Abstract
Vietnamese are the largest Asian ethnic group in Houston, Texas; however, research on this population is scarce. To address this dearth of knowledge, we developed the Vietnamese Aging and Care Survey. The objective of the study was to explore the sociodemographic and health characteristics of Vietnamese adults aged 65 years and older (n = 132) and their family caregivers (n = 64). Adult-child caregivers (n = 41) were aged between 21 and 65 years old. The majority were married, working, female, and in good to excellent health. Spousal caregivers (n = 23) were between 57 and 82 years old, retired, female, and in fair to good health. Adult children received more caregiving-related help from others compared to spousal caregivers; however, they felt more caregiver burden, had more perceived stress, and were in challenging relationships with care recipients. Differences in life stages of adult-child versus spousal caregivers may contribute to these results. Implications are discussed.
Keywords: Vietnamese, caregiver, adult children, spousal caregiver, filial piety
Introduction
Vietnamese immigrants are the sixth largest foreign-born population in the United States (U.S.), accounting for almost two million people in 2017 (U.S. Census, 2017a). Prior to 1975, Vietnamese migration to the U.S. was virtually nonexistent. After the Fall of Saigon in 1975, Vietnamese refugees migrated to the U.S. in three distinct waves. The first wave consisted of 125,000 Vietnamese refugees who were military personnel, educated professionals, and their families affiliated with the U.S. military or the South Vietnamese government (Rkasnuam & Batalova, 2014). From 1977 to the mid-1980s, the second wave of 280,500 refugees fled from persecution due to their religion and Chinese ethnicity. They were from rural areas with limited skills and little or no formal education (Klineberg & Wu, 2013; Rkasnuam & Batalova, 2014) and mostly fled by boat, and thus, were referred to as “boat people.” The last wave occurred throughout the 1980s and 1990s. This group of 532,000 refugees had relatives in the U.S. already, were children of U.S. servicemen and their mothers, or political prisoners (Alperin & Batalova, 2018; Klineberg & Wu, 2013). During the 2000s, the Vietnamese population steadily increased from 988,000 in 2000 to 1,241,000 in 2010.
There are currently over 40 million unpaid family caregivers of adults aged 65 and older in the U.S. (National Center on Caregiving, 2016). Asian Americans and Pacific Islanders (AAPI) are almost twice more likely to be caregivers (42%) than the same age groups of general population (22%), and two-thirds of AAPI caregivers are immigrants (AARP, 2014). Immigrant caregivers tend to struggle in their caregiving in the U.S. because their caregiving practices and expectations are different from those of their home countries (Miyawaki, 2015, 2016). For example, filial piety – the cultural value of adult children’s allegiance to parents is strongly valued in traditional Asian cultures (Uba, 1994; Zane & Yeh, 2002) and is a part of Vietnamese culture as well (Yeo, Tran, Hikoyeda, & Hinton, 2002). Filial piety is characterized by respect, honor, fidelity, devotion, dutifulness, and sacrifice on the part of children for their parents (Chen, 1982). This sense of obligation or reciprocity may put some Asians (immigrants) and Asian American caregivers at greater risk for caregiver burden, stress, and depression (Meyer et al., 2015; Wang, 2012).
Despite their growing numbers, health studies on Vietnamese population are scarce (Kim et al., 2010; Sorkin, Tan, Hays, Mangione, & Ngo-Metzger, 2008; Torr & Walshi, 2018). Vietnamese immigrants who came to the U.S. as a result of the Vietnam War often faced trauma from experiencing the war, reeducation camps, long boat journeys, pirate attacks, or government capture (Gold, 1992). Trauma is known to impact all aspects of health and to have multi-generational impact (Bloch & Shirin, 2018). Post-immigration factors (i.e., socioeconomic status), as well as the actual process of asylum and immigration (i.e., insecure visa status), are correlated with poor mental health in refugees (Li, Liddell, & Nickerson, 2016). It has been 45 years since the first wave of Vietnamese migrated to the U.S. Even if they were young at the time of migration, many are now aged and may require assistance. Thus, it is critical to examine the health status of older Vietnamese and their caregivers who are their immediate and extended family members.
