Abstract
BACKGROUND
The World Health Organization Labor Care Guide was introduced in December 2020 to implement World Health Organization (WHO) guidelines on intrapartum care for a positive childbirth experience.
OBJECTIVE
This study aimed to determine the effect of the WHO Labor Care Guide on labor outcomes, especially in reducing primary cesarean deliveries, and its acceptability by healthcare providers.
STUDY DESIGN
This open-label randomized control trial was conducted from September 2021 to December 2021 on 280 low-risk antenatal women admitted for delivery at a busy tertiary care institute in North India. After informed consent, women were allocated into the study and control groups. Labor monitoring was performed using the WHO Labor Care Guide in the study group and the World Health Organization–modified partograph in the control group. Women who had a cesarean delivery in the latent phase of labor were excluded from the study. The primary outcome was mode of delivery, whereas the secondary outcomes were duration of active labor, maternal complications (postpartum hemorrhage and puerperal sepsis), duration of hospital stay, Apgar score at 5 minutes, and neonatal intensive care unit admission. The labor outcomes in both groups were compared. In the study group, the acceptability, difficulty, and satisfaction levels of the users were assessed using a 5-point Likert scale. The “learning curve” for the use of the Labor Care Guide (LCG) was determined. SPSS software (version 21.0; IBM Corporation, Chicago, IL) was used for statistical analysis.
RESULTS
After excluding women who underwent cesarean delivery in the latent phase, 136 women in the study group and 135 women in the control group were observed for labor outcomes. The cesarean delivery rate was 1.5% in the study group vs 17.8% in the control group (P=.0001). The duration of the active phase of labor was significantly shorter in the study group than in the control group (P<.001). The 2 groups were similar in terms of maternal complications, duration of hospital stay, and Apgar score. The learning curve took average levels of 6.50 and 2.25 Labor Care Guide plots to shift from “very difficult” to “neutral” and “neutral” to “easy,” respectively. After an initial learning curve, acceptability and satisfaction levels were found to be high in the WHO Labor Care Guide users.
CONCLUSION
The WHO Labor Care Guide is a simple labor monitoring tool for the reducing primary cesarean delivery rate without increasing the duration of hospital stay and fetomaternal complications.
Key words: duration of labor, Labor Care Guide, labor monitoring, reducing primary cesarean delivery rate, World Health Organization–modified partograph
AJOG Global Reports at a Glance.
Why was this study conducted?
This study aimed to determine the effect of the World Health Organization (WHO)-released Labor Care Guide (LCG), the next-generation partograph, on the primary cesarean delivery (CD) rates.
Key findings
The use of the WHO LCG significantly decreased the number of primary CDs without increasing perinatal complications and the duration of hospital stay. The learning curve for the use of the LCG was small.
What does this add to what is known?
This study investigated the effect of the LCG on reducing CD rates and overall labor outcomes after the release of the WHO LCG in December 2020. An attempt was made to determine the learning curve for the use of the LCG by healthcare providers, which was quite encouraging.
Introduction
More than one-third of maternal deaths, half of stillbirths, and approximately a quarter of neonatal deaths result from delivery complications.1,2 Most of these deaths occur in low-resource settings and are mostly preventable through well-timed interventions.3 Optimum labor monitoring and early recognition and management of complications are crucial for improving these health indicators.
Rapidly soaring global CS rates without clear evidence of positive impact on maternal or neonatal morbidity or mortality has raised significant concern about CS overuse.4 WHO has stressed upon making CS available to women in need, rather than aiming to achieve specific goal.5 US CS rate has risen from 20.7 to 32% over last three decades. Primary C-sections were major contributors. Even in India, primary CS contributes to as high as 47.5% of total cesarean burden.6 For effective prevention of primary CS, it's important to work on modifiable indications, of which labor dystocia is very important.
In 2014, the American College of Obstetricians and Gynecologists (ACOG) redefined labor phases in an evidence-based manner to reduce primary cesarean delivery (CD) rates.7 It was emphasized to have the patience to allow normal progress of labor in the light of recent evidence that labor takes longer than previously thought.8 It was realized that a cervical dilatation rate slower than 1 cm/hour was poor in predicting adverse labor outcomes and must not be an indication for obstetrical interventions.9 The various phases of labor were redefined along with newer recommendations for their implementation during labor monitoring.10, 11, 12 For effective application of these new definitions and recommendations, the World Health Organization (WHO) introduced the WHO Labor Care Guide (LCG), the next-generation partograph, in December 2020. The new highlights of the LCG were respectful and supportive maternal care by documentation of numeric figures for parameters being monitored and precise threshold limits to trigger intervention after maternofetal assessment.
Any deviation in established medical practices is bound to be associated with anxiety, apprehension, and, at times, even antagonism among the healthcare providers (HCPs). The current study was designed to determine the effect of the LCG for labor monitoring on reducing CD rates and overall maternofetal outcomes by comparing it with the existing WHO-modified partograph and to determine the HCPs’ feedback on the difficulty, acceptability, and satisfaction levels of the LCG.
