Abstract
Objectives
COVID-19 is a global health concern due to its rapid spread and impact on morbidity and mortality. Implementing preventive measures plays an essential role in curbing the spread of COVID-19 infection. This study aimed to assess COVID-19 preventive practice and associated factors in Ethiopia.
Study design
This study was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines.
Methods
Medline, PubMed, Scopus, Cochrane, EMBASE, African Journal Online (AJOL) and Science Direct search engines were used to identify relevant articles published up to early December 2021. The Joana Brigg's Institute (JBI) checklist was used for quality appraisal. A random-effect model was fitted to calculate the pooled estimates. Higgins I2 statistics and Egger's test with funnel plots were analysed to check heterogeneity and publication bias, respectively. Due to significant heterogeneity, subgroup analysis by region, study population, study design and publication year, as well as sensitivity analysis, were done to assess the source of heterogeneity.
Results
The pooled level of poor preventive practice for COVID-19 in Ethiopia was 51.60% (95% confidence interval [CI]: 40.30–62.90). Poor COVID-19 preventive practice declined from 61% in studies published in 2020 to 45% in 2021. Lack of knowledge about COVID-19 (adjusted odds ratio [AOR] = 4.61 [95% CI: 2.49–10.73]), a negative attitude towards COVID-19 management (AOR = 2.64 [95% CI: 1.82–3.82]), rural residence (AOR = 2.95 [95% CI: 2.12–4.12]), a low educational level (AOR = 2.93 [95% CI: 2.16–3.98]) and being female (AOR = 1.75 [95% CI: 1.27–2.40]) were significantly associated with a poor level of COVID-19 preventive practice in Ethiopia.
Conclusions
The level of poor COVID-19 preventive practice in Ethiopia was relatively high. Poor COVID-19 prevention practices were significantly correlated with inadequate COVID-19 knowledge, a negative attitude towards COVID-19 management, low educational attainment, living in a rural area and being female. Creating awareness and health education programmes targeting COVID-19 prevention should be strengthened, especially in the target populations identified in this study.
Keywords: COVID-19, Poor practice, Preventive practice, Ethiopia
Abbreviations: COVID-19, Coronavirus disease 19; SARS-COV-2, Severe Acute Respiratory Syndrome Corona Virus 2; WHO, World Health Organization
1. Introduction
Coronavirus disease 2019 (COVID-19) is caused by the newly discovered Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) [1]. On the 11 March 2020, COVID-19 was declared a pandemic by the World Health Organisation (WHO) [2]. SARS-COV-2 was first identified on 30 December 2019 in Wuhan city, Hubei province, China. The virus is highly contagious, with flu-like symptoms, and spread globally within a short period of time [3]. The virus is transmitted by exposure to droplets and aerosols, particularly in overcrowded areas [4]. At the beginning of the pandemic, COVID-19 symptoms started with a high fever and mild respiratory problems, but within a few days, frequently developed to pneumonia [5]. Lockdowns and maintaining self-isolation/social distance are two measures used internationally to prevent COVID-19 transmission [6]. Other preventive mechanisms recommended by the WHO are frequent hand washing, avoiding touching the eyes, nose and mouth, and frequent disinfection of the surroundings and repeatedly touched surfaces [7,8].
COVID-19 preventive practices were implemented in Ethiopia to mitigate the impact of the pandemic [9,10]. Despite the rapid spread of COVID-19, studies suggest that communities have shown negative responses or carelessness towards the preventive measures of the COVID-19 pandemic [9]. In Ethiopia, adherence to preventive measures for COVID-19 was only 12.3%, regardless of the knowledge and attitude towards the virus. The level of poor COVID-19 preventive practice in Ethiopia was shown to vary from 20.9% [11] to 89.6% [12]. A low level of education, poor attitude towards COVID-19 management, younger age and inadequate knowledge of COVID-19 and its preventive practices were significantly associated with poor preventive practices in many studies [9,13,14].
In Ethiopia, there are barriers that delay control of viral transmission and implementation of preventive measures, such as limited supplies of hand sanitisers, testing kits and personal protective materials, high resistance to implementation of recommended prevention practices and low socio-economic status [15,16]. Although previous studies have measured COVID-19 preventive practices in Ethiopia, their results are inconsistent and inconclusive (12.3–90%) [9,10,17]. In addition, most of these studies were carried out in a single population and none of the studies showed comprehensive data about the poor level of COVID-19 preventive practice in Ethiopia. Therefore, the current study aimed to determine the level of poor COVID-19 preventive practice and its associated factors in Ethiopia.
2. Methods
2.1. Study design
This systematic review and meta-analysis was performed according to the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA-P 2015) guidelines [18] (Supplementary Table S1).
2.2. Eligibility criteria
All cross-sectional studies published up to early December 2021 in English and reporting poor levels of COVID-19 prevention practice and/or associated factors in Ethiopia were included. Only studies that were published or accepted in peer-reviewed journals were included in this review. Editorial reports, letters, reviews, commentaries and studies that did not report a poor level of COVID-19 preventive practice were excluded.
