Abstract
Background
The treatment of proximal humerus fracture complicated by bone fragility is still controversial. The aim of this study is to compare the Neer classification and the Control Volume severity grade for the accuracy in the selection of the type of treatment and for prognostic evaluation.
Materials and methods
We retrospectively collected the records of all patients admitted at the Emergency Department of our Institute, from 2013 to 2020, for a closed displaced proximal humerus fracture further investigated with a CT scan before treatment decision. We selected all patients with a minimum age of 65 years. The included fractures were retrospectively classified according to Neer, and Control Volume severity grade. The included patients were evaluated with Simple Shoulder Test (SST). A statistical analysis was performed to correlate the type of treatment and the clinical results to the Neer classification and the Control Volume severity grade.
Results
Sixty-four patients (80%), were available for the telephonically interview at a mean follow up of 4 years and were included. According to the Control Volume model, we identified fracture with a low, medium and high severity grade, in 23 (36%), 13 (20%), and, 28 (44%) cases, respectively. Fifteen patients (23,5%) were conservatively treated, whether fourty-nine patients (76,5%) were operated. We find a statistical correlation between control volume severity grade and type of treatment. No Therapeutic correlation was detected for the Neer classification. A statistical correlation between the severity grade and clinical outcome could be observed only for patients with the same type of treatment.
Conclusions
The use of Control Volume severity grade is associated with better therapeutic and prognostic informations in confront to the Neer classification.
Keywords: Proximal humerus fractures, bone fragility, plate synthesis, reverse prosthesis
INTRODUCTION
Proximal humeral fractures frequency is increasing, particularly in women aged older than 65 years, due to the lengthening of the average life and to the increase in osteoporosis.1–4 The evidences that surgical treatment is superior to conservative treatments, even for displaced fractures, are not clear.5,6 The latest Cochrane review suggests that non-operative management might have similar functional outcomes to operative management with lower risks of complications and reoperation.7,8 Moreover, there is no agreement about which type of fracture should be surgically treated, which type of surgery should be performed and which rehabilitation programs should be suggested.9 This high variability about surgical indication and type of surgery is present even among regions of the same country, leading to substantial variation worldwide in the management of this common injury. Generally, conservative treatment of proximal humerus displaced fractures, lead to bone healing in more than 90% of patients (malunion), with restriction of active range of motion, but acceptable functional results in elderly people.10 Surgery is usually indicated in more active patients with higher functional requests. Surgical treatment is associated with an higher complication rate, in confront to conservative treatment, such as: nonanatomic reduction, humeral head screws perforation, secondary displacement of the fracture, avascular necrosis, infection, greater tuberosity resorption and secondary cuff deficiency, stiffness and reintervention.11 In the last ’90 and early 2000s, the market popularized modular dedicated humeral prosthesis and locking plates with polyaxial screws, anyway their use, accompanied by encouraging biomechanical studies in the laboratory, did not show a significant reduction in postoperative complication.12 Moreover, the Neer classification,13,14 which is the most used classification system, does not allow to define the type of treatment or to predict the clinical results.15 Recently, a new classification system based on Control Volume (CV) theory has been described.16,17 The CV theory and its classification system are the result of a mathematical approach to the three-dimensional pattern of the fracture, which evaluate the head displacement, the amount of bone loss and, the comminution of the medial and lateral humeral columns in the metaphysis. The CV theory helps to define a severity grade of the fracture which could help the surgeon to understand the best treatment option. The purpose of this article is to evaluate the therapeutic and prognostic predictive value of the CV severity grade in confront to the Neer classification.
