Abstract
Introduction and importance
Caudal epidural block has been commonly practiced in recent years and is used for management of pain before surgery and chronic back pain in adult spine diseases.
Case presentation
A 58-year-old man visited the outpatient clinic complaining of recently aggravated severe low back pain, saddle anesthesia, and unbearable radiating pain in his left leg, with a previous history of caudal epidural block. He had problems with bladder and bowel function. Emergency exploration for cauda equina syndrome (CES) was performed. Decompression, extradural herniation, and entrapment of a cauda equina filament through a dural defect were observed, and surgical reduction with dural repair was performed.
Clinical discussion
The clinical signs at onset suggested cauda equina dysfunction after caudal epidural block. Magnetic resonance imaging showed spinal canal stenosis with a paracentral herniated intervertebral disc at the L4-L5 level without any other dural or nerve root abnormality. Exploration was the only option to identify the lesion.
Conclusion
This is the first case report of CES caused by extradural nerve root herniation and strangulation after caudal epidural block.
Abbreviations: CEB, caudal epidural block; CES, cauda equina syndrome; LEB, lumbar epidural block; MRI, magnetic resonance imaging
Keywords: Caudal epidural block, Complication, Cauda equina syndrome, Nerve root herniation
Highlights
-
•
The patient had cauda equina syndrome after previous caudal epidural block history.
-
•
Extradural herniation and entrapment of cauda equina filament was observed.
-
•
First identified case of delayed cauda equina syndrome after caudal epidural block
1. Introduction
Caudal epidural block (CEB) is widely used for anesthesia in pediatric surgeries and alleviates chronic pain from spinal stenosis or herniated discs in adults [1].
Significant complications of CEB, such as vasovagal reaction, post-dural puncture, epidural abscess, epidural hematoma, post-dural puncture headache, subdural injection, pneumocephalus, and air embolism, occur infrequently when the procedure is performed correctly. Minor complications, including back pain, headache, and nausea, are mostly transient, without residual morbidity [2], [3].
Several authors have reported cauda equina syndrome (CES) after lumbar epidural block (LEB) [4], [5], [6]. In contrast, only one case of CES after CEB, presumably due to mechanical compression by the injected solution, has been reported [7]. Another study reported a case of nerve root herniation secondary to repetitive lumbar puncture [8].
Nevertheless, to date, CES after CEB has presented with extradural nerve root herniation, and entrapment has not yet been reported. In this report, we describe a case of delayed-onset CES with nerve root incarceration that occurred after CEB, along with a review of the literature. This article has been written according to the SCARE criteria described by Agha et al. for the SCARE group [9].
2. Presentation of case
This case study was approved by the Institutional Review Board of Sanggye Paik Hospital (SGPAIK 2021-12-002), and written informed consent was obtained from the patient for publication of this case report and the accompanying images. A 58-year-old man visited the outpatient clinic with complaints of radiating pain in his left lower extremity and saddle anesthesia, which started three days before the visit. The patient denied any history of invasive intervention or trauma, except for a single procedure of CEB performed in another hospital eight weeks ago for spinal stenosis. Initially, he experienced partial relief of his symptoms after CEB; however, lower back pain with radiating pain in the left lower leg recurred one week before the outpatient clinic visit, just after he worked intensively as a landscaper. In addition, three days before his visit, he began experiencing a tingling sensation in the perineal area, followed by a deterioration in all sensations on the day before he visited our clinic (Fig. 1).
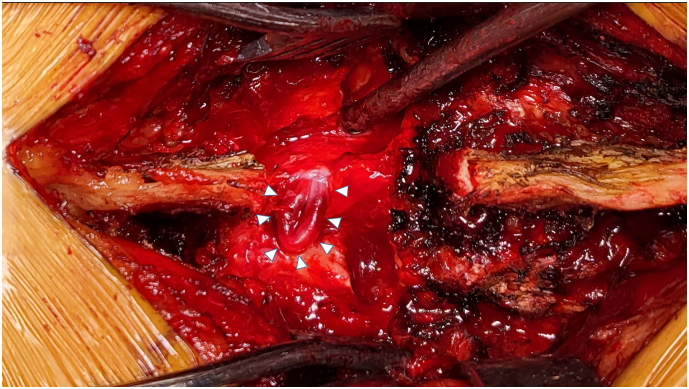
Fig. 1.