2.3. Outcome of interest
The primary outcome of interest was to estimate the level of poor COVID-19 prevention practice in Ethiopia, which was expressed as the proportion of participants with a poor level of prevention practice towards COVID-19. Poor levels of preventive practices were defined and assessed against the recommended prevention practices for COVID-19 safety, infection prevention and control guidelines; participants with a total score less than the average, mean or median of the questionnaire in each of the included studies were defined as having a poor level of COVID-19 prevention practice. The cut-off value to define a low level of prevention practice reported in each individual study was used as an operational definition to estimate the pooled level of COVID-19 poor practice because there was variation in the definition of poor level of COVID-19 preventive practice between studies. In addition, this review also aimed to identify variables associated with inadequate COVID-19 preventive practices.
2.4. Search strategy
Articles were identified by searching published studies in the following online databases: Medline, PubMed, Scopus, Cochrane, EMBASE, African Journal Online (AJOL) and Science Direct. All articles published up to early December 2021 were included. Additional studies were identified from the references cited in the relevant articles and through a manual search. Medical Subject Heading (MeSH), keywords and free text search terms were used. Search terms included “practice” OR “poor practice” OR “practice patterns” OR “level of practice” OR “preventive practice” AND “COVID-19” OR “SARS CoV-2” OR “coronavirus” OR “pandemic” AND “associated factors” OR “determinants” AND “Ethiopia” (Supplementary Table S2).
2.5. Study selection and quality appraisal
Retrieved articles were imported to EndNote X7 (Clarivate, London, UK) to collect and organise search outcomes and for the removal of duplicate articles. Subsequently, three authors (MDT, MM and SG) independently screened the titles and abstracts for potential inclusion in the review. Two authors (MM and SG) independently assessed the quality of studies. Any disagreements were resolved through discussion until mutual consensus was reached, with the involvement of a fourth author (TA) when necessary. The Joanna Briggs Institute (JBI) quality appraisal tool was used to evaluate the quality of the studies [19]. The checklist consists of nine items. The responses were scored ‘0’ for ‘not appropriate’ and ‘not reported’, and ‘1’ for ‘Yes’. Total scores ranged from 0 to 9. Studies scoring >50% on the quality assessment parameters were included for final analysis (Supplementary Table S3).
2.6. Data extraction
Studies that were approved by all authors in the selection processes were included for data extraction. For each included study, the first author's name, year of publication, the setting where the study was conducted, study design, study period, sample size, study population and poor levels of COVID-19 preventive practices were recorded. In addition, factors associated with poor levels of COVID-19 preventive practices, with their 95% confidence intervals (CIs), were extracted.
2.7. Data processing and analysis
Extracted data were entered into Microsoft Excel and then exported to STATA version 11.0 statistical software for analysis. A random-effect model meta-analysis was used to estimate the pooled effect size and effect of each study with a 95% CI. To summarise the data graphically, forest plots were used by estimating the pooled effect size and weight of each included study with a 95% CI. The degree of heterogeneity between the included studies was evaluated by the index of heterogeneity (I2 statistics) [20]. Subgroup analysis by region, study design, study population and year of publication, as well as sensitivity analysis, were conducted to determine the potential sources of heterogeneity. Funnel plot analysis and Egger weighted regression tests were used to detect publication bias [21,22]. A P-value <0.05 in Egger's test was considered as evidence of statistically significant publication bias.
3. Results
3.1. Identified studies
A total of 524 articles were initially retrieved; 184 were excluded due to duplication. A further 273 articles were excluded after reviewing the titles and abstracts, and an additional 49 were excluded as they did not fulfil the inclusion criteria. Finally, 18 articles were used in the analysis (Fig. 1).
Fig. 1.
Flow chart describing the selection of studies.
3.2. Characteristics of the included studies
A total of 18 studies that assessed the poor levels of COVID-19 preventive practice in Ethiopia were included in the current analysis. In total, 7717 study participants were involved in this review. Of the included articles, eight were from the Amhara region [14,[23], [24], [25], [26], [27], [28], [29]], four from the Oromia region [12,[30], [31], [32]], three from the Tigray region [11,33,34], two from the Addis Ababa city administration [35,36] and one from Southern Nations, Nationalities and Peoples (SNNP) region [37]. Four studies assessed the level of COVID-19 preventive practice at the community level [11,32,33,37]. From the included studies, the smallest sample size was in the study by Shibabaw et al., which involved 112 health workers [29]. The highest level of poor COVID-19 preventive practice (89.6%) was reported by Taye et al. in the Oromia region [12] (Table 1).
Table 1.
Characteristics of studies included in the meta-analysis of poor level of COVID-19 preventive practice and associated factors in Ethiopia.
