Abstract
目的
探讨子宫内膜非典型增生(complex atypical hyperplasia, CAH)及子宫内膜癌(endometrial cancer, EC)患者保留生育功能治疗的效果及妊娠结局。
方法
回顾性分析2009年1月至2021年9月北京大学人民医院进行保留生育功能治疗的EC患者及CAH患者共191例, 对患者的肿瘤缓解、复发及妊娠情况进行分析。
结果
(1) 疗效及相关因素: 总体完全缓解(complete response, CR)率为86.1%(161/187例), CAH组的CR率显著高于EC组(92.7% vs. 79.1%, P=0.007), Logistic回归分析显示, CAH组的CR率更高(OR=2.786, P=0.035);(2)复发率: 总体复发率为19.3%(31/161例), EC组显著高于CAH组(26.4% vs. 13.5%, P=0.039), 中位复发时间为22.5(9.0, 50.0)个月; (3)复发相关因素: 病理类型为EC(χ2=4.880, P=0.027)、未使用二甲双胍(χ2=7.075, P=0.008)、治疗达CR的时间>7个月(χ2=6.204, P=0.013)及未妊娠(χ2=6.765, P=0.009)患者的累积复发率显著更高; (4)妊娠结局及相关因素: 达到CR的患者中共有108例有生育意愿, 妊娠率为41.7%(45/108例), 生育率为34.3%(37/108), EC组的生育率显著低于CAH组(28.6% vs. 42.4%, P=0.045), 中位妊娠时间为10.50(5.75, 33.25)个月。既往有妊娠史(OR=9.468, P < 0.001)和接受辅助生殖治疗(OR=7.809, P < 0.001)患者的妊娠率更高。
结论
EC及CAH患者进行保留生育功能治疗的疗效肯定, 可以获得较高的疾病缓解率和一定的妊娠分娩率, 但仍存在复发率高及生育率低的问题。
Keywords: 子宫内膜非典型增生, 子宫内膜癌, 保留生育功能, 复发, 妊娠
Abstract
Objective
To analyze the efficacy and prognosis of fertility-sparing therapy of the patient with complex atypical hyperplasia (CAH) and endometrial cancer (EC).
Methods
Clinical data of 191 EC and CAH patients who received fertility-sparing therapy in Peking University People's Hospital between January 2009 and September 2021 were recruited retrospectively. Outcomes of remission, recurrence and pregnancy were analyzed.
Results
(1) Efficacy and efficacy-related factors: The complete response (CR) rate was 86.1% (161/187) for all the patients, and the CR rate of the CAH patients were higher than that of the EC patients (92.7% vs. 79.1%, P=0.007), the CR rate was significant higher in the CAH patients (OR=2.786, P=0.035). (2) The recurrence rate was 19.3% (31/161), and the recurrence rate of the EC patients were much higher than that of the CAH patients (26.4% vs. 13.5%, P=0.039). The median recurrence time was 22.5 (9.0, 50.0) months. (3) The high risk factors of recurrence were pathological type of EC (χ2=4.880, P=0.027), without the use of metfor-min (χ2=7.075, P=0.008), longer time to complete remission (>7 months) (χ2=6.204, P=0.013), and no pregnancy (χ2=6.765, P=0.009). (4) Results of pregnancy and related factors: Among the patients who achieved CR, 108 patients had fertility willing with the pregnancy rate of 41.7% (45/108), and the live birth rate was 34.3% (37/108). The live birth rate was lower in EC than that in the CAH patients (28.6% vs. 42.4%, P=0.045). The median time to achieve pregnancy was 10.50 (5.75, 33.25) months. The pregnancy rate was significant higher in the patients with pregnancy history (OR=9.468, P < 0.001) and in those who received assisted reproductive therapy (OR=7.809, P < 0.001).
Conclusion
Fertility-sparing therapy of CAH and EC patients is effective resulting in high disease remission and certain pregnancy. However, the high recurrence rate and low pregnancy rate are still key problems for EC and CAH patients, therefore close monitoring and follow-up are indicated.
