Abstract
Objectives
The COVID-19 pandemic and ensuing public health emergency has emphasized the need to study SARS-CoV-2 pathogenesis. The human microbiome has been shown to regulate the host immune system and may influence host susceptibility to viral infection, as well as disease severity. Several studies have assessed whether compositional alterations in the nasopharyngeal microbiota are associated with SARS-CoV-2 infection. However, the results of these studies were varied, and many did not account for disease severity. This study aims to examine whether compositional differences in the nasopharyngeal microbiota are associated with SARS-CoV-2 infection status and disease severity.
Methods
We performed Nanopore full-length 16S rRNA sequencing on 194 nasopharyngeal swab specimens from hospitalized and community-dwelling SARS-CoV-2-infected and uninfected individuals. Sequence data analysis was performed using the BugSeq 16S analysis pipeline.
Results
We found significant beta (PERMANOVA p < 0.05), but not alpha (Kruskal-Wallis p > 0.05) diversity differences in the nasopharyngeal microbiota among our study groups. We identified several differentially abundant taxa associated with SARS-CoV-2 infection status and disease severity using ALDEx2. Finally, we observed a trend towards higher abundance of Enterobacteriaceae in specimens from hospitalized SARS-CoV-2-infected patients.
Conclusions
This study identified several alterations in the nasopharyngeal microbiome associated with SARS-CoV-2 infection status and disease severity. Understanding the role of the microbiome in infection susceptibility and severity may open new avenues of research for disease prevention and treatment.
Introduction
The global COVID-19 pandemic and ensuing public health emergency has resulted in enormous economic costs and healthcare burdens worldwide. Over 580 million people have been infected and over 6 million people have died from COVID-19 (WHO: https://covid19.who.int/ accessed on August 8, 2022). COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); a positive-sense RNA virus of the Coronaviridae family [1]. There is wide variation in individual risk of SARS-CoV-2 infection and clinical outcomes; however, the mechanisms of SARS-CoV-2 pathogenesis and differences in COVID-19 disease progression remain unclear.
Associations between the human microbiome and the development of disease have been widely studied in recent years. The influence of the microbiome on viral infection and respiratory health has been explored [2], and the immunomodulatory role of the mucosal microbiome has been posed as a mechanism that may influence host susceptibility to viral infection [3, 4]. Indeed, the presence of certain commensals have been shown to influence host Toll-like receptor expression, which is involved in virus detection and immunity [5]. Elevated nasal and systemic levels of pro-inflammatory cytokines have also been implicated in adverse clinical outcomes in influenza patients [5]. Therefore, microbes that overstimulate host cytokine responses may influence viral infection severity.
Active viral infection has also been shown to alter the composition of the respiratory microbiota [6] and influenza infection may increase host susceptibility to bacterial co-infections [7]. Several studies have assessed the prevalence of bacterial co-infections in SARS-CoV-2 patients, with one systematic review estimating the prevalence of co-infections in COVID-19 patients at 6.9% [8]. As bacterial co-infections can lead to adverse patient outcomes, it is important to investigate whether there are associations between SARS-CoV-2 infection and disease severity, and the composition of the upper respiratory tract microbiome.
Several studies have examined the relationship between SARS-CoV-2 infection and the oral, nasal, lung, and gut microbiomes. However, the results of these studies have varied greatly. Pseudomonas aeruginosa [9], Fusobacterium periodonticum [10], and Propionibacteraceae [11] were all found to be differentially abundant in samples from SARS-CoV-2-infected patients versus healthy controls. Additionally, several studies have shown decreased alpha diversity in the nasal microbiome in SARS-CoV-2-infected patients compared to healthy controls [11, 12]. However, other groups reported no decrease in alpha diversity metrics for SARS-CoV-2-infected patients [9, 10], and one study found an increase in species richness among samples from SARS-CoV-2-infected patients [13]. These studies differ in their sample handling, subject inclusion criteria, and study groups definitions, which makes direct comparisons between studies difficult. Furthermore, many of these studies had limited small sample sizes and did not account for disease severity, viral load, collection date, or SARS-CoV-2 variant type, which may result in confounded study results. The relationship between SARS-CoV-2 infection and the nasopharyngeal microbiome composition remains unclear.
In this study, we will harness full-length 16S rRNA sequence data to assess compositional differences in the nasopharyngeal microbiota between four groups of patients: SARS-CoV-2-infected-hospitalized patients, SARS-CoV-2-infected community-dwelling patients, SARS-CoV-2-uninfected-hospitalized patients, and SARS-CoV-2-uninfected community-dwelling patients from British Columbia.
