Abstract
Purpose
To determine the diagnostic value of injury history, physical examination, six syndesmosis tests and overall clinical suspicion for syndesmosis injury.
Methods
All athletes (> 18 yrs) with an acute ankle injury presenting within 7 days post-injury were assessed for eligibility. Acute ankle injuries were excluded if imaging studies demonstrated a frank fracture or 3 T MRI could not be acquired within 10 days post-injury. Standardized injury history was recorded, and physical examination was performed by an Orthopaedic Surgeon or Sports Medicine Physician. Overall clinical suspicion was documented prior to MRI. Multivariate logistic regression was used to determine the association between independent predictors and syndesmosis injury.
Results
Between September 2016 and July 2019, a total of 150 acute ankle injuries were included. The median time from injury to acute clinical evaluation was 2 days (IQR 2). Prior to clinical evaluation, the median patient reported Visual Analog Scale for pain was 8/10 (IQR 2). Syndesmosis injury was present in 26 acute ankle injuries. An eversion mechanism of injury had a positive LR 3.47 (CI 95% 1.55–7.77). The squeeze tests had a positive LR of 2.20 (CI 95% 1.29–3.77) and a negative LR of 0.68 (CI 95% 0.48–0.98). Overall clinical suspicion had a sensitivity of 73% (CI 95% 52–88) and negative predictive value of 89% (CI 95% 78–95). Multivariate regression analyses demonstrated significant association for eversion mechanism of injury (OR 4.99; CI 95% 1.56–16.01) and a positive squeeze test (OR 3.25; CI 95% 1.24–8.51).
Conclusions
In an acute clinical setting with patients reporting high levels of ankle pain, a negative overall clinical suspicion reduces the probability of syndesmosis injury. Eversion mechanism of injury and a positive squeeze test are associated with higher odds of syndesmosis injury.
Level of evidence
Level III.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00167-022-06989-2.
Keywords: Ankle sprain, Syndesmosis, Physical examination
Introduction
Acute ankle sprains are among the most common sport-related injuries [7]. Sprains can affect the lateral ligaments, medial ligaments and the syndesmosis ankle ligaments. Complete rupture of the lateral ligaments is observed most commonly (40%) [19]. Within 2 days after injury, physical examination for diagnosing lateral ligament injury has a sensitivity of 71% and a specificity of 33% [6]. Delayed physical examination 5 days post-injury increases the sensitivity (96%) and specificity (84%). Syndesmosis injury is observed less frequently (20%) and is notoriously difficult to diagnose [19]. In the acute setting, the diagnosis of syndesmosis injury primarily relies on clinical evaluation [23].
Conflicting reports on the diagnostic value of physical examination have been published [15]. Two recent high-quality studies investigated the diagnostic value of clinical tests for partial or complete discontinuity of the syndesmosis using MRI [8, 22]. In a cohort of 96 patients presenting to an emergency department within 24 h after an acute ankle sprain, sensitivity (14–56%) and specificity (48–83%) of syndesmosis tests were reported as insufficient [8]. In a cohort of 87 athletes examined within 7 days after a suspected syndesmosis injury, tenderness of the anterior syndesmosis was reported to have the highest sensitivity (92%) and the squeeze test was found to have the highest specificity (88%) [22]. The heterogeneity in reported diagnostic values might be explained by the timing of physical examination and higher pre-test probability in the latter study. A study investigating the diagnostic value of injury history, physical examination, and overall clinical suspicion in athletes with an acute ankle injury is therefore warranted.
The aim of this study was to determine the diagnostic value of injury history, clinical findings, six syndesmosis tests (including the combination of these variables) and overall clinical suspicion for partial or complete discontinuity of the syndesmosis. The hypothesis is that in the acute setting, the diagnostic value of injury history, physical examination and overall clinical suspicion are sufficient to detect syndesmotic involvement in athletes with an acute ankle injury.
Materials and methods
Participants
Ethics approval was acquired from the Anti-Doping Lab Qatar Review Board (IRB No. F2016000153). Written informed consent was obtained from all athletes at time of inclusion. Between September 2016 and July 2019, athletes with acute ankle injuries were recruited for this prospective cohort study. All athletes presenting to the outpatient department of Aspetar Orthopaedic and Sports Medicine Hospital within 7 days after an acute ankle injury were assessed for eligibility. Inclusion criteria were: acute ankle injuries in adult athletes (≥ 18 yrs), participating in sports at a professional or recreational level. Ankle injuries were excluded if imaging demonstrated a frank fracture or if the 3 T MRI study could not be acquired within 10 days post-injury.
Clinical setting
A daily clinic for athletes with acute sports injuries is organized by Aspetar Orthopaedic and Sports Medicine Hospital. Patients can be seen by an Orthopaedic Surgeon or Sports Medicine Physician without the requirement of a referral. This results in a high volume of patients of which the majority presents within 24 h post-injury. The main language spoken by the medical staff at our institution is English; therefore, during consultation a nurse is present to provide Arabic translation.
Injury history and physical examination
An Orthopaedic Surgeon or Sports Medicine Physician recorded injury history and performed physical examination. Findings were recorded on a standardized reporting form. Injury history included: (1) Injury [new/recurrent] (2) Occasion [game/training/non-sports injury], (3) Contact [contact/non-contact], (4) Mechanism of injury [inversion/eversion/external-rotation/internal-rotation], (5) Perceived presence of swelling [yes/no], (6) Perceived ankle instability [yes/no], (7) Sensation of pain radiating up the leg [yes/no]. Physical examination included; (1) Presence of hematoma [yes/no] (2) Tenderness to palpation [lateral/medial/anterior/posterior] (3) Tenderness length over the syndesmosis [in cm], (4) Ability to walk normally [yes/no], (5) Ability to walk on toes [yes/no], Ability to walk on heels [yes/no], (6) Passive range of motion in dorsal flexion, plantar flexion, inversion and eversion [full/restricted/painful], (7) Presence of swelling [yes/no], (8) Swelling site [laterally/medially/anterior/posterior/syndesmosis].
