Abstract
Background
Physical child abuse affects 9 in every 1,000 children in the United States and associated traumatic injuries are often identified by the healthcare system. The COVID-19 pandemic has intensified risk factors for physical child abuse and increased avoidance of the healthcare system. This study examined the effect of the COVID-19 pandemic on presentation and severity of physical child abuse.
Methods
A retrospective, cross-sectional study utilizing the Pediatric Health Information System was performed. An interrupted time series analysis estimated the effect of the COVID-19 pandemic on the number of children <15 years old presenting with physical child abuse to children's hospitals from March 1st to June 30th of 2020 by comparing to those presenting during the same period for years 2016–2019. Hierarchical regression models estimated the effect of the pandemic on likelihood of operative intervention, ICU admission, traumatic brain injury, and mortality.
Results
Over the study period, 20,346 physical child abuse encounters were reported by 47 children's hospitals. An interrupted times series model predicted a significant decline in cases due to the effect of the COVID-19 pandemic, representing a deficit of 2,645 cases (p = 0.001). Children presenting during the pandemic had increased odds of requiring ICU admission (p = 0.03) and having a traumatic brain injury in those under 5 years of age (p=<0.001).
Conclusions
The number of children with physical child abuse presenting to children's hospitals significantly declined during the COVID-19 pandemic, but those that did were more likely to be severe. The pandemic may be a risk factor for worse outcomes associated with physical child abuse.
Keywords: Non-accidental trauma in children, Child abuse, COVID-19
Abbreviations: COVID-19, Coronavirus disease 2019; ED, Emergency department; PHIS, Pediatric Health Information System; ICD, International Classification of Disease; ICU, Intensive Care Unit
1. Background
Physical child abuse affects 9 in every 1000 children in the United States and is a leading cause of death in children under the age of 15 [1], [2], [3], [4]. In 2018, there were 678,000 reports of child abuse cases and 1770 deaths [2]. Risk factors for physical child abuse are well documented in the literature and can be described as intrinsic to the patient, abuser, or society as a whole [5,6]. Societal risk factors include parental perception of lack of community support, job loss, life stressors, and poverty [7,8]. Prior literature has shown the significant effect of economic recession on increased rates and severity of physical child abuse [9].
With the advent of the COVID-19 pandemic, the aforementioned risk factors associated with physical child abuse were quickly intensified as states issued stay-at-home orders beginning in early March [10]. By May 2020, over 21 million U.S. residents had lost their jobs, and the unemployment rate peaked at 14.7 percent [11]. Concerns for and reported increases in rates of domestic violence and child maltreatment were reported by media outlets and academic journals [12], [13], [14], [15]. The COVID-19 pandemic was identified early as a potential risk factor for increased physical child abuse.
Simultaneously, the pandemic also increased avoidance of the healthcare system. At one urban, tertiary pediatric emergency department (ED), the mean daily visits dropped by over 50% in the first 30 days after stay-at-home orders, and those who did present to the ED had higher acuity [16]. This is important with respect to physical child abuse, as medical personnel are an essential source of many child abuse referrals in the US, ranking among law enforcement and schools as highest reporters [2]. Therefore, our aims were to 1) describe the trend of overall cases of physical child abuse presenting to a group of tertiary children's hospitals during the COVID-19 pandemic and 2) characterize the severity of physical child abuse on presentation. We hypothesized that there was a significant decrease in physical child abuse cases and that those who presented were more likely to be severe than in previous years.
2. Methods
2.1. Study design, data, and population
This is a retrospective, cross-sectional study using data obtained from the Pediatric Health Information System (PHIS), an administrative database containing de-identified patient data from over 52 children's hospitals maintained by the Child Health Corporation of America (Shawnee Mission, KS). PHIS is updated monthly, and its hospitals represent 29 states, making it uniquely positioned as one of the most comprehensive and readily updated databases for multi-institutional pediatric health outcomes for analyzing COVID-19 trends. The study population included children <15 years old who presented to a PHIS hospital with a diagnosis of physical child abuse or traumatic injury associated with physical child abuse. To identify diagnoses of physical child abuse, International Classification of Disease (ICD) diagnosis codes were extracted using previously validated and collected codes for physical child abuse [17]. These included general diagnoses of child abuse, as well as codes for specific mechanisms of abuse including assault with or without a weapon/object, burns, assault via drowning, and assault via poisoning (see Supplemental Files for codes utilized). Cases were included if they had both a code for abuse or assault and injury, retinal hemorrhage, or anoxic brain injury consistent with previous studies [17,18,30]. To eliminate cases of assault by peers, cases which had ICD-10-CM codes occurring at school were excluded. Other types of abuse, such as sexual, verbal, psychologic, and emotional abuse etc., were not included [17]. Only data after 2016 were included to reduce the known bias and potential underestimation of case rates based on ICD-9-CM codes previously documented in the literature [18].