Materials & methods
Study population and specimen collection
Nasopharyngeal swab (NPS) specimens (n = 194) from adult individuals, collected in Copan Universal Transport Medium (Copan, Murrieta, CA) or Yocon Viral Transport Medium (Yocon Biology, Beijing, China), were tested for SARS-CoV-2 at the Vancouver General Hospital (VGH) Division of Medical Microbiology. Study samples were collected retrospectively throughout the COVID-19 pandemic in British Columbia (March 2020 –January 2022) and distributed across four study groups, SARS-CoV-2-uninfected community-dwelling (COMNEG) (n = 51), SARS-CoV-2-infected community-dwelling (COMPOS) (n = 47), SARS-CoV-2-uninfected hospitalized (HOSNEG) (n = 48), and SARS-CoV-2-infected hospitalized (HOSPOS) (n = 48) specimens. All samples were collected by healthcare professionals to minimize bias in sampling quality.
Routine diagnostic testing was performed using either a Roche MagNA Pure extraction system (Roche Diagnostics, Laval, Canada) in combination with a lab developed (LDT) real time PCR (RT-PCR) assay detecting the E-gene and RdRp gene targets, or the Panther Fusion SARS-CoV-2 assay (Hologic Inc., San Diego, CA), detecting two targets in ORF1ab. The LDT RT-PCR assay was developed at the British Columbia Center for Disease Control (BCCDC) and is based on the World Health Organization’s guidelines for COVID-19 RT-PCR diagnostic screening [14]. RT-PCR Ct values were available for most SARS-CoV-2 positive specimens. Several NPS underwent testing using the BioFire respiratory panel 2.1 (Biomerieux, St-Laurent, Canada), Ct values for these specimens were not available. Screening for potential SARS-CoV-2 variants of concern (VOCs) (e.g. alpha, beta, gamma, delta) was performed using PCR at the BCCDC using an assay developed in-house [no reference or report (or web URL) for this]. Primers and probes were designed to target the N501Y and E484K mutations; and PCR conditions are provided in S1 Table in S1 File.
Nucleic acid extraction & quantification
Total nucleic acids were extracted from NPS specimens using the MagNA Pure 24 Total NA Isolation Kit on the MagNA Pure 24 extraction system (Roche Diagnostics, Laval, Canada). The Pathogen 1000 protocol was used with a 500μL sample and 50μL elution volume. Total nucleic acid extracts were quantified with a Qubit 4 Fluorometer (Thermo Fisher Scientific) using the high-sensitivity dsDNA assay kit.
Library preparation & sequencing
We utilized the Oxford Nanopore Technologies (ONT) MinION sequencing platform for this study, which enables real-time, long read sequencing of biological samples. This approach may confer more accurate taxonomic resolution than short-read 16S rRNA sequencing approaches [15], and has been shown to confer comparable results to Illumina sequencing for the nasal microbiota specifically [16]. Library preparation was performed using the full-length 16S rRNA barcoding kit (ONT: SQK-16S024), with several key modifications. Briefly, 20ng of nucleic acid extract (up to 10μL) was combined with barcoded primers (ONT), LongAmp HotStart Taq 2x Master Mix (New England Biolabs), and PCR-grade water as specified in the SQK-16S024 protocol (ONT). Full-length 16S amplicon fragments were amplified through PCR, followed by magnetic bead cleanup using 30μL of PCRClean DX beads (Aline Biosciences). Amplified libraries were quantified as described above and 2ng of each sample (up to 2μL) was pooled together. Up to 23 clinical samples plus a negative control (extracted blank viral transport medium) were multiplexed per flowcell. Adaptor ligation was performed at room temperature using 15μL of pooled library, followed by addition of SQB and Loading Beads (ONT). Final libraries were loaded onto MinION flowcells (FLO-MIN106; R9.4.1) and sequenced using default run parameters in MinKNOW (Version 4.2.8, ONT) for up to 72 hours.
Sequence data analysis
Raw sequence data were basecalled using Guppy (Version 5.0.7, ONT) with default parameters and the–device cuda:0 flag to enable GPU basecalling. Basecalled fastq files were analyzed using the BugSeq 16S sequencing analysis pipeline [17]. Downstream analysis and visualization of Amplicon Sequence Variant (ASV) classification tables was performed using Rstudio (R Version 4.1.0) [18]. Relative abundance was calculated for each taxon and alpha/beta diversity metrics were estimated using the vegan R package [19]. Multivariate analyses (Principal coordinates analysis (PcoA), and permutational multivariate analysis of variance (PERMANOVA)) were performed to assess compositional differences in the nasopharyngeal microbiome among our four study groups. ALDEx2 [20] was used to contrast differential abundance of taxa across our study groups. Random Forest predictive models were built for our four study groups, as well as infected vs non-infected as the outcome variables using the randomForest R package [21]. Our models were configured using the flags ntree = 500 and mtry = 8, with the remaining parameters set to the default.