Syndesmosis tests
The physicians performing the syndesmosis tests were provided with a short description of the clinical tests. No calibration session was organized prior to initiation of this study, to reflect a true clinical setting. The standardized clinical examination included a total of six syndesmosis tests: palpation of the AITFL [23]; squeeze test [10, 23], weight-bearing dorsiflexion external rotation (WB DF ER) test, non-weight-bearing dorsiflexion external rotation (NWB DF ER) test [16, 23], fibular translation test [17] and the Cotton test [3] (Supplementary appendix). Tests were considered positive if they provoked pain over the distal tibiofibular joint or if the examiner noticed instability of the ankle syndesmosis (Cotton test) [3, 10, 16, 17]. If the patient was unable to weight-bear (WB DF ER) or if a clinical test was too painful to be completed fully (Squeeze test, NWB DF ER test, Fibular translation test) they were considered positive (Cotton test excluded).
Overall clinical suspicion of syndesmosis injury
Clinical suspicion was based on the physicians’ overall interpretation of injury history, physical examination, and syndesmosis tests. Clinical suspicion was recorded using the modified West Point grading system[4]: partial rupture of the Anterior Inferior Tibiofibular Ligament (AITFL) with a stable syndesmosis (Grade I); complete rupture of the AITFL and injury to the Interosseous Ligament (IOL) with a stable syndesmosis (Grade IIa); complete rupture of the AITFL, IOL and the Posterior Inferior Tibiofibular Ligament (PITFL) or Deltoid ligaments with dynamic instability of the syndesmosis (Grade IIb) and complete disruption of the syndesmosis with frank diastasis (Grade III). Overall clinical suspicion for syndesmosis injury was considered positive when the modified West Point grading system was scored grade I or higher.
Reference standard
In this study, MRI was used as reference standard. With a sensitivity of 100% and specificity of 93% for injury of the AITFL, MRI has demonstrated to be a valuable alternative to arthroscopy [24]. Patients underwent MRI scans using a wide-bore 3.0-T MRI system (GE Discovery, GE Healthcare, Chicago, Illinois, United States) with an 8-channel receive only Foot & Ankle array (Invivo, Philips Healthcare, Best, The Netherlands). In the sagittal plane T1-weighted and Proton-Density Fat-Saturated [PD-FS] sequences were obtained, axial T2-weighted and PD-FS sequences were acquired and in the coronal plane PD-FS sequences were obtained [1].
Grading of syndesmosis ligaments
The obtained MR scans were graded by two musculoskeletal radiologists (J.A. & M.A.) with 11 and 3 years of experience in MSK-imaging, respectively.
Acute injuries of the AITFL, IOL and PITFL were graded according the four grade Schneck grading system[20]: normal (Grade 0); low-grade sprain (Grade 1: peri-ligamentous high signal/edema on proton density-weighted sequences and no discontinuity of fibers); partial discontinuity (Grade 2: partial discontinuity but preserved remnant fibers) and complete discontinuity (Grade 3).
Due to limited interrater and intrarater reliability for grading of the individual syndesmosis ligaments according the Schneck grading system (K 0.37–0.89), diagnostic disagreements between the radiologists were resolved in a consensus meeting [1].
Evaluation of MRI-findings
In this study, we evaluated the diagnostic value of injury history, physical examination, syndesmosis tests and clinical suspicion for partial or complete discontinuity of the AITFL and/or IOL and/or PITFL. The individual syndesmosis ligament (AITFL/IOL/PITFL) with the highest grade of injury was used as reference standard. For this analysis, grading was dichotomized as: (1) No discontinuity (normal ligament or peri-ligamentous edema) (2) Discontinuity (partial or complete discontinuity).
Statistical analysis
The diagnostic value of injury history, clinical findings, syndesmosis tests and clinical suspicion were evaluated using the MRI findings. The results of injury history and physical examination were dichotomized if needed; Occasion was dichotomized to (1) game (2) other; Each mechanism of injury was dichotomized to i.e. (1) inversion (2) other mechanism of injury. Tenderness to palpation and presence of swelling were dichotomized per location to i.e. (1) tenderness to palpation laterally (2) no palpation to tenderness laterally and range of motion was dichotomized per direction to i.e. (1) dorsal flexion painful (2) dorsal flexion not painful.
For each variable, a contingency table was created. From the 2 × 2 tables prevalence of positive test results, sensitivity, specificity, positive and negative likelihood ratio’s (LR+ and LR-), positive predictive value (PPV) and negative predictive value (NPV) were calculated, including confidence intervals (CI 95%). For tenderness length an optimal cut-off (Youden’s index = maximal value) was calculated using a ROC curve. For each variable the area under the curve (AUC) was calculated.
To test if a combination of variables could predict the presence of syndesmosis injury, we performed a logistic regression analysis. First, we analyzed the association between each variable and the presence of syndesmosis injury in a univariate logistic regression analysis. Variables with a p value < 0.15 were included in a multivariate logistic regression model. Regression analysis was performed using the forward method. Odds ratios for each variable were presented with their corresponding confidence intervals (CI 95%) and statistical significance was set at p value < 0.05. Statistical analysis was performed using SPSS software (V.21; IBM Corp). No a priori power analysis was performed for the outcome of this study.