Cauda equina filament herniated and entrapped through a dural defect, which showed incarcerated and edematous hyperemic changes (arrow head).
At the initial visit, the patient experienced difficulty in walking due to radiating pain and saddle anesthesia. On physical examination, the straight leg raising test showed positive results in his left leg, along with a decreased motor function. His left tibialis anterior muscle, extensor hallucis longus muscle, and flexor hallucis longus showed weakened motor power of grades IV, III, and III, respectively (Fig. 2).
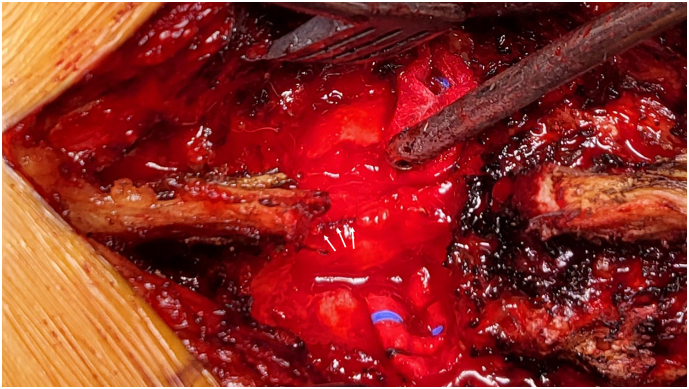
Fig. 2.
After the incarcerated root reduced back, The dural defect was repaired by continuous nylon suturing (arrow).
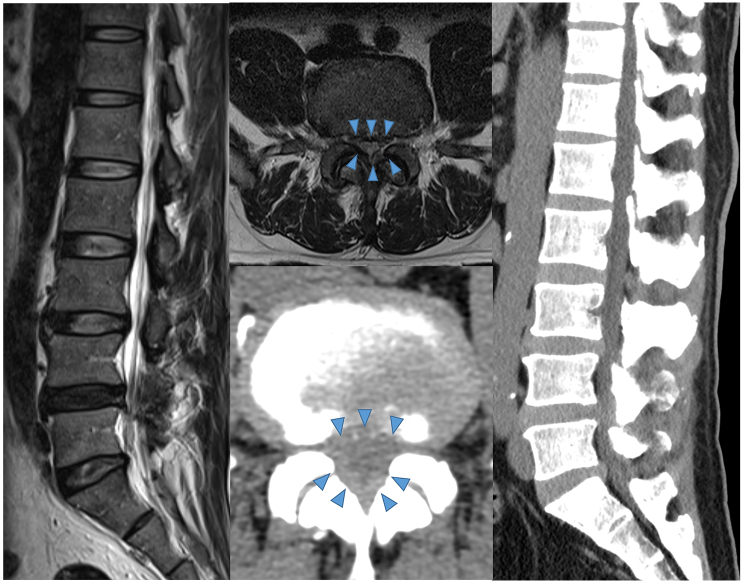
Bulging of multiple lumbar intervertebral discs and mild dural sac indentation due to herniated intervertebral disc at the L4–5 level was revealed on emergency magnetic resonance imaging (MRI), but no definitive lesion indicative of CES was found. Urinary bladder dysfunction was observed, with presence of >300 mL of residual urine through a transurethral catheter (Fig. 3).
Fig. 3.
No apparent abnormalities other than stenosis as detected on MRI and CT before surgery (arrow head).
Surgical exploration was performed to evaluate the clinically diagnosed CES. During left laminectomy, extradural herniation of the nerve root was observed just beneath the ligamentum flavum. After resection of the ligamentum flavum and posterior structures with appropriate care to avoid nerve root injury, the cauda equina was found to have herniated and become entrapped through a dural defect at the L4-L5 level. The incarcerated cauda equina filaments were edematous and hyperemic. The herniated nerve root could not be reduced back into the dural sac with a blunt probe because of a partially healed dural defect. After additional durotomy of approximately 2 mm to lengthen the defect, followed by neurolysis, the incarcerated root could be reduced. The dural defect was repaired by continuous suturing with nylon, and no cerebrospinal fluid leakage was found on Valsalva maneuver. Posterior decompression with discectomy, interbody fusion, and posterior instrumentation at the L4–5 level were performed.