Ethics approval & data availability
This study included de-identified samples collected from VGH and has obtained ethics board approval from the research ethics board at the University of British Columbia (H20-02152). All raw sequence data for this study is available on NCBI SRA under the accession number PRJNA868394.
Results
Study population
Our study groups exhibited similar age distributions (Table 1); however, there were a larger number of male subjects included in the study (39.7% female, 60.3% male). We did not observe sex-specific microbiome clustering in our analysis. Study samples were collected from March 2020 to January 2022, providing access to clinical specimens positive for a range of SARS-CoV-2 lineages and representing all seasons (Table 1; S1 Fig). Study specimens exhibited a range of RT-PCR Ct values (S2 Table in S1 File).
Table 1. Summary of study population demographics.
| Male (n) | Female (n) | Age | Patient location | Specimen collection | |
|---|---|---|---|---|---|
| COMNEG | 24 | 27 | 60.9 ± 12.2 | Community-dwelling | Mar-May 2020, n = 1 |
| Aug-Dec 2020, n = 3 | |||||
| Jan-May 2021, n = 29 | |||||
| Aug 2021-Jan 2022, n = 18 | |||||
| COMPOS | 27 | 20 | 61.7 ± 13.6 | Community-dwelling | Mar-May 2020, n = 0 |
| Aug-Dec 2020, n = 23 | |||||
| Jan-May 2021, n = 23 | |||||
| Aug 2021-Jan 2022, n = 1 | |||||
| HOSNEG | 33 | 15 | 61.9 ± 14.7 | Non-critical care unit, n = 44 | Mar-May 2020, n = 0 |
| Critical care unit, n = 4 | Aug-Dec 2020, n = 0 | ||||
| Jan-May 2021, n = 43 | |||||
| Aug 2021-Jan 2022, n = 5 | |||||
| HOSPOS | 33 | 15 | 64.1 ± 15.1 | Non-critical care unit, n = 12 | Mar-May 2020, n = 11 |
| Critical care unit, n = 36 | Aug-Dec 2020, n = 10 | ||||
| Jan-May 2021, n = 26 | |||||
| Aug 2021-Jan 2022, n = 1 |
COMNEG = Community SARS-CoV-2-uninfected, COMPOS = Community SARS-CoV-2-infected, HOSNEG = Hospitalized SARS-CoV-2-uninfected, HOSPOS = Hospitalized SARS-CoV-2-infected. Age distribution values reflect the mean and standard deviation for each study group.
Sequence data quality & filtering
Reads with low quality (mean Phred score < 7), low complexity (fastp complexity < 30%), and reads shorter than 1000bp or longer than 1850bp were discarded [17]. Samples with less than 1000 mapped sequence reads following 16S rRNA PCR amplification were also discarded. In total, 194 samples passed our sequence data quality thresholds.
Richness, evenness, & diversity metrics
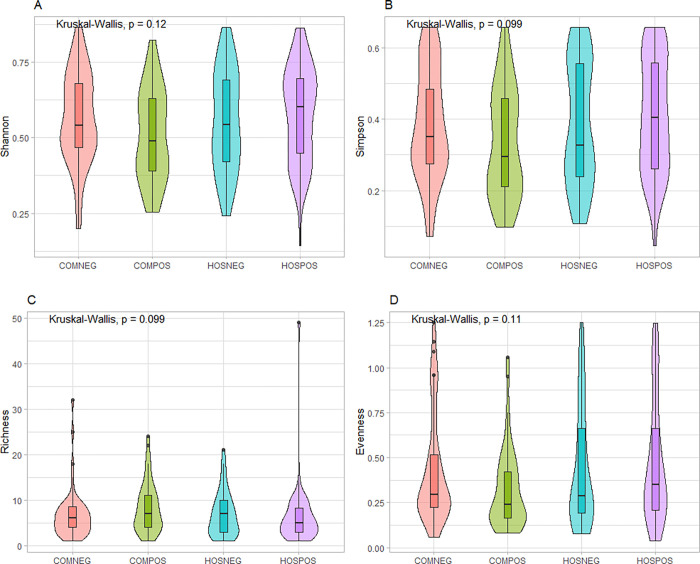
We did not observe any significant differences in alpha diversity among our study groups (Kruskal-Wallis p > 0.05) (Fig 1), although there did appear to be a trend towards lower mean Shannon/Simpson diversity and evenness for SARS-CoV-2-infected community-dwelling samples versus SARS-CoV-2-uninfected community-dwelling samples. This trend was not observed in hospitalized SARS-CoV-2-infected versus uninfected samples.
