Abstract
Although theoretical models highlight the role of coping motivations in promoting co-development of depression and alcohol use, few longitudinal studies have examined such processes across early adulthood. The current study examined the role of coping in the association between depression and alcohol use across late adolescence and early adulthood. A control sample of adolescents (N = 498) from a longitudinal prevention trial completed the Brief Symptom Inventory, Life Events Coping Inventory, and a self-report survey on alcohol use at ages 17, 22 and 23, as well as the Composite International Diagnostic Interview at age 28–30. Path analyses integrated self-report and diagnostic measures. Although gender differences were observed in mean levels of depression, alcohol use, and the use of substances to cope, we did not find gender differences in structural relations across these domains over time. Substance use coping served as an intervening pathway in the association between alcohol use and depression both at the symptom-level from age 17 to 23, and in predicting longer-term diagnostic outcomes at ages 28 to 30. Depressive symptoms in early adulthood were indirectly related to major depressive disorder (MDD) through two independent paths, including the stability of depressive symptoms over time, and through the influence of depression on increasing the tendency to use substances to cope with stress. Our results underscore that coping effects provide unique predictive power across developmental transitions, over and above the stability of depressive symptoms and alcohol use, underscoring coping motives as a promising intervention target that may prevent co-occurring depression and substance use.
Keywords: substance use coping, alcohol use, depression, longitudinal models, adolescence
Introduction
Both alcohol use and symptoms of depression show substantial escalations across adolescence (Willoughby & Fortner, 2015). For instance, alcohol abuse during early adolescence is associated with both short term negative consequences, including injuries and risky sexual behavior (Windle, 2016), and longer-term difficulties, including heightened risk for alcohol use disorders (AUDs), relationship instability, and broader mental health challenges in adulthood (Fergusson et al., 2013; Irons et al., 2015). Similarly, depression in adolescence may interfere with normal growth and development, educational achievement and interpersonal relationships (Lewinsohn et al., 2003; McLeod et al., 2016), and is associated with greater risk of suicide (Curtin et al., 2016). Suicidality merits particular attention, as the tragically high and escalating prevalence of suicide represents a serious public health concern, and is the second leading cause of death, globally, among those aged 15 to 29 (Turecki & Brent, 2016).
Alcohol use and depression are highly likely to co-occur in adolescence and early adulthood (e.g., Dawson et al., 2004). For instance, rates of alcohol abuse and depression in late adolescence and early adulthood have been shown to be as high as rates of depression alone (Archie et al., 2012). Further, such co-occurrence is associated with greater severity and chronicity of impairment, as well as heightened suicide risk (Archie et al., 2012; Brière et al., 2014; Turecki & Brent, 2016). Given the prevalence and significant consequences of such co-occurrence, improved understanding of the linkages between depression, suicidality and alcohol abuse across adolescence and early adulthood may have substantial public health consequences.
Directional Models
There are several models of the association between alcohol abuse and depression over time, differing in terms of the directions of influence (from alcohol abuse to later depression or vice-versa), as well as in the potential intervening mechanisms. First, one set of models highlights paths from early alcohol abuse to later depression. For instance, the cumulative failure model suggests that early substance use (and other forms of antisocial behavior) may lead to failures in peer-relational and academic domains, which may foster negative self-perception, and ultimately lead to escalating depression (Patterson & Stoolmiller, 1991). Further, alcohol may have neurotoxic effects during developmentally sensitive periods, including adolescence, which may cause executive functioning impairments that lead to self-regulatory difficulties and depression (Peeters et al., 2014). Similarly, in line with the Acquired Preparedness model, longitudinal research indicates that heavy drinking may facilitate learning that drinking may help individuals “forget their worries,” at least temporarily, thereby predicting escalations in drinking to cope over time (Settles et al., 2010). Such drinking to cope may, in turn, facilitate the development of depression as drinkers come to rely more heavily on alcohol as a maladaptive coping behavior. Indeed, a number of studies (e.g., Fergusson et al., 2009; Briere et al., 2014) support the directional link between early alcohol abuse and later depression, even after accounting for shared risk factors (Boden & Fergusson, 2010).
In contrast, the onset of depression may precede the development of problematic alcohol use (Schleider et al., 2019). For instance, the internalizing pathway model suggests that earlier difficulties with depression predict growth in problematic patterns of alcohol use through interpersonal (e.g., peer relational problems and peer deviance) and cognitive (e.g., alcohol use as a coping mechanism) pathways (Hussong et al., 2011; Kuntsche & Muller, 2012). The internalizing pathway is consistent with self-medication models, which suggest that drinking is often motivated by a desire to reduce distress and negative affect associated with depression and suicidal ideation, which in turn is reinforced in the short term through the pharmacological and situational consequences of alcohol use (Gonzalez & Hewell, 2012). Consistent with this model, there is a well-established association between drinking to regulate or avoid unpleasant emotions associated with negative affect and alcohol-related problems in adolescents and young adults (Gonzalez & Hewell, 2012). A number of studies have provided supportive evidence for the prediction of escalations in alcohol use from earlier depression. For instance, McCarty and colleagues (2012; 2013) found that depressive symptoms predicted subsequent escalations in alcohol use across grades 6 through 12. Similarly, in longitudinal work with girls followed from early through late adolescence, Schleider and colleagues (2019) found that depression consistently predicted subsequent escalations in alcohol use over yearly assessments, while alcohol use only predicted subsequent depression in later adolescence. In addition, Windle and Scheidt (2004) identified a “negative affect” pathway, characterized by higher levels of depression and anxiety during adolescence, associated with alcohol related problems in adulthood. Overall, results of longitudinal studies support pathways from depression to later alcohol use, as well as from alcohol use to later depression.
Coping and the Link Between Depression, Alcohol Use and Suicidality
Despite theoretical models underscoring the potential role of coping motives in predicting growth in depression from early alcohol use, and escalations in alcohol use from earlier depression, relatively few studies have explicitly examined coping as a mediator of these associations (Briere et al., 2014). Existing research has primarily supported the path from depression to alcohol use via the tendency to drink as a means of coping with stress or negative emotions (e.g., Kenney et al., 2018; Villarosa et al., 2018). More broadly, research also indicates that the use of alcohol while sad or depressed may serve as a risk factor for suicidal behavior among adolescents (Schilling et al., 2009). Of note, Gonzalez and Hewell (2012) found that suicidal ideation, more narrowly, predicted greater drinking to cope in heavy-drinking college students, controlling for depressive symptoms. Further, O’Brien and colleagues (2013) found that more frequent alcohol use among adolescents with suicidal ideation and low levels of depression was associated with increased odds of a suicide attempt (O’Brien et al., 2013). Taken together, these findings suggest that although suicidal ideation and depression are highly correlated, they differ in their relationship with drinking to cope, underscoring the importance of integrating suicidality into this research.
Much of the evidence supporting coping motives as mediators of the path from depression to alcohol-related problems has come from cross-sectional studies, that are limited in their ability to provide strong tests of mediation (e.g., Catanzaro & Laurent, 2004, Gonzalez et al., 2009; Blevins et al., 2016). Of note, in a 10-year longitudinal study of adults diagnosed with depression, individuals who had a stronger propensity to drink to cope at baseline showed a stronger connection between depressive symptoms and both alcohol consumption and drinking problems over time (Holahan et al., 2003). Similarly, in a three-week diary study with college-students, Grant and colleagues (2009) found that stronger coping motives at baseline were related to more positive associations between daily depressed mood and alcohol use. Given the translational significance of this pathway, further long-term longitudinal research is warranted.
