Abstract
Introduction and importance
Meckel's diverticulum (MD) is a common congenital anomaly of the digestive tract that affects around 4 % of the population. Although it is relatively common, diagnosis still remains very challenging; it requires an astute clinician with a high clinical index of suspicion to achieve the diagnosis. Once a diagnosis is reached, treatment is almost always surgical. This case report provides evidence of the effectiveness of a new robotic surgical system for resection of MD in the elderly.
Case presentation
61 year old male presented to the emergency room with recurrent hematochezia. After multiple diagnostic techniques, he was finally diagnosed with MD using Meckel's scan. After diagnosis, surgical resection using the Cambridge Medical Robotics (CMR) Versius robotic system was performed, which yielded good results.
Clinical discussion
This case highlights the use of a new robotic system for the treatment of Meckel's Diverticulum.
Conclusion
Our initial experience with the CMR Versius surgical system in small bowel resection was successful; however, further studies are needed to demonstrate the safety and efficacy of such a system.
Keywords: CMR, Versius surgical system, Meckel's diverticulum, Small bowel resection, Case report
Highlights
-
•
Meckel's diverticulum can persist in the elderly, thus ruling out the disease based on age is not reasonable.
-
•
Many diagnostic techniques can be used to investigate Meckel's diverticulum, however the most reliable is the Meckel's scan.
-
•
Once Meckel's is diagnosed surgical treatment is usually curative.
-
•
Small bowel resection can be done with this new robotic platform.
1. Introduction
Meckel's diverticulum (MD) is a congenital deformity affecting around 4 % of the general population [1]. MD occurs when the proximal portion of the omphalomesenteric duct is not completely obliterated, resulting in a fistula from the ileum to the umbilicus [2]. MD is the only true diverticulum that occurs in the small intestine; it usually follows the rule of two, meaning it occurs in 2 % of the population, two feet away from the ileocecal valve, approximately two inches long, may have two types of mucosal linings, 2 % are symptomatic, and it's twice as likely to occur in men rather than women [3]. MD is very hard to diagnose, and in most cases, it is usually an incidental finding during surgery. However, several risk factors such as a young age and symptoms such as colonic bleeding may sometimes elude the physician to believe that an individual may be suffering from MD [4], [5]. With that being said, MD does not exclusively occur in patients of younger age. Herein, we present the case of a sixty-one year old male with symptomatic MD that was successfully treated with small bowel resection using a new robotic system. Written consent was obtained from the patient and the report was composed in accordance with SCARE 2020 guidelines [6].
2. Case presentation
A sixty one year old male patient on aspirin (75 mg OD), atorvastatin (20 mg HS), metformin (1000 mg BID), sitagliptin (50 mg BID), Empagliflozin (2.5 mg OD), Carvedilol (12.5 mg BID), valsartan (80 mg BID), and prazosin (2.5 mg OD) with a history of CAD, HTN, Hyperlipidemia, T2DM, MI, Syncope, and recurrent rectal bleeding since the age of six. He has no pertinent family history and has undergone multiple colonoscopies for his recurrent rectal bleeding, as well as litigation of hemorrhoids and embolization of the inferior mesenteric artery.
The patient presented to a neighboring hospital experiencing bright red stools six times in the past twenty four hours. Upon admission, the physicians made sure his condition was stable and decided to admit him overnight with the plan of performing a sigmoidoscopy in the morning.
Come next day, the sigmoidoscopy was performed; it showed blood in the transverse colon with clots; however, the physicians were unable to complete the procedure due to reported vasovagal episodes with HTN and bradycardia. The patient was then admitted to the ICU where he received a fluid bolus and four units of blood. After admission into the ICU, the patient's family then decided to transfer him to our hospital.
Upon arrival, the patient's care was handled by the gastroenterology and general surgery departments. Their plan was to ensure the patient was stable, and then perform a colonoscopy. The patient was admitted overnight, and routine blood work was done, which revealed normal RBC, WBC, and Platelets (Table 1).
Table 1.
Admission laboratory results for the reported case.
| WBC (4 to 10 × 109/L) |
Hemoglobin (130–170 G/L) |
Platelets (150 to 410 × 109/L) |
CRP (<5 mg/L) |
Creatinine (59–104 umol/L) |
Sodium (136–146 mmol/L) |
|---|---|---|---|---|---|
| 8.3 × 109 | 112 | 166 × 109 | <1 | 71 | 143 |
| Potassium (3.5–5.1 mmol/L) |
Chloride (98–107 mmol/L) |
RBC (4.5 to 5.5 × 1012/L) |
Thrombin time (11–18 s) |
Prothrombin time (9.4–12.5 s) |
Glucose (3.9–6.0) |
|---|---|---|---|---|---|
| 3.9 mmol/L | 104 | 4.39 | 14.9 s | 12.8 s | 5.6 |
WBC: white blood cells; CRP: C-reactive protein; RBC: red blood cells.
