Abstract
A sensitive method has been developed for the quantification of cytomegalic endothelial cells (CEC) in peripheral blood (PB) of patients with active cytomegalovirus (CMV) infections. The three subsequent key steps of this method are density centrifugation to enrich endothelial cells (EC) in the mononuclear cell (MNC) fraction, EC-specific staining, and fluorescence-activated cell sorting (FACS) of EC onto adhesion slides. The FACS method was compared with the conventional method of cytocentrifugation of the MNC fraction onto slides, followed by EC-specific staining. The main advantage of the additional steps for the isolation and quantification of CEC in PB by FACS is a 10-times-greater sensitivity than by cytocentrifugation of the MNC fraction alone. The recovery percentages of EC from whole blood were comparable for both methods. Recoveries of EC obtained after FACS were 53% ± 16.5%, (mean ± standard deviation), and recoveries of EC obtained after cytocentrifugation of the MNC fraction were 43% ± 4.3%. In patients with active CMV infection, 5 to 72 CEC were detected by FACS, equivalent to 0.8 to 9.0 CEC/ml of blood. With this method for isolation and quantification, the characterization of CEC in PB of patients with CMV-associated clinical symptoms, as well as the quantification of EC in PB of patients with pathophysiological manifestations involving endothelial damage that are different from those caused by CMV infections, can be performed.
In immunocompromised patients, e.g., organ transplant recipients and human immunodeficiency virus-infected patients, cytomegalovirus (CMV) may cause symptomatic infections involving several organs (30). Patients with active CMV infection may show subtle disturbances in organ function, even without clinically manifest CMV disease symptoms. An indicator of subtle disturbances in the lungs is a decrease in pulmonary diffusion for CO (31). Effects of CMV infection on the intestines were shown by an increased intestinal permeability to lactulose (3). Although mechanisms of CMV-induced pathophysiology in patients are not clear, we think endothelial cells (EC) are involved. Results from histochemical studies of CMV-infected lung and gastrointestinal tissues show that EC are important targets for virus, together with epithelial cells, fibroblasts, and smooth muscle cells (23).
Another important finding is the occurrence of cytomegalic EC (CEC) in peripheral blood (PB), as described by Grefte et al. (9, 10); CEC appear during or shortly after the peak in CMV pp65 antigenemia in patients with active CMV infection. These CEC in PB might be correlated with the severity of CMV disease and organ involvement (8, 17), although we were unable to confirm a relationship between clinical symptoms and the mere presence of CEC in blood (9). Therefore, the development of a quantitative method to detect CEC in PB should give more insight into the relationship between CEC counts in PB and organ involvement. In addition, with this method further studies towards characterization of CEC should be possible.
In addition to CMV infections, EC or EC carcasses circulating in blood have been noticed in several other pathophysiological conditions, including damage due to heart catheterization, infections, or intravascular coagulation (7, 14, 20, 27). At present, different strategies to identify EC in blood have been described. One procedure makes use of Ficoll-Hypaque density centrifugation followed by cytocentrifuge preparation of cells on slides and subsequent immunocytochemical staining of EC. This strategy was described for EC in the mononuclear cell (MNC) fraction of PB from patients after heart catheterization (20). Also, CMV-infected EC were detected in MNC fractions (9).
Another method was originally designed for the isolation of rare cell populations from blood, for instance, epithelial cells in blood from cancer patients or isolation of stem cells from human cord blood (12, 19), and involves fluorescence-activated cell sorting (FACS).
For the development of a quantitative method, we isolated EC from whole blood by density centrifugation, followed by EC-specific staining and subsequent FACS of the MNC fraction onto adhesion slides. The FACS method was compared to centrifugation of the MNC fraction onto slides, followed by EC-specific staining. Experiments were performed with noninfected EC or human CMV-infected EC; with these cell populations, no differences in recovery between the two methods were observed.
We report FACS as a method with improved sensitivity for studying the kinetics of the occurrence of CEC in PB during CMV infection and for further characterization of the isolated CEC in PB of CMV patients.
MATERIALS AND METHODS
Antibodies.