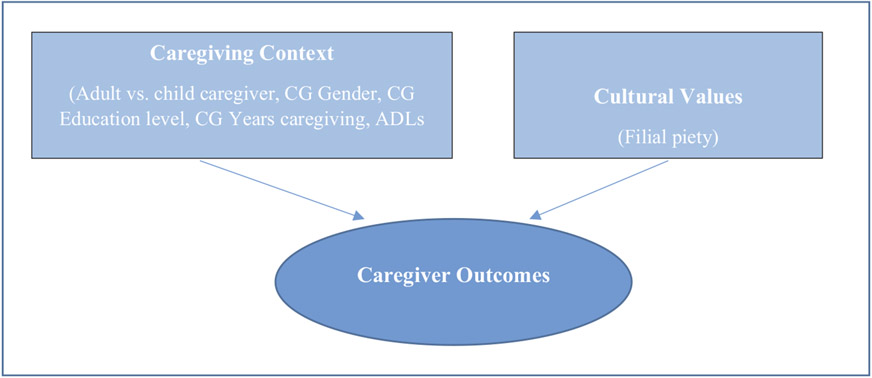
To fill this knowledge gap, we developed the Vietnamese Aging and Care Survey (VACS) and collected data on demographic and health information of Vietnamese older adults and their family caregivers in Houston, Texas. To our best knowledge, this is the first health survey exclusively focused on Vietnamese older adults and their caregivers in the U.S. Houston has the third largest Vietnamese population in the U.S. (U.S. Census Bureau, 2017b). In 2016, there were 81,000 Vietnamese in the greater Houston area, making Vietnamese the largest Asian ethnic group (von der Mehden, 2017). The purpose of this paper was to report the sociodemographic and health characteristics of Vietnamese family caregivers and similarities and differences between adult-child and spousal caregivers due to Vietnamese caregiving cultural expectation and its impact on caregiving. The conceptual model of the study is provided in Figure 1. Since there is dearth of information about the Vietnamese community, this study is vital to learn and better understand this rapidly growing, but understudied population.
Figure 1.
Conceptual model of caregiver outcomes.
Methods
Participants
Inclusion criteria for caregivers were (1) an adult-child (18 years and older) caring for her/his older parent(s), other relative(s) or friend(s) 65 years old or older, or a spousal caregiver caring for her/his spouse 65 years old or older; (2) self-identified as Vietnamese/Vietnamese American; (3) spoke English and/or Vietnamese; (4) had provided assistance with care recipients’ activities of daily living (ADLs) and instrumental activities of daily living (IADLs) for at least 6 months; (5) and lived in Houston, Texas at the time of caregiving.
Data were collected in November 2017 and April–May 2018. The principal investigator (PI) originally approached Executive Directors of Vietnamese social service agencies, introduced the project, and secured their support. Through the introduction from these agencies, bilingual community gatekeepers assisted the PI to connect with Vietnamese community organizations (e.g., senior residential facilities, adult daycare centers). Bilingual/bicultural Vietnamese research assistants (RAs) were hired to visit each center with the PI. Written informed consent was obtained from participants before conducting the interviews. Surveys were filled out by the participants themselves and/or conducted by RAs in Vietnamese if the participants were unable to do it by themselves. This study was approved by the PI’s university Institutional Review Board.
Measures
Modeled after the questionnaire design of the Hispanic Established Populations for Epidemiologic Studies of the Elderly (Markides, Chen, Angel, Palmer, & Graham, 2016), the Vietnamese Aging and Care Survey (VACS) was developed for Vietnamese older adults (care recipients) and their family caregivers (adult-child and spousal caregivers) as a pilot study. We formed a Vietnamese Community External Advisory Board of five Vietnamese professionals (two social workers, therapist, mental health counselor, and high school teacher) with whom we shared drafts of the VACS caregiver and care recipient surveys. We discussed the cultural appropriateness, required literacy level for each instrument, order and length of the survey, and participant fatigue in completing the survey. After their input and several revisions, the final versions of the VACS were developed. They were translated by a bilingual Vietnamese high school teacher and back-translated by a bilingual Vietnamese research scientist. Three versions of the VACS surveys targeted the: (1) care recipient; (2) adult-child caregiver; and (3) spousal caregiver survey. The VACS caregiver survey includes questionnaires on sociodemographic background, caregiving context variables, caregiver health and mental health, stress, social support, family interactions, care recipients’ health and disability, social services use, and adult children’s sense of filial responsibility.
Caregiver burden
The Zarit Burden Interview (Bédard et al., 2001), a 12-item 5-point Likert scale with scores ranging from 0 to 48, was used. Higher scores indicate more burden. Cronbach’s alpha was 0.94 in this study.
Perceived stress
We used a four-item scale to assess caregiver’s perceived stress (Cohen, Kamarck, & Mermelstein, 1983). Scores range from 0 (no stress) to 16 (high stress). In our sample, Cronbach’s alpha was 0.72.
Negative interactions with family
Caregiver’s negative interactions with family members were measured by a three-item 4-point Likert scale with higher scores indicating more positive interactions (scores between 3 and 12). This scale was modified from the original survey: The National Survey of American Life (Jackson et al., 2004) with questions about caregivers’ family members: “make too many demands on you,” “criticize you and the things you do,” and “try to take advantage of you.” In our sample, Cronbach’s alpha was 0.85.