To our knowledge, few, if any, longitudinal studies have examined the path from alcohol use to later depression or suicide-related behavior through escalating reliance on substance use to cope with stress. As discussed previously, however, there is solid theoretical justification for this pathway. For instance, the Acquired Preparedness model indicates that heavy drinking to deal with stress predicts escalations in drinking to cope over time, which in turn, facilitates the development of depression (Settles et al., 2010). The current study provides one of the few tests of this pathway from alcohol use to later depression via substance-use coping mechanisms. An important novel contribution of the current study is the use of longitudinal data across a critical developmental span, integrating both self-report and diagnostic measures.
Gender Differences
Gender differences in rates of depression have been widely documented, with girls significantly more likely to be diagnosed with depression (e.g., Kumpulainen, 2000; Marmorstein, 2009). Gender differences in patterns of alcohol use have also been documented. For instance, greater variability and stronger escalation in heavy alcohol use has been observed for males, but not females, over time (Hussong et al., 1998). However, gender differences in the relation between alcohol use and depression across development have been less studied, and results have been inconsistent. Several studies have observed the association between alcohol use and depression in girls, but not boys (e.g., Nolen-Hoeksema, 2004; Fleming et al., 2008; Miettunen et al., 2014; Edwards et al., 2014). For instance, Danzo and colleagues (2017) found that alcohol use and depression were independent across early adolescence for boys, while bidirectional associations were observed for girls across time. Others have either found earlier depression predicted subsequent alcohol use in boys, but not girls (e.g., Kumpulainen, 2000; Tapert et al., 2003), or have failed to find gender differences (e.g., McCarty et al., 2012). For instance, a 25-year longitudinal study by Fergusson and colleagues (2009) found no evidence for gender differences in the association between alcohol use and depression over time. Finally, Marmorstein (2009) found more complex patterns of gender differences, as baseline depression and alcohol use were more strongly interrelated for girls in early adolescence, while baseline depression was related to stronger growth in alcohol use through late adolescence for boys.
Research indicates possible gender differences in coping motives for alcohol use, although results have been somewhat inconsistent across studies. While the bulk of studies have shown that females are more likely than males to report drinking to cope (e.g., Timko, 2005; LaBrie et al., 2012), several have shown the reverse pattern (e.g., Cooper et al., 1992; Hussong, 2003), or have found no gender differences in drinking to cope (e.g., LaBrie et al., 2011). Moreover, there is evidence suggesting that drinking to cope may be more likely to mediate associations between depression and alcohol-use over time in females. For instance, Kenney and colleagues (2015) found that in college-aged women, depression predicted drinking to cope, which predicted alcohol use and negative alcohol consequences. However, given the variability of findings, and the very small number of studies testing whether intervening processes connecting depression and alcohol use may vary by gender, additional work examining the association between depression and alcohol use over time is needed (Marmorstein, 2009).
Current Study
Although research indicates that alcohol use and depression are related over time (Briere et al., 2014), relatively few studies have examined specific pathways linking the two, particularly using longitudinal data. In the current study we conducted secondary analyses to examine whether coping motives may serve to connect depression and alcohol use across adolescence and early adulthood. Given that the bulk of the literature has examined whether coping motives may mediate the association between depression and later alcohol use, we predicted that results would support this directional pathway. However, we also examined the possibility that earlier alcohol use may also predict subsequent depression, via coping motives, as alcohol use may erode effective coping strategies, over time. Of note, we also examined longer-term diagnostic outcomes at age 28 to 30, in relation to transactional processes between depressive symptoms, alcohol use, and coping in late adolescence and early adulthood. The inclusion of longer-term diagnostic outcomes represents a contribution of the current study, given the relative lack of longer-term longitudinal studies in this area, and the primary reliance on self-report data. Given that most studies examining alcohol use have done so using college student samples, one of the novel contributions of our study is that we examined long-term relationships spanning late adolescence and adulthood, a relatively understudied age range (Cooper et al., 2015). Additionally, we specifically examined suicide-related behaviors at age 28 to 30, given the public health importance of this outcome, and evidence that co-occurring depression and alcohol abuse may be strongly associated with suicide-risk over time. More broadly, we also examined possible gender differences in pathways between alcohol use and depression. Although results of prior studies in this area have been mixed, we predicted that the pattern of intermediary variables linking depression and alcohol use would differ based on gender, with stronger associations observed for girls relative to boys across early adulthood. Of note, we employed data collected as part of a prevention trial of the Family Check-Up (Dishion et al., 2012). Because the current analyses focused on developmental models, we only used data from the control condition (N = 498), which was “school as usual,” with families simply followed over time, but provided no treatment through the study.
Methods
Participants
Participants included 498 adolescents and their families, recruited in sixth grade from three middle schools within an ethnically diverse metropolitan community in the northwestern United States. Parents of all sixth-grade students in two cohorts were approached, and 90% consented to participate. The sample included 258 males (51.8%) and 240 females (48.2%), including 209 Caucasians (42%), 141 African Americans (28.3%), 37 Latinos (7.4%), 27 Asian Americans (5.4%), and 84 (16.9%) youths of other ethnicities (including biracial). Biological fathers were present in 307 families (61.6%). Approximately 80% of youths were retained to the end of high school, while diagnostic interviews at ages 28 to 30 were not available for 118 youths (23.7%). Although participants were recruited as part of a family-focused prevention trial, all participants included in the current analyses were randomly assigned to the control condition at baseline. The control condition was “school as usual,” in which participants were followed longitudinally, but were not provided any of the family-focused prevention services offered to families in the intervention condition. All procedures were approved by the university’s Institutional Review Board.
Measures
Alcohol Use
Participants completed a self-report survey about their alcohol use at ages 17, 22, and 23. Each year they were asked to report the frequency with which they had used alcohol (number of drinks) in the previous month. Similar individual item scores have been used in prior research on adolescent and young adult substance (Fosco et al., 2013; Stormshak et al., 2011), and have demonstrated validity for assessing alcohol use development over time (Fosco et al., 2013).
Depressive Symptoms
Participants completed the Brief Symptom Inventory (BSI; Derogatis & Spencer, 1982), a widely-used and well-validated self-report measure assessing a range of symptom dimensions, at ages 17, 22, and 23. The current analyses focused on the depression symptom scale, which includes 6 items assessing the frequency with which depressive symptoms (“Feeling no interest in things;” “Feeling lonely;” “Feeling blue;” “Feelings of worthlessness;” “Feeling hopeless about the future;” “Thoughts of ending your life”) were experienced during the prior week on a 5-point scale (1 = “Not at all” to 5 = “Very much”). High internal consistency was observed over time across participants in the control group (Chronbach’s alpha: Age 17 = .845, Age 22 = .859, Age 23 = .825).
Substance Use Coping
Reports of substance use as a means of coping with stress were assessed at ages 17, 22 and 23 with items from the Life Events Coping Inventory (LECI; Dise-Lewis, 1988), a 52-item measure that asks youth to rate the likelihood of engaging in a variety of behaviors when feeling stressed. Items were rated on a scale from 1 (“I would definitely not do this”) to 9 (“I would definitely do this”). The substance use coping scale was comprised of four items, including “drink alcohol,” “smoke cigarettes,” “get stoned,” and “take other drugs.” Acceptable internal consistency was observed over time across participants in the control group (Chronbach’s alpha: Age 17 = .711, Age 22 = .616, Age 23 = .608).
