Abstract
Background:
Underutilization of HIV pre-exposure prophylaxis (PrEP) in the Southern United States (US) is well-documented. Urgent care (UC) centers are positioned as community-facing access points to PrEP, but the feasibility of integrating PrEP services into this setting is unclear. We conducted a survey of UC clinicians in the Southern US to better understand their perceptions of the feasibility of providing PrEP in their practice setting.
Objective:
The study aims to determine the feasibility and acceptability of providing PrEP services in the UC setting through a cross-sectional survey of UC clinicians.
Methods:
We conducted a 48-item cross-sectional survey of UC clinicians in the Southern US, between July and September 2020. The survey was distributed through the Urgent Care Association (UCA) and American Academy of Urgent Care Medicine (AAUCM) professional listservs as well as directly to publicly listed e-mail addresses.
Results:
Eighty-two clinicians responded to the survey. Most clinicians had familiarity with PrEP (97%). All respondents rated PrEP as an effective way to prevent HIV. However, less than half felt UC facilities were an appropriate place to prescribe PrEP. Few respondents (8%) expressed doubts that expansion of PrEP access would decrease the incidence of HIV in their community.
Conclusion:
These findings show UC clinicians are familiar with PrEP, and many believe it would benefit their patients; however, provider opinions on the appropriateness of providing PrEP in the UC setting differ. Further studies on PrEP implementation in UC centers are needed.
Keywords: HIV pre-exposure prophylaxis, PrEP, urgent care, survey, southern United States, sexually transmitted infections
1. INTRODUCTION
HIV pre-exposure prophylaxis (PrEP) has emerged as an essential modality for HIV prevention [1-4]. Although PrEP has been available since 2012, new HIV infections nationwide have not declined as rapidly as anticipated over that period. The Centers for Disease Control and Prevention (CDC) recently estimated that although 1.2 million people are eligible for PrEP in the United States (US), only one in six eligible candidates are currently receiving it [5]. These findings are particularly concerning for the Southern US, which accounted for over half of new HIV infections in 2016, and where new infections have only declined by 2% over the last five years [6].
The CDC reports that in 2018, persons aged 13-24 accounted for 21% of new HIV infections [7]. Recent consumer research suggests that how healthcare is sought out among persons in this age group is fundamentally different from older adults: A survey of 5092 adults conducted by PNC Healthcare reported that 59% of persons aged 21-32 identified retail or Urgent Care (UC) clinics as their preferred destination for healthcare services, compared to 31% of persons aged 50-71 and 26% of seniors (age 72+) [8]. We believe that by making PrEP available at healthcare points of access frequented by this high HIV risk demographic, we will significantly enhance PrEP access to the people who need it most.
Urgent care practices, whether stand-alone or part of multispecialty facilities, are community-facing access points for healthcare that appear to be well-positioned to provide PrEP services to their regions. The ubiquity of UC clinics in both urban and rural locales makes them an important avenue for enhancing the availability of PrEP in otherwise hard-to-reach areas, particularly in municipalities without health department-run sexually transmitted infection (STI) clinics and large academic centers [9-11]. However, the feasibility of incorporating PrEP into the on-demand UC practice setting and the UC clinicians’ willingness to integrate PrEP into acute care practice are unknown. To address our gap in understanding the feasibility and acceptability of providing PrEP services in the UC setting, we conducted a survey of UC clinicians across the Southern US.
2. MATERIALS AND METHODS
We administered a 48-item online survey to urgent care clinicians in the Southern US between July and September 2020. The questionnaire was developed in conjunction with the Duke Initiative on Survey Methodology (DISM), and focused on the following domains: providing HIV/STI care, perception of PrEP, feasibility and acceptability of PrEP in the UC setting, and willingness to prescribe PrEP. Survey responses were offered using 4- to 6-point Likert scales as well as yes/no response options. Respondents were not required to answer every question asked on the survey.
After the survey items were finalized, DISM staff tested the questionnaire for content flow and comprehension with cognitive interviews, and timed survey administration to selected volunteers. This information was used to finalize the survey and, once it was finalized, UC clinicians who practiced in the Southern US (AL, AR, FL, GA, KY, LA, MO, MS, NC, SC, TN, VA, WV) were invited to participate either by direct e-mail messages or by messages sent from the Urgent Care Association (UCA) and American Academy of Urgent Care Medicine (AAUCM) professional listservs. These listservs included physicians, nurse practitioners, physician assistants, and registered nurses. Direct e-mail addresses were compiled by the research team from publicly listed contact information on departmental and clinical websites. Survey invitations were only sent to clinicians accessible through the listservs or with publicly listed e-mail addresses. Each clinician was sent an initial invitation to the survey followed by two reminder e-mails. The survey was delivered on a Qualtrics-based platform which is designed to flag any potentially duplicate respondents (Qualtrics, Provo, UT). During the survey, respondents could enter into a raffle for one of ten $75 gift cards.