Positive aspects of caregiving
Tarlow et al. (2004) Positive Aspects of Caregiving scale was used to measure the caregivers’ positive experiences. It is a nine-item 5-point Likert scale with Cronbach’s alpha of 0.98 in this study. Higher scores indicate a more positive caregiving experience with scores ranging from 9 to 45.
Relationship quality
The caregivers’ relationship quality with their care recipients was assessed by four questions from the National Study of Caregiving (2007), Round 7, Aspect of Caregiving questions. It consists of four items with 4-point Likert scale with higher scores indicating higher-quality relationships with a range of 0 to 12. Questions are, “How much do you enjoy being with your care recipient?” “How much does your care recipient argue with you?” “How much does your care recipient appreciate what you do for him/her?” and “How often does your care recipient get on your nerves?” In our sample, Cronbach’s alpha was 0.75.
Filial piety
Adult children’s sense of filial piety was assessed with the Filial Value Index (Jones, Lee, & Zhang, 2011). It is a 12-item, 9-point Likert scale with scores ranging from 1 (strongly disagree) to 9 (strongly agree). The total score is divided by 12 to get the final score, and higher scores indicate a stronger sense of filial piety. There are three factors in the instrument: sense of care, sense of responsibility, and sense of respect. In our sample of adult-child caregivers, Cronbach’s alpha was 0.86.
Statistical analysis
We used descriptive statistics to present caregiver information. To further examine the relationship between sociodemographic status and caregivers’ psychological outcomes, separate multivariable linear regression analyses were performed. The corresponding assumptions on linear regression analyses were inspected through residual analyses. All tests of statistical significance were two-sided with significance level, 0.05. Analyses were done using SAS v.9.4.
Results
Table 1 shows the sociodemographic characteristics of caregivers. Adult-child caregivers (n = 41) were aged 21 to 65 (Mean = 45.4) with an average education of 11 years. The majority were married (68%), employed (90%), female (61%), and in good (34%) or excellent (56%) health. The majority (95%) were born in Vietnam and immigrated to the U.S. at an average age of 23 (range: 1 to 46 years). Although five of them (12%) had no formal education, many attended up to high school (46%) and some had more than a high school education (34%) in Vietnam. Annual household income was at the $25,000-$50,000 level (58%). Spousal caregivers (n = 23) were between 57 and 82 years old (Mean = 70.6) and had an average of 8 years of education. Most were retired (74%), female (78%), and reported fair (48%) or good (35%) health. All of them were born in Vietnam and immigrated to the U.S. on average at age 44 (range: 20 to 68 years). Their education levels were mostly less than 6 years of formal education (43%) or high school or higher (57%). For the majority, annual household income was less than $25,000 (83%).
Table 1.
Sociodemographic characteristics of caregivers.
| Number of Caregivers | All Caregivers M ± SD, N (%) N = 64 |
Adult-Child Caregivers M ± SD, n (%) n = 41 |
Spousal Caregivers M ± SD, n (%) n = 23 |
p-Value |
|---|---|---|---|---|
| Age (year) | 54.4 ± 15.1 | 45.4 ± 9.9 | 70.6 ± 6.8 | < 0.001 |
| Gender | ||||
| Female | 43 (67.2%) | 25 (61.0%) | 18 (78.3%) | 0.16 |
| Male | 21 (32.8%) | 16 (39.0%) | 5 (21.7%) | |
| Marital Status | ||||
| Married | 51 (79.7%) | 28 (68.3%) | 23 (100.0%) | 0.002 |
| Not Married | 13 (20.3%) | 13 (31.7%) | 0 (0.0%) | |
| Nativity | ||||
| U.S.-Born | 2 (3.1%) | 2 (4.9%) | 0 (0.0%) | 0.53 |
| Vietnam-Born | 62 (96.9%) | 39 (95.1%) | 23 (100.0%) | |
| Age of Immigration (n = 62) | 31.0 ± 15.6 | 23.3 ± 11.4 | 44.1 ± 12.8 | < 0.001 |
| Education (year) | 10.1 ± 6.2 | 11.2 ± 5.8 | 8.2 ± 6.5 | 0.11 |
| Education | ||||
| 0 year | 11 (17.2%) | 5 (12.2%) | 6 (26.1%) | 0.25 |
| 1 to 6 years | 7 (10.9%) | 3 (7.3%) | 4 (17.4%) | |
| 9+ to 12 years | 27 (42.2%) | 19 (46.3%) | 8 (34.8%) | |
| > 12 years | 19 (29.7%) | 14 (34.2%) | 5 (21.7%) | |
| Employment | ||||
| Yes | 43 (67.2%) | 37 (90.2%) | 6 (26.1%) | < 0.001 |
| No | 21 (32.8%) | 4 (9.8%) | 17 (73.9%) | |
| Overall Health | ||||
| Excellent | 26 (40.6%) | 23 (56.1%) | 3 (13.0%) | < 0.001 |
| Good | 22 (34.4%) | 14 (34.1%) | 8 (34.8%) | |
| Fair | 15 (23.4%) | 4 (9.8%) | 11 (47.8%) | |
| Poor | 1 (1.6%) | 0 (0.0%) | 1 (4.4%) | |
| Household Income | ||||
| < $25,000 | 25 (39.7%) | 6 (15.0%) | 19 (82.6%) | < 0.001 |
| $25,000 to $50,000 | 26 (42.3%) | 23 (57.5%) | 3 (13.0%) | |
| $50,000 to $75,000 | 7 (11.1%) | 7 (17.5%) | 0 (0.0%) | |
| > $75,000 | 5 (7.9%) | 4 (10.0%) | 1 (4.4%) | |
| Overall Health | ||||
| Excellent | 26 (40.6%) | 23 (56.1%) | 3 (13.0%) | < 0.001 |
| Good | 22 (34.4%) | 14 (34.1%) | 8 (34.8%) | |
| Fair | 15 (23.4%) | 4 (9.8%) | 11 (47.8%) | |
| Poor | 1 (1.6%) | 0 (0.0%) | 1 (4.4%) | |
| Language at home | ||||
| Vietnamese | 58 (92.1%) | 37 (92.5%) | 21 (91.3%) | 1.00 |
| Vietnamese & English | 5 (7.9%) | 3 (7.5%) | 2 (8.7%) |
M = mean; SD = standard deviation.