DSM-IV Major Depressive Disorder and Alcohol Use Disorder Diagnoses
The standardized Composite International Diagnostic Interview (CIDI; World Health Organization, 1994) was administered to participants at ages 28 to 30 by trained research staff who were unaware of the participant’s intervention status. The CIDI is a fully structured diagnostic interview that generates diagnoses based on Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994) criteria. Current analyses examined lifetime Major Depressive Disorder (MDD) and Alcohol Use Disorder (AUD) diagnoses, which were coded dichotomously as 1 = affected and 0 = not affected.
Suicide Risk
The MDD section of the CIDI includes four items reflecting thoughts of death, suicidal ideation, suicidal ideation with a plan, and suicide attempts. Only respondents endorsing screening items were administered the entire depression module including suicide items (n = 200). A Suicide Risk Index was created by counting the number of items endorsed, with potential scores ranging from 0 to 4 (see Connell et al., 2016).
Assessment Procedures
Surveys were sent to participants’ homes to complete and return by mail. Participants were paid $20 for completing each assessment. Diagnostic interviews were primarily face-to-face in the research offices, except for participants living more than 100 miles from the study center, which were administered over the telephone. Evidence suggests good reliability between telephone and face-to-face diagnostic interviews (Briere et al., 2014).
Data Analysis
Hypothesis-testing analyses were conducted in Mplus version 7.11, using Full Information Maximum Likelihood Estimation (FIML) to account for missing data (Muthen & Muthen, 2015). Little’s (1988) Missing Completely at Random (MCAR) test indicated that the missing data was consistent with MCAR assumptions (χ2[72] = 87.67, n.s.), supporting the use of FIML estimation. To examine model fit, and possible need to include lag-2 paths (e.g. predicting age 22 depression from age 21 and age 17 depression), we first conducted a series of separate autoregressive models for depression, alcohol use and substance use coping. Next, we conducted nested model comparisons to examine gender differences in two stages, using a model that included depression, alcohol use and substance use coping. We compared a model with all structural paths, means, variances, and covariances constrained to be equal across gender groups, with a model allowing means and variances to vary by gender. Given nested model results, indicating that gender differences were observed in mean levels of depression, alcohol use, and the use of substances to cope, we included gender as a covariate in subsequent models, along with ethnicity. Of note, since there were no gender differences observed in structural relations over time, we presented subsequent analyses in which males and females were combined, controlling for gender in all subsequent models. We also expanded the model to include diagnostic outcomes at ages 28 to 30, and examined indirect effects to test the significance of pathways to these outcomes. Standard errors for indirect effects were calculated using the delta method (MacKinnon et al., 2004; MacKinnon et al., 2002), and the standardized indirect effect is reported as an effect size index (abcs; see Preacher & Kelley, 2011). A typical model-trimming approach was used to estimate the fewest necessary paths in the final model (e.g., Kline, 2015), and non-significant paths from the preliminary analysis were not included in the final models.
Results
Descriptive Analyses
Descriptive statistics and correlations are presented in Table 1 for depressive symptoms, alcohol use and substance-use coping scales. Female gender was associated with significantly higher depressive symptoms at ages 17, 22 and 23, but significantly lower alcohol use at ages 22 and 23, as well as lower reported substance use to cope with adverse experiences at age 23. Ethnic minority status was associated with lower self-reported alcohol use at ages 17, 22 and 23, and with lower tendency to engage in substance use in response to stress at age 17. Ethnic minority status was not significantly correlated with depressive symptoms at any age, however. Cross-sectional and longitudinal correlations between alcohol use and depression were modest. However, substance use coping was consistently correlated with both alcohol use and depressive symptoms, both concurrently and over time.
Table 1.
Correlations and descriptive statistics
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Female gender | -- | ||||||||||
| 2. | Ethnic minority status | .06 | -- | |||||||||
| 3. | Age 17 Alcohol use | .00 | −.20* | -- | ||||||||
| 4. | Age 17 Coping: Substance use | .04 | −.13* | .48* | -- | |||||||
| 5. | Age 17 depressive symptoms | .24* | −.06 | .19* | .20* | -- | ||||||
| 6. | Age 22 Alcohol use | −.26* | −.27* | .28* | .13* | −.04 | -- | |||||
| 7. | Age 22 Coping: Substance use | −.07 | −.03 | .31* | .40* | .03 | .41* | -- | ||||
| 8. | Age 22 depressive symptoms | .14* | .05 | .14* | .06 | .26* | −.01 | .28* | -- | |||
| 9. | Age 23 Alcohol use | −.15* | −.22* | .15* | .06 | −.05 | .60* | .23* | −.03 | -- | ||
| 10. | Age 23 Coping: Substance use | −.07 | −.02 | .16* | .43* | −.01* | .29* | .23* | .18* | .38* | -- | |
| 11. | Age 23 depressive symptoms | .16* | −.06 | .08* | .10 | .30* | −.08 | .09* | .41* | −.04 | .15* | -- |
|
| ||||||||||||
| Descriptive statistics: | 48.2% | 58% | 1.02 (2.18) |
1.95 (1.46) |
58.34 (4.76) |
7.06 (4.99) |
.64 (.74) |
59.03 (4.89) |
7.78 (5.10) |
.62 (.73) |
58.64 (4.59) |
|
Note:
p < .05;
For descriptive statistics, percentages are reported for categorical variables, and Means (SDs) for continuous variables.
At ages 28 to 30, 64 (16.8%) individuals were diagnosed with lifetime MDD, and 51 (13.1%) were diagnosed with lifetime AUD. MDD and AUD were not significantly related to ethnicity. MDD (but not AUD) diagnoses were related to gender. Females were significantly more likely than males to report lifetime depression (20% of females, 12.5% of males; χ2 [df = 1] = 7.67, p < .05). With respect to suicide-risk items, 52 (13.6%) individuals endorsed thoughts of death, 32 (8.4%) endorsed suicidal ideation, 9 (2.3%) endorsed ideation with a plan, and 7 (1.8%) reported suicide attempts.
Preliminary Models
For depression, the lag-1 model provided relatively poor fit, χ2 (df = 1) = 35.12, p < .05; CFI = .88, RMSEA = .21, SRMR = .06. Adding a lag-2 path, yielded a just-identified model. However, in predicting depressive symptoms at age 22, both the lag-1 (estimate = .39, SE = .03) and the lag-2 paths were statistically significant (estimate = .20, SE = .03).
For alcohol use, the lag-1 model provided excellent model fit, χ2 (df = 1) = .99, p = n.s.; CFI = 1.00, RMSEA = .00, SRMR = .01. Adding a lag-2 path, yielded a just-identified model, and the lag-2 path predicting age 22 alcohol use was not significant (estimate = .06, SE = .06).
For substance use coping, the lag-1 model provided adequate fit, χ2 (df = 1) = 28.66, p < .05; CFI = .95, RMSEA = .19, SRMR = .05. Adding a lag-2 path, yielded a just-identified model, in which the lag-1 (estimate = .61, SE = .03) and the lag-2 paths were both statistically significant (estimate = .16, SE = .03) in predicting age 22 substance use coping. Given these results, subsequent models included lag-2 paths for both substance use coping and depressive symptoms, but not for alcohol use.
