Abstract
Background
Cross-field ventilation is used as a conventional choice during carinal resection and anastomosis, but may interfere with surgical procedures. High-frequency jet ventilation (HFJV) allows for control of oxygenation in the open airways; nevertheless, there is a paucity of data to support its benefits versus cross-field ventilation. Herein, we aimed to investigate the efficacy of HFJV on intraoperative oxygen saturation compared with cross-field ventilation in patients undergoing carinal surgeries.
Methods
We conducted a retrospective analysis of 82 adults who underwent carinal resection and reconstruction (CRR) for benign or malignant diseases and received cross-field ventilation or HFJV at Shanghai Chest Hospital between January 2018 and September 2021. Patients were excluded when they had emergency surgeries or critical airway stenosis requiring extracorporeal life support, or limited resection without the need for cross-field ventilation or HFJV. Patients were classified into two groups based on the airway approach: cross-field ventilation group and HFJV group. The primary outcome was the area under the curve (AUC) of intraoperative hypoxemia defined as peripheral oxygen saturation (SpO2) below 90% lasting at least 1 minute. The secondary outcomes included cumulative time of SpO2 below 90%, AUC and cumulative time of severe intraoperative hypoxemia (defined as SpO2 below 80% lasting at least 1 minute), and AUC and cumulative time of suboptimal SpO2 (defined as SpO2 below 95% lasting at least 1 minute).
Results
Thirty-two patients were included in the final analysis, with 22 patients in cross-field ventilation group and 10 patients in HFJV group. The two groups did not differ in the severity and duration of intraoperative hypoxemia (P=0.366). The median (IQR) AUC of SpO2 below 90% was 21.92 (4.28, 54.48) min in cross-field ventilation group and 28.93 (10.78, 199.89) min in HFJV group. The cumulative time of SpO2 <90% was 16.67 (4.46, 37.11) min in cross-field ventilation group and 19.32 (7.50, 121.24) min in HFJV group, without statistical difference between groups (P>0.05). Severe intraoperative hypoxemia did not occur in either group.
Conclusions
This retrospective case series demonstrates that HFJV can be adopted to maintain oxygenation in CRR, without the interruption of surgical procedure.
Keywords: Carinal reconstruction, airway management, high-frequency jet ventilation (HFJV), hypoxemia, one-lung ventilation
Introduction
The inherent complexity and limited series of carinal surgeries pose great challenges for surgeons and anesthesiologists (1). Carinal surgeries are mainly performed via right posterolateral thoracotomy. Recently, the advance in minimally invasive surgery has made it possible to perform carinal resection and reconstruction (CRR) using video-assisted thoracoscopic surgery (VATS). For CRR, anesthesia management, especially airway management, is crucial to facilitate surgical procedures and decrease the risk of perioperative morbidity. To find a safer and more convenient approach to airway management during CRR is vital to improve patient-centered outcomes.
The conventional airway management during CRR uses cross-field ventilation to maintain oxygenation during one-lung ventilation (2), which is initiated by placing an endotracheal tube (ETT) across the surgical field into the contra-lateral main bronchus (3). This approach may interfere with ongoing surgical procedures and extend surgical time due to intermittent withdrawal and re-placement of the tube during anastomosis (4); other potential disadvantages include airway damage associated with repeated intubation and unintentional errors involved in exchanging the airway route (1). Still, cross-field ventilation remains the conventional choice in open carinal anastomosis; however, concerning thoracoscopic airway surgery, there is a lack of consensus on optimal airway management (1).
High-frequency jet ventilation (HFJV) is a modified method from high-frequency positive pressure ventilation. Its usage in thoracic surgery has expanded to many scenarios, including open airway surgeries, thoracoscopic airway surgeries, and interventional procedures for airway stenosis (5-7). HFJV is an alternative method of airway management that allows for control of oxygenation and has only minimal interference with the surgical field. The characteristics of low airway pressure and low tidal volume during HFJV are effective in airway management and hypoxemia prevention (8-10).
