Abstract
Background:
The 2019 coronavirus disease (COVID-19) is a mysterious and highly infectious disease that was declared a pandemic by the World Health Organization. The virus poses a great threat to global health and the economy. Currently, in the absence of effective treatment or vaccine, leveraging advanced digital technologies is of great importance. In this respect, the Internet of Things (IoT) is useful for smart monitoring and tracing of COVID-19. Therefore, in this study, we have reviewed the literature available on the IoT-enabled solutions to tackle the current COVID-19 outbreak.
Methods:
This systematic literature review was conducted using an electronic search of articles in the PubMed, Google Scholar, ProQuest, Scopus, Science Direct, and Web of Science databases to formulate a complete view of the IoT-enabled solutions to monitoring and tracing of COVID-19 according to the FITT (Fit between Individual, Task, and Technology) model.
Results:
In the literature review, 28 articles were identified as eligible for analysis. This review provides an overview of technological adoption of IoT in COVID-19 to identify significant users, either primary or secondary, required technologies including technical platform, exchange, processing, storage and added-value technologies, and system tasks or applications at “on-body,” “in-clinic/hospital,” and even “in-community” levels.
Conclusions:
The use of IoT along with advanced intelligence and computing technologies for ubiquitous monitoring and tracking of patients in quarantine has made it a critical aspect in fighting the spread of the current COVID-19 and even future pandemics.
Keywords: Coronavirus, COVID-19, Internet of Things, systematic review
Context
The 2019 coronavirus disease (COVID-19) is a highly contagious disease that has affected a large portion of the population. It is caused by severe acute respiratory syndrome coronavirus-2. The World Health Organization has declared COVID-19 as a public health emergency.[1,2,3,4] Currently, with the lack of approved pharmaceutical treatments or vaccines to cure this disease, there are many ongoing efforts to mitigate the spread of the virus (i.e., “flatten the curve”).[5,6] Governments across the world are struggling to control the spread of the virus by issuing severe restrictions, such as implementing social distancing, contact tracing, and quarantine, and adhering to the guidelines of safety and precautions provided by the health officials. But implementing such restrictive and large-scale procedures is a huge challenge.[7] Moreover, during this pandemic, health care facilities are looking for practical and cost-effective solutions for early detection, monitoring, and tracking of infected persons in the population who can be contagious (symptomatic or asymptomatic carriers).[8,9,10] It is thus highly desirable to develop a smarter and integrated virtual surveillance system to ensure effective COVID-19 control and to reduce the spread across the community.[11,12]
In recent years, Internet of Things (IoT) has received significant worldwide attention and has become ever more available for predicting, preventing, and monitoring infectious diseases.[6,13] In this context, IoT technology has been shown to be a safe and efficient way of dealing with the COVID-19 pandemic due to its ubiquitous sensing ability and seamless connectivity.[14] The IoT is an advanced technology that refers to an interconnected web of real objects, sensors, and appliances for sensing, compiling, processing, monitoring, and managing a variety of information of our daily life.[15,16] Besides, the reliable IoT networks provide timely crucial information that can help in taking timely decisions.[17,18] Health care can be identified as one of the major application domains for the IoT. Internet of Health Things is a health care–specific version of IoT that aims to connect patients to health care settings for real-time monitoring and control of their clinical features such as health status, activities, and vital signs.[19,20,21]
In this pandemic, IoT has the potential to deal with huge amounts of data received from sensors used by a number of applications to battle against COVID-19. Our goal in this study is to review the IoT-based solutions combating this pandemic according to the “Fit between Individuals, Task, and Technology” (FITT) framework for determining its target users, technological requirements, system tasks, and processes.
Evidence Acquisition
The FITT framework provides a theoretical foundation for this comprehensive systematic literature review (SLR), and data extraction was guided according this framework. FITT technology adoption model was presented by Ammenwerth et al.[22], which takes into account the system individuals, tasks, processes, and technologies. Our SLR is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standard guidelines, which describe the identification, screening, eligibility, and inclusion criteria of the articles that fall under the scope of review.[23]
Data sources and search strategy
An extensive SLR was performed using six scientific databases – PubMed, Google Scholar, Scopus, Web of Science, Science Direct, and ProQuest – from June 30 up to November 1, 2020. The following search terms were used (designed using English MeSH keywords and Emtree terms): [COVID-19 OR Novel coronavirus OR nCoV] AND [”Internet of Things” OR “Internet of Medical Things” OR “Internet of Health Things” OR “Medical Internet of Things” OR “IoT” OR “IoMT” OR “IoHT” OR “MIoT”]. After the adoption of advanced search option (search formula: combining key terms, search operators [AND and OR] and search fields: Title, Title/abstract and Topic) and applying the inclusion and exclusion criteria (via search filter or refine result), the titles and abstracts of potentially relevant studies were identified. Details of the search strategy are shown in Table 1.
Table 1.