Fig 1. Alpha diversity differences.
Genus-level differences in alpha diversity among our study groups summarized through A. Shannon diversity index, B. Simpson diversity index, C. Taxa richness, D. Evenness.
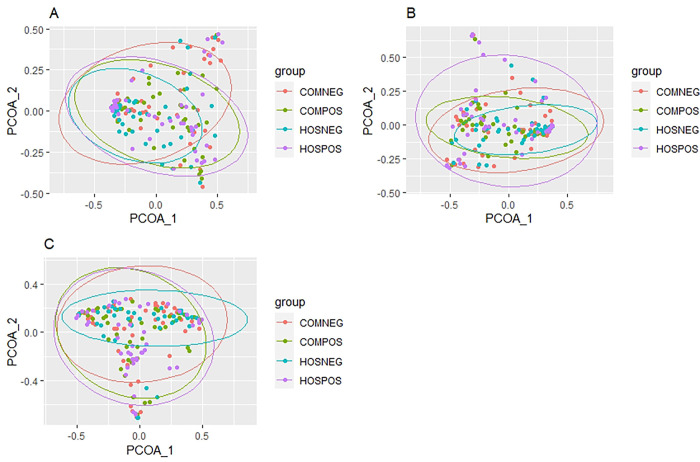
Bray-Curtis dissimilarity ordination was performed to assess differences in beta diversity among our study groups using PCoA at the species-, genus-, and family-level taxonomic ranks (Fig 2). Statistical analysis was performed to determine whether there was significant clustering among our study groups using adonis within the vegan R package. We observed significant clustering at all three taxonomic ranks (adonis: Species p = 0.009, Genus p = 0.028, Family p = 0.027), suggesting that there are differences in microbial community composition among our study groups, although, there was a large degree of overlap in the 95% confidence ellipses.
Fig 2. Beta diversity differences.
Principle coordinates analysis plots based on Bray-Curtis dissimilarity among our four study groups at the A. species, B. genus, and C. family taxonomic ranks. P-values were derived from PERMANOVA. 95% confidence ellipses are displayed around each study group.
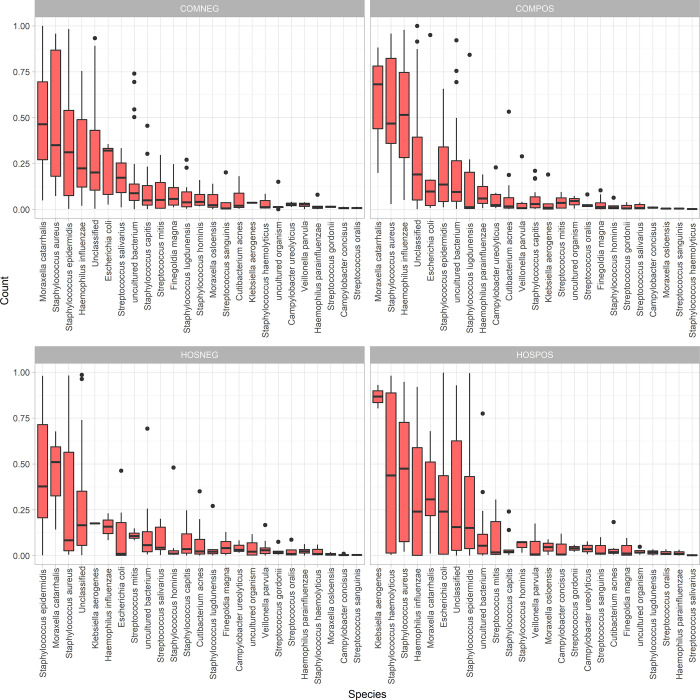
Taxonomic differences among our study groups
Relative abundance was calculated, and taxa present at less than 5% prevalence across all samples were removed. At the genus level, Staphylococcus was the most abundant genus on average for both SARS-CoV-2-uninfected study groups, whereas Acinetobacter was the most abundant genus in the hospitalized infected group and Moraxella was the most abundant genus in the community-dwelling SARS-CoV-2-infected group (S2 Fig). At the species level, both SARS-CoV-2-infected groups were dominated by common nasal pathobionts and opportunistic pathogens including Haemophilus influenzae, Staphylococcus haemolyticus, and Staphylococcus aureus, with the SARS-CoV-2-infected hospitalized group having the opportunistic pathogen Klebsiella aerogenes as the most abundant species (Fig 3). At the family rank, SARS-CoV-2-infected hospitalized patients displayed a higher mean relative abundance and broader range of Enterobacteriaceae then any of the other study groups (S3 Fig).