In tracheal-bronchial surgeries, HFJV interferes less with surgical procedures and provides continuous ventilation (11). This superiority of HFJV may be even more prominent in thoracoscopic airway surgery. Our preliminary experience has suggested that HFJV combined with the modified exchange tube can be successfully used in uni-portal CRR and also serve as a rescue airway management to cross-field ventilation. Since the number of reported CRR cases is limited, the optimal method of airway management remains uncertain, especially in minimally invasive carinal surgeries. There is little evidence of HFJV in CRR and the comparison between HFJV and cross-field ventilation has rarely been studied (11,12).
Herein, we aimed to investigate the efficacy of HFJV on intraoperative oxygen saturation (SpO2) compared with cross-field ventilation in patients undergoing CRR. We hypothesized that HFJV would not increase the severity of intraoperative hypoxemia compared to cross-field ventilation during CRR. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-355/rc).
Methods
Population
With approval from Institutional Review Board of Shanghai Chest Hospital (IRB#IS2146), we conducted this retrospective cohort analysis at Shanghai Chest Hospital. Individual consent for this retrospective analysis was waived. Patients met the criteria if they underwent CRR using HFJV or cross-filed ventilation for benign or malignant tumors from January 1, 2018, to September 30, 2021. Patients were excluded if they had emergency surgeries, critical airway stenosis that required extracorporeal circulation, or limited resection without the need for cross-field ventilation or HFJV. Data were retrospectively retrieved from the anesthesia information system and electronic health records using keywords (2018/1/1–2021/9/30, elective surgery, carinal surgery or CRR, HFJV and cross-field ventilation). Searching results were confirmed by two independent researchers, and a senior anesthesiologist was introduced when disagreement occurred.
Exposure
Patients were classified into two groups based on the ventilation approach during CRR: cross-field ventilation group and HFJV group.
CRRs were conventionally performed via either right thoracotomy or VATS, depending on the length of the main bronchus to be resected. Our selection criteria for minimally invasive approach were as follows: airway lesions less than 2 cm in length were located in the lower third of the trachea or partially involved carina, and tracheal resection length were less than 3 cm with predicted tension-free anastomosis. The mode of reconstruction depended on the extent of carinal resection. When a tumor involved a significant portion of the main bronchus, the opposite side bronchus was anastomosed end-to-end with the lower part of trachea, followed by the anastomosis of the shorter bronchus to the sidewall of the trachea. In our institution, end-to-end anastomosis of trachea to the left main bronchus was most commonly employed, with re-implantation of right main bronchus into the trachea (13). If the extent of resection exceeded 4 cm, anastomosis of trachea to a neo-carina was employed.
In cross-field ventilation group, an extended reinforced ETT was placed directly into left main bronchus by the surgical team after carinal resection. The ETT was connected to the ventilator via a sterile airway circuit traversing the surgical field. The ETT in place might interfere with the surgical visualization during the anastomosis; therefore, surgeons needed to withdraw the tube intermittently with the patient tolerating periods of apnea. If there was an evident drop in SpO2, the ETT was re-inserted and one-lung ventilation resumed. Once the sutures were in place, the airway was switched back to ventilating from above.