Search syntax
| Databases | Search syntax |
|---|---|
| PubMed | ((((((COVID-19[Title]) OR (coronavirus[Title])) OR (n-CoV2[Title])) AND (Internet of Things [Title/Abstract])) OR (IoT [Title/Abstract])) OR (Internet of Health Things [Title/Abstract])) OR (IoHT [Title/Abstract]) OR (Medical Internet of Things [Title/Abstract])) AND LANGUAGE: (English), limited to 2020. |
| Google Scholar | allintitle: “COVID-19” OR “novel Coronavirus” OR “n-CoV2” AND “Internet of Things” OR “IoT” OR “Internet of Health Things” OR “IoHT” OR “Medical Internet of Things” AND English[lang], limited to 2020-01-01 to 2020-11-1. |
| Scopus | (TITLE (COVID-19) OR TITLE (novel Coronavirus) OR TITLE (n-CoV2) AND TITLE-ABS-KEY (Internet of Things) OR TITLE-ABS-KEY (IoT) OR TITLE-ABS-KEY (Internet of Health Things) OR TITLE-ABS-KEY (IoHT) OR TITLE-ABS- KEY (Medical Internet of Things) AND (LIMIT-TO (LANGUAGE, “English”) AND PUBLICATION YEARS: (2020)). |
| Web of Science | TITLE: (COVID-19) OR TITLE: (novel Coronavirus) OR TITLE: (n-CoV2) AND TOPIC: (Internet of Things) OR TOPIC: (IoT) OR TOPIC: (Internet of Health Things) OR TOPIC: (IoHT) OR TOPIC: (Medical Internet of Things). Refined by: LANGUAGES: (ENGLISH) AND PUBLICATION YEARS: (2020). |
| ProQuest | ti (COVID-19) OR ti (novel Coronavirus) OR ti (n-CoV2) AND ab (Internet of Things) OR ab (IoT) OR ab (Internet of Health Things) OR ab (IoHT) OR ab (Medical Internet of Things). Applied filter: time span: 2020-01-01 to 2020-11-1 AND English. |
| Science Direct | TITLE (“COVID-19” OR “novel Coronavirus” OR “n-CoV2”) AND TITLE-ABS-KEY (“Internet of Things” OR “IoT” OR “Internet of Health Things” OR “IoHT” OR “Medical Internet of Things”) AND English[lang], limited to 2020. |
Study selection
Some inclusion and exclusion criteria were determined for screening articles. Full-text articles were obtained for detailed evaluation, and eligible studies that used IoT solutions or strategies based on the FITT framework during the COVID-19 pandemic were included in the systematic review. Editorials, commentaries, conferences papers, case reports, duplicates, non-English papers, letters to editor, commentary papers, book chapters, short briefs, technical reports, and those published before the year 2020 were excluded. As COVID-19 is a rapidly evolving field, we included preprint literature.
Data extraction and quality assessment
To minimize bias, two reviewers (H: K-A and M: SH) participated independently through each phase of review and screened the titles and abstracts of articles according to predefined criteria. The authors screened the full-text reports and decided whether they met the inclusion criteria. Any vagueness during the study selection process was resolved by further discussion. The studies that met our predefined inclusion criteria were screened, and the studies that completely fulfilled our inclusion criteria were extracted for deeper analysis and data extraction.
Summarizing results
The results were organized based on IoT adoption models (FITT framework).
Results
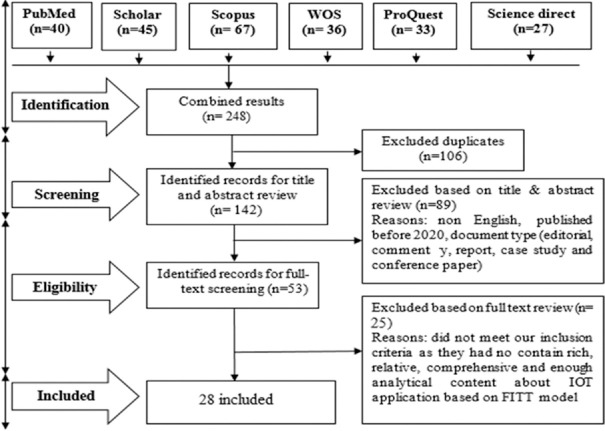
Characteristics of included studies
The initial search in scientific database yielded 248 citations; 142 of which remained after omitting the duplicates through the emerged endnote library (reference tools bar > find duplicates) and 53 of which remained after removing non-English, those published before 2020, and the document-type ones (editorial, commentary, report, case study, and conference paper). In the last screening phase, 28 articles were identified as eligible studies that met our criteria [Figure 1].
Figure 1.
PRISMA chart in the study selection process
Table 2 summarizes the general characteristics of the included studies based on author names, country, design and setting, and IoT digital services.
Table 2.