Results
Baseline characteristics
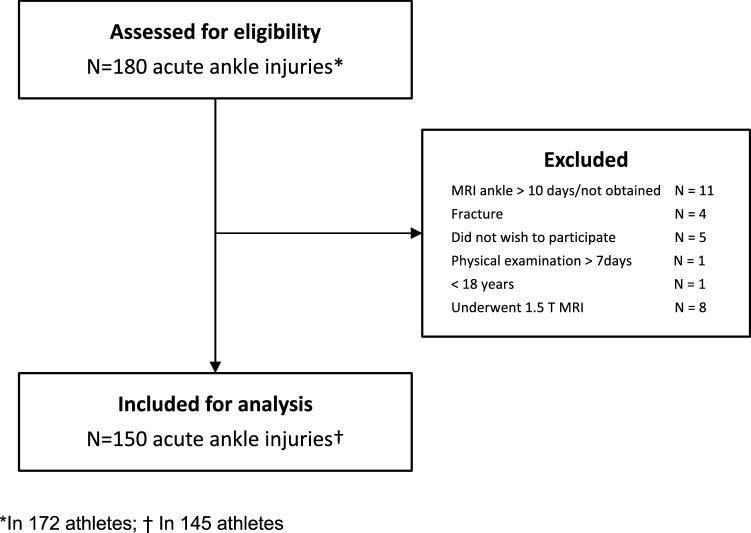
Between September 2016 and July 2019, a total of 180 acute ankle injuries were assessed for eligibility (Fig. 1). One-hundred-fifty were included in this study. (Flowchart 1) Of the included ankle injuries, four were subsequent injuries of the contralateral ankle and one was a re-injury (> 1 year). Most patients were male (91%). The median age at time of injury was 24 years (IQR 8). The median time from injury to physical examination was 2 days (IQR 2). At presentation, a median patient reported Visual Analog Scale (VAS) for pain of 8/10 (IQR 2) was recorded (in 129 patients). The MR scans were obtained a median 3 days (IQR 3) post-injury. Partial or complete discontinuity of the syndesmosis ligaments was observed in 26 of 150 (17%) acute ankle injuries. Injury of the AITFL was present in 26 acute ankle injuries (17%; 7 partial, 19 complete). The IOL was injured in 20 acute ankle injuries (13%; 8 partial, 12 complete) and the PITFL in 11 acute ankle injuries (7%; 10 partial, 1 complete). Concomitant injuries of the IOL or PITFL were not observed without injury of the AITFL.
Fig. 1.
Flowchart of patient inclusion
Diagnostic value of injury history, physical examination and overall clinical suspicion
The diagnostic value of injury history and physical examination are detailed in Tables 1 and 2. We found that an external rotation mechanism and eversion mechanism of injury had a positive LR of 4.77 (CI 95% 0.70–32.33) and 3.47 (CI 95% 1.55–7.77), respectively. Length of tenderness [≥ 2.5 cm] had a positive LR of 1.45 (CI 95% 1.02–2.04). Tenderness to palpation over the medial aspect of the ankle had a negative LR of 1.47 (CI 95% 1.06–2.03). The diagnostic values for the syndesmosis tests and clinical suspicion are detailed in Table 3. The squeeze test had the most diagnostic value with a positive LR of 2.20 (CI 95% 1.29–3.77) and a negative LR of 0.68 (CI 95% 0.48–0.98). Clinical suspicion for syndesmosis injury had a sensitivity of 73% and a negative predictive value of 89%.
Table 1.
Diagnostic accuracy of injury history for injury of the syndesmosis ligaments in 150 athletes with an acute ankle injury. MR imaging was used as reference standard
| Clinical history | Positive findings | Sensitivity % | Specificity % | LR+ | LR− | PPV % | NPV % | AUC |
|---|---|---|---|---|---|---|---|---|
| Injury [recurrent] | 37/150 (0.25) | 12 (3–31) | 73 (64–80) | 0.42 (0.14–1.27) | 1.22 (1.05–1.41) | 8 (2–23) | 80 (71–86) | 0.42 (0.31–0.53) |
| Occasion [game] | 78/150 (0.52) | 58 (37–76) | 49 (40–58) | 1.14 (0.78–1.65) | 0.86 (0.54–1.37) | 19 (12–30) | 85 (74–92) | 0.53 (0.41–0.66) |
| Contact [contact] | 69/138 (0.50) | 38 (19–61) | 48 (39–57) | 0.73 (0.41–1.29) | 1.29 (0.91–1.84) | 12 (5–22) | 81 (70–95) | 0.44 (0.34–0.54) |
| Mechanism of injury | ||||||||
| Inversion | 126/150 (0.84) | 65 (44–82) | 12 (7–19) | 0.74 (0.56–0.99) | 2.86 (1.50–5.44) | 13 (8–21) | 63 (41–80) | 0.39 (0.26–0.52) |
| Eversion | 19/150 (0.13) | 31 (15–52) | 91 (84–95) | 3.47 (1.55–7.77) | 0.76 (0.59–0.98) | 42 (21–66) | 86 (79–91) | 0.61 (0.48–0.74) |
| External rotation | 4/150 (0.03) | 8 (1–27) | 98 (94–99) | 4.77 (0.70–32.33) | 0.94 (0.84–1.05) | 50 (9–91) | 50 (9–91) | 0.53 (0.40–0.66) |
| Internal rotation | 6/150 (0.04) | 8 (1–27) | 97 (91–99) | 2.38 (0.46–12.34) | 0.95 (0.85–1.07) | 33 (6–76) | 83 (76–88) | 0.52 (0.40–0.65) |
| Perceived swelling | 126/149 (0.85) | 85 (64–95) | 15 (10–23) | 1.00 (0.84–1.20) | 1.00 (0.37–2.68) | 17 (11–25) | 83 (60–94) | 0.50 (0.38–0.62) |
| Perceived instability | 37/130 (0.28) | 21 (8–43) | 70 (60–78) | 0.69 (0.30–1.59) | 1.13 (0.92–1.40) | 14 (5–30) | 80 (70–87) | 0.47 (0.36–0.57) |
| Pain radiating up | 37/146 (0.25) | 26 (11–49) | 75 (66–82) | 1.04 (0.49–2.20) | 0.99 (0.77–1.27) | 16 (7–33) | 84 (76–90) | 0.50 (0.38–0.63) |
The prevalence of acute syndesmosis injuries and the diagnostic values of clinical history are presented. All values are presented with 95% confidence interval (95% CI); positive likelihood ratio (LR+); negative likelihood ratio (LR-); positive predictive value (PPV); negative predictive value (NPV)
Table 2.
