Abstract
BACKGROUND
Psychological issues usually accompany the pregnancy of first-time mothers, and psychoeducational interventions might be effective in addressing these concerns and preparing first-time mothers for childbirth and the postnatal period.
OBJECTIVE
This study aimed to identify, analyze, and synthesize the components and determine the effectiveness of psychoeducational interventions that are used for managing psychological issues and enhancing birth preparedness among primigravid women or couples in low- and middle-income countries.
STUDY DESIGN
A systematic search of 12 databases (APA PsycINFO, EmCare, Embase, MEDLINE(R), Ovid Nursing, British Nursing Index, Health & Medical Collection, ProQuest, CINAHL, Cochrane, Hinari, and PubMed) was conducted to identify relevant studies published between 1946 and October 2021. The quality of the included studies was appraised by the Joanna and Briggs Institute critical appraisal tool, and a narrative synthesis was performed to analyze data extracted from included articles. The systematic review protocol is registered with the International Prospective Register of Systematic Reviews (registration number: CRD42021237896).
RESULTS
The initial search yielded 8658 articles. Of note, 16 articles, including 7 randomized controlled trials and 9 nonrandomized trials, met the inclusion criteria and were selected and reviewed for quality. In addition, 31 outcomes were measured in the studies, including psychological outcomes, birth preparedness outcomes, and other outcomes. The design of the interventions included antenatal education that was delivered through lectures, role plays, trainings, and antenatal counseling. All the psychoeducational interventions had a significant effect (P<.05; Cohen's d or Hedges’ g=0.2–1.9) on certain psychological outcomes, including childbirth attitude, fear of childbirth, depression, fear, and anxiety, and birth preparedness outcomes.
CONCLUSION
Although first-time mothers experience a range of psychological issues during pregnancy, psychoeducational interventions were beneficial in addressing their psychological concerns. It would seem that these interventions are less expensive and could be easily implemented in low- and middle-income countries. However, rigorous research, such as randomized controlled trials, is hereby warranted to standardize the interventions and outcome assessment tools.
Keywords: Psychoeducation, Psychological issues, Birth preparedness, Low- and middle-income countries, First-time mothers
AJOG Global Reports at a Glance.
Why was this study conducted?
Evidence showing the extent of the positive effects and a suitable design for the antenatal psychological and/or birth preparedness education in this cohort is still lacking in most low- and middle-income countries (LMICs).
Key findings
Designing psychoeducational interventions based on evidence, culture, and available resources in LMICs and implementing policies to allow spouses to attend antenatal education with their pregnant partners can help to improve the psychological status and birth preparedness of the first-time parents. Most of the methods used to deliver the psychoeducational interventions resulted in a significant decrease in psychological outcomes and improved birth preparedness; however, antenatal education was mostly used
What does this add to what is known?
Most instruments used to assess the outcomes in LMICs were self-designed, and there is a need to standardize and validate instruments for assessing the outcomes among this cohort.
Introduction
Transition to parenthood is an important life event involving both pregnant individuals and their partners.1 Pregnancy of first-time mothers is often associated with issues affecting their psychological functioning.2 This is so because the period of pregnancy is usually associated with ambivalence and frequent mood changes, varying from anxiety, fatigue, exhaustion, sleepiness, and depression to excitement.3, 4, 5 To some persons, the thoughts of pregnancy can bring about several worries, which may be so intense that they acquire a feature of phobia.6 In most countries, the physical healthcare of pregnant women has improved significantly, but there is still a long way to go with psychological care.7 Most pregnant women in low- and middle-income countries (LMICs) have limited access to information and a lack of psychological care associated with pregnancy and birth preparedness.8 This is especially true for first-time mothers and couples8,9 experiencing psychological issues at the early stage of pregnancy, which increases with the advancement in pregnancy.10
According to Camoirano,11 a first-time mother may experience emotional fluctuations between positive feelings and negative ones during the first trimester of pregnancy. During the second trimester of pregnancy, the mood fluctuations continue, and the negative feelings could sometimes lessen, and during the third trimester of pregnancy, the negative emotional feelings could intensify again.11 Nevertheless, with appropriate birth preparedness through psychoeducation, first-time mothers and their partners can become empowered to cope with their psychological concerns, hence transiting safely into parenthood.11,12
Psychoeducation or psychoeducational interventions refer to activities that combine education and counseling. Psychoeducational interventions may be delivered individually or in groups.13,14 Often, the components of psychoeducation that enhance its effectiveness among pregnant women usually include activities that vitalize the capacity of giving birth, promote self-efficacy, provide psychological support, and equip pregnant women with realistic plans on transportation, delivery location, birth companionship, blood donors, materials for safe childbirth, and other delivery-related decision-making.12,15, 16, 17, 18
A previous systematic review found that the effects of psychoeducational intervention delivered to pregnant women only or with their partners can have a far-reaching effect on the postpartum period to ameliorate depression and paternal negative effects.19 Another study reported that psychoeducation for pregnant women, especially first-time mothers increased the rates of spontaneous vaginal delivery, reduced cesarean delivery (CD) rates, and improved women's delivery experience.20 Similarly, a comparative study evaluating midwife-led psychoeducation through counseling on 53 fearful women reported positive results in the intervention group compared with the control group.21
Aside from the beneficial effects of psychoeducational interventions, these interventions are easy to implement and less expensive.14 Thus, making psychoeducational interventions suitable for pregnant women and their partners in LMICs. Therefore, this review aimed to identify, analyze, and synthesize the components and determine the effectiveness of psychoeducational interventions that are used for managing psychological issues and enhancing birth preparedness among primigravid women or couples in LMICs.