Encounters classified as “ED Visit”, “Observation”, and “Inpatient” were included. Hospitals that did not have data updated through the second quarter of 2020 or ones that had missing data for encounter types and variables of interest were excluded. March 1st was used as a starting point based on the earliest stay-at-home orders that were put in place to best estimate the time where the effects of the COVID pandemic would influence physical child abuse presentation [15]. The time period was limited to encounters from March 1st to June 30th for each of the years from 2016 to 2020, respectively, to eliminate bias of seasonal variation.
2.2. Primary and secondary outcomes
Frequency of physical child abuse cases by year was the primary outcome of interest. Traumatic brain injury (TBI) in the <5 years old population, need for operative intervention, Intensive Care Unit (ICU) admission, and mortality were utilized as proxies for severity of physical child abuse and were the secondary outcomes of interest. We chose to analyze TBI in the under 5 years old group as a sensitive indicator of severity of physical child abuse based on prior studies [9,24] Data from PHIS extracted included demographics, such as age, sex, race, census region, and insurance payer type [17]. The study was deemed exempt from full review by our institution's International Review Board.
2.3. Data analyses
Descriptive statistics were used for demographics and clinical outcomes, including sex, age, race, insurance payer type, census region, need for operation, ICU admission, and mortality. Chi-square for categorical variables and student's t-test for continuous variables were used for uni-variate analyses to examine differences in patients with physical child abuse who presented during the COVID pandemic versus previous years. An interrupted time series model with cases of physical child abuse by month over the time periods collected was used to model the change in physical child abuse over time and estimate the effect of the COVID pandemic on the case trend.
To assess whether cases in the COVID-19 year were more likely to be severe than in prior years, four hierarchical multivariate regression models with patients nested within individual hospitals were estimated. In these models, the odds ratios (OR) for the likelihood of outcome (TBI < 5 years old, operative intervention, ICU admission, and mortality) during the COVID pandemic was compared to year 2016 as the reference year. TBI was defined as a case with one of the following ICD-10-CM diagnosis codes: T744XXA, S062XOA, S062X9A, S065X9A, S066X9A, S06300A, which includes the previously utilized clinical term “shaken baby syndrome”. Each of these also had a coinciding ICD-10-CM diagnosis of physical child abuse.
The models were adjusted for age, sex, race, payer type, and census region as covariates, and included a random intercept for each hospital. Adjusted odds ratios were reported with associated confidence intervals (CIs). Covariates were chosen based on prior literature and this study's uni-variate analysis demonstrating risk factors for physical child abuse. Significance was set at a p-value of 0.05. Analyses were conducted in SAS v 9.5 (SAS Institute, Cary, NC).
2.4. Sensitivity analysis
To test the robustness of the findings, a sensitivity analysis was performed to determine if the same trends were observed in two sub-groups. Interrupted time series models were created to estimate the effect of the pandemic on case numbers for children <5 years old and for children who had an ICD-10-CM diagnosis of unspecified physical child abuse (ICD10 codes: T7492XA, T7692XA, T7412XA, T7612XA), which excluded all “assault” codes.
3. Results
3.1. Descriptive statistics
Over the study period, there were 20,346 total encounters for physical child abuse identified across 47 children's hospitals. In this cohort, the mean age was 7.7 years (standard deviation: 5.6), and 58.04% (n = 11,891) were male. Patients were predominantly Black race (41.4%, n = 8415), from the South census region (39.2%, n = 7974), and were public insurance payers (71.7%, n = 14,592). (See supplemental Files for frequencies of injury types)
In a univariate analysis comparing 2020 to years prior (Table 1 ), patients who presented during the COVID pandemic were more likely to be younger (p=<0.001), either be White or “other” race (p=<0.001), have longer length of stay (p=<0.001), either be from the South and West census regions (p=<0.001), require operative intervention (p=<0.001), be admitted to the ICU (p=<0.001), and to have traumatic brain injury if they were <5 years old. No difference was observed in sex or mortality between groups.