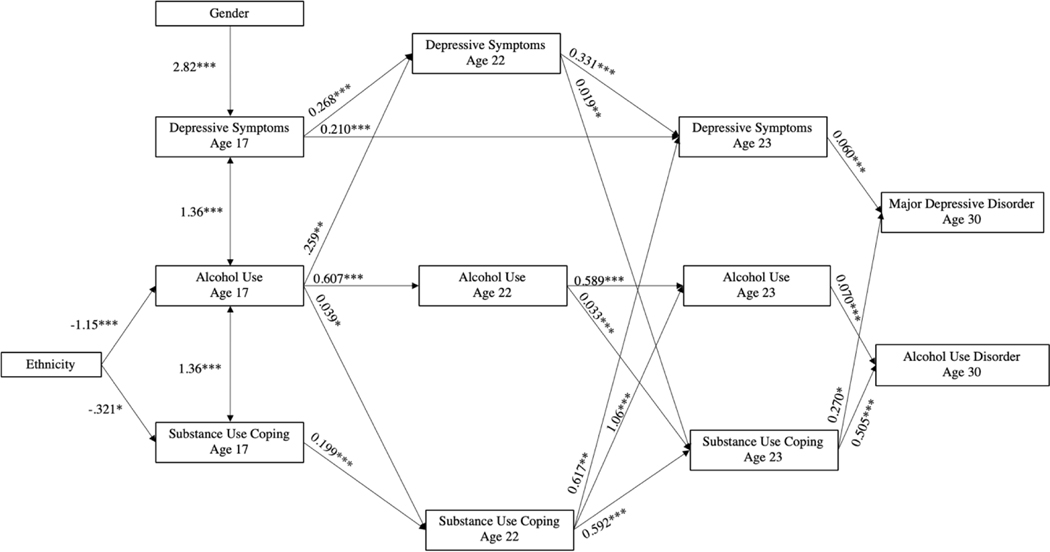
The nested model allowing means and variances to differ across gender groups provided significantly better fit to the data, Δχ2 [Δdf = 18] = 150.14, p < .05. However, further allowing the structural paths to vary by gender did not yield significantly improved model fit, Δχ2 [Δdf = 20] = 17.97, n.s. Therefore, results indicated that despite significant gender differences in mean levels of depression, alcohol use, and coping via substance-use, structural relations among these domains were similar for males and females. The final model provided adequate fit to the data, χ2 (df = 10) = 158.63; p < .05; CFI = .90; SRMR = .06; RMSEA = .14. The final model with lifetime depression and alcohol use disorder outcomes is shown in Figure 11.
Figure 1.
Final model with lifetime major depressive disorder and alcohol use disorder outcomes. Unstandardized coefficients are reported. Gender and ethnicity are included in the model as covariates, and significance levels are as follows: *p<.05; **p<.01; ***p<.001.
Associations Between Depression, Alcohol Use, and Substance Use Coping
Several aspects of the final model results are worth noting. First, depressive symptoms did not significantly predict either alcohol use or coping between ages 17 and 22. Depressive symptoms at age 22 did, however, predict greater substance use coping at age 23. Similarly, substance use coping at age 17 did not predict depression or alcohol use at age 22, but coping at age 22 did predict both greater depression and alcohol use at age 23. Alcohol use at age 17 was significantly related to both greater depressive symptoms and substance use coping at age 22, while alcohol use at age 22 was related to greater substance use coping at age 23, but not to depressive symptoms at age 23.
With respect to diagnostic outcomes at age 28 to 30, lifetime MDD was directly predicted by depression and substance-use coping, but was not directly related to alcohol use at age 23. Lifetime AUD was also directly predicted by alcohol use and substance use coping at age 23, but was not directly predicted by depressive symptoms at age 23.
Indirect Effects for Major Depressive Disorder at age 28 – 30
In describing significant indirect effects, we focused on cross-variable pathways for depression and alcohol use. However, it is worth noting that extended pathways from early depressive symptoms to later MDD diagnoses via intermediary depressive symptoms were significant, as were paths from early alcohol use to later AUD diagnoses via intermediary alcohol use. We also focus on the longest indirect pathways that were statistically significant, as all shorter indirect pathways contained within the longer paths were also significant.
There were two significant indirect paths from early alcohol use at age 17 to lifetime MDD by age 30. First, alcohol use at age 17 predicted greater depressive symptoms at age 22, in turn predicting continued depressive symptoms at age 23, which predicted greater likelihood of MDD diagnoses by age 30 (indirect effect = .005, SE = .002), with a small effect (abcs = .011). Similarly, alcohol use at age 17 predicted continued alcohol use at age 22, which predicted greater substance use coping at age 23, in turn predicting greater likelihood of MDD diagnoses by age 30 (indirect effect = .005, SE = .002). The overall Standardized Indirect Effect = 0.012, a small effect, while for the shorter two-step path (age 22 alcohol to age 23 coping to MDD), abcs = .04, a small to medium effect.
Several other indirect paths are worth noting. First, depression at age 22 was significantly indirectly related to MDD diagnoses both via depression at age 23 (indirect effect = .02, SE = .005; abcs = .10, a medium effect), as well as through greater substance use coping at age 23 (indirect effect = .005, SE = .002; abcs = .03, a small to medium effect). Similarly, substance use coping at age 17 was related to MDD at age 28 – 30 through the indirect pathway to substance-use coping at age 22 and subsequent elevations in depressive symptoms at age 23.
Indirect Effects for Alcohol Use Disorder at age 28 – 30
There was one significant indirect pathway from depressive symptoms at age 17 to lifetime AUD diagnoses by age 30. Depression at age 17 predicted greater depression at age 22, which predicted greater substance use coping at age 23, which, in turn, predicted greater likelihood of AUD diagnoses by age 30 (indirect effect = .003, SE = .001). The overall Standardized Indirect Effect = 0.012, a small effect, while for the shorter two-step path (age 22 depression to age 23 coping to AUD), abcs = .05, a small to medium effect.
Substance-use coping at age 17 was also significantly indirectly related to AUD in adulthood via its effect on continued substance-use coping at age 22, which predicted more frequent alcohol use at age 23 (indirect effect = .02, SE = .005). The overall Standardized Indirect Effect = 0.02, a small effect, while for the shorter two-step path (age 22 coping to age 23 alcohol use to AUD), abcs = .06, a small to medium effect.
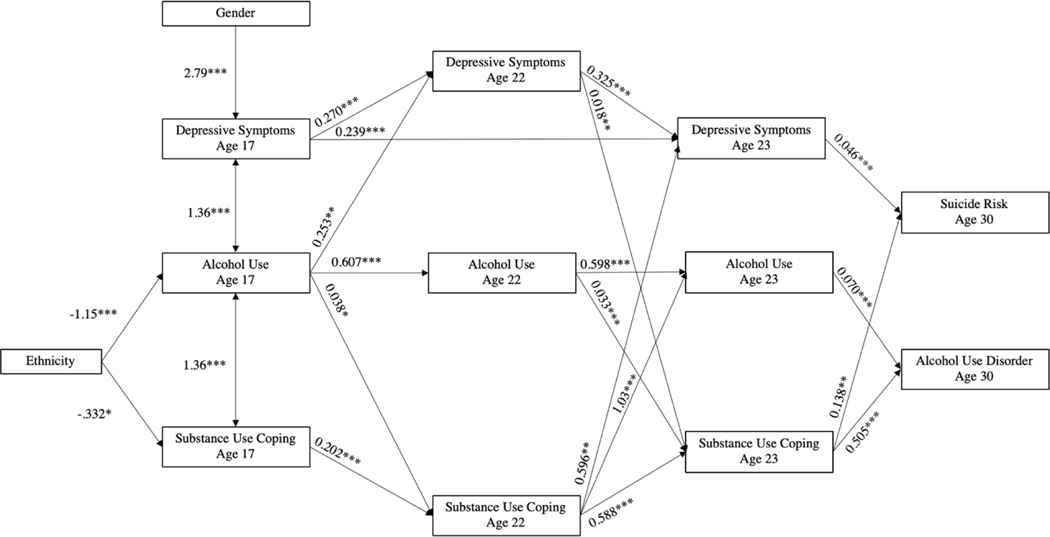
Suicide-risk Behaviors at Age 30
Finally, we ran a model in which MDD was replaced with a suicide-risk variable, derived from diagnostic data at age 30, reflecting the endorsement of thoughts of death, thoughts of suicide, suicidal ideation with a plan or attempted suicide. The final model, including effect sizes, shown in Figure 2, were very similar to the model with lifetime MDD, with suicide-risk directly predicted by depressive symptoms and substance-use coping at age 23. Suicide risk was directly predicted by depressive symptoms at age 23 (estimate = .05, SE = .006), and by substance use coping at age 23 (estimate = .14, SE = .05), but was not significantly related to alcohol use at age 23.
