Abstract
BACKGROUND
Single fetal demise after intervention for twin-twin transfusion syndrome is a relatively common complication and is often devastating for the patients.
OBJECTIVE
This meta-analysis aimed to evaluate the risk of single fetal demise based on gestational age and Quintero staging at the time of interventions in twin-to-twin transfusion syndrome after fetoscopic laser photocoagulation.
STUDY DESIGN
Systematic search was performed in PubMed, Web of Science, and Scopus from inception to August 2021. The primary outcome was to compare the incidence of fetal demise between low (I and II) and high (III and IV) twin-to-twin transfusion syndrome Quintero stages. The rate of donor and recipient fetal demise in each stage was compared with that in stage I. Gestational age at fetoscopic laser photocoagulation was compared between surviving fetuses and fetuses that died.
RESULTS
A total of 10 studies (4031 fetuses with twin-to-twin transfusion syndrome) were included in this review. Donor demise was associated with high Quintero stages compared with surviving donors (odds ratio, 2.42; 95% confidence interval, 1.78–3.29; P<.001; I2, 0%). Recipient fetal demise had a trend for higher Quintero stage compared with surviving recipients, but the analysis did not achieve statistical significance. Pregnancies with donor demise had lower gestational at the time of fetoscopic laser photocoagulation (mean difference, −0.56; 95% confidence interval, –0.93 to –0.18; P=.003; I2, 36%), whereas pregnancies complicated by recipient demise had similar gestational at time of fetoscopic laser photocoagulation compared with those without demise.
CONCLUSION
Demise of the donor fetus was significantly increased after fetoscopic laser photocoagulation for higher stages compared with lower ones. Lower gestational age at the time of fetoscopic laser photocoagulation was associated with an increased risk of single fetal demise in twin-to-twin transfusion syndrome. This was attributed to increased donor demise but not recipient death.
Key words: fetal demise, gestational age, meta-analysis, Quintero staging, twin-twin transfusion syndrome
AJOG Global Reports at a Glance.
Why was this study conducted?
This study aimed to systematically examine the risk of single fetal demise based on the gestational age (GA) and Quintero staging at the time of intervention for twin-twin transfusion syndrome (TTTS).
Key findings
The group with donor fetal demise had high Quintero stages and lower GA at laser therapy than surviving donor fetuses. Recipient fetal demise had a trend for higher Quintero stage compared with surviving recipient fetuses, but the analysis did not achieve statistical significance.
What does this add to what is known?
The demise of the donor fetus was significantly increased after laser therapy for higher Quintero stages compared with lower ones. Lower GA at the time of laser therapy was associated with an increased risk of single fetal demise in TTTS. This was attributed to increased donor demise but not recipient fetal death.
Introduction
Twin-to-twin transfusion syndrome (TTTS) complicates 9% to 15% of monochorionic twin pregnancies and, without treatment, is associated with high fetal loss rates (70%–100%).1, 2, 3 Fetoscopic laser photocoagulation (FLP) is the standard therapy for TTTS. However, FLP is associated with the risk of fetal demise of the donor and/or recipient, and this risk has been significantly reduced as a result of a technical improvement and learning curve. Proposed factors influencing single fetal death after FLP include laser technique, abnormal Doppler evaluation, selective fetal growth restriction (FGR), and estimated fetal weight discordance.
Quintero staging has been widely used since its introduction by Quintero et al4 in 1999 for classifying the disease severity and guiding the need for therapy. Although Quintero stages have not been associated with dual fetal survival, stratifications of the outcomes based on stages showed that advanced Quintero staging may be associated with increased risks of single fetal demise.5
In contrast to dual fetal demise after FLP for TTTS, single fetal demise is much more common and is often devastating for the parents after the procedure. Understanding the risk of fetal demise based on the most common variables, such as gestational age (GA) at the intervention and Quintero staging, would allow for better planning for FLP and more accurate counseling for the parents, allowing them to be prepared for unfavorable outcomes.
In this systematic review and meta-analysis, we sought to systematically examine the risk of single fetal demise based on the GA and Quintero staging at the time of interventions.
Methods and Materials
The meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist.6 The study protocol for this systematic review was registered in the International Prospective Register of Systematic Reviews (registration number: CRD42021237073).