Keywords: Complex atypical hyperplasia, Endometrial carcinoma, Fertility preservation, Recurrence, Pregnancy
随着肥胖、多囊卵巢综合征(polycystic ovarian syndrome,PCOS)等的患病率在育龄期女性中日益增多,子宫内膜癌(endometrial cancer,EC)的患病率也有所增加[1]。女性在绝经前被诊断为EC者约占25%[2]。EC在育龄期女性中肿瘤分化程度较高,期别较早,预后更好[3]。对于高分化EC、病理未浸润子宫肌层的低风险患者,可考虑采取保留生育功能治疗[4]。本研究对子宫内膜非典型增生(complex atypical hyperplasia,CAH)及早期EC患者行保留生育功能治疗,并对其疗效及妊娠情况进行分析,以期指导今后的临床诊治。
1. 资料与方法
1.1. 研究对象
回顾性分析2009年1月至2021年9月北京大学人民医院收治的EC患者及CAH患者共191例,研究对象均符合《早期子宫内膜癌保留生育功能治疗专家共识》中的纳入标准[2]。
1.2. 治疗方案
患者采用以下保留生育功能的治疗方案:(1)口服醋酸甲羟孕酮(medroxy progesterone acetate,MPA)者115例,剂量为250~500 mg/d;(2)口服醋酸甲地孕酮(megestrol acetate,MA)者9例,剂量为160~320 mg/d;(3)使用MPA/MA+促性腺激素释放激素激动剂(gonadotrophin releasing hormone agonist,GnRHa)者37例;(4)使用GnRHa+左炔诺孕酮宫内释放系统(levonorgestrel-releasing intrauterine system,LNG-IUS)者16例;(5)使用MPA/MA联合LNG-IUS方案者2例;(6)单用GnRHa方案者9例;(7)单用LNG-IUS方案者3例。
联合用药、单用GnRHa或LNG-IUS方案的患者大部分伴有肥胖、糖尿病或PCOS等合并症。治疗每3个月行子宫内膜组织病理学检查评估治疗反应,完全缓解后建议维持治疗,方案为使用LNG-IUS或月经后半周期口服黄体酮。有生育意愿的患者评估生殖功能,必要时行辅助生殖技术助孕。末次随访时间截止到2022年1月15日。
1.3. 疗效评价指标
参照《早期子宫内膜癌保留生育功能治疗专家共识》[2],疗效评价分为:完全缓解、部分缓解、疾病无反应、疾病进展、疾病复发。
1.4. 数据分析
使用SPSS 26.0软件完成数据分析,计量资料结果呈正态分布者以均值±标准差表示,非正态分布者以中位数(四分位数间距)表示,计数资料采用卡方检验。采用Logistic回归及Kaplan-Meier分析对疗效及预后相关因素进行分析,双侧检验P < 0.05为差异有统计学意义。
2. 结果
2.1. 一般情况
191例患者的年龄为(33.0±5.7)岁,体重指数(body mass index, BMI)为(27.5±5.1) kg/m2,EC和CAH组患者的一般资料差异无统计学意义(表 1)。
表 1.
191例EC及CAH患者的一般情况
General condition of 191 EC and CAH patients
| Items | Total (n=191) | EC (n=92) | CAH (n=99) | P value |
| Data are presented as x ± s or n (%). EC, endometrial cancer; CAH, complex atypical hyperplasia; BMI, body mass index; PCOS, polycystic ovarian syndrome. | ||||
| Age/years | 33.0±5.7 | 32.5±5.4 | 33.4±5.9 | 0.244 |
| Number of times of pregnancy | ||||
| 0 | 121 (63.4) | 59 (64.1) | 62 (62.6) | 0.829 |
| ≥1 | 70 (36.6) | 33 (35.9) | 37 (37.4) | |
| Number of times of delivery | ||||
| 0 | 157 (82.2) | 78 (84.8) | 79 (79.8) | 0.368 |
| ≥1 | 34 (17.8) | 14 (15.2) | 20 (20.2) | |
| BMI/(kg/m 2) | 27.5±5.1 | 27.5±5.2 | 27.6±5.1 | 0.973 |
| Complications | ||||
| Type Ⅱ diabetes | 22 (11.5) | 12 (13.0) | 10 (10.1) | 0.524 |
| PCOS | 23 (12.0) | 11 (12.0) | 12 (12.1) | 0.972 |
| Thyroid disease | 11 (5.8) | 6 (0.7) | 5 (0.5) | 0.663 |
2.2. 治疗结果和疗效相关因素
排除1例失访及3例随访时治疗未满3个月的患者,总体CR率为86.1%(161/187例)。EC及CAH组的CR率分别为79.1%(72/91例)和92.7%(89/96例),组间差异有统计学意义(P=0.007)。治疗达CR的中位时间为7个月,EC组和CAH组分别为8个月和6个月(P=0.053)。
MPA/MA+GnRHa方案治疗的CR率为89.2%,GnRHa+LNG-IUS方案的CR率为43.8%,MPA/MA联合LNG-IUS方案的CR率为2/2,单用GnRHa方案的CR率为7/9,单用LNG-IUS方案的CR率为3/3。
对疗效相关因素进行Logistic回归分析显示(表 2),多因素分析显示病理类型是缓解的相关因素,CAH组的CR率是EC组的2.786倍,差异有统计学意义(OR=2.786, P=0.035)。Kaplan-Meier法分析显示,EC组的累积CR率低于CAH组,差异有统计学意义(χ2=4.043,P=0.044,图 1)。
表 2.