Methodology
We conducted a systematic review to identify psychoeducational interventions and the designs of the intervention used to address psychological needs and improve birth preparedness of first-time mothers in LMICs. The methodology of this review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines.22 We searched 11 databases (APA PsycINFO, EmCare, Embase, MEDLINE(R), Ovid Nursing, British Nursing Index, Health & Medical Collection, ProQuest, CINAHL, Cochrane, Hinari, and PubMed) for studies that were published from the inception of the databases to October 1, 2021 (Table 1). The key words that were further adjusted for all databases included “low- and middle-income countries,” “LMICs,” “first-time mothers,” “first-time fathers,” “expectant couple,” “primigravida,” “psychoeducation,” “psychological education,” “client education,” “antenatal education,” “awareness program,” “pregnancy support,” “antepartum education,” and their combinations (Supplementary materials). Additional studies were identified from the references of the included studies, and there was no language and date restriction set during the search. The definition of LMICs was based on the World Banks’ data, which categorized countries based on various indicators, including human capital development (https://data.worldbank.org/country/XN).
Table 1.
Searched databases
| Platform | Serial number | Databases | Result |
|---|---|---|---|
| Ovid | 1 | APA PsycINFO (1946 to October 2021) | 65 |
| 2 | EmCare (1995 to 2021 week 40) | 322 | |
| 3 | Embase (1910 to present) | 479 | |
| 4 | MEDLINE(R) (1946 to October 01, 2021) | 242 | |
| 5 | Ovid Nursing Database (1946 to October 2021) | 204 | |
| 7 | Health & Medical Collection | 3978 | |
| ProQuest | 8 | ProQuest Dissertations & Theses A&I | 93 |
| EBSCOhost | 9 | CINAHL Complete | 158 |
| 6 | British Nursing Index | 557 | |
| Cochrane | 10 | Cochrane Trials | 339 |
| 11 | Hinari | 10 | |
| 12 | PubMed | 2211 | |
| Total | 8658 | ||
APA, American Psychological Association; S/N, serial number.
Tola. Psychoeducation, psychological, and birth preparedness. Am J Obstet Gynecol Glob Rep 2022.
The identified studies were screened first to exclude the duplicates. Next, the title and abstract were screened, followed by full-text screening. Eligible studies involved first-time mothers in LMICs, with singleton pregnancies attending antenatal clinics, aged ≥18 years, without existing mental health diagnoses, without medical or obstetrics risks, and not planning to undergo an elective CD. The studies provided psychological, educational, or a combination of psychological and educational interventions and clearly states the intervention procedure. Furthermore, the studies provided interventions during pregnancy and assessed at least 1 of the outcomes, including anxiety, depression, self-efficacy, and knowledge decision-making about the birth method before birth and/or after birth; compared an intervention group with usual care group or other forms of nonpharmacologic interventions; and were randomized controlled trials (RCTs) and nonrandomized intervention studies with 2 groups and pre- and posttest assessments.
O.A, E.O.A, T.M.A, and M.O.A assessed the quality of the included studies using the Joanna Briggs Institute critical appraisal tool.23 Where consensus could not be reached about the quality of a particular study, a fourth reviewer (Y.O.T.) was consulted.
Data analysis
The studies retrieved during the searches were screened for relevance, and data were extracted from the studies that met the eligibility criteria. Of note, 2 authors Y.O.T. and O.A performed the data extraction using the Joanna Briggs data extraction form. Information, such as the author's name, study date, location, setting, sample size, data collection instrument, intervention content, and result, were extracted (Supplementary materials). A narrative synthesis was performed to describe the study design, intervention characteristics, outcomes, instruments, and intervention effects. The effectiveness of the psychoeducation interventions was reported on the basis of the level of significance (P value) defined by each study, whereas the effect size was calculated and reported as Cohen's d or Hedges’ g value. A small effect size ranged from 0.2 to 0.49, a medium effect size ranged from 0.5 to 0.79, and a large effect size is a Cohen's d or Hedges’ g value that is ≥0.8.24,25
Results
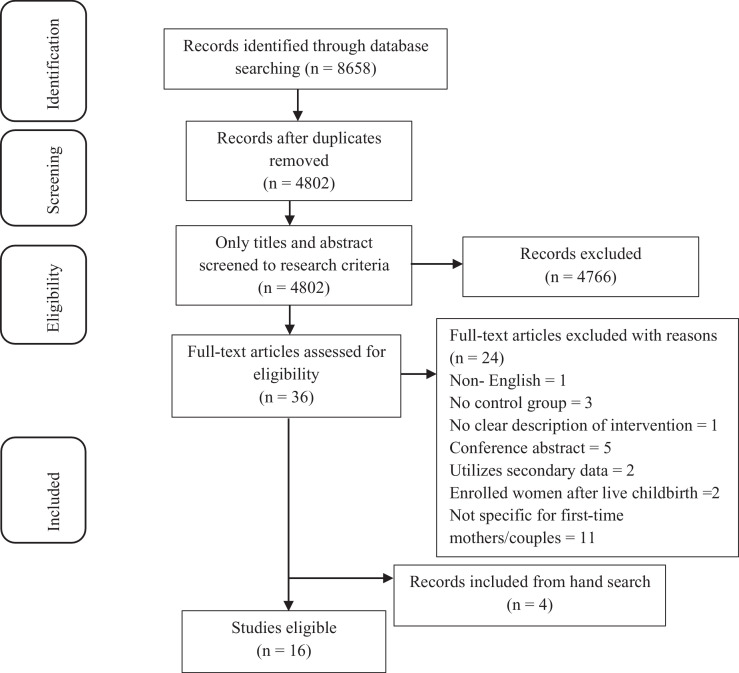
The initial search resulted in 8658 articles, which were screened for duplicates. There were 4802 articles left after duplicates were removed and 36 after titles and abstracts were screened. Of note, 12 studies were eligible for inclusion in this study after full-text screening, and 4 additional studies were identified from the reference lists of the eligible articles. Finally, 16 studies that met the inclusion criteria were included in this review (Figure). Most of the studies in this review were conducted in Iran (n=9) and Turkey (n=3). Other studies included in this review were conducted in Malawi (n=1), China (n=1), Jordan (n=1), and India (n=1). Studies included in this review were RCTs (n=7), quasi-experimental studies (n=3), clinical trials (n=3), and unspecified experimental design (n=3). Overall, the studies had low to moderate methodological quality (Tables 2 and 3).