Figure 2.
Final model with suicide risk and lifetime alcohol use disorder outcomes. Unstandardized coefficients are reported. Gender and ethnicity are included in the model as covariates, and significance levels are as follows: *p<.05; **p<.01; ***p<.001.
However, alcohol use at age 17 was indirectly related to suicide risk via two extended pathways. First alcohol use at age 17 predicted greater depressive symptoms at age 22, which predicted continued symptoms at age 23 and, in turn, greater suicide risk in adulthood (indirect effect = .004, SE = .001; abcs = .011, a small effect). Second, alcohol use at age 17 predicted greater alcohol use at age 22, which predicted greater substance-use coping at age 23 and, in turn, greater suicide risk in adulthood (indirect effect = .003, SE = .001). The overall Standardized Indirect Effect = 0.01, a small effect, while for the shorter two-step path (age 22 alcohol to age 23 coping to suicide risk), abcs = .03, a small to medium effect.
Finally, substance use coping at age 17 was indirectly related to suicide risk, via coping at age 22 and depressive symptoms at age 23 (indirect effect = .006, SE = .002). The overall Standardized Indirect Effect = 0.01, a small effect, while for the shorter two-step path (age 22 coping to age 23 depression to suicide risk), abcs = .03, a small to medium effect.
Discussion
Although the association between depression and alcohol use has been well-documented (e.g., Hussong et al., 2011; Pedrelli et al., 2016), a number of important questions remain. Given the substantial differences in depression prevalence and substance use patterns across development, as well as the mixed results regarding gender differences in connections between depression and alcohol use over time (e.g. Boden & Fergusson, 2011), we first sought to examine possible gender differences in pathways between depression and alcohol use in late adolescence and early adulthood. Second, we sought to examine the role of coping processes in the association between depression and alcohol use across late adolescence and early adulthood, a critical period for both the onset of depression and substance use, as well as to examine long-term diagnostic outcomes in adulthood. Elucidation of pathways between depression and alcohol across late adolescence and early adulthood may inform prevention and intervention efforts across this important developmental span.
Gender Differences
In line with our hypotheses, we found differences in mean levels of depression, alcohol use and the use of substances to cope with stress. As expected, higher levels of depression were observed for females in comparison to males at all three assessment waves. Conversely, females reported lower levels of alcohol use than males at ages 22 and 23, as well as a lower likelihood of using drugs or alcohol in response to stress (but only at age 23). Such gender differences in mean levels of depression, alcohol use, and coping via substance use are generally in line with prior work in this area (e.g. Pedrelli et al., 2016).
Critically, however, despite these mean-level differences between males and females, we did not find gender differences in structural relations across these domains over time. Evidence supporting gender differences in pathways between depression and alcohol use over time has been mixed, and our results are consistent with other studies in late adolescence and early adulthood that have found no gender differences in associations (e.g., McCarty et al., 2012; Fergusson et al., 2009). It is worth acknowledging that there may be stronger gender differences in association between depression and alcohol use in earlier adolescence, as females are more likely than males to develop depression in early adolescence, and tend to transition from initial alcohol use to abuse more rapidly in that age-range (see Boden & Fergusson, 2011). Given that our study covers the span from late adolescence to early adulthood, it is possible that earlier gender differences in associations between depression and alcohol use may have attenuated, although we were not able to examine such a possibility in the current study. Nevertheless, our results are consistent with other research in this area in late adolescence and early adulthood, in indicating that the pathways between depression and alcohol use over time use are similar in direction and magnitude for both genders, despite gender differences in mean-levels.
Direct and Indirect Pathways Between Depressive Symptoms and Alcohol Use
The second goal of the current study was to examine coping mechanisms that may serve as a link between depression and alcohol use over time. Our results, integrating data covering a more-than 10-year time-span from adolescence through adulthood, indicate significant indirect pathways between alcohol use and depression, both in terms of the prediction of later symptoms in early adulthood, and the prediction of diagnoses in adulthood. Indeed, a notable strength of the current study was the inclusion of diagnostic data for depression and suicidality, as well as for AUDs in adulthood, underscoring that these transactions are related to serious and impairing diagnostic difficulties in adulthood. Symptom-based and diagnostic effects are discussed, in turn.
Age-related trends in associations between alcohol use and depression were observed, with alcohol use during late adolescence directly predicting greater depressive symptoms and substance use coping at age 22. However, alcohol use at age 22 did not predict depressive symptoms one year later. Alcohol use during adolescence may be a more central predictor of later depression risk since it is illegal at this age and is therefore associated with broader aspects of deviancy. Indeed, reinforcement and modeling of alcohol use are important mechanisms by which delinquent peers influence the initiation of drinking during adolescence (Trucco et al., 2011; Danzo et al., 2017), both of which are known risk factors for the development of depression (Pesola et al., 2015). However, once alcohol use becomes legal following age 21 (in the U.S.), direct effects on later depression may weaken, as the concomitants of alcohol use change with the transition to legal drinking age when it loses some of its cache as a form of deviant behavior (e.g. Monahan et al., 2009; Fromme et al., 2010).
Following the transition to adulthood, alcohol effects on later depression appear primarily indirect and mediated by coping motives, a pattern that is generally consistent with the Acquired Preparedness model (Settles et al., 2010). We found that alcohol use at age 17 indirectly predicted higher levels of depressive symptoms at age 23, by predicting increases in the likelihood of engaging in substance use in response to stress at age 22. It is worth highlighting that the indirect effect of coping was significant above the direct effect of alcohol use, underscoring this pathway as an important, independent predictor of depression. Substance use coping motives may become more centrally related to the risk for depression following the transition to early adulthood when individuals experience increased developmental stress (Stone et al., 2012).
Although adolescent alcohol use was both directly and indirectly predictive of later depressive symptoms in early adulthood, depressive symptoms in adolescence were not directly or indirectly related to alcohol use across this developmental transition. Further, depressive symptoms were only predictive of greater substance use coping from age 22 to 23 and, substance use coping connected depressive symptoms in early adulthood with later AUD diagnoses (discussed more fully in the subsequent section). Although depressive symptoms in adolescence were not directly or indirectly predictive of alcohol use or substance use coping, young adults with depression may rely on substances to regulate negative affect (Gonzalez & Hewell, 2012) and to cope with increased educational, occupational, and social stressors associated with the transition to adulthood (Stone et al., 2012). Thus, substance use-focused prevention and intervention efforts should aim to target maladaptive coping patterns during early adulthood to prevent the development of AUDs.
Pathways to Diagnostic Outcomes and Suicidality
At the diagnostic level, AUD was directly, and independently predicted, by earlier alcohol use and substance use coping. Although depressive symptoms were not directly related to AUD diagnoses, they indirectly predicted such diagnoses via substance use coping, as mentioned previously. This finding supports the independent effect of substance use coping over and above the direct effect of alcohol use frequency on development of AUDs, consistent with the internalizing pathway model that identifies depressive symptoms as a precursor of alcohol use and AUDs, suggesting that self-medication via substance use is a primary reason for addiction (Hussong et al., 2011).