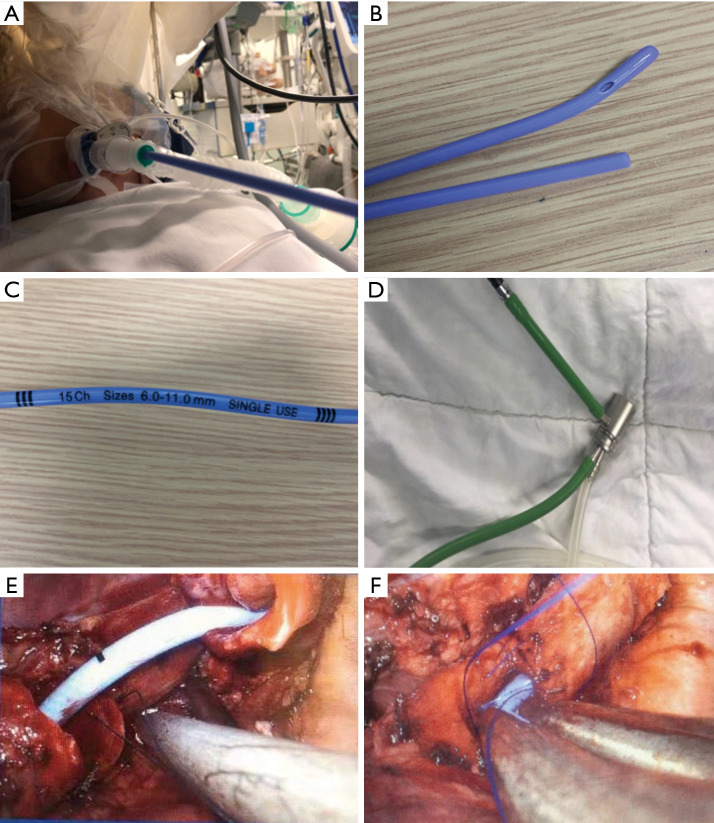
In HFJV group, we inserted a modified hollow exchange tube through either a laryngeal mask airway (LMA) or an ETT to provide HFJV (Figure 1). The modified hollow exchange tube had a side hole on the distal end, with a length of 90 cm and an outside diameter of 6 mm (Well Lead Medical Co., Ltd., Guangzhou, China), shown in Figure 1. The modified hollow exchange tube could be placed in the left main bronchus to achieve ventilation when connected to a high-frequency jet ventilator (HFJV, TwinStream, Carl Reiner, Austria). Ventilation was switched to HFJV when the airway was incised, and HFJV parameters were set to 1 LUMEN CAT MODE. The initial parameters of HFJV were set as follows: fraction of inspired oxygen (FiO2) jet 90%, frequency 100–120, I:E ratio 1:2 and pressure 0.9–1.2 bar. HFJV didn’t interrupt the bronchial suturing, and when SpO2 could not be kept above 80%, anesthesiologists on site might adjust the HFJV parameters or insert another ETT into the right bronchus. HFJV continued until the anastomosis was complete and then ventilation was switched back using LMA or ETT until the end of anesthesia.
Figure 1.
HFJV combined with an exchange tube. (A) The proximal end of the exchange tube was connected to LMA or ETT. (B) The distal end of the modified exchange tube was placed in the left main bronchus. (C) The length and outside diameter of the modified exchange tube. (D) The proximal end of the exchange tube was connected to HFJV adaptor. (E) During the anastomosis of the posterior tracheal wall, the exchange tube could be continuously in place without interfering with surgical exposure. (F) During the anastomosis of the anterior tracheal wall, HFJV could still continue in place. HFJV, high-frequency jet ventilation; LMA, laryngeal mask airway; ETT, endotracheal tube.
If cross-field ventilation failed to maintain optimal SpO2, HJFV could be used as a rescue option. In such a case, the patient was still classified in the cross-field ventilation group.
Outcomes
The primary outcome was the severity of intraoperative hypoxemia represented by the area under the curve (AUC). Intraoperative hypoxemia was defined as SpO2 <90% lasting at least one minute (14). The anesthesia information system recorded SpO2 every 10 seconds. AUC-SpO2 below each threshold was calculated as the cumulative sum of the areas below the given threshold using the trapezoid rule and measured in units of minutes. AUC-SpO2 summarized these areas across episodes. The original data were processed by Python, and we calculated the AUC of intraoperative SpO2 <90% based on a previous trial (15).
The secondary outcomes included: (I) the cumulative intraoperative hypoxemia time (defined as the cumulative time of SpO2 under 90%); (II) the AUC and cumulative time of severe intraoperative hypoxemia (defined as SpO2 <80% lasting at least one minute) (14); (III) the AUC and cumulative time of suboptimal SpO2 (defined as SpO2 <95%) (16).
Other outcomes included postoperative hospital stay and severe complications (continuous air leak, pneumonia and pulmonary infection, respiratory failure, re-intubation and death) during hospitalization.
Statistical analysis
The statistical analysis was performed using IBM SPSS 25.0 software. Measurement data of normal distribution were represented by mean ± standard deviation and were tested by t-test between groups. Measurement data of skewed distribution were represented by median (M) and interquartile range (IQR), and were tested by Mann-Whitney U test between groups. Category data were represented by number and/or percentile and were compared using Chi-squared test or Fisher’s exact test. A P value less than 0.05 was deemed statistically significant.