Summary of reviewed articles
| Reference | Country | Design and setting | IoT digital services |
|---|---|---|---|
| Xiao et al.[24] | China | Developmental | Smart real-time monitoring of physiological data |
| Wang et al.[25] | China | Developmental | Social relationships between mobile devices for geofencing |
| Moro Visconti et al.[26] | Italy | Literature review | Telesurveillance via digital public–private partnership |
| Vafea et al.[27] | USA | Review | Collaboration in the scientific community with open sharing of knowledge and expertise |
| Swayamsiddha et al.[19] | India | Literature review | Application of cognitive radio–based IoT for quarantine management and real-time monitoring |
| Siripongdee et al.[28] | Thailand | Literature review | Interaction, collaboration, and communication via blended learning technique |
| Pratap Singh et al.[29,30] | India | Review | IoMT-enabled remote tracking |
| Ye et al.[31] | China | Review | Real-time case detection and tracking through new health informatics |
| Rahman et al.[13] | USA | Review | Real-time surveillance, simultaneous reporting, and monitoring |
| Tripathy et al.[32] | USA | Developmental | Contact tracing over mobile phone location |
| Allam and Jones[18] | Australia | Prospective | Monitoring and management of diseases via open device connectivity |
| Adly et al.[33] | Egypt | Review | Self-quarantine and remote management and care for patients |
| Bai et al.[6] | China | Developmental | Medical IoT–aided diagnosis and treatment |
| Bayram et al.[34] | Turkey | Review | Public health decision and policy making using digital technologies |
| Ben Hassen et al.[35] | Tunisia | Developmental | Home telemonitoring (home telemetry) |
| Capobussi and Moja[36] | Italy | Review | Home telelaboratory and telemetry using IoT |
| Celesti et al.[37] | Italy | Developmental | Tele-medical laboratory |
| Chamola et al.[38] | India | Review | Remote thermometry and basic physiological data assessment |
| Chaudhari et al.[39] | India | Review | Real-time monitoring of the health parameters of patients and self-quarantine persons |
| Ting et al.[40] | Singapore | Review | Community-based real-time telemonitoring |
| Rehm et al.[41] | USA | Developmental | Tele-ICU monitoring of patient’s vital signs (biosensors) |
| Kumar Singh et al.[42] | India | Developmental | Telequarantine management |
| Yu et al.[43] | USA | Review | Spatiotemporal outbreak detection |
| Mohammed et al.[44] Praveena and Sruthi[45] | Malaysia | Developmental | Real-time early detection and tracking (biosensors) |
| Oyeniyi et al.[46] | Nigeria | Prospective | Improving medical decision accuracy and precision (decision supporting) |
| James et al.[47] | UK | Review | Real-time monitoring of mobility and lockdown assessment |
IoT=Internet of Things, IoMT=Internet of Medical Things, ICU=intensive care unit
All included studies are summarized in Table 3 based on the FITT model in three classes: Individual, Technology, and Task.
Table 3.
IoT-based FITT model to fight against COVID-19
| Reference | Individual | Technology | Task | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Platforms | Processing | Exchange | Storage | Added-value technologies | |||
| Xiao et al.[24] | Providers and patients | Wearable/portable devices | Decentralized applications and smart contract | WBAN | Cloud server and EHR | Combination of IoT and blockchain | Smart monitoring of the isolated persons (geofencing) |
| Wang et al.[25] | Epidemiologists, researchers, and IT vendors | Smartphone and wearable tools | Geospatial Processor System (GPS) | Wireless network signaling (Wi-Fi) | - | Big data analysis | Real-time telemonitoring |
| Moro Visconti et al.[26] | Patients and medical doctors | Digital kiosks and m-health apps | Spatial decision support system and deep learning | GSM | Interoperable cloud databases | Machine learning and blockchains | Real-time surveillance |
| Vafea et al.[27] | Researchers, scientists, and engineering | Biosensors, Nanotechnology, mobile apps | Mathematic and computational modeling | Wireless Bluetooth and radio-frequency technology | Central cloud server | Deep learning and big data analysis | Open sharing of knowledge and real-time telemonitoring |
| Swayamsiddha et al.[19] | Policy makers and city officials | Wearable biosensors | AI | 5G network, and Cognitive Radio Network | Local shared database | Blockchain and cloud computing | Remote and real-time tracking and surveillance |
| Siripongdee et al.[28] | Teachers and students | Narrowband IoT | AI | WSN, GSM | - | - | Web-based learning |
| Pratap Singh et al.[29,30] | Researchers, academicians, and scientists | Portable (mobile, wearable)/nonportable (e-kiosk) | Digital gadget, smart medicocare, and biosensors | Wireless Personal Area Network (e.g., Bluetooth) and internet) | Relational shared database | Cloud-based computing | Remote health monitoring and tracking, social distancing |
| Ye et al.[31] | Providers, patients, policy makers, IT vendors, third parties | m-health applications, wearable and portable devices | AI, in-depth mining | GSM | Personal Health Record | Drones, robots, and intelligent diagnoses | Real-time case detection and screening |
| Rahman et al.[13] | Public health and patients | m-health, social media and web-based tools | Intelligent systems | GSM | Personal smart card | Big data analysis | Predicting, preventing, and controlling |
| Tripathy et al.[32] | Society and policy makers | Telemetry based on wearable applications | Cloud computing | Wi-Fi, radiofrequencies | Centralized (state) database server | Cloud computing | Social distancing and telehealth |