Fig 3. Species-level relative abundance.
Side-by-side boxplots of relative abundance at the species-level among our four study groups. Only taxa with an overall prevalence greater than 5% across all samples are shown (i.e., taxa required to be present in 10 out of 194 samples). Taxa are ordered from highest to lowest mean relative abundance.
ADLEx2 was used to assess which of the taxa were significantly differentially abundant. The species Cutibacterium acnes, the genera Cutibacterium and Peptinophilus, and the families Propionibacteriaceae and Peptostreptococcales-Tissierellales were all differentially abundant over the four study groups (Kruskal-Wallis p < 0.05). An “uncultured” genus assigned to the family Neisseriaceae was also found to be differentially abundant. All the differentially abundant taxa were enriched in community-dwelling SARS-CoV-2 infected individuals. Our Random Forest predictive models for the binary outcome variable (infected vs non-infected) and our four study groups produced out-of-bag error estimates of 44.9% and 66.5% respectively.
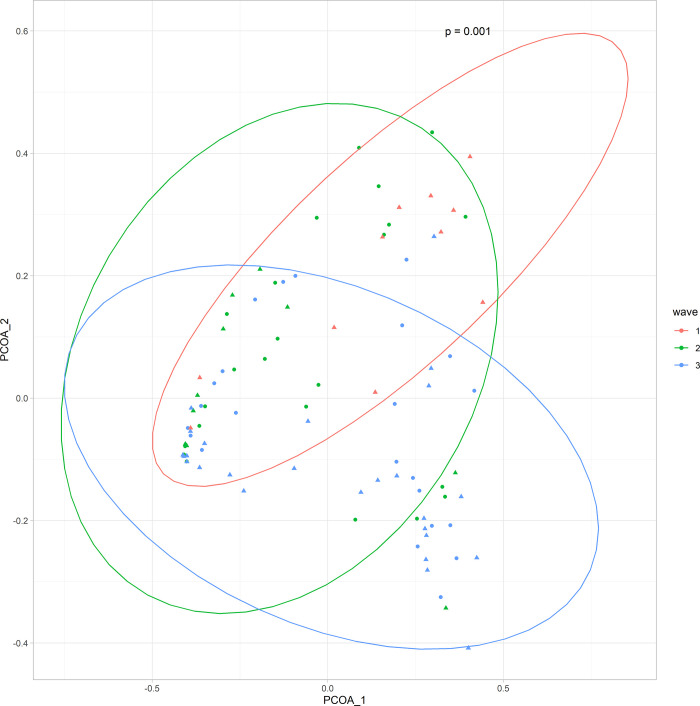
Alterations in the nasopharyngeal microbiome associated with Ct value, collection date, and variant status
Significant beta (PERMANOVA p < 0.05), but not alpha diversity differences in the nasopharyngeal microbiome composition were observed when stratified by sample collection date (Fig 4). ALDEx2 revealed significant differences (Kruskal-Wallis p < 0.05) in Streptococcus spp. and Corynebacterium spp. among samples from infected individuals collected during the first three waves of the pandemic in British Columbia (Wave 1: March-May 2020, Wave 2: August-December 2020, Wave 3: January- May 2021). We did not observe significant differences in alpha (Kruskal-Wallis p > 0.05), or beta diversity (adonis p > 0.05) associated with viral load or by SARS-CoV-2 variant infection status.
Fig 4. Beta diversity differences by collection date.
PCoA plot for genus-level differences in the nasopharyngeal microbiome based on Bray-Curtis dissimilarity stratified by collection date. Circles indicate community-dwelling SARS-CoV-2-infected subjects and triangles indicate hospitalized SARS-CoV-2-infected subjects.