Results
Patient characteristics
Between January 1, 2018, and September 30, 2021, 82 patients who underwent carinal surgeries were screened from the hospital information system. Among them, 4 (4.8%) patients with severe airway obstruction required extracorporeal circulation and 46 (56%) patients only received sleeve lobectomy or partial carinal resection without the need for cross-field ventilation or HFJV, and 32 (39%) patients were included in the final analysis: 22 patients in the cross-field ventilation group and 10 patients in the HFJV group, shown in Table 1. One patient in the cross-field ventilation group had insufficient oxygenation and was salvaged by HFJV. There was a significant difference in the surgical approach between the two groups (P<0.05). Only 1 patient (4.5%) received VATS in the cross-field group, while 6 patients (60%) received VATS in the HFJV group. No significant difference was observed in the diagnosis of disease: 18 (81.8%) and 9 (90%) patients had the diagnosis of tracheal tumor in cross-field group and HFJV group, respectively (Table 1). And no significant differences were observed in age, sex, height, weight, American Society of Anesthesiologists (ASA) classification, operation time or anesthesia time between the two groups (P>0.05, Table 1).
Table 1. Baseline, demographic and surgical characteristics.
| Variables | Cross-field ventilation group (n=22) | HFJV group (n=10) | P value |
|---|---|---|---|
| Age, years | 44±15 | 51±15 | 0.180 |
| Sex (male), n (%) | 8 (36.4) | 6 (60.0) | 0.267 |
| Height (cm) | 162.14±8.55 | 167.30±10.07 | 0.140 |
| Weight (kg) | 65.0±13.16 | 66.9±12.24 | 0.702 |
| ASA physical status (II/III), n | 8/14 | 5/5 | 0.699 |
| Pathologic diagnosis, n (%) | 1.000 | ||
| Squamous cell carcinoma | 4 (18.2) | 1 (10.0) | |
| Adenoid cystic carcinoma | 18 (81.8) | 9 (90.0) | |
| Surgical type, n (%) | 0.001* | ||
| Open thoracotomy | 21 (95.5) | 4 (40.0) | |
| Thoracoscopic surgery | 1 (4.5) | 6 (60.0) | |
| Operation time (min) | 194 [161, 237] | 237 [183, 288] | 0.504 |
| Anesthesia time (min) | 252 [204, 292] | 289 [232, 329] | 0.449 |
Data were presented as mean ± SD, number (%) or median [Q1, Q3]. *, P<0.05. HFJV, high-frequency jet ventilation; ASA, American Society of Anesthesiologists.
Primary outcome and secondary outcomes
The median AUC of intraoperative hypoxemia defined as SpO2 below 90% was 21.92 (Q1, Q3: 4.28, 54.48) min in cross-field ventilation group and 28.93 (10.78, 199.89) min in HFJV group. Compared to cross-field ventilation, HJFV did not increase the severity of intraoperative hypoxemia (P=0.366, Table 2).
Table 2. Primary outcome and secondary outcomes.
| Variables | Cross-field ventilation group (n=22) | HFJV group (n=10) | P value |
|---|---|---|---|
| Primary outcome | |||
| AUC of SpO2 <90% | 21.92 (4.28, 54.48) | 28.93 (10.78, 199.89) | 0.366 |
| Secondary outcome | |||
| Cumulative time of SpO2 <90% | 16.67 (4.46, 37.11) | 19.32 (7.50, 121.24) | 0.325 |
| AUC of SpO2 <80% | 0 (0, 0) | 0 (0, 0) | 0.675 |
| Cumulative time of SpO2 <80%, min | 0 (0, 0) | 0 (0, 0) | 0.675 |
| AUC of SpO2 <85% | 0 (0, 0) | 0 (0, 4.135) | 0.305 |
| Cumulative time of SpO2 <85%, min | 0 (0, 0) | 0 (0, 2.43) | 0.305 |
| AUC of SpO2 <95% | 215.46 (89.84, 381.44) | 209.35 (66.11, 1,143.54) | 0.734 |
| Cumulative time of SpO2 <95%, min | 52.63 (25.96, 97.75) | 47.91 (21.69, 209.17) | 0.857 |
Data were presented as median (Q1, Q3). Mann-Whitney U test was used to compare the difference between the two groups. HFJV, high-frequency jet ventilation; AUC, area under curve; SpO2, oxygen saturation.