Table 1.
Comparison of demographics and outcomes of 2016–2019 versus 2020 for encounters of physical child abuse presenting to 47 tertiary children's hospital with associated frequencies, percentages, and p-values for chi-square and student's t-tests, respectively. (N = number, ICU = intensive care unit).
| Total | 2016–2019 | 2020 | p-value | |
|---|---|---|---|---|
| N = 20,346 | N = 17,761 | N = 2585 | ||
| Length of Stay | 2.5 (8.8) | 2.4 (8.7) | 3.2 (9.7) | <0.001 |
| Age | 7.7 (5.6) | 7.9 (5.5) | 6.4 (5.7) | <0.001 |
| Age | <0.001 | |||
| 0–5 years | 40% (8158) | 38% (6792) | 53% (1366) | |
| 6–10 years | 17% (3500) | 18% (3148) | 14% (352) | |
| 11–15 years | 43% (8688) | 44% (7821) | 34% (867) | |
| Sex | 0.79 | |||
| Male | 58.4% (11,891) | 58.4% (10,377) | 58.6% (1514) | |
| Female | 41.5% (8441) | 41.5% (7377) | 41.2% (1064) | |
| Race/Ethnicity | <0.001 | |||
| White, non-Latino | 40.3% (8208) | 39.5% (7022) | 45.9% (1186) | |
| Black | 41.4% (8415) | 42.0% (7460) | 36.9% (955) | |
| Non-White, Latino | 2.6% (535) | 2.7% (487) | 1.9% (48) | |
| Asian | 1.2% (251) | 1.2% (205) | 1.8% (46) | |
| Other | 11.6% (2362) | 11.8% (2093) | 10.4% (269) | |
| Census Region | <0.001 | |||
| Midwest | 28.4% (5771) | 28.6% (5078) | 26.8% (693) | |
| Northeast | 14.2% (2891) | 14.5% (2582) | 12.0% (309) | |
| South | 39.2% (7974) | 39.0% (6923) | 40.7% (1051) | |
| West | 18.2% (3710) | 17.9% (3178) | 20.6% (532) | |
| Payer Status | 0.005 | |||
| Public | 71.7% (14,592) | 71.8% (12,749) | 71.3% (1843) | |
| Private | 15.7% (3202) | 15.9% (2826) | 14.5% (376) | |
| Self-Pay | 5.9% (1197) | 5.9% (1042) | 6.0% (155) | |
| Other | 6.7% (1355) | 6.4% (1144) | 8.2% (211) | |
| Mortality | 0.13 | |||
| No | 99.0% (20,136) | 99.0% (17,585) | 98.7% (2551) | |
| Yes | 1.0% (210) | 1.0% (176) | 1.3% (34) | |
| Underwent Operative Intervention | <0.001 | |||
| No | 98.0% (19,944) | 98.0% (17,412) | 97.9% (2532) | |
| Yes | 1.6% (320) | 1.5% (267) | 2.1% (53) | |
| ICU Stay | <0.001 | |||
| No | 94.0% (19,116) | 94.4% (16,764) | 91.0% (2352) | |
| Yes | 6.0% (1230) | 5.6% (997) | 9.0% (233) | |
| Traumatic Brain Injury <5 years old | <0.001 | |||
| No | 97.9% (19,914) | 98.1% (17,425) | 96.3% (2489) | |
| Yes | 2.1% (432) | 1.9% (336) | 3.7% (96) |
3.2. Effect of COVID-19 pandemic on number of reported physical child abuse cases
Interrupted time-series analysis showed a gradual increase in yearly cases of physical child abuse from 2016 to 2019, and a statistically significant decrease in 2020 during the pandemic (Fig. 1 , p = 0.001). Based on the model, 2645 fewer cases were reported compared to those predicted during the pandemic in 2020.
Fig. 1.
Interrupted time series model with observed and predicted values, trend, and mean number of cases of physical child abuse in children <15 years old presenting to 47 tertiary children's hospitals each month from March to June from 2016 to 2020. (95% CI = 95% Confidence Interval).