MATERIALS AND METHODS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
We retrospectively collected the data of all patients affected by a closed displaced proximal humerus fracture, admitted in a single Hospital emergency department from 2013 to 2020. From this population, we selected all patient aged older than 65, which performed a CT scan before the treatment decision. Exclusion criteria were: open fracture, polytrauma, associated scapula, clavicular or humeral shaft fracture, previous shoulder surgery and pathological fractures. According to these criteria, eighty patients were included in the study. The radiological examinations were retrospectively analyzed by two orthopedic surgeons, blinded to the patient treatment or data, asking to classify the fracture according to the Neer and the CV criteria. The CV criteria were: the head displacement, the amount of bone loss and, the comminution of the medial and lateral humeral columns in the metaphysis and humeral head. The output evaluations of CV criteria defined three grades of fracture severity: low, medium and high. The therapeutic treatment of each patient was recorded. A telephonically interview with Simple Shoulder Test (SST) was used to evaluate the final clinical outcome.
Statistical Analysis
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) Version 20.0 (IBM, Armonk, NY, USA). The values were tested for normal distribution using the Kolmogorov–Smirnov test and the Shapiro–Wilk test. Univariate comparisons of dichotomous data were performed with the use of the chi-square or Fisher exact test, while the T-test was used to compare group means with SD. Multiple regression was also used to evaluate the effect of the test variables on the values of the dependent variables. A two-sided p-values were calculated. The level of significance was defined as p < 0.05.
RESULTS
We identified eighty patients eligible for the study, according to the inclusion and exclusion criteria. Sixty-four patients (80%) were available for a telephonic evaluation, whether sixteen patients (20%) were lost at the follow-up and were excluded from the study. Mean age was 74 years (66-85). There were 19 males and 45 females. Mean follow-up was 4 years (1 to 7). Fracture types were classified according to Neer as two-part fracture in 6 cases (9%), as three-part fracture in 25 cases (39%), as four-part fracture in 33 cases (51%). According to the CV criteria, the severity grade was evaluated as low in 23 cases (36%), medium in 13 cases (20%) and high in 28 patients (44%). Fifteen patients (23,5%) were treated conservatively, with immobilization for 4 weeks before to start physiotherapy; forty-nine (76,5%) surgically. Three patients (4,5%) were treated with closed reduction and percutaneous osteosynthesis with Kirschner wires. One (1,5%) patient was treated with open reduction and synthesis with a locking plate. Nine patients (14%) were treated with an endomedullary autologous iliac crest bone graft and locking plate. Eight patients (12,5%) were treated with a titanium endomedullary cage and locking plate.18 Twenty-eight cases (44%) were treated with reverse prosthesis. In the immediate postoperative period, we did not observe any vascular complications. One patient need postoperative intensive care. In three patients we observed a postoperative temporary axillary palsy. Mean inpatient time was 3,5 days (±2,5). SST values are reported in table 1. The statistical regression test demonstrated that the severity grade (p<0,05) correlates better than the Neer classification (p=0,35) to the type of treatment. Indeed, no patient with a low severity grade was treated with a reverse prosthesis and the 85% of the conservatively treated patients are in the group graded as low severity grade. On the contrary, reverse prosthesis and conservative treatment were used with a similar frequency in 2-, 3- and 4- part fractures. In particular, we observed several 2-part fractures with high (Fig. 1) and medium (Fig. 2) severity grade characterized by calcar fracture and lateral comminution. On the other side, better SST values were not statistically associated to a lower severity grade neither to the Neer classification. Only if we calculate the SST values for a specific group of treatment we could find a significative correlation between severity grade and clinical outcomes.
Table 1. Clinical outcomes according to the type of treatment measured with Simple Shoulder Test.