Methodology
This was an open-label randomized controlled study conducted on 280 low-risk pregnant women admitted in labor in the labor room (LR) of a tertiary care center. Previous approval of the institutional ethical committee was taken. Enrollment was done at the time of admission as per inclusion and exclusion criteria and after informed consent. Antenatal women with term gestation between 37 and 40 weeks of gestation and women with a cephalic presentation in spontaneous labor were included in the study. Women with any medical comorbidities, such as hypertension, diabetes mellitus, renal disease, or pulmonary disease, or presence of any obstetrical complications, such as preterm birth, multiple gestation, previous CD, breech position, postdated pregnancy, or bad obstetrical history (any previous outcome that can adversely affect the current pregnancy outcome), and those who were given intrapartum epidural analgesia were excluded from the study. The women who did not require any medical or surgical method of induction for initiation of labor were said to be in “spontaneous labor.”
The sample size was determined by taking the CD rate of 7.1% in patients managed using the LCG as observed by Vogel et al15 for a superiority trial and assuming a difference of 15% in CD rate between modified partograph and LCG. The minimum required sample size with 95% power of study and 5% level of significance was calculated as 138 patients in each study group. The formula used was n≥([pc × (1−pc)+pe × (1−pe)] × [Zα+Zβ]2)/pc-pe)2 where pc is the CD rate in patients managed using the LCG, pe is the CD rate in patients managed using the WHO-modified partograph, Zα is the value of Z at a 2-sided alpha error of 5%, and Zβ is the value of Z at the power of 95%. To reduce the margin of error, the total sample size taken was 280 (140 patients per group).
After informed consent, randomization and allocation to study and control groups were conducted using a computer-generated sequence, and enrollment continued until the desired sample size of 280 was reached. Those who underwent CD in the latent phase were excluded from the study.
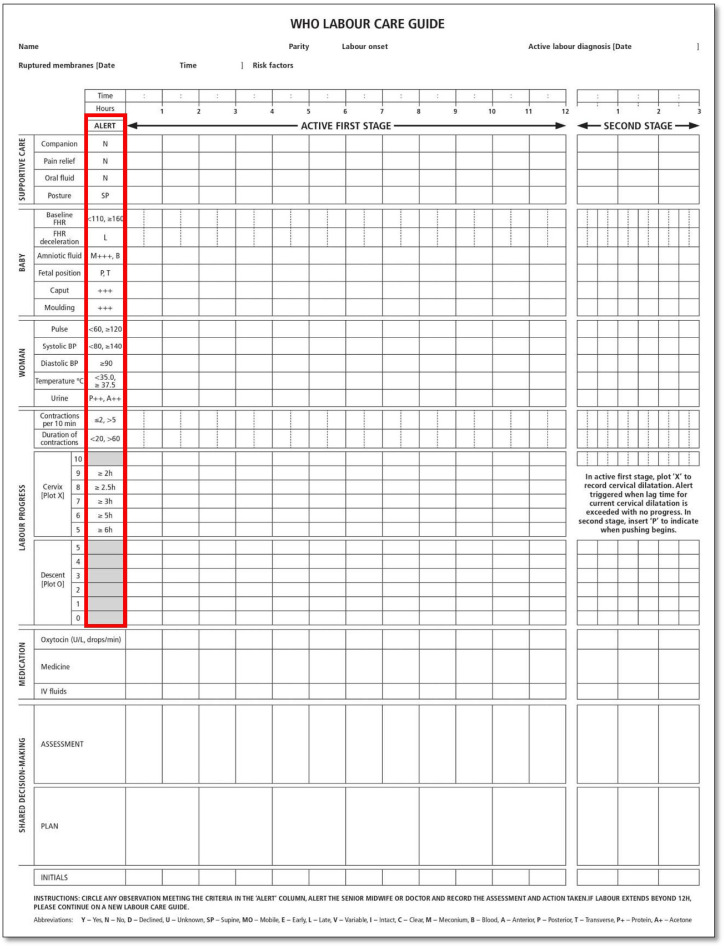
The labor progress was monitored, following the WHO LCG (2020) in the study group (Figure 2; Appendix 1) and the WHO-modified partograph (2000) in the control group (Figure 3: Appendix 2). Before application of the LCG, the concerned LR team (3 resident doctors and 2 nursing officers) underwent 1-day training for LCG usage. The investigators did this, every month just before the start of the LR posting of residents. Each month, a new LR team was posted over the study period. Moreover, they ensured the complete and correct entry of each LCG plot. The LR team was free to contact the investigators for any support whenever required (24 × 7).
Figure 2.