| Study, year, ref. | Region | Study design | Study population | Sample Size | Poor practice (%) | Quality score |
|---|---|---|---|---|---|---|
| Feleke et al., 2021(26) | Amhara | Institutional-based | Health service visitors | 404 | 44 | 8 |
| Gebretsadik et al., 2021 [27] | Amhara | Institutional-based | Health service visitors | 384 | 41.7 | 9 |
| Iyasu et al., 2021 [37] | Tigray | Institutional-based | Chronic disease patients | 422 | 40.5 | 8 |
| Akalu et al., 2020 [28] | Amhara | Institutional-based | Chronic disease patients | 404 | 47.3 | 9 |
| Adola et al., 2021 [33] | Oromia | Institutional-based | Healthcare workers | 281 | 38.2 | 7 |
| Kassie et al., 2020 [17] | Amhara | Institutional- based | Healthcare workers | 630 | 61.27 | 7 |
| Daba et al., 2021 [35] | Oromia | Community-based | Community | 634 | 73 | 9 |
| Tekeba et al., 2021 [34] | Oromia | Institutional-based | Health service visitors | 292 | 20.9 | 7 |
| Adhena et al., 2020 [14] | Tigray | Community-based | Community | 422 | 52.5 | 9 |
| Tesfaye et al., 2020 [39] | Addis Ababa | Institutional-based | Healthcare workers | 295 | 70.2 | 8 |
| Abate et al., 2020 [29] | Amhara | Institutional-based | Health service visitors | 392 | 41.6 | 9 |
| Gebretsadik et al., 2021 [30] | Amhara | Institutional-based | Health service visitors | 513 | 14.62 | 8 |
| Taye et al., 2020 [15] | Oromia | Institutional-based | Healthcare workers | 423 | 89.6 | 7 |
| Gebremeskel et al., 2021 [36] | Tigray | Community-based | Community | 421 | 32.2 | 7 |
| Dessu et al., 2021 [40] | SNNPs | Community-based | Community | 634 | 82.3 | 8 |
| Ademas et al., 2021 [31] | Amhara | Institutional-based | Healthcare workers | 426 | 68.8 | 8 |
| Shibabaw et al., 2021 [32] | Amhara | Institutional-based | Healthcare workers | 112 | 40.6 | 8 |
| Tadesse et al., 2020 [36] | Addis Ababa | Multicentre cross-sectional | Employee | 628 | 68.8 | 8 |
3.3. Poor level of COVID-19 preventive practice
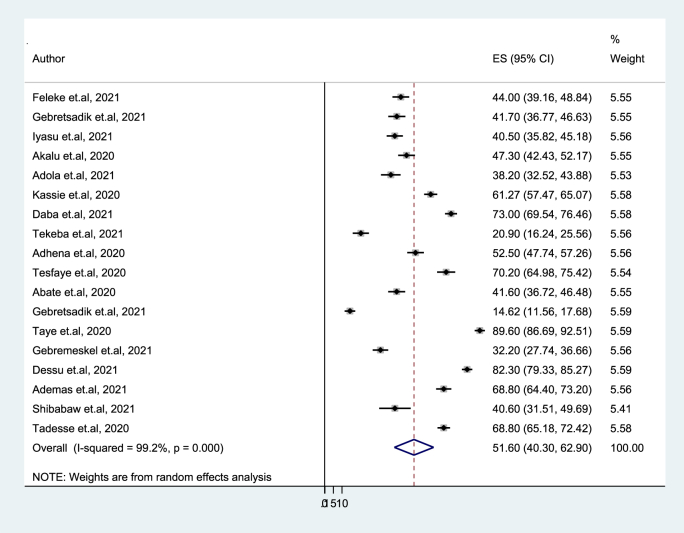
The overall pooled level of poor COVID-19 preventive practice in Ethiopia was 51.60% (95% CI: 40.30–62.90). There was a significant level of heterogeneity among included studies (I2 = 99.2%, p ≤ 0.001) (Fig. 2).
Fig. 2.
Forest plot showing the pooled level of poor COVID-19 preventive practice in Ethiopia.
The midpoint and the length of each segment indicates prevalence and a 95% confidence interval (CI), whereas the diamond shape shows the combined prevalence of all studies.
3.4. Subgroup analysis
The meta-analysis revealed significant levels of heterogeneity; thus, a subgroup analysis was performed to determine the source of heterogeneity. Accordingly, the pooled level of poor preventive practice for COVID-19 in the Oromia region was 55.48%, while in the Amhara region it was 44.99%. The levels of poor COVID-19 preventive practice were higher in studies conducted at the community level (61.82%) than in studies conducted on patients with chronic diseases and visitors to health services. Surprisingly, the level of poor preventive practice for COVID-19 among studies conducted by health professionals was 61.65%. The level of heterogeneity among studies included in each subgroup analysis was high (p < 0.05) (Table 2).
Table 2.
Subgroup analysis on poor levels of COVID-19 preventive practice in Ethiopia.
| Variables | Subgroup | Number of studies | Sample size | Prevalence (95% CI) | I2 (%) | P- value |
|---|---|---|---|---|---|---|
| Region | Amhara | 8 | 3265 | 44.99 (30.76–59.22) | 98.7 | ≤0.001 |
| Oromia | 4 | 1630 | 55.48 (24.96–86.00) | 99.6 | ≤0.001 | |
| Tigray | 3 | 1265 | 41.71 (30.15–53.27) | 94.6 | ≤0.001 | |
| Othersa | 3 | 1557 | 73.87 (64.37–83.38) | 94.6 | ≤0.001 | |
| Study design | Institutional based | 13 | 4978 | 47.66 (33.51–61.81) | 99.3 | ≤0.001 |
| Community based | 4 | 2111 | 60.05 (38.60–81.50) | 99.2 | ≤0.001 | |
| Multicentre | 1 | 682 | 68.80 (65.18–72.42) | – | – | |
| Study population | Healthcare center visitor | 6 | 1985 | 32.50 (19.29–45.71) | 97.8 | ≤0.001 |
| Healthcare workers | 6 | 2167 | 61.65 (46.04–77.27) | 98.6 | ≤0.001 | |
| Patients with chronic diseases | 2 | 826 | 43.87 (37.20–50.53) | 74.3 | 0.049 | |
| Community level | 4 | 2739 | 61.82 (45.42–78.22) | 99.2 | ≤0.001 | |
| Publication year | 2020 | 7 | 3194 | 61.66 (48.26–76.06 | 98.7 | ≤0.001 |
| 2021 | 11 | 4523 | 45.19 (29.63–60.76) | 99.3 | ≤0.001 |
CI, confidence interval.