Search strategy
A systematic literature search was performed by 2 independent authors (K.H. and A.A.N.) on PubMed, Web of Science, and Scopus from inception to February 9, 2021. A search was performed using the following key words: “co-twin,” “donor,” “recipient,” “twin,” “fetus,” “fetal,” “dead,” “death,” “demise,” “mortality,” “TTTS,” “twin-twin transfusion syndrome,” “twin to twin transfusion syndrome,” and “laser.” References of relevant articles were manually reviewed, and eligible studies were added to results from an electronic literature search.
Inclusion and exclusion
The inclusion criteria were pregnancies diagnosed with TTTS undergoing FLP complicated by donor or recipient fetal demise. The Table provides the definition of fetal demise among included studies.
Table.
Fetal demise among included studies
| First author (country) | Study design | Type of FLP | Number of analyzed fetuses in this meta-analysis | Number of donor demise | Number of recipient demise | Definition of fetal demise | Variables included in the meta-analysis | NOS | |
|---|---|---|---|---|---|---|---|---|---|
| Buskmiller et al7 2021 (United States) | Prospective | Selective or Solomon | 826 | 50 (6.1) | 10 (1.2) | Fetaldemise was identified by the referring physician on follow‐up ultrasounds, and the timing of demise was documented. | Quintero staging | 7 | |
| Kim et al8 2021 (Republic of Korea) | Retrospective | Selective or Solomon | 344 | 46 (13.4) | 24 (7.0) | NR | GA at FLP | 6 | |
| Snowise et al9 2015 (United States) | Prospective | Selective or Solomon | 154 | 20 (13.0) | — | Fetal demise was defined asthe absence of fetal heart activity on ultrasonographyafter the procedure and before the onset of labor. | GA at FLP and Quintero staging | 7 | |
| Tachibana et al10 2014 (Germany) | Retrospective | Selective | 214 | 10 (4.7) | 5 (2.3) | NR | Quintero staging | 7 | |
| Skupski et al11 2010 (United States) | Retrospective | Random (nonsequential) and selective | 932 | 111 (11.9) | 77 (8.3) | Fetal demise was defined asdeath before birth. | GA at FLP | 8 | |
| Purnell et al12 2020 (United States) | Retrospective | Selective with or without sequential technique | 153 | 43 (28.1) | — | NR | GA at FLP | 8 | |
| Morris et al13 (United Kingdom) | Prospective | Selective | 328 | 81 (24.7) | 24 (7.3) | NR | Quintero staging | 8 | |
| Kontopoulos et al14 (United States) | Retrospective | Selective | 401 | 91 (22.7) | — | Fetal demise was defined as demise of 1 twin at any time after laser therapy and before the onset of labor. | GA at FLP and Quintero staging | 6 | |
| Eschbach et al15 (The Netherlands) | Prospective | Sequential selective laser coagulation of all communicating vessels, with coagulation of the whole vascular equator (the Solomon technique) or without this additional coagulation | 249 | 30 (12.0) | 27 (10.8) | Fetal demise was defined as demise of 1 twin at any time after laser therapy and before the onset of labor. | GA at FLP and Quintero staging | 7 | |
| Eixarch et al16 (Spain) | Prospective | Selective | 430 | 33 (7.7) | 17 (4.0) | Fetal demise was defined as fetal death occurringwithin 1 wk after surgery. | GA at FLP and Quintero staging | 7 | |
FLP, fetoscopic laser photocoagulation; GA, gestational age; NOS, Newcastle-Ottawa Scale, NR, not reported.
Nassr. Gestational age and Quintero staging as predictors of single fetal demise in twin-twin transfusion syndrome. Am J Obstet Gynecol Glob Rep 2022.
The exclusion criteria were conservative management or amnioreduction (no FLP); triplet pregnancies; dual fetal demise; single fetal demise not determining the recipient or donor; obvious cause of fetal demise, such as premature rupture of membranes; and selective fetal reduction. Furthermore, case reports or case series, conference abstracts, and review articles were excluded. The search was limited to articles published in the English language with no time limitation. Initially selected studies were reviewed for eligibility by 2 independent authors (K.H. and A.A.N.), and discrepancies between reviewers were resolved by consulting the third investigator (A.A.S.).
Outcome measure
The primary outcome was to compare the incidence of fetal demise between low- and high-Quintero stage TTTS pregnancies. Low stage included Quintero stages 1 and 2, and high stage included Quintero stages 3 and 4.17 The rates of fetal demise in each Quintero stage were compared with that in stage 1. GA at FLP was obtained from studies and compared between surviving fetuses and fetuses that died as secondary outcomes. All analyses were performed for single donor demise and recipient demise as 2 separate groups.