| Simple Shoulder Test score results | |||||
| Treatments | Frequencies | Min | Max | Mean | 95% CI |
| RSA | 28 | 33% | 100% | 76% | (0,69;1) |
| ORIF | 18 | 50% | 100% | 78% | (0,73;1) |
| CRPO | 3 | 67% | 100% | 85% | (0,79;1) |
| NO | 15 | 67% | 92% | 75% | (0,7;1) |
(RSA revers shoulder arthroplasty, ORIF open reduction internal fixation with plate and screws, CRPO closed reduction and percutaneous fixation, NO non operative treatment)
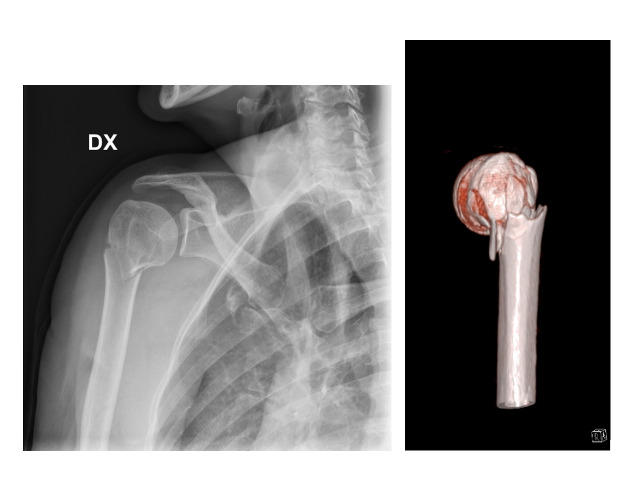
Figure 1.
- anteroposterior radiographs and B) 3D computed tomography showing a 2-part fracture with posterior calcar fracture and lateral comminution classified as high severity grade
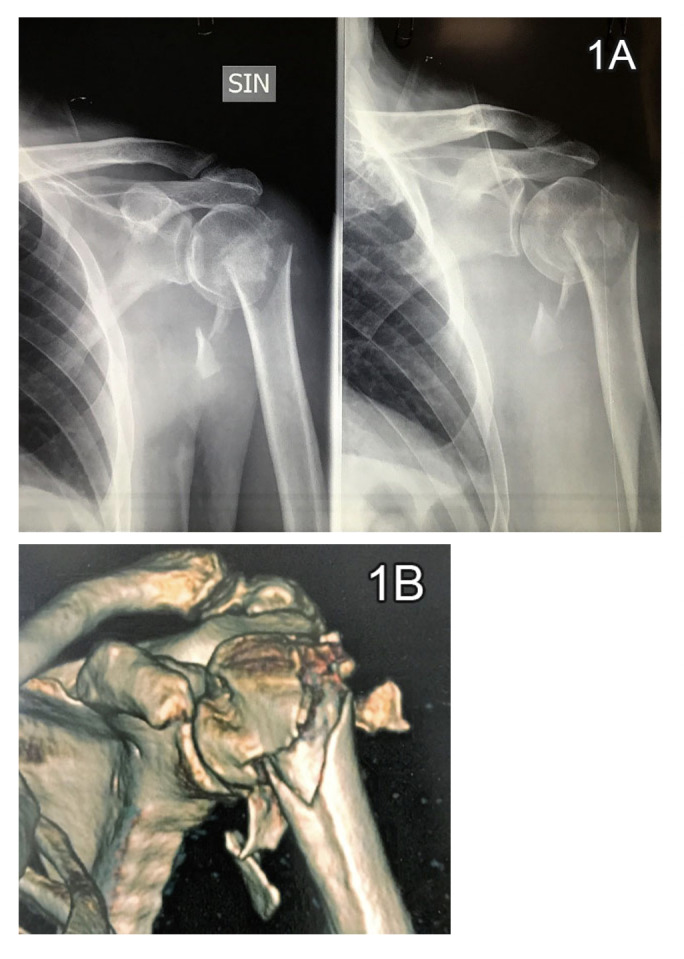
Figure 2.
- anteroposterior radiographs and B) 3D computed tomography showing a 2-part fracture with posterior calcar fracture and lateral comminution classified as moderate severity grade, requiring a surgical treatment with open reduction, internal fixation with plate and screws
According to our results, we try to create a therapeutic algorithm based on the control volume criteria. We suggest using an endomedullary graft in case of varus displacement or medial column bone loss. In case of impacted forms with penetration of cortical diaphysis in the humeral head and conservation of the head position, even in case of lateral column comminution, the conservative treatment allows a very good result. In case of comminution of the lateral column and loss of calcar in the posterior side with the head impacted in varus position reverse prosthesis is the best option. The comminuted lateral column can be the cause of insufficient healing and loss of external rotation both in case of osteosynthesis and reverse or anatomical prosthesis.