3.3. Effect of COVID-19 pandemic on severity of outcomes of reported physical child abuse cases
After controlling for covariates, hierarchical multivariate logistic regression demonstrated increased odds of ICU admission (adjusted OR: 1.26, 95%CI: 1.02–1.57, p = 0.03) and traumatic brain injury in children <5 years old (adjusted OR: 1.33, 95%CI: 1.26–1.4, p = 0.001) for patients presenting with physical child abuse during the COVID pandemic (Table 2 ). Odds of operative intervention (adjusted OR: 1.14, 95% CI: 0.92–1.42, p = 0.23) and increased mortality (adjusted OR: 1.12, 95% CI: 0.69–1.83, p = 0.641) were not significant after controlling for the same variables.
Table 2.
Multivariate regression models for predicting odds of traumatic brain injury (TBI) in children under 5 years old, operative intervention, ICU admission, and mortality for physical child abuse during the COVID-19 pandemic. Covariates included age, sex, race, insurance status, and census region. (TBI = traumatic brain injury, 95% CI = 95% confidence intervals).
| Odds Ratio | 95%CI | p-value | |
|---|---|---|---|
| TBI < 5 years old | 1.33 | 1.26–1.41 | <0.001* |
| ICU Admission | 1.26 | 1.05–1.58 | 0.02* |
| Operative Intervention | 1.14 | 0.92–1.42 | 0.23 |
| Mortality | 1.12 | 0.69–1.82 | 0.64 |
3.4. Sensitivity analysis
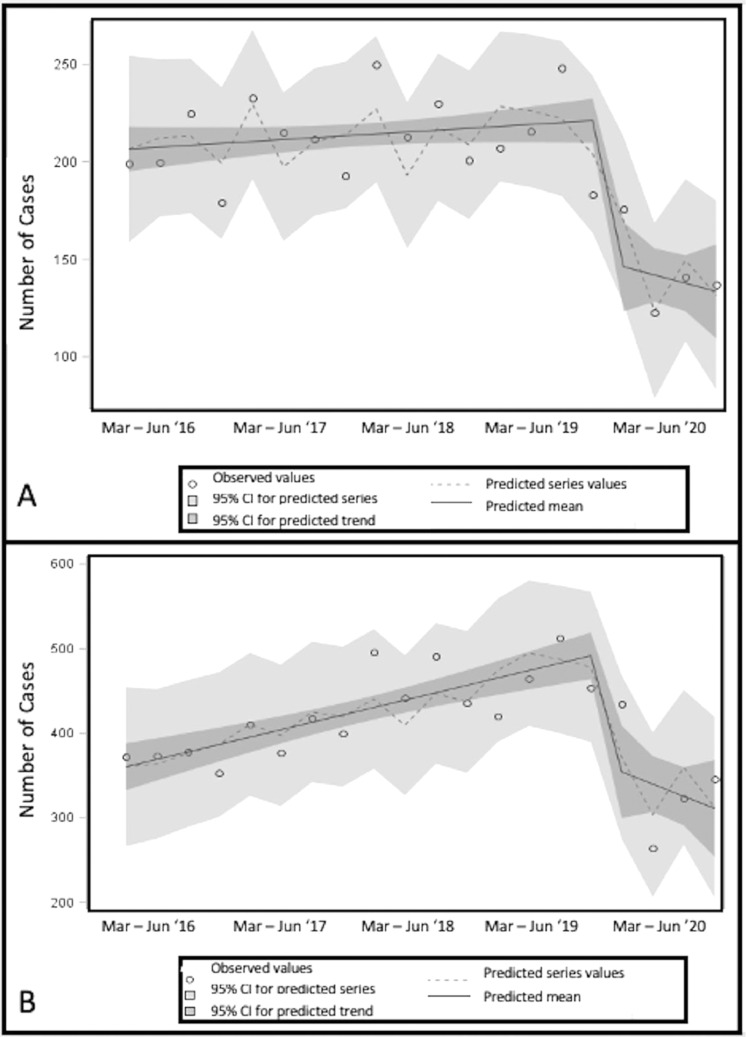
Interrupted time series models revealed significant decreases of cases of physical child abuse in children <5 years old and in children who had a primary diagnosis of confirmed or suspected physical child abuse after excluding those cases with “assault” codes (Fig. 2 ). For children <5 years old, an interrupted time series model predicted 724 fewer cases as the result of the pandemic (p = 0.01), and in children who had a specific ICD10 diagnosis of child abuse, the model predicted 334 fewer cases (<0.001).
Fig. 2.