Discussion
In this study, we used full-length 16S rRNA sequencing data to examine differences in the nasopharyngeal microbiota associated with SARS-CoV-2 infection and COVID-19 severity. We found significant beta (Fig 2), but not alpha (Fig 1) diversity differences in the nasopharyngeal microbiota between hospitalized and community-dwelling SARS-CoV-2-infected and uninfected specimens. Our results are consistent with two previous studies that found no significant difference in alpha diversity between SARS-CoV-2-infected and uninfected patient samples [9, 10]. Both studies displayed a similar trend towards decreasing alpha diversity in SARS-CoV-2 patients, consistent with our data (Fig 1). Our alpha diversity observations contrast with two previous studies [11, 12] that found a decrease in alpha diversity among SARS-CoV-2 infected specimens; however, these studies did not account for disease severity. We found significant differences in beta diversity among our study groups (Fig 2), consistent with other groups that have found significant beta diversity clustering between SARS-CoV-2-infected and uninfected subjects [9–11]. However, we did see significant overlap in the confidence ellipses (Fig 2), suggesting that although significant, the magnitude of compositional differences in the microbiota among our study groups are relatively small.
We identified several trends in the taxonomic composition of the nasal microbiota among our study groups, as well as a few differentially abundant taxa. The high relative abundance of Staphylococcus spp. among our SARS-CoV-2-uninfected groups (S2 Fig) is consistent with literature describing the core nasal microbiota among adults that is typically dominated by the phyla Actinobacteria and Firmicutes, including Staphylococcus [22]. A trend towards higher relative abundance of Moraxella spp. and Acinetobacter spp. in the SARS-CoV-2-infected study groups was observed (S2 Fig), potentially highlighting an increased abundance of pathobionts and opportunistic pathogens among SARS-CoV-2-infected individuals. At the species level, the trend towards non-statistically significant higher mean abundance of opportunistic pathogens and pathobionts such as Haemophilus influenzae, Staphylococcus haemolyticus, Staphylococcus aureus, and Klebsiella aerogenes among our SARS-CoV-2-infected specimens (Fig 3), is consistent with literature implicating some of these opportunistic pathogens in respiratory virus infection severity [5]. In particular, the presence of H. influenzae in the nasopharynx has been shown to promote human rhinovirus pathogenesis through the increased expression of pulmonary epithelial cell TLR-3 [23]. Additionally, non-influenza respiratory viral infection has been hypothesized to increase host susceptibility to S. aureus superinfection through alterations in host-S. aureus adhesion, increased epithelial cell permeability to S. aureus, or a reduction in the immune system’s ability to regulate S. aureus clearance from the nasal passage [24], in line with the trend we saw towards higher S. aureus abundance in our SARS-CoV-2-infected study groups. The trend towards increased abundance of Enterobacteriaceae among our hospitalized SARS-CoV-2-infected study group (S3 Fig) may be attributed to medical interventions in this group such as, intubation or antibiotic exposure. We found differential abundance of Cutibacterium acnes among our study groups. This nasal commensal has been implicated in patients with chronic rhinosinusitis [25] and is associated with increased host inflammatory response [26], which may explain why this species was most abundant in our community SARS-CoV-2-infected group. This species has also been hypothesized to play a role in regulating nasal microbiome homeostasis through its’ ability to influence S. aureus growth [27]. Finally, the presence of an “uncultured” Neisseriaceae member that was most abundant in our community-dwelling SARS-CoV-2-infected group is interesting. This family has been previously reported as a “core” nasopharyngeal microbiome taxon [28] and has been shown to be associated with swine influenza co-infection [29]. However, it’s role in SARS-CoV-2 infection remains unclear.
Our study has several limitations. First, our samples were de-identified, therefore, we were unable to adjust for potential confounders that may have influenced the nasopharyngeal microbiota among our study groups such as medications, medical interventions, antibiotic exposure, or hospitalization duration in our hospitalized study groups. SARS-CoV-2-uninfected community-dwelling individuals may have other respiratory viral infections. As antibiotic treatment is a common treatment for hospitalized COVID-19 patients, this may have influenced our study results. However, we did also include a study group of hospitalized COVID-19 negative patients in our study to partially control for this. Without knowledge of detailed symptoms that led individuals to seek COVID testing, it is impossible to determine if or how many of the samples recovered from uninfected subjects are representative of the microbiota composition of truly symptom-free, virus negative subjects. This may have led to an underestimate in the magnitude of our alpha and beta diversity estimate differences across groups. However, the incidence of other respiratory viruses was low in our patient population during the study period (https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance.html). We identified a high proportion of reads mapping to the genus Alishewanella, an environmental microbe (S2 Fig). This may be due to poor annotation of this taxon in the reference database. Functional analysis from metatranscriptomic data examining this relationship may reveal functional pathways that are differentially expressed in SARS-CoV-2 infection. Microbiome function may play a more significant role than taxonomic differences in infection progression and severity.
