Abstract
Introduction
In May 2007, the Trans-Atlantic Inter-Society Consensus document on peripheral arterial disease management (TASC II) was released. These guidelines were developed to assist in the rational choice of open or endovascular approaches to aortoiliac disease.
Case presentation
A 46-year-old woman was referred to the accident and emergency department, presenting with the chief complaint of pain in the left leg during activity. The pain had reduced after 10 min of resting before the time of admittance. Furthermore, there was weakness and sensory loss in the left leg; however, ulcers or gangrene were not found in the distal area. In addition, the left femoral pulse was not palpable, with ankle-brachial indices (ABIs) of 1.11 and 0 for the right and left, respectively. A computed tomography (CT) angiography of the aorta and lower limbs was requested. The findings were consistent with total occlusions from the distal portion of the aorta to the left common iliac artery, with atherosclerosis of the abdominal aorta (aortoiliac lesions type D TASC II classification). Subsequently, bypass grafting was performed immediately after revascularization with the femorofemoral artery. There were no post-operative sequelae, and the patient was admitted to the hospital for wound care.
Conclusion
Patients with aortoiliac occlusive disease are at risk of limb loss when revascularization is not performed and have an increased risk of cardiovascular events. The use of femorofemoral artery bypass grafting as a surgical technique had a high success rate, resulting in good perfusion to the lower extremities during a single operation.
Keywords: Aortoiliac occlusive disease, Bypass graft, Femoral artery, TASC II type D, Case report
Highlights
-
•
Endovascular treatment has often been recommended for the extensive disease of the common and external iliac arteries.
-
•
Patients with aortoiliac occlusive disease are at risk of limb loss when revascularization is not performed.
-
•
They also have an increased risk of cardiovascular events.
-
•
The use of femorofemoral artery bypass grafting as a surgical technique had a high success rate.
1. Introduction
In 1950, the first aortic reconstruction for aortoiliac occlusive disease (AIOD), also known as Leriche syndrome, was performed by Jacques Oudot in France through a retroperitoneal approach using a homograft [1]. Axillofemoral and femorofemoral artery grafting were introduced to provide inflow procedures for unilateral iliac disease, respectively [2].
In May 2007, the Trans-Atlantic Inter-Society Consensus document on peripheral arterial disease management (TASC II) was released. These guidelines were developed to help in the rational choice of open or endovascular approaches to aortoiliac disease [3,4]. Endovascular therapy is currently the treatment of choice for type A lesions and the most often utilized method for type B lesions. For type C lesions, surgical treatment has been recommended more often for the extensive disease of the external iliac or bilateral occlusions of the common iliac. Similarly, for type D lesions, surgery has been the treatment choice for the extensive disease of the common and external iliac arteries. However, endovascular treatment has documented many successes, even for TASC C and D lesions [5].
The typical indications for AIOD were intermittent claudication (IC), resting pain, threatened limb viability, tissue-loss that manifested as non-healing ulcers, and/or frank gangrene. Furthermore, pain while at rest and threatened limb viability implied extensive disease of the deep femoral artery or the femoropopliteal segments [6,7]. Research has found that the prevalence of IC rose from about 1 % in patients under the age of 60 years to 3 %–8 % in those over the age of 70 years [8]. Claudication was more common in men in younger age groups. However, there was a minimal difference between men and women as they aged [7]. Following the 2020 Surgical Case Report guidelines [9], we report the successful case of woman with the aortoiliac occlusive disease who required femorofemoral bypass surgery.
2. Case presentation
A 46-year-old woman was referred to the accident and emergency department (A&E), presenting with a chief complaint of pain in the left leg during activity. The pain reduced after 10 min of resting in the period of time before admittance. Furthermore, the pain was commonly localized in the thigh and buttocks. The patient sometimes experienced muscle fatigue, aches, and cramping on exertion, which could be relieved by resting. There was also a history of balloon angioplasty that had been performed once at the referral hospital by the cardiothoracic department. However, the patient complained of a thickness of the left leg and a small amount of pain after the ballooning. There was no history of trauma or another infection. In addition, there were no complaints of chest tightness, pain, or pounding. The patient had a history of hypertension and diabetes mellitus but not of smoking or alcoholism (Fig. 1).
Fig. 1.