EC-specific antibodies were E1/1 2.3, a mouse monoclonal antibody directed to a 90-kDa cell surface antigen (18), and a polyclonal rabbit antibody against vWf (Dakopatts A/S, Glostrup, Denmark). Antibodies directed against exon 2 of the major immediate early gene were E13 (15) (fluorescein isothiocyanate [FITC]) (Biosoft, Paris, France) and C10/C11, a mixture of two mouse monoclonal antibodies directed to CMV pp65 (29).
Cell culture.
Human umbilical vein EC were isolated from human umbilical cord veins (13, 16). Briefly, EC were harvested from umbilical cords by using chymotrypsin and were grown on 1% gelatin in endothelial growth medium (RPMI 1640, 20% pooled human serum or 20% foetal calf serum, 50 μg of EC growth factor per ml, 5 U of heparin per ml, 2 mM glutamine, 100 U of penicillin per ml, and 0.1 mg of streptomycin per ml). EC were used at passage two or three.
CMV-infected EC.
The endotheliotropic CMV clinical isolate TB42 (24) was used to infect EC cultures. Viral infection of EC was achieved by seeding trypsinized CMV-infected EC together with uninfected EC at a ratio 1:10 in culture flasks. After 6 days, more than 95% of the EC were infected, as determined by immunostaining of cytocentrifuged cells (Cytospin II, Shandon, Astmoor, United Kingdom). Cells were analyzed by immunofluorescence staining for the CMV major immediate early viral protein.
Patients.
Blood samples were obtained from two patients: three blood samples from one patient at different time points and one blood sample from the other patient. The samples were drawn from a cubital vein via venapuncture after 10 min of venous stasis (by tourniquet) and gentle rubbing of the forearm. The samples were from two kidney transplant recipients with an active CMV infection, as diagnosed by positive CMV antigenemia (29).
CMV antigenemia.
The CMV antigenemia assay was performed according to the method described by Van der Bij et al. (29). Briefly, peripheral blood leukocytes were dextran sedimented, followed by lysis of remaining erythrocytes with NH4Cl. After two washes, the leukocytes were counted and cytospots were prepared. Spots were indirectly stained with C10/C11, a mixture of two mouse monoclonal antibodies directed against CMV pp65 (11). Cells positive for pp65 were counted, the number of negative cells were counted by automated image analysis (Quantimet, Leica, Rijswijk, The Netherlands), and positive cells were expressed per 50,000 leukocytes screened. Two spots were analyzed for each patient sample.
Enrichment of EC by density gradient centrifugation.
Using an in vitro model to study EC in blood, we added EC to whole blood or to MNC fractions. Diluted EC were counted twice in a Nageotte (Omnilabo, Etten-Leur, The Netherlands) hemocytometer before the cells were added to 1 ml of whole blood or 106 MNC. Blood obtained by venapuncture from healthy donors was collected in siliconized tubes (Vacutainer; Becton Dickinson, Meylan, France) containing EDTA or heparin. Cell differentiation of whole blood samples was performed on a Coulter STKS (Coulter Electronics, Hialeah, Fla.). The MNC fraction with or without added EC was isolated by Lymfoprep (Nycomed Pharma AS, Oslo, Norway) (d = 1.077 g/cm2) density gradient centrifugation and washed twice with RPMI 1640. Cells were counted in a Coultercounter (Cell-Dyn 610; Abbott Diagnostics, Irving, Tex.).
FACS.
EC were added to whole blood or to MNC or were first stained with E1/1 2.3, quantified, and added immediately prior to FACS. MNC with or without EC were stained with E1/1 2.3 on ice for 30 min, washed twice with ice-cold Hanks’ balanced salt solution and 5% human pooled serum, and subsequently labelled with FITC-conjugated rabbit anti-mouse immunoglobulin G on ice for 30 min. Cells were washed twice and collected in Hanks’ balanced salt solution and 5% human pooled serum. FACS was performed on a Coulter Epics Elite equipped with a gated amplifier and upgraded with enhanced system performance. A sortgate was set by measuring MNC and E1/1 2.3-labelled EC, whereby the gate was selected for log forward scatter/log side scatter and FITC-positive cells. Cells were triggered for sorting by a positive FITC signal. The FITC-positive cells were sorted onto adhesion slides (Bio-Rad, Munich, Germany) and fixed with 1% paraformaldehyde in phosphate-buffered saline. Afterwards, the adhered cells were stained with DAPI (4′,6-diamidino-2-phenylindole dihydrochloride) (Boehringer Mannheim, Almere, The Netherlands), which binds selectively to DNA. Recovery was determined by counting FITC-positive cells with a pale oval nucleus. Three samples were processed and tested for each measurement, unless mentioned otherwise.