Figure.
PRISMA flow diagram of the study
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Tola. Psychoeducation, psychological, and birth preparedness. Am J Obstet Gynecol Glob Rep 2022.
Table 2.
Methodologic quality of the included randomized controlled trials
| Questions |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 |
| Gao et al,38 2012 | Y | N | Y | N | N | N | Y | N | Y | Y | Y | Y | Y |
| Abedian et al,32 2017 | N | N | U | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Alipour et al,43 2020 | Y | N | Y | N | N | N | Y | N | Y | Y | Y | Y | Y |
| Darmian et al,34 2018 | Y | N | N | N | N | N | Y | N | Y | Y | Y | Y | Y |
| Hatamleh et al,40 2019 | Y | N | U | N | N | N | Y | N | Y | Y | Y | Y | Y |
| Kordi et al,30 2017 | Y | N | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Navaee and Abedian,35 2015 | N | N | U | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Uçar and Golbasi,26 (2019) | N | N | Y | N | N | N | Y | N | Y | Y | Y | Y | Y |
| Valiani et al,44 2014 | N | N | U | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Boz et al,29 2021 | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | Y | Y |
| Vasegh et al,39 2012 | Y | N | Y | N | N | N | N | Y | Y | Y | Y | Y | Y |
| Ghasemi et al,31 2018 | Y | N | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y |
Q1 = randomization; Q2 = participant allocation; Q3 = similarity at baseline; Q4 = participant blinding; Q5 = intervener blinding; Q6 = outcome assessor blinding; Q7 = similar treatment of the treatment group; Q8 = follow-up completion; Q9 = analysis based on assigned group; Q10 = similar assessment tool; Q11 = reliable assessment method; Q12 = appropriate statistics; and Q13 = appropriate trial design.
Y, yes; N, no; U, unclear.
Tola. Psychoeducation, psychological, and birth preparedness. Am J Obstet Gynecol Glob Rep 2022.
Table 3.
Methodologic quality of the included nonrandomized studies
| Questions |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
| Pinar et al,37 (2018) | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Munkhondya et al,27 2020 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Andaroon et al,33 2020 | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Ghasemi et al,28 2017 | Y | Y | Y | Y | Y | N | Y | Y | Y |
Q1 = variable clarity; Q2 = participant similarity; Q3 = similarity of usual care; Q4 = use of control group; Q5 = pre- and postassessment; Q6 = complete follow-up; Q7 = similar outcome assessment; Q8 = reliability of outcome assessment; and Q9 = appropriate statistics.
Y, yes; N, no.
Tola. Psychoeducation, psychological, and birth preparedness. Am J Obstet Gynecol Glob Rep 2022.
Of note, 4 of the included studies underpinned their intervention with theories. However, each of the studies used different theories. The theories included the cognitive behavioral theory,26 the Meleis transition theory,27 the theory of planned behavior,28 and the human caring theory.29 Studies included in this review recruited women carrying their first pregnancy with or without their spouses. Most of the women were recruited at approximately ≥20 weeks of gestation (n=14), and only 1 study recruited participants starting from 14 weeks of gestation.30 The total sample size in all the included studies was 1571 participants ranging from 24 to 194 participants.
Overall, the included studies assessed 39 outcomes. These outcomes can be categorized as psychological outcomes or birth preparedness outcomes, to name a few. For the psychological outcomes, fear of childbirth was assessed in 5 studies,26,27,29,31 whereas childbirth attitude was assessed in 6 studies.31, 32, 33, 34, 35 Other psychological outcomes assessed included maternal stress,36 acceptance of pregnancy, and confidence in the ability to cope with childbirth,37 anxiety,28 and depression.38 Concerning the birth preparedness outcomes, self-efficacy was assessed in 4 studies27,31,38,39; knowledge was assessed in 3 studies32,36; decision-making was assessed in 2 studies32,35; and delivery type selection,34 cervical dilation and breastfeeding initiation,40 identification of maternal role and birth concern,37 childbirth experience,36 childbirth satisfaction,26 decisional conflict,33 outcome expectancy,39 and vaginal birth preference29 were assessed in 1 study each. Other outcomes assessed included acceptance of pregnancy and satisfaction with motherhood37; spontaneous onset of labor, Apgar score, and infant birthweight40; duration of labor stage26,40; amniotomy, induction of labor, episiotomy, laceration, fetal distress, and pain26; childbirth companion support27; satisfaction38; behavioral belief, outcome evaluation, perceived behavioral control, control beliefs, perceived power, and normative belief28; and birth type.29
For the fear of childbirth outcome, the instruments used included the Wijma Delivery Expectancy/Experience Questionnaire (A and B),26,29,30 the Childbirth Attitudes Questionnaire,27 and a self-developed questionnaire.31 Childbirth attitude was assessed using the self-developed questionnaires28,32,34,35 and Childbirth Attitude Scale,33 whereas maternal stress was assessed using the maternal stress scale.36 The State-Trait Anxiety Inventory was used to assess the level of anxiety,31 whereas the Edinburgh Postnatal Depression Scale38 and the Postpartum Self-Evaluation Questionnaire37 were used to assess depression and confidence in the ability to cope with childbirth, respectively. The birth concern scale, labor observation form, prenatal self-evaluation questionnaire and knowledge evaluation form B,37 decisional conflict scale,33 self-developed birth outcome datasheet,40 and childbirth experience scale36 were used to assess birth preparedness–related outcomes.