| Allam and Jones[18] | Politicians, economists, providers, and patients | Mobile apps, wearable tools (thermal cameras) | AI and machine learning | Wireless Metropolitan Area Network | Cloud storage and local and central databases | AI and machine learning capabilities | Social distancing |
| Adly et al.[33] | Governments, researchers, and public health | Self-tracking devices and social media platforms | Biosensor processors | Wireless sensor network apps | EHR | Big data analysis and data mining | Social distancing and teletracking |
| Bai et al.[6] | Patients and providers | Intelligent Diagnosis and Treatment Assistant Program (nCapp) | RFID, GPS and core Graphics Processing Unit | GSM | Cloud base central data center | Cloud computing | Telemonitoring and tracking |
| Bayram et al.[34] | Society, scientists, and administrators | Wearable and implanted tools | Biosensors processors and AI | Worldwide interoperability for Microwave Access (WiMAX) | Local/central shared database | Big public health data analysis | Social distancing |
| Ben Hassen et al.[35] | Patients and health care providers | NodeMCU V3 platform | Biosensor processors | Zigbee Wireless Technology | NoSQL shared database | Fog/cloud computing | Home telemetry |
| Capobussi and Moja [36] | Family doctors and patients | Smartphones | - | Wi-Fi | - | Cloud computing and 3D printing | Real-time telemonitoring |
| Celesti et al.[37] | Laboratory specialists, medical doctors, and patients | Telehealthcare-based mobile phone and PDA technology using IoT | - | - | Mongo NoSQL DataBase | Blockchain engine and cloud computing | Telelaboratory or tele-medical laboratory service |
| Chamola et al.[38] | Public health authorities, researchers, and epidemiologists | Smart wearable and portable devices (thermometer) connected to cell phone for sharing and analysis using IoMT | Geofencing, GIS, GPS, voice detection and special phone base application softwares | 5G network and wireless technology | Decentralized databases (local end) and centralized databases (central end) | Unmanned Aerial Vehicles, blockchain, AI | Monitoring and tracking patients from a remote location |
| Chaudhari et al.[39] | Health care team, patients, and society | Smart phone, digital platforms, and biosensors in the bed of IoT | Biosensors, GPS, and RFID | GSM: 5G network | Cloud base database | Cloud base technologies | Real-time monitoring of self-quarantine, tracking the location |
| Ting et al.[40] | Public health agencies, government, researchers, and epidemiologists | Portable smart devices in the bed of IoT Worldometer platform | - | Next-generation telecommunication networks (e.g., 5G) and cloud base technology | - | Big data, blockchain, AI, and deep learning | Real-time tracking and monitoring of virus spread patterns |
| Rehm et al.[41] | Providers, patients, and health administrators | PDA or smartphones equipped with sensor | Biosensors | Bluetooth, Zigbee, and Wi-Fi, | Ventilator Waveform Database | ML algorithms | Telemonitoring |
| Kumar Singh et al.[42] | Patient and health authorities | Wearable devices with the bundled mobile app | GPS units | Bluetooth and internet connection | Cloud base database | - | Quarantine management, social distancing |
| Yu et al.[43] | Public health and city officials | Spatiotemporal event detection using health sensing technology | ML, image processing, statistical and probabilistic | WSN technology | Cloud base database | Cloud computing | Timely detection of events (disease outbreak) |
| Mohammed et al.[44] Praveena and Sruthi [45]] | Patients, providers, public health and city officials | Smart helmet | GPS module and Google Location History | RFID and Wi-Fi network | Biobanks | Big data, cloud computing, and telemedicine modules | Telemonitoring, remote tracking, and telehealth |
| Oyeniyi et al.[46] | Patients and physicians | Smartphone apps | CDSS | GSM | - | - | Contact tracing and case tracking |
| James et al.[47] | City officials, public health | Decision dashboard | ML and GPS | Wi-Fi | - | IoT sensors, and AI | Lockdown policy and social distancing |
IoT=Internet of Things, FITT=Fit between Individual, Task, and Technology, COVID-19=Coronavirus disease 2019, WBAN=Wireless body area networks, IoMT=Internet of Medical Things, IT=Information technology, m-health=Mobile health, GSM=Global System for Mobile Communications, AI=Artificial intelligence, WSN=Wireless sensor network, EHR=Electronic Health Record, RFID=Radio-frequency identification, PDA=Personal digital assistant, GIS=Geographical Information System, GPS=Global Positioning System, ML=Machine learning, CDSS=Clinical decision support system
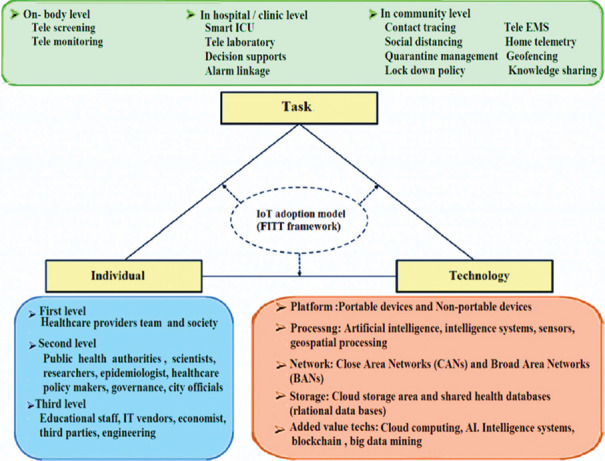
The analysis revealed that the IoT platforms that were used to fight against the COVID-19 pandemic were classified into three main sections as follows.
1. IoT individuals
Based on the findings of the “Individual” column in Table 3, IoT stakeholders are categorized into three classes according the degree of their interactions. In this regard, the main stakeholders of IoT for managing COVID-19 classified as first level include the health care providers[6,13,18,19,24,26,29,30,31,32,33,34,35,36,37,39,42,43,44,45,46] and society.[6,13,18,19,24,26,29,30,31,32,33,34,35,36,37,39,42,43,44,45,46] The next level of IoT stakeholders include public health authorities,[6,13,24,33,38,40,43,44,45,47] academicians, scientists, and researchers.[18,25,27,29,30,31,33,34,38,40] Finally, the third level includes educational staff,[28] IT (information technology) vendors,[25,31] economists,[18] third parties,[31] and engineering[25] [see Figure 2].
Figure 2.