Quality assessment
Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of included studies and the risk of bias. NOS is composed of “participant selection,” “comparability of study groups,” and “assessment of outcome or exposure.” A score of >7 is considered high quality.18
Statistical analysis
Statistical analysis was performed using Review Manager (version 5.4; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). If data were presented as median (range) or median (interquartile range), data were converted to mean and standard deviation using the Hozo formula.19 Pooled effect sizes were presented using mean difference (MD) or odds ratio (OR) with a 95% confidence interval (CI) for continuous and categorical variables, respectively. Only outcomes that were reported in >2 studies were analyzed. I-squared tests (I2) were used to examine heterogeneity across the included studies; I2≥50% and P<.05 indicated heterogeneity. A random-effects model was used because of the anticipated heterogeneity of included studies.
Results
A total of 993 articles were retrieved. Of those articles, 351 were excluded for duplication. The remaining 642 studies were screened for eligibility. Title and abstract screening resulted in 100 potentially eligible studies. After a full-text assessment was performed, 10 studies met the inclusion criteria defined in our methodology (Figure 1). Studies by Gapp-Born et al20 and Leduc et al21 were excluded because data on single and dual fetal demises were not separated and individual data were not available on request.
Figure 1.
PRISMA flowchart
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Nassr. Gestational age and Quintero staging as predictors of single fetal demise in twin-twin transfusion syndrome. Am J Obstet Gynecol Glob Rep 2022.
Study characteristics
All included studies were published between 2007 and 2021. Of note, 5 studies were conducted in the United States,7,9,11,12,14 1 study was conducted in the Netherlands,15 1 study was conducted in Spain,16 1 study was conducted in Germany,10 1 study was conducted in Republic of Korea,8 and 1 study was conducted in the United Kingdom.13 One of the studies was a multicenter cohort conducted in the United States, Belgium, and Spain.16 Moreover, 5 studies were designed as retrospective, and 5 studies were designed as prospective. A total of 4031 fetuses were eligible for this meta-analysis, of whom 515 were identified as donor demise, 184 were identified as recipient demise, and the remaining fetuses were identified as survivors. Details of included studies are reported in the Table.
Quintero staging and fetal demise (donor and recipient)
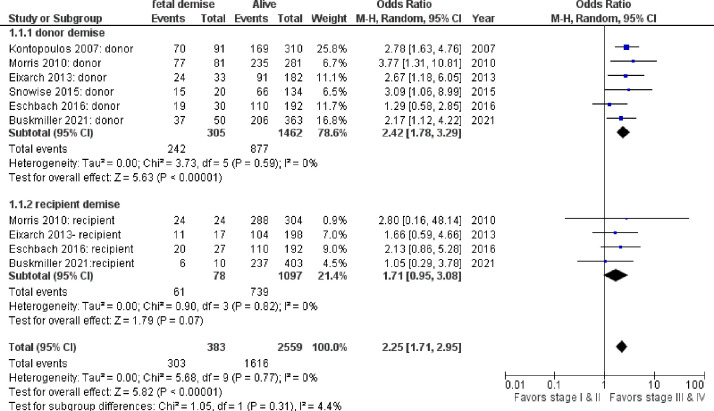
Donor fetal demise was more likely to be associated with higher Quintero stages than surviving donors (OR, 2.42; 95% CI, 1.78–3.29; P<.001; I2, 0%). Cases with fetal demise involving the recipient twin had a trend for higher Quintero stage compared with cases where the recipient twins survived, but the analysis did not achieve statistical significance (OR, 1.71; 95% CI, 0.95–3.08; P=.07; I2, 0%) (Figure 2).
Figure 2.
The risk of stages III and IV Quintero stage among pregnancies complicated with single fetal demise vs those without single fetal demise
CI, confidence interval.
Nassr. Gestational age and Quintero staging as predictors of single fetal demise in twin-twin transfusion syndrome. Am J Obstet Gynecol Glob Rep 2022.