Most of the included studies had an education component (n=13) delivered in various forms, such as training, role play, and lecture. However, other studies (n=2) used components related to counseling. The intervention was delivered face to face in small groups of approximately 4 to 10 participants. Of note, 14 studies delivered the intervention to pregnant women alone. The number of sessions varied across studies with the lowest being 1 contact session (n=3) and the highest being 6 contact sessions (n=2). Other studies delivered their intervention within 3 sessions (n=6), 2 sessions (n=20), 4 sessions (n=1), and 5 sessions (n=1). Most of the interventions were delivered once a week (n=8). Only 1 study delivered their intervention once in 2 weeks,33 although another study permitted the participants to have the intervention anytime they liked.39 Moreover, 3 studies28,29,38 did not report the frequency of their intervention delivery. The duration of the intervention delivery ranged from 20 minutes to 4 hours per session. Most of the studies employed the help of an expert to develop the intervention but were mostly delivered to the participants by the researcher.
Antenatal education intervention
Of note, 9 studies delivered their intervention using an educational method.26, 27, 28, 29,36, 37, 38, 39, 40 Some of the studies reported that antenatal education has a significant effect on psychological outcomes, such as attitude (P<.001; Hedges’ g=0.91),28 fear of childbirth (P<.05; Cohen's d=−1.018 to 4.339),26,27,29 and depression (P<.01; Hedges g: T1=0.538 and T2=−0.312).38 Moreover, antenatal education was effective for some birth preparedness outcomes, including birth concern (P<.01; Hedges’ g=−1.018),37 cervical dilation (P=.03; Cohen's d=0.392), breastfeeding initiation (P=.03; Cohen's d=−0.881),40 knowledge (P=.001; Cohen's d=2.766),36 and childbirth satisfaction (P=0.33; Hedges’ g=−1.201).26 The significant effect of antenatal education on self-efficacy and efficacy has low to very large effect sizes across the studies that assessed self-efficacy and efficacy,27,28,38,39 and the effects of antenatal education on outcome expectancy (P<.01; Cohens d=10.987) was large.39
In addition, antenatal education was reported to significantly influence vaginal birth preference (P=.12).29 Similarly, antenatal education resulted in a statistically significant effect on other outcomes, including acceptance of pregnancy,37 spontaneous onset of labor (P=.02),40 duration of stage II labor and pain (P=.033; Hedges’ g=−0.469), satisfaction (P=.001; Hedges’ g=0.626),26 childbirth companion support (P=.001; Cohen's d=2.440),27 social support (P<.01; Hedges’ g: T1=0.760 and T2=0.334)38 and behavioral belief (P<.001; Hedges’ g=0.99), perceived control (P<.001; Hedges g=0.54), outcome evaluation (P<.001; Hedges’ g=0.62), and control beliefs (P<.001; Hedges’ g=0.45).28
Antenatal training
Of note, 2 studies that used antenatal training reported a significant effect on the psychological outcomes assessed. Antenatal training resulted in a statistically significant difference with a medium effect size (P=.007; Hedges’ g=0.450) on the fear of childbirth30 and childbirth attitude toward CD and normal vaginal delivery (NVD).34 The effect size of the intervention in the study of Darmian et al34 was calculated on the basis of 3 groups, and it was found that antenatal training between the optimism training group and the control group and between the NVD training group and the control group had medium effect size, respectively, on childbirth attitude toward CD (P=.002; Hedges’ g=−0.789) and NVD (P<.001; Cohen's d=−0.787). Moreover, antenatal training between the optimism training group and control group and between the NVD training group and the control group had a large effect size (Hedges’ g=−2.055 and Cohen's d=−2.255, respectively) on childbirth attitude toward NVD.34 However antenatal training (optimism training and NVD training) was not significantly effective (P>.05) for the birth preparedness outcome related to delivery type selection (Table 4).34
Table 4.