Clinical presentation of left lower extremities.
Vital sign examination showed high blood pressure, and physical examinations were within normal limits. Normal perfusion was found when the right inferior limb was palpated. The results from examinations of the sensation of pulse and saturation are shown in Table 1, Table 2, Table 3.
Table 1.
Local status of the inferior limb.
| Characteristics | Right | Left |
|---|---|---|
| Ulcers | – | – |
| Active bleeding | – | – |
| Edema | – | – |
| Hematoma | – | – |
| Color | – | – |
| Deformities | – | – |
| Sensation of pain | – | – |
| Crepitation | – | – |
| Temperature | Warm | Cold |
| Pus | – | – |
Table 2.
Vascular status of the inferior limb.
| Inferior limb arteries | Right | Left |
|---|---|---|
| Femoral artery | ++ | – |
| Popliteal artery | ++ | – |
| Anterior tibialis artery | ++ | – |
| Posterior tibialis artery | ++ | – |
| Dorsalis pedis artery | ++ | – |
| Capillary refill time | <3 s | >3 s |
| Ankle-brachial index | 1.11 | 0 |
Table 3.
Blood Oxygen Saturation (spO2) in the inferior limb.
| spO2 inferior limb | Right | Left |
|---|---|---|
| Digit I | 98 % | Difficult to evaluate |
| Digit II | 97 % | Difficult to evaluate |
| Digit III | 99 % | Difficult to evaluate |
| Digit IV | 97 % | Difficult to evaluate |
| Digit V | 98 % | Difficult to evaluate |
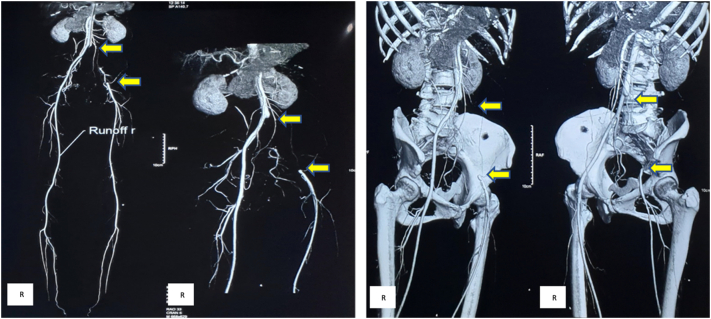
The laboratory tests showed an elevation in blood glucose levels. The chest X-ray showed cardiomegaly with mild vascular dilatation at suprahilus. The echocardiogram report showed moderate-to-severe regurgitation, mild mitral stenosis, severe tricuspid regurgitation, mild pulmonary regurgitation. Left atrium (LA), right atrium (RA), and right ventricle (RV) dilatation, and a normal left ventricle (LV) systolic function ejection fraction (EF) of 58 % were shown. Duplex ultrasonography of the lower extremities showed a large thrombus in the lumen of the left common femoral artery. This would have caused total occlusion to the distal left lower extremities. Before femorofemoral bypass, computed tomography (CT) angiography results showed a total occlusion from the distal portion of the aorta to the left common iliac artery, with atherosclerosis of the abdominal aorta (Fig. 2). The aortoiliac lesion showed the Type D TASC II classification.
Fig. 2.
CT scan angiography pre-operative showed a total occlusion from the distal portion of the aorta to the left common iliac artery (arrow).
In terms of the coronavirus 2019 (COVID-19) assessment, a chest X-ray revealed no ground-glass opacity, and RT-Polymerase Chain Reaction testing was negative.
Elective femorofemoral bypass surgery was conducted by Vascular Surgeon and resident surgeon, and a thrombus was obtained from the distal aorta to the left common iliac artery (Type D TASC II classification aortoiliac lesions). The bypass was conducted with a synthetic graft (diameter [D] 6 mm and length [L] 40 cm) from the right to the left femoral artery (Fig. 3). The patient was administered an intravenous broad-spectrum antibiotic (ceftriaxone 1 g every 12 h [q12hr]) for 6 days, along with intraoperative and post-operative systemic heparinization. In addition, an analgesic drug (ketorolac 30 mg q8hr) was administrated for 3 days when required. The patient orally received an antiplatelet agent (clopidogrel 75 mg q24hr), vasodilator agent (cilostazol 100 mg q12hr), and oral anticoagulation (simarc 2 mg q24hr). After surgery, a CT angiography was performed to evaluate the graft (Fig. 4). There were no post-operative sequelae, and the patient was admitted to the hospital for wound care. The patient was able to perform daily activities of living at 1-month post-operative
Fig. 3.