Cytocentrifugation.
MNC fractions with or without EC were cytocentrifuged onto slides at 550 rpm for 5 min (Cytospin II). Cytospots were fixed with 1% paraformaldehyde in phosphate-buffered saline and stained for EC markers. DAPI (Boehringer Mannheim) was used for counterstaining. Recovery was determined by counting FITC-positive stained cells. Three samples were processed and tested for each measurement, unless mentioned otherwise.
Statistical analysis.
The unpaired t test was used to compare differences in recovery.
RESULTS
EC recovery after FACS.
To develop a quantitative method, we determined EC recoveries for the different steps during isolation and we correlated EC losses to losses of MNC. The FACS method was composed of three key steps: density centrifugation, EC-specific staining, and FACS of EC out of the MNC fraction onto adhesion slides. Cell losses after the density centrifugation step were 17.6% ± 15% (mean ± standard deviation) of MNC and also of EC. EC were obtained solely from the MNC fraction after density centrifugation, as no EC were detected in the granulocyte fraction. The largest loss of MNC, including EC, was 30% ± 25% due to washing of the cells during the staining procedure. Losses due to FACS onto adhesion slides and adhesion of the sorted EC were negligible. Loss percentages of MNC and EC isolated from whole blood were similar at 30% ± 25% and 38%, respectively (EC recovery, 62% ± 17.2%). During FACS purification itself, virtually no EC were lost (EC recovery, 98% ± 3.6%), whereas most of the blood MNC (>99%) were removed. EC added directly to adhesion slides were recovered at a rate of 94% ± 11.4%. Thus, recovery of EC added to whole blood was 53% ± 16.5%, caused by losses due to isolation of the MNC fraction and EC-specific staining.
EC recovery after cytocentrifugation of MNC fractions.
Similarly, the effects of every step on specific losses of added EC were examined for the cytocentrifugation procedure. Density centrifugation resulted in a loss of 25.8% ± 13.8% of the cells, and cytocentrifugation of the MNC fraction caused an additional loss of MNC of approximately 33%. Recovery of EC from whole blood after density centrifugation and cytocentrifugation was 43% ± 4.3%. For each sample of the MNC fraction, four or more cytospots were analyzed for quantification of EC among the MNC on a spot. We also determined the variance between samples and the different spots per sample. The spread in recovery of EC between spots appeared to be larger (intratest variance, 23.5%) than between different samples (intertest variance, 6.0%). Thus, EC isolated from whole blood by FACS sorting or cytocentrifugation of MNC resulted in similar recovery percentages of preadded EC from whole blood, 43% ± 4.3% and 53% ± 16.5%, respectively.
CMV-infected EC.
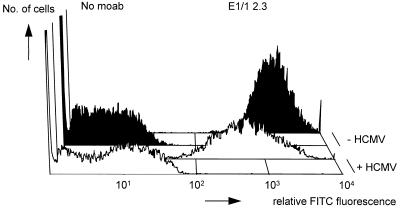
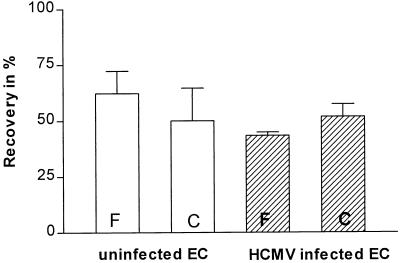
The surface expression level of the antigen for monoclonal antibody E1/1 2.3 was more heterogeneous on CMV-infected EC, and the mean fluorescence intensity was lower, than on noninfected EC (Fig. 1). However, the expression level was sufficiently high to discriminate between FITC-positive and -negative cells (FITC fluorescence is used as the sortpulse). During the FACS procedure or cytocentrifugation of MNC, CMV-infected EC and uninfected EC behaved similarly (Fig. 2). FACS of CMV-infected EC showed an extra decrease of 18% in recovery; uninfected EC did not show any decrease (Fig. 2). However, this difference was not statistically significant.