3. RESULTS
3.1. Survey Response Rate
We sent invitations to participate in the survey to 771 e-mail addresses. A total of 82 respondents took the survey for an overall response rate of 11%. The Qualtrics software is designed to flag any potentially duplicate respondents; no such individuals were identified. The majority of the respondents were from the direct e-mail invitation, yielding 48 complete surveys and 8 partial responses where the end of the survey was not reached. The remaining 26 respondents (22 complete and 4 partial responses) were from the listserv invitations.
3.2. Respondent Characteristics
Survey respondents self-identified as 66% Caucasian, 46% female, and 37% male (Table 1). The majority of the respondents (51%) were physicians, 23% were physician assistants, and 11% were nurse practitioners. Respondents specialties of practice were as follows: Family Medicine (62%), Internal Medicine (2%), Pediatrics (5%), Combined Internal Medicine/Pediatrics (1%), and Emergency Medicine (9%). Thirty-one respondents reported also working in areas other than UC: 21 worked in outpatient clinics, 3 in inpatient hospital settings, and 7 in Emergency Departments. The mean year in clinical practice for the survey respondents was 14.7 years (range 1-40). Respondents practiced in urban (24%), suburban (34%), small city/town (23%), and rural (4%) locations. Survey respondents estimated that their patient population was, on average, 44% low income, 42% from urban locations, 25% uninsured, and 47% had some college education.
Table 1.
Survey respondent demographics.
| Characteristic | N (%) (N=82) |
|---|---|
| Gender | - |
| Male | 30 (37) |
| Female | 38 (46) |
| Prefer Not to Answer | 14 (17) |
| Race | - |
| White | 54 (66) |
| Black or African American | 3 (4) |
| Asian | 7 (9) |
| Prefer Not to Answer | 18 (22) |
| Ethnicity | - |
| Hispanic/Latino | 2 (2) |
| Not Hispanic/Latino | 60 (73) |
| Prefer Not to Answer | 20 (24) |
| Professional Title | - |
| Physician | 42 (51) |
| Physician Assistant | 19 (23) |
| Nurse Practitioner | 9 (11) |
| Registered Nurse | 0 (0) |
| Prefer Not to Answer | 12 (15) |
| Medical Specialty | - |
| Family Medicine | 51 (62) |
| Internal Medicine | 2 (2) |
| Pediatrics | 4 (5) |
| Internal Medicine/Pediatrics | 1 (1) |
| Emergency Medicine | 7 (9) |
| Prefer Not to Answer | 17 |
| Other Areas of Practice (N = 31) | - |
| Outpatient Clinic | 21 (68) |
| Inpatient Hospital | 3 (10) |
| Emergency Department | 7 (23) |
| Practice Location | - |
| Urban | 20 (24) |
| Suburban | 28 (34) |
| Small City/Town | 19 (23) |
| Rural | 3 (4) |
| Prefer Not to Answer | 12 (15) |
3.3. Perceptions on HIV, Sexual Health, and Sexually Transmitted Infection Care
Fifty-two percent of the survey respondents viewed HIV as uncommon in their community and 44% reported that new infections are “very uncommon” in their practice (Table 2). However, 92% of the respondents had provided care for persons living with HIV. Eighty-nine percent of the clinicians surveyed indicated that STIs were a common diagnosis made at UC clinics. Similarly, almost all respondents (99%) had provided STI care in their practice, and 71% were “very comfortable” treating this diagnosis. All but one respondent noted that they cared for patients who identify as lesbian, gay, bisexual, transgender, queer, intersex, and/or asexual (LGBTQIA), but only half were “very comfortable” providing care to this patient population. Over half of the respondents (59%) were “very comfortable” obtaining a sexual health history from their patients, but only 4 (5%) reported always obtaining a sexual history from their patients. Open-ended survey questions revealed that one of the reasons respondents did not obtain a sexual health history was because “sexual health should be better obtained with a primary care doctor” (Supplemental Table S1 (225.4KB, pdf) ).
Table 2.
Urgent Care Providers’ Survey Responses: Perceptions on HIV, Sexual Health, and Sexually Transmitted Infection Care. Respondents were not required to answer each question.