MDD diagnoses were directly, and independently, predicted by depressive symptoms and substance use coping. Further, two independent, indirect pathways were observed from depressive symptoms in adolescence and early adulthood to MDD, including through the stability of depressive symptoms over time, and through the influence of depression on increasing the tendency to use substances to cope with stress. Relatedly, although alcohol use was not directly related to MDD diagnoses, alcohol use in early adulthood did indirectly predict MDD diagnoses and suicidality via substance use coping. It is worth highlighting that, although the path from alcohol to later depression via escalating use of substances to cope is consistent with theoretical perspectives, there are very few direct longitudinal tests of this pathway in the literature. Future work replicating and extending our findings is needed, for instance, by examining demographic or setting-effects that may moderate the strength of this pathway. Taken together, these findings, as well as those at the symptom level, highlight that substance use coping represents an important, unique predictor of escalating depression across critical developmental transitions, over and above the effects of either earlier alcohol use or of earlier depression. Thus, coping motives are a promising intervention target that may prevent co-occurring depression and substance use, ultimately reducing their deleterious impact on functioning throughout adulthood.
Summary and Implications for Prevention and Intervention
Overall, we found significant pathways between alcohol use and depression, in terms of the prediction of both later symptoms and diagnoses in adulthood. Our results are novel in that they underscore that alcohol use is indirectly associated with later depression via coping mechanisms across an extended developmental span into adulthood, across both self-report and diagnostic outcomes. Further, depressive symptoms and alcohol use represent important early risk factors for the development of MDD and AUD, via stability in symptoms and escalations in the tendency to use drugs or alcohol as a means to deal with stress.
Although long-term longitudinal studies in this area remain relatively scarce, the predictive pathways between depression and alcohol use observed in the current study are generally consistent with other longitudinal work (e.g., Briere et al., 2014). The current results add to the literature by indicating that substance use coping behaviors may be a central mediator of the association between alcohol use and depression, and serve as a critical link between depressive symptoms and alcohol use and later MDD and AUD diagnoses, underscoring coping motives as modifiable risk factor that can be used to orient a focus for prevention and intervention programs that may prevent co-occurring depression and substance use during the transition into adulthood. Adolescents who use substances to cope with stress may benefit from early intervention aimed at developing alternative coping strategies, including more positive ways to regulate emotions (Stapinski et al., 2016). Such clinical efforts to target substance use coping may help to lessen the severity of and long-term problems associated with both depression and alcohol use among at-risk adolescents.
Limitations and Future Directions
Several possible limitations may influence our interpretation of the results. First, assessments were conducted at yearly intervals, but it is possible that important changes occur across domains within smaller time frames. Second, although we examined a large age range (17–30 years), diagnostic was not collected until ages 28–30, thus, baseline diagnostic data is not available. The emergence of symptoms during earlier periods of development may be relevant, too, and should be incorporated in future studies. A third limitation is that the effect sizes of the 3-step indirect paths (from age 17 to age 28 diagnostic outcomes) were generally small in magnitude, while the effect sizes of the 2-step paths (from age 22 to age 28 diagnostic outcomes) were generally small to moderate in magnitude. These effect sizes were generally small to moderate in magnitude, which may be due in part to the 5–7 year gap in assessments from ages 23 to 28–30. Finally, our study included a sample of adolescents in the United States where the legal drinking age is 21 years, which may limit the generalizability of results across countries.
The current study focused on coping mechanisms connecting depression and alcohol use, but other mechanisms may be important as well (e.g., deviant peer processes), and should be examined in future work. Further, although the LECI provides a comprehensive assessment of life events and coping strategies of children and adolescents (Dise-Lewis, 1988), it captured a general measure of substance use coping that was not specific to alcohol use. However, other substances, including tobacco and marijuana, tend to co-occur with alcohol use, and existing models of substance use coping are fairly non-specific across substances (e.g., Patterson & Stoolmiller, 1991; Patrick et al., 2011; Leonard et al., 2015). We speculate that similar results may be obtained from an alcohol use measure on volume consumed, since studies have shown that using alcohol to cope (i.e., heavy episodic drinking) is strongly correlated with long-term drinking problems and AUDs (Cooper et al., 1992; Kuntsche et al., 2005; Patrick et al., 2011). Finally, it is important to acknowledge that the current analyses were examined within the context of a control sample that was recruited as part of a larger prevention-trial. We did not see treatment effects on depression and alcohol use in preliminary analyses, but focused only on the control condition given the developmental focus of the current analysis. Despite these limitations, the current study expands upon the existing literature, delineating the associations between depression, alcohol use and suicide risk. The long developmental span and inclusion of diagnostic outcomes at age 28 to 30 are important strengths of the current study, which contribute to our understanding of possible gender-differences and mechanisms of association between depression and alcohol use across an important time-frame. Relatively few studies, have tested this model using such long-term longitudinal data, or incorporating MDD and AUD diagnoses, underscoring one of the contributions of the current study to the literature in this area.
Our results have implications in prevention and intervention efforts, indicating that targeting maladaptive coping mechanisms, such as substance use, may attenuate the association between alcohol use and depression over time. Further research will contribute to these findings by identifying additional coping variables that strengthen the association between depression and alcohol use, and to better understand the motivation behind substance use coping.
Supplementary Material
Public Significance Statement.
This study indicates that substance use coping mechanisms may be a central mediator of the association alcohol use and depression, throughout adolescence and early adulthood, a critical developmental period. The tendency to use substances to cope with stress also serves as an indirect link between early depressive symptoms and alcohol use to later diagnoses. Thus, substance use coping is a modifiable risk factor that serve as an important target for developmentally focused prevention and intervention programs.
Acknowledgements
This project was supported by grants DA07031 and DA13773 from the National Institute on Drug Abuse, and AA12702 from the National Institute on Alcohol Abuse and Alcoholism, originally to Dr. Thomas Dishion (deceased). Dr. Connell was supported by grant MH122213 from the National Institute of Mental Health. The funding sources had no other role other than financial support.
Ms. Kelsey Magee and Dr. Arin Connell made a substantial contribution to the analysis and interpretation of data, as well as writing the intellectual content of the manuscript. Both authors have read and approved the final manuscript.
We acknowledge the contribution of the Project Alliance staff, Portland Public Schools, and the participating youth and families.
Footnotes
Additional analyses were conducted in an attempt to improve overall model fit. These results are available as an online supplement, although the results were conceptually very similar to the results presented in the text.
Disclosures
Ms. Kelsey Magee and Dr. Arin Connell have no conflicts of interest to disclose.
