 0.7365 |
| Male | 3353 (60.64) | 1258 (61.07) | |
| Length of stay, days | |||
| < 9 | 1236 (22.35) | 595 (28.88) | < 0.0001 |
| ≥ 9 | 4293 (77.65) | 1465 (71.12) | |
| ICU | |||
| No | 4294 (77.66) | 1742 (84.56) | < 0.0001 |
| Yes | 1235 (22.34) | 318 (15.44) | |
| CCI, mean ± SD | |||
| < 5 | 3711 (67.12) | 1318 (63.98) | 0.0101 |
| ≥ 5 | 1818 (32.88) | 742 (36.02) | |
| Mean ± SD | 3.96 ± 2.76 | 4.16 ± 2.72 | 0.0040 |
| Diabetes mellitus | |||
| No | 3917 (70.84) | 1334 (64.76) | < 0.0001 |
| Yes | 1612 (29.16) | 726 (35.24) | |
| Hypertension | |||
| No | 751 (13.58) | 91 (4.42) | < 0.0001 |
| Yes | 4778 (86.42) | 1969 (95.58) | |
| Hyperlipidemia | |||
| No | 3955 (71.53) | 1295 (62.86) | < 0.0001 |
| Yes | 1574 (28.47) | 765 (37.14) | |
| AF | |||
| No | 5332 (96.44) | 1937 (94.03) | < 0.0001 |
| Yes | 197 (3.56) | 123 (5.97) | |
| CVD | |||
| No | 4289 (77.57) | 1298 (63.01) | < 0.0001 |
| Yes | 1240 (22.43) | 762 (36.99) | |
| CHF | |||
| No | 3250 (58.78) | 914 (44.37) | < 0.0001 |
| Yes | 2279 (41.22) | 1146 (55.63) | |
| The history of IS | |||
| No | 5314 (96.11) | 1958 (95.05) | 0.0396 |
| Yes | 215 (3.89) | 102 (4.95) | |
| Recurrent stroke | |||
| No | 4792 (86.67) | 1800 (87.38) | < 0.0001 |
| Yes | 737 (13.33) | 260 (12.62) | |
| IS | 306 (5.53) | 159 (7.72) | 0.0004 |
| Hemorrhagic stroke | 431 (7.79) | 101 (4.90) | < 0.0001 |
ICU, intensive care unit; CCI, clinical comorbidity index; AF, atrial fibrillation; CHF, congestive heart failure; IS, ischemic stroke; SD, standard deviation; CVD, cardiovascular disease.
During the 5-year follow-up period, stroke in 997 patients recurred; the recurrence rate of stroke was 13.1% (997/7589), of whom 7.01% (532/7589) had hemorrhagic stroke and 6.12% (465/7589) had ischemic stroke. The rate of stroke recurrence was 13.3% (737/5529) in the without antiplatelet group and 12.6% (260/2060) in the antiplatelet group. Moreover, the rate of hemorrhagic stroke recurrence was lower in the antiplatelet group and the rate of ischemic stroke recurrence was higher in the antiplatelet group. The recurrence rates of hemorrhagic stroke were 7.79% (431/5529) and 4.9% (101/2060) in the without antiplatelet and antiplatelet groups (P < 0.01), while the recurrence rates of ischemic stroke were5.53% (306/5529) and 7.72% (159/2060) (P < 0.01) respectively.
The risk factors for ischemic stroke recurrence were age, sex, diabetes mellitus, hypertension, atrial fibrillation, cardiovascular disease, and ischemic stroke history. The HR of ischemic stroke was 2.17 (95% CI 1.38–3.41) in patients aged between 45 and 59 years and 2.99 (95% CI 1.91–4.68) in patients aged ≥ 60 years. The HR of ischemic stroke was 1.28 (95% CI 1.04–1.57) in patients with diabetes mellitus, 2.68 (95% CI 1.55–4.63) in patients with hypertension, 1.97 (95% CI 1.40–2.76) in patients with atrial fibrillation, 1.42 (95% CI 1.15–1.74) in patients with cardiovascular disease, and 1.69 (95% CI 1.18–2.40) in patients with a history of ischemic stroke. The antiplatelet group did not reduce risk of ischemic stroke with an HR of 0.90 (95% CI 0.74–1.09) (Table 2).