Appendix 1 : WHO Labor Care Guide, the next generation partograph. Red column highlights the alert parameters for each observation. Alert parameters include: Supportive Care [No Companion (N), No Pain relief (N), No oral fluid intake (N), Supine posture (S)]; Foetal parameters [(FHS≤110/≥150, Late deceleartions (L), Meconium stained liquor (M+++), Blood stained liquor (B), posterior (P)/ Transverse (T) position, Caput (+++), Moulding (+++)]; Maternal parameters [PR<60/≥120, Systolic BP<80/≥140, Diastolic BP≥90, Temperature <35/≥37.5 °C, Urine proteins/acetones (++)]; Labour Progress [uterine contractions (≤2/>5), duration of contractions (<20/>60 seconds). Alert time threshold in hours (h) for each cervical dialataion are as follows: 5cm≥6h,6≥5h,7cm≥3h,8cm≥2.5h,9h≥2h.
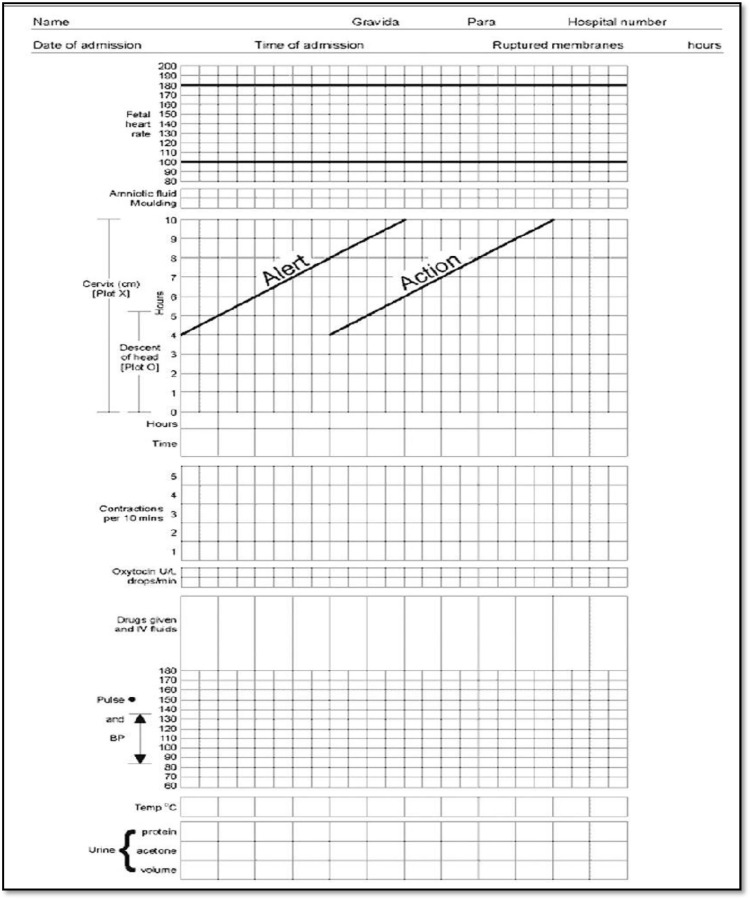
Figure 3.
Appendix 2 : WHO Modified partograph
In the study group, the active phase of labor started with a 5-cm cervical dilatation. Maternofetal monitoring was performed following the parameters described in the LCG. The alert parameters were highlighted, and a corresponding intervention or response was recorded (Appendix 1: red column).13 Oxytocin was started when uterine contractions tallied with that defined under an “alert parameter” in the LCG. For each centimeter of cervical dilatation, a lag time has been mentioned (eg, 5 cm [≥6.0 hours], 6 cm [≥5.0 hours], 7 cm [≥3.0 hours], 8 cm [≥2.5 hours], and 9 cm [≥2 hours]). The alert was triggered if lag time at a particular dilatation exceeded with no progress. The LCG is based on “action-oriented labor,” which follows the “assess-record-check-plan approach” (ie, the parameters are assessed, recorded in the LCG, and checked against the “alert thresholds” for each parameter, and further management plan is decided accordingly) (Appendix 1). In the control group, the active labor started from a cervical dilatation of 4 cm. Deviation of labor progress to the right of the alert or action lines indicated reevaluation or intervention.14 Oxytocin was started when contractions were not adequate and the labor graph was on the right of the alert line.
Each partograph was analyzed for its role in influencing decision-making in labor management. In the study group, protracted or arrest of labor was defined as cervical dilatation of ≥5 cm with ruptured membranes with slow or no cervical change despite adequate contractions or ≥6 hours of maximum dose of oxytocin administration in the absence of adequate contractions respectively. In the control group, protracted or arrest of labor was defined as slow or no improvement in cervical dilatation or descent of the head in the active phase of labor (≥4 cm) for ≥4 hours with adequate uterine contractions or ≥6 hours with inadequate uterine contractions even after a maximum permissible dose of oxytocin. “Adequate contractions” were defined as 3 to 5 contractions in 10 minutes (frequency), each lasting 30 to 40 seconds (duration) and increasing in intensity or with progressive pain according to the perception of the parturient.
Oxytocin for augmentation was started at 1 mIU/min and escalated by 1 to 2 mIU/min every 20 to 30 minutes to a maximum dose of 32 mIU/min (as per the institutional protocol) or to a dose where adequate contractions were achieved (whichever was earlier).