Diagnostic accuracy of physical examination for injury of the syndesmosis ligaments in 150 athletes with an acute ankle injury. MR imaging was used as reference standard
| Clinical findings | Positive findings | Sensitivity % | Specificity % | LR+ | LR− | PPV % | NPV % | AUC |
|---|---|---|---|---|---|---|---|---|
| Presence of hematoma | 49/148 (0.33) | 28 (13–50) | 66 (57–74) | 0.82 (0.42–1.61) | 1.09 (0.85–1.41) | 14 (6–28) | 82 (73–89) | 0.47 (0.35–0.59) |
| Tenderness to palpation | ||||||||
| Lateral | 135/150 (0.90) | 88 (69–97) | 10 (5–17) | 0.97 (0.84–1.13) | 1.19 (0.35–4.00) | 17 (11–25) | 80 (51–95) | 0.49 (0.37–0.61) |
| Medial | 82/150 (0.55) | 38 (21–59) | 42 (33–51) | 0.66 (0.40–1.10) | 1.47 (1.06–2.03) | 12 (6–22) | 76 (64–86) | 0.40 (0.28–0.52) |
| Anterior | 47/150 (0.32) | 23 (10–44) | 67 (58–75) | 0.70 (0.33–1.47) | 1.15 (0.92–1.43) | 13 (5–26) | 81 (71–87) | 0.45 (0.33–0.57) |
| Posterior | 19/150 (0.13) | 12 (3–31) | 87 (80–92) | 0.89 (0.28–2.85) | 1.02 (0.88–1.17) | 16 (4–40) | 82 (75–88) | 0.49 (0.37–0.61) |
| Tenderness length [≥ 2.5 cm] | 69/139 (0.50) | 67 (45–84) | 54 (44–63) | 1.45 (1.02–2.04) | 0.62 (0.35–1.10) | 23 (14–35) | 89 (78–95) | 0.60 (0.48–0.73) |
| Normal walk | 77/150 (0.51) | 62 (41–79) | 51 (42–60) | 1.25 (0.88–1.78) | 0.76 (0.46–1.25) | 21 (13–32) | 86 (76–93) | 0.56 (0.44–0.68) |
| Walk on toes | 89/147 (0.61) | 69 (48–85) | 41 (33–51) | 1.18 (0.88–1.59) | 0.74 (0.41–1.36) | 20 (13–30) | 86 (74–93) | 0.55 (0.43–0.67) |
| Walk on heels | 79/144 (0.55) | 56 (35–75) | 45 (36–55) | 1.03 (0.70–1.51) | 0.97 (0.61–1.54) | 18 (10–28) | 83 (71–91) | 0.51 (0.38–0.63) |
| Range of motion | ||||||||
| Pain on dorsal flexion | 94/150 (0.63) | 58 (37–76) | 36 (28–45) | 0.90 (0.63–1.29) | 1.17 (0.72–1.88) | 16 (9–25) | 80 (67–89) | 0.47 (0.35–0.59) |
| Pain on plantar flexion | 83/150 (0.55) | 56 (35–75) | 43 (35–53) | 0.99 (0.68–1.45) | 1.01 (0.64–1.61) | 17 (10–27) | 83 (71–91) | 0.50 (0.37–0.62) |
| Pain on inversion | 99/150 (0.66) | 69 (48–85) | 34 (26–43) | 1.05 (0.79–1.40) | 0.90 (0.49–1.65) | 18 (11–27) | 84 (70–92) | 0.52 (0.40–0.64) |
| Pain on eversion | 85/150 (0.56) | 56 (35–75) | 42 (33–50) | 0.95 (0.65–1.39) | 1.06 (0.67–1.70) | 16 (10–26) | 82 (70–90) | 0.49 (0.36–61) |
| Presence of swelling | ||||||||
| Lateral | 102/131 (0.78) | 88 (67–97) | 24 (17–34) | 1.16 (0.96–1.39) | 0.51 (0.17–1.57) | 21 (13–30) | 90 (72–97) | 0.56 (0.44–0.68) |
| Medial | 47/131 (0.36) | 38 (20–59) | 64 (55–73) | 1.06 (0.59–1.88) | 0.97 (0.70–1.33) | 19 (10–34) | 82 (72–89) | 0.51 (0.38–0.64) |
| Anterior | 37/131 (0.28) | 25 (11–47) | 71 (61–79) | 0.86 (0.41–1.83) | 1.06 (0.83–1.34) | 16 (7–33) | 81 (71–88) | 0.48 (0.35–0.61) |
| Posterior | 12/131 (0.09) | 8 (1–28) | 91 (83–95) | 0.89 (0.21–3.81) | 1.01 (0.89–1.14) | 17 (3–49) | 82 (73–88) | 0.50 (0.37–0.62) |
The prevalence of acute syndesmosis injuries and the diagnostic values of clinical findings are presented. All values are presented with 95% confidence interval (95% CI); positive likelihood ratio (LR+); negative likelihood ratio (LR-); positive predictive value (PPV); negative predictive value (NPV)
Table 3.