FIG. 1.
Expression of E1/1 2.3 on CMV-infected (white histograms) and noninfected (black histograms) EC. For each group, an E1/1 2.3-stained sample and a nonstained sample are shown. moab, monoclonal antibody.
FIG. 2.
Recovery of CMV-infected and noninfected EC. One hundred noninfected EC (open bars) or CMV-infected EC (hatched bars) were added to 106 MNC. No differences in recovery between CMV-infected EC and noninfected EC were observed after FACS (F) (P = 0.239) or cytocentrifugation followed by subsequent immunofluorescent staining (C) (P = 0.917) (unpaired t test). Experiments were performed in triplicate (FACS of CMV-infected EC, n = 2). For each sample, three or four cytospots were analyzed.
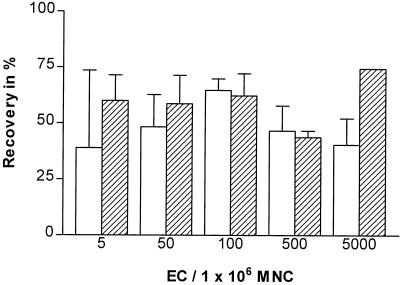
Detection range.
Next, we studied the recovery of a dilution series of EC added to MNC, varying from 5,000 to 5 EC added to 106 MNC. A minimum of 5 EC was reproducibly detected by FACS as well as by cytocentrifugation and immunofluorescent staining (Fig. 3). The quantification of EC on cytospots with limited spread in recovery was possible only with a minimum of 50 EC added to 106 MNC. Below this level, recovery decreased and the variation of recovery increased (Fig. 3). With the FACS procedure, about 60% of the preadded EC were recovered over the whole range of added EC tested. In addition, recovery was also constant when 50 EC were isolated from either 1 × 106, 5 × 106, or 10 × 106 MNC (data not shown).
FIG. 3.
Lower limit of detection. A range of 5 to 5,000 EC were added to 106 MNC. Recovery was determined by FACS (hatched bars) or by cytocentrifugation and immunofluorescent staining (open bars). Experiments were performed in triplicate (where no error bar is depicted, n = 1). For each sample, at least three or four cytospots were analyzed.
Quantification of CEC in PB from patients.
To evaluate the quantification procedure for CEC in PB, we determined CEC counts in PB from four blood samples of patients with active CMV infection and compared detected CEC numbers after FACS or cytocentrifugation. After FACS of a range of 4 to 8 ml of blood (Table 1), 5 to 72 CEC were detected, equivalent to 0.8 to 9.0 CEC/ml of blood (sample 4, sample 1). Counting of CEC on cytospots of MNC fraction resulted in the detection of maximally 14 CEC (sample 1). Although fewer CEC were detected per cytospot, the recoveries of CEC per milliliter of blood were comparable in the samples containing approximately 10 CEC per ml of blood.
TABLE 1.
Detection of CEC in blood of patients after FACS or after cytocentrifugation of MNC fractions
| Blood samplea | Amt of blood analyzed (ml)b
|
No. of MNC in MNC fraction/ml of blood (106) | No. of CEC detected
|
No. of CEC/ml of blood
|
No. of CEC/500,000 MNC (Cytospot) | |||
|---|---|---|---|---|---|---|---|---|
| FACS | Cytospot | FACS | Cytospot | FACS | Cytospot | |||
| 1 | 8.0 | 1.9 | 0.43 | 72 | 14 | 9.0 | 7.4 | 17.5 |
| 2 | 4.0 | 0.8 | 1.0 | 43 | 9 | 10.8 | 11.3 | 11 |
| 3 | 5.8 | 0.7 | 0.43 | 13 | 0 | 2.2 | 0 | 0 |
| 4 | 6.0 | 1.0 | 0.1 | 5 | 0 | 0.8 | 0 | 0 |
Three blood samples were obtained from a single patient at different time points (samples 1 to 3), and one blood sample was from another patient (sample 4).
The amount of blood analyzed refers to the final number of MNC analyzed. MNC were originally obtained from the indicated blood volumes.