Table 2.
The relationship between antiplatelet agent use and 5-year rate of ischemic stroke recurrence among patients with first-time hemorrhage stroke (n = 7589).
| Variables | Number | Number of IS event | Person-years | Incidence rate per 100 person-years | Crude HR (95% CI) | Adjusted HR (95% CI) |
|---|---|---|---|---|---|---|
| Age | ||||||
| 20–44 | 970 | 22 | 4259.6 | 0.52 | Ref | Ref |
| 45–59 | 2704 | 157 | 11,294.0 | 1.39 | 2.68 (1.71–4.18) | 2.17 (1.38–3.41) |
| ≥ 60 | 3915 | 286 | 13,318.7 | 2.15 | 4.05 (2.62–6.24) | 2.99 (1.91–4.68) |
| Sex | ||||||
| Female | 2978 | 171 | 11,381.1 | 1.50 | Ref | Ref |
| Male | 4611 | 294 | 17,491.3 | 1.68 | 1.12 (0.93–1.35) | 1.23 (1.02–1.49) |
| Length of stay, days | ||||||
| < 9 | 1831 | 140 | 7485.4 | 1.87 | Ref | Ref |
| ≥ 9 | 5758 | 325 | 21,386.9 | 1.52 | 0.81 (0.66–0.99) | 0.90 (0.73–1.11) |
| ICU | ||||||
| No | 6036 | 399 | 23,614.7 | 1.69 | Ref | Ref |
| Yes | 1553 | 66 | 5257.6 | 1.26 | 0.74 (0.57–0.96) | 0.86 (0.76–0.97) |
| CCI | ||||||
| < 5 | 5029 | 295 | 20,121.6 | 1.47 | Ref | Ref |
| ≥ 5 | 2560 | 170 | 8750.7 | 1.94 | 1.29 (1.07–1.56) | 0.87 (0.70–1.08) |
| Antiplatelet agents | ||||||
| No | 5529 | 306 | 19,990.5 | 1.53 | Ref | Ref |
| Yes | 2060 | 159 | 8881.8 | 1.79 | 1.18 (0.97–1.43) | 0.90 (0.74–1.09) |
| Diabetes mellitus | ||||||
| No | 5251 | 286 | 20,459.9 | 1.40 | Ref | Ref |
| Yes | 2338 | 179 | 8412.4 | 2.13 | 1.50 (1.25–1.81) | 1.28 (1.04–1.57) |
| Hypertension | ||||||
| No | 842 | 14 | 3237.6 | 0.43 | Ref | Ref |
| Yes | 6747 | 451 | 25,634.7 | 1.76 | 4.02 (2.36–6.84) | 2.68 (1.55–4.63) |
| Hyperlipidemia | ||||||
| No | 5250 | 287 | 19,453.8 | 1.48 | Ref | Ref |
| Yes | 2339 | 178 | 9418.5 | 1.89 | 1.29 (1.07–1.55) | 1.11 (0.92–1.35) |
| AF | ||||||
| No | 7269 | 425 | 27,910.2 | 1.52 | Ref | Ref |
| Yes | 320 | 40 | 962.1 | 4.16 | 2.64 (1.91–3.65) | 1.97 (1.40–2.76) |
| CVD | ||||||
| No | 5587 | 291 | 21,742.8 | 1.34 | Ref | Ref |
| Yes | 2002 | 174 | 7129.5 | 2.44 | 1.80 (1.49–2.17) | 1.42 (1.15–1.74) |
| CHF | ||||||
| No | 4164 | 220 | 16,216.6 | 1.36 | Ref | Ref |
| Yes | 3425 | 245 | 12,655.8 | 1.94 | 1.41 (1.18–1.69) | 0.98 (0.81–1.20) |
| The history of IS | ||||||
| No | 7272 | 429 | 27,966.0 | 1.53 | Ref | Ref |
| Yes | 317 | 36 | 906.3 | 3.97 | 2.51 (1.79–3.53) | 1.69 (1.18–2.40) |
ICU, intensive care unit; CI, confidence interval; AF, atrial fibrillation; CHF, congestive heart failure; IS, ischemic stroke; HR, hazard ratio; CVD, cardiovascular disease.