| HIV, Sexual Health, and STI Care | |||||||
|---|---|---|---|---|---|---|---|
| - | Very Common | Moderately Common | Slightly Common | Slightly Uncommon | Moderately Uncommon | Very Uncommon | Total Respondents |
| How common/uncommon is HIV in the community where you practice? | 4 (5%) | 14 (17%) | 21 (25%) | 17 (21%) | 17 (21%) | 9 (11%) | 82 |
| How common/uncommon are new infections of HIV in your practice? | 2 (2%) | 1 (1%) | 12 (15%) | 11 (13%) | 20 (24%) | 36 (44%) | 82 |
| How common/uncommon are new STI diagnoses in your practice? | 39 (48%) | 23 (28%) | 10 (12%) | 5 (6%) | 1 (1%) | 3 (4%) | 81 |
| How comfortable/uncomfortable are you with treating sexually transmitted infections (STI)? | 55 (71%) | 17 (22%) | 4 (5%) | 0 (0%) | 1 (1%) | 1 (1%) | 78 |
| How comfortable/uncomfortable are you with obtaining a sexual health history from patients? | 46 (59%) | 24 (31%) | 6 (8%) | 1 (1%) | 1 (1%) | 0 (0%) | 78 |
| How comfortable/uncomfortable are you with providing care to persons who identify as lesbian, gay, bisexual, transgender, queer, intersex, and asexual (LGBTQIA)? | 38 (50%) | 29 (38%) | 7 (9%) | 1 (1%) | 1 (1%) | 0 (0%) | 76 |
| Very Adequate | Moderately Adequate | Slightly Adequate | Slightly Inadequate | Moderately Inadequate | Very Inadequate | - | |
| How adequate was your training in professional schools to address the needs of persons who identify as LGBTQIA? | 5 (7%) | 8 (11%) | 21 (28%) | 6 (8%) | 16 (21%) | 19 (25%) | 75 |
| - | Always | Most of the Time | About Half the Time | Sometimes | Never | - | - |
| How often do you obtain sexual health history? | 4 (5%) | 28 (36%) | 16 (21%) | 29 (38%) | 0 (0%) | - | 77 |
| - | Yes | No | - | - | - | - | - |
| Do you provide STI care? | 77 (99%) | 1 (1%) | - | - | - | - | 78 |
| Do you provide care for patients living with HIV? | 72 (92%) | 6 (8%) | - | - | - | - | 78 |
| Do you provide care for patients who identify as LGBTQIA? | 74 (99%) | 1 (1%) | - | - | - | - | 75 |
| Have you attended post-professional school training to care for LGBTQIA patients? | 37 (49%) | 38 (51%) | - | - | - | - | 75 |
| Perceptions of HIV Pre-Exposure Prophylaxis | |||||||
| - | Extremely Familiar | Very Familiar | Moderately Familiar | Slightly Familiar | Not at All Familiar | - | Total Respondents |
| How Familiar are you with PrEP? | 15 (20%) | 12 (16%) | 23 (31%) | 23 (31%) | 2 (3%) | - | 75 |
| - | Very Effective | Moderately Effective | Slightly Effective | Slightly Ineffective | Moderately Ineffective | Very Ineffective | - |
| How effective/ineffective is PrEP at preventing HIV? | 36 (49%) | 28 (38%) | 9 (12%) | 0 (0%) | 0 (0%) | 0 (0%) | 73 |
| - | Extremely Effective | Very Effective | Somewhat Effective | Not that Effective | Not Effective at all | - | - |
| How effective/ineffective would expanding PrEP access be in decreasing HIV incidence in your practice community? | 16 (21%) | 26 (35%) | 27 (36%) | 4 (5%) | 2 (3%) | - | 75 |
| How beneficial would providing PrEP be to your patient population? | 8 (11%) | 23 (31%) | 31 (42%) | 11 (15%) | 1 (1%) | - | 74 |
| - | Very Aware | Moderately Aware | Slightly Aware | Slightly Unaware | Moderately Unaware | Very Unaware | |
| How aware are persons at risk for HIV in your community of PrEP? | 2 (3%) | 12 (16%) | 18 (25%) | 16 (22%) | 16 (22%) | 9 (12%) | 73 |
| - | Yes | No | - | - | - | - | - |
| Do you think the concern that PrEP will lead to more high-risk sexual encounters is legitimate? | 41 (59%) | 29 (41%) | - | - | - | - | 70 |
| Feasibility and Acceptability of PrEP in Urgent Care | |||||||
| - | Strongly Support | Somewhat Support | Somewhat Oppose | Strongly Oppose | - | - | Total Respondents |
| Do you think your community would support or oppose offering PrEP at your facility? | 30 (41%) | 34 (46%) | 6 (8%) | 4 (5%) | - | - | 74 |
| - | Yes | No | Unsure | - | - | - | - |
| Would most of your clientele be able to afford PrEP or not? | 12 (17%) | 28 (39%) | 31 (44%) | - | - | - | 71 |
| Can urgent care improve PrEP access in your practice community? | 55 (76%) | 17 (24%) | NA | - | - | - | 72 |
| Do you think providing PrEP follow-up (HIV testing every 3 months) would be challenging in an urgent care setting or not? | 60 (83%) | 12 (17%) | NA | - | - | - | 72 |
| - | Appropriate | Inappropriate | - | - | - | - | - |
| Are urgent care facilities in general an appropriate or inappropriate place to prescribe PrEP? | 35 (48%) | 38 (52%) | - | - | - | - | 73 |
| Willingness to Prescribe PrEP | |||||||
| - | Very Ready | Somewhat Ready | Not that Ready | Not Ready at All | - | - | Total Respondents |
| How ready is the community where you practice for PrEP Services? | 14 (20%) | 36 (51%) | 18 (25%) | 3 (4%) | - | - | 71 |
| How ready, is your Urgent Care Practice for PrEP Services? | 8 (11%) | 27 (38%) | 20 (28%) | 17 (24%) | - | - | 72 |
| How ready are you as a provider to offer PrEP Services? | 16 (22%) | 35 (49%) | 6 (8%) | 15 (21%) | - | - | 72 |
| - | Yes | No | - | - | - | - | - |
| Would you be open to obtaining specialist support through infectious diseases to help administer PrEP care? | 63 (89%) | 8 (11%) | - | - | - | - | 71 |
| Do you have moral objections to prescribing PrEP | 3 (4%) | 67(96%) | - | - | - | - | 70 |
Note: * Indicated percentages may not sum to 100% due to rounding.