187例保留生育功能治疗患者疗效相关因素的Logistic回归分析
Logistic regression analysis of efficacy-related factors in 187 patients undergoing fertility-sparing therapy
| Items | One factor analysis | Multiple factors analysis | ||||
| OR (95% CI) | P value | OR (95% CI) | P value | |||
| EC, endometrial cancer; CAH, complex atypical hyperplasia; BMI, body mass index; PCOS, polycystic ovarian syndrome; MPA, medroxy progesterone acetate; MA, megestrol acetate. | ||||||
| Age/years | ≥30 | 1.833 (0.653-5.147) | 0.25 | 2.256 (0.717-7.100) | 0.164 | |
| < 30 | 1 | 1 | ||||
| BMI/(kg/m2) | ≥25 | 1.774 (0.664-4.738) | 0.253 | 1.729 (0.631-4.733) | 0.287 | |
| < 25 | 1 | 1 | ||||
| Pathology | CAH | 3.355 (1.336-8.424) | 0.01 | 2.786 (1.073-7.235) | 0.035 | |
| EC | 1 | 1 | ||||
| Complication with PCOS | Yes | 0.588 (0.129-2.677) | 0.492 | |||
| No | 1 | |||||
| Complication with diabetes | Yes | 1.036 (0.283-3.799) | 0.957 | |||
| No | 1 | |||||
| Types of progesterone | MPA | 0.916 (0.194-4.330) | 0.912 | |||
| MA | 1 | |||||
| Using metformin | Yes | 1.361 (0.582-3.180) | 0.477 | |||
| No | 1 | |||||
图 1.
保留生育功能治疗不同病理类型的Kaplan-Meier累积完全缓解率曲线
Kaplan-Meier cumulative complete response rate curve of fertility-sparing therapy for different pathological types
EC, endometrial cancer; CAH, complex atypical hyperplasia.