a Others = Addis Ababa and Southern Nations, Nationalities and Peoples (SNNP) Region.
3.5. A leave-out-one analysis
Due to the significant level of heterogeneity, a sensitivity analysis was carried out by removing each study individually to determine how each one affected the combined estimated prevalence. Accordingly, all of the point estimates are within the overall 95% CI, which confirms that the omission of any one of the studies included in this systematic review and meta-analysis does not affect the overall pooled levels of poor COVID-19 preventive practice (Table 3).
Table 3.
Sensitivity analysis on poor levels of COVID-19 preventive practice in Ethiopia.
| Study omitted, year, ref. | Estimate (95% CI) | Heterogeneity |
|
|---|---|---|---|
| I2 (%) | P-value | ||
| Feleke et al., 2021 [26] | 52.05 (40.21–63.88) | 99.3 | ≤0.001 |
| Gebretsadik et al., 2021 [27] | 52.18 (40.38–63.98) | 99.3 | ≤0.001 |
| Iyasu et al., 2021 [37] | 52.25 (40.45–64.05) | 99.3 | ≤0.001 |
| Akalu et al., 2020 [28] | 51.81 (39.99–63.71) | 99.3 | ≤0.001 |
| Adola et al., 2021 [33] | 52.38 (40.66–64.11) | 99.3 | ≤0.001 |
| Kassie et al., 2020 [17] | 51.03 (38.98–63.07) | 99.3 | ≤0.001 |
| Daba et al., 2021 [35] | 50.33 (38.46–62.21) | 99.3 | ≤0.001 |
| Tekeba et al., 2021 [34] | 53.41 (42.11–64.71) | 99.2 | ≤0.001 |
| Adhena et al., 2020 [14] | 51.55 (39.64–63.45) | 99.3 | ≤0.001 |
| Tesfaye et al., 2020 [39] | 50.51 (38.72–62.29) | 99.3 | ≤0.001 |
| Abate et al., 2020 [29] | 52.19 (40.38–63.99) | 99.3 | ≤0.001 |
| Gebretsadik et al., 2021 [30] | 53.81 (43.88–63.74) | 98.9 | ≤0.001 |
| Taye et al., 2020 [15] | 49.36 (38.70–60.01) | 99.0 | ≤0.001 |
| Gebremeskel et al., 2021(36) | 52.74 (41.10–64.38) | 99.2 | ≤0.001 |
| Dessu et al., 2021 [40] | 49.78 (38.42–61.15) | 99.2 | ≤0.001 |
| Ademas et al., 2021 [31] | 50.59 (38.72–62.45) | 99.3 | ≤0.001 |
| Shibabaw et al., 2021 [32] | 52.23 (40.56–63.90) | 99.3 | ≤0.001 |
| Tadesse et al., 2020 [38] | 50.58 (38.61–62.55) | 99.3 | ≤0.001 |
| Combined | 51.60 (40.30–62.90) | 99.2 | ≤0.001 |
3.6. Publication bias
Potential publication bias of the included studies was assessed visually using a funnel plot. As shown in Fig. 3, the funnel plot is symmetrical and indicates the absence of publication bias because all studies are in the triangular region. In addition, the Egger's regression test result showed no evidence of publication bias (p = 0.121) (Table 4).
Fig. 3.
Funnel plots for publication bias of the studies that were included in the level of poor COVID-19 preventive practice in Ethiopia.
Table 4.
Egger's test assessing publication bias of included studies.
| Std_Eff | Coef. | Std. Err. | T | P > t | 95% CI | |
|---|---|---|---|---|---|---|
| Slope | 91.60 | 22.41 | 4.09 | 0.001 | 44.09 | 139.11 |
| Bias | −17.40 | 10.62 | −1.64 | 0.121 | −39.92 | 5.114 |
CI, confidence interval.
3.7. Factors associated with a poor level of COVID-19 preventive practice
In total, seven studies were used to assess the association between the level of knowledge about COVID-19 and the level of poor COVID-19 preventive practice. Participants with poor COVID-19 knowledge were 5.17 times more likely to have a poor level of COVID-19 preventive practice than participants with good COVID-19 knowledge (adjusted OR [AOR] = 5.17 [95% CI: 2.49–10.73]).
Eight studies were used to evaluate the association between educational level and poor levels of COVID-19 preventive practice. Results showed that participants with a low level of education were 2.93 times more likely to have poor COVID-19 preventive practice than participants with higher levels of education.