Intraoperative image femorofemoral artery bypass grafting (arrow).
Fig. 4.

CT Scan Angiography post-operative shows femorofemoral artery bypass grafting (arrow; L, left).
3. Discussion
AIOD is a type of peripheral arterial disease that affects the aorta and iliac arteries in the infrarenal region. AIOD, like other arterial disorders, obstructs blood flow to the distal organs by narrowing the lumen or embolization of plaques [10]. Furthermore, patients with AIOD may experience claudication, which is a more common presentation than tissue-loss or resting pain. Tissue-loss or resting pain indicates disease of the deep femoral artery or femoropopliteal segments with the aorta and iliac segments. Atherosclerosis is the most common cause of AIOD, with hypertension, high homocysteine levels, diabetes mellitus, cigarette smoking, and hyperlipidemia as contributing factors. Age, race, family history, and gender are all risk factors [11,12]. Large-vessel vasculitis, notably Takayasu arteritis, is another uncommon but important cause [10,13].
Historically, physical examinations have been accurate in these patients. A decreased femoral pulse indicated a common femoral disease or more proximal aortoiliac disease [14,15]. However, since the advent of the obesity epidemic, the accuracy of the physical examination of femoral pulses has been questioned [16]. Determination of wave patterns and ABI is necessary to localize the disease in aortoiliac and femoropopliteal segments. Generally, ABI examination is the initial screening test for the diagnosis of arterial diseases due to its low cost, reliability, and non-invasive nature. It is usually accurate in detecting the presence of AIOD and determining the degree of the disease [17,18]. The ABI score of 0 for the left femoral indicated severe arterial disease. With a tentative diagnosis of AIOD, the most commonly used modality to provide detailed information about the location and degree of stenosis was duplex ultrasonography and a CT angiogram. Furthermore, CT angiography showed the classification of type D TASC II was occlusion from the distal of the aorta to the left common iliac artery, with atherosclerosis of the abdominal aorta.
Revascularization is used to treat symptomatic lower-extremity ischemia, such as resting pain, claudication, gangrene or ulceration, and embolization causing blue-toe syndrome, as well as to restore and preserve inflow to the lower extremities in the presence of a pre-existing or planned distal bypass. This also includes obtaining access to more proximal vascular beds in preparation for invasive procedures. Several surgical revascularization approaches are available, including open surgery, endovascular and hybrid procedures. However, so far, there is no approach that is universally suitable for all patients with AIOD [19].
The standard of treatment, including bypass surgery and/or an endovascular approach in patients with AIOD, remains under debate. The TASC II guidelines [3,10] were developed to assist in the rational choice of an open or endovascular approach to aortoiliac disease in specific patients. Currently, endovascular therapy is the treatment of choice for type A lesions; it is also the most commonly used modality for type B. For type C lesions, surgical treatment is recommended due to the more extensive disease of the external iliac or bilateral occlusions of the common iliac. Similarly, for type D lesions, surgical treatment of choice is recommended for an extensive disease of the common and external iliac arteries. However, several successes have been documented with endovascular treatment, even for TASC C and type D lesions [16].
The CT angiography of this patient showed a good distal run-off status, despite the severe angiographic TASC D lesions. Furthermore, bypass surgery was applied more commonly in patients with complete occlusions. Open surgical femorofemoral revascularization in the left common iliac arteries showed good results. Patients with AIOD often require complete revascularization at all occlusion sites to renew blood flow. Furthermore, when it comes to formulating strategies, the anatomical distribution of arterial occlusive disease is the most important element owing to the link to therapeutic success [3,4].