2.3. 复发情况和复发相关因素
达到CR的161例患者随访29(16,64)个月后,复发率为19.3%(31/161例),EC组的复发率显著高于CAH组(26.4% vs. 13.5%, P=0.039),使用二甲双胍组的复发率低于未使用二甲双胍组(13.5% vs. 24.1%, P=0.088)。中位复发时间为22.5(9.0,50.0)个月,EC组和CAH组分别为21个月和24个月(P=0.533)。
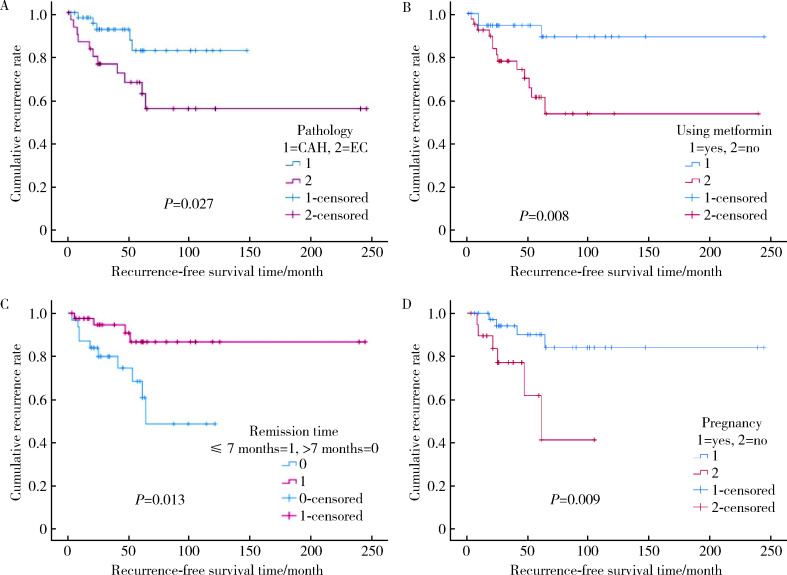
复发相关因素的Logistic回归分析结果见表 3,单因素分析显示,病理类型是复发的独立危险因素,EC组的复发风险是CAH组的2.300倍。进一步对复发相关因素采用Kaplan-Meier分析显示,病理类型为EC(χ2=4.880,P=0.027,图 2A)、未使用二甲双胍(χ2=7.075,P=0.008,图 2B)、治疗达C R的时间>7个月(χ2=6.204,P=0.013,图 2C)及未妊娠(χ2=6.765,P=0.009,图 2D)患者的累积复发率明显更高。
表 3.
保留生育功能治疗患者复发相关因素的Logistic回归分析
Logistic regression analysis of recurrence-related factors in patients with fertility-sparing therapy
| Items | One factor analysis | Multiple factors analysis | ||||
| OR (95% CI) | P value | OR (95% CI) | P value | |||
| EC, endometrial cancer; CAH, complex atypical hyperplasia; BMI, body mass index; PCOS, polycystic ovarian syndrome; MPA, medroxy progesterone acetate; MA, megestrol acetate; GnRHa, gonadotrophin releasing hormone agonist. | ||||||
| Age/years | ≥30 | 0.844 (0.361-1.973) | 0.696 | |||
| < 30 | 1 | |||||
| BMI/(kg/m2) | ≥25 | 0.960 (0.416-2.218) | 0.924 | |||
| < 25 | 1 | |||||
| Pathology | CAH | 2.300 (1.031-5.134) | 0.042 | 1.779 (0.729-4.343) | 0.206 | |
| EC | 1 | 1 | ||||
| Complication with PCOS | Yes | 0.712 (0.195-2.601) | 0.608 | |||
| No | 1 | |||||
| Complication with diabetes | Yes | 0.821 (0.222-3.034) | 0.768 | |||
| No | 1 | |||||
| Complication with thyroid disease | Yes | 0.689 (0.080-5.939) | 0.735 | |||
| No | 1 | |||||
| Types of progesterone | MPA | 2.800 (0.845-9.283) | 0.092 | 2.288 (0.653-8.014) | 0.196 | |
| MA | 1 | 1 | ||||
| Using metformin | Yes | 2.036 (0.890-4.660) | 0.092 | 1.662 (0.691-3.994) | 0.256 | |
| No | 1 | 1 | ||||
| Using GnRHa | Yes | 1.960 (0.870-4.415) | 0.104 | 1.667 (0.675-4.117) | 0.268 | |
| No | 1 | 1 | ||||
| Maintenance treatment | Yes | 0.734 (0.297-1.812) | 0.502 | |||
| No | 1 | |||||
| Pregnancy | Yes | 1.024 (0.358-2.933) | 0.964 | |||
| No | 1 | |||||
| Delivery | Yes | 2.13 (0.333-13.666) | 0.424 | |||
| No | 1 | |||||
图 2.
EC和CAH患者的累积复发率Kaplan-Meier曲线图
Kaplan-Meier curve of cumulative recurrence rate for EC and CAH patients
A, pathology; B, combination with metformin; C, with treatment time to complete response more than 7 months or not; D, with or without pregnancy. EC, endometrial cancer; CAH, complex atypical hyperplasia.