Table 2 presents adult-child and spousal caregivers’ psychological characteristics. Overall, similar positive patterns emerged. Overall mean scores were relatively low for caregiver burden (Mean = 6.3) and perceived stress (Mean = 2.8). Results indicated high relationship quality with the care recipient (Mean = 9.7), and high scores on positive aspects of caregiving (Mean = 37.9). Adult children reported a high level of filial piety (Mean = 8.6). However, adult children felt close to twice the amount of caregiver burden (Mean = 7.1) compared to spousal caregivers (Mean = 4.9) (p = .05) and experienced more stress (Mean = 3.1) than spousal caregivers (Mean = 2.3) (p = .17). Adult children’s interactions with care recipients were not as positive (Mean = 10.2) as those of spousal caregivers (Mean = 10.7) (p = .08), feeling too many demands from their family member fairly to very often (15%) compared to spousal caregivers (13%) (p = .07). Spouses’ positive aspects of caregiving scale showed high rates of positive answers as well: [“agree a little” to “agree a lot”] in between 87% and 94% (data not shown).
Table 2.
Psychological characteristics of caregivers (CG).
| All M ± SD | Adult-Child CG M ± SD |
Spouse CG M ± SD |
p-Value | |
|---|---|---|---|---|
| Number of Caregivers | N = 64 | n = 41 | n = 23 | |
| Caregiver Burden | 6.3 ± 7.1 | 7.1 ± 7.1 | 4.9 ± 6.9 | 0.05 |
| Perceived Stress | 2.8 ± 3.0 | 3.1 ± 3.0 | 2.3 ± 3.0 | 0.17 |
| Negative Interactions with Family | 10.4 ± 2.1 | 10.2 ± 1.9 | 10.7 ± 2.3 | 0.08 |
| Positive Aspects of Caregiving | 37.9 ± 7.7 | 37.6 ± 7.3 | 38.3 ± 8.4 | 0.62 |
| Relationship Quality | 9.7 ± 2.3 | 9.5 ± 2.4 | 10.1 ± 2.1 | 0.41 |
| Filial Piety | – | 8.6 ± 0.5 | – | – |
M = mean; SD = standard deviation.
In regards to caregiving-related characteristics (Table 3), length of caregiving was similar: adult children reported an average of 6.4 years while spousal caregivers reported 7.2 years. Adult children lived with their care recipients (64%) or in close distance (within 2–8 blocks) (23%) whereas 100% of spousal caregivers lived with their care recipients. Adult children had more people who can help with caregiving (46%) than spousal caregivers (26%) (p = .18). The majority of adult children cared for their own parents (85%) but some cared for other relatives such as their uncle/aunt (n = 2) and grandparent (n = 2) (15%) because some care recipients utilized their Medicaid benefits to hire their family members to care for them. Caregivers provided an average of two ADL assistance to their care recipients. Dressing was the most frequently provided help for adult children (34%) followed by bathing (29%) while spousal caregivers tended to provide heavier ADL help such as bathing (44%) and dressing and transferring help in getting in and out of bed or chair (39% each).
Table 3.