Diagnostic accuracy of six syndesmosis tests and clinical suspicion for injury of the syndesmosis ligaments in 150 athletes with an acute ankle injury. MR imaging was used as reference standard
| Positive findings | Sensitivity % | Specificity % | LR+ | LR− | PPV % | NPV % | AUC | |
|---|---|---|---|---|---|---|---|---|
| Syndesmosis tests | ||||||||
| Tenderness AITFL | 78/150 (0.52) | 58 (37–76) | 49 (40–58) | 1.14 (0.78–1.65) | 0.86 (0.54–1.37) | 19 (12–30) | 85 (74–92) | 0.52 (0.43–0.61) |
| Squeeze test | 38/150 (0.25) | 46 (27–66) | 79 (71–86) | 2.20 (1.29–3.77) | 0.68 (0.48–0.98) | 32 (18–49) | 88 (80–93) | 0.60 (0.49–0.71) |
| NWB DF ER test | 74/148 (0.50) | 58 (37–76) | 52 (42–61) | 1.19 (0.82–1.74) | 0.82 (0.52–1.30) | 20 (12–32) | 85 (75–92) | 0.53 (0.44–0.62) |
| WB DF ER test | 99/149 (0.66) | 69 (48–85) | 34 (26–43) | 1.05 (0.79–1.40) | 0.90 (0.49–1.65) | 18 (11–27) | 84 (70–92) | 0.51 (0.42–0.61) |
| Fibular translation test | 26/147 (0.18) | 15 (5–36) | 82 (74–88) | 0.85 (0.32–2.25) | 1.03 (0.87–1.22) | 15 (5–36) | 82 (74–88) | 0.49 (0.37–0.61) |
| Cotton test | 21/139 (0.15) | 27 (12–48) | 88 (80–93) | 2.17 (0.98–4.84) | 0.83 (0.66–1.06) | 33 (15–57) | 84 (76–90) | 0.59 (0.45–0.73) |
| All tests negative | 35/147 (0.23) | 23 (10–44) | 76 (67–83) | 0.96 (0.45–2.08) | 1.01 (0.82–1.26) | 17 (7–34) | 82 (74–88) | 0.50 (0.37–0.62) |
| Clinical suspicion | ||||||||
| Syndesmosis injury | 79/143 (0.55) | 73 (52–88) | 49 (39–58) | 1.43 (1.06–1.91) | 0.55 (0.29–1.06) | 24 (15–35) | 89 (78–95) | 0.61 (0.49–0.73) |
The prevalence of acute syndesmosis injuries and the diagnostic values of six syndesmosis tests (including the combination of these six tests) and clinical suspicion are presented. All values are presented with 95% confidence interval (95% CI); positive likelihood ratio (LR +); negative likelihood ratio (LR-); positive predictive value (PPV); negative predictive value (NPV)
Univariate analysis
Various predictors were associated with injury of the syndesmosis ligaments in univariate logistic regression analysis. (Table 4). Eversion mechanism of injury (OR 4.57; CI 95% 1.62–12.89; p < 0.00), a positive squeeze test (OR 3.23; CI 95% 1.34–7.82; p = 0.01), tenderness length [≥ 2.5 cm] (2.34; CI 95%0.93–5.90; p = 0.07) and clinical suspicion (OR 2.58; 1.01–6.60; p = 0.05) were associated with higher odds of syndesmosis injury. Inversion mechanism of injury (OR 0.26; 0.10–0.69; p = 0.01) was associated with lower odds of syndesmosis injury.
Table 4.
Univariate logistic regression analysis for the association between injury history, physical examination, syndesmosis tests and clinical suspicion for the presence of syndesmosis injury
| N | OR (95%CI) | SE | P-value | |
|---|---|---|---|---|
| Clinical history | ||||
| Injury [recurrent] | 150 | 0.35 (0.10–1.23) | 0.65 | 0.10 |
| Occasion [game] | 150 | 1.32 (0.56–3.10) | 0.44 | n.s |
| Contact [contact] | 138 | 0.57 (0.22–1.46) | 0.49 | n.s |
| Mechanism of injury | ||||
| Inversion | 150 | 0.26 (0.10–0.69) | 0.50 | 0.01 |
| Eversion | 150 | 4.57 (1.62–12.89) | 0.53 | 0.00 |
| External rotation | 150 | 5.08 (0.68–37.87) | 1.03 | 0.11 |
| Internal rotation | 150 | 2.50 (0.43–14.43) | 0.89 | n.s |
| Perceived swelling | 149 | 1.01 (0.31–3.25) | 0.60 | n.s |
| Pain radiating up | 146 | 1.05 (0.38–2.89) | 0.52 | n.s |
| Clinical findings | ||||
| Presence of hematoma | 148 | 0.75 (0.29–1.94) | 0.48 | n.s |
| Tenderness to palpation | ||||
| Lateral | 150 | 0.82 (0.22–3.14) | 0.69 | n.s |
| Medial | 150 | 0.45 (0.19–1.07) | 0.44 | 0.07 |
| Anterior | 150 | 0.61 (0.23–1.63) | 0.50 | n.s |
| Posterior | 150 | 0.85 (0.24–3.27) | 0.67 | n.s |
| Tenderness length [≥ 2.5 cm] | 139 | 2.34 (0.93–5.90) | 0.47 | 0.07 |
| Normal walk | 150 | 1.65 (0.70–3.93) | 0.44 | n.s |
| Walk on toes | 147 | 1.59 (0.64–3.93) | 0.46 | n.s |
| Walk on heels | 144 | 1.06 (0.44–2.52) | 0.44 | n.s |
| Range of motion | ||||
| Pain with passive dorsal flexion | 150 | 0.77 (0.33–1.84) | 0.44 | n.s |
| Presence of swelling | 142 | 1.26 (0.34–4.67) | 0.67 | n.s |
| Lateral | 131 | 2.25 (0.62–8.15) | 0.66 | n.s |
| Medial | 131 | 1.09 (0.44–2.72) | 0.47 | n.s |
| Anterior | 131 | 0.82 (0.30–2.25) | 0.52 | n.s |
| Posterior | 131 | 0.88 (0.18–4.31) | 0.81 | n.s |
| Syndesmosis tests | ||||
| Tenderness AITFL | 150 | 1.32 (0.56–3.10) | 0.44 | n.s |
| Squeeze test | 150 | 3.23 (1.34–7.82) | 0.45 | 0.01 |
| NWB DF ER test | 148 | 1.00 (0.98–1.01) | 0.01 | n.s |
| WB DF ER test | 149 | 1.00 (0.97–1.02) | 0.01 | n.s |
| Fibular translation test | 147 | 0.82 (0.26–2.61) | 0.59 | n.s |
| Cotton test | 139 | 1.00 (0.99–1.00) | 0.00 | n.s |
| All tests clinical tests negative | 147 | 0.92 (0.35–2.60) | 0.51 | n.s |
| Clinical suspicion | ||||
| Syndesmosis injury | 143 | 2.58 (1.01–6.60) | 0.48 | 0.05 |
The odds ratios of the independent variables associated with syndesmosis injury are presented. Values are presented as β-coefficients with corresponding 95% confidence interval (95% CI); Standard Error (SE); P-value > 0.15 (n.s.)