Furthermore, participants from rural areas (AOR = 2.95 [95% CI: 2.12–4.12]), participants with a negative attitudes towards COVID-19 management (AOR = 2.64 [95% CI: 1.82–3.82]) and female participants (AOR = 1.75 [95% CI: 1.27–2.40]) were significantly more likely to have a poor level of COVID-19 prevention practice (Table 5).
Table 5.
Odds ratio of factors associated with level of poor COVID-19 preventive practice in Ethiopia.
| Variables | OR (95% CI) | I2 | P-value |
|---|---|---|---|
| Poor COVID-19 knowledge | 5.17 (2.49–10.73 | 89.0% | 0.000 |
| Rural residence | 2.95 (2.12–4.12) | 0.0% | 0.505 |
| Negative attitude towards COVID-19 management | 2.64 (1.82–3.82) | 37.3% | 0.207 |
| Low level of education | 2.93 (2.16–3.98) | 0.0% | 0.955 |
| Female | 1.75 (1.27–2.40) | 0.0% | 0.608 |
OR, Odds ratio; CI, Confidence interval; I2, Heterogeneity.
4. Discussion
COVID-19 is a highly contagious disease that has become a serious public health problem globally. Ethiopia has experienced the rapid spread of COVID-19 [38]. Widespread transmission of the virus is due to poor COVID-19 prevention practices [39]. Thus, this study aimed to estimate the level of poor COVID-19 preventive practice and associated factors in Ethiopia. Estimating the pooled proportion of poor COVID-19 prevention practices will help policymakers plan and implement interventions.
In the current study, the overall pooled level of poor COVID-19 preventive practice in Ethiopia was 51.60% (95% CI: 40.30–62.90). This finding was consistent with previous systematic reviews and meta-analyses in Ethiopia that found the pooled prevalence of poor COVID-19 prevention practice to be 58.3% [40], 40% [41] and 47% [42]. However, when compared with global systematic reviews and meta-analyses, the pooled proportion of poor COVID-19 preventive practice in Ethiopia is higher, with less than a 30% pooled level of poor COVID-19 prevention practice globally [[43], [44], [45], [46]]. The variation could be attributed to poor COVID-19 prevention practices in low-income and developing nations, such as Ethiopia [43].
Subgroup analysis by publication year showed that poor levels of COVID-19 preventive practice declined from 61% in 2020 to 45% in 2021. This result is encouraging for the future prevention of COVID-19 in Ethiopia, but contradicts a systematic review conducted in the global setting [43]. The disparity could be attributed to the fact that the COVID-19 pandemic has only recently emerged in Ethiopia and people have only recently become aware of the pandemic compared to developed countries. Another factor could be the lack of modern sources of pandemic information in developing countries, leading to passive understanding [47].
Poor COVID-19 preventive practice has been found to be more prevalent in community-based studies than in studies of patients with chronic disease patients and visitors to health services. This may be due to good institutional preventative procedures compared with practices in communities; this finding is similar to the results of Azene et al. [40]. However, a subgroup analysis revealed that 61.65% of health professionals had a significant degree of inadequate preventive practice. This finding contradicts results of earlier systematic reviews and meta-analyses conducted in Ethiopia [41]. This could be due to the long duration of the pandemic, which makes it more difficult for healthcare providers to continue to follow and maintain COVID-19 prevention practices. Furthermore, a decrease in perceived vulnerability to and severity of COVID-19 may decrease COVID-19 preventive practice by health professionals [48].
In the present study, there is a positive association between poor knowledge about COVID-19 and poor preventive practice. Studies conducted by Gebretsadik et al. [27], Desalegn et al. [49] and Dessu et al. [37] support these findings. Participants with less knowledge about COVID-19 made fewer attempts to engage in various preventive behaviours, such as wearing a facemask in public, washing hands and social distancing [50]. Similarly, a poor attitude towards COVID-19 management contributes to a poor level of COVID-19 prevention practice. This finding corresponds with previous studies conducted in Ethiopia [14,26]. Individuals were more likely to participate in inefficient COVID-19 preventative actions when they had a negative attitude and low expectations for COVID-19 management [51].
Women are more likely to have poor COVID-19 preventive practices than men. This finding is in line with other studies conducted in Cameron [52]. One possible reason for this result could be that females have a lower level of education in Ethiopia [53], which leads to inadequate knowledge and poor practice towards COVID-19 [26]. This suggests that health promotion strategies should aim to improve the level of COVID-19 preventive practice, especially in the female population.
Participants from rural areas are more likely have poor COVID-19 preventive practices than urban participants. This finding is consistent with results from a study conducted in Southern Ethiopia [54]. This could be due to low socio-economical level, lack of media coverage about the impact of COVID-19 and negligence in rural areas [54]. In addition, low educational levels among the rural population increases the level of poor COVID-19 preventive efforts. Individuals living in rural areas may also experience limited access to preventive materials, such as facemasks, disinfectants and other personal protective equipment, which play an important role in the preventive practice of COVID-19 [55].
A low level of education was also associated with a poor level of COVID-19 preventive practices. This finding is similar to previous single-centre studies conducted in Ethiopia [[55], [56], [57]]. A possible reason for this result might be that educated people can access information from the internet since they may work in different organisations and discuss the issue openly [55]. Participants who have a low level of education might also use the preventive measures inappropriately due to their limited education, even if they have access to the materials.