Comparison of the effectiveness of the psychoeducational interventions
| Mode of intervention | Psychological outcomes | P value; effect size (Cohen's d or Hedges’ g) | Birth preparedness outcomes | P value; effect size (Cohen's d or Hedges’ g) | Other outcomes | P value; effect size (Cohen's d or Hedges’ g) |
|---|---|---|---|---|---|---|
| Antenatal education | Attitude | P<.001; Hedges’ g=0.91 (Ghasemi et al,28 2017) | Birth concern | P<.01; Hedges’ g=−1.018 (Pinar et al,37 2018) | Acceptance of pregnancy | P=.041; Hedges’ g =0.351 (Pinar et al,37 2018) |
| Fear of childbirth |
P<.001; Hedges’ g=−1.018 (Uçar and Golbasi,26 2019) Antenatal: P<.05; Cohen's d=−1.159 Postnatal: P<.001; Cohen's d=−1.808 (Bolz et al, 2020) P=.001; Cohen's d=−4.339 (Munkhondya et al,27 2020) |
Cervical dilation | P=.03; Cohen's d=0.392 (Hatamleh et al, 2019) | Duration of stage 2 labor | P=.033; Hedges’ g=−0.469 (Uçar and Golbasi,26 2019) | |
| Depression | T1: P<.01; Hedges’ g=−0.536 T2: P<.01; Hedges’ g=−0.342 (Gao et al,38 2012) |
Breastfeeding initiation | P>.01; Cohen's d=−0.881 (Hatamleh et al, 2019) | Pain | P<.001; Hedges g=−1.201 (Uçar and Golbasi,26 2019) | |
| None | Knowledge | P<.01; Hedges’ g=2.766 (Nair et al,36 2015) | Childbirth companion or social support |
P=.001; Cohen's d=−2.440 (Munkhondya et al,27 2020) T1: P<.01; Hedges’ g=0.760) T2: P<.01; Hedges’ g=0.334 (Gao et al,38 2012) |
||
| Self-efficacy |
P=001; Cohen's d=−4.136 (Munkhondya et al,27 2020) T1: P<.01; Hedges’ g=0.574) T2: P<.01; Hedges’ g=0.347 (Gao et al,38 2012) P=.01; Cohen's d=12.680 (Vasegh et al,39 2012) P<.001; Cohen's d=3.207 and 2.081 (Ghasemi et al,28 2017) |
Satisfaction | P=.033; Hedges’ g=−0.626 (Uçar and Golbasi,26 2019) | |||
|
None |
Behavioral belief | P<.001; Hedges g=0.99 (Ghasemi et al,28 2017) | ||||
| Perceived control | P<.001; Hedges g=0.54 (Ghasemi et al,28 2017) | |||||
| Outcome evaluation | P<.001; Hedges g=0.62 (Ghasemi et al,28 2017) | |||||
| Outcome expectancy | P=.01; Cohen's d=10.987 (Vasegh et al,39 2012) | |||||
| Control beliefs | P<.001; Hedges g=0.45 (Ghasemi et al,28 2017) | |||||
| Antenatal training | Fear of childbirth | P=.007; Hedges’ g=−0.450 (Kordi et al,30 2017) | None | |||
| Childbirth attitude toward CD and NVD | CD: P=.002a; Hedges’ g=−0.789b and Cohen's d=0.787c NVD: P<.001a; Hedges’ g=−2.055b; Cohen's d=−2.255c (Darmian et al,34 2018) |
|||||
| Role play | Childbirth attitude | P=.003; Hedges’ g=0.537 (Abedian et al,32 2017) | ||||
| Fear of childbirth | P=.007; Hedges’ g=0.677 (Navaee and Abedian,35 2015) | |||||
| Counseling | Fear of childbirth | P<.001; Cohen's d=−3.762 and −2.316 | Decisional conflict | P<.001; Cohen's d=−0.742 | Expected outcomes | P<.001; Cohen's d=2.608 and 2.359 |
| Anxiety | P<.001; Cohen's d=−2.304 and −1.687 | |||||
| Childbirth attitude | P<.00; Cohen's d=0.978 (Andaroon et al,33 2020) | None | ||||
CD, cesarean delivery; NVD, normal vaginal delivery.
aP value among 3 groups.
bEffect size of optimism training vs control group.
cEffect size of NVD training vs control group.
Tola. Psychoeducation, psychological, and birth preparedness. Am J Obstet Gynecol Glob Rep 2022.
Role play
Of note, 2 studies delivered their intervention using role play and usual antenatal lecture for the intervention group and control group, respectively.32,35 Role play resulted in a statistically significant difference with medium effect size in psychological outcomes, such as childbirth attitude (P=.003; Hedges’ g=0.537)32 and fear of childbirth (P=.007; Hedges’ g=0.677).35 However, there was no statistically significant difference in birth preparedness outcomes related to delivery method decision-making.32
Counseling
Of note, 2 studies delivered their intervention through antenatal counseling. Antenatal counseling resulted in a statistically significant effect on psychological outcomes (P<. 001) and birth preparedness outcomes (P<.01). The psychological outcomes included fear of childbirth and anxiety31 and childbirth attitude.33 However, the birth preparedness outcomes included decisional conflict,33 self-efficacy, and expected outcome.31
Fear, anxiety, self-efficacy, and expected outcome were assessed immediately after the intervention and in the last month of pregnancy in the study of Ghasemi et al,31 and antenatal counseling resulted in a large effect size (Cohen's d) both immediately after the intervention (fear of childbirth, −3.762; anxiety, −2.304; self-efficacy, 3.207; expected outcome, 2.608) and in the last month of pregnancy (fear of childbirth, −2.316; anxiety, −1.687; self-efficacy, 2.081; expected outcome, 2.359), respectively. Similarly, antenatal counseling also resulted in a large and medium effect size for childbirth attitude and decisional conflict (Cohen's d=0.978 and 0.742), respectively.33 The summary of the effects of the intervention is presented in Table 4.
Discussion
This systematic review narratively analyzed and synthesized relevant evidence on psychoeducational interventions used for addressing psychological issues and promoting birth preparedness among first-time mothers in LMICs. Of note, 16 studies were included in this review, including 7 RCTs, 3 quasi-experimental studies, and 6 nonrandomized experimental studies. The studies were conducted in 5 LMICs, such as Iran, Turkey, Malawi, Jordan, and India. The included studies were riddled with several methodological issues. For the RCT studies, only 1 study blinded the participants and conducted allocation of concealment. None of the studies performed outcome assessor blinding. None of the studies was conducted with the intention-to-treat principle during the data analysis. In RCTs studies, bias can be minimized through allocation concealment, participant and assessor blinding, and analysis of all recruited participants into the group in which they were recruited whether they dropped out or not.41 Most of the included studies did not use any theory to underpin their intervention. However, the few studies that used theories used different types of theories, such as the Meleis transition theory, cognitive behavioral theory, theory of planned behavior, and human caring theory. It remains unclear whether the outcomes assessed in these studies26, 27, 28, 29 were derivatives of the theory that underpinned their intervention.