Multivariate analysis
In the multivariate logistic regression analysis mechanism of injury [eversion] (OR 4.99; CI 95% 1.56–16.01; p = 0.01) and a positive squeeze test (OR 3.25; CI 95% 1.24–8.51); p = 0.02) were associated with higher odds of syndesmosis injury (Table 5).
Table 5.
Multivariate logistic regression analysis for the association between injury history, physical examination and syndesmosis tests for the presence of syndesmosis injury
| N | Multivariate | |||
|---|---|---|---|---|
| OR (95%CI) | SE | P-value | ||
| Clinical history | ||||
| Mechanism of injury [eversion] | 150 | 4.99 (1.56–16.01) | 0.60 | 0.01 |
| Physical examination | ||||
| Tenderness to palpation [medial] | 150 | 0.32 (0.12–0.83) | 0.49 | 0.02 |
| Syndesmosis tests | ||||
| Squeeze test | 150 | 3.25 (1.24–8.51) | 0.49 | 0.02 |
The odds ratios of the independent variables associated with syndesmosis injury are presented. Values are presented as β-coefficients with corresponding 95% confidence interval (95% CI); Standard Error (SE)
Discussion
The most important finding in this study is that despite high levels of pain in the acute clinical setting, a negative overall clinical suspicion reduces the probability of syndesmosis injury. An eversion mechanism of injury and a positive squeeze test are associated with higher odds of syndesmosis injury. None of the included variables had sufficient diagnostic value to completely rule out syndesmosis injury.
Diagnostic value of injury history
Injury history is of major importance for the diagnosis of syndesmosis injury as demonstrated in this study. With an external rotation mechanism of injury the probability of syndesmosis injury increased from a pre-test probability of 17% to a post-test probability of 49%. An eversion mechanism of injury changed the post-test probability to 42%. Despite high specificity, external rotation did not reach significance in the logistic regression analyses as only few patients reported this mechanism of injury. A previous study investigating the diagnostic value of the mechanism of injury reported a positive likelihood ratio of 1.07 (CI 95% 0.87–1.32) with an external rotation and/or dorsiflexion mechanism [22]. As the study by Sman et al. only included patients with at least one positive syndesmosis test or a clinical suspicion of syndesmosis injury selection bias may have occurred. Based on our results we emphasize the importance of history taking and the mechanism of injury in particular [5, 11, 25].
Diagnostic value of physical examination
The test characteristics of physical examination were insufficient to completely rule out syndesmosis injury in the acute setting. The presence of tenderness over the syndesmosis [≥ 2.5 cm] resulted in a post-test probability of 23%. While peri-ligamentous edema of the syndesmosis was considered disease negative, it is an important source of tenderness and might therefore have had a negative effect on the diagnostic value [6, 14]. Medial tenderness to palpation demonstrated an inverse association in the multivariate logistic regression analysis. Two previous studies reported similar findings [8, 22]. This might be due to the low number of high grade syndesmosis injuries with associated deltoid ligament injury included in these studies [21]. In contrast, compression injury of the deltoid ligaments is commonly observed in inversion injuries [14, 19]. To put our findings into perspective, physical examination of the lateral ankle ligaments within 48 h post-injury has a sensitivity of 71% and a specificity of 33% [6]. Delayed physical examination has a sensitivity of 96% and specificity of 84%. Future studies should therefore aim to investigate the diagnostic value of delayed physical examination for syndesmosis injury.
Diagnostic value of the individual syndesmosis tests
The squeeze test had the highest discriminative value for the presence of syndesmosis injury in the acute setting. A positive squeeze tests resulted in a post-test probability of 31% and a negative squeeze test resulted in a post-test probability of 12%. None of the six individual syndesmosis tests had sufficient diagnostic value to completely rule out syndesmosis injury. A previous study reported on the diagnostic value of five syndesmosis tests in a cohort of patients presenting to an Emergency department within 24 h post-injury [8]. Of the included tests, the external rotation stress test was found to have the highest sensitvity (56%). It was therefore concluded that clinical tests could not be relied upon. In another study the diagnostic value was investigated in a cohort of athletes examined within 7 days after a suspected syndesmosis injury [22]. The squeeze test was found to have the highest positive likelihood ratio (positive LR 2.15 CI 95% 0.86–5.39). Sensitivity was highest for tenderness over the syndesmosis ligaments (92%) and the non-weight-bearing dorsiflexion external rotation test (71%). Sman et al. therefore advised to combine sensitive tests (tenderness of the syndesmosis ligaments and the dorsiflexion-external rotation stress test) with specific tests (the squeeze tests). As high levels of pain are present in the acute setting, the discrepancy of reported diagnostic values might be attributed to the timing of physical examination. Based on our results, we recommend use of the squeeze test in the acute clinical setting.