The current study has some limitations. First, all of the studies included in this analysis are cross-sectional in nature; thus, it is difficult to establish a causal relationship between the independent and dependent variables. Second, the high level of heterogeneity among included studies could potentially limit the findings of this study.
5. Conclusions
More than half of the study participants in Ethiopia showed an inadequate level of COVID-19 preventive practice; however, the poor levels of COVID-19 preventive practice declined from 2020 to 2021. Surprisingly, a subgroup analysis revealed that 61.65% of health professionals had a significant degree of poor COVID-19 preventive practice. Inadequate knowledge and a negative attitude towards COVID-19 management, as well as a low educational level, rural residence and being female, were all associated with poor COVID-19 prevention practice. Creating awareness and health education programmes targeting COVID-19 prevention should be strengthened, especially in the target populations identified in this study.
Ethical approval
Not applicable.
Funding
None declare.
Competing interests
The authors declare that there are no conflicts of interest.
Availability of data and materials
The datasets are available within the manuscript and its supporting materials.
Author contributions
SG and MDT were involved in the design, conducted the review, data analysis, interpretation of the findings and drafted the manuscript. MM and TA were involved in drafting the manuscript, reviewing and editing the manuscript. All the authors critically revised the paper and agreed to be accountable for all aspects of the work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhip.2022.100329.
Contributor Information
Masresha Derese Tegegne, Email: masrederese@gmail.com.
Mamaru Melkam, Email: mamarumelkam@gmail.com.
Tiruneh Adane, Email: tirunehadane01@gmail.com.
Solomon Getawa, Email: solomon.getawa@uog.edu.et.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.McIntosh K., Hirsch M.S., Bloom A. Coronavirus disease 2019 (COVID-19) UpToDate Hirsch MS Bloom. 2020;5(1) [Google Scholar]
- 2.Di Gennaro F., Pizzol D., Marotta C., Antunes M., Racalbuto V., Veronese N., et al. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int. J. Environ. Res. Publ. Health. 2020;17(8):2690. doi: 10.3390/ijerph17082690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amgain K., Neupane S., Panthi L., Thapaliya P. Myths versus truths regarding the novel coronavirus disease (COVID-2019) outbreak. J. Karnali Acad. Health Sci. 2020;3(1) [Google Scholar]
- 4.Ingram C., Downey V., Roe M., Chen Y., Archibald M., Kallas K.-A., et al. COVID-19 prevention and control measures in workplace settings: a rapid review and meta-analysis. Int. J. Environ. Res. Publ. Health. 2021;18(15):7847. doi: 10.3390/ijerph18157847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhong N., Zheng B., Li Y., Poon L., Xie Z., Chan K., et al. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People's Republic of China, in February, 2003. Lancet. 2003;362(9393):1353–1358. doi: 10.1016/S0140-6736(03)14630-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olson D.R., Huynh M., Fine A., Baumgartner J., Castro A., Chan H.T., et al. 2020. Preliminary Estimate of Excess Mortality during the COVID-19 Outbreak—New York City. March 11–May 2, 2020. [DOI] [PubMed] [Google Scholar]
- 7.Bekele D., Tolossa T., Tsegaye R., Teshome W. The knowledge and practice towards COVID-19 pandemic prevention among residents of Ethiopia. An online cross-sectional study. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0234585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahman A., Sathi N.J. Knowledge, attitude, and preventive practices toward COVID-19 among Bangladeshi internet users. Electr. J. General Med. 2020;17(5) [Google Scholar]
- 9.Tadesse A.W., Abebe N.M., Tadesse S.E., Wube M.C., Abate A.A. Preventive practice and associated factors towards COVID-19 among college students in Amhara region, Ethiopia: a cross-sectional study. Ethiopian J. Health Sci. 2021;31(1) doi: 10.4314/ejhs.v31i1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jemal B., Ferede Z.A., Mola S., Hailu S., Abiy S., Wolde G.D., et al. 2020. Knowledge, Attitude and Practice of Healthcare Workers towards COVID-19 and its Prevention in Ethiopia: a Multicenter Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adhena G., Hidru H.D. Knowledge, attitude, and practice of high-risk age groups to Coronavirus Disease-19 prevention and control in Korem District, Tigray, Ethiopia: cross-sectional study. Infect. Drug Resist. 2020;13:3801. doi: 10.2147/IDR.S275168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taye G.M., Bose L., Beressa T.B., Tefera G.M., Mosisa B., Dinsa H., et al. COVID-19 knowledge, attitudes, and prevention practices among people with hypertension and diabetes mellitus attending public health facilities in Ambo, Ethiopia. Infect. Drug Resist. 2020;13:4203. doi: 10.2147/IDR.S283999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dagne H., Alemu K.A., Dagnew B., Taddesse D., Alemayehu A.M., Andualem Z., et al. 2020. Prevention Practice and Associated Factors of Coronavirus Disease 2019 (COVID-19) Outbreak Among Educated Ethiopians: an Online Based Cross-Sectional Survey. [Google Scholar]
- 14.Kassie B.A., Adane A., Abebe Kassahun E., Ayele A.S., Kassahun Belew A. Poor COVID-19 preventive practice among healthcare workers in Northwest Ethiopia. Adv. Public Health. 2020:2020. 2020. [Google Scholar]