Femorofemoral crossover grafting is considered to be a low-risk procedure, with operative mortality ranging from 0 % to 5 %. As with the iliofemoral graft, the procedure is considered when the affected limb has no inflow and the contralateral iliac and femoral vessels are free of disease [20]. The only contraindication is a large abdominal apron, which can affect the base of the graft, especially in the seated position. This approach does not involve an abdominal incision as the femoral arteries are exposed in the standard manner. Currently, a bucket-handle approach is recommended rather than an antegrade sigmoid-shape reconstruction. This is superior to the pubis at the subcutaneous level and uses expanded polytetrafluoroethylene (ePTFE) or polyester. A graft of at least 7–8 mm is usually preferred. However, the patency rate was no better than the initial rate, ranging from 60 % to 80 % at 5 years [21].
4. Conclusion
Patients with AIOD are at risk of losing a limb when revascularization is not performed with an increased cardiovascular event. Revascularization is necessary when the procedure can prevent limb loss and maintain ambulation and function. Medical therapy is focused on addressing the risk factors that contribute to atherosclerosis. Pre- and post-angiography is necessary in determining the etiology of graft success. It is important to exclude problems with proximal anastomosis. Furthermore, the use of femorofemoral artery bypass grafting as a surgical technique has high success and a low complication rate.
Sources of funding
No funding or sponsorship.
Ethical approval
The study is exempt from ethical approval in our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
Not applicable – single case report.
Guarantor
Mulawardi
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Mulawardi and Tom Christy Adriani: study concept and surgical therapy for this patient. Mulawardi, Tom Christy Adriani, and Jancung: Data collection and Writing-Original draft preparation. Mulawardi: senior author and the manuscript reviewer. Muhammad Faruk: Editing and Writing. All authors read and approved the final manuscript.
Declaration of competing interest
Nothing to declare.
Acknowledgment
None.
Contributor Information
Mulawardi, Email: mulawardivanbasten@yahoo.com.
Jancung, Email: dr.jancung@gmail.com.
Tom Christy Adriani, Email: tca2909@gmail.com.
Hendry Lie, Email: hendrylie666@gmail.com.
Muhammad Faruk, Email: faroex8283@gmail.com.
References
- 1.Liang H.-L., Li M.-F., Hsiao C.-C., Wu C.-J., Wu T.-H. Endovascular management of aorto-iliac occlusive disease (Leriche syndrome) J. Formos. Med. Assoc. 2021;120:1485–1492. doi: 10.1016/j.jfma.2020.10.033. [DOI] [PubMed] [Google Scholar]
- 2.E. Aboian, A.S. Rao, Extra-anatomic bypass in the management of the peripheral artery disease, in: Panvascular Med., Springer Berlin Heidelberg, Berlin, Heidelberg, 2015: pp. 3297–3320. doi: 10.1007/978-3-642-37078-6_137. [DOI]
- 3.Jaff M.R., White C.J., Hiatt W.R., Fowkes G.R., Dormandy J., Razavi M., Reekers J., Norgren L. An update on methods for revascularization and expansion of the TASC lesion classification to include below-the-knee arteries: a supplement to the inter-society consensus for the management of peripheral arterial disease (TASC II) Vasc. Med. 2015;20:465–478. doi: 10.1177/1358863X15597877. [DOI] [PubMed] [Google Scholar]
- 4.Amini A., Gordon I., Wilson S., Williams R.A. Noncompressible arteries correlate with increased cardiovascular mortality at 2 Years. Ann. Vasc. Surg. 2013;27:918–923. doi: 10.1016/j.avsg.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Cvetic V., Sagic D., Koncar I., Kovacevic V., Radmili O., Antonic Z., Lukic B., Aleksic N., Davidovic L., Radak D. Endovascular treatment of different types of iliac occlusions—Results from an observational study. PLoS One. 2019;14 doi: 10.1371/journal.pone.0222893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hardman R.L., Jazaeri O., Yi J., Smith M., Gupta R. Overview of classification systems in peripheral artery disease. Semin. Intervent. Radiol. 2014;31:378–388. doi: 10.1055/s-0034-1393976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teodorescu V.J., Vavra A.K., Kibbe M.R. Peripheral arterial disease in women. J. Vasc. Surg. 2013;57:18S–26S. doi: 10.1016/j.jvs.2012.10.115. [DOI] [PubMed] [Google Scholar]
