Abstract
Background
The study was conducted to establish use of printed investigation sheets as checklists for timely workup and clinical evaluation of antenatal women with medical diseases; admitted in maternity ward, by third day of their hospital admission. This was aimed to standardize care, avoid repeated blood sampling of patients, avoid delay in starting the treatment and help teams perform optimally by systematic use of quality improvement (QI) tools.
Methods
The present study was conducted in the Department of Obstetrics and Gynaecology at a tertiary care teaching hospital using point-of-care quality improvement methodology systematically. A QI team was made who formulated an aim statement, conducted a root-cause analysis, performed plan-do-study-act (PDSA) cycles. The outcome was measured as complete clinical evaluation of antenatal women with anaemia, hypertension, and/or diabetes by third day of admission in the maternity ward.
Results
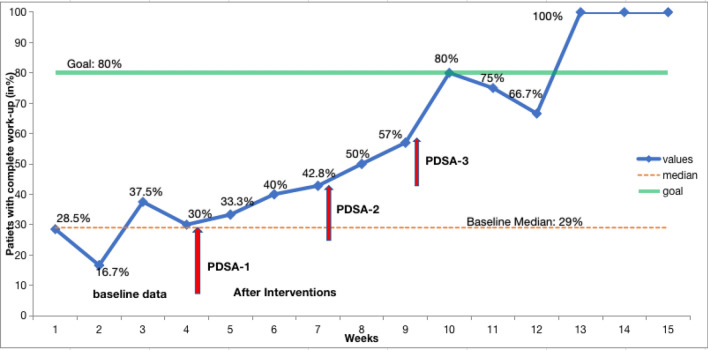
The baseline data showed that median percentage of patients with complete clinical evaluation was only 29.2%. After a root-cause analysis with fishbone tool, three PDSA cycles were conducted to achieve the target of 80%. After the third PDSA cycle, complete clinical evaluation in anaemia, hypertension, diabetes showed an improving trend with a median of 75%.
Conclusion
Adopting simple principles of quality improvement, initiating use of printed investigation sheets as checklist can streamline and expedite clinical evaluation of antenatal patients with medical problems so as to avoid unnecessary delay in initiating the management in busy maternity wards.
Keywords: Quality improvement, Checklists, Standardized care, Patient safety, Quality of care, Printed investigation sheet, Plan-do-study-act (PDSA) cycle, Antenatal
Introduction
Quality of care should be safe, effective, and patient-centred [1]. There is a definite gap between the desired and the delivered practises, which should be overcome to improve patient satisfaction. Though improving the quality of patient care has been identified as an important aspect of daily clinical work, the task in itself seems mammoth. Thus, the use of quality improvement (QI) tools can make this seemingly huge task achievable by breaking it into small steps. This is based on teamwork and rational thinking, resulting in improved processes and higher satisfaction [2, 3] in clients as well as caregivers. The present work was conducted to use QI principles in establishing the use of printed investigation sheets as checklists for achieving complete work-up and clinical evaluation of antenatal women admitted in maternity ward, by the third of their admission in the hospital.
Problem Description
In obstetric wards, it is a routine to send investigations the next morning after the antenatal women get admitted. They include routine investigations and specific ones pertaining to a particular problem such as anaemia, hypertension, or diabetes. Quite often it was observed in our wards that all the investigations required for clinical evaluation of new admissions were not sent on the same day. It was noted that some tests were missed by the residents due to recall issues and they would take sample for investigations that they could remember. This would get exaggerated even more when there was a posting-change to the maternity ward or when a resident of the newly-joined batch was posted. And even though most reports could be collected the same day from labs or could be checked online in the hospital computers; frequently complete reports would not be entered in the case sheets of patients. Few investigations like high-performance liquid chromatography (HPLC), iron studies, or cultures could only be collected after 48 h due to lab processing time. Thus, sometimes the residents would forget to collect and note these reports which were sent 2 days back. In our setting, the printed investigation sheets enumerating the tests already existed with designated spaces to enter the reports. However, they were not being used by the residents on a regular basis. This led to incomplete clinical evaluation, need for taking repeat blood samples, delay in starting treatment, and possible increase in length of hospital stay.