There was no significant difference in cumulative hypoxemia time (SpO2 <90%) between two groups: 16.67 (4.46, 37.11) min in cross-field ventilation group and 19.32 (7.50, 121.24) min in HFJV group, P=0.325 (Table 2).
Severe hypoxemia was not observed in either group (Table 2). In addition, AUC and cumulative time of suboptimal SpO2 (defined as SpO2 below 95%) were similar between the two groups [AUC: 215.46 (89.84, 381.44) min in cross-field ventilation group, and 209.35 (66.11, 1,143.54) min in HFJV group; cumulative time: 52.63 (25.96, 97.75) min in cross-field ventilation group and 47.91 (21.69, 209.17) min in HFJV group, P>0.05, Table 2].
Other outcomes
There was no significant difference in postoperative hospital stay: 9 (7, 11.5) days in cross-field ventilation group and 9 (7, 10.5) days in HFJV group (P>0.05). One death and one continuous air leak were observed in the cross-field ventilation group, while no severe complications occurred in the HFJV group.
Airway injury and pulmonary barotrauma were absent in both groups. The highest level of PaCO2 did not exceed 80 mmHg in HFJV group.
Discussion
Airway management in CRR is one of the greatest challenges in thoracic anesthesia. The ideal airway management for patients undergoing CRR includes ensuring adequate oxygenation and ventilation, preventing surgical debris into the distal airway, and providing adequate surgical conditions (1). Unfortunately, none of the existing airway approaches fulfills all these goals. Cross-field ventilation remains the most commonly used approach for CRR airway management. However, cross-field intubation tube in place might hinder surgical procedures during the anastomosis of the posterior tracheal wall, thus requiring intermittent withdrawal of the tube. HFJV during CRR provides advantages of improving surgical exposure during anastomosis without the need for intermittent withdrawal, minimizing the effect of respiratory movement on the surgical field, and decreasing peak airway pressure (1). As the rise of minimally invasive surgery has made it possible to perform CRR under VATS after careful selection, the benefits of HFJV may be more prominent because it can avoid the need for an additional port to insert the cross-field endobronchial tube. Hence, HFJV is more non-invasive and can further simplify the surgical procedures compared to cross-field intubation. Noticeably, another benefit of HFJV in VATS CRR is that HFJV could be successfully conducted through the LMA; therefore, it could be used under non-intubation anesthesia. With the recent advances in minimally invasive CRR, HFJV has the potential to be adopted as a routine airway management method, not just served as an alternative or a rescue airway technique.
Even though previous literature reported several case series of HFJV in tracheal or carinal surgeries, there is a paucity of data to compare HFJV with cross-field intubation (3,11,17). Our study was the first to compare HFJV with cross-field intubation in CRR. Our data showed no significant differences in both severity and duration of intraoperative hypoxemia between the two approaches. AUC of SpO2 below 90% and the cumulative time was similar between the two groups. We noticed that the median operation time of HFJV group was 240 minutes, about 40 minutes longer than that of cross-field ventilation group. This increase in surgical time between the two groups may be mainly attributed to anastomosis time since more patients underwent minimally invasive CRR in HFJV group. VATS may lengthen the anastomosis duration, which might increase hypoxemia AUC and cumulative time accordingly. However, there was only a 3-minute increase in median hypoxemia time in HFJV group, which might indicate the potential benefits of HFJV. We set a series of SpO2 thresholds to test the efficacy and safety of HFJV and our results demonstrated that HFJV did not increase the intraoperative hypoxemia at different thresholds and can be served as a routine method of airway management in CRR.