The factors for hemorrhagic stroke recurrence included hypertension. The HR of hemorrhagic stroke was 1.87 (95% CI 1.32–2.64) in patients with hypertension. After adjusting for possible confounding factors (age, sex, stroke severity, diabetes mellitus, hypertension, hyperlipidemia, atrial fibrillation, cerebrovascular disease, congestive heart failure, and ischemic stroke history), the use of antiplatelet drugs was found to decrease the risk of hemorrhagic stroke with an HR of 0.53 (95% CI 0.42–0.66) (Table 3).
Table 3.
The relationships between antiplatelet agent use and 5-year rate of hemorrhagic stroke recurrence among patients with first-time hemorrhagic stroke (n = 7589).
| Variables | Number | Number of HS event | Person-years | Incidence rate per 100 person-years | Crude HR (95% CI) | Adjusted HR (95% CI) |
|---|---|---|---|---|---|---|
| Age | ||||||
| 20–44 | 970 | 70 | 4259.6 | 1.64 | Ref | Ref |
| 45–59 | 2704 | 202 | 11,294.0 | 1.79 | 1.07 (0.82–1.41) | 0.93 (0.70–1.23) |
| ≥ 60 | 3915 | 260 | 13,318.7 | 1.95 | 1.11 (0.86–1.45) | 1.09 (0.90–1.32) |
| Sex | ||||||
| Female | 2978 | 208 | 11,381.1 | 1.83 | Ref | Ref |
| Male | 4611 | 324 | 17,491.3 | 1.85 | 1.01 (0.85–1.20) | 1.00 (0.84–1.19) |
| Length of stay, days | ||||||
| < 9 | 1831 | 134 | 7485.4 | 1.79 | Ref | Ref |
| ≥ 9 | 5758 | 398 | 21,386.9 | 1.86 | 1.03 (0.84–1.25) | 1.00 (0.82–1.23) |
| ICU | ||||||
| No | 6036 | 427 | 23,614.7 | 1.81 | Ref | Ref |
| Yes | 1553 | 105 | 5257.6 | 2.00 | 1.08 (0.87–1.34) | 0.99 (0.93–1.06) |
| CCI | ||||||
| < 5 | 5029 | 392 | 20,121.6 | 1.95 | Ref | Ref |
| ≥ 5 | 2560 | 140 | 8750.7 | 1.60 | 0.78 (0.65–0.95) | 0.79 (0.64–0.98) |
| Antiplatelet agents | ||||||
| No | 5529 | 431 | 19,990.5 | 2.16 | Ref | Ref |
| Yes | 2060 | 101 | 8881.8 | 1.14 | 0.54 (0.44–0.67) | 0.53 (0.42–0.66) |
| Diabetes mellitus | ||||||
| No | 5251 | 390 | 20,459.9 | 1.91 | Ref | Ref |
| Yes | 2338 | 142 | 8412.4 | 1.69 | 0.86 (0.71–1.05) | 0.97 (0.79–1.20) |
| Hypertension | ||||||
| No | 842 | 39 | 3237.6 | 1.20 | Ref | Ref |
| Yes | 6747 | 493 | 25,634.7 | 1.92 | 1.57 (1.13–2.17) | 1.87 (1.32–2.64) |
| Hyperlipidemia | ||||||
| No | 5250 | 392 | 19,453.8 | 2.02 | Ref | Ref |
| Yes | 2339 | 140 | 9418.5 | 1.49 | 0.75 (0.62–0.91) | 0.78 (0.64–0.96) |
| AF | ||||||
| No | 7269 | 510 | 27,910.2 | 1.83 | Ref | Ref |
| Yes | 320 | 22 | 962.1 | 2.29 | 1.16 (0.76–1.78) | 1.32 (0.85–2.04) |
| CVD | ||||||
| No | 5587 | 419 | 21,742.8 | 1.93 | Ref | Ref |
| Yes | 2002 | 113 | 7129.5 | 1.58 | 0.80 (0.65–0.99) | 0.89 (0.71–1.11) |
| CHF | ||||||
| No | 4164 | 307 | 16,216.6 | 1.89 | Ref | Ref |
| Yes | 3425 | 225 | 12,655.8 | 1.78 | 0.92 (0.78–1.09) | 0.96 (0.80–1.16) |
| The history of IS | ||||||
| No | 7272 | 513 | 27,966.0 | 1.83 | Ref | Ref |
| Yes | 317 | 19 | 906.3 | 2.10 | 1.06 (0.67–1.67) | 1.14 (0.72–1.82) |
ICU, intensive care unit; CI, confidence interval; AF, atrial fibrillation; CHF, congestive heart failure; IS, ischemic stroke; HS, hemorrhagic stroke; CVD, cardiovascular disease.