3.4. Perceptions of PrEP
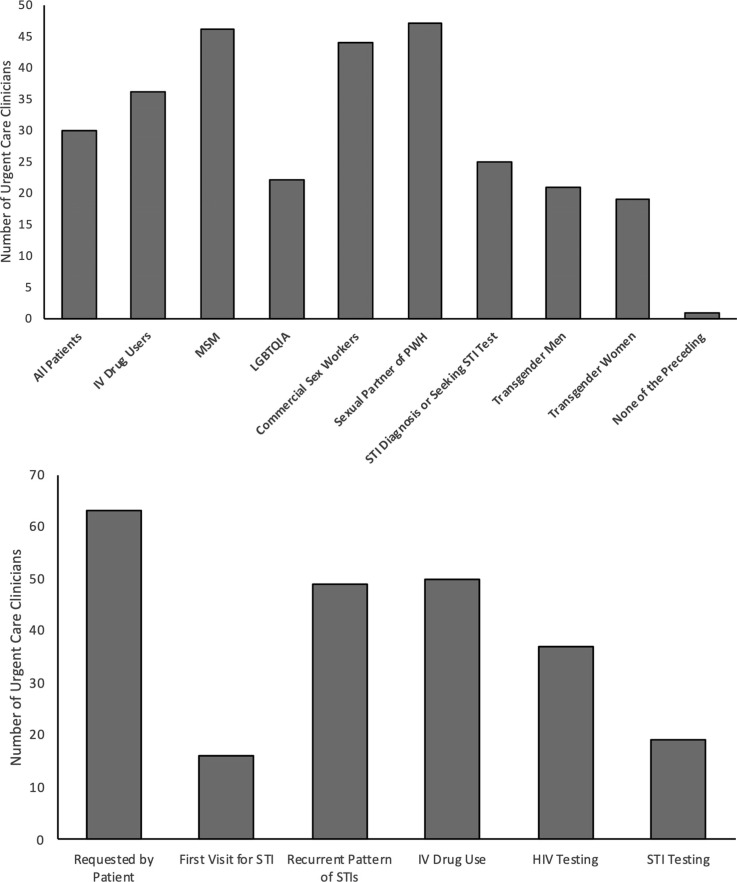
Ninety-seven percent of surveyed clinicians reported having some level of familiarity with PrEP, and all clinicians felt that it is an effective way to prevent new HIV infections. However, 62% of clinicians reported only a “moderate” or “slight familiarity” with the medication. A few respondents (8%) expressed doubts that expansion of PrEP access would decrease the incidence of HIV in their community, and a slightly higher amount (16%) did not see PrEP as beneficial for their patient population. There was a wide range of opinions on who should be offered PrEP and in what situations PrEP should be prescribed (Figs. 1A and B). Only 16 of the respondents reported that they would consider prescribing PrEP for a patient during their first visit for an STI. More than half (59%) of the respondents agreed with concerns that PrEP would lead some individuals to have more high-risk sexual encounters and that persons at risk for HIV in the community where they practice had some unawareness of PrEP (56%).
Fig. (1).
Urgent Care Clinician Perceived PrEP Eligibility. Respondents could select multiple answers (N=73). A) Perceived Eligibility by Patient Groups. B) Perceived Eligibility by Clinical Situation. IV Intravenous, MSM Men who have sex with men, LGBTQIA lesbian, gay, bisexual, transgender, queer, intersex and asexual, PWH persons with HIV, STI sexually transmitted infection.