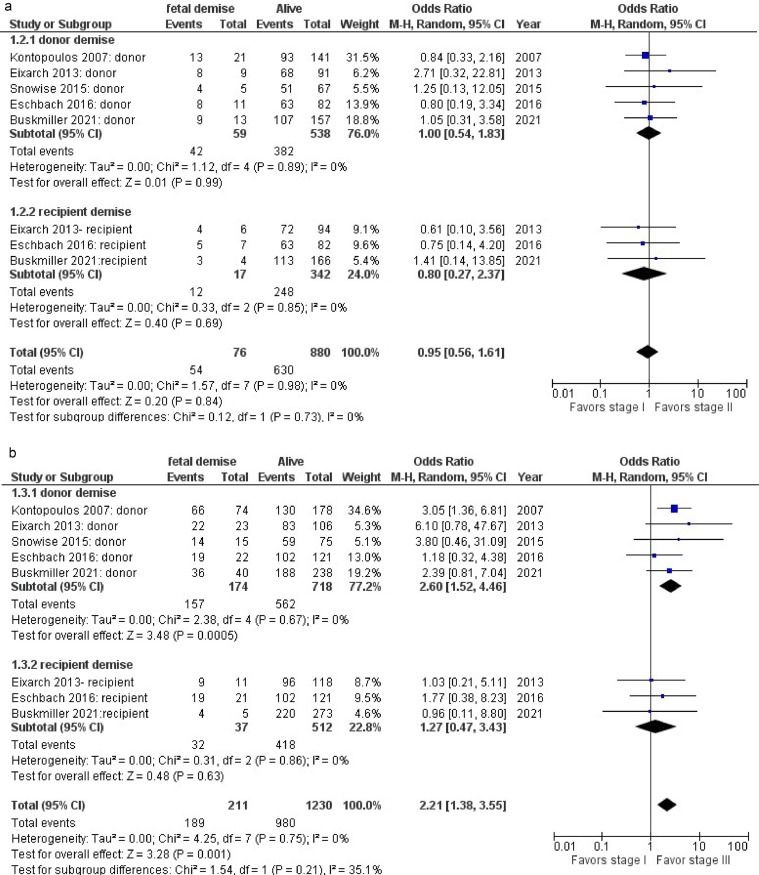
When the incidence of fetal demise was compared between Quintero stage 2 and Quintero stage 1 fetuses, no statistically significant difference was found for donor demise (OR, 1.00; 95% CI, 0.54–1.83; P=.99; I2, 0%) and recipient demise (OR, 0.80; 95% CI, 0.27–2.37; P=.69; I2, 0%) (Figure 3, A).
Figure 3.
The risk of stages II and III Quintero among pregnancies complicated with single fetal demise vs those without single fetal demise
A, Risk of stage II Quintero. B, Risk of stage III Quintero.
CI, confidence interval.
Nassr. Gestational age and Quintero staging as predictors of single fetal demise in twin-twin transfusion syndrome. Am J Obstet Gynecol Glob Rep 2022.
When the incidence of fetal demise was compared between Quintero stage 3 and Quintero stage 1 fetuses, the donor fetal demise was significantly more common in stage 3 (OR, 2.60; 95% CI, 1.52–4.46; P<.001; I2, 0%), but for the recipient fetal demise, no significant difference was found between stage 3 and stage 1 (OR, 1.27; 95% CI, 0.47–3.43; P, 0.63; I2, 0%) (Figure 3, B).
Gestational age at surgery and risk of fetal demise
The pooled results showed that pregnancies with donor fetal demise had significantly lower GA at the time of FLP than pregnancies with surviving donors (weeks) (MD, −0.56; 95% CI, −0.93 to −0.18; P=.003; I2, 36%), whereas pregnancies complicated with recipient fetal demise had similar GA at the time of FLP compared with those without recipient fetal demise (MD, −0.51; 95% CI, −1.17 to 0.15; P=.13; I2, 35%) (Figure 4).
Figure 4.
Gestational age among pregnancies complicated with single fetal demise vs those without single fetal demise
CI, confidence interval; FLP, fetoscopic laser photocoagulation; GA, gestational age; SD, standard deviation.
Nassr. Gestational age and Quintero staging as predictors of single fetal demise in twin-twin transfusion syndrome. Am J Obstet Gynecol Glob Rep 2022.
Discussion
Principal findings
This systematic review and meta-analysis demonstrated that earlier GA at FLP is associated with an increased risk of donor fetal demise in cases of TTTS compared with later GA. In addition, the odds of single fetal demise of the donor were significantly increased after FLP for higher Quintero staging (stages III and IV) compared with lower Quintero staging (stages I and II). When rates of single fetal demise after FLP for stages II and III were individually compared with that for stage I, mortality was similar in stage II but not in stage III. The finding of Quintero stage III in TTTS increased the risk of single fetal demise of the donor but not the recipient.
Interpretation of findings
Increased risks of single fetal demise, particularly for the donor, with earlier GA at intervention could be explained by susceptibility of fetuses with TTTS to hemodynamic compromise at early GA after FLP of the anastomotic vessels. Because donor fetuses tend to be growth restricted, these abrupt changes could particularly affect severely growth-restricted donor fetuses with abnormal umbilical artery Doppler.