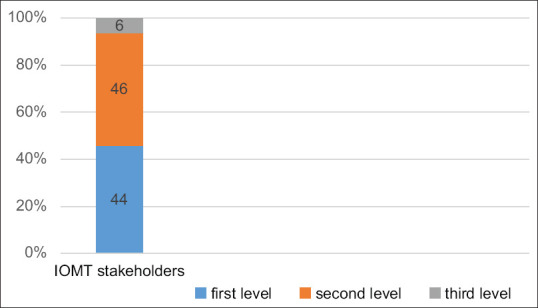
IoT-based COVID-19 stakeholders
2. IoT technologies
Technological requirements that used to establish IoT for COVID-19 management are classified into five classes, which include technical platform,[13,18,19,25,30,31,34,35,40,41,42,43,47,48,49,50] processing,[6,25,31,35,36,47,49,50,51] network,[6,25,35,49,50] storage,[6,18,19,25,31,34,36,37,46,48] and added-value technologies[19,27,34,36,40,41,42,47,51] [see Figure 3].
Figure 3.
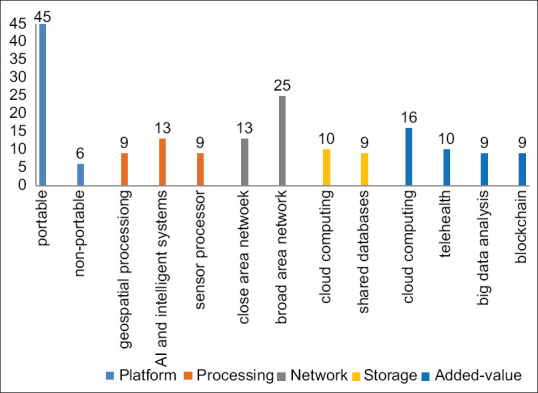
IoT-based COVID-19 technologies
Platform
Smart cell phones,[13,18,19,25,28,30,31,35,36,37,38,40,41,42,43,44,46,47,50,52] portable digital tools (e.g., microcomputers such as palmtop, tablet, notebook),[27,28,34,37,39,40,43,46,47] and wearable devices[13,18,19,25,30,31,34,35,41,42,43,40,47,48,49,50] are the most commonly used technological platforms in the IoT. But the application of nonportable technologies[25,36,39,41,42,45] was insignificant.
Processing
Application of location-aware technologies (e.g., GPS [Global Positioning Systems], GIS [Geographic Information Systems], remote sensing, and geofencing),[6,25,31,35,36,47,49,50,51] intelligence systems (CDSS [clinical decision support system] and decision dashboards),[13,28,44,52] artificial intelligence (AI) technologies (machine learning and deep learning),[18,19,36,37,39,43,44,45,51] and biosensor processors such as wearable or nonwearable technologies,[25,41,42,45,46] special sensor (voice, image, and facial processors)[47,48,49,50] are the well-known techniques in providing added-value capabilities for real-time tracking, online telemonitoring, effective identification, and decision supports.
Exchange (Network)
According to network application in different geographical areas, we categorized Wireless Field Connectors into two classes as follows:
Close Area Networks such as Bluetooth,[28,30,31,37,41,42] RFID (radio-frequency identification),[6,25,35,49,50] WBAN (wireless body area networks)[1] and Zigbee[28,46]
Broad Area Networks such as mobile technology (GSM [Global System for Mobile Communications] or 4G and 5G networks),[6,13,19,27,28,36,43,47,52] Wi-Fi,[13,28,30,35,38,47,49,50,51] WSN (wireless sensor network),[39,48] WiMAX (Worldwide Interoperability for Microwave Access),[12] and internet connection.[31,36,41,42]
Storage
Using cloud storage area[6,18,19,25,31,34,36,37,46,48] and shared health databases[18,19,30,40,41,42,45,46,47] for backup and permanent accessibility to data is compatible with IoT requirements during the COVID-19 pandemic.
Added-value technologies
The most prominent technologies to provide added value for IoT-based COVID-19 data processing, storage, and communication were cloud computing,[6,13,19,25,30,31,36,38,40,41,42,43,46,48,49,50] telehealth,[18,27,28,36,37,39,43,45,47,51] blockchain,[19,27,34,36,40,41,42,47,51] and big data mining.[13,27,35,37,43,44,45,49,50]
3. IoT tasks
The most important IoT tasks and use cases related to COVID-19 management in multiple “on-body,” “in-clinic/hospital,” and even “in-community” levels include real-time telemonitoring,[6,18,19,24,25,29,30,35,36,38,39,40,41,44,45] effective screening and surveillance programs,[13,19,26,31] case tracking or mobility tracing,[6,19,29,30,32,33,39,40,46] timely case identification,[31,43,44,45,46] self-quarantine and lockdown policy,[39,42,47] smart social distancing,[32,34] and smart contact tracing.[32,47] Other applications include remote education,[28] knowledge sharing,[27] and decision supports[41,46] [see Figure 4].
Figure 4.
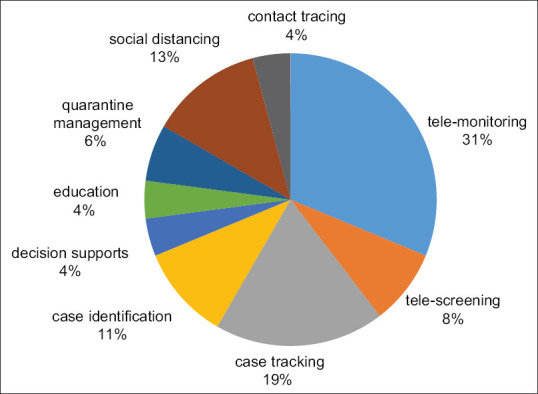
IoT-based COVID-19 tasks
The IoT adoption framework for COVID-19 management is shown in Figure 5.