3.5. Feasibility and Acceptability of PrEP in an Urgent Care Location
Even though the majority of UC clinicians acknowledged the effectiveness of PrEP and its potential benefits for their practice, only 48% felt UC facilities were an appropriate place to prescribe PrEP, and 83% felt that providing PrEP follow-up would be challenging. Respondents expressed concerns with providing PrEP in a UC setting: challenges with continuity of care, obtaining lab work including HIV testing every 3 months, lack of time to address PrEP care, and feeling that this is more appropriate for a primary care provider. Conversely, reasons supporting UC facilities as appropriate places for PrEP provision include being the first or potentially only point of healthcare for some patients, being a site for high rates of STI diagnosis, and serving as a contact point for patients at risk for HIV.
Most respondents (76%) thought UC clinics could improve access to PrEP in their community. Still more (86%) thought that the community they practice in would be supportive of having UC facilities provide PrEP. Similarly, 73% of the clinicians surveyed reported the community they practice in to be at least somewhat ready for PrEP services. However, 31 (44%) clinicians were unsure if their patient population could afford PrEP while only 12 (17%) stated that most of their patients could afford the service.
3.6. Willingness to Prescribe PrEP
While 49% of clinicians indicated their practice was at least somewhat ready to provide PrEP, a noticeably larger proportion, 71%, felt the same about their own ability to offer PrEP services. Even more clinicians (88%) stated they would be willing to have infectious disease (ID) specialist support to assist in managing PrEP care. One respondent suggested: “Urgent Care providers could work with ID/HIV and set up [a] system to obtain initial labs, then refer to ID/HIV clinic. Maybe you could do this via virtual visits via the ID/HIV department.” Nearly all respondents (96%) had no moral objections to providing PrEP care. One provider commented, “PrEP saves lives. Not offering PrEP would violate my medical ethics”.
Eighty-three percent of the survey respondents believed that PrEP follow-up visits and repeat HIV testing would be challenging in an UC setting; one clinician commented in the survey: “Most [UC] providers do not want to take the necessary time to learn about PrEP or the time required when prescribing it.” In other survey comments, clinicians requested assistance with linkage of patients to primary care financial services and noted time constraints in clinic flow. For instance, one clinician commented, “I do not think an urgent care setting is the best setting due to the time component. As a ‘recovery point’ or ‘refill point’ it would be fine.”
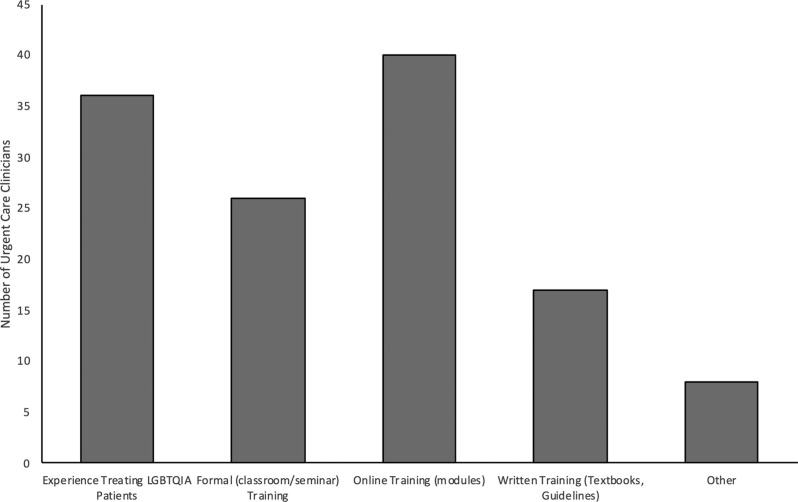
In working with at-risk patient populations, over half (55%) of surveyed clinicians reported that their training during professional school in addressing the needs of individuals who identify as LGBTQIA was “slightly inadequate” or worse. Almost half (49%) of clinicians reported having already attended supplemental training to care for these populations. Additional online training was most frequently reported as a need to be more comfortable addressing the needs of patients who identify as LGBTQIA (Fig. 2).
Fig. (2).
Reported Needs of Urgent Care Clinicians to Increase Comfort Caring for LGBTQIA Individuals. Respondents could select multiple answers (N=74). LGBTQIA lesbian, gay, bisexual, transgender, queer, intersex and asexual.
4. DISCUSSION
To our knowledge, this study is the first to examine the perceptions of Southern US urgent care clinicians toward PrEP. UC clinicians report familiarity with PrEP, and many believe that it would be beneficial for their patients. They also believe that PrEP is an effective means to prevent HIV transmission and that providing PrEP services at a UC facility would increase the accessibility of this treatment. Yet, opinions on the appropriateness and feasibility of providing PrEP in the UC setting differ. The majority of the clinicians surveyed felt ready to provide PrEP services, but less than half felt that their practice was ready for PrEP. Barriers to the provision of PrEP services included time constraints, affordability of medication, and difficulty with patient continuity of patient care. This survey was conducted prior to current changes in insurance coverage for PrEP, yet the perception of financial barriers may persist. These concerns are similar to those reported in a prior practice brief where a model of utilizing UC as an entry or refill access point to PrEP was suggested [12]. Our findings suggest that many southern UC clinicians are personally ready to incorporate PrEP into their clinical practice - an encouraging finding for dissemination of PrEP in the region - but acknowledge many challenges their practice would need to overcome. Our survey results also suggest that a range of factors, including familiarity with PrEP indications, PrEP management experience, caring for patients who identify as LGBTQIA, and systemic barriers to health system access, may be the primary barriers to unlocking UC centers as a critical point of access for PrEP in the Southern US.