Sensitivity Analysis: Interrupted time series models with observed and predicted values, trend, and mean number of cases of physical child abuse for A.) children <5 years old and B.) children <15 years old who had an ICD10-CM specific for child abuse (“assault” codes omitted) presenting to 47 tertiary children's hospitals each month from March to June from 2016 to 2020. (95% CI = 95% Confidence Interval, Mar = March, Jun = June).
4. Discussion
In this study we sought to examine the effects of the COVID-19 pandemic on the overall presentation of physical child abuse at tertiary children's hospitals in the US and characterize the severity of those cases that did present. We found that overall cases of physical child abuse significantly decreased during the COVID-19 pandemic, and these cases were more likely to be severe as evidenced by increased odds of ICU admission and traumatic brain injury in children <5 years old. These results have important clinical and policy implications.
To our knowledge, this is the first study to describe national, multi-institutional physical child abuse trends during the COVID pandemic. Most previous findings of increasing rates of physical child abuse have been limited to reports, news articles, and smaller institution-specific studies [12], [13], [14], [15]. The statistically significant decrease in physical child abuse during the COVID-19 pandemic is concerning, as our time-series model predicted a deficit of nearly 3000 cases of physical child abuse during the first 4 months of the pandemic, which was consistent in sub-group sensitivity analysis (Figs. 1 and 2). Given the known exacerbation of risk factors during the pandemic [15], it is highly unlikely that this represents a true decrease of physical child abuse in the community. Rather, this decrease is likely a result of fewer physical child abuse cases captured within the healthcare system due to avoidance of the healthcare system during the pandemic [19,20], as well as cancellation of routine and elective healthcare visits and procedures where physical child abuse is incidentally discovered by providers. The importance of this cannot be understated as recurrent physical child abuse is known to be more severe with increased risk of mortality [1,21]. Not identifying many of these cases early and breaking the cycle of abuse could potentially lead to increased morbidity and mortality.
While prior literature examining rates of traumatic injuries due to physical child abuse during a global pandemic is limited, our study is consistent with recent reports that suggest overall presentation to healthcare systems is decreased across age groups and pathologies, including in children where more severe disease has also been observed [16,19,20]. One report found a ten-fold increase in traumatic head injury at a single institution in the United Kingdom. Further research will be needed to determine if the trend of increased TBI in the context of decreased overall presentation of physical child abuse is affected by the local setting, both within and outside the United States [15]. Our findings are concordant with the literature regarding risk factors for physical child abuse [5], [6], [7], [8], although subtle differences were found in our analysis that may be related to factors associated with the regional and temporal differences in the spread of COVID-19 and resulting political and socioeconomic factors. We found that younger age, public insurance, and geographic location were associated with increased physical child abuse during the COVID-19 pandemic (Table 1) [22], [23], [24]. Rates decreased the most in the Northeast Census Region which may be related to the earliest emergence of the pandemic and associated stay-at-home orders [10]. Interpretations of race or ethnicity as a risk factor are notoriously difficult in the literature due to the competing factors of socioeconomic systems that disadvantage minority groups, affecting rates of physical child abuse and, conversely, racial bias in surveillance and reporting of physical child abuse that may disproportionately inflate the rates of physical child abuse in minority groups [[25], [26], [27]]. The intricate interplay between these factors in the midst of the COVID-19 pandemic, which has not affected racial groups equally [28], needs to be examined to further interpret our findings. In particular, Latino and Black children face the intersection of these factors along with the unequal burden of COVID-19 infection [29].
This study also shows that those who presented to the healthcare system were more likely to have severe physical child abuse during the pandemic than in prior years. We found increased odds of ICU admission and traumatic brain injury in children <5 years old during the COVID-19 pandemic (Tables 1 and 2). We recognize that the increasing severity of physical child abuse presenting to children's hospitals during the pandemic is likely due to decreased presentation of more minor physical child abuse, but should nevertheless serve as an alarm that novel systems of case identification in the community are urgently needed to break cycles of abuse. If typical interfaces with the healthcare and education systems are not occurring for more minor cases, new methods of identification of physical child abuse both within healthcare and in the community should be considered, such as screening via telemedicine, school, or home visits and community outreach for high-risk children. As the pandemic continues, trends of severity should be monitored and addressed to prevent potential increased morbidity and mortality. Risk factors such as pandemic-related caregiver job loss, stress, and financial insecurity should be examined so that children who may be particularly high risk can be identified. These known risk factors need to be considered alongside the potential unknown effects of stay-at-home orders to elucidate the primary drivers of physical child abuse during a pandemic, which may inform policy and public health recommendations in the future.