Diagnostic value of clinical suspicion
This is the first study investigating the diagnostic value of clinical suspicion for syndesmosis in the acute clinical setting. Despite high levels of pain, overall clinical suspicion had a sensitivity of 73% and negative predictive value of 89%. When there was no clinical suspicion of syndesmosis injury the post-test probability of syndesmosis injury was reduced to 10%.
The strengths of this study include its prospective design, broad inclusion criteria and acquisition of 3.0-T MR scans within 10 days post-injury [18]. Standardized clinical examination was performed by 19 physicians, trained in 10 different countries. This provides external validity to our findings. To date, this is the largest study evaluating the diagnostic value of injury history, physical examination, syndesmosis tests and overall clinical suspicion for syndesmosis injury. A limitation of this study is that most patients presented to our walk-in clinic within 48 h post-injury. High levels of pain might therefore have affected the reported diagnostic values negatively. Despite our aim to recruit female athletes, only few presented to our walk-in clinic. Although physical examination was standardized and clear test instructions were provided, minor variations in the execution might have influenced the reported diagnostic accuracy. Finally, MRI was used as reference standard despite its inability to diagnose syndesmosis instability [9, 13].
In the acute setting, clinical evaluation may aid in the early recognition of syndesmosis injuries [12]. Clinical evaluation can be used to decide whether to refer for immediate further diagnostic tests or delayed physical examination. Athletes reporting an external rotation mechanism of injury and/or a positive squeeze test might be referred for MRI. Athletes with a negative overall clinical suspicion can be referred for delayed physical examination 5–10 days post-injury. In the acute setting none of the included variables was sufficient to completely rule out the presence of syndesmosis injury. When the aim is to completely rule out syndesmosis injury, diagnostic methods such as (dynamic-) ultrasound might provide a viable alternative [2].
Conclusion
In an acute clinical setting with patients reporting high levels of ankle pain, a negative overall clinical suspicion reduces the probability of syndesmosis injury. An eversion mechanism of injury and a positive squeeze test are associated with higher odds of syndesmosis injury.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank the colleagues at Aspetar Orthopaedic and Sports Medicine Hospital and the National Sports Medicine Programme for their contribution.
Abbreviations
- AITFL
Anterior inferior tibiofibular ligament
- AUC
Area under the curve
- CI
Confidence interval
- IOL
Interosseous ligament
- IQR
Interquartile range
- K
Kappa
- LR−
Negative likelihood ratio
- LR+
Positive likelihood ratio
- MRI
Magnetic resonance imaging
- MSK
Musculoskeletal
- NPV
Negative predictive value
- NWB DF ER
Non-weight-bearing dorsal flexion external rotation
- OR
Odd ratio
- PD-FS
Proton-density fat-saturated
- PITFL
Posterior tibiofibular ligament
- PPV
Positive predictive value
- T
Tesla
- VAS
Visual analog scale
- WB DF ER
Weight-bearing dorsal flexion external rotation
Authors’ contribution
Study concepts: TPAB, GMMJK, JLT; Study design: TPAB, OA-S, JA, CG, LG, PD’H, GMMJK, JLT; Data acquisition: TPAB, OA-S, JA, MRA-N, CG, LG, LH, PD’H; Quality control of data and algorithms: TPAB, JLT; Data analysis and interpretation: TPAB, JLT, GMMJK; Statistical analysis: TPAB, JLT; Manuscript preparation: TPAB, GMMJK, JLT; Manuscript editing: TPAB, OA-S, JA, MRA-N, CG, LG, PD’H, GMMJK, JLT; Manuscript review: TPAB, OA-S, JA, MRA-N, CG, LG, PD’H, GMMJK, JLT.
Funding
This prospective cohort study was funded by Aspetar Orthopaedic and Sports Medicine Hospital.
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Ethics approval was acquired from the Anti-Doping Lab Qatar Review Board (IRB No. F2016000153).