There has been support for UC outlets providing PrEP due to the increased rates of STIs, which in turn increase the risk of HIV acquisition, being evaluated and treated in this clinical setting [13]. This viewpoint was corroborated in our survey results, with nearly all responding clinicians in this study reporting they are comfortable with managing STI care. In addition, UC clinics serve a population similar to Emergency Departments, which prior studies have described as a prime location for PrEP implementation [14-16]. Yet, in a prior study, UC clinicians had many concerns, including managing side effects of PrEP, adherence to medication, and increased PrEP-associated high-risk sexual behavior [17]. Supporting UC clinicians with these issues is of utmost importance in determining the feasibility of UC-managed PrEP in this region.
The need for further education and training regarding PrEP and HIV prevention is a common theme throughout the survey. Few clinicians reported consistently taking a sexual history from their patients. They also reported that new HIV diagnoses were uncommon despite working in the South, a geographic region accounting for the majority of new HIV infections. Misperceptions regarding who should be offered PrEP were also common among respondents. For instance, few UC clinicians indicated they would offer PrEP during a first time encounter for an STI, one of the indications to start the medication regimen per CDC treatment guidelines [18]. Yet, many (99%) UC clinicians stated that they frequently encountered STIs in their practice, suggesting that UC facilities are prime target areas for PrEP implementation. Furthermore, UC facilities are a low barrier location for sexual health services, especially for young persons who may benefit from PrEP. If the availability of easily accessible PrEP increases through UC facilities, it may in turn drive awareness and demand for this preventative medication. While PrEP has been shown to be associated with increased STI transmission, UC clinicians should be well equipped to manage these issues [19, 20]. These results suggest that a customized curriculum for prescribing and managing PrEP could be developed for UC clinicians to address these concerns and increase their awareness of PrEP eligibility among persons seeking STI care at their clinic. We believe that such a curriculum may improve UC clinicians’ confidence in providing PrEP services.
Many clinicians also admitted the need for additional training to address the needs of their LGBTQIA patients. Prior educational campaigns targeting Southern primary care physicians to improve PrEP prescription have been successful [21]. Similarly, the creation of a protocol for prescribing PrEP has increased comfort and reduced barriers to UC prescribed PrEP in Louisiana [22]. It is encouraging that while some clinicians currently are not comfortable treating LGBTQIA patients and providing PrEP, they are willing to learn more about these topics. We are hopeful that tailored educational campaigns can improve knowledge and comfort with PrEP among UC clinicians. In turn, this would lead to increased feasibility and willingness to prescribe and manage PrEP in the UC setting.
Our respondents represent a diverse group of urgent care clinicians. While we did not have access to the demographics of all persons who were invited to participate, we suspect the demographics of Southern UC clinicians would be comparable to those reported nationally among health care workers by the United States Department of Health and Human Services Bureau of Health Workforce [23]. The respondents to our survey were similar to national demographics by gender, but not by race and ethnicity. Indeed, Black and Hispanic clinicians were underrepresented in our results. Black and Hispanic persons are disproportionately affected by the HIV epidemic and comprise the majority of new HIV infections nationally [24]. It is important to engage Black and Hispanic clinicians to aid in providing PrEP services to these communities.
Our study has limitations. The overall response rate was less than expected, but followed trends of low response rates for online surveys. The response rate may be underestimated due to the overlap in survey invitations sent to clinicians with e-mails from both professional listservs. If so, this would result in a denominator smaller than we have estimated, but would not affect the numerator as the Qualtrics survey tool did not detect any duplicate survey responses. Also, we were unable to survey every Southern UC practice due to lack of freely accessible e-mail addresses which reduced the overall sample size. Nonetheless, low response rates to surveys have been described by the American Association for Public Opinion Research (AAPOR) across all modes of survey administration, and low response surveys can still provide good quality data [25]. In addition, low response rates from medical clinicians have been frequently reported in the literature overall [26, 27] and in response to surveys on PrEP specifically [28-31].