Figure 5.
IoT adoption framework for COVID-19 management
Discussion
Currently, given the lack of definitive and effective treatment, as well as the increase in the number of infected cases and mortalities, social isolation and containment strategy have been the best preventive interventions to limit the disease transmission.[13,18,48] Therefore, there has been an increasing demand for adoption of innovative technologies. Accordingly, many governments and policy-making agencies have emphasized on adopting innovative solutions to tackle the current health crisis, which is leading to health care's digital revolution.[29,31,34,39,46,49] In this sense, “the smart public health surveillance” is a novel concept derived from adopting advanced technologies such as IoT, which uses an internet-like structure for the integration of heterogeneous “medical objects” to address real-time screening, epidemic tracing, case identification, quarantine management, decision support, and accurate predictions.[50,51,52] Furthermore, IoT, by providing digital contact tracing and case tracking capabilities, plays a crucial role in maintaining social distancing and implementing lockdown policies.[24,42]
In the present study, we review current literature about IoT-enabled platforms from technical requirements, expected system tasks, and target user aspects during the COVID-19 outbreak according to the FITT model. Integration of such interrelated technologies can help generate solutions within the health care sector for smart screening, prediction, and prevention of diseases.
Use of portable microcomputers, cell phones, and wearable devices equipped with wireless networks (e.g., Wi-Fi, Bluetooth, and GSM), along with added-value technologies such as new AI algorithms (e.g., machine learning and deep learning), cloud computing, and big data mining, leads to better adoption of IoT in the current and even future pandemics.[25,31] This study showed, applied to the current crisis, that IoT can be leveraged to help patients receive at-home timely monitoring and smart surveillance through mobile communications, internet connectivity, and other wireless technologies. It can also provide a comprehensive database and flexible data exchange infrastructure for governments, public health authorities, health care settings, and so on.[6,53] In addition, with regard to big data mining, there are various applications, including machine learning, deep learning, and geospatial processing, in which intelligent algorithms are used for decision making based on the data generated from IoT-enabled devices.[17,18,19,20] Moreover, this technology is also suitable to simultaneously capture the necessary physiological or geospatial data of the confirmed or suspected cases from various locations and manage the collected data in combination with GPS, AI algorithms, cloud computing, and intelligent and virtual management systems.[29,54,55]
This study also opens opportunities for health care industry in designing customized IoT-based solutions for real-time monitoring and tracking of current and probable future pandemics. However, our study also has some limitations. In future studies, with the increased usage of IoT-based smart surveillance systems, it is important to analyze the actual use of such systems in the form of longitudinal studies rather than as review or cross-sectional study. In addition, because of our search inclusion/exclusion criteria (IoT-based COVID-19 studies conducted in 2020), we may have missed some valuable studies in this field.
Conclusion
In this article, we reviewed the IoT-enabled solutions according to the FITT framework to better understand the IoT applications to tackle the COVID-19 pandemic.
As a concluding remark, the IoT-based portable devices equipped with wireless broadband networks that take advantage of added-value and innovative complementary technologies such as new AI algorithms, big data mining, geospatial processors, and cloud computing have been broadly used in public health surveillance. Future researches should focus on novel computational and telematics approaches especially in the field of public health big data mining, deep learning, 5G/6G networks, smart implants, robotics, blockchain, and so on. These innovation technologies could be applied to diminish the destructive effects of probable future pandemics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article is the result of a research project approved by the research committee at Abadan University of Medical Sciences, Iran (Ethic code number: IR.ABADANUMS.REC.1399.095).