Informed consent
Written informed consent was obtained from all athletes at time of inclusion.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baltes TPA, Arnaiz J, Al-Naimi MR, Al-Sayrafi O, Geertsema C, Geertsema L, et al. Limited intrarater and interrater reliability of acute ligamentous ankle injuries on 3 T MRI. J ISAKOS. 2021;6:153–160. doi: 10.1136/jisakos-2020-000503. [DOI] [PubMed] [Google Scholar]
- 2.Baltes TPA, Arnáiz J, Geertsema L, Geertsema C, D’Hooghe P, Kerkhoffs GMMJ, et al. Diagnostic value of ultrasonography in acute lateral and syndesmotic ligamentous ankle injuries. Eur Radiol. 2021;31:2610–2620. doi: 10.1007/s00330-020-07305-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beumer A, Swierstra BA, Mulder PGH. Clinical diagnosis of syndesmotic ankle instability: evaluation of stress tests behind the curtains. Acta Orthop Scand. 2002;73:667–669. doi: 10.1080/000164702321039642. [DOI] [PubMed] [Google Scholar]
- 4.Calder JD, Bamford R, Petrie A, McCollum GA. Stable versus unstable grade II high ankle sprains: a prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy. 2016;32:634–642. doi: 10.1016/j.arthro.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Delahunt E, Farrell G, Boylan A, Kerin F, Tierney P, Hogan H, et al. Mechanisms of acute ankle syndesmosis ligament injuries in professional male rugby union players: a systematic visual video analysis. Br J Sports Med. 2021;55:691–696. doi: 10.1136/bjsports-2020-102281. [DOI] [PubMed] [Google Scholar]
- 6.van Dijk CN, Mol BW, Lim LS, Marti RK, Bossuyt PM. Diagnosis of ligament rupture of the ankle joint. Physical examination, arthrography, stress radiography and sonography compared in 160 patients after inversion trauma. Acta Orthop Scand. 1996;67:566–570. doi: 10.3109/17453679608997757. [DOI] [PubMed] [Google Scholar]
- 7.Fong DT-P, Hong Y, Chan L-K, Yung PS-H, Chan K-M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 8.Großterlinden LG, Hartel M, Yamamura J, Schoennagel B, Bürger N, Krause M, et al. Isolated syndesmotic injuries in acute ankle sprains: diagnostic significance of clinical examination and MRI. Knee Surgery Sport Traumatol Arthrosc. 2016;24:1180–1186. doi: 10.1007/s00167-015-3604-x. [DOI] [PubMed] [Google Scholar]
- 9.Hagemeijer NC, Elghazy MA, Waryasz G, Guss D, DiGiovanni CW, Kerkhoffs GMMJ. Arthroscopic coronal plane syndesmotic instability has been over-diagnosed. Knee Surgery Sport Traumatol Arthrosc. 2021;29:310–323. doi: 10.1007/s00167-020-06067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hopkinson WJ, St PP, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10:325–330. doi: 10.1177/107110079001000607. [DOI] [PubMed] [Google Scholar]
- 11.Jain N, Murray D, Kemp S, Calder J. High-speed video analysis of syndesmosis injuries in soccer—can it predict injury mechanism and return to play? A pilot study. Foot Ankle Orthop. 2018;3:247301141878042. doi: 10.1177/2473011418780429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kent S, Yeo G, Marsland D, Randell M, Forster B, Lutz M, et al. Delayed stabilisation of dynamically unstable syndesmotic injuries results in worse functional outcomes. Knee Surgery Sport Traumatol Arthrosc. 2020;28:3347–3353. doi: 10.1007/s00167-020-05962-1. [DOI] [PubMed] [Google Scholar]
- 13.Lubberts B, Guss D, Vopat BG, Johnson AH, van Dijk CN, Lee H, et al. The arthroscopic syndesmotic assessment tool can differentiate between stable and unstable ankle syndesmoses. Knee Surgery Sport Traumatol Arthrosc. 2020;28:193–201. doi: 10.1007/s00167-018-5229-3. [DOI] [PubMed] [Google Scholar]
- 14.McCollum GA, van den Bekerom MPJ, Kerkhoffs GMMJ, Calder JDF, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21:1328–1337. doi: 10.1007/s00167-012-2205-1. [DOI] [PubMed] [Google Scholar]
- 15.Netterström-Wedin F, Bleakley C. Diagnostic accuracy of clinical tests assessing ligamentous injury of the ankle syndesmosis: a systematic review with meta-analysis. Phys Ther Sport. 2021;49:214–226. doi: 10.1016/j.ptsp.2021.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29:31–35. doi: 10.1177/03635465010290011001. [DOI] [PubMed] [Google Scholar]
- 17.Ogilvie-Harris DJ, Reed SC. Disruption of the ankle syndesmosis: diagnosis and treatment by arthroscopic surgery. Arthroscopy. 1994;10:561–568. doi: 10.1016/S0749-8063(05)80015-5. [DOI] [PubMed] [Google Scholar]
- 18.Randell M, Marsland D, Ballard E, Forster B, Lutz M. MRI for high ankle sprains with an unstable syndesmosis: posterior malleolus bone oedema is common and time to scan matters. Knee Surgery Sport Traumatol Arthrosc. 2019;27:2890–2897. doi: 10.1007/s00167-019-05581-5. [DOI] [PubMed] [Google Scholar]
- 19.Roemer FW, Jomaah N, Niu J, Almusa E, Roger B, D’Hooghe P, et al. Ligamentous injuries and the risk of associated tissue damage in acute ankle sprains in athletes. Am J Sports Med. 2014;42:1549–1557. doi: 10.1177/0363546514529643. [DOI] [PubMed] [Google Scholar]
- 20.Schneck CD, Mesgarzadeh M, Bonakdarpour A. MR imaging of the most commonly injured ankle ligaments Part II Ligament injuries. Radiology. 1992;184:507–512. doi: 10.1148/radiology.184.2.1620856. [DOI] [PubMed] [Google Scholar]
- 21.Sikka RS, Fetzer GB, Sugarman E, Wright RW, Fritts H, Boyd JL, et al. Correlating MRI findings with disability in syndesmotic sprains of NFL players. Foot Ankle Int. 2012;33:371–378. doi: 10.3113/FAI.2012.0371. [DOI] [PubMed] [Google Scholar]
- 22.Sman AD, Hiller CE, Rae K, Linklater J, Black DA, Nicholson LL, et al. Diagnostic accuracy of clinical tests for ankle syndesmosis injury. Br J Sports Med. 2015;49:323–329. doi: 10.1136/bjsports-2013-092787. [DOI] [PubMed] [Google Scholar]
- 23.Sman AD, Hiller CE, Refshauge KM. Diagnostic accuracy of clinical tests for diagnosis of ankle syndesmosis injury: a systematic review. Br J Sports Med. 2013;47:620–628. doi: 10.1136/bjsports-2012-091702. [DOI] [PubMed] [Google Scholar]
- 24.Takao M, Ochi M, Oae K, Naito K, Uchio Y. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85:324–329. doi: 10.1302/0301-620X.85B3.13174. [DOI] [PubMed] [Google Scholar]
- 25.Tampere T, D’Hooghe P. The ankle syndesmosis pivot shift “Are we reviving the ACL story?”. Knee Surgery Sport Traumatol Arthrosc. 2021;29:3508–3511. doi: 10.1007/s00167-020-06008-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.