While an academic affiliation was not identified, our survey may also be subject to sampling bias as academic UC practices were more likely to publicly list their clinicians’ contact information. We also suspect that practices with connections to Infectious Disease specialists may be more aware of PrEP and more willing to respond to this survey. Similarly, clinicians who desire to learn more about PrEP or view PrEP favorably may have been more likely to respond to the survey request. There is also the chance of desirability bias insofar as respondents wanted to appear more willing to prescribe and knowledgeable about HIV PrEP. In turn, this may lead to leveling and confirmation bias in which respondents may omit negative viewpoints regarding PrEP. Regardless, we believe the clinicians responding to the survey have an interest in PrEP and may be more willing to become the first to take on the provision of PrEP in their practice. By addressing these clinicians’ needs, we can then increase the uptake of PrEP provision in UC facilities with the hope of influencing the practice behavior of other clinicians in their practice.
CONCLUSION
Overall, we found that UC clinicians in the South are familiar with PrEP and that many believe it would be beneficial for their patients, but the viewpoints on feasibility in the UC setting differ. Further studies to better ascertain the feasibility, acceptability, and barriers to providing PrEP in urgent care, as well as tailored educational programs, are needed. Using these data, a model of PrEP provision in UC can be developed and integrated in healthcare systems across the South and potentially other geographic regions. By increasing access points to PrEP, we are hopeful that PrEP use will increase and HIV transmission will decline in the Southern United States–an area of the critical need to end the HIV epidemic.
ACKNOWLEDGEMENTS
CMB and NLO contributed to the study concept and design. CMB, KE, CM, AC, MSM and NLO participated in the survey design. KE and LF collected survey data. CB, KE, CM, BS, MSM and NLO analyzed survey data. CB and NLO drafted the manuscript. All authors revised the manuscript and approved the final version for publication. The authors would like to thank Kara McGee and Isabelle Sico for their assistance with survey development.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The overall study was approved by the Duke University Institutional Review Board (IRB) in the United States (Pro00103302).
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. All human procedures were followed in accordance with the Helsinki Declaration.
CONSENT FOR PUBLICATION
Survey participants provided implied consent by responding to the survey and could opt-out at any time.
STANDARDS OF REPORTING
STROBE guidelines were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of their study are available from the corresponding author [CMB] upon reasonable request.
FUNDING
This research was supported by the Duke University Center for AIDS Research (CFAR), an NIH-funded program (5P30 AI064518). CMB was supported by the Ruth L. Kirschstein National Research Service Award of the National Institutes of Health under award number T32AI007392.
CONFLICT OF INTEREST
MSM received a grant from the Gilead Foundation paid to her institution.
DISCLAIMER
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publisher’s website along with the published article.
REFERENCES
- 1.Baeten J.M., Donnell D., Ndase P., et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mayer K.H., Krakower D.S. Editorial commentary: Scaling up antiretroviral preexposure prophylaxis: Moving from trials to implementation. Clin. Infect. Dis. 2015;61(10):1598–1600. doi: 10.1093/cid/civ665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant R.M., Lama J.R., Anderson P.L., et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant R.M., Anderson P.L., McMahan V., et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: A cohort study. Lancet Infect. Dis. 2014;14(9):820–829. doi: 10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith D.K., Van Handel M., Wolitski R.J., et al. Vital signs: Estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition--United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 2015;64(46):1291–1295. doi: 10.15585/mmwr.mm6446a4. [DOI] [PubMed] [Google Scholar]
- 6. CDC. Diagnosis of HIV infection in the united states and dependent areas, 2017. HIV Surveillance Report, 2018; 29 Available from: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2017-vol-29.pdf Accessed on May 12 2019.
- 7. CDC. HIV and youth. 2021. Available from: https://www.cdc. gov/hiv/group/age/youth/index.html Accessed on February 19 2021.
- 8. NC-Healthcare. Five ways tech-savvy millenials alter health care landscape 2015. Available from: https://www.prnewswire. com/news-releases/five-ways-tech-savvy-millennials-alter-health-care-landscape-300054028.html Accessed on March 9, 2019.
- 9.Burns D.N., Grossman C., Turpin J., Elharrar V., Veronese F. Role of oral pre-exposure prophylaxis (PrEP) in current and future HIV pre-vention strategies. Curr. HIV/AIDS Rep. 2014;11(4):393–403. doi: 10.1007/s11904-014-0234-8. [DOI] [PubMed] [Google Scholar]
- 10.Mayer K.H., Chan P.A.R., Patel R., Flash C.A., Krakower D.S. Evolving models and ongoing challenges for HIV preexposure prophylaxis im-plementation in the United States. J. Acquir. Immune Defic. Syndr. 2018;77(2):119–127. doi: 10.1097/QAI.0000000000001579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang H.L., Rhea S.K., Hurt C.B., et al. HIV preexposure prophylaxis implementation at local health departments: A statewide assessment of activities and barriers. J. Acquir. Immune Defic. Syndr. 2018;77(1):72–77. doi: 10.1097/QAI.0000000000001546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ng Y.C., Caires A., Mayeux J. Message from an urgent care PrEP provider for health care professionals. J. Assoc. Nurses AIDS Care: JANAC. 2018;29(1):130–132. doi: 10.1016/j.jana.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 13. Ayers AA. Is PrEP appropriate for urgent care? 2018. Available from: https://wwwjucmcom/is-prep-appropriate-for-urgent-care/ Accessed March 3 2021.