Available Knowledge
The purpose of a checklist is to minimize the error of omission and to ensure that each and every detail is taken care of [4]. It is a very effective way to ensure that uniformity is maintained irrespective of the operator. For instance, a study was conducted by Janicki et al. [5], to determine if using a specific ultrasound image criteria to screen fetal heart improved the cardiac exam completion rate. In this study, a checklist was used to categorize the cardiac exams as complete-normal, complete-abnormal or incomplete. The performance was compared with a 7-month period prior to the introduction of the checklist. The checklist utilization improved the cardiac exam completion rate significantly by 8.9% [5]. If predesigned proformas are used or a checklist for investigations pertaining to a problem is used, then the number of missing data or reports is significantly less, resulting in improvement in patient care. Therefore, a checklist maybe a straightforward and inexpensive intervention to reduce process variability with the potential to significantly improve outcomes [4].
Rationale and Specific Aim
This project aimed to use the principles of QI which included analysis of the identified problem and implementation of plan-do-study-act (PDSA) cycles for a step-by-step approach to improvement. Printed investigation sheets for various medical disorders in obstetrics exist in the wards but are not routinely used by the residents. Thus, it was decided to implement the use of these sheets as checklists for common obstetric problems in order to avoid missing out any investigation and for complete, detailed, and organized manner of entering the reports in the case sheets. The baseline data showed that the two most common indications of admissions in our maternity ward were hypertensive disorders and diabetes. Moreover, anaemia coexisted in 50% in-patients. Thus, the complete work-up and clinical evaluation of these three conditions by day-3 of admission to maternity ward were chosen for the QI project.
Customized investigation checklists for hypertension in pregnancy, gestational diabetes, and anaemia were prepared. They were printed utilizing both sides of a single paper along with the list of routine antenatal investigations.
This project aimed to increase complete clinical evaluation of new admissions in admitted antenatal patients with anaemia, hypertension, or diabetes from existing baseline median of 29–80% by third day of admission by initiating the use of printed investigation sheets as checklist in next 12 weeks.
Materials and Methods
Context
A prospective study was conducted in the Department of Obstetrics and Gynaecology at a tertiary care teaching apex institute in India.
Intervention
The maternity team consisting of doctors and nurses was first sensitized to the QI initiative and methodology. The four steps were introduced systematically. A team was formed which consisted of faculty, senior resident, and junior resident from Department of Obstetrics and Gynaecology. Baseline data was collected from case sheets of in-patients in the maternity ward over 4 weeks. A team meeting was held initially daily for 2 weeks and then weekly to review the data.
Measures
The process measure was complete blood and other relevant tests and collection of reports by third day of admission in antenatal in-patients with diagnosis of anaemia, hypertension, and diabetes. Complete clinical workup was defined as < 2 required investigations pertaining to the medical condition pending on third day of admission and if 2 or more required investigations were pending, it was labeled as incomplete work-up i.e. either the tests were not sent or the reports were not collected or entered in the case records. Baseline data collection was done initially followed by data collection on the morning of third day of patient’s admission by making observations from first to the fourth week respectively.
Analysis
For initial two weeks, the team decided to hold meetings every morning after clinical rounds to review the data collected over last 24 h, then the frequency of meeting was decreased to twice a week. The baseline percentage of antenatal in-patients with complete clinical evaluation on day-3 of admission over 4 weeks was analysed. The root-cause analysis was done using the fishbone tool. Based on the inputs, several successive interventions were undertaken in the P-D-S-A cycle, outcome was measured and next intervention was planned. SQUIRE 2.0 guidelines were followed for standardizing the documentation of the improvement project [6].