The next day physical examination revealed stable vital signs with a soft, non-tender abdomen with positive bowel sounds and no mass or organomegaly. Following physical examination, a colonoscopy was performed, which revealed some patchy erythema and erosions in the upper rectum. After the colonoscopy, the GI team decided to perform a capsule endoscopy which revealed a small arteriovenous malformation in the proximal small bowel.
Following these investigations, physicians suspected that the patient might be suffering from MD. Due to the high index of clinical suspicion, a Meckel's scan was performed.
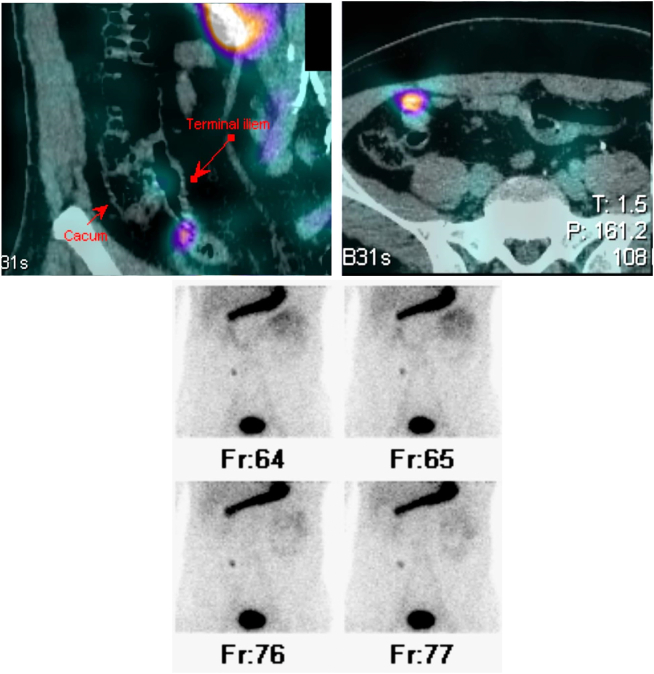
Meckel's scan yielded a positive result (Fig. 1,1.1,1.2). The patient's care was then exclusively handled by the surgical department.
Figs. 1,1.1,1.2.
Results of the Meckel's scan. A small focal activity noted at the terminal ileum, about 60 cm from the ileocecal valve, is suggestive of Meckel's diverticulum.
After further discussion between the surgeon and the patient, a decision was made that the best course of action would be a robotic-assisted segmental resection of the small bowel, using the CMR Versius surgical system (Cambridge Medical Robotics, Cambridge, United Kingdom). The resection was done and histological findings confirmed Meckel's diverticulum with ectopic pancreatic tissue (Fig. 2). The patient recovered well, with no postoperative complications.
Fig. 2.
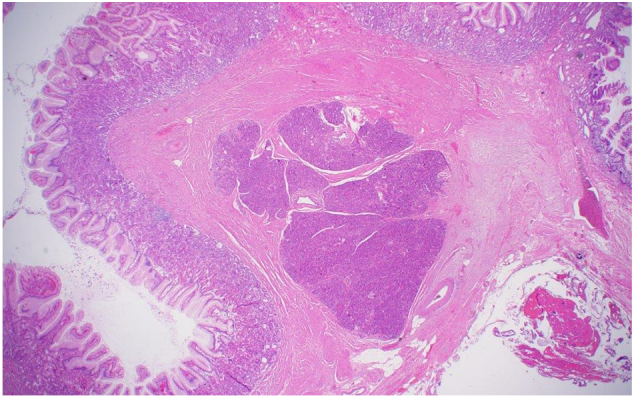
Histological image of Meckel's diverticulum.
Sections demonstrate a small intestinal mucosa with normal maturation. There is no evidence of dysplasia or adenomatous changes. Focally, there is a pancreatic tissue consisting of acini and ducts with a linear extension of a 3.6 mm involving the small intestinal wall associated with stromal fibrosis, serosal adhesions and subserosal congested blood vessels. No abnormal infiltrates or malignancy identified.
3. Discussion
Meckel's diverticulum (MD) is a relatively uncommon entity, as most cases are asymptomatic. A retrospective study by Soltero et al. determined that the lifetime risk for symptomatic MD occurrence is around 4 % [7]. Such symptoms may include obstruction, but the most common by far is gastrointestinal bleeding. Other uncommon complications may include neoplasia [8]. Symptomatic MD rarely progresses to adulthood, but when it does, it presents itself as a diagnostic challenge, as there are no clear-cut guidelines for the diagnosis of MD. An experienced clinician with a high index of suspicion is needed to properly diagnose MD.