- 14.Haukoos J.S., White D.A.E., Rowan S.E., et al. HIV risk and pre-exposure prophylaxis eligibility among emergency department patients. AIDS Patient Care STDS. 2021;35(6):211–219. doi: 10.1089/apc.2021.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ridgway J.P., Friedman E.E., Bender A., et al. Evaluation of an electronic algorithm for identifying cisgender female pre-exposure prophylax-is candidates. AIDS Patient Care STDS. 2021;35(1):5–8. doi: 10.1089/apc.2020.0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ridgway J.P., Almirol E.A., Bender A., et al. Which patients in the emergency department should receive preexposure prophylaxis? imple-mentation of a predictive analytics approach. AIDS Patient Care STDS. 2018;32(5):202–207. doi: 10.1089/apc.2018.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ayers A.A. New lawsuits re-examine prescribing of PrEP in urgent care. JUCM; 2020. [Google Scholar]
- 18. CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States - 2021 update: A clinical practice guideline. 2021. Available from: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf .
- 19.Traeger M.W., Cornelisse V.J., Asselin J., et al. Association of HIV preexposure prophylaxis with incidence of sexually transmitted infec-tions among individuals at high risk of HIV infection. JAMA. 2019;321(14):1380–1390. doi: 10.1001/jama.2019.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ong J.J., Baggaley R.C., Wi T.E., et al. Global epidemiologic characteristics of sexually transmitted infections among individuals using preex-posure prophylaxis for the prevention of HIV infection: A systematic review and meta-analysis. JAMA Netw. Open. 2019;2(12):e1917134. doi: 10.1001/jamanetworkopen.2019.17134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clement M.E., Seidelman J., Wu J., et al. An educational initiative in response to identified PrEP prescribing needs among PCPs in the South-ern U.S. AIDS Care. 2018;30(5):650–655. doi: 10.1080/09540121.2017.1384534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mayeux J.J., Ng Y.C., Bice M.M. Outcomes from an urgent care pre-exposure prophylaxis protocol for the prevention of HIV. J. Assoc. Nurses AIDS Care: JANAC. 2020;31(6):678–684. doi: 10.1097/JNC.0000000000000178. [DOI] [PubMed] [Google Scholar]
- 23. U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. Sex, Race, and Ethnic Diversity of US, Health Occupations (2011-2015). Rockville, Maryland 2017. [Google Scholar]
- 24. CDC. Statistics overview - new HIV diagnoses among adults and adolescents in the US and dependent areas by race/ethnicity. 2021. Available from: https://www.cdc.gov/hiv/statistics/overview/index.html Accessed on June 24, 2021.
- 25. AAPOR. Response rates - an overview. 2021. Available from: https://www.aapor.org/Education-Resources/For-Researchers/Poll-Survey-FAQ/Response-Rates-An-Overview.aspx Accessed on February 19 2021.
- 26.Wiebe E.R., Kaczorowski J., MacKay J. Why are response rates in clinician surveys declining? Can. Fam. Physician. 2012;58(4):e225–e228. [PMC free article] [PubMed] [Google Scholar]
- 27.Cunningham C.T., Quan H., Hemmelgarn B., et al. Exploring physician specialist response rates to web-based surveys. BMC Med. Res. Methodol. 2015;15:32. doi: 10.1186/s12874-015-0016-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adams L.M., Balderson B.H. HIV providers’ likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: A short report. AIDS Care. 2016;28(9):1154–1158. doi: 10.1080/09540121.2016.1153595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krakower D.S., Oldenburg C.E., Mitty J.A., et al. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: Results from a survey of healthcare providers in new England. PLoS One. 2015;10(7):e0132398. doi: 10.1371/journal.pone.0132398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tellalian D., Maznavi K., Bredeek U.F., Hardy W.D. Pre-exposure prophylaxis (PrEP) for HIV infection: Results of a survey of HIV healthcare providers evaluating their knowledge, attitudes, and prescribing practices. AIDS Patient Care STDS. 2013;27(10):553–559. doi: 10.1089/apc.2013.0173. [DOI] [PubMed] [Google Scholar]
- 31.Silverman T.B., Schrimshaw E.W., Franks J., et al. Response Rates of medical providers to internet surveys regarding their adoption of preexposure prophylaxis for HIV: Methodological implications. J. Int. Assoc. Provid. AIDS Care. 2018;17:2325958218798373. doi: 10.1177/2325958218798373. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material is available on the publisher’s website along with the published article.
Data Availability Statement
The data that support the findings of their study are available from the corresponding author [CMB] upon reasonable request.