The interventions in the included studies were delivered through antenatal education,26, 27, 28, 29,36, 37, 38, 39, 40 counseling,31,33 and role play.32,35 The outcomes assessed included psychological outcomes, birth preparedness outcomes, and other outcomes. This review revealed that although some studies assessed similar outcomes, most of the similar outcomes were not assessed with the same tools. Most of the tools used were developed by the researchers for that study. This implies that the validity and reliability of the instruments were not well established; hence, it cannot be concluded that the outcomes were assessed in a reliable way for most studies. This is a major challenge with studies conducted in developing countries as some researchers and students lack the skills and knowledge about validity and reliability testing.42
All psychoeducational intervention modes, such as antenatal education, antenatal counseling, antenatal training, and role play, had a significant effect on some of the psychological outcomes assessed, including childbirth attitude, fear of childbirth, depression, fear, and anxiety. These findings further reiterate that psychoeducational interventions provided during the antenatal period can be quite effective for controlling psychological issues in pregnant women and postpartum women.14 Hence, the findings of this review about psychoeducation interventions in this review were consistent with the findings of a previous systematic review conducted by Park et al.19 Similarly, all psychoeducational intervention modes were effective for improving birth preparedness outcomes, including birth concern, cervical dilation, breastfeeding initiation, knowledge, self-efficacy, and decisional conflict. Moreover, this finding held for other outcomes, such as acceptance of pregnancy, duration of stage 2 of labor, pain, childbirth companion support of social support, satisfaction, behavioral belief, perceived control, outcome evaluation and expectancy, and control beliefs. The findings from this review revealed that depending on the intervention mode, the effect sizes for each outcome ranged from small to large effect size.
Despite the effectiveness of the psychological interventions on most psychological, birth preparedness, and other outcomes assessed in the included studies, this review revealed that psychoeducational intervention was not effective in managing some outcomes, including the mother's confidence to cope with motherhood; satisfaction with motherhood and infant care; identification with a motherhood role37; birth information, such as anxiety during active labor, duration of stage 1 and 2 labor, fetal distress, episiotomy, induction of labor, laceration, and amniotomy26,27; Apgar score at 1 and 5 minutes; gestational age at delivery; length of the first and second stage of labor, and infant birthweight.40 Others included childbirth experience, maternal stress,36 normative belief, perceived power and perceived behavioral control,28 birth preference,29 decision-making about the type of delivery, and mode of delivery.32,34,35 This nonsignificant effect of psychoeducational intervention on these outcomes could be because several of these outcomes are influenced by several physiological, environmental, and cultural factors.
Overall, the findings from this review have indicated that in LMICs, psychoeducational interventions have been used to address several psychological issues and enhance birth preparedness among first-time mothers; and it was found to be significantly effective. This review was not without limitations, one of which was the inability of included studies to be used in a meta-analysis because of the differences in the design of the study and data collection instrument. Another limitation was the inclusion of studies that focused on women who did not have existing mental health diagnoses. Therefore, because of the methodological quality and different instruments used in the included studies and the exclusion of studies that included only women who did not have existing mental health diagnoses, caution needs to be taken when interpreting and using the findings of this review.
Research implication
The first research implication is the need for standardized data collection tools for measuring outcomes in future studies. The second research implication is that future research needs to use a robust methodology, such as RCTs, and involve spouses of first-time mothers in their research.
Strengths and limitations
The strength of this review lies in the utilisation of previously tested critical appraisal tools as well as the pooling of evidence through rigorous search of data from all the low - and middle - income countries as defined by the world bank. Nevertheless, the study is not without limitation. Due to the diverse research methodologies and data collection instruments, the data from the included articles could not be pooled into a meta-analysis.
Clinical implications
This review has some clinical implications. First, although psychoeducation has proven useful, hospitals and healthcare facilities in LMICs attending to pregnant women, especially first-time mothers and their partners, need to incorporate the various methods of psychoeducation (education, role play, counseling, and training) to manage psychological issues and enhance birth preparedness. Second, nursing leaders and policymakers in LMICs need to develop policies that can enhance the implementation of focused psychological care and birth preparedness for first-time mothers and their partners.
Conclusion
Primigravid women or first-time mothers and their partners face several psychological issues during pregnancy and immediately after the birth of their baby because of their need to adjust to the physiological changes in the body and parenthood. However, engaging primigravid and their partners through psychoeducation is effective for addressing psychological issues, and no doubt, it could enhance birth preparedness. Psychoeducation is an intervention that is less expensive for pregnant individuals and their spouses from LMICs compared with high-income countries where pregnant individuals and their spouses may be able to afford private birthing sessions or employ the services of a personal midwife. Therefore, there is a need for this intervention to be used routinely in LMICs for first-time mothers and their partners.
Footnotes
The authors report no conflict of interest.
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
This study did not receive a grant from any grant-awarding agency or institution.
Cite this article as: Tola YO, Akingbade O, Akinwaare MO, et al. Psychoeducation for psychological issues and birth preparedness in low- and middle-income countries: a systematic review. Am J Obstet Gynecol Glob Rep 2022;2:100072.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xagr.2022. 100072.