References
- 1.Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi S, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int J Epidemiol. 2020;49:717–26. doi: 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Long C, Xu H, Shen Q, Zhang X, Fan B, Wang C, et al. Diagnosis of the Coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020;126:108961. doi: 10.1016/j.ejrad.2020.108961. doi: 10.1016/j.ejrad.2020.108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect Dis. 2020;20:425–34. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl Jof Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Papadopoulos T, Baltas KN, Balta ME. The use of digital technologies by small and medium enterprises during COVID-19: Implications for theory and practice. Int J Inf Manage. 2020:102192. doi: 10.1016/j.ijinfomgt.2020.102192. doi: 10.1016/j.ijinfomgt. 2020.102192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bai L, Yang D, Wang X, Tong L, Zhu X, Zhong N, et al. Chinese experts’ consensus on the internet of things-aided diagnosis and treatment of coronavirus disease 2019 (COVID-19) Clinical eHealth. 2020;3:7–15. [Google Scholar]
- 7.Nguyen CT, Saputra YM, Van Huynh N, Nguyen N-T, Khoa TV, Tuan BM, et al. A comprehensive survey of enabling and emerging technologies for social distancing—Part I: Fundamentals and enabling technologies. IEEE Access. 2020;8:153479–507. doi: 10.1109/ACCESS.2020.3018140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang T, Gentile M, Shen CF, Cheng CM. Combining point-of-care diagnostics and internet of medical things (IoMT) to combat the COVID-19 pandemic. Diagnostics (Basel) 2020;10:224. doi: 10.3390/diagnostics10040224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 2020;26:571–3. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 10.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 Pandemic and rapid implementation of adolescent and young adult telemedicine: Challenges and opportunities for innovation. J Adolesc Health. 2020;67:164–71. doi: 10.1016/j.jadohealth.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhardwaj K. Digital surveillance systems to combat COVID-19 may do more harm than good. Econ Polit Wkly. 2020;55 [Google Scholar]
- 12.Magee LA, Khalil A, Von Dadelszen P. Covid-19: UK Obstetric Surveillance System (UKOSS) study in context. BMJ. 2020;370:m2915. doi: 10.1136/bmj.m2915. doi: 10.1136/bmj.m2915. [DOI] [PubMed] [Google Scholar]
- 13.Rahman MS, Peeri NC, Shrestha N, Zaki R, Haque U, Ab Hamid SH. Defending against the novel coronavirus (COVID-19) outbreak: How can the internet of things (IoT) help to save the world? Health Policy Technol. 2020;9:136–8. doi: 10.1016/j.hlpt.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ketu S, Mishra PK. Enhanced Gaussian process regression-based forecasting model for COVID-19 outbreak and significance of IoT for its detection. Appl Intelligence. 2021;51:1492–512. doi: 10.1007/s10489-020-01889-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ashton K. That ’internet of things’ thing. RFID J. 2009;22:97–114. [Google Scholar]
- 16.Dong Y, Yao YD. IoT platform for COVID-19 prevention and control: A survey. Ieee Access. 2021;9:49929–41. doi: 10.1109/ACCESS.2021.3068276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kamal M, Aljohani A, Alanazi E. IoT meets COVID-19: Status, challenges, and opportunities. arXiv preprint arXiv:2007. 2020;12268 [Google Scholar]
- 18.Allam Z, Jones DS. On the coronavirus (COVID-19) outbreak and the smart city network: Universal data sharing standards coupled with artificial intelligence (AI) to benefit urban health monitoring and management. Healthcare (Basel) 2020;8:46. doi: 10.3390/healthcare8010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swayamsiddha S, Mohanty C. Application of cognitive internet of medical things for COVID-19 pandemic. Diabetes Metab Syndr. 2020;14:911–5. doi: 10.1016/j.dsx.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Song Y, Jiang J, Wang X, Yang D, Bai C. Prospect and application of Internet of Things technology for prevention of SARIs. Clinical eHealth. 2020;3:1–4. [Google Scholar]
- 21.Rodrigues JJ, Segundo DBDR, Junqueira HA, Sabino MH, Prince RM, Al-Muhtadi J, et al. Enabling technologies for the internet of health things. IEEE Access. 2018;6:13129–41. [Google Scholar]
- 22.Ammenwerth E, Iller C, Mahler C. IT-adoption and the interaction of task, technology and individuals: A fit framework and a case study. BMC Med Inform Dec Mak. 2006;6:3. doi: 10.1186/1472-6947-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Xiao C, Zheng L, Chen F, Xiao Y. Design and research of a smart monitoring system for 2019-nCoV infection-contact isolated people based on blockchain and Internet of things technology. 2020 [Google Scholar]
- 25.Wang B, Sun Y, Duong TQ, Nguyen LD, Hanzo L. Risk-aware identification of highly suspected COVID-19 cases in social IoT: A joint graph theory and reinforcement learning approach. IEEE Access. 2020;8:115655–61. doi: 10.1109/ACCESS.2020.3003750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moro Visconti R, Morea D. Healthcare digitalization and pay-for-performance incentives in smart hospital project financing. Int J Environ Res Public Health. 2020;17:2318. doi: 10.3390/ijerph17072318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vafea MT, Atalla E, Georgakas J, Shehadeh F, Mylona EK, Kalligeros M, Mylonakis E. Emerging Technologies for use in the study, diagnosis, and treatment of patients with COVID-19. Cell Mol Bioeng. 2020;13:1–9. doi: 10.1007/s12195-020-00629-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siripongdee K, Pimdee P, Tuntiwongwanich S. A blended learning model with IoT-based technology: Effectively used when the COVID-19 pandemic? J Educ Gift Young Sci. 2020;8:905–17. [Google Scholar]