As advanced stages of TTTS reflect some degree of cardiovascular compromise in either the donor or the recipient twin, hemodynamic effects of FLP may accentuate cardiovascular compromise in these fetuses and can be responsible for higher risks of single fetal demise in advanced Quintero staging TTTS. Compared with baseline stage I TTTS, a higher risk of single fetal demise was observed in donors with stage III TTTS but not in recipients with stage II or III TTTS. An expected explanation for this finding would be the associated severe FGR with abnormal umbilical artery blood flow. These growth-restricted donor fetuses eventually develop severe placental insufficiency after coagulation of the placental vascular anastomoses, particularly arterioarterial anastomoses.
Clinical implications
This meta-analysis provided valuable information, which helps counsel and guide the management of patients with TTTS. Better understanding of the chances of single fetal demise in TTTS cases is of paramount importance to prepare the expectant parents preoperatively. In addition, in difficult cases of FLP when selective coagulation is not possible or very challenging, favoring recipient territories should be considered when chances of donor demise are expected to be high. Favoring donor territories in such cases may result in dual fetal demise.
Strengths and limitations
This systematic review analyzed the risk of single fetal demise based on Quintero staging and GA at intervention. Given the heterogeneous data and analyses for other possible predictors for single fetal demise, such as selective FGR, estimated fetal weight discordance, and velamentous or marginal cord insertion, we decided to focus on GA and Quintero staging. This allowed the analysis of homogeneous data with low risks of bias. In addition, patients with stage III TTTS were subclassified on the basis of donor or recipient abnormal Doppler studies, which permitted subgroup analyses for the donor and recipient survival.
The main limitation of our meta-analysis was the lack of adjustment for other possible confounders, such as operator experience, presence and degree of selective FGR, maternal body mass index, and placental locations. Other limitations were the inclusion of retrospective studies with inherent flaws and heterogeneity in some of the analyzed outcomes.
Conclusions
The risks of donor fetal demise after FLP in TTTS cases increased with earlier GA at intervention and with advanced Quintero staging. Given the limitation of the current systematic reviews and meta-analyses, the findings need to be interpreted with caution.
Footnotes
The authors report no conflict of interest.
This study received no funding.
Patient consent was not required because no personal information or detail was included.
Cite this article as: Nassr AA, Hessami K, Espinoza J, et al. Gestational age and Quintero staging as predictors of single fetal demise in twin-twin transfusion syndrome after fetoscopic laser photocoagulation: a systematic review and meta-analysis. Am J Obstet Gynecol Glob Rep 2022;2:100055.
References
- 1.Lewi L, Jani J, Blickstein I, et al. The outcome of monochorionic diamniotic twin gestations in the era of invasive fetal therapy: a prospective cohort study. Am J Obstet Gynecol. 2008;199:514. doi: 10.1016/j.ajog.2008.03.050. e1–8. [DOI] [PubMed] [Google Scholar]
- 2.Sebire NJ, Souka A, Skentou H, Geerts L, Nicolaides KH. Early prediction of severe twin-to-twin transfusion syndrome. Hum Reprod. 2000;15:2008–2010. doi: 10.1093/humrep/15.9.2008. [DOI] [PubMed] [Google Scholar]
- 3.Urig MA, Clewell WH, Elliott JP. Twin-twin transfusion syndrome. Am J Obstet Gynecol. 1990;163:1522–1526. doi: 10.1016/0002-9378(90)90618-h. [DOI] [PubMed] [Google Scholar]
- 4.Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol. 1999;19:550–555. doi: 10.1038/sj.jp.7200292. [DOI] [PubMed] [Google Scholar]
- 5.Chmait RH, Kontopoulos EV, Korst LM, Llanes A, Petisco I, Quintero RA. Stage-based outcomes of 682 consecutive cases of twin-twin transfusion syndrome treated with laser surgery: the USFetus experience. Am J Obstet Gynecol. 2011;204:393. doi: 10.1016/j.ajog.2011.02.001. e1–6. [DOI] [PubMed] [Google Scholar]