2.4. 妊娠情况和妊娠相关因素
达到CR的患者中108例有生育意愿(表 4)。妊娠率为41.7%(45/108例),EC组和CAH组分别为38.8%和44.1%(P=0.579)。生育率为34.3%(37/108例),EC组的生育率显著低于CAH组(28.6% vs. 42.4%,P=0.045)。中位妊娠时间为10.50(5.75,33.25)个月,EC组和CAH组分别为13个月和9个月(P=0.196)。妊娠期合并症包括:9例妊娠期糖尿病及糖尿病合并妊娠,5例妊娠期高血压,3例甲状腺功能减退,3例产后出血。
表 4.
保留生育功能治疗达到完全缓解后有生育意愿的108例患者妊娠情况
Pregnancy status of 108 patients with fertility intention after achieving complete remission with the conservative treatment
| Items | Total | CAH (n=89) | EC (n=72) | P value |
| EC, endometrial cancer; CAH, complex atypical hyperplasia. | ||||
| Patients with fertility intention | 108 | 59 | 49 | |
| Patients with assisted human reproduction | 34 | 19 | 15 | |
| Patients with pregnancy (pregnancy times) | 45 (50) | 26 (29) | 19 (21) | |
| Patients with delivery (delivery times) | 39 (37) | 27 (25) | 12 (12) | |
| Pregnancy rate/% | 41.7 | 44.1 | 38.8 | 0.579 |
| Fertility rate/% | 34.3 | 42.4 | 28.6 | 0.045 |
| Pregnancy duration/months, M (P25, P75) | 10.50 (5.75, 33.25) | 9.00 (2.50, 29.50) | 13.00 (7.00, 46.50) | 0.196 |
妊娠相关因素的Logistic回归分析结果见表 5。单因素及多因素分析显示,既往有妊娠史和辅助生殖技术助孕是妊娠成功的相关因素,有妊娠史患者的妊娠率是无妊娠史的9.468倍,辅助生殖技术治疗组患者的妊娠率是未行辅助生殖治疗组的7.809倍。
表 5.
108例有生育意愿的患者妊娠相关因素的Logistic回归分析
Logistic regression analysis of pregnancy-related factors of the 108 patients with fertility intention
| Items | One factor analysis | Multiple factors analysis | ||||
| OR (95% CI) | P value | OR (95% CI) | P value | |||
| EC, endometrial cancer; CAH, complex atypical hyperplasia; BMI, body mass index; PCOS, polycystic ovarian syndrome; GnRHa, gonadotrophin releasing hormone agonist. | ||||||
| Age/years | ≥30 | 0.773 (0.338-1.772) | 0.543 | |||
| < 30 | 1 | |||||
| Pregnancy history | Yes | 10.711 (4.206-27.271) | < 0.001 | 9.468 (2.928-30.618) | < 0.001 | |
| No | 1 | 1 | ||||
| BMI/(kg/m2) | ≥25 | 0.731 (0.324-1.647) | 0.45 | |||
| < 25 | 1 | |||||
| Complication with PCOS | Yes | 2.508 (0.762-8.253) | 0.13 | 2.209 (0.374-13.046) | 0.382 | |
| No | 1 | 1 | ||||
| Complication with diabetes | Yes | 0.247 (0.051-1.186) | 0.081 | 0.627 (0.061-6.432) | 0.695 | |
| No | 1 | 1 | ||||
| Complication with thyroid disease | Yes | 0.999 | ||||
| No | ||||||
| Pathology | CAH | 0.804 (0.372-1.738) | 0.579 | |||
| EC | 1 | |||||
| Using metformin | Yes | 0.822 (0.379-1.785) | 0.621 | |||
| No | 1 | |||||
| Using GnRHa | Yes | 1.099 (0.469-2.576) | 0.828 | |||
| No | 1 | |||||
| Assisted human reproduction | Yes | 12.768 (4.763-34.244) | < 0.001 | 7.809 (2.600-23.457) | < 0.001 | |
| No | 1 | |||||
| Recurrence | Yes | 1.024 (0.358-2.933) | 0.964 | |||
| No | 1 | |||||
3. 讨论
3.1. EC保留生育功能治疗的疗效及相关因素