The results of this study present several key alterations in the nasopharyngeal microbiota associated with SARS-CoV-2 infection and disease severity. These results emphasize the possible role of the respiratory microbiome in host susceptibility to viral infection and subsequent disease severity. This study adds to the current literature emphasizing the value of microbiome data in relation to respiratory infection severity and disease progression. Our study accounted for COVID-19 severity and harnessed full-length 16S rRNA sequence data that may provide a more granular representation of the microbiota differences in SARS-CoV-2-infected and uninfected individuals. Further work is necessary to determine whether functional characteristics of the nasopharyngeal microbiome are associated with respiratory viral infection and adverse patient outcomes, or if emerging SARS-CoV-2 variants have alternate influences on the nasal microbiota. Understanding these microbiome-driven mechanisms could present novel prognostic markers, or offer new approaches to disease prevention and treatment.
Supporting information
(PNG)
(PNG)
(PNG)
(DOCX)
Acknowledgments
We would like to acknowledge the technicians at the Division of Medical Microbiology at VGH for their help in sample nucleic acid extractions. We would also like to thank Josh Chorlton from BugSeq Bioinformatics Inc. for his assistance in coordinating data analysis.
Data Availability
All raw sequence data for this study is available on NCBI SRA under the accession number PRJNA868394.
Funding Statement
The authors received no specific funding for this work. Funding was provided internally from Vancouver General Hospital.
References
- 1.Tavares R de CA, Mahadeshwar G, Pyle AM. The global and local distribution of RNA structure throughout the SARS-CoV-2 genome. J Virol. 2020;(December). doi: 10.1101/2020.07.06.190660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilks J, Golovkina T. Influence of microbiota on viral infections. PLoS Pathog. 2012;8(5):5–7. doi: 10.1371/journal.ppat.1002681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallo O, Locatello LG, Mazzoni A, Novelli L, Annunziato F. The central role of the nasal microenvironment in the transmission, modulation, and clinical progression of SARS-CoV-2 infection. Mucosal Immunol. 2021;14(2):305–16. doi: 10.1038/s41385-020-00359-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bao L, Zhang C, Dong J, Zhao L, Li Y, Sun J. Oral Microbiome and SARS-CoV-2: Beware of Lung Co-infection. Front Microbiol. 2020;11(July):1–13. doi: 10.3389/fmicb.2020.01840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pichon M, Lina B, Josset L. Impact of the respiratory microbiome on host responses to respiratory viral infection. Vaccines. 2017;5(4):1–14. doi: 10.3390/vaccines5040040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiang Z, Koo H, Chen Q, Zhou X, Liu Y, Simon-Soro A. Potential implications of SARS-CoV-2 oral infection in the host microbiota. J Oral Microbiol. 2021;13(1). 10.1080/20002297.2020.1853451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jia L, Xie J, Zhao J, Cao D, Liang Y, Hou X, et al. Mechanisms of severe mortality-associated bacterial co-infections following influenza virus infection. Front Cell Infect Microbiol. 2017;7(AUG):1–7. doi: 10.3389/fcimb.2017.00338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26(12):1622–9. doi: 10.1016/j.cmi.2020.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhoades NS, Pinski AN, Monsibais AN, Jankeel A, Doratt BM, Cinco IR, et al. Acute SARS-CoV-2 infection is associated with an increased abundance of bacterial pathogens, including Pseudomonas aeruginosa in the nose. Cell Rep. 2021;36(9):109637. doi: 10.1016/j.celrep.2021.109637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nardelli C, Gentile I, Setaro M, Di Domenico C, Pinchera B, Buonomo AR, et al. Nasopharyngeal Microbiome Signature in COVID-19 Positive Patients: Can We Definitively Get a Role to Fusobacterium periodonticum? Front Cell Infect Microbiol. 2021;11(February):1–7. doi: 10.3389/fcimb.2021.625581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mostafa HH, Fissel JA, Fanelli B, Bergman Y, Gniazdowski V, Dadlani M, et al. Metagenomic next-generation sequencing of nasopharyngeal specimens collected from confirmed and suspect covid-19 patients. MBio. 2020;11(6):1–13. doi: 10.1128/mBio.01969-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rueca M, Fontana A, Bartolini B, Piselli P, Mazzarelli A, Copetti M, et al. Investigation of nasal/oropharyngeal microbial community of covid-19 patients by 16s rdna sequencing. Int J Environ Res Public Health. 