When considering factors of sex, age, and stroke severity, we analyzed the risk factors of stroke recurrence in patients post propensity score matching (n = 6180).
The risk factors for ischemic stroke recurrence were age, sex, diabetes mellitus, hypertension, atrial fibrillation, cardiovascular disease, and ischemic stroke history. The HR of ischemic stroke was 1.98 (95% CI 1.10–3.57) in patients aged between 45 and 59 years and 2.49 (95% CI 1.38–4.47) in patients aged ≥ 60 years. The HR of ischemic stroke was 2.24 (95% CI 1.27–3.93) in patients with hypertension, 1.87 (95% CI 1.30–2.71) in patients with atrial fibrillation, 1.42 (95% CI 1.15–1.77) in patients with cardiovascular disease, and 1.56 (95% CI 1.06–2.30) in those with a history of ischemic stroke. The antiplatelet group did not reduce the risk of ischemic stroke with an HR of 0.80 (95% CI 0.70–1.05) (Table 4).
Table 4.
The relationship between antiplatelet agent use and 5-year rate of ischemic stroke recurrence among patients with first-time hemorrhagic stroke (n = 6180).
| Variables | Number | Number of IS event | Person-years | Incidence rate per 100 person-years | Crude HR (95% CI) | Adjusted HR (95% CI) |
|---|---|---|---|---|---|---|
| Age | ||||||
| 20–44 | 405 | 12 | 1782.4 | 0.67 | Ref | Ref |
| 45–59 | 2319 | 149 | 9696.5 | 1.54 | 2.27 (1.26–4.09) | 1.98 (1.10–3.57) |
| ≥ 60 | 3456 | 260 | 12,180.0 | 2.13 | 3.10 (1.75–5.53) | 2.49 (1.38–4.47) |
| Sex | ||||||
| Female | 2415 | 156 | 9258.4 | 1.68 | Ref | Ref |
| Male | 3765 | 265 | 14,400.5 | 1.84 | 1.09 (0.90–1.33) | 1.18 (0.96–1.45) |
| Length of stay, days | ||||||
| < 9 | 1502 | 129 | 6133.4 | 2.10 | Ref | Ref |
| ≥ 9 | 4678 | 292 | 17,525.5 | 1.67 | 0.79 (0.64–0.97) | 0.87 (0.7–1.09) |
| ICU | ||||||
| No | 4945 | 364 | 19,444.9 | 1.87 | Ref | Ref |
| Yes | 1235 | 57 | 4214.0 | 1.35 | 0.72 (0.54–0.95) | 0.86 (0.76–0.97) |
| CCI | ||||||
| < 5 | 4002 | 265 | 16,027.4 | 1.65 | Ref | Ref |
| ≥ 5 | 2178 | 156 | 7631.4 | 2.04 | 1.21 (0.99–1.48) | 0.93 (0.74–1.17) |
| Antiplatelet agents | ||||||
| No | 4120 | 262 | 14,777.1 | 1.77 | Ref | Ref |
| Yes | 2060 | 159 | 8881.8 | 1.79 | 1.02 (0.84–1.24) | 0.8 (0.7–1.05) |
| Diabetes mellitus | ||||||
| No | 4161 | 261 | 16,263.2 | 1.60 | Ref | Ref |
| Yes | 2019 | 160 | 7395.7 | 2.16 | 1.34 (1.10–1.63) | 1.21 (0.97–1.50) |
| Hypertension | ||||||
| No | 523 | 13 | 1944.2 | 0.67 | Ref | Ref |
| Yes | 5657 | 408 | 21,714.7 | 1.88 | 2.79 (1.60–4.84) | 2.24 (1.27–3.93) |
| Hyperlipidemia | ||||||
| No | 4185 | 264 | 15,572.2 | 1.70 | Ref | Ref |
| Yes | 1995 | 157 | 8086.7 | 1.94 | 1.15 (0.95–1.40) | 1.03 (0.84–1.27) |
| AF | ||||||
| No | 5919 | 388 | 22,843.5 | 1.70 | Ref | Ref |
| Yes | 261 | 33 | 815.3 | 4.05 | 2.32 (1.63–3.31) | 1.87 (1.30–2.71) |
| CVD | ||||||
| No | 4455 | 263 | 17,368.4 | 1.51 | Ref | Ref |
| Yes | 1725 | 158 | 6290.5 | 2.51 | 1.64 (1.35–2.00) | 1.42 (1.15–1.77) |
| CHF | ||||||
| No | 3267 | 197 | 12,734.5 | 1.55 | Ref | Ref |