Dextran sedimentation of granulocytes with subsequent cytocentrifuge preparation (routinely performed to monitor CMV antigenemia [29]) and immunocytochemical staining specific for EC were performed to detect numbers of CEC in PB. Similar blood samples were processed as used for FACS and cytocentrifugation of MNC fractions. The number of CEC per milliliter of blood obtained by dextran sedimentation (Table 2) did not correlate with the number of CEC per milliliter of blood by FACS onto slides or on cytospots of MNC fractions (Table 1).
TABLE 2.
Detection of CEC in PB from CMV patients by dextran sedimentation
| Blood samplea | Amt of blood analyzed (ml)b | No. of granu- locytes/ml of blood (106) | No. of CEC detected | No. of CEC/ml of blood | CMV antigen- emiac |
|---|---|---|---|---|---|
| 1 | n.d.d | n.d. | n.d. | n.d. | 3410 |
| 2 | 0.14 | 5.9 | 0 | 0 | 3500 |
| 3 | 1.0 | 0.5 | 0 | 0 | 1571 |
| 4 | 1.0 | 0.56 | 1 | 1 | 52 |
Samples 1 to 4 are the same as in Table 1. However, CEC were isolated by dextran sedimentation.
The amount of blood analyzed refers to the final number of MNC analyzed. MNC were originally obtained from the indicated blood volumes.
Values are the numbers of pp65-positive granulocytes per 50,000 polymorphonuclear leukocytes.
n.d., not determined.
DISCUSSION
We present a three-step method to isolate and quantify CEC from PB samples. For the development of this quantitative method, we used in vitro-cultured EC preadded to different steps of the isolation procedure, and cell losses during the individual isolation steps were determined. Because EC were detected only in the MNC fraction, we anticipated that these cells would behave like MNC during isolation and staining procedures. As expected, the losses of MNC and EC were comparable. Thus, determination of MNC losses before isolation and just before sorting indicated a loss factor for EC showing that the numbers of EC in blood were approximately twice the number of detected EC. After FACS and binding of sorted cells to adhesion slides, almost all cells were recovered on the slides. After cytocentrifugation of the MNC fraction, approximately 40% of all cells were lost. These inevitable losses were due both to adherence of cells to the centrifugation cups and to cells being drawn into the paper cards. Cell losses were negligible after binding to adhesion slides (recovery, 94% ± 11.4%). Determination of MNC counts prior to FACS, therefore, indicates losses of EC during the whole three-step quantification procedure.
Because functional and morphological properties of CMV-infected EC are seriously disturbed (1, 2, 5, 9, 21, 22, 25, 26, 28), isolation characteristics of CEC from patients could differ from noninfected EC. In particular, expression of surface antigens is influenced by infection of EC with CMV (2, 9, 21, 25). Therefore, we verified the expression of the antigen of monoclonal antibody E1/1 2.3 on CMV-infected EC and confirmed staining of EC with E1/1 2.3. Although decreased expression of this EC antigen after infection of EC with CMV was observed (Fig. 1), the monoclonal antibody could still be used as a tool for immunoaffinity methods. In addition, little or no cross-reactivity with other blood cells should occur. Some monocytes stained weakly positive with E1/1 2.3; however, this background did not disturb our quantification because the isolated cells were also evaluated afterwards by fluorescence microscopy for cytomegalic morphology and fluorescence intensity.
The present study with infected EC, including late-stage-infected EC with the owl’s eye appearance, showed a slight reduction in recovery, which could be due to a decreased expression of the antigen for monoclonal antibody E1/1 2.3 (Fig. 1). Another reason for the reduction in recovery could be the increased fragility of EC after CMV infection (30% more cell death of CMV-infected EC than of uninfected EC).
For the development of a quantitative method to detect CEC in PB by using FACS, the MNC fraction with EC was stained with monoclonal antibody E1/1 2.3, followed by FITC-conjugated rabbit anti-mouse immunoglobulin. Because an additional staining step involves additional washings, the recovery of EC out of the MNC fraction could be improved by using primary antibodies which are conjugated directly to a fluorescent dye, e.g., an E1/1 2.3-FITC conjugate.