Our study has limitations. Utilization of the PHIS database means all hospitals in our study were large, tertiary children's hospitals which underrepresents areas where physical child abuse may present to smaller community hospitals. In addition, referrals from non-PHIS hospitals to PHIS hospitals may have been altered because of COVID. Prevalence of COVID-19 and corresponding political and economic downstream effects have fluctuated widely based on geographic location and timing which may influence our findings, and we chose to focus on the first four months of the pandemic when it was at its peak and responses were more homogenous. Utilization of ICD-10-CM codes means cases were defined by clinical diagnosis but may not have been confirmed by law enforcement or child protective services, which may bias results. Given the coinciding transition to virtual schooling, less severe cases may be underreported as educators are frequent reporters of abuse as well.
In conclusion, this study demonstrated that rates of traumatic injuries due to physical child abuse presenting to tertiary children's hospitals in the U.S. significantly declined during the COVID-19 pandemic, but those cases that did present were more likely to be severe, consistent with the overall trend of decreased healthcare utilization. Implications of these data cannot be underestimated. If more minor cases of child abuse are not presenting to care due to the pandemic, an early opportunity to intervene and interrupt escalating cycles of abuse is lost, which could result in increased mortality and morbidity for this population.
Author contributions and disclosures
All listed authors were involved with study design/conception, data analysis and interpretation, manuscript drafting, and final approval. This work is original, has not been simultaneously submitted to another journal, and all authors have given permission for the manuscript to be submitted. The authors have no conflicts of interest to disclose and no funding was secured for this study.
Footnotes
Level of Evidence: III (retrospective comparative study)
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jpedsurg.2021.06.014.
Appendix. Supplementary materials
References
- 1.Deans K.J., Thackeray J., Askegard-Giesmann J.R., et al. Mortality increases with recurrent episodes of non-accidental trauma in children. J Trauma Acute Care Surg. 2013;75(1):161–165. doi: 10.1097/ta.0b013e3182984831. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health and Human Services. Child Maltreat. 2018 https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment 2020.[Accessed 10.20.2020] [Google Scholar]
- 3.Estroff J.M., Foglia R.P., Fuchs J.R. A comparison of accidental and non-accidental trauma: it is worse than you think. J Emerg Med. 2015;48(3):274–279. doi: 10.1016/j.jemermed.2014.07.030. [DOI] [PubMed] [Google Scholar]
- 4.Kim P.T., Falcone R.A. Non-accidental trauma in pediatric surgery. Surg Clin. 2017;97(1):21–33. doi: 10.1016/j.suc.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Mulpuri K., Slobogean B.L., Tredwell S.J. The epidemiology of non-accidental trauma in children. Clin Orthop Relat Res. 2011;469(3):759–767. doi: 10.1007/s11999-010-1565-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paul A.R., Adamo M.A. Non-accidental trauma in pediatric patients: a review of epidemiology, pathophysiology, diagnosis and treatment. Transl Pediatr. 2014;3(3):195–207. doi: 10.3978/j.issn.2224-4336.2014.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miragoli S., Balzarotti S., Camisasca E., et al. Parents' perception of child behavior, parenting stress, and child abuse potential: individual and partner influences. Child Abuse Negl. 2018;84:146–156. doi: 10.1016/j.chiabu.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 8.Altemeier W.A., O'Connor S., Vietze P.M., et al. Antecedents of child abuse. J Pediatr. 1982;100(5):823–829. doi: 10.1016/s0022-3476(82)80604-5. [DOI] [PubMed] [Google Scholar]
- 9.Huang M.I., O'Riordan M.A., Fitzenrider E., et al. Increased incidence of non-accidental head trauma in infants associated with the economic recession. J Neurosurg Pediatr. 2011;8(2):171–176. doi: 10.3171/2011.5.PEDS1139. [DOI] [PubMed] [Google Scholar]
- 10.Moreland A., Herlihy C., Tynan M.A., et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement—United States, March 1–May 31. 2020. Morbid Mortal Wkly Rep. 2020;69(35):1198. doi: 10.15585/mmwr.mm6935a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Bureau of Labor Statistics. Economic new release: employment status of the civilian population by sex and age, https://www.bls.gov/news.release/empsit.t01.htm; 2020. [Accessed 10.20.2020].