| Yes | 2913 | 224 | 10,924.4 | 2.05 | 1.32 (1.09–1.59) | 1.01 (0.82–1.24) |
| The history of IS | ||||||
| No | 5905 | 391 | 22,855.6 | 1.71 | Ref | Ref |
| Yes | 275 | 30 | 803.3 | 3.73 | 2.13 (1.47–3.09) | 1.56 (1.06–2.30) |
ICU, intensive care unit; CI, confidence interval; AF, atrial fibrillation; CHF, congestive heart failure; IS, ischemic stroke; HR, hazard ratio; CVD, cardiovascular disease.
The factors for hemorrhagic stroke recurrence included hypertension. The HR of hemorrhagic stroke was 1.87 (95% CI 1.32–2.64) in patients with hypertension. The use of antiplatelet drugs was found to decrease the risk of hemorrhagic stroke with an HR of 0.52 (95% CI 0.42–0.66) (Table 5).
Table 5.
The relationships between antiplatelet agent use and 5-year rate of hemorrhagic stroke recurrence among patients with first-time hemorrhagic stroke (n = 6180).
| Variables | Number | Number of HS event | Person-years | Incidence rate per 100 person-years | Crude HR (95% CI) | Adjusted HR (95% CI) |
|---|---|---|---|---|---|---|
| Age | ||||||
| 20–44 | 405 | 30 | 1782.4 | 1.68 | Ref | Ref |
| 45–59 | 2319 | 165 | 9696.5 | 1.70 | 1.00 (0.68–1.48) | 1.10 (0.74–1.63) |
| ≥ 60 | 3456 | 260 | 12,180.0 | 1.90 | 1.07 (0.73–1.57) | 1.10 (0.89–1.35) |
| Sex | ||||||
| Female | 2415 | 156 | 9258.4 | 1.84 | Ref | Ref |
| Male | 3765 | 265 | 14,400.5 | 1.78 | 0.97 (0.80–1.18) | 0.95 (0.78–1.15) |
| Length of stay, days | ||||||
| < 9 | 1502 | 129 | 6133.4 | 1.87 | Ref | Ref |
| ≥ 9 | 4678 | 292 | 17,525.5 | 1.77 | 0.94 (0.76–1.16) | 0.90 (0.72–1.12) |
| ICU | ||||||
| No | 4945 | 364 | 19,444.9 | 1.78 | Ref | Ref |
| Yes | 1235 | 57 | 4214.0 | 1.90 | 1.05 (0.82–1.34) | 1.01 (0.95–1.07) |
| CCI | ||||||
| < 5 | 4002 | 265 | 16,027.4 | 1.90 | Ref | Ref |
| ≥ 5 | 2178 | 156 | 7631.4 | 1.59 | 0.80 (0.65–0.99) | 0.82 (0.65–1.04) |
| Antiplatelet agents | ||||||
| No | 4120 | 262 | 14,777.1 | 2.20 | Ref | Ref |
| Yes | 2060 | 159 | 8881.8 | 1.14 | 0.53 (0.42–0.66) | 0.52 (0.42–0.66) |
| Diabetes mellitus | ||||||
| No | 4161 | 261 | 16,263.2 | 1.86 | Ref | Ref |
| Yes | 2019 | 160 | 7395.7 | 1.68 | 0.89 (0.72–1.09) | 0.98 (0.78–1.23) |
| Hypertension | ||||||
| No | 523 | 13 | 1944.2 | 1.08 | Ref | Ref |
| Yes | 5657 | 408 | 21,714.7 | 1.87 | 1.71 (1.10–2.65) | 2.05 (1.31–3.22) |
| Hyperlipidemia | ||||||
| No | 4185 | 264 | 15,572.2 | 1.96 | Ref | Ref |
| Yes | 1995 | 157 | 8086.7 | 1.50 | 0.78 (0.63–0.96) | 0.81 (0.65–1.01) |
| AF | ||||||
| No | 5919 | 388 | 22,843.5 | 1.78 | Ref | Ref |
| Yes | 261 | 33 | 815.3 | 2.33 | 1.24 (0.78–1.96) | 1.40 (0.87–2.24) |
| CVD | ||||||
| No | 4455 | 263 | 17,368.4 | 1.91 | Ref | Ref |
| Yes | 1725 | 158 | 6290.5 | 1.51 | 0.78 (0.62–0.98) | 0.86 (0.67–1.10) |
| CHF | ||||||
| No | 3267 | 197 | 12,734.5 | 1.85 | Ref | Ref |
| Yes | 2913 | 224 | 10,924.4 | 1.75 | 0.94 (0.77–1.13) | 0.98 (0.80–1.20) |
| The history of IS | ||||||
| No | 5905 | 391 | 22,855.6 | 1.78 | Ref | Ref |