Results
The baseline median percentage of antenatal in-patients with complete clinical evaluation by the third day of hospital admission was 28.5%, 16.7%, 37.5%, and 30% in week 1, 2, 3, and 4 respectively; the median being 29.2%. Hence, interventions in the form of P-D-S-A cycles were planned to improve this percentage for better patient care.
1st P-D-S-A Cycle
Intervention 1: Attaching the printed investigation sheet by staff nurse on-duty in case sheet of patients upon admission.
The first PDSA was undertaken in which the printed investigation sheet with lists of tests and space to enter the reports relevant to anaemia, hypertension, and diabetes were attached in all case sheets. It was decided that the staff nurse on duty would attach this sheet upon any new admission in the ward. The use of investigation sheets as checklist was then observed and data was collected over next 21 days. The median percentage of patients with complete evaluation as defined was 42.8%.
2nd P-D-S-A Cycle
Intervention 2: Sensitization of residents about the process of use of printed investigation sheets.
From the results of PDSA 1, it was observed that attaching the printed investigation sheet was not enough to bring about a change. Thus, to further improve quality of care, it was decided to sensitize residents in batches regarding the printed investigation sheets as the defined checklist, on frequent intervals as tutorials. This was further reinforced during daily ward rounds to use these checklists, rather than sending investigations based on memory and recall. The practise was then observed and data was collected over next 14 days. The median percentage of complete work in admitted in-patients pertaining to anaemia, hypertension, diabetes was 57%.
3rd P-D-S-A Cycle
Intervention 3: Re-sensitization of residents at the time of duty change over and modification in the printed investigation sheet (Fig. 1).
Fig. 1.
Printed investigation sheet used as checklist
It was noticed that there was a decline in the use of sheet as checklist at the first day of duty change-over at the beginning of each month. Thus, it was decided to re-sensitize the residents one day prior and on the day of duty change over in the maternity ward in the 3rd PDSA cycle. In addition, the printed investigation sheet was modified to avoid congestion as suggested by the residents. The practise was then observed and data was collected over next 14 days. The median percentage of complete clinical evaluation in admitted patients with anaemia, hypertension, diabetes was 75%. The three PDSA cycles have been depicted in Table 1 and the time series chart is depicted in Fig. 2.
Table 1.
Plan- Do –Study- Act cycle as implemented for QI initiative
| Plan | Do | Study | Act |
|---|---|---|---|
| PDSA 1: 21 days | |||
| Attaching the printed investigation sheets by staff nurse on duty in each case sheet of patient upon admission | 1. The printed investigation sheets were attached by staff nurse on duty in each case sheet of patient upon admission |
Lessons learnt: 1. This was useful but not enough as the use of these sheets as checklist and complete work-up was still low (Adapt the change Idea) |
|
| PDSA 2: 14 days | |||
| All residents should be oriented and sensitized about the process of use of printed investigation sheets |
1. Orientation of residents was done on the first day of joining the ward 2. Teaching about the relevant investigations of medical conditions at frequent intervals as tutorials in batches of few |
Lessons Learnt Adopt the change Idea: Effective change idea but long-term feasibility needs to assessed |
|
| PDSA 3: 14 days | |||
| The printed investigation sheet needed modification and re-sensitization of residents at the time of duty change over |
1. The printed investigation sheet was modified as it was too congested which posed difficulty in writing reports 2. Re-sensitization of residents one day prior and on the day of duty change over in the maternity ward was done |
Lessons learnt There was a positive response from the residents (Adopt the change idea) |
|
Fig. 2.