Currently, common diagnostic modalities for MD may include fluoroscopy, CT, MRI, colonoscopy, and a Meckel's scan (nuclear medicine) [2]. Fluoroscopy is not very reliable as MD is often missed due to the complex structure of the overlying bowel. CT and MRI are also unreliable as an MRI does not have the resolution needed to make a distinctive diagnosis of MD, and a CT may often be misleading if no high index of clinical suspension is present, as most of the time, MD may be mistaken for a bowel loop. Colonoscopies are also unreliable due to the anatomy of Meckel's. It's usually located two feet from the ileocecal valve, which a colonoscopy cannot reach.
The most reliable diagnostic method for Meckel's diverticulum is known as a Meckel's scan. Technetium-99 pertechnetate is injected intravenously, which is then taken up by the ectopic gastric mucosa; this can effectively localize the area of MD. In our case, we saw that apart from the Meckel's scan, all other diagnostic methods failed; thus, we believe physicians should not rule out performing a Meckel's scan, due to the sole reason of old age.
Once MD is diagnosed, the definitive curative treatment for Meckel's diverticulum is surgery. The type of surgery done depends on the location and integrity of the ectopic tissue [9]. After assessment, two main procedures can be performed, a diverticulectomy or segmental resection [9]. In the case of our patient, we decided to perform a robotic-assisted laparoscopic segmental resection of the small bowel using the CMR Versius robotic system. Briefly, the CMR Versius surgical robot is a teleoperated robot surgical system that consists of four portable bedside units. The surgeon interacts with the four arms of the robot through two handheld controllers via feedback from an endoscopic camera that is able to project a high-definition three-dimensional display for the surgeon [10]. With regards to our case, to start off, the patient was placed in the Lithotomy position, three bedside surgical units for this procedure. One unit was placed between the legs and two units were placed to the left of the patient. Based on previous experience, we noticed that this is the best position to use to avoid clashing of the surgical arms, as well as provide some room for the surgical assistant at the bedside.
In total, four trocars that consisted of a blunt obturator with a balloon (Applied Medical, Rancho Santa Margarita, California, United states) were used; three were used for the Versius surgical system and one was used as an assistant port.
The first port for the Versius surgical system was placed in the anterior axillary line two inches above the umbilical line (5 mm). The second was placed in the anterior axillary line one inch below the umbilical line (10 mm, camera). The third trocar was placed in suprapubic region (5 mm). Finally, the assistant port was placed in the supraumbilical region (10 mm).
Once that was done, the surgeon was then able to enter the peritoneal cavity using the Versius robot. An area of the diverticulum was identified around 2 ft from the ileocecal valve with the area of inflammation and adhesions, this was thought to be the source of the bleeding. He was then able to mobilize and dissect through the adhesive bands and free the small bowel from its attachment. The left loop of the intestine was brought out through a small infraumbilical incision. An endo-GIA- 60 (Ethicon, Raritan, New Jersey, United States) was then used for small bowel resection, side to side anastomosis was carried out, and the enterotomy was closed using the same stapler. After that, the specimen was taken out by widening the supraumbilical incision (which was used for the assistant port), followed by the closure of the fascia with 0 vicryl. The patient successfully tolerated the procedure with no early postoperative complications. The surgeon opted for extraperitoneal resection as it allowed the procedure to be carried out faster, which was ideal in the case of our patient.
Although a segmental resection can be done laparoscopically, it is usually associated with complications such as hemorrhage or bowel obstruction. [11]. Due to this, our surgeon decided to use the system because of the better 3-dimensional view of the anatomy and the flexibility offered by the robotic arms, both of which allowed our surgeon to better approximate the extent of resection and maneuver easily in the confined space. This allowed for less complications and blood loss.
A recent study by Kelkar et al. demonstrates the safety and efficacy of the Versius surgical system in gallbladder surgery. They report that the platform allows for versatility in the operation room, flexible port placement, and better surgical dexterity [12]. These findings are in line with a previous report by Collins et al. [13]. Collins et al. also reports that the Versius is safe and feasible for colorectal surgery [13].
We can confirm that the Versius surgical system does allow for flexible port placement. It also provides better surgical dexterity when compared to the conventional laparoscopic approach.
The CMR Versius surgical system has recently been introduced as a new surgical platform. Due to the novelty of the system, our first goal was to surpass the learning curve by performing basic procedures (gallbladder surgery and inguinal hernia repair) for the first fifty cases. By doing this, we were able to perfect port placement, patient positioning, and surgical technique before moving on to more complex procedures. With this being our fifty first case, we were able to demonstrate that complex surgery with the Versius surgical system is also possible.
To our knowledge, this is the first report that demonstrates a successful outcome with performing a small bowel segmental resection using the CMR Versius robot.