| Yes | 275 | 30 | 803.3 | 2.37 | 1.24 (0.79–1.97) | 1.35 (0.84–2.17) |
ICU, intensive care unit; CI, confidence interval; AF, atrial fibrillation; CHF, congestive heart failure; IS, ischemic stroke; HS, hemorrhagic stroke; CVD, cardiovascular disease.
Discussion
The main findings of this study include the following: (1) in patients with ICH stroke, the 5-year rate of stroke recurrence was 13.1%; (2) stroke recurrence was more frequent in patients with hemorrhagic stroke than that in patients with ischemic stroke with a ratio of 1.13; (3) antiplatelet therapy cannot decrease the risk of ischemic stroke but may decrease the risk of hemorrhagic stroke recurrence; (4) hypertension may increase the risk of hemorrhagic and ischemic stroke recurrence.
Studies have shown that in patients with ICH stroke who were followed for less than 3–5 years, the rate of hemorrhagic stroke recurrence was between 7 and 12%. In a single-center study, with a mean follow-up period of less than 3.6 years, Hill et al. have found that the rate of hemorrhagic stroke recurrence was 8.72% (15/172)10. Bailey et al. reviewed data with a mean follow-up of 3.4 person-year and found that the rate of hemorrhagic stroke recurrence was 8.35% (157/1880) and 2.4% per patient-year11. In a study with a follow-up duration of less than 5 years, Vermeer has reported that the rate of hemorrhagic stroke recurrence was 12% (30/243) and the annual rate of ICH recurrence was 2.1%19. In this study, with a follow-up duration of less than 5 years, the rate of hemorrhagic stroke recurrence was 7.01%, with incidence 1.64–1.95 patient-years in each age group, which is mildly lower than that reported in a previous study. The difference may be due to the stroke type. Studies have shown that patients with lobar hemorrhage have a higher risk of hemorrhage recurrence than those with deep hemorrhage9,11,12. Vermeer has reported a higher rate of hemorrhagic stroke recurrence than this study; the difference may be related to the higher proportion (55%) of patients with lobar hemorrhage in Vermeer’s study19.
The rate of ischemic stroke recurrence was 6.12% in patients who did not use antiplatelet drugs. The rate of ischemic stroke recurrence was close to that reported by Vermeer et al.19 but lower than that found in another study13. In a study with a 5-year follow-up period, Casolla et al. have found that the cumulative rate of ischemic stroke recurrence was 9.8%. The difference could be because the patients in this study was younger than those in Casolla et al.’s study (mean age, 62.2 years vs. 70 years, respectively), and this study included patients with subarachnoid hemorrhage. Moreover, patients with hemorrhagic stroke have a higher risk of ischemic stroke recurrence than those without stroke history. Murthy et al. have found that patients with a history of hemorrhagic stroke had a higher risk of ischemic stroke recurrence than those without hemorrhagic stroke history, with an HR of 3.114.