- 12.Lawson M., Piel M.H., Simon M. Child maltreatment during the covid-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 2020 doi: 10.1016/j.chiabu.2020.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taub A. A new Covid-19 crisis: domestic abuse rises worldwide. The New York Times. 2020;6 [Google Scholar]
- 14.Thomas E.Y., Anurudran A., Robb K., et al. Spotlight on child abuse and neglect response in the time of COVID-19. The Lancet Public Health. 2020;5(7):e371. doi: 10.1016/S2468-2667(20)30143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuehn B.M. Surge in child Abuse, harm during COVID-19 pandemic reported. JAMAJAMA. 2020;324(7):621. doi: 10.1001/jama.2020.14433. [DOI] [PubMed] [Google Scholar]
- 16.Chaiyachati B.H., Agawu A., Zorc J.J., et al. Trends in pediatric emergency department utilization after Institution of Coronavirus Disease-19 mandatory social distancing. J Pediatr. 2020;226:274–277. doi: 10.1016/j.jpeds.2020.07.048. .e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Children's Hospital Association. Physical child abuse codes, https://www.childrenshospitals.org/Research-and-Data/Pediatric-Data-and-Trends/2019/Physical-Child-Abuse-Codes; 2019 [accessed 10.20.2020].
- 18.Hooft A., Ronda J., Schaeffer P., et al. Identification of physical abuse cases in hospitalized children: accuracy of International Classification of Diseases codes. J. Pediatr. 2013;162(1):80–85. doi: 10.1016/j.jpeds.2012.06.037. [DOI] [PubMed] [Google Scholar]
- 19.Moroni F., Gramegna M., Ajello S., et al. Collateral damage: medical care avoidance behavior among patients with acute coronary syndrome during the COVID-19 pandemic. JACC: Case Rep. 2020 doi: 10.1016/j.jaccas.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Czeisler M.É., Marynak K., Clarke K.E., et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. Morbid Mortal Wkly Rep. 2020;69(36):1250. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deans K.J., Thackeray J., Groner J.I., et al. Risk factors for recurrent injuries in victims of suspected non-accidental trauma: a retrospective cohort study. BMC Pediatr. 2014;14(1):217. doi: 10.1186/1471-2431-14-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nunez Lopez O., Hughes B.D., Adhikari D., et al. Sociodemographic determinants of non-accidental traumatic injuries in children. Am J Surg. 2018;215(6):1037–1041. doi: 10.1016/j.amjsurg.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Jones R.E., Babb J., Gee K.M., et al. An investigation of social determinants of health and outcomes in pediatric nonaccidental trauma. Pediatr Surg Int. 2019;35(8):869–877. doi: 10.1007/s00383-019-04491-4. [DOI] [PubMed] [Google Scholar]
- 24.Rosenfeld E.H., Johnson B., Wesson D.E., et al. Understanding non-accidental trauma in the United States: a national trauma databank study. J Pediatr Surg. 2020;55(4):693–697. doi: 10.1016/j.jpedsurg.2019.03.024. [DOI] [PubMed] [Google Scholar]
- 25.Lane W.G., Rubin D.M., Monteith R., et al. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMAJAMA. 2002;288(13):1603–1609. doi: 10.1001/jama.288.13.1603. [DOI] [PubMed] [Google Scholar]
- 26.Drake B., Jolley J.M., Lanier P., et al. Racial bias in child protection? A comparison of competing explanations using national data. PediatricsPediatrics. 2011;127(3):471–478. doi: 10.1542/peds.2010-1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laskey A.L., Stump T.E., Perkins S.M., et al. Influence of race and socioeconomic status on the diagnosis of child abuse: a randomized study. J Pediatr. 2012;160(6):1003–1008. doi: 10.1016/j.jpeds.2011.11.042. .e1. [DOI] [PubMed] [Google Scholar]
- 28.Price-Haywood E.G., Burton J., Fort D., et al. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim L., Whitaker M., O'Halloran A., et al. Hospitalization rates and characteristics of children aged< 18 years hospitalized with laboratory-confirmed COVID-19—COVID-NET, 14 States, March 1–July 25, 2020. Morbid Mortal Wkly Rep. 2020;69(32):1081. doi: 10.15585/mmwr.mm6932e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leventhal J.M., Gaither J.R. Incidence of serious injuries due to physical abuse in the United States: 1997 to 2009. Pediatrics. 2012;130(5):e847–e852. doi: 10.1542/peds.2012-0922. Nov 1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.