Caregiving-related characteristics.
| Number of Caregivers | All M ± SD, N (%) N = 64 |
Adult-Child Caregiver M ± SD, n (%) n = 41 |
Spousal Caregiver M ± SD, n (%) n = 23 |
p-Value |
|---|---|---|---|---|
| Length of Caregiving (year) | 6.7 ± 7.2 | 6.4 ± 4.7 | 7.2 ± 10.5 | 0.34 |
| Availability of Other Caregivers (Yes) | 25 (39.1%) | 19 (46.3%) | 6 (26.1%) | 0.18 |
| Relationship with Care Recipients | ||||
| Spouse | 23 (36.5%) | 0 (0.0%) | 23 (100.0%) | < 0.001 |
| Adult-child | 34 (54.0%) | 34 (85.0%) | 0 (0.0%) | |
| Other relatives | 6 (9.5%) | 6 (15.0%) | 0 (0.0%) | |
| Living Arrangements | ||||
| With care recipient | 48 (77.4%) | 25 (64.1%) | 23 (100%) | 0.002 |
| Nearby (2–8 blocks) | 9 (14.5%) | 9 (23.1%) | 0 (0.0%) | |
| Other city | 5 (8.1%) | 5 (12.8%) | 0 (0.0%) | |
| ADL Help of Care Recipients Reported by Caregivers |
||||
| Walking | 19 (29.7%) | 11 (26.8%) | 8 (34.8%) | 0.57 |
| Bathing | 22 (34.4%) | 12 (29.3%) | 10 (43.5%) | 0.28 |
| Grooming | 18 (28.1%) | 10 (24.4%) | 8 (34.8%) | 0.40 |
| Dressing | 23 (35.9%) | 14 (34.1%) | 9 (39.1%) | 0.79 |
| Eating | 18 (28.1%) | 11 (26.8%) | 7 (30.4%) | 0.78 |
| Transferring | 19 (29.7%) | 10 (24.4%) | 9 (39.1%) | 0.26 |
| Toileting | 18 (28.1%) | 11 (26.8%) | 7 (30.4%) | 0.78 |
| Any ADL Help Needed | 34 (53.1%) | 21 (51.2%) | 13 (56.5%) | 0.79 |
| Number of ADL Help Needed | 2.1 ± 2.6 | 1.9 ± 2.5 | 2.5 ± 2.8 | 0.46 |
M = mean; SD = standard deviation.
Table 4 presents the association between caregivers’ characteristics and their psychological outcomes performed by multivariable regression analyses. More education years was positively associated with caregiver burden (b = 0.45, p = .004) and perceived stress (b = 0.15, p = .02), as well as with more negative family interactions (b = −0.10, p = .02) and lower relationship quality with the care recipients (b = −0.14, p = .007). Length of time caregiving was positively associated with perceived stress (b = 0.12, p = .02) and with more challenging interactions with family members (b = −0.15, p < .001). Similarly, more ADL help was associated with more perceived stress (b = 0.34, p = .02) and negative interactions (b = −0.22, p = .02).
Table 4.
Multivariable regression analyses on psychological outcomes of all caregivers (CG) (N = 64).*
| Caregiving Burden |
Perceived Stress |
Negative Interactions with Family |
Relationship Quality with Care Recipients |
|||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Estimate (b) | p-Value | Estimate (b) | p-Value | Estimate (b) | p-Value | Estimate (b) | p-Value |
| Caregiver Type (ref. spousal CG) | ||||||||
| Adult-Child CG | 1.04 | 0.56 | 0.66 | 0.39 | −0.54 | 0.27 | −0.13 | 0.83 |
| Gender (ref. male) | ||||||||
| Female | −1.21 | 0.53 | −0.37 | 0.66 | −0.08 | 0.88 | 0.01 | 0.99 |
| Education (years) | 0.45 | 0.004 | 0.15 | 0.02 | −0.10 | 0.02 | −0.14 | 0.007 |
| Length of Caregiving (years) | 0.15 | 0.22 | 0.12 | 0.02 | −0.15 | < 0.001 | 0.004 | 0.91 |
| Number of ADL Help Needed | 0.53 | 0.13 | 0.34 | 0.02 | −0.22 | 0.02 | 0.07 | 0.52 |
The type of caregivers and caregiver’s age were highly correlated. To avoid collinearity on regression analyses, only the type of caregivers was included.