In minimally invasive CRR, surgeons conventionally introduce a cross-field endobronchial tube through either the operating port or an additional port to facilitate the exposure of surgical field (11). However, the cross-field endobronchial tube might not work well in uni-port CRR. Moreover, the endobronchial tube obstructs the view of the anastomosis site and therefore requires intermittent withdrawal during anastomosis (11). In our institution, we successfully implemented HFJV with the exchange tube in several cases. Data showed that HFJV with a modified exchange tube could be a better choice for CRR under VATS. Although the duration of anastomosis was approximately 45 minutes to 1 hour, we didn’t find any severe adverse events during HFJV and all patients after surgery were extubated in post-anesthesia care unit. In addition to the potential risk of hypoxemia, accumulation of CO2 resulting from insufficient ventilation was also a concern with HFJV. During HFJV and conventional cross-field ventilation, ETCO2 monitoring became inaccurate; therefore, we intermittently drew blood gas to check PaCO2. Although previous reports documented that brief permissive hypercapnia up to 100 mmHg was well-tolerated without any detrimental outcomes (18,19), avoiding higher PaCO2 was still our target. Unfortunately, since this was a retrospective study, we couldn’t accurately compare PaCO2 between the two groups because the blood samples were not drawn at fixed time.
Meanwhile, HFJV might be indicated when conventional cross-field ventilation fails. We observed that in our case series, one patient in cross-field ventilation group was unable to maintain oxygenation, then HFJV was successfully used for salvage.
Because open and thoracoscopic CRRs are performed infrequently at most centers, there is limited experience for anesthesiologists to select the optimal airway management. Herein, we conducted this retrospective analysis to explore the safety of HFJV compared with cross-field ventilation in CRR. Selection bias may exist due to the small sample size, and some confounders like smoking history or pre-operative forced expiratory volume in 1 second (FEV1) could not be adjusted. Moreover, since HJFV was performed by different anesthesiologists, parameters for optimal oxygenation during one-lung ventilation were not standardized. Therefore, large randomized prospective trials were needed for further confirmation.
In summary, this single-center retrospective series showed HFJV didn’t increase the severity and duration of perioperative hypoxemia during carinal resection and reinstruction at different thresholds of SpO2 (below 90%, 85% and 80%), compared to cross-field ventilation. HFJV combined with the exchange tube could be safely adopted to maintain oxygenation in CRR, without the interruption of surgical procedures. We have the reason to believe that under the trend of minimally invasive tracheal surgery, HFJV might be a better approach to airway management.
Supplementary
The article’s supplementary files as
Acknowledgments
The authors would like to thank Xiaofeng Zhang, in the Department of Anesthesiology at Shanghai Chest Hospital, for his assistance with record extraction.
Funding: This work was supported by Shanghai Municipal Commission of Health (No. 202040200), National Natural Science Foundation of China (No. 82071233) and Shanghai Shen Kang Hospital Development Center Project (No. SHDC2020CR4063).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by Institutional Review Board of Shanghai Chest Hospital (IRB#IS2146). Individual consent for this retrospective analysis was waived.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-355/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-355/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-355/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-355/coif). YQ reports funding from Shanghai Municipal Commission of Health (No. 202040200). JW reports funding from National Natural Science Foundation of China (No. 82071233) and Shanghai Shen Kang Hospital Development Center (No. SHDC2020CR4063). The other authors have no conflicts of interest to declare.
References
- 1.Smeltz AM, Bhatia M, Arora H, et al. Anesthesia for Resection and Reconstruction of the Trachea and Carina. J Cardiothorac Vasc Anesth 2020;34:1902-13. 10.1053/j.jvca.2019.10.004 [DOI] [PubMed] [Google Scholar]