Some studies have found that patients with hemorrhagic stroke have a higher risk of brain hemorrhage than those with ischemic stroke11. However, some studies have found that ischemic stroke is more frequent than hemorrhagic stroke9,10,13. Our study found that hemorrhagic stroke was more frequent than ischemic stroke. The difference may be related to patient characteristics and location of ICH. Studies have found that patients with lobar hemorrhage have a higher risk of ICH recurrence, and deep hemorrhage increases the risk of ischemic stroke recurrence10,20. ICH is also a risk factor for ischemic stroke recurrence.
It is reasonable to consider that antiplatelet therapy may increase the risk of hemorrhage and decrease the risk of ischemic stroke. However, this study found that antiplatelet therapy did not decrease the risk of ischemic stroke but may decrease the risk of hemorrhagic stroke. The result agrees with those reported in a previous study. Murthy et al. have found that antiplatelet therapy did not affect mortality and clinical outcomes in patients with ICH21. The condition may be because most patients with hemorrhagic stroke have many stroke risk factors, which may affect the recurrence of ischemic and hemorrhagic stroke (Table 1).
The study found that hypertension may increase the risk of hemorrhagic and ischemic stroke recurrence. Age, atrial fibrillation, cardiovascular disease, and history of ischemic stroke are also risk factors of ischemic stroke recurrence. Intensive control blood pressure may decrease the risk of ischemic and hemorrhagic stroke recurrence.
This study has several limitations. First, this was a retrospective study; we did not have data regarding deep hemorrhage or lobar hemorrhage. Second, stroke recurrence was based on the diagnosis of ischemic or hemorrhagic stroke among hospitalized patients, which may have underestimated the rate of stroke recurrence. Third, information on stroke risk control, such as blood pressure, blood sugar, and blood lipid level, was unavailable, which may have affected the rate of stroke recurrence and stroke type. Fourth, this is a retrospective observational study, we cannot rule out the possibility that antiplatelet agent were prescribed to the patient whom less likely to have recurrence of hemorrhagic stroke.
In conclusion, the risk of stroke recurrence is high in patients with ICH. Antiplatelet therapy does not decrease risk of ischemic stroke recurrence but may decrease risk of hemorrhagic stroke recurrence. Hypertension is a risk factor of ischemic and hemorrhagic stroke recurrence.
Supplementary Information
Acknowledgements
This study was supported by a research grant from Ditmanson Medical Foundation Chiayi Christian Hospital (R110-007).
Author contributions
Y.-S.W. contributed to data interpretation and draft of the manuscript. C.-F.T. contributed to data collection, statistical analysis and data interpretation. C.-T.O. contributed to concepted idea and supervised the study. All authors discussed and reviewed the manuscript.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-22090-7.
References
- 1.Jolink WM, Klijn CJ, Brouwers PJ, Kappelle LJ, Vaartjes I. Time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology. 2015;85(15):1318–1324. doi: 10.1212/WNL.0000000000002015. [DOI] [PubMed] [Google Scholar]
- 2.Hsieh FI, Chiou HYH-Y. Stroke: Morbidity, risk factors, and care in Taiwan. J. Stroke. 2014;16(2):59–64. doi: 10.5853/jos.2014.16.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovelock CE, Molyneux AJ, Rothwell PM, Oxford Vascular Study Change in incidence and etiology of intracerebral hemorrhage in Oxfordshire, UK, between 1981 and 2006: A population-based study. Lancet Neurol. 2007;6(6):487–493. doi: 10.1016/S1474-4422(07)70107-2. [DOI] [PubMed] [Google Scholar]
- 4.Pennlert JMD, Eriksson MP, Carlberg BPMD, Wiklund PG. Long-term risk and predictors of recurrent stroke beyond the acute phase. Stroke. 2014;45(6):1839–1841. doi: 10.1161/STROKEAHA.114.005060. [DOI] [PubMed] [Google Scholar]