- 29.Singh RP, Javaid M, Haleem A, Suman R. Internet of things (IoT) applications to fight against COVID-19 pandemic. Diabetes Metab Syndr. 2020;14:521–4. doi: 10.1016/j.dsx.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh RP, Javaid M, Haleem A, Vaishya R, Ali S. Internet of medical things (IoMT) for orthopaedic in COVID-19 pandemic: Roles, challenges, and applications. J Clin Orthop Trauma. 2020;11:713–7. doi: 10.1016/j.jcot.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ye J. The role of health technology and informatics in a global public health emergency: Practices and implications from the COVID-19 pandemic. JMIR Med Inform. 2020;8:e19866. doi: 10.2196/19866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tripathy AK, Mohapatra AG, Mohanty SP, Kougianos E, Joshi AM, Das G. EasyBand: A wearable for safety-aware mobility during pandemic outbreak. IEEE Consum Electron Mag. 2020;9:57–61. [Google Scholar]
- 33.Adly AS, Adly AS, Adly MS. Approaches Based on Artificial Intelligence and the Internet of Intelligent Things to Prevent the Spread of COVID-19: Scoping Review. J Med Internet Res. 2020;22:e19104. doi: 10.2196/19104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bayram M, Springer S, Garvey CK, Ázdemir V. COVID-19 Digital health innovation policy: A portal to alternative futures in the making. OMICS. 2020;24:460–9. doi: 10.1089/omi.2020.0089. [DOI] [PubMed] [Google Scholar]
- 35.Ben Hassen H, Ayari N, Hamdi B. A home hospitalization system based on the Internet of things, Fog computing and cloud computing. Inform Med Unlocked. 2020;20:100368. doi: 10.1016/j.imu.2020.100368. doi: 10.1016/j.imu. 2020.100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Capobussi M, Moja L. 3D printing technology and internet of things prototyping in family practice: Building pulse oximeters during COVID-19 pandemic. 3D Print Med. 2020;6:32. doi: 10.1186/s41205-020-00086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Celesti A, Ruggeri A, Fazio M, Galletta A, Villari M, Romano A. Blockchain-based healthcare workflow for tele-medical laboratory in federated hospital IoT clouds. Sensors. 2020;20:2590. doi: 10.3390/s20092590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chamola V, Hassija V, Gupta V, Guizani M. A comprehensive review of the COVID-19 pandemic and the role of IoT, drones, AI, blockchain, and 5G in managing its impact. IEEE Access. 2020;8:90225–65. [Google Scholar]
- 39.Chaudhari SN, Mene SP, Bora RM, Somavanshi KN. Role of internet of things (IOT) in pandemic Covid-19 condition. Int J Eng Res Appl. 2020;10:57–61. [Google Scholar]
- 40.Ting DSW, Carin L, Dzau V, Wong TY. Digital technology and COVID-19. Nat Med. 2020;26:459–61. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rehm GB, Woo SH, Chen XL, Kuhn BT, Cortes-Puch I, Anderson NR, et al. Leveraging IoTs and machine learning for patient diagnosis and ventilation management in the intensive care unit. IEEE Pervasive Comput. 2020;19:68–78. doi: 10.1109/MPRV.2020.2986767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singh VK, Chandna H, Kumar A, Kumar S, Upadhyay N, Utkarsh K. IoT-Q-Band: A low cost internet of things based wearable band to detect and track absconding COVID-19 quarantine subjects. EAI Endorsed Trans Internet Things. 2020;6 doi: 10.4108/eai. 13-7-2018163997. [Google Scholar]
- 43.Yu M, Bambacus M, Cervone G, Clarke K, Duffy D, Huang Q, et al. Spatiotemporal event detection: A review. Int J Digit Earth. 2020;13:1339–65. [Google Scholar]
- 44.Mohammed M, Hazairin NA, Al-Zubaidi S, AK S, Mustapha S, Yusuf E. Toward a novel design for coronavirus detection and diagnosis system using iot based drone technology. Int J Psychosoc Rehabilitation. 2020;24:2287–95. [Google Scholar]
- 45.Praveena G, Sruthi D. Novel covid-19 detection and diagnosis system using IOT based smart helmet. JAC J Compos Theory. 2020;13:457–65. [Google Scholar]
- 46.Oyeniyi J, Ogundoyin I, Oyeniran O, Omotosho L. Application of internet of things (IoT) to enhance the fight against COVID-19 pandemic. Int J Multi Sci Adv Technol. 2020;1:38–42. [Google Scholar]
- 47.James P, Das R, Jalosinska A, Smith L. Smart cities and a data-driven response to COVID-19. Dialogues Hum Geogr. 2020;2043820620934211 doi: 10.1177/2043820620934211. [Google Scholar]
- 48.Xing Y, Mo P, Xiao Y, Zhao O, Zhang Y, Wang F. Post-discharge surveillance and positive virus detection in two medical staff recovered from coronavirus disease 2019 (COVID-19), China, January to February 2020. Euro Surveill. 2020;25:2000191. doi: 10.2807/1560-7917.ES.2020.25.10.2000191. doi: 10.2807/1560-7917.ES.2020.25.10.2000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ndiaye M, Oyewobi SS, Abu-Mahfouz AM, Hancke GP, Kurien AM, Djouani K. IoT in the wake of COVID-19: A survey on contributions, challenges and evolution. IEEE Access. 2020;8:186821–39. doi: 10.1109/ACCESS.2020.3030090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang H, Kan C, Krall A, Finke D. Network modeling and Internet of things for smart and connected health systems—a case study for smart heart health monitoring and management. IISE Trans Healthc Syst Eng. 2020;10:159–7. [Google Scholar]
- 51.Kang M, Park E, Cho BH, Lee K-S. Recent patient health monitoring platforms incorporating internet of things-enabled smart devices. Int Neurourol J. 2018;22((Suppl 2)):S76. doi: 10.5213/inj.1836144.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sun G, Trung NV, Hiep PT, Ishibashi K, Matsui T. Visualisation of epidemiological map using an Internet of things infectious disease surveillance platform. Crit Care. 2020;24:400. doi: 10.1186/s13054-020-03132-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Joyia GJ, Liaqat RM, Farooq A, Rehman S. Internet of medical things (IOMT): Applications, benefits and future challenges in healthcare domain. J Commun. 2017;12:240–7. [Google Scholar]
- 54.Javaid M, Haleem A, Vaishya R, Bahl S, Suman R, Vaish A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab Syndr. 2020;14:419–22. doi: 10.1016/j.dsx.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kumar K, Kumar N, Shah R. Role of IoT to avoid spreading of COVID-19. Int J Intell Netw. 2020;1:32–5. [Google Scholar]