Discussion
The main finding of our study is that the use of Control Volume severity grade could help to define the stability and the complexity of proximal humerus fracture and, consequently, the better type of treatment. The therapeutical choice, of course, should take into account also several patients factors, such as: age, functional requests, comorbidities, expectative.19 Another important aspect of our study, is that displaced proximal humeral fractures cannot be evaluated just with plain radiographs, even if performed with the trauma series views. The use of a CT-scan and of a 3D model evaluation let the surgeon knows the real position of the humeral head, the measurement of anterior or posterior head tilting, the percentage of bone loss of the calcar. The amount of comminution is a key point, especially when referred to the calcar. Calcar comminution significantly decreases the stability of fracture reconstruction and gives direct information on the technical demand of fracture repair. On the other side, the Control Volume classification has some critical points. First, it is difficult to calculate the accurate topographic evaluation of bone loss without the help of specific researchers. Second, similar head displacement with equivalent bone loss could be associated with different severity, due to high comminution or different topographical involvement. This means that, the Control Volume measurements are not easy to evaluate and requires experts support. However, we believe that the spread of this preoperative study of the fracture, could reduce the tendency to treat indiscriminately with a reverse prosthesis all the displaced proximal humerus fracture associated to bone loss. According to the Control Volume severity grade, even fractures characterized by significant fragments displacement with posterior and superior displacement of the greater tuberosity equal or superior to 5 mm, could be treated non-operative, if the humeral head remains in a neutral position. The use of conservative treatment and of osteosynthesis, for the right fracture type, could reduce the complication, historically observed with these types of treatment, especially in case of bone fragility.10–12 We believe that previous studies demonstrating no difference between conservative and surgical treatment have not specifically assessed the type of fracture. The PROHFER study, for example, assessed only the surgical neck fracture by plain radiographs.5,6 Finally, the Control Volume criteria and the severity grade, in our series could predict the clinical outcome for patients treated with the same procedure. For patients treated with reverse prosthesis, the clinical outcomes are directly related to the healing of the tuberosities around the prosthetic stem. One of the factors influencing the severity grade is the multi-fragmentation of the greater tuberosity. In fact, in these cases, despite the accurate reconstruction of the tuberosity and the use of bone chips to fill the interface between cortical tuberosity and prosthesis, the external rotation was less effective than when the great tuberosity is intact or with a large fragment.20 This study has several weaknesses: it is a retrospective study, including a relatively small number of patients. The use of Control Volume criteria should be tested in prospective multicentric observational studies.
CONCLUSIONS
The use of Control Volume criteria and severity grade are associated with better therapeutic and prognostic informations in confront to the Neer classification.
Contributions
Author contributions: the authors contributed equally
Conflict of interest
The authors declare that they have no conflict of interest
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgments
Acknowledgments
None
Funding Statement
None
References
- 1. Launonen AP, Lepola V, Saranko A, Flinkkilä T, Laitinen M, Mattila VM. Epidemiology of proximal humerus fractures. Arch Osteoporos. 2015;10(1). doi:10.1007/s11657-015-0209-4 [DOI] [PubMed]
- 2. Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clinical Orthopaedics Related Research. 2006;442:87-92. doi:10.1097/01.blo.0000194672.79634.78 [DOI] [PubMed]