- 15.Gilbert M., Pullano G., Pinotti F., Valdano E., Poletto C., Boëlle P.-Y., et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395(10227):871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdelhafiz A.S., Mohammed Z., Ibrahim M.E., Ziady H.H., Alorabi M., Ayyad M., et al. Knowledge, perceptions, and attitude of Egyptians towards the novel coronavirus disease (COVID-19) J. Community Health. 2020;45(5):881–890. doi: 10.1007/s10900-020-00827-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mersha A., Shibiru S., Girma M., Ayele G., Bante A., Kassa M., et al. Health professionals practice and associated factors towards precautionary measures for COVID-19 pandemic in public health facilities of Gamo zone, southern Ethiopia: a cross-sectional study. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0248272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys. Ther. 2009;89(9):873–880. [PubMed] [Google Scholar]
- 19.Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Base. Healthc. 2015;13(3):147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 20.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta‐analysis. Stat. Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterne J.A., Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J. Clin. Epidemiol. 2001;54(10):1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 23.Feleke B.T., Wale M.Z., Yirsaw M.T. Knowledge, attitude and preventive practice towards COVID-19 and associated factors among outpatient service visitors at Debre Markos compressive specialized hospital, north-west Ethiopia, 2020. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0251708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gebretsadik D., Gebremichael S., Belete M.A. Knowledge, attitude and practice toward covid-19 pandemic among population visiting dessie health center for covid-19 screening, northeast Ethiopia. Infect. Drug Resist. 2021;14:905. doi: 10.2147/IDR.S297047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Akalu Y., Ayelign B., Molla M.D. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infect. Drug Resist. 2020;13:1949. doi: 10.2147/IDR.S258736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abate H., Mekonnen C.K. Knowledge, attitude, and precautionary measures towards covid-19 among medical visitors at the university of gondar comprehensive specialized hospital northwest Ethiopia. Infect. Drug Resist. 2020;13:4355. doi: 10.2147/IDR.S282792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gebretsadik D., Ahmed N., Kebede E., Gebremicheal S., Belete M.A., Adane M. Knowledge, attitude, practice towards COVID-19 pandemic and its prevalence among hospital visitors at Ataye district hospital, Northeast Ethiopia. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246154. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 28.Ademas A., Adane M., Keleb A., Berihun G., Lingerew M., Sisay T., et al. COVID-19 prevention practices and associated factors among diabetes and HIV/AIDS Clients in South-Wollo zone, Ethiopia: a health facility-based cross-sectional study. J. Multidiscip. Healthc. 2021;14:2079. doi: 10.2147/JMDH.S325207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shibabaw T., Teferi B. Knowledge and practice toward prevention of SARS-CoV-2 among healthcare workers at Delghi primary hospital during a massive test Campaign in northwest gondar, Ethiopia: institution-based Descriptive cross-sectional survey. Infect. Drug Resist. 2021;14:381. doi: 10.2147/IDR.S289965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adola S.G., Degavi G., Edwin S.E.K., Utura T., Gemede U., Kasimayan P. Assessment of factors affecting practice towards COVID-19 among health care workers in health care facility of West Guji Zone, South Ethiopia. Pan African Med. J. 2020;39 doi: 10.11604/pamj.2021.39.53.27798. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tekeba T. 2021. Knowledge, Attitude, and Practice towards COVID-19 Among Antenatal Care Clients of Adama Hospital Medical College, Adama, Ethiopia: A Cross Sectional Study. [Google Scholar]
- 32.Daba A., Yazew T., Kibr G., Gebissa B. Knowledge, attitude and preventive practice (KAP) towards covid-19 pandemic among the residents from Western Oromia, Ethiopia: cross sectional survey study. J. Biology Today's World. 2021;10(7):1–5. [Google Scholar]
- 33.Gebremeskel F., III, Teklay E., Gebrehaweria M. Preventive practice and associated factors toward coronavirus disease 19 in Adigrat Town, northern Ethiopia: community-based cross-sectional study. Infect. Drug Resist. 2021;14:2379. doi: 10.2147/IDR.S288941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iyasu A., Kidanu B.H., Zereabruk K. Knowledge, attitude, and practice towards COVID-19 among chronic disease patients at Aksum Hospital, Northern Ethiopia, 2020: a cross-sectional study. Asthma Res. Practice. 2021;7(1):1–9. doi: 10.1186/s40733-021-00074-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tadesse T., Alemu T., Amogne G., Endazenaw G., Mamo E. Predictors of Coronavirus Disease 2019 (COVID-19) prevention practices using health belief model among employees in Addis Ababa, Ethiopia, 2020. Infect. Drug Resist. 2020;13:3751. doi: 10.2147/IDR.S275933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tesfaye Z.T., Yismaw M.B., Negash Z., Ayele A.G. COVID-19-related knowledge, attitude and practice among hospital and community pharmacists in Addis Ababa, Ethiopia. Integrated Pharm. Res. Pract. 2020;9:105. doi: 10.2147/IPRP.S261275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dessu S., Tsehay T., Girum T., Timerga A., Solomon M., Tsegaye B., et al. The applicability of basic preventive measures of the pandemic COVID-19 and associated factors among residents in Guraghe Zone. PLoS One. 2021;16(8) doi: 10.1371/journal.pone.0256598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.ŠTĚPÁNKOVÁ L. Effects of COVID-19 Pandemic on Current Globalized International System.