The details of the parturient were noted as per the corresponding partographs. The women in both groups were followed from active labor until 6 weeks after discharge from the hospital. The hemoglobin level and total leucocyte count were taken on postnatal day 1. They were called for a postnatal checkup at the end of 6 weeks or earlier in case of any complaint. The primary outcome recorded was mode of delivery, whereas the secondary outcomes were measured in terms of the duration of the active stage of labor, intra- or postpartum labor–related complications (postpartum hemorrhage [PPH] or infection), duration of hospital stay, Apgar score at 5 minutes, neonatal intensive care unit (NICU) admission, and final neonatal outcome (ie, whether discharged in satisfactory condition or any adverse neonatal outcome). PPH was defined as excessive bleeding from the genital tract affecting the vital signs (pulse rate of ≥90 beats per minute and/or falling blood pressure and/or need for fluid resuscitation and/or blood transfusion). Infection was defined as the presence of ≥2 of the following signs within 6 weeks after delivery: fever (≥100.4°F on 2 occasions for 4 hours), pelvic pain, purulent or foul smelling vaginal discharge, or subinvolution of uterus. In addition, the HCPs involved were asked to give their feedback on the difficulty, acceptability, and satisfaction levels based on a 5-point Likert scale on the use of the WHO LGC. The 5-point Likert scale for the difficulty level was 1 for very difficult, 2 for difficult, 3 for neutral, 4 for easy, and 5 for very easy; for acceptability and satisfaction, the levels were 1 for highly acceptable, 2 for acceptable, 3 for moderately acceptable, 4 for fairly acceptable, 5 for not acceptable. In addition, the “learning curve” was analyzed in terms of shifting of difficulty level from “very difficult” to “easy.”
Statistical analysis
Categorical variables were presented in number and percentage and quantitative variables were presented as mean±standard deviation. Comparison of the quantitative variables was performed using the independent t test. The comparison of the qualitative variables was done using the chi-squared test. If any cell had an expected value of <5, then a Fisher exact test was used. The data entry was recorded in the Microsoft Excel spreadsheet, and the final analysis was performed with the use of SPSS software (version 21.0; IBM Corporation, Chicago, IL). For statistical significance, a P value of <.05 was considered statistically significant.
Results
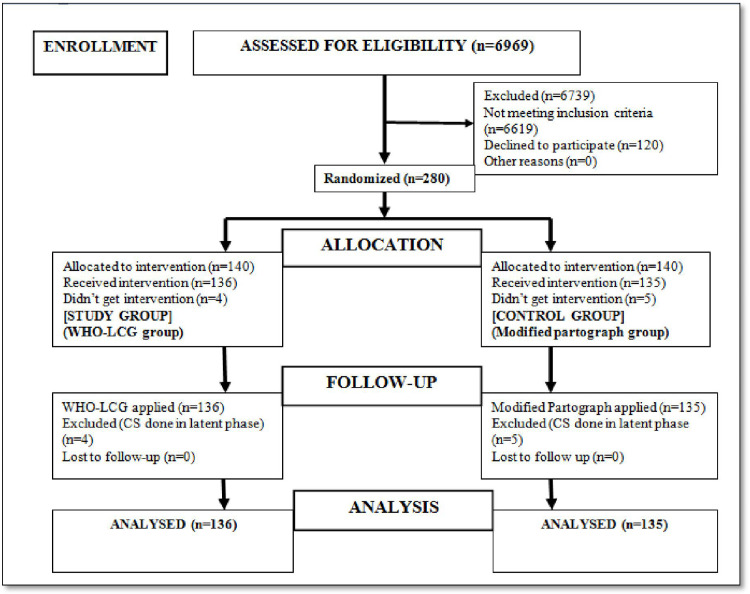
Of 6969 women screened for eligibility, final sample sizes of 136 and 135 in the study and control groups, respectively were reached in 4 months (Figure 1). The mean ages of women in the study and control groups were 25.0±3.5 and 25.1±3.6 years, respectively. The 2 groups were comparable in terms of clincodemographic characteristics (Table 1).
Figure 1.
Consort diagram for the study
WHO LCG, World Health Organization Labor Care Guide.
Pandey. Reduction of primary cesarean delivery by use of World Health Organization Labor Care Guide. Am J Obstet Gynecol Glob Rep 2022.
Table 1.
Clinical and demographic profiles of the study population
| Serial no. | Parameters | Study group (n=136) | Control group (n=135) | P value |
|---|---|---|---|---|
| 1 | Maternal age (y), mean±SD | 25.0±3.5 | 25.1±3.6 | .817a |
| 2 | Parity, n (%) | .753a | ||
| Nullipara | 60 (44.12) | 57 (42.22) | ||
| Multipara | 76 (55.88) | 78 (57.78) | ||
| 3 | Literacy status, n (%) | .193b | ||
| Illiterate | 30 (22.1) | 27 (20.0) | ||
| Primary | 36 (26.5) | 41 (30.4) | ||
| Secondary | 30 (22.1) | 41 (30.4) | ||
| Graduate | 39 (28.6) | 24 (17.8) | ||
| Postgraduate | 1 (0.7) | 2 (1.4) | ||
| 4 | Cervical dilatation at the start of the partogram (cm) | 5.125±0.331 | 4.190±0.431 | .721a |
| 5 | Body mass index (kg/m2), mean±SD | 21.0±1.7 | 20.9±1.4 | .598a |
| 6 | Gestational age at the time of delivery, mean±SD | 38.0±0.8 | 38.2±1.0 | .070a |
SD, standard deviation.