According to our results obtained by in vitro-added EC (approximately 50% recovery for both methods), isolation of CEC from PB from patients by FACS or by cytocentrifugation resulted in an equal yield of CEC per milliliter of blood for each method. However, after isolation of CEC from patients by FACS, a fivefold greater level of CEC was detected than by cytocentrifugation and immunofluorescent staining. The increased detection level of CEC after FACS was the result of the higher number of cells that could be processed and the almost complete removal of MNC. Consequently, a high signal (CEC)-to-noise (MNC) ratio was obtained, allowing for easy quantification of the sorted CEC after their binding to adhesion slides.
Another aspect of the comparison between FACS and cytocentrifugation is the influence of clinical symptoms like leukopenia (30) or lymphocytosis (4). Both symptoms can occur in transplant recipients after rejection therapy or due to CMV infection and result in altered MNC levels in blood. Alteration in the MNC levels alters the number of CEC in PB per number of MNC. Until now, CEC have been correlated with MNC numbers present on cytospots instead of blood volume (8–10, 17). However, CEC in PB are likely to originate from the venous vessel wall and might therefore be more indicative of vascular damage. To correct for high levels of CEC in patients caused by low MNC numbers, we argue for a relationship between CEC and blood volume.
Regarding a total body blood volume of approximately 5 liters, the detected concentrations of 10 CEC/ml of PB actually represented 50,000 EC. No data about the kinetics of the clearing of circulating EC are available. Data obtained from CEC in PB after angioplasty showed comparable concentrations of EC in arterial and venous blood (6, 20), suggesting that released EC might circulate. In the case of CMV-infected cytomegalic altered EC (size, 30 to 40 μm), it is unknown whether these cells recirculate or become trapped in capillary vessels, thus evoking disturbances in organ function.
In conclusion, a reliable three-step method based on FACS was developed to isolate and quantify CEC from PB of patients with active CMV infection. This method resulted in greater sensitivity than analysis of the MNC fraction on cytospots, as described by us earlier (9). Furthermore, we argue that relating CEC counts to the blood volume analyzed makes the results more comparable.
EC in PB are described for several pathophysiological conditions involving endothelial damage; thus, our quantitative method could be applied to study of the release of cells caused by vascular damage. In addition, our method is useful for detection of different kinds of rare cells circulating in the bloodstream.
ACKNOWLEDGMENTS
We thank Geert Mesander for assistance with FACS, Roelie van Wijk and Lucien Gjaltema for EC culture assistance, M. A. Gimbrone, Jr., Department of Pathology, Harvard Medical School, Boston, Mass., for monoclonal antibody E1/1 2.3, and C. Sinzger for providing the EC-adapted CMV clinical isolate TB42.
Grant support was provided by the Dutch Kidney foundation (C94.1386) and the European Commission (ERB BMH4CT-0471 [DG12-SSMA]).
REFERENCES
- 1.Almeida G D, Porada C D, St. Jeor S S, Ascensao J L. Human cytomegalovirus alters interleukin-6 production by endothelial cells. Blood. 1994;83:370–376. [PubMed] [Google Scholar]
- 2.Bruggeman C A, Debie W H M, Muller A D, Schutte B, van Dam-Mieras M C E. Cytomegalovirus alters the von Willebrand factor content in human endothelial cells. Thromb Haemostasis. 1988;58:264–268. [PubMed] [Google Scholar]
- 3.de Maar E F, Kleibeuker J H, Boersma-van Ek W, The T H, van Son W J. Increased intestinal permeability during cytomegalovirus infections in renal transplant recipients. Transplant Int. 1996;9:576–580. doi: 10.1007/BF00335558. [DOI] [PubMed] [Google Scholar]