- 39.Brauer M., Zhao J.T., Bennitt F.B., Stanaway J.D. Global access to handwashing: implications for COVID-19 control in low-income countries. Environ. Health Perspect. 2020;128(5) doi: 10.1289/EHP7200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Azene A.G., Workie M.S., Aragaw A.M. Knowledge, attitude, and prevention practice towards Covid-19 in Ethiopia: systematic review and Meta-analysis. Curr. Ther. Res. 2021 doi: 10.1016/j.curtheres.2021.100633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lake E.A., Demissie B.W., Gebeyehu N.A., Wassie A.Y., Gelaw K.A., Azeze G.A. Knowledge, attitude and practice towards COVID-19 among health professionals in Ethiopia: a systematic review and meta-analysis. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0247204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yazew B.G., Abate H.K., Mekonnen C.K. Knowledge, attitude and practice towards COVID-19 in Ethiopia: a systematic review. Patient Prefer. Adherence. 2020;15:337. doi: 10.2147/PPA.S288186. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siddiquea B.N., Shetty A., Bhattacharya O., Afroz A., Billah B. Global epidemiology of COVID-19 knowledge, attitude and practice: a systematic review and meta-analysis. BMJ Open. 2021;11(9) doi: 10.1136/bmjopen-2021-051447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bekele F., Sheleme T., Fekadu G., Bekele K. vol. 8. SAGE open medicine; 2020. (Patterns and Associated Factors of COVID-19 Knowledge, Attitude, and Practice Among General Population and Health Care Workers: a Systematic Review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hesaraki M., Akbarizadeh M., Ahmadidarrehsima S., Moghadam M.P., Izadpanah F. Reviews on Environmental Health; 2020. Knowledge, Attitude, Practice and Clinical Recommendations of Health Care Workers towards COVID-19: A Systematic Review. [DOI] [PubMed] [Google Scholar]
- 46.Tegegne G.T., Kefale B., Engidaw M.T., Degu A., Tesfa D., Ewunetei A., et al. Knowledge, attitude, and practice of healthcare providers toward novel coronavirus 19 during the first months of the pandemic: a systematic review. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.606666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baye K. Intl Food Policy Res Inst; 2020. COVID-19 Prevention Measures in Ethiopia: Current Realities and Prospects. [Google Scholar]
- 48.Morgul E., Bener A., Atak M., Akyel S., Aktaş S., Bhugra D., et al. COVID-19 pandemic and psychological fatigue in Turkey. Int. J. Soc. Psychiatr. 2021;67(2):128. doi: 10.1177/0020764020941889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Desalegn Z., Deyessa N., Teka B., Shiferaw W., Hailemariam D., Addissie A., et al. COVID-19 and the public response: knowledge, attitude and practice of the public in mitigating the pandemic in Addis Ababa, Ethiopia. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0244780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li S., Feng B., Liao W., Pan W. Internet use, risk awareness, and demographic characteristics associated with engagement in preventive behaviors and testing: cross-sectional survey on COVID-19 in the United States. J. Med. Internet Res. 2020;22(6) doi: 10.2196/19782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhong B.-L., Luo W., Li H.-M., Zhang Q.-Q., Liu X.-G., Li W.-T., et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int. J. Biol. Sci. 2020;16(10):1745. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ngwewondo A., Nkengazong L., Ambe L.A., Ebogo J.T., Mba F.M., Goni H.O., et al. Knowledge, attitudes, practices of/towards COVID 19 preventive measures and symptoms: a cross-sectional study during the exponential rise of the outbreak in Cameroon. PLoS Neglected Trop. Dis. 2020;14(9) doi: 10.1371/journal.pntd.0008700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Project T.B. The rise and fall of girls’ education. https://borgenproject.org/the-rise-and-fall-of-girls-education-in-ethiopia/ IN ETHIOPIA 2018 [cited 2021 December 18]. Available from:
- 54.Bante A., Mersha A., Tesfaye A., Tsegaye B., Shibiru S., Ayele G., et al. Adherence with COVID-19 preventive measures and associated factors among residents of Dirashe district, southern Ethiopia. Patient Prefer. Adherence. 2021;15:237. doi: 10.2147/PPA.S293647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Asemahagn M.A. Factors determining the knowledge and prevention practice of healthcare workers towards COVID-19 in Amhara region, Ethiopia: a cross-sectional survey. Trop. Med. Health. 2020;48(1):1–11. doi: 10.1186/s41182-020-00254-3. 020) 48:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tesfaye A., Asefa B., Gebremeskel G., Washo A., Muche T. 2021. Adherence with COVID-19 Preventive Measures and Associated Factors Among Residents of Shashemane, Central Ethiopia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ayele A.D., Mihretie G.N., Belay H.G., Teffera A.G., Kassa B.G., Amsalu B.T. Knowledge and practice to prevent COVID-19 and its associated factors among pregnant women in Debre Tabor Town Northwest Ethiopia, a community-based cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):1–12. doi: 10.1186/s12884-021-03877-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets are available within the manuscript and its supporting materials.