Independent t test
Chi-squared test.
Pandey. Reduction of primary cesarean delivery by use of World Health Organization Labor Care Guide. Am J Obstet Gynecol Glob Rep 2022.
The duration of the active phase of labor was found to be significantly short in the study group compared with the control group (2.27±1.44 vs 4.12±1.6 hours, respectively). There was no difference in terms of the duration of the second stage of labor, maternal complications, postdelivery hematological parameters, duration of hospital stay, Apgar score, average NICU stay, and final neonatal outcome (Tables 2 and 3).
Table 2.
Maternal outcomes of labor in study population
| Serial no. | Maternal parameters | Study group | Control group | P value |
|---|---|---|---|---|
| n=136 | n=135 | |||
| 1 | Mode of delivery, n (%) | |||
| Normal delivery | 127 (93.4) | 103 (76.3) | .0001a | |
| Operative vaginal delivery | 7 (5.14) | 8 (5.9) | .779a | |
| CD | 2 (1.5%)b | 24 (17.8)c | .000002d | |
| Total | 136 | 135 | ||
| 2 | Complications,e n (%) | |||
| PPH | 1 (0.9) | 1 (0.9) | 1d | |
| Infection | 0 (0) | 1 (0.9)e | .498d | |
| Total | 1 (0.9) | 2 (1.8) | .622d | |
| 3 | After delivery | |||
| Hb (gram%) | 9.940±1.220 | 9.644±1.096 | .037f | |
| Total leucocyte count (cells/mL) | 10,316.88±2383.90 | 10,553.46±2244.30 | .401f | |
| 4 | Duration of hospital stay (d), mean±SD | 2.014±1.092 | 2.210±1.170 | .155f |
| 5 | Oxytocin used | 25 (18.4) | 70 (51.8) | .000000008a |
| n=134g | n=111g | |||
| 6 | Duration of active phase of labor (h), mean±SD | 2.27±1.44 | 4.12±1.60 | .0000000000000000019f |
| 7 | Second stage of labor (min), mean±SD | 28.01±16.70 | 31.10±18.50 | .171f |
CD, cesarean delivery; PPH, postpartum hemorrhage; SD, standard deviation.
Chi-squared test
Study group: Of 2 CDs, the indications were arrest of labor and arrest of the second stage of labor
Control group: Of 24 CDs, 12 (50%) were performed for arrest of labor in the active phase, 3 (12.5%) were performed for second–stage arrest, and 9 (37.5%) were performed for fetal distress
Fisher exact test
Atonic PPH in 1 in each group, which was medically managed. Of note, 1 case in the control group had malarial infection
Independent t test
Of note, 2 women in the study group and 24 women in the control group underwent CD.
Pandey. Reduction of primary cesarean delivery by use of World Health Organization Labor Care Guide. Am J Obstet Gynecol Glob Rep 2022.
Table 3.
Neonatal outcomes of labor in the study population
| Serial no. | Neonatal parameters | Study group (n=136) | Control group (n=135) | P value |
|---|---|---|---|---|
| 1 | Birthweight, mean±SD | 2.84±0.33 | 2.79±0.31 | .200a |
| 2 | Apgar score at 5 min, mean±SD | 8.74±0.44 | 8.711±0.501 | .613a |
| 3 | Vital status at birth, n (%) | — | ||
| Live birth | 136 (100.0) | 135 (100.0) | ||
| Still birth | 0 (0) | 0 (0) | ||
| 4 | NICU admission, n (%) | .018d | ||
| Yes | 3 (2.2)b | 12 (8.9)c | ||
| No | 133 (97.8) | 123 (91.1) | ||
| 5 | Average NICU stay (d), mean±SD | 3.00±0.82 | 3.00±1.04 | 1a |
| 6 | Neonatal outcome | — | ||
| Discharged in satisfactory condition, n (%) | 136 (100.0) | 135 (100.0) |
NICU, neonatal intensive care unit; SD, standard deviation.
Independent t test
Indication for NICU admission: for observation in 3 neonates of study group
Of note, 12 NICU admissions in the control group for observation after operative vaginal delivery (n=2) and cesarean delivery (n=10: 9 for fetal distress and 1 arrest of active phase of labor). Moreover, 10 cases developed neonatal jaundice (the mothers of all 10 neonates received intrapartum oxytocin)
Fisher exact test.
Pandey. Reduction of primary cesarean delivery by use of World Health Organization Labor Care Guide. Am J Obstet Gynecol Glob Rep 2022.