- 4.Einsele H, Ehninger G, Steidle M, Fischer I, Bihler S, Gerneth F, Vallbracht A, Schmidt H, Waller H D, Muller C A. Lymphocytopenia as an infavorable prognostic factor in patients with cytomegalovirus infection after bone marrow transplantation. Blood. 1993;82:1672–1678. [PubMed] [Google Scholar]
- 5.Garrett J S, Narus J C, Bohnsack J F, Carling D E, Grieves K G, Waldman W J, Shaddy R E. Effects of cytomegalovirus infection on growth factor production in endothelial cells and fibroblasts. Pediatr Res. 1995;38:1003–1008. doi: 10.1203/00006450-199512000-00029. [DOI] [PubMed] [Google Scholar]
- 6.George F, Brisson C, Poncelet P, Laurent J C, Massot O, Arnoux D, Ambrosi P, Klein-Soyer C, Cavenaze J P. Rapid isolation of human endothelial cells from whole blood using S-Endo1 monoclonal antibody coupled to immuno-magnetic beads: demonstration of endothelial injury after angioplasty. Thromb Haemostasis. 1992;67:147–153. [PubMed] [Google Scholar]
- 7.George F, Brouqui P, Boffa M C, Mutin M. Demonstration of Rickettsia Conorii-induced endothelial injury in vivo by measuring circulating endothelial cells, thrombomodulin, and von Willebrand factor in patients with Mediterranean Spotted Fever. Blood. 1993;82:2109–2116. [PubMed] [Google Scholar]
- 8.Gerna G, Percivalle E, Revello M G, Morini F. Correlation of quantitative human cytomegalovirus pp65-, p72- and p150-antigenemia, viremia and circulating endothelial giant cells with clinical symptoms and antiviral treatment in immunocompromised patients. Clin Diagn Virol. 1993;1:47–59. doi: 10.1016/0928-0197(93)90033-2. [DOI] [PubMed] [Google Scholar]
- 9.Grefte A, van der Giessen M, van Son W J, The T H. Circulating cytomegalovirus (CMV)-infected endothelial cells in patients with an active CMV infection. J Infect Dis. 1993;167:270–277. doi: 10.1093/infdis/167.2.270. [DOI] [PubMed] [Google Scholar]
- 10.Grefte A, Blom N, van der Giessen M, van Son W J, The T H. Ultrastructural analysis of circulating cytomegalic cells in patients with active cytomegalovirus infection: evidence for virus production and endothelial origin. J Infect Dis. 1993;168:1110–1118. doi: 10.1093/infdis/168.5.1110. [DOI] [PubMed] [Google Scholar]
- 11.Grefte J M M, van der Gun B T F, Schmolke S, van der Giessen M, van Son W J, Plachter B, Jahn G, The T H. The lower matrix protein pp65 is the principal viral antigen present in peripheral blood leukocytes during an active cytomegalovirus infection. J Gen Virol. 1992;73:923–932. doi: 10.1099/0022-1317-73-11-2923. [DOI] [PubMed] [Google Scholar]
- 12.Gross H-J, Verwer B, Houch D, Hoffman R A, Recktenwald D. Model study detecting breast cancer cells in peripheral blood mononuclear cells at frequencies as low as 10−7. Proc Natl Acad Sci USA. 1995;92:537–541. doi: 10.1073/pnas.92.2.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaffe E A, Nachman R L, Becher C G, Minick C R. Culture of human endothelial cells derived from umbilical veins: identification by morphologic and immunologic criteria. J Clin Investig. 1973;52:2745–2756. doi: 10.1172/JCI107470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lefevre P, George F, Durand J M, Sampol J. Detection of circulating endothelial cells in thrombotic thrombocytopenic purpura. Thromb Haemostasis. 1993;69:522–532. [PubMed] [Google Scholar]
- 15.Mazeron M C, Jahn G, Plachter B. Monoclonal antibody E-13 (M-810) to human cytomegalovirus recognizes an epitope encoded by exon 2 of the major immediate early gene. J Gen Virol. 1992;73:2699–2703. doi: 10.1099/0022-1317-73-10-2699. [DOI] [PubMed] [Google Scholar]
- 16.Mulder A B, Blom N R, Ruiters M H J, van der Meer J, Halie M R, Bom V J J. Basal tissue factor expression in endothelial cell cultures is caused by contaminating smooth muscle cells: reduction by using chymotrypsin instead of collagenase. Thromb Res. 1995;80:399–411. doi: 10.1016/0049-3848(95)00192-t. [DOI] [PubMed] [Google Scholar]