本研究中,EC和CAH患者保留生育功能治疗的CR率为86.1%,以往多项研究报道口服孕激素保留生育功能治疗的CR率为62.9%~81.1%[5-9]。本研究中CAH组的CR率显著高于EC组,Gunderson等[10]的研究也显示,CAH患者的CR率(65.8%)显著高于EC患者(48.2%,P=0.002)。本组患者达到CR的中位时间为7个月,既往研究报道达到CR的中位时间为4~9个月[5-7]。本研究结果显示,CR率与患者年龄、BMI、是否合并PCOS、糖尿病、口服孕激素种类及是否使用二甲双胍均无关。本组EC和CAH患者的CR率稍高于以往的研究报道,提示保留生育功能治疗的疗效肯定,EC患者疗效较CAH患者差,治疗达CR所需的时间更长,考虑与病变严重程度相关。
3.2. 复发及复发相关因素
本研究患者的复发率为19.3%,中位复发时间为22.5个月。既往研究报道CAH患者的复发率为2.9%~28.1%[11-13],EC患者的复发率为4.1%~81.8%[5, 7-9, 11-14]。本研究中,CAH组的复发率显著低于EC组。Ohyagi-Hara等[9]的研究中EC患者的复发率显著高于CAH组(81.8% vs. 0, P < 0.001)。另外,本研究发现使用二甲双胍患者的累积复发率低于未使用二甲双胍的患者,与Mitsuhashi等[15]的研究结果一致,使用MPA联合二甲双胍治疗组的复发情况明显优于单用MPA治疗组(OR=0.38,95%CI:0.16~0.92,P=0.032),两组患者的3年无复发生存率分别为79.3%和45.2%。治疗达CR的时间较长(>7个月)也是复发的危险因素,Chen等[6]的研究显示,达到CR所需时间≤6个月的患者复发率显著低于>6个月的患者,两组的复发率分别为4%(1/24例)和60%(9/15例,P < 0.001)。本研究中,妊娠患者的累积复发率低于非妊娠患者,以往研究也显示成功妊娠可作为一种保护性因素,可预防患者复发,妊娠组和非妊娠组患者的复发率差异有统计学意义(RR=0.382,P=0.025)[16]。
保留生育功能治疗达CR后仍存在复发情况,复发多发生在CR后的2年内。达到CR所需时间较长的患者考虑存在一些肿瘤高危因素,对于此类患者及病理为EC的患者应加强随访,及时发现病变复发。二甲双胍降低保留生育功能治疗后的复发率,推测与改善患者的胰岛素抵抗,去除EC的危险因素有关,因此可考虑用于合并代谢综合征的患者。孕期高水平的孕激素及产后哺乳均对子宫内膜起到保护作用,因此建议有生育意愿的患者达到CR后应尽早妊娠,可考虑采取辅助生殖技术助孕,以降低复发风险。
3.3. 妊娠及妊娠相关因素
本组患者的妊娠率为41. 7%,中位妊娠时间为10.50(5.75,33.25)个月,与既往报道的妊娠率18.8%~83.3%相符[5-7, 9, 17-20]。本组患者的生育率为34.3%,CAH组的生育率高于EC组。既往有妊娠史患者组的妊娠率是无妊娠史组的9.468倍,接受辅助生殖技术治疗患者组的妊娠率是未行辅助生殖技术治疗组的7.809倍。Gallos等[21]的研究显示,辅助生殖受孕和自然受孕患者的生育率分别为39.4%(56/142例)和14.9%(46/309例),两者差异有统计学意义(P=0.001)。因此,保留生育功能治疗可获得一定的妊娠结局,对于存在不孕史、排卵功能障碍、卵巢功能低下、肥胖等不孕因素的患者,应积极给予辅助生殖助孕,提高妊娠率。
综上所述,本研究对EC和CAH患者的保留生育功能治疗有临床指导意义,保留生育功能治疗的疗效肯定,有较高的疾病缓解率,但仍存在疾病复发情况,使用二甲双胍、尽快妊娠是预后保护因素;对于EC患者及缓解所需时间较长的患者应加强随访监测,采取维持治疗预防复发以及复发后及时处理。保留生育功能治疗能获得一定的成功妊娠结局,既往有妊娠史是妊娠的有利因素,对于存在不孕因素的患者应积极给予辅助生殖助孕以提高妊娠率。本研究为回顾性研究,今后仍需进一步开展前瞻性研究,并对改善预后和妊娠结局进行深入探讨。
Biography
王建六,妇产科教授,博士生导师,北京大学人民医院副院长、党委委员,北京大学妇产科学系主任,北京大学人民医院妇产科教研室主任,北京市女性盆底疾病防治重点实验室主任。担任中华医学会妇产科学分会常务委员,中华医学会妇科肿瘤分会常务委员,中国研究型医院学会妇产科学专业委员会主任委员,北京医学会妇产科学分会主任委员,北京市医师协会妇产科专科医师分会会长,Gynecology and Obstetrics Clinical Medicine (GOCM), Journal of Gynecological Surgery, Journal of Gynecological Oncology等杂志主编及编委,《中华妇产科杂志》编委,《现代妇产进展》副主编,《中国妇产科临床杂志》副主编。 主要研究领域:妇科肿瘤和盆底疾病。在妇科肿瘤方面,对常见妇科恶性肿瘤宫颈癌、卵巢癌和子宫内膜癌进行了系列研究,特别是子宫内膜癌的发病机制和分子分型研究,研究成果发表在Advanced Science及Science(suppl)等国内外学术期刊,主编科技部重点图书《子宫内膜癌》;在盆底疾病方面,建立了盆底功能障碍性疾病多学科联合诊疗模式,推广盆底功能障碍性疾病的诊疗规范,探索新型补片在盆腔器官脱垂手术中的应用,牵头编写国内外首部专著《盆底医学》,促进了我国盆底疾病诊疗的发展。 承担科技部“十三五”规划项目、国家自然科学基金、卫生部优秀人才基金等科研项目。曾获霍英东基金会教师奖、吴阶平-杨森医学药学奖(2013),荣获卫生部优秀科研人才、科学中国人(2016)、国家名医(2018)等称号
Funding Statement
国家重点研发计划(2019YFC1005200、2019YFC1005204)
Supported by the National Key Technology Research and Development Program of China (2019YFC1005200, 2019YFC1005204)
References
- 1.Corzo C, Barrientos SN, Westin SN, et al. updates on conservative management of endometrial cancer. J Minim Invasive Gynecol. 2018;25(2):308–313. doi: 10.1016/j.jmig.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 2.中国研究型医院学会妇产科专业委员会 早期子宫内膜癌保留生育功能治疗专家共识. 中国妇产科临床杂志. 2019;20(4):369–373. doi: 10.13390/j.issn.1672-1861.2019.04.025. [DOI] [Google Scholar]