- 3. Roux A, Decroocq L, El Batti S, et al. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98(6):715-719. doi:10.1016/j.otsr.2012.05.013 [DOI] [PubMed]
- 4. Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: Nationwide emergency department sample, 2008. Arthritis Care Res. 2012;64(3):407-414. doi:10.1002/acr.21563 [DOI] [PubMed]
- 5. Rangan A, Handoll H, Brealey S, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus the PROFHER randomized clinical trial. JAMA - J Am Med Assoc. 2015;313(10). doi:10.1001/jama.2015.1629H [DOI] [PubMed]
- 6. Handoll HH, Keding A, Corbacho B, Brealey SD, Hewitt C, Rangan A. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J. 2017;99-B(3):383-392. doi:10.1302/0301-620x.99b3.bjj-2016-1028 [DOI] [PMC free article] [PubMed]
- 7. Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2015;2015(11). doi:10.1002/14651858.cd000434.pub4 [DOI] [PubMed]
- 8. Beks RB, Ochen Y, Frima H, et al. Operative versus nonoperative treatment of proximal humeral fractures: a systematic review, meta-analysis, and comparison of observational studies and randomized controlled trials. J Shoulder Elb Surg. 2018;27(8):1526-1534. doi:10.1016/j.jse.2018.03.009 [DOI] [PubMed]
- 9. Petit CJ, Millett PJ, Endres NK, Diller D, Harris MB, Warner JJP. Management of proximal humeral fractures: Surgeons don’t agree. J Shoulder Elb Surg. 2010;19(3):446-451. doi:10.1016/j.jse.2009.06.012 [DOI] [PubMed]
- 10. Tepass A, Blumenstock G, Weise K, Rolauffs B, Bahrs C. Current strategies for the treatment of proximal humeral fractures: An analysis of a survey carried out at 348 hospitals in Germany, Austria, and Switzerland. J Shoulder Elb Surg. 2013;22(1):e8-e14. doi:10.1016/j.jse.2012.04.002 [DOI] [PubMed]
- 11. Schumaier A, Grawe B. Proximal Humerus Fractures: Evaluation and Management in the Elderly Patient. Geriatr Orthop Surg Rehabil. 2018;9:215145851775051. doi:10.1177/2151458517750516 [DOI] [PMC free article] [PubMed]
- 12. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22(4):542-549. doi:10.1016/j.jse.2012.06.008 [DOI] [PubMed]
- 13. Neer CS II. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52(6):1090-1103. doi:10.2106/00004623-197052060-00002 [PubMed]
- 14. Neer CS II. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077-1089. doi:10.1002/acr.21563 [PubMed]
- 15. Klug A, Wincheringer D, Harth J, Schmidt-Horlohé K, Hoffmann R, Gramlich Y. Complications after surgical treatment of proximal humerus fractures in the elderly—an analysis of complication patterns and risk factors for reverse shoulder arthroplasty and angular-stable plating. J Shoulder Elbow Surg. 2019;28(9):1674-1684. doi:10.1016/j.jse.2019.02.017 [DOI] [PubMed]
- 16. Russo R, Guastafierro A, Rotonda G della, et al. A new classification of impacted proximal humerus fractures based on the morpho-volumetric evaluation of humeral head bone loss with a 3D model. J Shoulder Elb Surg. 2020;29(10):e374-e385. doi:10.1016/j.jse.2020.02.022 [DOI] [PubMed]
- 17. Russo R, Guastafierro A, Pietroluongo LR. A morphovolumetric study of head malposition in proximal humeral fractures based on 3-dimensional computed tomography scans: the control volume theory. J Shoulder Elb Surg. 2018;27(5):940-949. doi:10.1016/j.jse.2017.12.004 [DOI] [PubMed]
- 18. Russo R, Visconti V, Lombardi LV, Ciccarelli M, Giudice G. The block-bridge system: A new concept and surgical technique to reconstruct articular surfaces and tuberosities in complex proximal humeral fractures. Journal of Shoulder and Elbow Surgery. 2008;17(1):29-36. doi:10.1016/j.jse.2007.03.027 [DOI] [PubMed]
- 19. Miquel J, Elisa C, Fernando S, Alba R, Torrens C. Non-medical patient-related factor influence in proximal humeral fracture outcomes: a multicentric study. Arch Orthop Trauma Surg. 2020;141(11):1919-1926. doi:10.1007/s00402-020-03643-9 [DOI] [PubMed]
- 20. O’Sullivan J, Lädermann A, Parsons BO, et al. A systematic review of tuberosity healing and outcomes following reverse shoulder arthroplasty for fracture according to humeral inclination of the prosthesis. J Shoulder Elbow Surg. 2020;29(9):1938-1949. doi:10.1016/j.jse.2020.03.032 [DOI] [PubMed]