Discussion
We developed the Vietnamese Aging and Care Survey (VACS) specifically for older Vietnamese and their caregivers, and this paper reports the very first results of the data on caregivers’ sociodemographic, health, and caregiving-related characteristics in Houston, Texas. There have been a couple of qualitative studies conducted with Vietnamese dementia caregivers in California, and these studies found poor mental health due to caregiving stress, stigma around dementia, and filial obligation as caregivers (Bui, Han, & Diwan, 2018; Lee & Casado, 2017; Meyer et al., 2015, 2018a; Park et al., 2018). Similar to these studies, our caregivers performed their duties within a tight-knit family network, adopting cultural expectations that caring for older family members is the younger generation’s responsibility. This filial piety is ingrained in family caregivers from a young age and embedded in Vietnamese culture (Lee & Casado, 2017; Meyer et al., 2015, 2018a; Park et al., 2018; Tran & Hinton, 2010). Not practicing filial obligation can result in the family losing face in the Vietnamese community (Tran & Hinton, 2010). This cultural practice may have influenced survey responses as the majority of our caregivers reported low burden and stress. However, compared to spousal caregivers, adult-child caregivers felt more burden and stress. This could be due to the stage of their lives, as 90% of adult-child caregivers were currently working while only 26% of spousal caregivers were employed. Adult children tend to have more stress because they are fulfilling multiple competing demands. In addition, adult children’s strong sense of filial piety to perform their caregiving duties and satisfy their parents’ caregiving expectations as their sons and daughters (Liu, Wu, & Dong, 2019; Miyawaki, 2015) and the level of acculturation (Meyer et al., 2015, 2018a) could contribute to greater stress and burden. At the same time, they also have to adjust their lifestyle to a new country and learn the new healthcare systems. These adjustments are challenging, especially when they are supporting their families while maintaining Vietnamese traditional caregiving practices (Miyawaki, 2015; Strumphf, Glicksman, Goldberg-Glen, Fox, & Logue, 2001).
Regression analyses showed that more educated caregivers reported higher psychological distress than their less educated counterparts. A similar pattern was reported by Meyer, Liu, Nguyen, Hinton, and Tancredi (2018b) that Asian Americans, including Vietnamese, with high educational attainment, reported more caregiving distress while more educated white caregivers showed less psychological distress from caregiving. A possible reason could be that more educated Vietnamese caregivers were more aware of their own psychological health and willing to report distress compared to those with less education (Meyer et al., 2018b). This also could be associated with their employment status. More educated caregivers may have more highly demanding jobs. In this study, as the vast majority of adult-child caregivers (90%) were employed at the time of survey, the younger generation (i.e., adult children) tended to have more education. Further investigation is warranted.
Limitations of the study
Some study limitations need to be stated. Data are based on a small purposive and convenience sample from Vietnamese residential facilities, senior centers, and an adult daycare center limited to Houston, Texas, and this bias might skew the results toward those who are highly connected to Vietnamese communities. Moreover, much of the sample lived in a multi-generation household, and that maybe one of the major reasons for helping and supporting each other without seeking outside help (Pishori, 2018; Torr & Walshi, 2018). Future research should include a more diverse Vietnamese sample such as those who may not be connected to Vietnamese communities and who are more acculturated Vietnamese Americans. Previous studies frequently discussed issues of religion and spiritual support in caregiving practices as religion is an important part of Vietnamese people’s lives, especially the prominence of prayer to cope with caregiving challenges (Meyer et al., 2015; Yeo et al., 2002). Although we surveyed at one church with a small number of participants, there were no specific questions regarding religion except one question in the filial piety index. Since the vast majority of Vietnamese people participate in religious services (Jarvis, Kirmayer, Weinfeld, & Lasry, 2005; Min & Jang, 2015), we should consider including questions about their religious affiliations so that we will have a better understanding of their caregiving behaviors and support systems.
Conclusion and implications
Despite limitations, this study was the first pilot health and mental health survey of Vietnamese caregivers of older adults in Houston, Texas and has added new knowledge base to the literature. Vietnamese caregivers are trying to meet their loved ones’ health needs in a new country while learning a new language under new health-care systems. Living in a multi-generational household and hiring their family members as paid caregivers while other family members work outside the home may alleviate their financial burden and provide psychological support. These findings have implications for health-care professionals, especially social workers who have direct access to and contact with Vietnamese families, to develop new approaches to encourage caregivers to utilize available social services to further ease their transition into caregiving and the caregiving experience itself. Interdisciplinary collaboration among helping professionals such as social workers, religious sectors, educators, and healthcare is critical in designing preventive measures and treatment programs. Bilingual and bicultural social workers, as well as culturally and linguistically appropriate social services, are in immediate need. Social workers can educate adult-child caregivers who are juggling multiple jobs and caregiving responsibilities and introduce adult day programs. Spousal caregivers can enjoy their religious activities while their spouses are attending adult day care activities so that both caregivers and care recipients can socialize and maintain their quality of life. One of the strengths of this study includes the assessment of positive aspects of caregiving. Social workers can utilize this information to better understand caregivers’ strengths and empower them in their caregiving efforts.