- 3.Silverberg SG, Makowski EL, Roche WD. Endometrial carcinoma in women under 40 years of age: Comparison of cases in oral contraceptive users and non-users. Cancer. 1977;39(2):592–598. doi: 10.1002/1097-0142(197702)39:2<592::AID-CNCR2820390233>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 4.Gynecologic Oncology Branch of the Chinese Medical Association Guidelines for fertility-preserving treatment of gynecological malignant tumors (Chinese) Chin J Obstet Gynecol. 2014;4:243–248. [Google Scholar]
- 5.Park JY, Kim DY, Kim JH, et al. Long-term oncologic outcomes after fertility-sparing management using oral progestin for young women with endometrial cancer (KGOG 2002) Eur J Cancer. 2013;49(4):868–874. doi: 10.1016/j.ejca.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 6.Chen M, Jin Y, Li Y, et al. Oncologic and reproductive outcomes after fertility-sparing management with oral progestin for women with complex endometrial hyperplasia and endometrial cancer. Int J Gynaecol Obstet. 2016;132(1):34–38. doi: 10.1016/j.ijgo.2015.06.046. [DOI] [PubMed] [Google Scholar]
- 7.Hahn HS, Yoon SG, Hong JS, et al. Conservative treatment with progestin and pregnancy outcomes in endometrial cancer. Int J Gynecol Cancer. 2009;19(6):1068–1073. doi: 10.1111/IGC.0b013e3181aae1fb. [DOI] [PubMed] [Google Scholar]
- 8.Wang CJ, Chao A, Yang LY, et al. Fertility-preserving treatment in young women with endometrial adenocarcinoma: A long-term cohort study. Int J Gynecol Cancer. 2014;24(4):718–728. doi: 10.1097/IGC.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 9.Ohyagi-Hara C, Sawada K, Aki I, et al. Efficacies and pregnant outcomes of fertility-sparing treatment with medroxyprogesterone acetate for endometrioid adenocarcinoma and complex atypical hyperplasia: Our experience and a review of the literature. Arch Gynecol Obstet. 2015;291(1):151–157. doi: 10.1007/s00404-014-3417-z. [DOI] [PubMed] [Google Scholar]
- 10.Gunderson CC, Fader AN, Carson KA, et al. Oncologic and reproductive outcomes with progestin therapy in women with endometrial hyperplasia and grade 1 adenocarcinoma: a systematic review. Gynecologic Oncology. 2012;125(2):477–482. doi: 10.1016/j.ygyno.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Yang YF, Liao YY, Liu XL, et al. Prognostic factors of regression and relapse of complex atypical hyperplasia and well-differentiated endometrioid carcinoma with conservative treatment. J Gynecol Oncol. 2015;139(3):419–423. doi: 10.1016/j.ygyno.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 12.Zhou H, Cao D, Yang J, et al. Gonadotropin-releasing hormone agonist combined with a levonorgestrel-releasing intrauterine system or letrozole for fertility-preserving treatment of endometrial carcinoma and complex atypical hyperplasia in young women. Int J Gynecol Cancer. 2017;27(6):1178–1182. doi: 10.1097/IGC.0000000000001008. [DOI] [PubMed] [Google Scholar]