2021;18(4):1–12. doi: 10.3390/ijerph18042174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosas-Salazar C, Kimura KS, Shilts MH, Strickland BA, Freeman MH, Wessinger BC, et al. SARS-CoV-2 infection and viral load are associated with the upper respiratory tract microbiome. J Allergy Clin Immunol. 2021;147(4):1226–1233.e2. doi: 10.1016/j.jaci.2021.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 -nCoV by RT-PCR. Euro Surveill. 2020;25(3):1–8. doi: 10.2807/1560-7917.ES.2020.25.3.2000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsuo Y, Komiya S, Yasumizu Y, Yasuoka Y, Mizushima K, Takagi T, et al. Full-length 16S rRNA gene amplicon analysis of human gut microbiota using MinIONTM nanopore sequencing confers species-level resolution. BMC Microbiology. 2020;1–13. doi: 10.1101/2020.05.06.078147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heikema AP, Horst-Kreft D, Boers SA, Jansen R, Hiltemann SD, de Koning W, et al. Comparison of illumina versus nanopore 16s rRNA gene sequencing of the human nasal microbiota. Genes (Basel). 2020;11: 1–17. doi: 10.3390/genes11091105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jung A, Chorlton SD. BugSeq 16S: NanoCLUST with Improved Consensus Sequence Classification 1. bioRxiv. 2021;2021.03.16.434153. 10.1101/2021.03.16.434153 [DOI] [Google Scholar]
- 18.Team RS. RStudio: Integrated Development for R [Internet]. Boston, MA: RStudio, PBC; 2020. Available from: http://www.rstudio.com/ [Google Scholar]
- 19.Dixon P. Computer program review VEGAN, a package of R functions for community ecology. J Veg Sci. 2003;14(6):927–30. http://doi.wiley.com/10.1111/j.1654-1103.2002.tb02049.x [Google Scholar]
- 20.Fernandes AD, Macklaim JM, Linn TG, Reid G, Gloor GB. ANOVA-Like Differential Expression (ALDEx) Analysis for Mixed Population RNA-Seq. PLoS One. 2013;8(7). doi: 10.1371/journal.pone.0067019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liaw A, Wiener M (2002). “Classification and Regression by randomForest.” R News, 2(3), 18–22. https://CRAN.R-project.org/doc/Rnews/ [Google Scholar]
- 22.Brugger SD, Bomar L, Lemon KP. Commensal–Pathogen Interactions along the Human Nasal Passages. PLoS Pathog. 2016;12(7):1–9. doi: 10.1371/journal.ppat.1005633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sajjan US, Jia Y, Newcomb DC, Bentley JK, Lukacs NW, LiPuma JJ, et al. H. influenzae potentiates airway epithelial cell responses to rhinovirus by increasing ICAM‐1 and TLR3 expression. FASEB J. 2006;20(12):2121–3. doi: 10.1096/fj.06-5806fje [DOI] [PubMed] [Google Scholar]
- 24.Fedy Morgene M, Botelho-Nevers E, Grattard F, Pillet S, Berthelot P, Pozzetto B, et al. Staphylococcus aureus colonization and non-influenza respiratory viruses: Interactions and synergism mechanisms. Virulence. 2018;9(1):1354–63. doi: 10.1080/21505594.2018.1504561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Urbán E, Gajdács M, Torkos A. The incidence of anaerobic bacteria in adult patients with chronic sinusitis: A prospective, single-centre microbiological study. Eur J Microbiol Immunol. 2020;10(2):107–14. doi: 10.1556/1886.2020.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fischer K, Tschismarov R, Pilz A, Straubinger S, Carotta S, McDowell A, et al. Cutibacterium acnes Infection Induces Type I Interferon Synthesis Through the cGAS-STING Pathway. Front Immunol. 2020;11(October):1–16. doi: 10.3389/fimmu.2020.571334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hardy BL, Merrell DS. Friend or foe: Interbacterial competition in the nasal cavity. J Bacteriol. 2020;203(5):1–13. doi: 10.1128/JB.00480-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen CH, Liou ML, Lee CY, Chang MC, Kuo HY, Chang TH. Diversity of nasal microbiota and its interaction with surface microbiota among residents in healthcare institutes. Sci Rep. 2019;9(1):1–10. 10.1038/s41598-019-42548-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chrun T, Leng J, La Ragione RM, Graham SP, Tchilian E. Changes in the nasal microbiota of pigs following single or co-infection with porcine reproductive and respiratory syndrome and swine influenza a viruses. Pathogens. 2021;10(10). doi: 10.3390/pathogens10101225 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PNG)
(PNG)
(PNG)
(DOCX)
Data Availability Statement
All raw sequence data for this study is available on NCBI SRA under the accession number PRJNA868394.