- 2.Schieren M, Böhmer A, Dusse F, et al. New Approaches to Airway Management in Tracheal Resections-A Systematic Review and Meta-analysis. J Cardiothorac Vasc Anesth 2017;31:1351-8. 10.1053/j.jvca.2017.03.020 [DOI] [PubMed] [Google Scholar]
- 3.Macchiarini P, Altmayer M, Go T, et al. Technical innovations of carinal resection for nonsmall-cell lung cancer. Ann Thorac Surg 2006;82:1989-97; discussion 1997. 10.1016/j.athoracsur.2006.07.016 [DOI] [PubMed] [Google Scholar]
- 4.Schleicher A, Groeben H. Anesthetic considerations for tracheobronchial surgery. J Thorac Dis 2020;12:6138-42. 10.21037/jtd.2020.02.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishiyama T, Iwashita H, Shibuya K, et al. High-frequency jet ventilation during video-assisted thoracoscopic surgery in a patient with previous contralateral pneumonectomy. J Clin Anesth 2013;25:55-7. 10.1016/j.jclinane.2012.05.008 [DOI] [PubMed] [Google Scholar]
- 6.Ogawa E, Takenaka K, Kawashita F, et al. Prevention of overlooked bullae during video-assisted thoracic surgery (VATS) with a combination of high frequency jet ventilation (HFJV) and positive end-expiratory pressure (PEEP) for spontaneous pneumothorax. Thorac Cardiovasc Surg 2005;53:56-60. 10.1055/s-2004-830386 [DOI] [PubMed] [Google Scholar]
- 7.Fritzsche K, Osmers A. Anesthetic management in laryngotracheal surgery. High-frequency jet ventilation as strategy for ventilation during general anesthesia. Anaesthesist 2010;59:1051-61; quiz 1062-3. 10.1007/s00101-010-1815-6 [DOI] [PubMed] [Google Scholar]
- 8.Bunnell JB. High-frequency jet ventilation. Respir Care 2001;46:826-8. [PubMed] [Google Scholar]
- 9.Lemay F, Cooper J, Thompson S, et al. Combination of transnasal humidified rapid-insufflation ventilatory exchange with high frequency jet ventilation for shared airway surgery. Can J Anaesth 2020;67:1264-5. 10.1007/s12630-020-01635-2 [DOI] [PubMed] [Google Scholar]
- 10.Buise M, van Bommel J, van Genderen M, et al. Two-lung high-frequency jet ventilation as an alternative ventilation technique during transthoracic esophagectomy. J Cardiothorac Vasc Anesth 2009;23:509-12. 10.1053/j.jvca.2008.12.025 [DOI] [PubMed] [Google Scholar]
- 11.Li J, Wang W, Jiang L, et al. Video-Assisted Thoracic Surgery Resection and Reconstruction of Carina and Trachea for Malignant or Benign Disease in 12 Patients: Three Centers' Experience in China. Ann Thorac Surg 2016;102:295-303. 10.1016/j.athoracsur.2016.01.080 [DOI] [PubMed] [Google Scholar]
- 12.Ujiie H, Yasufuku K. New era of "resection of the carina and lower trachea". J Thorac Dis 2017;9:4932-6. 10.21037/jtd.2017.11.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blasberg JD, Wright CD. Surgical considerations in tracheal and carinal resection. Semin Cardiothorac Vasc Anesth 2012;16:190-5. 10.1177/1089253212450342 [DOI] [PubMed] [Google Scholar]
- 14.de Graaff JC, Bijker JB, Kappen TH, et al. Incidence of intraoperative hypoxemia in children in relation to age. Anesth Analg 2013;117:169-75. 10.1213/ANE.0b013e31829332b5 [DOI] [PubMed] [Google Scholar]
- 15.Maheshwari K, Khanna S, Bajracharya GR, et al. A Randomized Trial of Continuous Noninvasive Blood Pressure Monitoring During Noncardiac Surgery. Anesth Analg 2018;127:424-31. 10.1213/ANE.0000000000003482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Zanten HA, Tan RN, Thio M, et al. The risk for hyperoxaemia after apnoea, bradycardia and hypoxaemia in preterm infants. Arch Dis Child Fetal Neonatal Ed 2014;99:F269-73. 10.1136/archdischild-2013-305745 [DOI] [PubMed] [Google Scholar]
- 17.Zhu GQ, Wu XM, Cao DH. High frequency jet ventilation at the distal end of tracheostenosis during flexible bronchoscopic resection of large intratracheal tumor: Case series. Medicine (Baltimore) 2020;99:e19929. 10.1097/MD.0000000000019929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schieren M, Egyed E, Hartmann B, et al. Airway Management by Laryngeal Mask Airways for Cervical Tracheal Resection and Reconstruction: A Single-Center Retrospective Analysis. Anesth Analg 2018;126:1257-61. 10.1213/ANE.0000000000002753 [DOI] [PubMed] [Google Scholar]
- 19.Chin JH, Lee EH, Choi DK, et al. High frequency jet ventilation of one lung using a bronchial blocker of Univent during carinal resection. J Korean Med Sci 2010;25:1083-5. 10.3346/jkms.2010.25.7.1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as