- 13.Pronin SM, Novikova OV, Andreeva JY, et al. Fertility-sparing treatment of early endometrial cancer and complex atypical hyperplasia in young women of childbearing potential. Int J Gynecol Cancer. 2015;25(6):1010–1014. doi: 10.1097/IGC.0000000000000467. [DOI] [PubMed] [Google Scholar]
- 14.Dursun P, Erkanli S, Güzel AB, et al. A Turkish Gynecologic Oncology Group study of fertility-sparing treatment for early-stage endometrial cancer. Int J Gynaecol Obstet. 2012;119(3):270–273. doi: 10.1016/j.ijgo.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 15.Mitsuhashi A, Habu Y, Kobayashi T, et al. Long-term outcomes of progestin plus metformin as a fertility-sparing treatment for atypical endometrial hyperplasia and endometrial cancer patients. J Gynecol Oncol. 2019;30(6):e90. doi: 10.3802/jgo.2019.30.e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.柳 晓肃, 郭 红燕, 宋 雪凌, et al. 早期高分化子宫内膜癌及子宫内膜不典型增生患者保留生育功能治疗的结局分析. 实用妇产科杂志. 2020;36(9):685–689. [Google Scholar]
- 17.Pashov AI, Tskhay VB, Ionouchene SV, et al. The combined GnRH-agonist and intrauterine levonorgestrel-releasing system treatment of complicated atypical hyperplasia and endometrial cancer: A pilot study. Gynecol Endocrinol. 2012;28(7):559–561. doi: 10.3109/09513590.2011.649813. [DOI] [PubMed] [Google Scholar]
- 18.Kim MK, Seong SJ, Kim YS, et al. Combined medroxyproges-terone acetate/levonorgestrel-intrauterine system treatment in young women with early-stage endometrial cancer. Am J Obstet Gynecol. 2013;209(4):358.e1–e4. doi: 10.1016/j.ajog.2013.06.031. [DOI] [PubMed] [Google Scholar]
- 19.Cade TJ, Quinn MA, Rome RM, et al. Progestogen treatment options for early endometrial cancer. BJOG. 2010;117(7):879–884. doi: 10.1111/j.1471-0528.2010.02552.x. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Z, Huang H, Feng F, et al. A pilot study of gonadotropin-releasing hormone agonist combined with aromatase inhibitor as fertility-sparing treatment in obese patients with endometrial cancer. J Gynecol Oncol. 2019;30(4):e61. doi: 10.3802/jgo.2019.30.e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gallos ID, Yap J, Rajkhowa M, et al. Regression, relapse, and live birth rates with fertility-sparing therapy for endometrial cancer and atypical complex endometrial hyperplasia: a systematic review and metaanalysis. Am J Obstet Gynecol. 2012;207(4):261–266. doi: 10.1016/j.ajog.2012.08.011. [DOI] [PubMed] [Google Scholar]