- 6.Moher D, Altman DG, Liberati A, statement Tetzlaff J.PRISMA. Epidemiology. 2011;22:128. doi: 10.1097/EDE.0b013e3181fe7825. [DOI] [PubMed] [Google Scholar]
- 7.Buskmiller C, Bergh EP, Johnson A, Jr Moise KJ, Papanna R. Predicting fetal and neonatal demise after fetoscopy for twin-twin transfusion syndrome using recursive partitioning. Prenat Diagn. 2021;41:1541–1547. doi: 10.1002/pd.5948. [DOI] [PubMed] [Google Scholar]
- 8.Kim R, Lee MY, Won HS, et al. Perinatal outcomes and factors affecting the survival rate of fetuses with twin-to-twin transfusion syndrome treated with fetoscopic laser coagulation: a single-center seven-year experience. J Matern Fetal Neonatal Med. 2021:1–12. doi: 10.1080/14767058.2021.1888286. [DOI] [PubMed] [Google Scholar]
- 9.Snowise S, Moise KJ, Johnson A, Bebbington MW, Papanna R. Donor death after selective fetoscopic laser surgery for twin-twin transfusion syndrome. Obstet Gynecol. 2015;126:74–80. doi: 10.1097/AOG.0000000000000858. [DOI] [PubMed] [Google Scholar]
- 10.Tachibana D, Glosemeyer P, Diehl W, et al. Time-interval analysis of ductus venosus flow velocity waveforms in twin-to-twin transfusion syndrome treated with laser surgery. Ultrasound Obstet Gynecol. 2015;45:544–550. doi: 10.1002/uog.13449. [DOI] [PubMed] [Google Scholar]
- 11.Skupski DW, Luks FI, Walker M, et al. Preoperative predictors of death in twin-to-twin transfusion syndrome treated with laser ablation of placental anastomoses. Am J Obstet Gynecol. 2010;203:388. doi: 10.1016/j.ajog.2010.06.018. e1–11. [DOI] [PubMed] [Google Scholar]
- 12.Purnell ME, Chon AH, Korst LM, Llanes A, Grubbs BH, Chmait RH. Percent absent end-diastolic velocity in the umbilical artery and donor twin demise after laser surgery for twin-twin transfusion syndrome. Fetal Diagn Ther. 2020;47:572–579. doi: 10.1159/000505780. [DOI] [PubMed] [Google Scholar]
- 13.Morris RK, Selman TJ, Harbidge A, Martin WI, Kilby MD. Fetoscopic laser coagulation for severe twin-to-twin transfusion syndrome: factors influencing perinatal outcome, learning curve of the procedure and lessons for new centres. BJOG. 2010;117:1350–1357. doi: 10.1111/j.1471-0528.2010.02680.x. [DOI] [PubMed] [Google Scholar]
- 14.Kontopoulos EV, Quintero RA, Chmait RH, Bornick PW, Russell Z, Allen MH. Percent absent end-diastolic velocity in the umbilical artery waveform as a predictor of intrauterine fetal demise of the donor twin after selective laser photocoagulation of communicating vessels in twin-twin transfusion syndrome. Ultrasound Obstet Gynecol. 2007;30:35–39. doi: 10.1002/uog.4055. [DOI] [PubMed] [Google Scholar]
- 15.Eschbach SJ, Boons LS, Wolterbeek R, et al. Prediction of single fetal demise after laser therapy for twin-twin transfusion syndrome. Ultrasound Obstet Gynecol. 2016;47:356–362. doi: 10.1002/uog.15753. [DOI] [PubMed] [Google Scholar]
- 16.Eixarch E, Valsky D, Deprest J, et al. Preoperative prediction of the individualized risk of early fetal death after laser therapy in twin-to-twin transfusion syndrome. Prenat Diagn. 2013;33:1033–1038. doi: 10.1002/pd.4191. [DOI] [PubMed] [Google Scholar]
- 17.Chang YL, Chao AS, Chang SD, et al. Outcome of twin-twin transfusion syndrome treated by laser therapy in Taiwan's single center: role of Quintero staging system. Taiwan J Obstet Gynecol. 2016;55:700–704. doi: 10.1016/j.tjog.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 19.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gapp-Born E, Sananes N, Guerra F, et al. Predictive value of cardiovascular parameters in stages 1 and 2 of twin-to-twin transfusion syndrome. Prenat Diagn. 2014;34:908–914. doi: 10.1002/pd.4393. [DOI] [PubMed] [Google Scholar]
- 21.Leduc F, Delabaere A, Gendron R, et al. Aortic isthmus flow recording predicts the outcome of the recipient twin after laser coagulation in twin-twin transfusion syndrome. Fetal Diagn Ther. 2018;44:135–141. doi: 10.1159/000479736. [DOI] [PubMed] [Google Scholar]