Oxytocin was used in 25 of 136 women (18.4%) in the study group vs 70 of 135 women (51.8%) in the control group (P=.000000008) (Table 2). It was observed that mothers of 10 neonates in the control group, who developed neonatal jaundice, received intrapartum oxytocin (Table 3). The average maximum dose of oxytocin used was significantly lesser in the study group (16.90±10.10 mIU/min) than in the control group (19.50±9.26 mIU/min) (P=.000), and it was used for significantly more duration in the control group than in the study group (266.8±120.6 vs 184.8±125.3 minutes; P=.000).
The acceptability, difficulty, and satisfaction levels of the HCPs were recorded. For 4 months, each team needed an average of 6.5 LCG plots to shift the difficulty level from very difficult to neutral and 2.25 LCG plots to shift the difficulty level from neutral to easy level (Table 4).
Table 4.
Feedback on LCG use for labor monitoring on HCPs’ difficulty, acceptability, and satisfaction based on the 5-point Likert scale
| Serial no. | Assessment parameter and 5-point Likert scale | LCG user group (n=136) | |
|---|---|---|---|
| 1 | Difficulty | ||
| 1 very difficult | 10 (7.4) | ||
| 2 difficult | 8 (5.9) | ||
| 3 neutral | 9 (6.6) | ||
| 4 easy | 84 (61.8) | ||
| 5 very easy | 25 (18.3) | ||
| 2 | Acceptability | ||
| 1 highly acceptable | 75 (55.1) | ||
| 2 acceptable | 37 (27.2) | ||
| 3 moderately acceptable | 22 (16.2) | ||
| 4 fairly acceptable | 2 (1.5) | ||
| 5 not acceptable | 0 (0) | ||
| 3 | Satisfaction | ||
| 1 highly acceptable | 82 (60.3) | ||
| 2 acceptable | 33 (24.3) | ||
| 3 moderately acceptable | 20 (14.7) | ||
| 4 fairly acceptable | 1 (0.7) | ||
| 5 not acceptable | 0 (0) | ||
| 4 | Number of the LCG plotted to shift difficulty level | From very difficult to neutral | From neutral to easy |
| Teama 1 | 7 | 2 | |
| Team 2 | 6 | 2 | |
| Team 3 | 7 | 3 | |
| Team 4 | 6 | 2 | |
| Average | 6.50 | 2.25 | |
HCP, healthcare provider; LCG, Labor Care Guide.
Team refers to a team of HCPs posted in the labor room every month for 4 months.
Pandey. Reduction of primary cesarean delivery by use of World Health Organization Labor Care Guide. Am J Obstet Gynecol Glob Rep 2022.
Discussion
The control of maternal and neonatal mortality rates is one of the very important United Nations 2030 Sustainable Development Goals. The WHO has been working to accomplish a reduction in these health indicators for the last 50 years. CD contributes to significant maternal short-term and long-term morbidity rates. Globally, CD rates are on the rise. Different studies have shown that approximately 50% to 75% of primary CDs were due to indications about intrapartum management. As per the Robson Ten Group Classification System recommended by the WHO, Robson group 5 has been cited as the biggest contributor group for CD followed by groups 2 and 1.6 Thus, to reduce the overall CD rates, there is a need to focus on these 3 groups. If primary CD rates are controlled by justified labor monitoring, it will automatically reduce the burden of group 5, bringing down the overall CD rates. Thus, there was a clear need of refining labor monitoring to reduce the increasing figures of primary CD.9,16
Different partograph designs, under the WHO Safe Motherhood Initiative (1987), were introduced. The utilization rate and correct completion rates have been observed as low as 31% and 3%, respectively.17 The WHO recommendation on positive intrapartum care and birth experience (2018) brought forward updated and evidence-based definitions with an ultimate goal to reduce the overall maternal and neonatal mortality and morbidity rates.10 The WHO LCG, the next-generation partograph, was introduced for the application of these recommendations.13
Although the LCG has been developed after obtaining a comprehensive understanding, discussion, and field implementation, Hofmeyr et al18 suggested more research on the implementation and effect of the LCG on labor outcomes.15
After the release of the LCG in December 2020, although there are a few surveys of maternity care providers on LCG use, no study has been conducted to determine its effect on labor outcomes, including the reduction of CD rates.19
The potential confounders, which could have affected the labor outcome, such as age, parity, body mass index, gestational age, and cervical dilatation at the start of the partogram, were similar in both groups (P>.05) (Table 1). The duration of labor in the study group was found to be significantly shorter than in the control group (P<.001). This is clearly due to the difference in the definition of the “active phase of labor” by both partographs. The active phase of labor, starting after 4 cm following the WHO-modified partograph, took more time for labor progress (Table 2). Zhang et al20 analyzed the labor pattern of 62,415 parturients at 19 centers and demonstrated that labor may take >6 hours to progress from 4 to 5 cm of dilatation and more than 3 hours to progress from 5 to 6 cm of dilatation. Moreover, labor progressed at a similar yet slow pace before 6 cm of dilatation irrespective of parity. However, after 6 cm of dilatation, the curve turns steeper because of fast progress, much faster in multiparas than in nulliparas. Thus, they suggested the active phase of labor to start from 6 cm dilatation, which has been endorsed by the ACOG in 2014.7 The WHO-updated recommendations10 defined the active phase of labor as starting from 5 cm of dilatation, which is the starting point of the LCG. The LCG has allowed almost 18.5 hours maximum duration from 5 cm of dilatation to full dilatation. Allowing this amount of time distinguishes abnormal labor from normal ones very effectively. Here, of 136 women in the study group, only 2 CDs were performed for the arrest of the active phase of labor and second stage of labor. This was in contrast to the 17.8% CD rate in the control group. Of 24 CDs performed in the control group, 12 (50%) were due to arrest of the active phase of labor, 3 (12.5%) were due to arrest of the second stage of labor, and 9 (37.5%) were due to fetal distress. Hitherto, the contribution of primary CD performed in spontaneous labor (Robson groups 1 and 3) at our center was approximately 17.7%.6
Thus, using the LCG, significant improvement in the CD rate was achieved in Robson groups 1 and 3, which were focused on in this study. The result of the CD rate by use of the LCG in the only study available that was published before LCG release was 7.1%. The lower CD rate with LCG use in this study could be because of the difference in the sample size and better understanding of the LCG after the release of the user guidelines by the WHO.