- 5.Howard GD, Cushman MMM, Howard VJ, et al. Risk factors for intracerebral hemorrhage: The Reasons for geographic and racial differences in stroke (REGARDS) study [Article] Stroke. 2013;44(5):1282–1287. doi: 10.1161/STROKEAHA.111.000529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ariesen MJ, Claus SP, et al. Risk factors for intracerebral hemorrhage in the general population: A systematic review. Stroke. 2003;34(8):2060–2065. doi: 10.1161/01.STR.0000080678.09344.8D. [DOI] [PubMed] [Google Scholar]
- 7.Martini SR, Flaherty ML, Brown WM. Risk factors for intracerebral hemorrhage differ according to hemorrhage location. Neurology. 2012;79(23):2275–2282. doi: 10.1212/WNL.0b013e318276896f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinho J, Costa AS, Araújo JM, Amorim JM, Ferreira C. Intracerebral hemorrhage outcome: A comprehensive update. J Neurol. Sci. 2019;398:54–66. doi: 10.1016/j.jns.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Weimar C, Benemann J, Terborg C, et al. Recurrent stroke after lobar and deep intracerebral hemorrhage: A hospital-based cohort study. Cerebrovasc. Dis. 2011;32(3):283–288. doi: 10.1159/000330643. [DOI] [PubMed] [Google Scholar]
- 10.Hill MD, Silver FL, Austin PC, Tu JV. Rate of stroke recurrence in patients with primary intracerebral hemorrhage. Stroke. 2000;31(1):123–127. doi: 10.1161/01.STR.31.1.123. [DOI] [PubMed] [Google Scholar]
- 11.Bailey RD, Hart RG, Benavente O, Pearce LA. Recurrent brain hemorrhage is more frequent than ischemic stroke after intracranial hemorrhage. Neurology. 2001;56(6):773–777. doi: 10.1212/WNL.56.6.773. [DOI] [PubMed] [Google Scholar]
- 12.Nakase T, Yoshioka S, Sasaki M, Suzuki A. Clinical features of recurrent stroke after intracerebral hemorrhage. Neurol. Int. 2012;4(2):e10. doi: 10.4081/ni.2012.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casolla B, Moulin S, Kyheng M, et al. Five-year risk of major ischemic and hemorrhagic events after intracerebral hemorrhage. Stroke. 2019;50(5):1100–1107. doi: 10.1161/STROKEAHA.118.024449. [DOI] [PubMed] [Google Scholar]
- 14.Murthy SB, Zhang C, Diaz I, et al. Association between intracerebral hemorrhage and subsequent arterial ischemic events in participants from 4 population-based cohort studies. JAMA Neurol. 2021;78(7):809–816. doi: 10.1001/jamaneurol.2021.0925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biffi A, Anderson CD, Battey TW, et al. Association between blood pressure control and risk of recurrent intracerebral hemorrhage. JAMA. 2015;314(9):904–912. doi: 10.1001/jama.2015.10082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flynn RWVM, MacDonald TMMD, Murray GDP, MacWalter RSMD, Doney AS. Prescribing antiplatelet medicine and subsequent events after intracerebral hemorrhage. Stroke. 2010;41(11):2606–2611. doi: 10.1161/STROKEAHA.110.589143. [DOI] [PubMed] [Google Scholar]
- 17.Sansing LH, Messe SR, Cucchiara BL, et al. Prior antiplatelet use does not affect hemorrhage growth or outcome after ICH. Neurology. 2009;72(16):1397–1402. doi: 10.1212/01.wnl.0000342709.31341.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064–2089. doi: 10.1161/STR.0b013e318296aeca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vermeer SE, Algra A, Franke CL, Koudstaal PJ, Rinkel GJ. Long-term prognosis after recovery from primary intracerebral hemorrhage. Neurology. 2002;59(2):205–209. doi: 10.1212/WNL.59.2.205. [DOI] [PubMed] [Google Scholar]
- 20.Greenberg SM, Eng JA, Ning M, Smith EE, Rosand J. Hemorrhage burden predicts recurrent intracerebral hemorrhage after lobar hemorrhage. Stroke. 2004;35(6):1415–1420. doi: 10.1161/01.STR.0000126807.69758.0e. [DOI] [PubMed] [Google Scholar]
- 21.Murthy SB, Biffi A, Falcone GJ, et al. Antiplatelet therapy after spontaneous intracerebral hemorrhage and functional outcomes. Stroke. 2019;50(11):3057–3063. doi: 10.1161/STROKEAHA.119.025972. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.