Run Chart depicting the baseline median (29%), the goal (80%), and progress of QI project i.e. percentage of patients with complete evaluation by day-3 of admission after starting plan-do-study-act (PDSA) cycles 1, 2 and 3
Discussion
A checklist is a simple tool that enumerates items which are to be confirmed as accomplished and does not rely on memory. It is a vital tool as it enlists the actions or tasks, needed to optimize patient outcome. The use of checklists in patient care has been remarkable since the World Health Organization (WHO) Surgical Safety Checklist which showed a clear reduction in both surgery-related mortality and post-operative infections. Human errors are common and could be caused by lack of concentration, lack of knowledge or experience, and training. However, it is believed that most commonly these errors in the health care are just slips and use of a standard checklist could reduce the number of slips. In our setting, the printed investigation sheets for obstetric in-patients already existed. However, they were not being used on a regular basis This often led to repeat sampling and incomplete clinical evaluation as the investigations would be sent on memory-recall basis and entered in case sheet without a pre-designed checklist. Thus, using the printed investigation sheets as customized checklist for the QI project avoided delay and also avoided repeat blood sampling. It also aided in patient care by avoiding delays in starting treatment and possibly reduced hospital stay. Additionally, there was a positive response from the residents as their work was simplified too, with a set of investigations already listed out related to hypertension, anaemia, and diabetes.
In the present QI initiative, a simple change idea led to the change of practise without any additional resources. This paper thus, recounts that we can improve care in maternity ward by using the QI tools and address a problem with teamwork in our own context.
The limitation was this practise being followed in maternity ward only, and not when admissions were made to labour room or private wards of the hospital. Once these patients were shifted from labour room to maternity ward, it was very difficult to convince the residents to replace the hand-written sheets with printed ones, once the former ones were already attached due to shortage of time. This was discussed as a future prospect and there was a positive response from residents. Many other change ideas suggested by the enthusiastic residents for the next QI projects include the use of these printed sheets for all the obstetric conditions meriting admission in the ward, also starting the use of these sheets in labour room and establish the use of growth charts for faetal growth monitoring in growth-restricted faetuses.
Conclusion
A simple change idea with the proper and systematic use of principles of quality improvement can bring about significant changes in the smooth day-to-day functioning in the wards and also improve patient care. Thus, despite limitations, these interventions may lead to change in practise in the maternity ward without any additional resources. With ongoing educational sessions and regular audits, these are likely to sustain and spread in other units/hospitals too.
Acknowledgments
We would like to acknowledge the support of Resident doctors of Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, New Delhi.
Funding
None.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This project was deemed an improvement study and local policy meant that ethical approval was not required.
Human or Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Not applicable (Direct data of patients was not analysed as it a quality improvement initiative).
Consent for Publication
Obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bergman B, Hellström A, Lifvergren S, et al. An emerging science of improvement in health care. Qual Eng. 2015;27(1):17–34. doi: 10.1080/08982112.2015.968042. [DOI] [Google Scholar]
- 2.Langley GJ, Moen R, Nolan KM, et al. The improvement guide: a practical approach to enhancing organizational performance. San Francisco: Jossey-Bass; 2009. [Google Scholar]
- 3.Plsek PE. Quality improvement methods in clinical medicine. Pediatrics. 1999;103((Supplement E1)):203–14. doi: 10.1542/peds.103.SE1.203. [DOI] [PubMed] [Google Scholar]
- 4.Society for Maternal-Fetal Medicine (SMFM) Bernstein PS, Andrew Combs C, Shields LE, et al. The development and implementation of checklists in obstetrics. Am J Obstet Gynecol. 2017;217(2):B2–B6. doi: 10.1016/j.ajog.2017.05.032. [DOI] [PubMed] [Google Scholar]
- 5.Janicki MB, Fernandez CG, Wakefield D, et al. Improving fetal congenital heart disease screening using a checklist-based approach. Prenat Diagn. 2020;40(2):223–231. doi: 10.1002/pd.5581. [DOI] [PubMed] [Google Scholar]
- 6.Ogrinc G, Davies L, Goodman D, et al. Standards for quality improvement reporting excellence 2.0 revised publication guidelines from a detailed consensus process. J Surg Res. 2016;200(2):676–82. doi: 10.1016/j.jss.2015.09.015. [DOI] [PubMed] [Google Scholar]