References
- Alperin E, & Batalova J (2018). Vietnamese people in the United States. Migration Information Source. Retrieved from https://www.migrationpolicy.org/article/vietnamese-immigrants-united-states-5 [Google Scholar]
- American Association of Retired Persons (AARP) Research Center. (2014). Caregiving among Asian Americans and Pacific Islanders age 50+. Retrieved from https://www.aarp.org/content/dam/aarp/research/surveys_statistics/general/2014/caregiving-among-asian-americans-and-pacific-islanders-age-50-plus.doi.10.26419%252Fres.00092.001.pdf [Google Scholar]
- Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, & O’Donnell M (2001). The Zarit Burden Interview: A new short version and screening version. The Gerontologist, 41, 652–657. doi: 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- Bloch A, & Shirin H (2018). Inter-generational transnationalism: The impact of refugee backgrounds on second generation. Comparative Migration Studies, 6, 3. doi: 10.1186/s40878-018-0096-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bui QN, Han M, & Diwan DT (2018). Vietnamese-American family caregivers of persons with mental illness: Exploring caregiving experience in cultural context. Transcultural Psychiatry, 55, 846–865. doi: 10.1177/1363461518793185 [DOI] [PubMed] [Google Scholar]
- Chen PN (1982). Eroding filial piety and its implications for social work practice. Journal of Sociology & Social Welfare, 9, 511–523. [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Gold SJ (1992). The employment potential of refugee entrepreneurship Soviet Jews and Vietnamese in California. Review of Policy Research, 11(2), 176–186. doi: 10.1111/j.1541-1338.1992.tb00400.x [DOI] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, & Williams DR (2004). The National Survey of American Life: A study of racial, ethnic, and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research, 13, 196–207. doi: 10.1002/(ISSN)1557-0657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvis GE, Kirmayer LJ, Weinfeld M, & Lasry J-C (2005). Religious practice and psychological distress: The importance of gender, ethnicity and immigrant status. Transcultural Psychiatry, 42(4), 657–675. doi: 10.1177/1363461505058921 [DOI] [PubMed] [Google Scholar]
- Jones PS, Lee JW, & Zhang XE (2011). Clarifying and measuring filial concepts across five cultural groups. Research in Nursing & Health, 34, 310–326. doi: 10.1002/nur.20444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim G, Chiriboga DA, Jang Y, Lee S, Huang C-H, & Parmelee P (2010). Health status of older Asian Americans in California. Journal of American Geriatric Society, 58, 2003–2008. doi: 10.1111/j.1532-1415.2010.03034.x [DOI] [PubMed] [Google Scholar]
- Klineberg SL, & Wu J (2013). Diversity and transformation among Asians in Houston: Findings from the Kinder Institute’s Houston Area Asian Survey (1995, 2002, 2011). Retrieved from https://kinder.rice.edu/sites/g/files/bxs1676/f/documents/Kinder%20Institute%20Houston%20Area%20Asian%20Survey_0.pdf [Google Scholar]
- Lee SE, & Casado BL (2019). Knowledge of Alzheimer’s disease among Vietnamese Americans and correlates of their knowledge about Alzheimer’s disease. Dementia, 18(2), 713–724. doi: 10.1177/1471301217691616 [DOI] [PubMed] [Google Scholar]
- Li SS, Liddell BJ, & Nickerson A (2016). The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Current Psychiatry Reports, 18 (9), 82. doi: 10.1007/s11920-016-0723-0 [DOI] [PubMed] [Google Scholar]
- Liu J, Wu B, & Dong X (2019). Psychological well-being of Chinese immigrant adult-child caregivers: How do filial expectation, self-rated filial performance, and filial discrepancy matter? Aging and Mental Health, 1–8. doi: 10.1080/13607863.2018.1544210 [DOI] [PubMed] [Google Scholar]
- Markides K, Chen N-W, Angel R, Palmer R, & Graham J (2016). Hispanic established populations for the epidemiologic study of the elderly (HEPESE) Wave 7, 2010-2011 [Arizona, California, Colorado, New Mexico, and Texas]. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; [distributor]. doi: 10.3886/ICPSR36537.v2 [DOI] [Google Scholar]
- Meyer OL, Fukurai M, Ho J, Limtiaco P, Nguyen HH, Dang J, & Hinton L (2018a). Dementia caregiver intervention development and adaptation in the Vietnamese American community: A qualitative study. Dementia. doi: 10.1177/147130218792704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer OL, Liu X, Nguyen T-N, Hinton L, & Tancredi D (2018b). Psychological distress of ethnically diverse adult caregivers in the California Health Interview Survey. Journal of Immigrant and Minority Health, 20, 784–791. doi: 10.1007/s10903-017-0634-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer OL, Nguyen KH, Dao TN, Vu P, Arean P, & Hinton L (2015). The sociocultural context of caregiving experiences for Vietnamese dementia family caregivers. Asian American Journal of Psychology, 6, 263–272. doi: 10.1037/aap0000024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min PG, & Jang SH (2015). The diversity of Asian immigrants’ participation in religious institutions in the United States. Sociology of Religion, 76(3), 253–274. doi: 10.1093/socrel/srv025 [DOI] [Google Scholar]