Appendix. Supplementary materials
References
- 1.Røsand GM, Slinning K, Eberhard-Gran M, Røysamb E, Tambs K. Partner relationship satisfaction and maternal emotional distress in early pregnancy. BMC Public Health. 2011;11:161. doi: 10.1186/1471-2458-11-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gourounti K, Anagnostopoulos F, Sandall J. Poor marital support associate with anxiety and worries during pregnancy in Greek pregnant women. Midwifery. 2014;30:628–635. doi: 10.1016/j.midw.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Figueiredo B, Conde A. Anxiety and depression symptoms in women and men from early pregnancy to 3-months postpartum: parity differences and effects. J Affect Disord. 2011;132:146–157. doi: 10.1016/j.jad.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Dareshouri MZ, Bosaknejad S, Sarvghad S. A survey on the effectiveness of stress management training with cognitive-behavioral group therapy approach on state/trait anxiety, pregnancy anxiety and mental health of primiparous women. Jentashapir J Cell Mol Biol. 2012;3:e94054. [Google Scholar]
- 5.Akbarzadeh M, Toosi M, Zare N, Sharif F. Effect of learning attachment behaviors on anxiety and maternal fetal attachment in first pregnant women. Evid Base Care J. 2011;1:21–34. [Google Scholar]
- 6.Bjelica A, Kapor-Stanulović N. [Pregnancy as a psychological event] Med Pregl. 2004;57:144–148. doi: 10.2298/mpns0404144b. [DOI] [PubMed] [Google Scholar]
- 7.Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28:25–35. doi: 10.1016/j.bpobgyn.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 8.Farias DR, Pinto Tde J, Teofilo MM, et al. Prevalence of psychiatric disorders in the first trimester of pregnancy and factors associated with current suicide risk. Psychiatry Res. 2013;210:962–968. doi: 10.1016/j.psychres.2013.08.053. [DOI] [PubMed] [Google Scholar]
- 9.Roos A, Faure S, Lochner C, Vythilingum B, Stein DJ. Predictors of distress and anxiety during pregnancy. Afr J Psychiatry (Johannesbg) 2013;16:118–122. doi: 10.4314/ajpsy.v16i2.15. [DOI] [PubMed] [Google Scholar]
- 10.Vythilingum B. Anxiety disorders in pregnancy. Curr Psychiatry Rep. 2008;10:331–335. doi: 10.1007/s11920-008-0053-y. [DOI] [PubMed] [Google Scholar]
- 11.Camoirano A. Mentalizing makes parenting work: a review about parental reflective functioning and clinical interventions to improve it. Front Psychol. 2017;8:14. doi: 10.3389/fpsyg.2017.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malata A, Chirwa E. Childbirth information needs for first time Malawian mothers who attended antenatal clinics. Malawi Med J. 2011;23:43–47. doi: 10.4314/mmj.v23i2.70747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donker T, Griffiths KM, Cuijpers P, Christensen H. Psychoeducation for depression, anxiety and psychological distress: a meta-analysis. BMC Med. 2009;7:1–9. doi: 10.1186/1741-7015-7-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Missler M, van Straten A, Denissen J, Donker T, Beijers R. Effectiveness of a psycho-educational intervention for expecting parents to prevent postpartum parenting stress, depression and anxiety: a randomized controlled trial. BMC Pregnancy Childbirth. 2020;20:658. doi: 10.1186/s12884-020-03341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell V. Research overview: self-efficacy-a key construct for antenatal education. Perspective. 2014;24:17–20. [Google Scholar]
- 16.Schwartz L, Toohill J, Creedy DK, Baird K, Gamble J, Fenwick J. Factors associated with childbirth self-efficacy in Australian childbearing women. BMC Pregnancy Childbirth. 2015;15:1–9. doi: 10.1186/s12884-015-0465-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Serçekuş P, Mete S. Effects of antenatal education on maternal prenatal and postpartum adaptation. J Adv Nurs. 2010;66:999–1010. doi: 10.1111/j.1365-2648.2009.05253.x. [DOI] [PubMed] [Google Scholar]
- 18.Soubeiga D, Gauvin L, Hatem MA, Johri M. Birth Preparedness and Complication Readiness (BPCR) interventions to reduce maternal and neonatal mortality in developing countries: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2014;14:1–11. doi: 10.1186/1471-2393-14-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park S, Kim J, Oh J, Ahn S. Effects of psychoeducation on the mental health and relationships of pregnant couples: a systemic review and meta-analysis. Int J Nurs Stud. 2020;104 doi: 10.1016/j.ijnurstu.2019.103439. [DOI] [PubMed] [Google Scholar]
- 20.Hutton EK, Hall W. Psychoeducation for pregnant women with fear of childbirth increases rates of spontaneous vaginal delivery, reduces caesarean rates and improves delivery experience. Evid Based Nurs. 2014;17:105. doi: 10.1136/eb-2013-101284. [DOI] [PubMed] [Google Scholar]
- 21.Ryding EL, Persson A, Onell C, Kvist L. An evaluation of midwives’ counseling of pregnant women in fear of childbirth. Acta Obstet Gynecol Scand. 2003;82:10–17. doi: 10.1034/j.1600-0412.2003.820102.x. [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG, Group PRISMA. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 23.Briggs J. The Joanna Briggs institute; 2017. Checklist for systematic reviews and research syntheses.https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Systematic_Reviews2017_0.pdf Available at. [Google Scholar]