- 17.Percivalle E, Revello M G, Vago L, Gerna G. Circulating endothelial giant cells permissive for human cytomegalovirus (CMV) are detected in disseminated CMV infections with organ involvement. J Clin Investig. 1993;92:663–670. doi: 10.1172/JCI116635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pober J S, Gimbrone M A, Jr, Lapiere L A, Mendrick D L, Fiers W, Rothlein R, Springer T A. Overlapping patterns of activation of human endothelial cells by interleukin 1, tumor necrosis factor, and immune interferon. J Immunol. 1986;137:1893–1896. [PubMed] [Google Scholar]
- 19.Radbruch A, Recktenwald D. Detection and isolation of rare cells. Curr Opin Immunol. 1995;7:270–273. doi: 10.1016/0952-7915(95)80014-x. [DOI] [PubMed] [Google Scholar]
- 20.Sbarbati R, de Boer M, Marzilli M. Immunologic detection of endothelial cells in human whole blood. Blood. 1991;77:764–769. [PubMed] [Google Scholar]
- 21.Sedmak D D, Knight D A, Vook N C, Waldman W J. Divergent patterns of ELAM-1, ICAM-1, and VCAM-1 expression on cytomegalovirus-infected endothelial cells. Transplantation. 1994;58:1379–1385. [PubMed] [Google Scholar]
- 22.Shahgasempour S, Woodroffe S B, Sullivan-Tailyour G, Garnett H M. Alterations in the expression of endothelial cell integrin receptors α5β1 and α2β1 and α6β1 after in vitro infection with a clinical isolate of human cytomegalovirus. Arch Virol. 1997;142:125–138. doi: 10.1007/s007050050063. [DOI] [PubMed] [Google Scholar]
- 23.Sinzger C, Grefte A, Plachter B, Gouw A S H, The T H, Jahn G. Fibroblasts, epithelial cells, endothelial cells and smooth muscle cells are major targets of human cytomegalovirus infection in lung and gastrointestinal tissues. J Gen Virol. 1995;76:741–750. doi: 10.1099/0022-1317-76-4-741. [DOI] [PubMed] [Google Scholar]
- 24.Sinzger C, Knapp J, Plachter B, Schmidt K, Jahn G. Quantification of replication of clinical cytomegalovirus isolates in cultured endothelial cells and fibroblasts by a focus expansion assay. J Virol Methods. 1997;63:103–112. doi: 10.1016/s0166-0934(97)02082-x. [DOI] [PubMed] [Google Scholar]
- 25.Span A H, Mullers W, Miltenburg A M, Bruggeman C A. Cytomegalovirus induced PMN adherence in relation to an ELAM-1 antigen present on infected endothelial cell monolayers. Immunology. 1991;72:355–360. [PMC free article] [PubMed] [Google Scholar]
- 26.Span A H, van Dam Mieras M C, Mullers W, Endert J, Muller A D, Bruggeman C A. The effect of virus infection on the adherence of leukocytes or platelets to endothelial cells. Eur J Clin Investig. 1991;21:331–338. doi: 10.1111/j.1365-2362.1991.tb01378.x. [DOI] [PubMed] [Google Scholar]
- 27.Takahashi H, Harker L A. Measurement of human endothelial cells in whole blood. Thromb Res. 1983;31:1–12. doi: 10.1016/0049-3848(83)90002-6. [DOI] [PubMed] [Google Scholar]
- 28.van Dam Mieras M C, Muller A D, van Hinsbergh V W, Mullers W J, Bomans P H, Bruggeman C A. The procoagulant response of cytomegalovirus infected endothelial cells. Thromb Haemostasis. 1992;68:364–370. [PubMed] [Google Scholar]
- 29.van der Bij W, Torensma R, van Son W J, Anema J, Schirm J, Tegzess A M C, The T H. Rapid immunodiagnosis of active cytomegalovirus infection by monoclonal antibody staining of blood leucocytes. J Med Virol. 1988;25:179–188. doi: 10.1002/jmv.1890250208. [DOI] [PubMed] [Google Scholar]
- 30.van Son W J, The T H. Cytomegalovirus infection after organ transplantation: an update with special emphasis on renal transplantation. Transplant Int. 1989;2:147–164. doi: 10.1007/BF02414602. [DOI] [PubMed] [Google Scholar]
- 31.van Son W J, Peset R, Duipmans J C, van der Mark T M, The T H, Tegzess A M. Cytomegalovirus infection after renal transplantation: pulmonary dysfunction measured by decreased diffusing capacity for carbon monoxide in patients with symptomatic and asymptomatic infection. Transplantation. 1987;44:149–150. doi: 10.1097/00007890-198707000-00029. [DOI] [PubMed] [Google Scholar]