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association. [Google Scholar]
- Archie S, Zangeneh K, & Akhtar-Danesh N. (2012). Concurrent binge drinking and depression among Canadian youth: prevalence, patterns, and suicidality. Alcohol, 46, 165–172. 10.1016/j.alcohol.2011.07.001 [DOI] [PubMed] [Google Scholar]
- Blevins CE, Abrantes AM, & Stephens RS (2016). Motivational pathways from antecedents of alcohol use to consequences: a structural model of using alcohol to cope with negative affect. The American Journal of Drug and Alcohol Abuse, 42, 395–403. 10.3109/00952990.2016.1141915 [DOI] [PubMed] [Google Scholar]
- Boden JM, & Fergusson DM (2010). Alcohol and depression. Addiction, 106, 906–914. 10.1111/j.1360-0443.2010.03351.x [DOI] [PubMed] [Google Scholar]
- Briere F, Rohde P, Seeley J, Klein D, & Lewinhson P. (2014). Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Comprehensive Psychiatry, 55, 526–533. 10.1016/j.comppsych.2013.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catanzaro SJ, & Laurent J. (2004). Perceived family support, negative mood regulation expectancies, coping, and adolescent alcohol use: Evidence of mediation and moderation effects. Addictive Behaviors, 29, 1779–1797. 10.1016/j.addbeh.2004.04.001 [DOI] [PubMed] [Google Scholar]
- Connell AM, McKillop HN, & Dishion TJ (2016). Long-term effects of the Family Check-Up in early adolescence on risk of suicide in early adulthood. Suicide and Life-Threatening Behavior, 46(Suppl 1): S15–S22. 10.1111/Fsltb.12254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, & Wolf S. (2015). Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana and tobacco. In Sher KJ (Ed.), The Oxford Handbook of Substance Use Disorders (pp. 36). Oxford Handbooks; Online. 10.1093/oxfordhb/9780199381678.013.017. [DOI] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, & Mudar P. (1992). Stress and alcohol use: moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology, 101, 139–152. 10.1037//0021-843x.101.1.139 [DOI] [PubMed] [Google Scholar]
- Curtin SC, Warner M, & Hedegaard H. (2016). Increase in suicide in the United States, 1999–2014. NCHS Data Brief, 241, 1–8. [PubMed] [Google Scholar]
- Danzo S, Connell AM, & Stormshak EA (2017). Associations between alcohol-use and depression symptoms in adolescence: examining gender differences and pathways over time. Journal of Adolescence, 56, 64–74. 10.1016/j.adolescence.2017.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D, Grant B, Stinson F, & Chou P. (2004). Another Look at Heavy Episodic Drinking and Alcohol Use Disorders among College and Noncollege Youth. Journal of Studies on Alcohol, 65, 477–488. 10.15288/jsa.2004.65.477 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Spencer PM (1982). Brief Symptom Inventory: Administration, scoring, and procedure manual. Baltimore: Clinical Psychometric Research. [Google Scholar]
- Dise-Lewis JE (1988). The life events and coping inventory: an assessment of stress in children. Psychosomatic Medicine, 50(5), 484–499. 10.1097/00006842-198809000-00005 [DOI] [PubMed] [Google Scholar]
- Dishion T, Stormshak E, & Kavanagh K. (2012). Everyday parenting: A professional’s guide to building family management skills. Champaign, IL, US: Research Press. [Google Scholar]
- Edwards AC, Joinson C, Dick DM, Kendler KS, Macleod J, Munafo M, Hickman M, Lewis G, & Heron J. (2014). The association between depressive symptoms from early to late adolescence and later use and harmful use of alcohol. European Child & Adolescent Psychiatry, 23, 1219–1230. 10.1007/s00787-014-0600-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2009). Tests of causal links between alcohol abuse or dependence and major depression. Archives of General Psychiatry, 66, 260–266. 10.1001/archgenpsychiatry.2008.543 [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2013). Alcohol misuse and psychosocial outcomes in young adulthood: results from a longitudinal birth cohort studied to age 30. Drug and Alcohol Dependence, 133(2), 513–519. 10.1016/j.drugalcdep.2013.07.015 [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, & Catalano RF (2008). Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychology of Addictive Behaviors, 22(2), 186–197. 10.1037/0893-164X.22.2.186 [DOI] [PubMed] [Google Scholar]
- Fosco GM, Frank JL, Stormshak EA, & Dishion TJ (2013). Opening the “black box”: Family check-up intervention effects on self-regulation that prevents growth in problem behavior and substance use. Journal of School Psychology, 51, 455–468. 10.1016/j.jsp.2013.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fromme K, Wetherill R, & Neal D. (2010). Turning 21 and the associated changes in drinking and driving after drinking among college students. Journal of American College Health, 59(1), 21–27. 10.1080/07448481.2010.483706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant VV, Stewart SH, & Mohr CD (2009). Coping-anxiety and coping-depression motives predict different daily mood-drinking relationships. Psychology of Addictive Behaviors, 23, 226–237. 10.1037/a0015006 [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, Bradizza CM, & Collins RL (2009). Drinking to cope as a statistical mediator in the relationship between suicidal ideation and alcohol outcomes among underage college drinkers. Psychology of Addictive Behaviors, 23, 443–451. 10.1037/a0015543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM, & Hewell VM (2012). Suicidal ideation and drinking to cope among college binge drinkers. Addictive behaviors, 37, 994–997. 10.1016/j.addbeh.2012.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, & Randall PK (2003). Drinking to cope and alcohol use and abuse in unipolar depression: a 10-year model. Journal of Abnormal Psychology, 112, 159. 10.1037/0021-843X.112.1.159 [DOI] [PubMed] [Google Scholar]
- Hussong AM (2003). Further refining the stress-coping model of alcohol involvement. Addictive Behaviors, 28, 1515–1522. 10.1016/s0306-4603(03)00072-8 [DOI] [PubMed] [Google Scholar]
- Hussong A, Curran P, & Chassin L. (1998). Pathways of risk for accelerated heavy alcohol use among adolescent children of alcoholic parents. Journal of Abnormal Child Psychology, 26, 453–466. 10.1023/a:1022699701996 [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, & Boeding S. (2011). An internalizing pathway to alcohol use disorder. Psychology of Addictive Behaviors, 25, 390–404. 10.1037/a0024519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irons DE, Iacono WG, & McGue M. (2015). Tests of the effects of adolescent alcohol exposures on adult outcomes. Addiction, 110, 269–278. 10.1111/add.12747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Anderson BJ, & Stein MD (2018). Drinking to cope mediates the relationship between depression and alcohol risk: Different pathways for college and non-college young adults. Addictive Behaviors, 80, 116–123. 10.1016/j.addbeh.2018.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney S, Jones RN, & Barnett NP (2015). Gender differences in the effect of depressive symptoms on prospective alcohol expectancies, coping motives, and alcohol outcomes in the first year of college. Journal of Youth and Adolescence, 44, 1884–1897. 10.1007/s10964-015-0311-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2015). Principles and practice of structural equation modeling. Guilford Press: New York, NY. [Google Scholar]
- Kumpulainen K. (2000). Psychiatric symptoms and deviance in early adolescence predict heavy alcohol use 3 years later. Addiction, 95, 1847–1857. 10.1046/j.1360-0443.2000.9512184713.x [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Muller S. (2012). Why do young people start drinking? Motives for first-time alcohol consumption and links to risky drinking in early adolescence. European Addiction Research, 18, 34–39. 10.1159/000333036. [DOI] [PubMed] [Google Scholar]