- Miyawaki CE (2015). A review of ethnicity, culture, and acculturation among Asian caregivers of older adults (2000-2012). SAGE Open, 5(1), 1–18. doi: 10.1177/2158244014566365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyawaki CE (2016). Caregiving practice patterns of Asian, Hispanic, and non-Hispanic White American family caregivers of older adults across generations. Journal of Cross-Cultural Gerontology, 31(1), 35–55. doi: 10.1007/s10823-016-9281-5 [DOI] [PubMed] [Google Scholar]
- National Center on Caregiving (2016). Caregiver statistics: Demographics. Family Caregiver Alliance. Retrieved from https://www.caregiver.org/caregiver-statistics-demographics [Google Scholar]
- National Study of Caregiving (NSOC). (2007). National Study of Caregiving Round 7 data collection instrument section. Retrieved from https://www.nhats.org/scripts/instruments/All_NSOC_Round7_Data_Collection_Instrument_Sections.pdf [Google Scholar]
- Pishori AZ (2018). The impact of stigmatized identities and culture on the mental health of East and South Asian Americans (Doctoral Dissertations). Paper 836. [Google Scholar]
- Rkasnuam H, & Batalova J (2014). Vietnamese immigrants in the United States. Migration Information Source. Retrieved from https://www.migrationpolicy.org/article/vietnamese-immigrants-united-states-2 [Google Scholar]
- Sorkin D, Tan AL, Hays RD, Mangione CM, & Ngo-Metzger Q (2008). Self-reported health status of Vietnamese and non-Hispanic white older adults in California. Journal of the American Geriatrics Society, 56, 1543–1548. doi: 10.1111/j.1532-5415.2008.01805.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strumphf NE, Glicksman A, Goldberg-Glen RS, Fox RC, & Logue EH (2001). Caregiver and elder experiences of Cambodian, Vietnamese, Soviet Jewish, and Ukrainian refugees. The International Journal of Aging and Human Development, 53, 233–252. doi: 10.2190/PXUG-J0T8-DGUK-08MD [DOI] [PubMed] [Google Scholar]
- Ta Park V, Nguyen K, Tran V, Yeo G, Tiet Q, Suen J, & Gallagher-Thompson D (2018). Perspectives and insights from Vietnamese American mental health professionals on how to culturally tailor a Vietnamese dementia caregiving program. Clinical Gerontologist, 42, 184–199. doi: 10.1080/07317115.2018.1432734 [DOI] [PubMed] [Google Scholar]
- Tarlow BJ, Wisniewski SR, Belle SH, Rubert M, Ory MG, & Gallagher-Thompson D (2004). Positive aspects of caregiving: Contributions of the REACH project to the development of new measures for Alzheimer’s caregiving. Research on Aging, 26, 429–453. doi: 10.1177/0164027504264493 [DOI] [Google Scholar]
- Torr BM, & Walshi ET (2018). Does the refugee experience overshadow the effect of SES? An examination of self-reported health among older Vietnamese refugees. Race and Social Problems, 10, 259–271. doi: 10.1007/s12552-018-9240-6 [DOI] [Google Scholar]
- Tran C, & Hinton L (2010). Health and health care of Vietnamese American older adults. Retrieve from http://Geriatrics.stanford.edu/ethnomed/Vietnamese/. In Periyakoil (eds). eCampus Geriatrics, Stanford: CA. [Google Scholar]
- U.S. Census Bureau. (2017a). American community survey (ACS). American Community Survey 1-Year Estimates. Retrieved from https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. [Google Scholar]
- U.S. Census Bureau. (2017b). American community survey (ACS). American FactFinder; 2017. Retrieved from https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/2017/ [Google Scholar]
- Uba L (1994). Asian Americans: Personality patterns, identity, and mental health. New York, NY: Guilford Press. [Google Scholar]
- von der Mehden FR (2017). Vietnamese, handbook of texas online. Texas State Historical Association. Retrieved from https://tshaonline.org/handbook/online/articles/pjv01 [Google Scholar]
- Wang DS (2012). Caregiving for dementia in Asian communities: Implications for practice. Journal of Ethnic and Cultural Diversity in Social Work, 21, 249–273. doi: 10.1080/15313204.2012.700496 [DOI] [Google Scholar]
- Yeo G, Tran NU, Hikoyeda N, & Hinton L (2002). Conceptions of dementia among Vietnamese American caregivers. Journal of Gerontological Social Work, 36, 131–152. doi: 10.1300/J083v36n01_08 [DOI] [Google Scholar]
- Zane N, & Yeh M (2002). The use of culturally-based variables in assessment: Studies on loss of face. In Kurasaki KS, Okazaki S, & Sue S (Eds.), Asian American mental health: Assessment theories and methods (pp. 123–138). New York, NY: Kluwer Academic/Plenum Press Publishers. doi: 10.1007/978-1-4615-0735-2_9 [DOI] [Google Scholar]