Compared with the WHO-modified partograph, the LCG has dropped the concept of the alert line with a slope of 1 cm/hour and allows much more duration (18.5 hours after 5 cm for the first stage of labor) along with the documentation of the monitoring of the second stage of labor. The active phase of labor starts at 5 cm of dilatation. Supportive care, which includes companionship, analgesia, and opportunity to have the posture of choice during labor, with shared decision-making and use of medical interventions only when required, makes labor a positive experience for women. A birth companion can be anyone of the parturient's choice, such as the doulas, spouse, family member, or healthcare professional.
Here, fewer women in the study group required oxytocin (P<.0001). It was observed that oxytocin was used in all women where CD was done for fetal distress and that the neonates developed neonatal jaundice. This stresses that interventions during labor must be restricted and that the LCG guides relevantly about the judicious use of these interventions.
The 2 groups were similar in terms of the duration of the second stage of labor, maternal complications, duration of hospital stay, Apgar score, and overall neonatal outcome (P>.05). This suggested that shifting from the previous partograph design to the LCG does not affect the maternofetal outcome adversely and has an additional advantage of actively cutting down the primary CD rates, which will be helpful in the prevention of other dreadful morbidities associated with CD, such as the future risk of increased CDs, developing placenta accreta spectrum disorders, and uterine rupture.
The most common cause of NICU admission in the control group was physiological jaundice, which was closely associated with the use of oxytocin (Tables 2 and 3). Oxytocin is known to lead to an increased incidence of neonatal jaundice, owing to the immature activity of glucuronyltransferase and increased erythrocyte fragility. The LCG does not support interventions, such as oxytocin administration and stripping of membranes until the maternofetal condition is reassuring.5 Oxytocin use can be guided by following the “alert parameters” described in the LCG. In addition, a recent systematic review by Dupont et al21 has recommended the judicious use of intrapartum oxytocin and suggested amniotomy as the first choice to augment labor in the event of dystocia.
Here, the authors realized the importance of HCP training. We suggest providing a free access online training video to enhance the widespread acceptability of the LCG. The tertiary centers can get trained and further train their feeder centers to optimize the use of resources.
Ours is a tertiary center with an average annual delivery rate of approximately 28,000 per year. The HCPs at this center are under a very heavy workload. One of them, during the early phase of LCG use, commented that “continuous filling LCG was tough and bound to be inflicted with inaccurate entries owing to human error.” However, following consistent use of the LCG, the HCPs at our institute became increasingly convinced that it helped reduce unnecessary interventions during labor. They realized that owing to the reduction in unwarranted interventions, their workload was reduced.
Few of the HCPs in their initial phase of LCG use felt the need for an action line to guide them and found it challenging to exactly understand when to respond. Similar HCP responses were also recorded by Vogel et al.15
Later with the use of approximately 6 and 2 LCG plots, the difficulty level reduced from very difficult to neutral to easy, respectively. Furthermore, their outlook toward the LCG changed, emphasizing the need for training followed by consistent use to overcome the inhibitions of adopting a new method. Our training and regular motivation for consistently using the LCG finally convinced the HCPs. High acceptability and satisfaction levels were observed among the LCG users.
Implications of future research
Further study with a larger sample size, including high-risk laboring women, is suggested to extend the benefits of the LCG.
Strengths and limitations
This study investigated the effect of the LCG on reducing CD rates and overall labor outcomes after the release of the WHO LCG in December 2020. An attempt was made to determine the learning curve for use of the LCG by HCPs, which was quite encouraging. With the progression of the study, we have been able to convince our HCPs to the easy adoption of the new LCG in routine practice.