- Kuntsche EN, Knibbe R, Gmel G, & Engels R. (2005). Why do young people drink? A review of drinking motives. Clinical Psychology Review, 25, 841–861. 10.1016/j.cpr.2005.06.002 [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Ehret PJ, Hummer JF, & Prenovost K. (2012). Poor adjustment to college life mediates the relationship between drinking motives and alcohol consequences: A look at college adjustment, drinking motives, and drinking outcomes. Addictive Behaviors, 37, 379–386. 10.1016/j.addbeh.2011.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Lac A, Kenney SR, & Mirza T. (2011). Protective behavioral strategies mediate the effect of drinking motives on alcohol use among heavy drinking college students: Gender and race differences. Addictive Behaviors, 36, 354–361. 10.1016/j.addbeh.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard NR, Gwadz MV, Ritchie A, Linick JL, Cleland CM, Elliott L, Grethel M. (2015). A multi-method exploratory study of stress, coping, and substance use among high school youth in private schools. Frontiers in Psychology, 6, 1–16. 10.3389/fpsyg.2015.01028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn P, Rohde P, Seeley J, Klein D, & Gotlib I. (2003). Psychosocial functioning of young adults who have experienced and recovered from Major Depressive Disorder during adolescence. Journal of Abnormal Psychology, 112, 353–363. 10.1037/0021-843x.112.3.353 [DOI] [PubMed] [Google Scholar]
- Little RJA (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83, 1198–1202. 10.2307/2290157 [DOI] [Google Scholar]
- Marmorstein NR (2009). Longitudinal associations between alcohol problems and depressive symptoms: Early adolescence through early adulthood. Alcoholism: Clinical & Experimental Research, 33(1), 49–59. 10.1111/j.1530-0277.2008.00810.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Vander Stoep A, McCauley E, & Baer J. (2012). Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs, 73, 444–453. 10.15288/jsad.2012.73.444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty C, Wymbs B, Mason W, King K, McCauley E, Baer J, & Vander Stoep A. (2013). Early adolescent growth in depression and conduct problem symptoms as predictors of later substance use impairment. Journal of Abnormal Child Psychology, 41, 1041–1051. 10.1007/s10802-013-9752-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod G, Horwood L, & Fergusson D. (2016). Adolescent depression, adult mental health and psychosocial outcomes at 30 and 35 years. Psychological Medicine, 46, 1401–1412. 10.1017/S0033291715002950 [DOI] [PubMed] [Google Scholar]
- Monahan KC, Steinberg L, & Cauffman E. (2009). Affiliation with antisocial peers, susceptibility to peer influence, and antisocial behavior during the transition to adulthood. Developmental Psychology, 45, 1520–1530. 10.1037/a0017417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miettunen J, Murray GK, Jones PB, & Maki P. (2014). Longitudinal associations between childhood and adulthood externalizing and internalizing psychopathology and adolescent substance use. Psychological Medicine, 44, 1727–1738. 10.1017/S0033291713002328 [DOI] [PubMed] [Google Scholar]
- Muthén L, & Muthén B. (2015). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nolen-Hoeksema S. (2004). Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review, 24, 981–1010. 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- O’Brien KHM, Becker SJ, Spirito A, Simon V, Prinstein MJ (2013). Differentiating adolescent suicide attempters from ideators: Examining the interaction between depression severity and alcohol use. Suicide and Life-Threatening Behavior, 44, 23–33. 10.1111/sltb.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Schulenberg JE, O’Malley PM, Johnston LD, Bachman JG (2011). Adolescents’ reported reasons for alcohol and marijuana use as predictors of substance use and problems in adulthood. Journal of Studies on Alcohol and Drugs, 72, 106–116. 10.15288/jsad.2011.72.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, & Stoolmiller M. (1991). Replications of a dual failure model for boys’ depressed mood. Journal of Consulting and Clinical Psychology, 59, 491–498. 10.1037/0022-006X.59.4.491 [DOI] [PubMed] [Google Scholar]
- Pedrelli P, Borsari B, Lipson S, Heinze J, & Eisenberg D. (2016). Gender differences in the relationships among major depressive disorder, heavy alcohol use, and mental health treatment engagement among college students. Journal of Studies on Alcohol and Drugs, 77, 620–628. 10.15288/jsad.2016.77.620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters M, Vollebergh W, Wiers R, & Field M. (2014). Psychological changes and cognitive impairments in adolescent heavy drinkers. Alcohol and Alcoholism, 49, 182–186. 10.1093/alcalc/agt162 [DOI] [PubMed] [Google Scholar]
- Pesola F, Shelton KH, Heron J, Munafo M, Maughan B, Hickman M, & van den Bree MBM (2015). The mediating role of deviant peers on the link between depressed mood and harmful drinking. Journal of Adolescent Health, 56, 153–159. 10.1016/j.jadohealth.2014.10.268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Kelley K. (2011). Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychological methods, 16, 93–115. [DOI] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, Glanovsky JL, James A, & Jacobs D. (2009). Adolescent alcohol use, suicidal ideation and suicide attempts. Journal of Adolescent Health, 44, 335–341. 10.1016/j.jadohealth.2008.08.006 [DOI] [PubMed] [Google Scholar]
- Schleider J, Ye F, Wang F, Hipwell A, Chung T, & Sartor S. (2019). Longitudinal reciprocal associations between anxiety, depression, and alcohol use in adolescent girls. Alcoholism, Clinical and Experimental Research, 43, 98–107. 10.1111/acer.13913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settles RF, Cyders M, & Smith GT (2010). Longitudinal validation of the acquired preparedness model of drinking risk. Psychology of Addictive Behaviors, 24, 198–208. 10.1037/a0017631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapinski LA, Edwards AC, Hickman M, Araya R, Teesson M, Newton NC, Kendler KS, & Heron J. (2016). Drinking to cope: a latent class analysis of coping motives for alcohol use in a large cohort of adolescents. Prevention Science, 17, 584–594. 10.1007/s11121-016-0652-5 [DOI] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, & Catalano RF (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors, 37, 747–775. 10.1016/j.addbeh.2012.02.014 [DOI] [PubMed] [Google Scholar]
- Stormshak E, Connell A, Veronneau M, Myers M, Dishion T, Kavanagh K, & Caruthers A. (2011). An ecological approach to promoting early adolescent mental health and social adaptations: Family-centered intervention in public middle schools. Child Development, 82, 209–225. 10.1111/j.1467-8624.2010.01551.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapert SF, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers MG, & Monti PM (2003). Depressed mood, gender, and problem drinking in youth. Journal of Child & Adolescent Substance Use, 12, 55–68. 10.1300/J029v12n04_04 [DOI] [Google Scholar]
- Timko C. (2005). The 8-year course of alcohol abuse: Gender differences in social context and coping. Alcoholism, Clinical and Experimental Research, 29, 612–621. 10.1097/01.alc.0000158832.07705.22 [DOI] [PubMed] [Google Scholar]
- Trucco EM, Colder CR, & Wieczorek WF (2011). Vulnerability to peer influence: A moderated mediation study of early adolescent alcohol use initiation. Addictive Behaviors, 36, 729–736. 10.1016/j.addbeh.2011.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turecki G, & Brent DA (2016). Suicide and suicidal behavior. The Lancet, 387, 1227–1239. 10.1016/S0140-6736(15)00234-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarosa MC, Messer MA, Madson MB, & Zeigler-Hill V. (2018). Depressive symptoms and drinking outcomes: The mediating role of drinking motives and protective behavioral strategies among college students. Substance Use & Misuse, 53, 143–153. 10.1080/10826084.2017.1327974 [DOI] [PubMed] [Google Scholar]
- Willoughby T, & Fortner A. (2015). At-risk depressive symptoms and alcohol use trajectories in adolescence: A person-centered analysis of co-occurrence. Journal of Youth and Adolescence, 44, 793–805. 10.1007/s10964-014-0106-y. [DOI] [PubMed] [Google Scholar]
- Windle M. (2016). Drinking over the lifespan: Focus on early adolescents and youth. Alcohol Research Current Reviews, 38, 95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Scheidt D. (2004). Alcoholic subtypes: are two sufficient? Addiction, 99, 1508–1519. 10.1111/j.1360-0443.2004.00878.x [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1994). Composite International Diagnostic Interview (CIDI) researcher’s manual (Version 1.1, 1994). Geneva, Switzerland: World Health Organization; Arlington, VA, US: American Psychiatric Association. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.