- 24.Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun Stat Simul Comput. 2010;39:860–864. [Google Scholar]
- 25.Tola YO, Chow KM, Liang W. Effects of non-pharmacological interventions on preoperative anxiety and postoperative pain in patients undergoing breast cancer surgery: a systematic review. J Clin Nurs. 2021;30:3369–3384. doi: 10.1111/jocn.15827. [DOI] [PubMed] [Google Scholar]
- 26.Uçar T, Golbasi Z. Effect of an educational program based on cognitive behavioral techniques on fear of childbirth and the birth process. J Psychosom Obstet Gynaecol. 2019;40:146–155. doi: 10.1080/0167482X.2018.1453800. [DOI] [PubMed] [Google Scholar]
- 27.Munkhondya BMJ, Munkhondya TE, Chirwa E, Wang H. Efficacy of companion-integrated childbirth preparation for childbirth fear, self-efficacy, and maternal support in primigravid women in Malawi. BMC Pregnancy Childbirth. 2020;20:48. doi: 10.1186/s12884-019-2717-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghasemi S, Nazari M, Vafaei H, Fararouei M. The impact of educational intervention based on the theory of planned behavior in choosing delivery mode in primigravida pregnant women. Int J Women's Health Reprod Sci. 2017;5:47–54. [Google Scholar]
- 29.Boz İ, Akgün M, Duman F. A feasibility study of a psychoeducation intervention based on Human Caring Theory in nulliparous women with fear of childbirth. J Psychosom Obstet Gynaecol. 2021;42:300–312. doi: 10.1080/0167482X.2020.1752173. [DOI] [PubMed] [Google Scholar]
- 30.Kordi M, Bakhshi M, Masoudi S, Esmaily H. Effect of a childbirth psychoeducation program on the level of fear of childbirth in primigravid women. Evid Based Care J. 2017;7:26–34. [Google Scholar]
- 31.Ghasemi F, Bolbol-Haghighi N, Mottaghi Z, Hosseini SR, Khosravi A. The effect of group counseling with cognitive-behavioral approach on self-efficacy of pregnant women's choice of vaginal delivery. Iran J Psychiatry Behav Sci. 2018;12:e7632. [Google Scholar]
- 32.Abedian Z, Navaee M, Sani HJ, Ebrahimzadeh S. Comparing two instructional methods of role playing and lecture on primigravida females, decision about type of delivery. J Educ Health Promot. 2017;6:29. doi: 10.4103/jehp.jehp_85_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andaroon N, Kordi M, Kimiaee SA, Esmaeili H. The effect of individual counseling on attitudes and decisional conflict in the choice of delivery among nulliparous women. J Educ Health Promot. 2020;9:35. doi: 10.4103/jehp.jehp_472_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Darmian ME, Yousefzadeh S, Najafi TF, Javadi SV. Comparative study of teaching natural delivery benefits and optimism training on mothers’ attitude and intention to select a type of delivery: an educational experiment. Electron Physician. 2018;10:7038–7045. doi: 10.19082/7038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Navaee M, Abedian Z. Effect of role play education on primiparous women's fear of natural delivery and their decision on the mode of delivery. Iran J Nurs Midwifery Res. 2015;20:40–46. [PMC free article] [PubMed] [Google Scholar]
- 36.Nair DG, Fernandes SJ, Roach EJ. Effectiveness of video assisted childbirth preparation on knowledge, childbirth experience and stress. Int J Nurs Educ. 2015;7:229–234. [Google Scholar]
- 37.Pinar G, Avsar F, Aslantekin F. Evaluation of the impact of childbirth education classes in Turkey on adaptation to pregnancy process, concerns about birth, rate of vaginal birth, and adaptation to maternity: a case-control study. Clin Nurs Res. 2018;27:315–342. doi: 10.1177/1054773816682331. [DOI] [PubMed] [Google Scholar]
- 38.Gao LL, Chan SW, Sun K. Effects of an interpersonal-psychotherapy-oriented childbirth education programme for Chinese first-time childbearing women at 3-month follow up: randomised controlled trial. Int J Nurs Stud. 2012;49:274–281. doi: 10.1016/j.ijnurstu.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 39.Vasegh Rahimparvar SF, Hamzehkhani M, Geranmayeh M, Rahimi R. Effect of educational software on self-efficacy of pregnant women to cope with labor: a randomized controlled trial. Arch Gynecol Obstet. 2012;286:63–70. doi: 10.1007/s00404-012-2243-4. [DOI] [PubMed] [Google Scholar]
- 40.Hatamleh R, Abujilban S, AbuAbed ASA, Abuhammad S. The effects of a childbirth preparation course on birth outcomes among nulliparous Jordanian women. Midwifery. 2019;72:23–29. doi: 10.1016/j.midw.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 41.Polit DF, Beck CT. Lippincott Williams & Wilkins; Philadelphia, PA: 2008. Nursing research: generating and assessing evidence for nursing practice. [Google Scholar]
- 42.Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22:195–201. doi: 10.4103/1117-1936.173959. [DOI] [PubMed] [Google Scholar]
- 43.Alipour Z., Kazemi A., Kheirabadi G., et al. Marital communication skills training to promote marital satisfaction and psychological health during pregnancy: a couple focused approach. Reprod Health. 2020;17:23. doi: 10.1186/s12978-020-0877-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Valiani M, Haghighatdana Z, Ehsanpour S. Comparison of childbirth training workshop effects on knowledge, attitude, and delivery method between mothers and couples groups referring to Isfahan health centers in Iran. Iran J Nurs Midwifery Res. 2014;19(6):653–8. PMID: 25558265; PMCID: PMC4280732. [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.