4. Conclusion
Although MD is the most common congenital anomaly of the GI tract, it is relatively rare in adults. Due to this, MD presents itself as a diagnostic challenge, a high index of clinical suspension is needed to accurately identify the complications of MD in the elderly population. However, once diagnosed, prompt surgical treatment is usually curative. This report shows that small bowel resection with the CMR Versius surgical system is possible; however, more extensive studies are needed to determine the safety of such a system.
5. Patient perspective
The patient was satisfied with both the operative outcomes as well as the team management. The patient follow up was done for a total of three times. The first time was two weeks post op, the second time was six weeks post op, and finally the last follow up was twelve weeks post op. At each follow up the patient was fine, and no complications were noted; the patient remains asymptomatic.
Abbreviations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Ethical approval was obtained from the American Hospital Dubai IRB.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
MH: Data collection and Manuscript Writing. GA: Manuscript Writing. MZ: Manuscript Review. HM: Conception and design of the study, manuscript review.
Research registration
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Guarantor
Hatem Moussa, MD.
Declaration of competing interest
HM is a proctor for Intuitive Surgical and CMR Surgical. MZ is a board member of the Academic Medical Professionals Insurance Risk Retention Group and is a consultant for Mohamed & Obaid Almulla group of companies LLC. MH and GA have no competing interests to declare.
References
- 1.Levy A.D., Hobbs C.M. From the archives of the AFIP. Meckel diverticulum: radiologic features with pathologic correlation. Radiographics. 2004;24:565–587. doi: 10.1148/rg.242035187. [DOI] [PubMed] [Google Scholar]
- 2.Kuru S., Kismet K. Meckel’s diverticulum: clinical features, diagnosis and management. Rev. Esp. Enferm. Dig. 2018;110:726–732. doi: 10.17235/reed.2018.5628/2018. [DOI] [PubMed] [Google Scholar]
- 3.Hansen C.C., Søreide K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine (United States) 2018;97 doi: 10.1097/MD.0000000000012154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park J.J., Wolff B.G., Tollefson M.K., Walsh E.E., Larson D.R. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950–2002) Ann. Surg. 2005;241:529–533. doi: 10.1097/01.sla.0000154270.14308.5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kusumoto H., Yoshida M., Takahashi I., Anai H., Maehara Y., Sugimachi K. Complications and diagnosis of Meckel’s diverticulum in 776 patients. Am. J. Surg. 1992;164:382–383. doi: 10.1016/S0002-9610(05)80909-2. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Soltero M.J., Bill A.H. The natural history of Meckel’s diverticulum and its relation to incidental removal. A study of 202 cases of diseased Meckel’s diverticulum found in King County, Washington, over a fifteen year period. Am. J. Surg. 1976;132:168–173. doi: 10.1016/0002-9610(76)90043-X. [DOI] [PubMed] [Google Scholar]
- 8.Choi S.Y., Hong S.S., Park H.J., Lee H.K., Shin H.C., Choi G.C. The many faces of Meckel’s diverticulum and its complications. J. Med. Imaging Radiat. Oncol. 2017;61:225–231. doi: 10.1111/1754-9485.12505. [DOI] [PubMed] [Google Scholar]
- 9.Blouhos K., Boulas K.A., Tsalis K., Barettas N., Paraskeva A., Kariotis I., Keskinis C., Hatzigeorgiadis A. Meckel’s diverticulum in adults: surgical concerns. Front. Surg. 2018;5:3–6. doi: 10.3389/fsurg.2018.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puntambekar S.P., Rajesh K.N., Goel A., Hivre M., Bharambe S., Chitale M., Panse M. Colorectal cancer surgery: by Cambridge medical robotics versius surgical robot system—a single-institution study. Our experience. J. Robot. Surg. 2021 doi: 10.1007/s11701-021-01282-9. [DOI] [PubMed] [Google Scholar]
- 11.Zani A., Eaton S., Rees C.M., Pierro A. Incidentally detected meckel diverticulum: to resect or not to resect? Ann. Surg. 2008;247:276–281. doi: 10.1097/SLA.0b013e31815aaaf8. [DOI] [PubMed] [Google Scholar]
- 12.Kelkar D.S., Kurlekar U., Stevens L., Wagholikar G.D., Slack M. An early prospective clinical study to evaluate the safety and performance of the versius surgical system in robot-assisted cholecystectomy. Ann. Surg. 2022 doi: 10.1097/sla.0000000000005410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collins D., Paterson H.M., Skipworth R.J.E., Speake D. Implementation of the versius robotic surgical system for colorectal cancer surgery: first clinical experience. Color. Dis. 2021;23:1233–1238. doi: 10.1111/codi.15568. [DOI] [PubMed] [Google Scholar]