The main limitations of the study were that only low-risk antenatal women were recruited and recruitment was done during spontaneous labor. Further studies can be contemplated, including high-risk pregnancies. After the release of the LCG manual (December 2020), this study was used as a pilot project for a small sample size. Studies with a larger sample size can be planned.
Conclusion
The WHO LCG, the-next generation partograph, is a complex-looking yet simple and feasible labor-monitoring tool that can reduce the number of primary CDs by patiently allowing labor to progress. The implementation and widespread applicability of the LCG require initial proper training of the HCPs and supervision in the early phases to make the HCPs well acquainted with this next-generation partograph.
Footnotes
This study was registered on ClinicalTrials.gov (registration number: CTRI/2021/09/036189; http://ctri.nic.in/Clinicaltrials/login.php) on March 9, 2021. The Date of initial participant enrollment was on July 9, 2021.
The authors report no conflict of interest.
Patient consent was taken in each case.
Cite this article as: Pandey D, Bharti R, Dabral A, et al. Impact of WHO Labor Care Guide on reducing cesarean sections at a tertiary center: an open-label randomized controlled trial. Am J Obstet Gynecol Glob Rep 2022;2:100075.
References
- 1.Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323–e333. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 2.Lawn JE, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016;387:587–603. doi: 10.1016/S0140-6736(15)00837-5. [DOI] [PubMed] [Google Scholar]
- 3.Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012;29:7–18. doi: 10.1055/s-0031-1285829. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary; 2019. Trends in maternal mortality 2000 to 2017: estimates by WHO.https://apps.who.int/iris/handle/10665/327596 Available at. Accessed August 10, 2022. [Google Scholar]
- 5.WHO statement on caesarean section rates . Geneva; 2015. World Health Organization.https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf Available at. Accessed August 10, 2022. [Google Scholar]
- 6.Mittal P, Pandey D, Suri J, Bharti R. Trend prediction for cesarean deliveries based on Robson classification system at a tertiary referral unit of North India. J Obstet Gynaecol India. 2020;70:111–118. doi: 10.1007/s13224-019-01275-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American College of Obstetricians and Gynecologists (College), Society for Maternal-Fetal Medicine. Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210:179–193. doi: 10.1016/j.ajog.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 8.Wiklund I, Malata AM, Cheung NF, Cadée F. Appropriate use of caesarean section globally requires a different approach. Lancet. 2018;392:1288–1289. doi: 10.1016/S0140-6736(18)32325-0. [DOI] [PubMed] [Google Scholar]
- 9.Zhang J, Troendle J, Reddy UM, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203:326. doi: 10.1016/j.ajog.2010.06.058. e1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Recommendations: intrapartum care for a positive childbirth experience. [PubMed] [Google Scholar]
- 11.Oladapo OT, Diaz V, Bonet M, et al. Cervical dilatation patterns of ‘low-risk’ women with spontaneous labour and normal perinatal outcomes: a systematic review. BJOG. 2018;125:944–954. doi: 10.1111/1471-0528.14930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abalos E, Oladapo OT, Chamillard M, et al. Duration of spontaneous labour in ‘low-risk’ women with ‘normal’ perinatal outcomes: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2018;223:123–132. doi: 10.1016/j.ejogrb.2018.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. WHO labour care guide: user's manual. 2021. Available at:https://www.who.int/publications/i/item/9789240017566. Accessed March 19, 2022.
- 14.World Health Organization, United Nations Population Fund & United Nations Children's Fund (UNICEF) 2nd ed. World Health Organization; Geneva, Switzerland: 2017. Managing complications in pregnancy and childbirth: a guide for midwives and doctors. [Google Scholar]
- 15.Vogel JP, Comrie-Thomson L, Pingray V, et al. Usability, acceptability, and feasibility of the World Health Organization Labour Care Guide: a mixed-methods, multicountry evaluation. Birth. 2021;48:66–75. doi: 10.1111/birt.12511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118:29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bedada KE, Huluka TK, Bulto GA, Roga EY. Low utilization of partograph and its associated factors among obstetric care providers in governmental health facilities at West Shoa Zone, Central Ethiopia. Int J Reprod Med. 2020;2020 doi: 10.1155/2020/3738673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hofmeyr GJ, Bernitz S, Bonet M, et al. WHO next-generation partograph: revolutionary steps towards individualised labour care. BJOG. 2021;128:1658–1662. doi: 10.1111/1471-0528.16694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pingray V, Bonet M, Berrueta M, et al. The development of the WHO Labour Care Guide: an international survey of maternity care providers. Reprod Health. 2021;18:66. doi: 10.1186/s12978-021-01074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang J, Landy HJ, Ware Branch D, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116:1281–1287. doi: 10.1097/AOG.0b013e3181fdef6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dupont C, Carayol M, Le Ray C, et al. [Oxytocin administration during spontaneous labour: guidelines for clinical practice. Guidelines short text] Gynecol Obstet Fertil Senol. 2017;45:56–61. doi: 10.1016/j.gofs.2016.12.017. [DOI] [PubMed] [Google Scholar]