- 8.Lakshmanan R., Hyde Z., Jamrozik K., Hankey G.J., Norman P.E. Population-based observational study of claudication in older men: the Health in Men Study. Med. J. Aust. 2010;192:641–645. doi: 10.5694/j.1326-5377.2010.tb03663.x. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Miguel D., Pagano D., Millham F.H., Roy G., Kadioglu H., Nixon I.J., Mukhejree I., McCaul J.A., Chi-Yong Ngu J., Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., De Wilde R.L., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Karanth V.K., Kasivisvanathan V., Mei Z., The S.C.A.R.E. Guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84(2020):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Wooten C., Hayat M., du Plessis M., Cesmebasi A., Koesterer M., Daly K.P., Matusz P., Tubbs R.S., Loukas M. Anatomical significance in aortoiliac occlusive disease. Clin. Anat. 2014;27:1264–1274. doi: 10.1002/ca.22444. [DOI] [PubMed] [Google Scholar]
- 11.Heaton J., Khan Y.S. Aortoiliac Occlusive Disease, StatPearls. 2022. https://www.ncbi.nlm.nih.gov/books/NBK559086/?report=classic [PubMed]
- 12.Valentine E.A., Ochroch E.A. Essentials Card. Anesth. Noncardiac Surg. Elsevier; 2019. Vascular surgery; pp. 313–339. [DOI] [Google Scholar]
- 13.Piazza M., Ricotta J.J., Bower T.C., Kalra M., Duncan A.A., Cha S., Gloviczki P. Iliac artery stenting combined with open femoral endarterectomy is as effective as open surgical reconstruction for severe iliac and common femoral occlusive disease. J. Vasc. Surg. 2011;54:402–411. doi: 10.1016/j.jvs.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 14.Gerhard-Herman M.D., Gornik H.L., Barrett C., Barshes N.R., Corriere M.A., Drachman D.E., Fleisher L.A., Fowkes F.G.R., Hamburg N.M., Kinlay S., Lookstein R., Misra S., Mureebe L., Olin J.W., Patel R.A.G., Regensteiner J.G., Schanzer A., Shishehbor M.H., Stewart K.J., Treat-Jacobson D., Walsh M.E. AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2016;135(2017):e686–e725. doi: 10.1161/CIR.0000000000000470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlton-Ouw K.M., Davies M.G., Lumsden A.B. In: Endovasc. Surg. Moore W.S., Ahn S.S., editors. Fourth, Elsevier; Philadelphia: 2011. Balloon angioplasty in aortoiliac arterial occlusive disease; pp. 261–270. [DOI] [Google Scholar]
- 16.Ye W., Liu C.-W., Ricco J.-B., Mani K., Zeng R., Jiang J. Early and late outcomes of percutaneous treatment of TransAtlantic Inter-Society Consensus class C and D aorto-iliac lesions. J. Vasc. Surg. 2011;53:1728–1737. doi: 10.1016/j.jvs.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Crawford F., Welch K., Andras A., Chappell F.M. Ankle brachial index for the diagnosis of lower limb peripheral arterial disease. Cochrane Database Syst. Rev. 2016;9:CD010680. doi: 10.1002/14651858.CD010680.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhat M., Parry A., Maqsood S., Ganie F. Utility of ankle brachial index in the diagnosis of peripheral arterial disease in a resource limited setting. Indian J. Vasc. Endovasc. Surg. 2022;9:22–26. doi: 10.4103/ijves.ijves_65_21. [DOI] [Google Scholar]
- 19.Zhou M., Huang D., Liu C., Liu Z., Zhang M., Qiao T., Liu C.-J. Comparison of hybrid procedure and open surgical revascularization for multilevel infrainguinal arterial occlusive disease. Clin. Interv. Aging. 2014:1595. doi: 10.2147/CIA.S66860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park K.-M., Park Y.-J., Kim Y.-W., Hyun D., Park K.B., Do Y.-S., Kim D.-I. Long term outcomes of femorofemoral crossover bypass grafts. Vasc. Spec. Int. 2017;33:55–58. doi: 10.5758/vsi.2017.33.2.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rychlik I.J., Davey P., Murphy J., O’Donnell M.E. A meta-analysis to compare Dacron versus polytetrafluroethylene grafts for above-knee femoropopliteal artery bypass. J. Vasc. Surg. 2014;60:506–515. doi: 10.1016/j.jvs.2014.05.049. [DOI] [PubMed] [Google Scholar]