Postoperatively, immediate partial relief of the radiating pain in the left lower leg was obtained. Intravenous dexamethasone injection was continued until postoperative day 3. The patient complained of a remnant perineal sensory decrease, for which pregabalin 75 mg was administered orally twice a day. On postoperative day 4, the urinary catheter was removed, and the patient could urinate spontaneously without any difficulties. On the twelfth day postoperatively, the patient could ambulate freely with near-complete resolution of the radiating pain; however, saddle anesthesia remained partially until the follow-up visit to our clinic at six weeks after the surgery.
3. Discussion
CES is a neuropathy caused by the compression of multilevel cauda equina filaments below L1, resulting in various symptoms including lumbar back pain, radiating pain to the lower extremities, motor decrease, saddle anesthesia, and difficulty in urination and defecation. It is a surgical emergency, and perineal sensory loss or bulbocavernosus dysfunction is closely related to a poor prognosis. Early diagnosis and surgical intervention are critical to prevent permanent nerve damage [10], [11].
Reports of CES after epidural block can be found in several studies, and CES mainly occurs immediately after injection of the drug mixture or within a few days after the procedure. The development of CES after LEB can be explained by meningitis, osmotic pressure, direct toxicity of injected drugs, injury due to intradural or intraneural injection, mechanical compression due to spinal stenosis, or hematoma [4], [5], [6]. A case of CES after CEB has been reported by Wibowo et al. However, it differs from the current case with respect to the mechanism of extradural nerve root herniation [7].
Extradural herniation of the nerve root can be caused by vertebral fractures [12], [13] or intra-operative injury of the dura mater, such as in laminectomy, discectomy, and posterior spinal fusion, although the overall incidence is known to be low [14], [15], [16]. According to previous reports, dural injuries are minimal, as no cerebrospinal fluid leakage is found intraoperatively, and often can be neglected and can lead to herniation of the arachnoid mater and cauda equina filaments due to the increased intra-abdominal and intradural pressure during extubation. Similar to bowel incarcerations in the abdominal area, the herniated roots can be entrapped at the opening of the dural defect, and unreduced filaments can become incarcerated [15], [16]. Nakayama et al. and Matsumoto et al. also reported that minor dural injury from a drainage or suction tube could cause nerve root herniation and entrapment [17], [18]. Furthermore, Hasegawa et al. reported a case of nerve root herniation occurring after repetitive lumbar puncture for myelography in a spinal stenosis patient [8]. However, the literature review showed no such case of delayed-onset CES by extradural nerve root herniation and entrapment after CEB as in this patient. In this case, we hypothesized that CEB causes delayed CES after the procedure; after the dural injury, a part of the cauda equina did not come out immediately, but it is thought that the filament came out after time elapsing due to Valsalva pressure.
Radiographically, in most cases of nerve root herniation, pseudo-meningocele or herniated nerve root per se was visualized by MRI or on a myelogram [16], [19]. In contrast, in our case, definitive cauda equina filament herniation was not found by MRI, probably because of the narrow space below the lamina, which made this case more complicated.
The authors assumed that unrecognized minimal dural injury from the initial CEB resulted in nerve root herniation, which was aggravated by the patient's occupational activity, and finally caused delayed-onset CES. However, considering the gap between the onset of symptoms and suspected injury from CEB, the exact cause and course of disease progression cannot be elucidated.
4. Conclusions
This is the first case report of CES caused by extradural nerve root herniation and strangulation after caudal epidural block. When a patient complains of neurological symptoms that can be clinically diagnosed as CES after minimally invasive procedures of the lumbosacral area, surgical exploration should be performed even in the absence of radiographic evidence, considering the devastating outcomes of untreated CES.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Institutional review board of Sanggye Paik Hospital, Inje University with waived informed consent (SGPAIK2021-12-002).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Guarantor
Dong-Ju, Lim.
Research registration number
Registered - researchregistry8296.
CRediT authorship contribution statement
Dong-Ju, Lim – study concept, design, writing the paper and data interpretation.
Hyung-Tae, Kim - data collection, data analysis.
Declaration of competing interest
None.
References
- 1.Kao S.C., Lin C.S. Caudal epidural block: an updated review of anatomy and techniques. Biomed. Res. Int. 2017;2017:9217145. doi: 10.1155/2017/9217145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Botwin K.P., Gruber R.D., Bouchlas C.G., Torres-Ramos F.M., Hanna A., Rittenberg J., et al. Complications of fluoroscopically guided caudal epidural injections. Am. J. Phys. Med. Rehabil. 2001;80:416–424. doi: 10.1097/00002060-200106000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Goodman B.S., Posecion L.W., Mallempati S., Bayazitoglu M. Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr. Rev. Musculoskelet. Med. 2008;1:212–222. doi: 10.1007/s12178-008-9035-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seo Y.T., Kong H.H., Lee G.J., Bang H.J. Persistent cauda equina syndrome after caudal epidural injection under severe spinal stenosis: a case report. J. Pain Res. 2017;10:1425–1429. doi: 10.2147/JPR.S134636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merino-Urrutia W., Villagrán-Schmidt M., Ulloa-Vásquez P., Carrasco-Moyano R., Uribe A., Stoicea N., et al. Cauda equina syndrome following an uneventful spinal anesthesia in a patient undergoing drainage of the Bartholin abscess: a case report. Medicine (Baltimore) 2018;97 doi: 10.1097/MD.0000000000010693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bilir A., Gulec S. Cauda equina syndrome after epidural steroid injection: a case report. J. Manip. Physiol. Ther. 2006;29(492):e1–e3. doi: 10.1016/j.jmpt.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Wibowo H.A., Rhatomy S. Cauda equina syndrome after caudal epidural sacral injection in severe lumbar spinal stenosis: case report. Int. J. Surg. Case Rep. 2020;77:12–14. doi: 10.1016/j.ijscr.2020.10.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasegawa K., Yamamoto N. Nerve root herniation secondary to lumbar puncture in the patient with lumbar canal stenosis. A case report. Spine. 1999;24:915–917. doi: 10.1097/00007632-199905010-00015. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.McLaren A.C., Bailey S.I. Cauda equina syndrome: a complication of lumbar discectomy. Clin. Orthop. Relat. Res. 1986;204:143–149. [PubMed] [Google Scholar]
- 11.Shephard R.H. Diagnosis and prognosis of cauda equina syndrome produced by protrusion of lumbar disk. Br. Med. J. 1959;2:1434–1439. doi: 10.1136/bmj.2.5164.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brant-Zawadzki M., Jeffrey R.B., Jr., Minagi H., Pitts L.H. High resolution CT of thoracolumbar fractures. AJR Am. J. Roentgenol. 1982;138:699–704. doi: 10.2214/ajr.138.4.699. [DOI] [PubMed] [Google Scholar]
- 13.Keenen T.L., Antony J., Benson D.R. Dural tears associated with lumbar burst fractures. J. Orthop. Trauma. 1990;4:243–245. doi: 10.1097/00005131-199004030-00001. [DOI] [PubMed] [Google Scholar]
- 14.Pavlou G., Bucur S.D., van Hille P.T. Entrapped spinal nerve roots in a pseudomeningocoele as a complication of previous spinal surgery. Acta Neurochir. 2006;148:215–219. doi: 10.1007/s00701-005-0696-y. discussion 219–20. [DOI] [PubMed] [Google Scholar]
- 15.Kothbauer K.F., Seiler R.W. Transdural cauda equina incarceration after microsurgical lumbar discectomy: case report. Neurosurgery. 2000;47:1449–1451. [PubMed] [Google Scholar]
- 16.Kamali R., Naderi Beni Z., Naderi Beni A., Forouzandeh M. Postlaminectomy lumbar pseudomeningocele with nerve root entrapment: a case report with review of literature. Eur. J. Orthop. Surg. Traumatol. 2012;22:57–61. doi: 10.1007/s00590-011-0934-3. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto T., Okuda S., Haku T., Maeda K., Maeno T., Yamashita T., et al. Neurogenic shock immediately following posterior lumbar interbody fusion: report of two cases. Global Spine J. 2015;5:e13–e16. doi: 10.1055/s-0034-1395422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakayama Y., Ohta H., Matsumoto Y. Reports of two cases for dural tear due to drainage tube after lumbar spinal surgery. Seikei Geka Saigaigeka. 2013;62:261–265. [Google Scholar]
- 19.Shu W., Wang H., Zhu H., Li Y., Zhang J., Lu G., et al. Nerve root entrapment with pseudomeningocele after percutaneous endoscopic lumbar discectomy: a case report. J. Spinal Cord Med. 2020;43:552–555. doi: 10.1080/10790268.2018.1507802. [DOI] [PMC free article] [PubMed] [Google Scholar]